Professional Documents
Culture Documents
Update On Acute Myeloid Leukemia Stem Cells New Di PDF
Uploaded by
Mini Bekti NingsihOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Update On Acute Myeloid Leukemia Stem Cells New Di PDF
Uploaded by
Mini Bekti NingsihCopyright:
Available Formats
Submit a Manuscript: http://www.wjgnet.
com/esps/ World J Stem Cells 2016 October 26; 8(10): 316-331
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1948-0210 (online)
DOI: 10.4252/wjsc.v8.i10.316 © 2016 Baishideng Publishing Group Inc. All rights reserved.
REVIEW
Update on acute myeloid leukemia stem cells: New
discoveries and therapeutic opportunities
Maximilian Stahl, Tae Kon Kim, Amer M Zeidan
Maximilian Stahl, Tae Kon Kim, Amer M Zeidan, Section of established in acute myeloid leukemia. Initial proof
Hematology, Department of Internal Medicine, Yale School of of the existence of leukemia stem cells (LSCs) was
Medicine, New Haven, CT 06510-3222, United States accomplished by functional studies in xenograft models
making use of the key features shared with normal
Author contributions: Stahl M and Zeidan AM wrote the first
draft of the manuscript; Stahl M, Kim TK and Zeidan AM edited hematopoietic stem cells (HSCs) such as the capacity
the manuscript. of self-renewal and the ability to initiate and sustain
growth of progenitors in vivo . Significant progress
Conflict-of-interest statement: Amer M Zeidan receives has also been made in identifying the phenotype and
Honoraria from Ariad, Pfizer, Incyte and Celgene. Maximilian signaling pathways specific for LSCs. Therapeutically, a
Stahl and Tae Kon Kim have no conflict of interests to declare for multitude of drugs targeting LSCs are in different phases
this article. of preclinical and clinical development. This review
focuses on recent discoveries which have advanced
Open-Access: This article is an open-access article which was
selected by an in-house editor and fully peer-reviewed by external our understanding of LSC biology and provided rational
reviewers. It is distributed in accordance with the Creative targets for development of novel therapeutic agents.
Commons Attribution Non Commercial (CC BY-NC 4.0) license, One of the major challenges is how to target the self-
which permits others to distribute, remix, adapt, build upon this renewal pathways of LSCs without affecting normal
work non-commercially, and license their derivative works on HSCs significantly therefore providing an acceptable
different terms, provided the original work is properly cited and therapeutic window. Important issues pertinent to the
the use is non-commercial. See: http://creativecommons.org/
successful design and conduct of clinical trials evaluating
licenses/by-nc/4.0/
drugs targeting LSCs will be discussed as well.
Manuscript source: Invited manuscript
Key words: Leukemia stem cells; Cancer stem cells;
Correspondence to: Amer M Zeidan, MBBS, Assistant Acute myeloid leukemia; Stem cell niche; Xenotrans
Professor, Section of Hematology, Department of Internal plantation; Plerixafor; NF-kB; C-X-C chemokine receptor
Medicine, Yale School of Medicine, 300 George Street, New type 4
Haven, CT 06510-3222, United States. amer.zeidan@yale.edu
Telephone: +1-203-2004363
Fax: +1-203-2002360 © The Author(s) 2016. Published by Baishideng Publishing
Group Inc. All rights reserved.
Received: May 23, 2016
Peer-review started: May 23, 2016 Core tip: Leukemia stem cell (LSC) directed therapy
First decision: July 6, 2016 targets: (1) Cell surface markers expressed on LSC:
Revised: August 11, 2016
CD33, CD44, CD123, CD47, etc. ; (2) Crucial pathways
Accepted: August 27, 2016
Article in press: August 29, 2016 for maintenance of their stemness: NF-κB, PI3K/
Published online: October 26, 2016 AKT/mTOR and bcl-2; and (3) Interactions between
LSC in the bone marrow niche: LSC mobilization with
granulocyte-colony stimulating factor and inhibition of
LSC homing to the bone marrow by interrupting the
C-X-C chemokine receptor type 4-CXCL12 and VCAM-
Abstract
VLA4 axis.
The existence of cancer stem cells has been well
WJSC|www.wjgnet.com 316 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
intrinsic (transcription factors and signaling pathways)
Stahl M, Kim TK, Zeidan AM. Update on acute myeloid
leukemia stem cells: New discoveries and therapeutic opportuni and extrinsic (host factors, tumor microenvironment
[10]
ties. World J Stem Cells 2016; 8(10): 316-331 Available from: and immune response) factors . In the cancer stem
URL: http://www.wjgnet.com/1948-0210/full/v8/i10/316.htm cell (CSC) model, a tumor follows the principles of
DOI: http://dx.doi.org/10.4252/wjsc.v8.i10.316 normal, healthy tissue development with a stem cell
at the top of the hierarchy, which gives rise to all
other cells in the tumor. In this model only these rare
population of CSCs are able to initiate tumor growth:
They possess self-renewal capacity and can be isolated
INTRODUCTION
from the bulk non-tumorigenic population. Importantly,
Despite extensive research efforts in myeloid malig both models appreciate the existence of a CSC but
nancies, minimal progress has been made in intro differ in their assessment what cells within the tumor
ducing new effective treatment strategies for acute can be CSCs. In the stochastic model CSCs are created
myeloid leukemia (AML) since the introduction of the randomly and every cell has the potential to be a CSC,
anthracycline-cytarabine combination chemotherapy whereas in the CSC model only a subset of cancer cells
regimens (known as 7 + 3) more than 40 years [11]
has the potential to behave like a stem cell .
[1]
ago . Despite achieving complete remission (CR) with Whether the stochastic model or the CSC model best
intensive induction chemotherapy in about 70% of reflects tumorigenesis/leukemogenesis, has significant
patients with AML, relapse is frequent and the rate of impact on how cancer/leukemia should be treated .
[10]
5-year disease free survival is only about 30%-40%. It In the stochastic model, the cells within a tumor are
has been long proposed that the high rate of relapse is relatively homogeneous in terms of genetic makeup
due to the persistence of a rare subset of malignant cells and function and therapy can be uniformly directed at
that are not effectively eliminated by current treatment the bulk of tumor cells. However, per the CSC model,
[2-4]
regimens, the so called leukemia stem cells (LSCs) . tumorigenic pathways might operate differently in
LSC were first identified but tumor cells with stem CSCs compared with the bulk cells and therapy must
cell-like behavior were later found to be also present specifically target the CSCs in order to be truly effective.
[5-9]
in a variety of solid tumors . LSC remain the best Most of the current targeted therapies against leukemia
studied and characterized cancer stem cell (CSC) due and cancer focuses on inhibiting the molecular drivers
to the easy accessibility of tumor tissue for (i.e., blood found in all cancer cells but do not necessarily target
and bone marrow) and the availability of a number CSCs .
[11]
of cell surface markers that allow their prospective
identification and isolation by flow cytometry followed
by assays to examine their function both in vitro and in BIOLOGY OF LSCS
[10]
vivo . This review will focus on the biology of LSC, the CSC characteristics
impact they have on current leukemia diagnosis and The definition of a LSC is adapted from normal HSC:
prognosis and treatment as well as future directions of It is a cell that possesses the capacity to self-renew, pro
[6]
leukemia therapy based on targeting LSC . liferates and gives rise to leukemic blasts, which are
morphologically homogeneous but biologically hetero
[12]
geneous . Apart from self-renewal potential, dor
CSC VS CLONAL EVOLUTION THEORY mancy/quiescence and a protective stem cell niche are
It is now well understood that not only tumors from shared characteristics between HSCs and LSCs.
different patients but also cells within a single tumor
are characterized by heterogeneity in terms of the Self-renewal capacity: As the definition of CSCs is
morphology, cell surface markers, genetic variations a functional definition, CSCs can thus only be defined
[11]
and response to therapy . Why there is significant experimentally by their ability to recapitulate the
variation in genetic and epigenetic abnormalities generation of a continuously growing tumor. Immuno
between different cells or locations within a tumor deficient mice, such as the non-obese diabetic/severe
despite the clonal origin of all tumor cells, is a question combined immunodeficiency (NOD/SCID) mouse
that has puzzled researchers for decades. There and newer generations of xenograft models, are used
are essentially two different explanations for this to functionally define human hematopoietic stem
fundamental problem of cancer biology: The hierarchy [13]
and progenitor cells as well as LSCs . Long-term
or CSC model vs the stochastic or clonal evolution repopulating cells, thought to be LSC are able to be
[6]
model . In the stochastic model, all cells in a tumor successfully engrafted in these mice over prolonged
have a similar biological function but are heterogeneous periods as well as in secondary recipients
[2,14]
. Bonnet et
[15]
(e.g., expression of cell surface markers) because of al in the John Dick laboratory isolated subpopulations
clonal evolution resulting in small but entirely random/ of cells from primary human AML bone marrow based
stochastic variations triggered by external and internal on their immunophenotype and xenotransplanted
factors based on Darwinian principles. Importantly, all them into NOD/SCID mice. It demonstrated that the
+ -
cells within the tumor have an equal sensitivity to both CD34 CD38 expressing sub-population of AML cells
WJSC|www.wjgnet.com 317 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
were capable of being serially transplanted in these limited amount of cell divisions and regenerate all cells in
[15,16] [33,34]
immunodeficient mice . Reflecting the emphasis on a tissue .
functional assessment, these cells were named as SCID Similarly, LSCs are quiescent, which explains the
leukemia-initiating cells (SL-IC) and are considered the difficulties to eradicate LSCs with standard chemo
equivalent of LSC. therapies that preferentially target rapid proliferating
[35-37]
cells .
Symmetrical vs asymmetrical cell division: Similar
to HSCs, LSCs have the ability to undergo symmetrical Key signaling pathways relevant for retaining
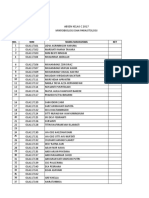
self-renewing cell division, generating identical daughter stemness: Similar signaling pathways involved in the
stem cells that retain self-renewal capacity (expansion), control of self-renewal of HSCs are also key elements
or an asymmetrical self-renewing cell division, resulting maintaining stemness in LSCs (Figure 1). Among many
[38]
in one stem cell and one more differentiated progenitor others, these pathways include PI3K/Akt/mTOR ,
[12,17-19] [39,40] [41,42] [43,44]
cell (maintenance) . Normal stem cells are able Wnt/beta-catenin , Hedgehog , NF-kB ,
[45] [46,47]
to switch between symmetrical and asymmetrical Notch and Bcl-2 . Several drugs targeting these
division based on the demands of the tissue they are pathways are in different stages of preclinical and
meant to maintain. During early embryogenesis normal clinical development (Figure 1).
stem cells undergo symmetrical cell division in order to
expand the total pool of stem cells giving rise to tissues Stem cell niche: The bone marrow niche is quintes
whereas in adult tissues stem cells give rise to mature sential for normal HSC to maintain their quiescence
[19,20]
cells though asymmetrical cell division . There is but at the same time enable HSC to generate cells in
[48]
increasing amount of evidence that in CSCs this delicate the blood stream to meet the organism’s needs .
balance seems to be disturbed in favor of symmetric cell The stem cell niche is formed by a complex network
[19,21,22]
division . For example, CSCs isolated from ERBB2- of different cells including vascular endothelial cells,
expressing breast cancer have been demonstrated to perivascular mesenchymal cells, megakaryocytes,
prefer symmetric cell division compared to normal breast osteoblastic lineage cells, macrophages and nerve
[23] [49-53]
tissue stem cells . Furthermore, the adenomatous cells . Dysregulation of the bone marrow niche plays
polyposis coli tumor suppressor gene (APC) has been an important role in preventing the detection of LSC
shown to paly a major role in regulating asymmetric cell by the immune system and protecting LSC from the
[48,54]
division in drosophila and its mutational loss is suspected effects of chemotherapy . Similar to normal HSCs,
to lead to an expansion of CSCs by symmetric cell LSCs are retained in the marrow niche by interactions
[22,24,25]
division . between CXCR4, on stem cells, and CXCL12 (SDF-1), on
osteoblasts and mesenchymal cells in the bone marrow
[55,56]
Stem cell quiescence and exhaustion: Normal stem niche . Chemokine interactions through CXCL12
cells need to be quiescent to avoid exhaustion of a stem can lead to up-regulation of vascular cell adhesion
[26]
cell pool and to minimize the risk of oncogenic events . molecule-1 (VCAM-1) and very late antigen-4 (VLA-4)
In fact, stem cell exhaustion has been described as one expression, which further strengthen LSC retention in
[57,58]
reason for aging and as a consequence of the attempt the marrow niche (Figure 1). The significance of
[27]
of the body to prevent the development of cancer . the interaction between LSCs and the protective bone
Aging leads to an accumulation of DNA damage in all marrow niche is exemplified by the fact that elevated
cells of the body, including stem cells, which in turn levels of CXCR4 and VLA-4 have been associated
leads to an increased risk of developing cancer. Aging with poor response to chemotherapy and decreased
[59-61]
stem cells are affected by sophisticated mechanisms survival . Several therapeutic approaches attempt
cells have developed to suppress the development of to break the dormancy of LSCs by induction of stem
cancer, mainly induction of senescence and apoptosis, cell cycling with granulocyte-colony stimulating factor
which are mediated through telomere shortening and (G-CSF) and inhibition of the CXCR4-SDF-1 axis
[28-30]
activation of tumor suppressor genes p16 and p53 . involved in LSC retention in the protective bone marrow
[62,63]
The diminished ability of aging HSC to reconstitute the niche (Figure 1).
hematopoietic system is demonstrated by prolonged
myelosuppression after cytotoxic chemotherapy in older Identification of LSCs by surface markers
patients as well as age of the stem cell donor being Recent studies have shown that LSCs may reside not
+ - + + -
significantly associated with overall and disease-free only in CD34 CD38 , but also in CD34 CD38 and CD34
[31,32] +
survival after hematopoietic stem cell transplant . CD38 compartments demonstrating the lack of a
[64-66]
However, normal stem cells are also required to definitive phenotype for LSCs . Several studies have
+ +
continuously replenish the cells that are lost in a tissue. shown that the CD34 CD38 fraction has repopulating
[18,67,68]
In order to fulfill both purposes-avoid exhaustion as well ability when immunosuppression is applied . It
as maintaining the cellular integrity of a tissue-stem cells was demonstrated that by treating mice with immuno
+ +
undergo asymmetric cell divisions, which give rise to suppressive antibodies, the CD34 CD38 fraction of
another stem cell as well as a rapidly dividing progenitor AML samples is able to initiate leukemia in immuno
[64]
cells. These progenitor cells proliferate quickly for a deficient mice . Furthermore, by transplanting sorted
WJSC|www.wjgnet.com 318 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
H90
Gemtuzumab ozogamicin
A3D8
Hu5F9-G4 (mylotarg)
CSL360
DT388IL3/SL-401
MGD006/S80880
Natalizumab
CD44
CD33
Bortezomib CD47 CD123
VLA-4 Stromal
Pr
ot cell
ea VCAM-1
so
m
e CXCR-4 Homing of LSC in
SDF
the bone marrow
niche
Bcl-2
IkBa
t
las
Plerixafor
ob
NF-kB AMD3465
te
Os
mTOR BMS-936564
GC
Parthenolide SF
PI3K Oblimersen -R
celastrol
Obatoclax
4-hydroxy- Br G-CSF
AKT ing
2-nonenal ing
LS
BKM120 C G-CSF
in
CAL-101 cy
cle
GSK21110183 Sirolimus,
MK-2206 everolimus,
Therapy targeting LSC surface markers
Perifosine temsirolimus
Therapy targeting signal transduction Blood vessels
Therapy targeting LSC microenvironment Endothelial cells
Figure 1 Leukemia stem cells biology and selected therapeutic strategies/agents targeting leukemia stem cell. Leukemia stem cells (LSC) directed therapy
targets cell surface markers expressed on LSC (grey boxes), crucial pathways for maintenance of stemness (orange boxes) and interactions between LSC and the
bone marrow niche (white boxes). Important LSC surface markers are CD33, CD44, CD123, CD47. Essential pathways are NF-κB, PI3K/AKT/mTOR and bcl-2.
LSC mobilization is accomplished with G-CSF and LSC homing to the bone marrow is regulated by the CXCR4–CXCL12 and VCAM-VLA4 axis. VCAM-1: Vascular
cell adhesion protein-1; VLA-4: Very late antigen-4; CXCR4: C-X-C chemokine receptor type 4; SDF: Stromal cell-derived factor 1; PI3K: Phosphatidylinositol-4,5-
bisphosphate 3-kinase; AKT: Protein kinase B; mTOR: Mechanistic target of rapamycin; bcl-2: B-cell lymphoma 2; G-CSF: Granulocyte-colony stimulating factor.
fractions of primary NPM-mutated AML into immuno complexity and heterogeneity of human LSC. Several
deficient mice, it was shown that approximately one- important observations have been made along the way
-
half of cases had LICs exclusively within the CD34 of discovery.
+
fraction, whereas the CD34 fraction contained normal
[66]
multilineage hematopoietic repopulating cells . Most of LSC heterogeneity within a patient: First, there is
+ -
the remaining cases had LICs in both CD34 and CD34 heterogeneity of the stem cell population within the
fractions and when samples were sorted based on same patient as not all LSC have the same self-renewal
[10,76]
CD34 and CD38 expression, multiple fractions initiated capacity . Use of lentiviral gene marking to track the
leukemia in primary and secondary recipients (Table 1). behavior of individual leukemia initiating cells following
serial transplantation has revealed heterogeneity
Heterogeneity within the LSC population in their ability to repopulate secondary and tertiary
Over the last years several groups have found a wide recipients and this enabled researchers to classify long
[76,77]
variety of other markers that appear to be expressed term (LT-LSC) and short term (ST-LSC) LSCs .
higher in LSCs than normal HSCs .
[14]
LT-LSCs are defined by a long-termed persistence in
These include CD123, CD96, CLL-1, TIM3, CD33, xenotransplantion models given an extensive self-
CD13, CD44, CD47 and others
[69-75]
(Table 1). In renewal capacity while ST-LSCs have a reduced self-
essence, these studies suggest that leukemogenic renewal capacity and only a transient repopulation
+ -
activity is not restricted to the CD34 CD38 fraction and capability in xenotransplantation models.
there is heterogeneity among patients in leukemogenic
cell phenotype. Over the last years, there has been LSC heterogeneity based on the specific xeno
significant advancement in the understanding of the transplantation model used: The LSC phenotype
WJSC|www.wjgnet.com 319 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
also a recreation of the cytokine environment supporting
Table 1 Markers of leukemia stem cells [14]
stem cell self-renewal and quiescence . This has led to
Cell surface Patient samples used Mouse model Ref. the development of mice models that express human
markers used [13,81]
cytokines like human SCF, GM-SCF, IL3 and TPO .
CD34+CD38- FAB M1, M4, M5 NOD/SCID [15,16]
CD34+CD38+ CN-AML, MLL-ENL NOD/SCID + [18,64,67,68] LSC heterogeneity between patients: It has
IVIG or
become increasingly evident that the LSC phenotype
anti-CD122
CD34-CD38+ AML with NPM1 NOD/SCID β-2 [66] varies between patients based on the specific subtype of
mutation microglobulin leukemia that they suffer from (Table 1). As mentioned
NOD/SCID IL2 above, the majority of AML cells express CD34, however
receptor γ−/− + in AML cells carrying a mutation in NPM1 the CD34
+
IVIG
CD34+CD123+ FAB M1, M2, M4 NOD/SCID [69]
percentage is very low and LSC activity is exclusively
- [66]
CD34+CD38-CD96+ CK-AML, CBFB- Rag2-/- IL2RG-/- [70] restricted to the CD34 population . Furthermore,
MYH11, specific subtypes of AML (in particular less aggressive
PML-RARA, subtypes) are significantly more difficult to be engrafted
AML1-ETO,
as they may have low progenitor cell frequency or are
FAB
M4
particularly sensitive to a specific cytokine or cell type
[14]
CD34+CLL1+ AMLs with FLT3- NOD/SCID [71] missing in the particular xenotransplantation model .
ITD For example, AML samples with a t(8;21) translocation
TIM3+ FAB M1, M2, M4 NOD/Rag1-/- [72] were shown to be difficult to be engrafted and found
IL2RG-/-
to be dependent on signaling though the TPO/mpl
CD34+CD38- CN-AML, NOD/SCID [73] [82,83]
CD33+CD13+ CBF-AML,
pathway . Subsequently, human TPO knock-in mice
MLL-ENL were shown to have improved engraftment for t(8;21)
[84]
AML samples .
FAB: French-American-British classification system; CN: Cytogenetically
normal; CK: Cytogenetically complex; MLL-ENL: Mixed-lineage
leukemia-eleven nineteen leukemia; NPM1: Nucleophosmin 1; CBFB-
Cell of origin of LSCs
MYH11: Core binding factor beta unit-Myosin heavy chain 11; PML- It is important to distinguish the concept of the cell of
[10]
RARA: Promyelocytic leukemia-retinoic acid receptor alpha; AML1-ETO: origin from the CSC . The CSC has stem cell like pro
Acute myeloid leukemia 1 protein- eight twenty one; FLT3-ITD: Fms- perties and is capable of initiating and sustaining tumor
like tyrosine kinase 3 Internal tandem duplication; NOD/SCID: Non- growth, whereas the cell of origin refers to the normal
obese diabetic/severe combined immunodeficiency; Rag: Recombination
cell in which the initial transforming event occurs. Impor
activating gene; IL2RG: Interleukin 2 receptor subunit gamma.
tantly, cancer and LSCs do not have to arise from a
normal stem cell, in fact, it is not entirely clear what the
depends on what mouse model is used for functional cell of origin for most LSCs is
[11,12]
. One hypothesis is
assessment of stem cell properties of human AML that LSCs are only able to arise from normal HSCs but
[14]
cells (Table 1). The bone marrow niche in mice differ not from committed progenitor cells
[10,15]
. This theory is
from that of humans in terms of architecture, stromal supported by the observation that LSCs and HSCs share
cells, cytokines, growth factors, adhesion molecules many characteristics like self-renewal capacity controlled
and most importantly the immune cell composition, by genes like Bmi1 and PTEN and quiescence
[35,85,86]
. On
which potentially impairs growth of human HSC or the contrary, transformation might occur in a variety
[78]
LSC in the mouse bone marrow . Normal HSCs and of cell types in the hematopoietic hierarchy, including
LSC are therefore more likely to be detected in more HSCs and committed progenitors
[10,87]
. Experimental
highly immunodeficient mice. As different xenotrans evidence in mice shows that LSCs may arise either
plantation mouse models display different levels of through neoplastic changes initiated in normal self-
immunodeficiency they are associated with different renewing HSCs or downstream progenitors cells
[10,11,88]
.
levels of engraftment of normal human HSCs and Some oncogenes including MOZ-TIF, MLL-AF9 and
[6,14]
LSCs . In nude mice T cells are absent whereas in MLL-ENL can induce LSCs regardless of what target
severe combined immunodeficiency mice (SCID mice) cell population they are expressed in
[88-90]
. Other
both B and T cells are inactivated. NOD/SCID mice, oncogenes like BCR-ABL, FLT3-ITD, Hoxa9 and Meis1
which harbor defects in T, B, and macrophage activity, were found to be oncogenic when expressed in HSCs
[14]
support higher levels of human engraftment . NOD/ but not when expressed in progenitor cells
[39,89,91]
.
SCID gamma (NSG) mice have almost no murine However, experimental data in murine studies might be
immune system left as a complete null mutation in the confounded by non-physiologic levels of expression from
gene encoding the interleukin 2-receptor gamma chain exogenous promoters, such as transgenes or retroviral
[79] [11]
blocks NK cell differentiation . Similarly, NK cells can be vectors . This was demonstrated by the recent finding
depleted by treating NOD/SCID mice with anti-CD122 that in an MLL-AF9 knock-in model of the same construct
[80]
antibodies . In creating a supportive bone marrow shown to initiate disease in both HSCs and progenitor
niche for engraftment of human AML cells not only a cells by retroviral expression only initiated leukemia
suppression of the hosts immune system is essential but from HSCs when expressed from the endogenous MLL
WJSC|www.wjgnet.com 320 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
[92] [107-109]
promoter . In vivo clonality studies in humans suggest LSCs .
variations in the cells of origin and is was demonstrated To improve survival in AML, traditional chemotherapy
+ -
that in patients with t(8;21) AML primitive CD34 CD90 targeting the blast population needs to be combined
-
CD38 HSC like cells from leukemic bone marrow give with therapy specifically targeting LSCs to maintain
rise to normally differentiating progenitors, whereas prolonged remission.
+ - +
more mature CD34 CD90 CD38 multi-potent progenitor
[93-95]
like cells form exclusively leukemic blast colonies .
These observations suggest that the truth about the cell FUTURE DIRECTIONS FOR THERAPY
of origin might be reflected by a combination of both Despite the recent increased interest in LSCs, experi
theories depicted above: Although the initial genetic mental studies have not been translated into improved
mutation might happen in HSCs subsequent events survival outcomes for cancer patients. However, several
occur in the committed progenitor pool, giving rise to new agents targeting LSC specific surface molecules
[11]
LSCs . and pathways as well as the LSC microenvironment
remains under different stages of preclinical and clinical
development (Table 2 and Figure 1). To rationally design
IMPACT OF LSC ON CURRENT clinical trials testing drugs for efficacy against LSCs, it
TREATMENT AND PROGNOSIS is important to appreciate the fundamental differences
[102]
between drug design targeting blast cells and LSCs .
Impact on prognosis Principles and challenges faced by targeting LSCs will be
The LSC burden of AML patient is suggested to be a
[96-100]
discussed first followed by an overview of various new
strong biomarker for clinical outcome in AML . The
therapeutic options targeting LSCs.
ability of cells from AML patients to engraft NOD/SCID
mice and the LSC frequency (simplistically characterized
+ - General principles and challenges faced by targeting
as CD34 CD38 frequency) are associated with worse
[99-101] LSCs
clinical outcomes . AML patients with greater than
+ - Limiting side effects: As LSCs and HSCs have many
3.5% of CD34 CD38 AML cells show a median relapse
similar properties (see above), therapeutic approaches
free survival of 5.6 mo vs 16 mo in those with a lower
+ - [96] targeting LSCs also have the potential of causing
percentage of CD34 CD38 cells . Furthermore,
severe side effects by eliminating healthy HSCs. To
poor clinical outcome seems to correlate with the
develop novel therapies with limited side effects,
degree to which the LSCs matched normal HSC gene [102,110]
[98] unique properties of LSCs have to be identified .
expression .
While expression of several surface markers is similar
It is noted that it is controversial whether the
between normal HSCs and LSCs (CD34, CD38, CD71
simplistically phenotypically defined LSC frequency
+ - and HLA-DR), other surface antigens are only displayed
(characterized as CD34 CD38 ) in AML is prognostic [110]
[14]
on LSCs (CD33, CD90, CD117 and CD123) . Apart
and correlates with xenograft potential . Also, as
from a similar immunophenotype, HSCs and LSCs
described above, LSCs can be found outside of the
+ -
share many pathways important for maintaining
CD34 CD38 cell fraction. An improved characterization
features of “stemness” like quiescence and self-renewal
of subpopulations of LSCs is expected to be associated [111]
capacity . Pathways, which are up-regulated in
with improved prediction of prognosis. LSCs compared to normal HSCs, are the ideal target
for therapeutic approaches directed towards LSCs. For
Impact on current therapies example, the active form of NF-κB and bcl-2, which are
It is thought that LSCs have a significant role in the associated with anti-apoptotic activity in cancer cells,
relapse of leukemia as induction chemotherapy targets are overexpressed in LSCs compared to normal HSC
[102]
the bulk of blast cells but not LSC . Minimal residual and drugs targeting both NF-κB and bcl-2 are in clinical
disease (MRD) is an important determinant for relapse development
[36,46,112]
.
and poor outcomes in AML and it is likely that the MRD
[103-105]
cell population contains LSCs . Thus, in order to Using biomarkers for LSC eradication: To assess
improve outcomes in AML, MRD needs to be reduced the efficacy of investigational therapies targeting
to prevent disease relapse. LSCs seem to be only LSCs, precise diagnostic methods are needed to
[35,106]
minimally affected by traditional chemotherapy . assess the quantity of LSCs present in leukemia
Several reasons for chemotherapy resistance have been patients. Unfortunately, current characterization of LSC
proposed, which are related to the key features of LSCs phenotype is not precise enough to permit real-time
discussed above. LSCs are quiescent in the G0 phase of [113]
tracking of LSCs in vivo . As discussed above, current
the cell cycle but chemotherapy is only effective in killing strategies for purification do not yield functionally
[36,37]
rapidly cycling cells . LSCs are supported by a stem homogeneous population: The frequency of LSCs within
+ - 4
cell niche in the bone marrow protecting them from the CD34 CD38 fraction in AML ranges from 1 in 10
[65] 6
the effect of classical chemotherapy . Furthermore, to 1 in 5 × 10 cells and several other populations
[15]
LSCs express high levels of ATP transporters, which are contain LSCs as well . Functional assessment of LSC
involved in extrusion of chemotherapeutic drugs from frequency with xenotransplantation models offers a
WJSC|www.wjgnet.com 321 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
GSK21110183 AKT NCT00881946 Phase [38,155-157]
Table 2 Emerging therapy targeting leukemia stem cells
MK-2206 inhibitors NCT01253447 I-II
Perifosine NCT01231919
Drug Mechanism Selected Phase Ref.
NCT00301938
clinical trials
Sirolimus, mTOR NCT01184898 Phase [38,158]
Therapy targeting cell surface markers everolimus, inhibitors NCT01611116 I-II
GO Anti-CD33 NCT00882102 Phase [124,126, temsirolimus NCT01074086
monoclonal NCT01869803 I-III 130,132,133] NCT01074086
antibody NCT00968071 NCT01154439
conjugated NCT01409161 NCT00775593
with NCT00766116 NCT02583893
calicheamicin, NCT02724163 NCT01869114
a potent NCT00658814 NCT01822015
antitumor NCT02473146 Oblimersen bcl-2 antisense NCT00085124 Phase [46,159,160]
anthracycline NCT00895934 (Genasense, oligodeoxy NCT00039117 I-III
antibiotic NCT00006265 G3139) nucleotide NCT00017589
NCT00860639 Obatoclax Small NCT00438178 Phase [161-163]
NCT00927498 Mesylate molecule bcl-2 NCT00684918 I-II
NCT00085709 (GX15-070MS) inhibitor NCT00684918
NCT00195000 Therapy targeting the LSC microenvironment
NCT00893399 G-CSF Mobilization NCT00820976 Phase [165-168]
NCT00017589 of LSC from NCT00602225 I-III
Hu5F9-G4 Anti-CD47 NCT02678338 Phase [74,141] the protective NCT00199147
monoclonal I bone marrow NCT01723657
antibody niche - > NCT01101880
CSL360 Anti-CD123 NCT00401739 Phase [69,134] increased NCT00943943
monoclonal I susceptibility NCT00906945
antibody to traditional
DT388IL3/ Anti-CD123 NCT02113982 Phase [69,134,136] chemotherapy
SL-401 recombinant NCT00397579 I-II Plerixafor CXCR4 NCT00943943 Phase [61,135,178]
immunotoxin (AMD3100) inhibitor NCT00906945 I-II
created by Decreased NCT01236144
the fusion of homing to the NCT00512252
diphtheria bone marrow NCT01319864
toxin with NCT01352650
a ligand NCT02416908
targeting the AMD3465 CXCR4 N/A N/A [61,135,169,179]
IL-3 receptor inhibitor
MGD006/ Anti-CD3 and NCT02152956 Phase [137] Decreased
S80880 CD123 DART I homing to the
H90 Anti-CD44 N/A N/A [75,139] bone marrow
monoclonal BMS-936564 Anti-CXCR4 NCT01120457 Phase [172]
antibody antibody I
A3D8 anti-CD44 N/A N/A [139] Decreased
monoclonal homing to the
antibody bone
Therapy targeting LSC-specific molecular pathways marrow
Bortezomib Proteasome NCT00789256 Phase [36,143-147, Natalizumab Anti-VLA4 N/A N/A [174]
inhibitor NCT00382954 I-III 175-177] antibody
inhibits the NCT01127009 Decreased
degradation NCT00666588 homing to the
of the IkBa NCT00703300 bone marrow
creating an NCT01534260
anti-NF-kB NCT00383474 GO: Gemtuzumab ozogamicin; DART: Dual-affinity retargeting molecule;
effect N/A: Not available; LSC: Leukemia stem cell; IkBa: Inhibitor of kappa
Parthenolide Inhibitor of N/A N/A [149] B alpha; CXCR4: C-X-C chemokine receptor type 4; mTOR: Mechanistic
NF-kB target of rapamycin; G-CSF: Granulocyte-colony stimulating factor.
Celastrol Inhibitor of N/A N/A [150]
Hsp90 and by
extension NF- more robust method to evaluate eradication of LSCs but
kB [102]
might not be feasible in large clinical trials . Similarly,
4-hydroxy- Product N/A N/A [151,152]
2-nonenal of lipid methods for detecting MRD might guide decisions by
peroxidation, detecting patients who do require additional therapy
inhibiting the to prevent relapse. However, detecting MRD does not
proteasome distinguish persistent LSCs, which may cause relapse,
and NF-kB
from residual blasts and normal HSCs that do not have
function
BKM120 PI3K NCT01396499 Phase [38,153,154] tumor-initiating activity. Distinguishing residual LSCs
CAL-101 inhibitors NCT01833169 I-II from residual blasts might be accomplished by gene
NCT00710528 expression analysis showing reactivation of self-renewal
WJSC|www.wjgnet.com 322 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
[88,114] [122-124]
genes in LSCs but not in blast cells . In preclinical as increased fatal toxicity . In contrast, other large
development, the recently published Connectivity Map clinical trials showed improvement in outcomes more
could be investigated for agents that attenuate a stem relevant for therapies targeting LSC- event-free survival,
[115,116]
cell gene signature or induce a differentiated state . disease-free survival and OS- despite no differences in
[125-128]
disease response rates .
Timing of LSC targeted therapy: Therapy targeting
LSCs is effective in eradicating a small amount of Targeting LSC surface molecules
leukemia initiating cells but not the bulk of blasts Anti-CD33 antibodies: CD33 is found on LSCs alth
[102]
cells in the blood and bone marrow . By combining ough it is not a consistent feature of all LSCs studi
drugs eradicating LSCs with standard chemotherapy ed
[73,118,129]
. As discussed above, there have been con
targeting the bulk of the disease, both the aggressive flicting reports surrounding the efficacy and safety of
proliferating process as well as the root of the leukemia GO and currently GO is not available on the market in
[117]
can be targeted . An example serves the successful [130]
the United States or Europe . Apart from the different
combination of the anti-CD33 immunoconjugate anti endpoints studied, there are additional explanations
body gemtuzumab ozogamicin (GO) with standard for the discrepancies observed: First, the dose of
[118]
chemotherapy . This is associated with challenges daunorubicin as the combination partner of GO did vary
in a meaningful design of clinical trials in terms of the between trials, although it is known that treatment with
correct timing of these therapies. LSC targeting therapy daunorubicin-based schedules of 90 mg/m for 3 d is
2
can either be given after reduction of the bulk population more effective than similar schedules with daunorubicin
with standard chemotherapy as remission therapy at 45 mg/m
2[131]
. In the SWOG trial, which questioned
or concomitant with chemotherapy as an induction the efficacy of GO, single bolus combined with dau
[102]
regimen . Upfront combination would allow assessing 2
norubicin at 45 mg/m was studied against a control
for additive and/or synergistic properties between drugs group with daunorubicin at 60 mg/m
2[124]
. However, the
and would allow targeting of LSCs early on in the disease best effect of GO was seen when higher dose of GO (3
[102]
process, which might improve outcomes . On the 2
d at 3 mg/m for 2 cycles) was added to a daunorubicin
other hand, LSC targeted therapy might be particular 2
regimen of 60 mg/m in both comparator groups .
[126]
valuable as post-consolidation therapy as no current Furthermore, GO seems to be quite active in acute
post-consolidation intervention has led to improved OS promyelocytic leukemia (APL) as APL cells express high
[102,119,120]
for patients with AML . LSC targeting therapies levels of CD33
[132,133]
. These results have prompted calls
have the potential to fill the gap as they eradicate the to reconsider the approval status of GO .
[130]
cells responsible for relapses of AML.
Anti-IL-3 receptor (CD123) antibodies: The inter
Assessing clinical endpoints: Classical response leukin-3 receptor alpha chain (IL-3Rα or CD123) is
criteria like CR and hematologic improvement might + -
strongly expressed in CD34 /CD38 LSCs and can be
not be the best parameters to assess the efficacy of targeted with monoclonal antibodies
[69,134]
. The blockage
therapeutic approaches targeting LSCs as these drugs of CD123 has pleiotropic anti-leukemic effects including
do not eradicate the bulk of blast cells but rather inhibition of LSC homing to the bone marrow, activation
[102]
eliminate the rare population of LSCs . Progression- of innate immunity and inhibition of intracellular signa
free survival (PFS), event free survival and overall ling events
[135]
. Several different agents targeting
survival (OS) may be a more relevant endpoint for CD123 are currently evaluated in clinical trials: CD123
assessing the effectiveness of LSC elimination than targeting antibodies can either be naked antibodies
tumor response as they better account for whether or be conjugated to toxins (e.g., diphteriod toxin) or
[113]
the root of the leukemia has been eliminated . chemotherapeutic agents (chemo-immune conjugates)
Importantly, while LSC frequency was found to be or be the backbone of a bi-specific T cell engager (BITE,
[134,136,137]
prognostic for survival, response rates did not correlate e.g., CD3-CD123) (Table 2).
[96]
with LSC burden . Subsequently, drugs targeting LSCs
may show little activity if tested in traditional phase Anti-CD44 antibodies: CD44 regulates interaction
I/II trials as a proper assessment of endpoints relevant between LSCs and the bone marrow niche by controlling
for LSCs, like PFS and OS, is generally only feasible in cell-cell adhesion and cell-matrix interaction through
a phase III trial with a larger numbers of patients and binding to hyaluronic acid, osteopontin, collagens and
[113,121] [138]
long-term follow-up . others .
One example for the importance of assessing Inhibition of CD44 with monoclonal antibodies was
relevant endpoints for LSC targeting therapy, is incon shown to reduce the numbers of LSCs in NOD/SCID
sistency of clinical trials evaluating the efficacy of mice and to increase the survival of the primary reci
[102]
GO . Single agent studies of GO showed overall pient mice as well prevent engraftment into the secon
[75,139]
response rates only approaching 30% at best and dary receipt mice (Table 2).
GO was voluntarily withdrawn from the United States
market in 2010 after a study showed no improvements Anti-CD47 antibodies: CD47 is overexpressed on
in outcomes when used in combination therapy as well LSCs and high expression of CD47 is associated with
WJSC|www.wjgnet.com 323 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
[74]
worse outcomes . By interaction with the extracellular in combination with chemotherapy are conflicting.
[166]
region of signal-regulatory protein alpha (SIRPα) Löwenberg et al randomized 640 newly diagnosed
on phagocytic cells, LSCs deliver a “do not eat me” AML patients to receive cytarabine plus idarubicin with
[140]
message to these phagocytic cells . Antibodies G-CSF (321 patients) or without G-CSF (319 patients)
blocking the interaction between CD47 and SIRPα for the first cycle of induction of chemotherapy. Patients
promote LSC phagocytosis and are in development in CR after induction chemotherapy plus G-CSF had
[74,141]
(Table 2) . a higher rate of disease-free survival than patients
who did not receive G-CSF (42% vs 33% at four
Targeting LSC-specific molecular pathways years, P = 0.02), owing to a reduced probability of
NF-κB signaling pathway: Bortezomib is able to relapse (relative risk, 0.77; P = 0.04). Other studies
suppress the NF-κB signaling pathway by inhibiting the did not show a benefit of adding G-CSF to traditional
[167,168]
destruction of IκB, a cellular inhibitory protein of NFκB, chemotherapy regimens . These different res
[142]
by the ubiquitin-proteasome pathway . Several clinical ponses to G-CSF might be explained by differences in
[63]
trials are examining the efficacy of Bortezomib targeting the group of patients included in these trials . In the
[166]
AML LSCs (Table 2): Two clinical trials combining trial by Löwenberg et al patients with standard-risk
Bortezomib with Cytarabine and Anthracyclines resulted AML benefited from G-CSF therapy whereas G-CSF
in CR rates of 61% and 65%
[143,144]
, whereas other trials did not improve the outcome in the subgroup with an
that co-administrated Bortezomib with other drugs did unfavorable prognosis. In the trials without improvement
not show encouraging CR rates
[145-147]
. Several other with G-CSF, patients had a more unfavorable prognosis
inhibitors of NF-κB signaling are in different phases of based on age, cytogenetic abnormalities or response to
development (Table 2)
[148-152]
. previous treatment. Several clinical trials are ongoing
to investigate the efficacy of G-CSF in combination of
PI3K/AKT/mTOR pathway: The PI3K/AKT/mTOR chemotherapy in different risk groups of AML (Table 2).
pathway is of utmost importance in regulating cellular
growth, survival, and metabolism and is frequently Inhibition of homing: LSC dormancy can be targeted
[38]
dysregulated in cancers and AML . A multitude of by specifically interrupting the CXCR4-CXCL12 and
PI3K inhibitors
[153,154]
, AKT inhibitors
[155-157]
and mTOR VCAM-VLA4 axis as well as inhibiting CD44 and CD123
inhibitors
[158]
is currently investigated for their efficacy on LSCs to prevent homing of LSCs to the bone
targeting LSCs in clinical trials (Table 2). marrow.
Bcl-2 pathway: LSCs, similar to other tumor cells, CXCR4-CXCL12 axis: SDF-1 was shown to promote
are able to avoid apoptosis due to overexpression of survival of AML cells, whereas addition of neutralizing
[46]
bcl-2 . Currently, bcl-2 inhibition is investigated in CXCR4 antibodies, SDF-1 antibodies, or AMD3100
[169]
clinical trials in form of the bcl-2 antisense oligodeo significantly decreased their survival . Furthermore,
xynucleotide oblimersen
[159,160]
and the small molecule pretreatment of primary human AML cells with
inhibitor of bcl-2 obatoclax
[161-163]
(Table 2). neutralizing CXCR4 antibodies blocked their homing into
null
the BM and spleen of transplanted NOD/SCID/B2m
[169]
Targeting the LSC microenvironment mice . Additionally, CXCR4 inhibition with AMD3465
Approaches targeting the interactions of LSCs with the was shown to increase the sensitivity of FLT3-mutated
bone marrow niche focus on breaking the dormancy leukemic cells to the apoptogenic effects of the FLT3
[170]
of LSCs in the bone marrow in order to make them inhibitor sorafenib . Recently a phase 1/2 study
sensitive to traditional chemotherapy
[62,164]
. examined the efficacy of the CXCR4 inhibitor plerixafor
in combination with mitoxantrone, etoposide, and
LSC mobilization: LSC mobilization from the marrow cytarabine in 52 patients with relapsed or refractory
[171]
niche can be achieved by nonspecific stimulators like AML . Overall CR was found to be 46% and corre
[62]
G-CSF, Interferon-α and Arsenic trioxide . Using the lative studies demonstrated a 2-fold mobilization in
NOD/SCID/IL2rgamma (null) mouse model, Saito leukemic blasts into the peripheral circulation without
[165]
et al showed that quiescent human AML LSCs, at evidence of symptomatic hyperleukocytosis or delayed
first resistant to cytarabine, start proliferating and count recovery. BMS-936564, a fully human IgG4
become susceptible to cytarabine once exposed to monoclonal antibody against CXCR4, exhibits antitumor
G-CSF. Combining chemotherapy with G-CSF leads to activity in cytarabine-resistant mouse xenograft models
significantly increased survival of secondary recipients of AML and is currently tested in a phase I clinic trial
[172]
after transplantation of leukemia cells compared with (Table 2) .
chemotherapy alone. Furthermore, they showed that
treatment with G-CSF before cytarabine did not increase VCAM-VLA4 axis: Integrin alpha4beta1 (VLA4)
apoptosis of normal HSCs making this approach a mediates adhesion of LSCs to stromal cells and extra
particular attractive option for targeting LSCs but at cellular matrix in the marrow niche and can be blocked
[59,69,173]
the same time avoiding side effects from depletion of by the monoclonal antibody Natalizumab .
HSCs. The data from clinic trials using G-CSF priming AML cells were shown to de-adhere from a layer of
WJSC|www.wjgnet.com 324 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
immobilized human VCAM1 expressing human stromal brain tumour initiating cells. Nature 2004; 432: 396-401 [PMID:
cells when exposed to Natalizumab and NSG mice 15549107 DOI: 10.1038/nature03128]
10 Wang JC, Dick JE. Cancer stem cells: lessons from leukemia.
transplanted with human AML cells survived significantly
Trends Cell Biol 2005; 15: 494-501 [PMID: 16084092 DOI: 10.1016/
longer when they received intraperitoneal Natalizumab j.tcb.2005.07.004]
[174]
injections . 11 Dick JE. Stem cell concepts renew cancer research. Blood 2008; 112:
4793-4807 [PMID: 19064739 DOI: 10.1182/blood-2008-08-077941]
12 Clarke MF, Dick JE, Dirks PB, Eaves CJ, Jamieson CH, Jones DL,
CONCLUSION Visvader J, Weissman IL, Wahl GM. Cancer stem cells--perspectives
on current status and future directions: AACR Workshop on cancer
AML remains one of the most difficult malignancies stem cells. Cancer Res 2006; 66: 9339-9344 [PMID: 16990346 DOI:
to treat. Despite significant advancements in the 10.1158/0008-5472.CAN-06-3126]
understanding of disease biology, this has not been 13 Wunderlich M, Chou FS, Link KA, Mizukawa B, Perry RL,
translated yet into new treatment modalities improving Carroll M, Mulloy JC. AML xenograft efficiency is significantly
improved in NOD/SCID-IL2RG mice constitutively expressing
outcomes. The relapse of AML is frequent and is
human SCF, GM-CSF and IL-3. Leukemia 2010; 24: 1785-1788
responsible for the inability to cure AML. LSCs are [PMID: 20686503 DOI: 10.1038/leu.2010.158]
understood to be the root of relapse and their presence 14 Goyama S, Wunderlich M, Mulloy JC. Xenograft models for
has been found to be prognostic for the disease course. normal and malignant stem cells. Blood 2015; 125: 2630-2640
Unfortunately, LSCs are not easy to target as they are [PMID: 25762176 DOI: 10.1182/blood-2014-11-570218]
15 Bonnet D, Dick JE. Human acute myeloid leukemia is organized
quiescent, able to self-renew and well protected by
as a hierarchy that originates from a primitive hematopoietic
a supportive bone marrow niche. Furthermore, their cell. Nat Med 1997; 3: 730-737 [PMID: 9212098 DOI: 10.1038/
inconsistent phenotype and similarity to normal HSCs nm0797-730]
hamper specific drug development. Nevertheless, a 16 Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-
multitude of potential targets have been identified Cortes J, Minden M, Paterson B, Caligiuri MA, Dick JE. A cell
initiating human acute myeloid leukaemia after transplantation into
and are currently tested in different phases of clinical
SCID mice. Nature 1994; 367: 645-648 [PMID: 7509044 DOI:
and preclinical development. Successful eradication of 10.1038/367645a0]
LSCs will require combination of different strategies 17 Till JE, Mcculloch EA, Siminovitch L. A stochastic model of stem
including targeting LSC specific surface molecules cell proliferation, based on the growth of spleen colony-forming
and pathways as well as interactions of LSCs with the cells. Proc Natl Acad Sci USA 1964; 51: 29-36 [PMID: 14104600
DOI: 10.1073/pnas.51.1.29]
microenvironment. Furthermore, clinical trials have
18 McKenzie JL, Gan OI, Doedens M, Wang JC, Dick JE. Individual
to be designed in a way that they are able to detect stem cells with highly variable proliferation and self-renewal
a specific effect of LSCs, which is easy to miss in a properties comprise the human hematopoietic stem cell com
traditional trial design. Overall, targeting LSCs has the partment. Nat Immunol 2006; 7: 1225-1233 [PMID: 17013390
promise to not only effectively reduce disease burden DOI: 10.1038/ni1393]
but to eradicate the root of leukemia itself. 19 Morrison SJ, Kimble J. Asymmetric and symmetric stem-cell
divisions in development and cancer. Nature 2006; 441: 1068-1074
[PMID: 16810241 DOI: 10.1038/nature04956]
20 Huttner WB, Kosodo Y. Symmetric versus asymmetric cell
REFERENCES division during neurogenesis in the developing vertebrate central
1 Roboz GJ. Novel approaches to the treatment of acute myeloid nervous system. Curr Opin Cell Biol 2005; 17: 648-657 [PMID:
leukemia. Hematology Am Soc Hematol Educ Program 2011; 2011: 16243506 DOI: 10.1016/j.ceb.2005.10.005]
43-50 [PMID: 22160011 DOI: 10.1182/asheducation-2011.1.43] 21 Boman BM, Wicha MS, Fields JZ, Runquist OA. Symmetric
2 Felipe Rico J, Hassane DC, Guzman ML. Acute myelogenous division of cancer stem cells--a key mechanism in tumor growth
leukemia stem cells: from Bench to Bedside. Cancer Lett 2013; that should be targeted in future therapeutic approaches. Clin
338: 4-9 [PMID: 22713929 DOI: 10.1016/j.canlet.2012.05.034] Pharmacol Ther 2007; 81: 893-898 [PMID: 17460605 DOI:
3 Crews LA, Jamieson CH. Selective elimination of leukemia stem 10.1038/sj.clpt.6100202]
cells: hitting a moving target. Cancer Lett 2013; 338: 15-22 [PMID: 22 Powell AE, Shung CY, Saylor KW, Müllendorff KA, Weiss JB,
22906415 DOI: 10.1016/j.canlet.2012.08.006] Wong MH. Lessons from development: A role for asymmetric
4 Lutz C, Hoang VT, Buss E, Ho AD. Identifying leukemia stem stem cell division in cancer. Stem Cell Res 2010; 4: 3-9 [PMID:
cells--is it feasible and does it matter? Cancer Lett 2013; 338: 10-14 19853549 DOI: 10.1016/j.scr.2009.09.005]
[PMID: 22820159 DOI: 10.1016/j.canlet.2012.07.014] 23 Cicalese A, Bonizzi G, Pasi CE, Faretta M, Ronzoni S, Giulini
5 Ailles LE, Weissman IL. Cancer stem cells in solid tumors. Curr B, Brisken C, Minucci S, Di Fiore PP, Pelicci PG. The tumor
Opin Biotechnol 2007; 18: 460-466 [PMID: 18023337 DOI: suppressor p53 regulates polarity of self-renewing divisions in
10.1016/j.copbio.2007.10.007] mammary stem cells. Cell 2009; 138: 1083-1095 [PMID: 19766563
6 Magee JA, Piskounova E, Morrison SJ. Cancer stem cells: impact, DOI: 10.1016/j.cell.2009.06.048]
heterogeneity, and uncertainty. Cancer Cell 2012; 21: 283-296 24 Yamashita YM, Mahowald AP, Perlin JR, Fuller MT. Asymmetric
[PMID: 22439924 DOI: 10.1016/j.ccr.2012.03.003] inheritance of mother versus daughter centrosome in stem cell
7 Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, division. Science 2007; 315: 518-521 [PMID: 17255513 DOI:
and cancer stem cells. Nature 2001; 414: 105-111 [PMID: 11689955 10.1126/science.1134910]
DOI: 10.1038/35102167] 25 Yamashita YM, Jones DL, Fuller MT. Orientation of asymmetric
8 Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke stem cell division by the APC tumor suppressor and centrosome.
MF. Prospective identification of tumorigenic breast cancer cells. Science 2003; 301: 1547-1550 [PMID: 12970569 DOI: 10.1126/
Proc Natl Acad Sci USA 2003; 100: 3983-3988 [PMID: 12629218 science.1087795]
DOI: 10.1073/pnas.0530291100] 26 Nakamura-Ishizu A, Takizawa H, Suda T. The analysis, roles and
9 Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, regulation of quiescence in hematopoietic stem cells. Development
Henkelman RM, Cusimano MD, Dirks PB. Identification of human 2014; 141: 4656-4666 [PMID: 25468935 DOI: 10.1242/
WJSC|www.wjgnet.com 325 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
dev.106575] activity in acute myeloid leukemia: from molecular pathogenesis
27 Sharpless NE, DePinho RA. How stem cells age and why this to therapeutic target. Oncotarget 2015; 6: 5490-5500 [PMID:
makes us grow old. Nat Rev Mol Cell Biol 2007; 8: 703-713 [PMID: 25823927 DOI: 10.18632/oncotarget.3545]
17717515 DOI: 10.1038/nrm2241] 44 Kagoya Y, Yoshimi A, Kataoka K, Nakagawa M, Kumano K, Arai S,
28 Allsopp RC, Morin GB, DePinho R, Harley CB, Weissman Kobayashi H, Saito T, Iwakura Y, Kurokawa M. Positive feedback
IL. Telomerase is required to slow telomere shortening and between NF-κB and TNF-α promotes leukemia-initiating cell
extend replicative lifespan of HSCs during serial transplantation. capacity. J Clin Invest 2014; 124: 528-542 [PMID: 24382349 DOI:
Blood 2003; 102: 517-520 [PMID: 12663456 DOI: 10.1182/ 10.1172/JCI68101]
blood-2002-07-2334] 45 Liu N, Zhang J, Ji C. The emerging roles of Notch signaling
29 Kim WY, Sharpless NE. The regulation of INK4/ARF in cancer in leukemia and stem cells. Biomark Res 2013; 1: 23 [PMID:
and aging. Cell 2006; 127: 265-275 [PMID: 17055429 DOI: 24252593 DOI: 10.1186/2050-7771-1-23]
10.1016/j.cell.2006.10.003] 46 Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ,
30 Tyner SD, Venkatachalam S, Choi J, Jones S, Ghebranious N, Minhajuddin M, Ashton JM, Pei S, Grose V, O’Dwyer KM, Liesveld
Igelmann H, Lu X, Soron G, Cooper B, Brayton C, Park SH, JL, Brookes PS, Becker MW, Jordan CT. BCL-2 inhibition targets
Thompson T, Karsenty G, Bradley A, Donehower LA. p53 mutant oxidative phosphorylation and selectively eradicates quiescent human
mice that display early ageing-associated phenotypes. Nature 2002; leukemia stem cells. Cell Stem Cell 2013; 12: 329-341 [PMID:
415: 45-53 [PMID: 11780111 DOI: 10.1038/415045a] 23333149 DOI: 10.1016/j.stem.2012.12.013]
31 Lenhoff S, Hjorth M, Westin J, Brinch L, Bäckström B, Carlson 47 Domen J, Weissman IL. Hematopoietic stem cells need two signals
K, Christiansen I, Dahl IM, Gimsing P, Hammerström J, Johnsen to prevent apoptosis; BCL-2 can provide one of these, Kitl/c-Kit
HE, Juliusson G, Linder O, Mellqvist UH, Nesthus I, Nielsen JL, signaling the other. J Exp Med 2000; 192: 1707-1718 [PMID:
Tangen JM, Turesson I. Impact of age on survival after intensive 11120768 DOI: 10.1084/jem.192.12.1707]
therapy for multiple myeloma: a population-based study by the 48 Schepers K, Campbell TB, Passegué E. Normal and leukemic stem
Nordic Myeloma Study Group. Br J Haematol 2006; 133: 389-396 cell niches: insights and therapeutic opportunities. Cell Stem Cell 2015;
[PMID: 16643445 DOI: 10.1111/j.1365-2141.2006.06042.x] 16: 254-267 [PMID: 25748932 DOI: 10.1016/j.stem.2015.02.014]
32 Kollman C, Howe CW, Anasetti C, Antin JH, Davies SM, 49 Orkin SH, Zon LI. Hematopoiesis: an evolving paradigm for stem
Filipovich AH, Hegland J, Kamani N, Kernan NA, King R, cell biology. Cell 2008; 132: 631-644 [PMID: 18295580 DOI:
Ratanatharathorn V, Weisdorf D, Confer DL. Donor characteristics 10.1016/j.cell.2008.01.025]
as risk factors in recipients after transplantation of bone marrow 50 Butler JM, Nolan DJ, Vertes EL, Varnum-Finney B, Kobayashi H,
from unrelated donors: the effect of donor age. Blood 2001; 98: Hooper AT, Seandel M, Shido K, White IA, Kobayashi M, Witte
2043-2051 [PMID: 11567988 DOI: 10.1182/blood.V98.7.2043] L, May C, Shawber C, Kimura Y, Kitajewski J, Rosenwaks Z,
33 Watt FM, Jensen KB. Epidermal stem cell diversity and Bernstein ID, Rafii S. Endothelial cells are essential for the self-
quiescence. EMBO Mol Med 2009; 1: 260-267 [PMID: 20049729 renewal and repopulation of Notch-dependent hematopoietic stem
DOI: 10.1002/emmm.200900033] cells. Cell Stem Cell 2010; 6: 251-264 [PMID: 20207228 DOI:
34 Moore N, Lyle S. Quiescent, slow-cycling stem cell populations 10.1016/j.stem.2010.02.001]
in cancer: a review of the evidence and discussion of significance. 51 Crisan M, Yap S, Casteilla L, Chen CW, Corselli M, Park TS,
J Oncol 2011; 2011: pii: 396076 [PMID: 20936110 DOI: Andriolo G, Sun B, Zheng B, Zhang L, Norotte C, Teng PN, Traas
10.1155/2011/396076] J, Schugar R, Deasy BM, Badylak S, Buhring HJ, Giacobino JP,
35 Terpstra W, Ploemacher RE, Prins A, van Lom K, Pouwels Lazzari L, Huard J, Péault B. A perivascular origin for mesenchymal
K, Wognum AW, Wagemaker G, Löwenberg B, Wielenga JJ. stem cells in multiple human organs. Cell Stem Cell 2008; 3:
Fluorouracil selectively spares acute myeloid leukemia cells with 301-313 [PMID: 18786417 DOI: 10.1016/j.stem.2008.07.003]
long-term growth abilities in immunodeficient mice and in culture. 52 Morrison SJ, Scadden DT. The bone marrow niche for haema
Blood 1996; 88: 1944-1950 [PMID: 8822911] topoietic stem cells. Nature 2014; 505: 327-334 [PMID: 24429631
36 Guzman ML, Neering SJ, Upchurch D, Grimes B, Howard DS, DOI: 10.1038/nature12984]
Rizzieri DA, Luger SM, Jordan CT. Nuclear factor-kappaB is 53 Bruns I, Lucas D, Pinho S, Ahmed J, Lambert MP, Kunisaki
constitutively activated in primitive human acute myelogenous Y, Scheiermann C, Schiff L, Poncz M, Bergman A, Frenette PS.
leukemia cells. Blood 2001; 98: 2301-2307 [PMID: 11588023 DOI: Megakaryocytes regulate hematopoietic stem cell quiescence through
10.1182/blood.V98.8.2301] CXCL4 secretion. Nat Med 2014; 20: 1315-1320 [PMID: 25326802
37 Guan Y, Gerhard B, Hogge DE. Detection, isolation, and DOI: 10.1038/nm.3707]
stimulation of quiescent primitive leukemic progenitor cells from 54 Lane SW, Scadden DT, Gilliland DG. The leukemic stem cell niche:
patients with acute myeloid leukemia (AML). Blood 2003; 101: current concepts and therapeutic opportunities. Blood 2009; 114:
3142-3149 [PMID: 12468427 DOI: 10.1182/blood-2002-10-3062] 1150-1157 [PMID: 19401558 DOI: 10.1182/blood-2009-01-202606]
38 Fransecky L, Mochmann LH, Baldus CD. Outlook on PI3K/AKT/ 55 Sugiyama T, Kohara H, Noda M, Nagasawa T. Maintenance of
mTOR inhibition in acute leukemia. Mol Cell Ther 2015; 3: 2 the hematopoietic stem cell pool by CXCL12-CXCR4 chemokine
[PMID: 26056603 DOI: 10.1186/s40591-015-0040-8] signaling in bone marrow stromal cell niches. Immunity 2006; 25:
39 Wang Y, Krivtsov AV, Sinha AU, North TE, Goessling W, Feng Z, 977-988 [PMID: 17174120 DOI: 10.1016/j.immuni.2006.10.016]
Zon LI, Armstrong SA. The Wnt/beta-catenin pathway is required 56 Ara T, Tokoyoda K, Sugiyama T, Egawa T, Kawabata K, Nagasawa
for the development of leukemia stem cells in AML. Science 2010; T. Long-term hematopoietic stem cells require stromal cell-
327: 1650-1653 [PMID: 20339075 DOI: 10.1126/science.1186624] derived factor-1 for colonizing bone marrow during ontogeny.
40 Lento W, Congdon K, Voermans C, Kritzik M, Reya T. Wnt Immunity 2003; 19: 257-267 [PMID: 12932359 DOI: 10.1016/
signaling in normal and malignant hematopoiesis. Cold Spring S1074-7613(03)00201-2]
Harb Perspect Biol 2013; 5: pii: a008011 [PMID: 23378582 DOI: 57 Juneja HS, Schmalsteig FC, Lee S, Chen J. Vascular cell adhesion
10.1101/cshperspect.a008011] molecule-1 and VLA-4 are obligatory adhesion proteins in the
41 Mar BG, Amakye D, Aifantis I, Buonamici S. The controversial heterotypic adherence between human leukemia/lymphoma cells
role of the Hedgehog pathway in normal and malignant hema and marrow stromal cells. Exp Hematol 1993; 21: 444-450 [PMID:
topoiesis. Leukemia 2011; 25: 1665-1673 [PMID: 21660044 DOI: 7680000]
10.1038/leu.2011.143] 58 Avecilla ST, Hattori K, Heissig B, Tejada R, Liao F, Shido K, Jin
42 Irvine DA, Copland M. Targeting hedgehog in hematologic DK, Dias S, Zhang F, Hartman TE, Hackett NR, Crystal RG, Witte
malignancy. Blood 2012; 119: 2196-2204 [PMID: 22223823 DOI: L, Hicklin DJ, Bohlen P, Eaton D, Lyden D, de Sauvage F, Rafii S.
10.1182/blood-2011-10-383752] Chemokine-mediated interaction of hematopoietic progenitors with
43 Zhou J, Ching YQ, Chng WJ. Aberrant nuclear factor-kappa B the bone marrow vascular niche is required for thrombopoiesis. Nat
WJSC|www.wjgnet.com 326 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
Med 2004; 10: 64-71 [PMID: 14702636 DOI: 10.1038/nm973] 73 Taussig DC, Pearce DJ, Simpson C, Rohatiner AZ, Lister TA, Kelly
59 Matsunaga T, Takemoto N, Sato T, Takimoto R, Tanaka I, Fujimi G, Luongo JL, Danet-Desnoyers GA, Bonnet D. Hematopoietic
A, Akiyama T, Kuroda H, Kawano Y, Kobune M, Kato J, Hirayama stem cells express multiple myeloid markers: implications for
Y, Sakamaki S, Kohda K, Miyake K, Niitsu Y. Interaction between the origin and targeted therapy of acute myeloid leukemia.
leukemic-cell VLA-4 and stromal fibronectin is a decisive factor for Blood 2005; 106: 4086-4092 [PMID: 16131573 DOI: 10.1182/
minimal residual disease of acute myelogenous leukemia. Nat Med blood-2005-03-1072]
2003; 9: 1158-1165 [PMID: 12897778 DOI: 10.1038/nm909] 74 Majeti R, Chao MP, Alizadeh AA, Pang WW, Jaiswal S, Gibbs
60 Rombouts EJ, Pavic B, Löwenberg B, Ploemacher RE. Relation KD, van Rooijen N, Weissman IL. CD47 is an adverse prognostic
between CXCR-4 expression, Flt3 mutations, and unfavorable factor and therapeutic antibody target on human acute myeloid
prognosis of adult acute myeloid leukemia. Blood 2004; 104: leukemia stem cells. Cell 2009; 138: 286-299 [PMID: 19632179
550-557 [PMID: 15054042 DOI: 10.1182/blood-2004-02-0566] DOI: 10.1016/j.cell.2009.05.045]
61 Spoo AC, Lübbert M, Wierda WG, Burger JA. CXCR4 is a 75 Jin L, Hope KJ, Zhai Q, Smadja-Joffe F, Dick JE. Targeting of
prognostic marker in acute myelogenous leukemia. Blood 2007; 109: CD44 eradicates human acute myeloid leukemic stem cells. Nat
786-791 [PMID: 16888090 DOI: 10.1182/blood-2006-05-024844] Med 2006; 12: 1167-1174 [PMID: 16998484 DOI: 10.1038/
62 Essers MA, Trumpp A. Targeting leukemic stem cells by breaking nm1483]
their dormancy. Mol Oncol 2010; 4: 443-450 [PMID: 20599449 76 Hope KJ, Jin L, Dick JE. Acute myeloid leukemia originates from
DOI: 10.1016/j.molonc.2010.06.001] a hierarchy of leukemic stem cell classes that differ in self-renewal
63 Mikkola HK, Radu CG, Witte ON. Targeting leukemia stem capacity. Nat Immunol 2004; 5: 738-743 [PMID: 15170211 DOI:
cells. Nat Biotechnol 2010; 28: 237-238 [PMID: 20212485 DOI: 10.1038/ni1080]
10.1038/nbt0310-237] 77 Misaghian N, Ligresti G, Steelman LS, Bertrand FE, Bäsecke J,
64 Taussig DC, Miraki-Moud F, Anjos-Afonso F, Pearce DJ, Allen Libra M, Nicoletti F, Stivala F, Milella M, Tafuri A, Cervello M,
K, Ridler C, Lillington D, Oakervee H, Cavenagh J, Agrawal SG, Martelli AM, McCubrey JA. Targeting the leukemic stem cell: the
Lister TA, Gribben JG, Bonnet D. Anti-CD38 antibody-mediated Holy Grail of leukemia therapy. Leukemia 2009; 23: 25-42 [PMID:
clearance of human repopulating cells masks the heterogeneity 18800146 DOI: 10.1038/leu.2008.246]
of leukemia-initiating cells. Blood 2008; 112: 568-575 [PMID: 78 Manz MG. Human-hemato-lymphoid-system mice: opportunities
18523148 DOI: 10.1182/blood-2007-10-118331] and challenges. Immunity 2007; 26: 537-541 [PMID: 17521579
65 Ishikawa F, Yoshida S, Saito Y, Hijikata A, Kitamura H, Tanaka DOI: 10.1016/j.immuni.2007.05.001]
S, Nakamura R, Tanaka T, Tomiyama H, Saito N, Fukata M, 79 Shultz LD, Lyons BL, Burzenski LM, Gott B, Chen X, Chaleff
Miyamoto T, Lyons B, Ohshima K, Uchida N, Taniguchi S, Ohara S, Kotb M, Gillies SD, King M, Mangada J, Greiner DL,
O, Akashi K, Harada M, Shultz LD. Chemotherapy-resistant human Handgretinger R. Human lymphoid and myeloid cell development
AML stem cells home to and engraft within the bone-marrow in NOD/LtSz-scid IL2R gamma null mice engrafted with mobilized
endosteal region. Nat Biotechnol 2007; 25: 1315-1321 [PMID: human hemopoietic stem cells. J Immunol 2005; 174: 6477-6489
17952057 DOI: 10.1038/nbt1350] [PMID: 15879151 DOI: 10.4049/jimmunol.174.10.6477]
66 Taussig DC, Vargaftig J, Miraki-Moud F, Griessinger E, Sharrock 80 McDermott SP, Eppert K, Lechman ER, Doedens M, Dick JE.
K, Luke T, Lillington D, Oakervee H, Cavenagh J, Agrawal SG, Comparison of human cord blood engraftment between immu
Lister TA, Gribben JG, Bonnet D. Leukemia-initiating cells from nocompromised mouse strains. Blood 2010; 116: 193-200 [PMID:
some acute myeloid leukemia patients with mutated nucleophosmin 20404133 DOI: 10.1182/blood-2010-02-271841]
reside in the CD34(-) fraction. Blood 2010; 115: 1976-1984 [PMID: 81 Rongvaux A, Willinger T, Martinek J, Strowig T, Gearty SV,
20053758 DOI: 10.1182/blood-2009-02-206565] Teichmann LL, Saito Y, Marches F, Halene S, Palucka AK, Manz
67 Civin CI, Almeida-Porada G, Lee MJ, Olweus J, Terstappen LW, MG, Flavell RA. Development and function of human innate
Zanjani ED. Sustained, retransplantable, multilineage engraftment immune cells in a humanized mouse model. Nat Biotechnol 2014;
of highly purified adult human bone marrow stem cells in vivo. 32: 364-372 [PMID: 24633240 DOI: 10.1038/nbt.2858]
Blood 1996; 88: 4102-4109 [PMID: 8943843] 82 Chou FS, Griesinger A, Wunderlich M, Lin S, Link KA, Shrestha
68 Hogan CJ, Shpall EJ, Keller G. Differential long-term and M, Goyama S, Mizukawa B, Shen S, Marcucci G, Mulloy JC.
multilineage engraftment potential from subfractions of human The thrombopoietin/MPL/Bcl-xL pathway is essential for survival
CD34+ cord blood cells transplanted into NOD/SCID mice. Proc and self-renewal in human preleukemia induced by AML1-ETO.
Natl Acad Sci USA 2002; 99: 413-418 [PMID: 11782553 DOI: Blood 2012; 120: 709-719 [PMID: 22337712 DOI: 10.1182/
10.1073/pnas.012336799] blood-2012-01-403212]
69 Jordan CT, Upchurch D, Szilvassy SJ, Guzman ML, Howard 83 Pulikkan JA, Madera D, Xue L, Bradley P, Landrette SF, Kuo
DS, Pettigrew AL, Meyerrose T, Rossi R, Grimes B, Rizzieri DA, YH, Abbas S, Zhu LJ, Valk P, Castilla LH. Thrombopoietin/MPL
Luger SM, Phillips GL. The interleukin-3 receptor alpha chain is a participates in initiating and maintaining RUNX1-ETO acute
unique marker for human acute myelogenous leukemia stem cells. myeloid leukemia via PI3K/AKT signaling. Blood 2012; 120:
Leukemia 2000; 14: 1777-1784 [PMID: 11021753 DOI: 10.1038/ 868-879 [PMID: 22613795 DOI: 10.1182/blood-2012-03-414649]
sj.leu.2401903] 84 Chin DW, Watanabe-Okochi N, Wang CQ, Tergaonkar V, Osato M.
70 Hosen N, Park CY, Tatsumi N, Oji Y, Sugiyama H, Gramatzki M, Mouse models for core binding factor leukemia. Leukemia 2015;
Krensky AM, Weissman IL. CD96 is a leukemic stem cell-specific 29: 1970-1980 [PMID: 26165235 DOI: 10.1038/leu.2015.181]
marker in human acute myeloid leukemia. Proc Natl Acad Sci 85 Lessard J, Sauvageau G. Bmi-1 determines the proliferative
USA 2007; 104: 11008-11013 [PMID: 17576927 DOI: 10.1073/ capacity of normal and leukaemic stem cells. Nature 2003; 423:
pnas.0704271104] 255-260 [PMID: 12714970 DOI: 10.1038/nature01572]
71 van Rhenen A, van Dongen GA, Kelder A, Rombouts EJ, Feller N, 86 Yilmaz OH, Valdez R, Theisen BK, Guo W, Ferguson DO, Wu H,
Moshaver B, Stigter-van Walsum M, Zweegman S, Ossenkoppele Morrison SJ. Pten dependence distinguishes haematopoietic stem
GJ, Jan Schuurhuis G. The novel AML stem cell associated antigen cells from leukaemia-initiating cells. Nature 2006; 441: 475-482
CLL-1 aids in discrimination between normal and leukemic [PMID: 16598206 DOI: 10.1038/nature04703]
stem cells. Blood 2007; 110: 2659-2666 [PMID: 17609428 DOI: 87 Griffin JD, Löwenberg B. Clonogenic cells in acute myeloblastic
10.1182/blood-2007-03-083048] leukemia. Blood 1986; 68: 1185-1195 [PMID: 3535923]
72 Kikushige Y, Shima T, Takayanagi S, Urata S, Miyamoto T, 88 Krivtsov AV, Twomey D, Feng Z, Stubbs MC, Wang Y, Faber J,
Iwasaki H, Takenaka K, Teshima T, Tanaka T, Inagaki Y, Akashi Levine JE, Wang J, Hahn WC, Gilliland DG, Golub TR, Armstrong
K. TIM-3 is a promising target to selectively kill acute myeloid SA. Transformation from committed progenitor to leukaemia stem
leukemia stem cells. Cell Stem Cell 2010; 7: 708-717 [PMID: cell initiated by MLL-AF9. Nature 2006; 442: 818-822 [PMID:
21112565 DOI: 10.1016/j.stem.2010.11.014] 16862118 DOI: 10.1038/nature04980]
WJSC|www.wjgnet.com 327 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
89 Huntly BJ, Shigematsu H, Deguchi K, Lee BH, Mizuno S, Duclos development of clinical trials. Haematologica 2014; 99: 1277-1284
N, Rowan R, Amaral S, Curley D, Williams IR, Akashi K, Gilliland [PMID: 25082785 DOI: 10.3324/haematol.2013.085209]
DG. MOZ-TIF2, but not BCR-ABL, confers properties of leukemic 103 Feller N, van der Pol MA, van Stijn A, Weijers GW, Westra AH,
stem cells to committed murine hematopoietic progenitors. Evertse BW, Ossenkoppele GJ, Schuurhuis GJ. MRD parameters
Cancer Cell 2004; 6: 587-596 [PMID: 15607963 DOI: 10.1016/ using immunophenotypic detection methods are highly reliable in
j.ccr.2004.10.015] predicting survival in acute myeloid leukaemia. Leukemia 2004; 18:
90 Cozzio A, Passegué E, Ayton PM, Karsunky H, Cleary ML, 1380-1390 [PMID: 15201848 DOI: 10.1038/sj.leu.2403405]
Weissman IL. Similar MLL-associated leukemias arising from 104 Venditti A, Buccisano F, Del Poeta G, Maurillo L, Tamburini A,
self-renewing stem cells and short-lived myeloid progenitors. Cox C, Battaglia A, Catalano G, Del Moro B, Cudillo L, Postorino
Genes Dev 2003; 17: 3029-3035 [PMID: 14701873 DOI: 10.1101/ M, Masi M, Amadori S. Level of minimal residual disease after
gad.1143403] consolidation therapy predicts outcome in acute myeloid leukemia.
91 Kvinlaug BT, Chan WI, Bullinger L, Ramaswami M, Sears C, Blood 2000; 96: 3948-3952 [PMID: 11090082]
Foster D, Lazic SE, Okabe R, Benner A, Lee BH, De Silva I, Valk 105 van Rhenen A, Moshaver B, Kelder A, Feller N, Nieuwint AW,
PJ, Delwel R, Armstrong SA, Döhner H, Gilliland DG, Huntly Zweegman S, Ossenkoppele GJ, Schuurhuis GJ. Aberrant marker
BJ. Common and overlapping oncogenic pathways contribute expression patterns on the CD34+CD38- stem cell compartment
to the evolution of acute myeloid leukemias. Cancer Res 2011; in acute myeloid leukemia allows to distinguish the malignant
71: 4117-4129 [PMID: 21505102 DOI: 10.1158/0008-5472. from the normal stem cell compartment both at diagnosis and in
CAN-11-0176] remission. Leukemia 2007; 21: 1700-1707 [PMID: 17525725 DOI:
92 Chen W, Kumar AR, Hudson WA, Li Q, Wu B, Staggs RA, Lund 10.1038/sj.leu.2404754]
EA, Sam TN, Kersey JH. Malignant transformation initiated by 106 Costello RT, Mallet F, Gaugler B, Sainty D, Arnoulet C, Gastaut
Mll-AF9: gene dosage and critical target cells. Cancer Cell 2008; JA, Olive D. Human acute myeloid leukemia CD34+/CD38-
13: 432-440 [PMID: 18455126 DOI: 10.1016/j.ccr.2008.03.005] progenitor cells have decreased sensitivity to chemotherapy and
93 Fialkow PJ, Singer JW, Raskind WH, Adamson JW, Jacobson RJ, Fas-induced apoptosis, reduced immunogenicity, and impaired
Bernstein ID, Dow LW, Najfeld V, Veith R. Clonal development, dendritic cell transformation capacities. Cancer Res 2000; 60:
stem-cell differentiation, and clinical remissions in acute 4403-4411 [PMID: 10969785]
nonlymphocytic leukemia. N Engl J Med 1987; 317: 468-473 107 de Grouw EP, Raaijmakers MH, Boezeman JB, van der Reijden
[PMID: 3614291 DOI: 10.1056/NEJM198708203170802] BA, van de Locht LT, de Witte TJ, Jansen JH, Raymakers RA.
94 Miyamoto T, Weissman IL, Akashi K. AML1/ETO-expressing Preferential expression of a high number of ATP binding cassette
nonleukemic stem cells in acute myelogenous leukemia with 8; transporters in both normal and leukemic CD34+CD38- cells.
21 chromosomal translocation. Proc Natl Acad Sci USA 2000; 97: Leukemia 2006; 20: 750-754 [PMID: 16467867 DOI: 10.1038/
7521-7526 [PMID: 10861016 DOI: 10.1073/pnas.97.13.7521] sj.leu.2404131]
95 Majeti R, Park CY, Weissman IL. Identification of a hierarchy of 108 Bunting KD. ABC transporters as phenotypic markers and
multipotent hematopoietic progenitors in human cord blood. Cell functional regulators of stem cells. Stem Cells 2002; 20: 11-20
Stem Cell 2007; 1: 635-645 [PMID: 18371405 DOI: 10.1016/ [PMID: 11796918 DOI: 10.1002/stem.200011]
j.stem.2007.10.001] 109 de Jonge-Peeters SD, Kuipers F, de Vries EG, Vellenga E. ABC
96 van Rhenen A, Feller N, Kelder A, Westra AH, Rombouts E, transporter expression in hematopoietic stem cells and the role in
Zweegman S, van der Pol MA, Waisfisz Q, Ossenkoppele GJ, AML drug resistance. Crit Rev Oncol Hematol 2007; 62: 214-226
Schuurhuis GJ. High stem cell frequency in acute myeloid leukemia [PMID: 17368038 DOI: 10.1016/j.critrevonc.2007.02.003]
at diagnosis predicts high minimal residual disease and poor 110 Jordan CT. Unique molecular and cellular features of acute
survival. Clin Cancer Res 2005; 11: 6520-6527 [PMID: 16166428 myelogenous leukemia stem cells. Leukemia 2002; 16: 559-562
DOI: 10.1158/1078-0432.CCR-05-0468] [PMID: 11960332 DOI: 10.1038/sj.leu.2402446]
97 Gentles AJ, Plevritis SK, Majeti R, Alizadeh AA. Association of a 111 Chen K, Huang YH, Chen JL. Understanding and targeting
leukemic stem cell gene expression signature with clinical outcomes cancer stem cells: therapeutic implications and challenges. Acta
in acute myeloid leukemia. JAMA 2010; 304: 2706-2715 [PMID: Pharmacol Sin 2013; 34: 732-740 [PMID: 23685952 DOI: 10.1038/
21177505 DOI: 10.1001/jama.2010.1862] aps.2013.27]
98 Eppert K, Takenaka K, Lechman ER, Waldron L, Nilsson B, 112 Guzman ML, Swiderski CF, Howard DS, Grimes BA, Rossi RM,
van Galen P, Metzeler KH, Poeppl A, Ling V, Beyene J, Canty Szilvassy SJ, Jordan CT. Preferential induction of apoptosis for
AJ, Danska JS, Bohlander SK, Buske C, Minden MD, Golub TR, primary human leukemic stem cells. Proc Natl Acad Sci USA 2002;
Jurisica I, Ebert BL, Dick JE. Stem cell gene expression programs 99: 16220-16225 [PMID: 12451177 DOI: 10.1073/pnas.252462599]
influence clinical outcome in human leukemia. Nat Med 2011; 17: 113 Wang JC. Evaluating therapeutic efficacy against cancer stem cells:
1086-1093 [PMID: 21873988 DOI: 10.1038/nm.2415] new challenges posed by a new paradigm. Cell Stem Cell 2007; 1:
99 Pearce DJ, Taussig D, Zibara K, Smith LL, Ridler CM, 497-501 [PMID: 18938746 DOI: 10.1016/j.stem.2007.10.005]
Preudhomme C, Young BD, Rohatiner AZ, Lister TA, Bonnet D. 114 Krivtsov AV, Feng Z, Armstrong SA. Transformation from committed
AML engraftment in the NOD/SCID assay reflects the outcome progenitor to leukemia stem cells. Ann N Y Acad Sci 2009; 1176:
of AML: implications for our understanding of the heterogeneity 144-149 [PMID: 19796242 DOI: 10.1111/j.1749-6632.2009.04966.x]
of AML. Blood 2006; 107: 1166-1173 [PMID: 16234360 DOI: 115 Michnick SW. The connectivity map. Nat Chem Biol 2006; 2:
10.1182/blood-2005-06-2325] 663-664 [PMID: 17108982 DOI: 10.1038/nchembio1206-663]
100 Terwijn M, Zeijlemaker W, Kelder A, Rutten AP, Snel AN, 116 Lamb J, Crawford ED, Peck D, Modell JW, Blat IC, Wrobel
Scholten WJ, Pabst T, Verhoef G, Löwenberg B, Zweegman S, MJ, Lerner J, Brunet JP, Subramanian A, Ross KN, Reich M,
Ossenkoppele GJ, Schuurhuis GJ. Leukemic stem cell frequency: a Hieronymus H, Wei G, Armstrong SA, Haggarty SJ, Clemons PA,
strong biomarker for clinical outcome in acute myeloid leukemia. Wei R, Carr SA, Lander ES, Golub TR. The Connectivity Map:
PLoS One 2014; 9: e107587 [PMID: 25244440 DOI: 10.1371/ using gene-expression signatures to connect small molecules, genes,
journal.pone.0107587] and disease. Science 2006; 313: 1929-1935 [PMID: 17008526 DOI:
101 Vargaftig J, Taussig DC, Griessinger E, Anjos-Afonso F, Lister 10.1126/science.1132939]
TA, Cavenagh J, Oakervee H, Gribben J, Bonnet D. Frequency of 117 Huff CA, Matsui WH, Smith BD, Jones RJ. Strategies to eliminate
leukemic initiating cells does not depend on the xenotransplantation cancer stem cells: clinical implications. Eur J Cancer 2006; 42:
model used. Leukemia 2012; 26: 858-860 [PMID: 21926966 DOI: 1293-1297 [PMID: 16644203 DOI: 10.1016/j.ejca.2006.01.045]
10.1038/leu.2011.250] 118 Walter RB, Appelbaum FR, Estey EH, Bernstein ID. Acute
102 Pollyea DA, Gutman JA, Gore L, Smith CA, Jordan CT. Targeting myeloid leukemia stem cells and CD33-targeted immunotherapy.
acute myeloid leukemia stem cells: a review and principles for the Blood 2012; 119: 6198-6208 [PMID: 22286199 DOI: 10.1182/
WJSC|www.wjgnet.com 328 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
blood-2011-11-325050] in acute myeloid leukemia. N Engl J Med 2009; 361: 1249-1259
119 Cassileth PA, Lynch E, Hines JD, Oken MM, Mazza JJ, Bennett [PMID: 19776406 DOI: 10.1056/NEJMoa0904544]
JM, McGlave PB, Edelstein M, Harrington DP, O’Connell MJ. 132 Lo-Coco F, Cimino G, Breccia M, Noguera NI, Diverio D, Finolezzi E,
Varying intensity of postremission therapy in acute myeloid Pogliani EM, Di Bona E, Micalizzi C, Kropp M, Venditti A, Tafuri A,
leukemia. Blood 1992; 79: 1924-1930 [PMID: 1562720] Mandelli F. Gemtuzumab ozogamicin (Mylotarg) as a single agent for
120 Hewlett J, Kopecky KJ, Head D, Eyre HJ, Elias L, Kingsbury molecularly relapsed acute promyelocytic leukemia. Blood 2004; 104:
L, Balcerzak SP, Dabich L, Hynes H, Bickers JN. A prospective 1995-1999 [PMID: 15187030 DOI: 10.1182/blood-2004-04-1550]
evaluation of the roles of allogeneic marrow transplantation and 133 Breccia M, Cimino G, Diverio D, Gentilini F, Mandelli F, Lo Coco
low-dose monthly maintenance chemotherapy in the treatment of F. Sustained molecular remission after low dose gemtuzumab-
adult acute myelogenous leukemia (AML): a Southwest Oncology ozogamicin in elderly patients with advanced acute promyelocytic
Group study. Leukemia 1995; 9: 562-569 [PMID: 7723385] leukemia. Haematologica 2007; 92: 1273-1274 [PMID: 17768126
121 Jones RJ, Matsui WH, Smith BD. Cancer stem cells: are we DOI: 10.3324/haematol.11329]
missing the target? J Natl Cancer Inst 2004; 96: 583-585 [PMID: 134 Jin L, Lee EM, Ramshaw HS, Busfield SJ, Peoppl AG, Wilkinson
15100335 DOI: 10.1093/jnci/djh095] L, Guthridge MA, Thomas D, Barry EF, Boyd A, Gearing DP, Vairo
122 Sievers EL, Larson RA, Stadtmauer EA, Estey E, Löwenberg B, G, Lopez AF, Dick JE, Lock RB. Monoclonal antibody-mediated
Dombret H, Karanes C, Theobald M, Bennett JM, Sherman ML, targeting of CD123, IL-3 receptor alpha chain, eliminates human
Berger MS, Eten CB, Loken MR, van Dongen JJ, Bernstein ID, acute myeloid leukemic stem cells. Cell Stem Cell 2009; 5: 31-42
Appelbaum FR. Efficacy and safety of gemtuzumab ozogamicin in [PMID: 19570512 DOI: 10.1016/j.stem.2009.04.018]
patients with CD33-positive acute myeloid leukemia in first relapse. 135 Konopleva MY, Jordan CT. Leukemia stem cells and micro
J Clin Oncol 2001; 19: 3244-3254 [PMID: 11432892] environment: biology and therapeutic targeting. J Clin Oncol 2011;
123 Bross PF, Beitz J, Chen G, Chen XH, Duffy E, Kieffer L, Roy S, 29: 591-599 [PMID: 21220598 DOI: 10.1200/JCO.2010.31.0904]
Sridhara R, Rahman A, Williams G, Pazdur R. Approval summary: 136 Frankel A, Liu JS, Rizzieri D, Hogge D. Phase I clinical study of
gemtuzumab ozogamicin in relapsed acute myeloid leukemia. Clin diphtheria toxin-interleukin 3 fusion protein in patients with acute
Cancer Res 2001; 7: 1490-1496 [PMID: 11410481] myeloid leukemia and myelodysplasia. Leuk Lymphoma 2008; 49:
124 Petersdorf SH, Kopecky KJ, Slovak M, Willman C, Nevill T, 543-553 [PMID: 18297533 DOI: 10.1080/10428190701799035]
Brandwein J, Larson RA, Erba HP, Stiff PJ, Stuart RK, Walter 137 Al-Hussaini M, Rettig MP, Ritchey JK, Karpova D, Uy GL,
RB, Tallman MS, Stenke L, Appelbaum FR. A phase 3 study of Eissenberg LG, Gao F, Eades WC, Bonvini E, Chichili GR, Moore
gemtuzumab ozogamicin during induction and postconsolidation PA, Johnson S, Collins L, DiPersio JF. Targeting CD123 in acute
therapy in younger patients with acute myeloid leukemia. myeloid leukemia using a T-cell-directed dual-affinity retargeting
Blood 2013; 121: 4854-4860 [PMID: 23591789 DOI: 10.1182/ platform. Blood 2016; 127: 122-131 [PMID: 26531164 DOI:
blood-2013-01-466706] 10.1182/blood-2014-05-575704]
125 Burnett AK, Hills RK, Milligan D, Kjeldsen L, Kell J, Russell 138 Zhou J, Chng WJ. Identification and targeting leukemia stem cells:
NH, Yin JA, Hunter A, Goldstone AH, Wheatley K. Identification The path to the cure for acute myeloid leukemia. World J Stem Cells
of patients with acute myeloblastic leukemia who benefit from the 2014; 6: 473-484 [PMID: 25258669 DOI: 10.4252/wjsc.v6.i4.473]
addition of gemtuzumab ozogamicin: results of the MRC AML15 139 Gadhoum Z, Delaunay J, Maquarre E, Durand L, Lancereaux
trial. J Clin Oncol 2011; 29: 369-377 [PMID: 21172891 DOI: V, Qi J, Robert-Lezenes J, Chomienne C, Smadja-Joffe F. The
10.1200/JCO.2010.31.4310] effect of anti-CD44 monoclonal antibodies on differentiation
126 Castaigne S, Pautas C, Terré C, Raffoux E, Bordessoule D, Bastie and proliferation of human acute myeloid leukemia cells. Leuk
JN, Legrand O, Thomas X, Turlure P, Reman O, de Revel T, Gastaud Lymphoma 2004; 45: 1501-1510 [PMID: 15370200 DOI: 10.1080/
L, de Gunzburg N, Contentin N, Henry E, Marolleau JP, Aljijakli 1042819042000206687]
A, Rousselot P, Fenaux P, Preudhomme C, Chevret S, Dombret H. 140 Jaiswal S, Jamieson CH, Pang WW, Park CY, Chao MP, Majeti R,
Effect of gemtuzumab ozogamicin on survival of adult patients with Traver D, van Rooijen N, Weissman IL. CD47 is upregulated on
de-novo acute myeloid leukaemia (ALFA-0701): a randomised, circulating hematopoietic stem cells and leukemia cells to avoid
open-label, phase 3 study. Lancet 2012; 379: 1508-1516 [PMID: phagocytosis. Cell 2009; 138: 271-285 [PMID: 19632178 DOI:
22482940 DOI: 10.1016/S0140-6736(12)60485-1] 10.1016/j.cell.2009.05.046]
127 Hills RK, Castaigne S, Appelbaum FR, Delaunay J, Petersdorf 141 Liu J, Wang L, Zhao F, Tseng S, Narayanan C, Shura L,
S, Othus M, Estey EH, Dombret H, Chevret S, Ifrah N, Cahn Willingham S, Howard M, Prohaska S, Volkmer J, Chao M,
JY, Récher C, Chilton L, Moorman AV, Burnett AK. Addition Weissman IL, Majeti R. Pre-Clinical Development of a Humanized
of gemtuzumab ozogamicin to induction chemotherapy in Anti-CD47 Antibody with Anti-Cancer Therapeutic Potential. PLoS
adult patients with acute myeloid leukaemia: a meta-analysis of One 2015; 10: e0137345 [PMID: 26390038 DOI: 10.1371/journal.
individual patient data from randomised controlled trials. Lancet pone.0137345]
Oncol 2014; 15: 986-996 [PMID: 25008258 DOI: 10.1016/ 142 Shen M, Schmitt S, Buac D, Dou QP. Targeting the ubiquitin-
S1470-2045(14)70281-5] proteasome system for cancer therapy. Expert Opin Ther Targets
128 Burnett AK, Russell NH, Hills RK, Kell J, Freeman S, Kjeldsen L, 2013; 17: 1091-1108 [PMID: 23822887 DOI: 10.1517/14728222.2
Hunter AE, Yin J, Craddock CF, Dufva IH, Wheatley K, Milligan 013.815728]
D. Addition of gemtuzumab ozogamicin to induction chemotherapy 143 Attar EC, De Angelo DJ, Supko JG, D’Amato F, Zahrieh D,
improves survival in older patients with acute myeloid leukemia. J Sirulnik A, Wadleigh M, Ballen KK, McAfee S, Miller KB, Levine
Clin Oncol 2012; 30: 3924-3931 [PMID: 22851554 DOI: 10.1200/ J, Galinsky I, Trehu EG, Schenkein D, Neuberg D, Stone RM,
JCO.2012.42.2964] Amrein PC. Phase I and pharmacokinetic study of bortezomib in
129 Bernstein ID. Monoclonal antibodies to the myeloid stem cells: combination with idarubicin and cytarabine in patients with acute
therapeutic implications of CMA-676, a humanized anti-CD33 myelogenous leukemia. Clin Cancer Res 2008; 14: 1446-1454
antibody calicheamicin conjugate. Leukemia 2000; 14: 474-475 [PMID: 18316568 DOI: 10.1158/1078-0432.CCR-07-4626]
[PMID: 10720144 DOI: 10.1038/sj.leu.2401663] 144 Attar EC, Johnson JL, Amrein PC, Lozanski G, Wadleigh M,
130 Rowe JM, Löwenberg B. Gemtuzumab ozogamicin in acute DeAngelo DJ, Kolitz JE, Powell BL, Voorhees P, Wang ES, Blum
myeloid leukemia: a remarkable saga about an active drug. W, Stone RM, Marcucci G, Bloomfield CD, Moser B, Larson RA.
Blood 2013; 121: 4838-4841 [PMID: 23591788 DOI: 10.1182/ Bortezomib added to daunorubicin and cytarabine during induction
blood-2013-03-490482] therapy and to intermediate-dose cytarabine for consolidation in
131 Fernandez HF, Sun Z, Yao X, Litzow MR, Luger SM, Paietta patients with previously untreated acute myeloid leukemia age 60 to
EM, Racevskis J, Dewald GW, Ketterling RP, Bennett JM, Rowe 75 years: CALGB (Alliance) study 10502. J Clin Oncol 2013; 31:
JM, Lazarus HM, Tallman MS. Anthracycline dose intensification 923-929 [PMID: 23129738 DOI: 10.1200/JCO.2012.45.2177]
WJSC|www.wjgnet.com 329 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
145 Blum W, Schwind S, Tarighat SS, Geyer S, Eisfeld AK, Whitman 157 Krawczyk J, Keane N, Swords R, O’Dwyer M, Freeman CL,
S, Walker A, Klisovic R, Byrd JC, Santhanam R, Wang H, Curfman Giles FJ. Perifosine--a new option in treatment of acute myeloid
JP, Devine SM, Jacob S, Garr C, Kefauver C, Perrotti D, Chan KK, leukemia? Expert Opin Investig Drugs 2013; 22: 1315-1327 [PMID:
Bloomfield CD, Caligiuri MA, Grever MR, Garzon R, Marcucci 23931614 DOI: 10.1517/13543784.2013.826648]
G. Clinical and pharmacodynamic activity of bortezomib and 158 Altman JK, Sassano A, Platanias LC. Targeting mTOR for the
decitabine in acute myeloid leukemia. Blood 2012; 119: 6025-6031 treatment of AML. New agents and new directions. Oncotarget
[PMID: 22566605 DOI: 10.1182/blood-2012-03-413898] 2011; 2: 510-517 [PMID: 21680954 DOI: 10.18632/oncotarget.290]
146 Lancet JE, Duong VH, Winton EF, Stuart RK, Burton M, Zhang S, 159 Moore J, Seiter K, Kolitz J, Stock W, Giles F, Kalaycio M, Zenk
Cubitt C, Blaskovich MA, Wright JJ, Sebti S, Sullivan DM. A phase D, Marcucci G. A Phase II study of Bcl-2 antisense (oblimersen
I clinical-pharmacodynamic study of the farnesyltransferase inhibitor sodium) combined with gemtuzumab ozogamicin in older patients
tipifarnib in combination with the proteasome inhibitor bortezomib with acute myeloid leukemia in first relapse. Leuk Res 2006; 30:
in advanced acute leukemias. Clin Cancer Res 2011; 17: 1140-1146 777-783 [PMID: 16730060 DOI: 10.1016/j.leukres.2005.10.025]
[PMID: 21233404 DOI: 10.1158/1078-0432.CCR-10-1878] 160 Marcucci G, Moser B, Blum W, Stock W, Wetzler M, Kolitz JE,
147 Walker AR, Klisovic RB, Garzon R, Schaaf LJ, Humphries K, Devine Thakuri M, Carter T, Stuart RK, Larson RA. A phase III randomized
SM, Byrd JC, Grever MR, Marcucci G, Blum W. Phase I study of trial of intensive induction and consolidation chemotherapy { /-}
azacitidine and bortezomib in adults with relapsed or refractory acute oblimersen, a pro-apoptotic Bcl-2 antisense oligonucleotide in
myeloid leukemia. Leuk Lymphoma 2014; 55: 1304-1308 [PMID: untreated acute myeloid leukemia patients >60 years old. J Clin
23952243 DOI: 10.3109/10428194.2013.833333] Oncol 2007; 25 (June 20 Supplement): 7012
148 Guzman ML, Rossi RM, Neelakantan S, Li X, Corbett CA, 161 Rahmani M, Aust MM, Attkisson E, Williams DC, Ferreira-
Hassane DC, Becker MW, Bennett JM, Sullivan E, Lachowicz Gonzalez A, Grant S. Inhibition of Bcl-2 antiapoptotic members
JL, Vaughan A, Sweeney CJ, Matthews W, Carroll M, Liesveld by obatoclax potently enhances sorafenib-induced apoptosis in
JL, Crooks PA, Jordan CT. An orally bioavailable parthenolide human myeloid leukemia cells through a Bim-dependent process.
analog selectively eradicates acute myelogenous leukemia stem and Blood 2012; 119: 6089-6098 [PMID: 22446485 DOI: 10.1182/
progenitor cells. Blood 2007; 110: 4427-4435 [PMID: 17804695 blood-2011-09-378141]
DOI: 10.1182/blood-2007-05-090621] 162 Xie C, Edwards H, Caldwell JT, Wang G, Taub JW, Ge Y. Obatoclax
149 Hassane DC, Sen S, Minhajuddin M, Rossi RM, Corbett CA, Balys potentiates the cytotoxic effect of cytarabine on acute myeloid
M, Wei L, Crooks PA, Guzman ML, Jordan CT. Chemical genomic leukemia cells by enhancing DNA damage. Mol Oncol 2015; 9:
screening reveals synergism between parthenolide and inhibitors of 409-421 [PMID: 25308513 DOI: 10.1016/j.molonc.2014.09.008]
the PI-3 kinase and mTOR pathways. Blood 2010; 116: 5983-5990 163 Schimmer AD, Raza A, Carter TH, Claxton D, Erba H, DeAngelo
[PMID: 20889920 DOI: 10.1182/blood-2010-04-278044] DJ, Tallman MS, Goard C, Borthakur G. A multicenter phase
150 Sethi G, Ahn KS, Pandey MK, Aggarwal BB. Celastrol, a novel I/II study of obatoclax mesylate administered as a 3- or 24-hour
triterpene, potentiates TNF-induced apoptosis and suppresses infusion in older patients with previously untreated acute myeloid
invasion of tumor cells by inhibiting NF-kappaB-regulated gene leukemia. PLoS One 2014; 9: e108694 [PMID: 25285531 DOI:
products and TAK1-mediated NF-kappaB activation. Blood 2007; 10.1371/journal.pone.0108694]
109: 2727-2735 [PMID: 17110449] 164 Adams GB, Martin RP, Alley IR, Chabner KT, Cohen KS, Calvi
151 Page S, Fischer C, Baumgartner B, Haas M, Kreusel U, Loidl LM, Kronenberg HM, Scadden DT. Therapeutic targeting of a stem
G, Hayn M, Ziegler-Heitbrock HW, Neumeier D, Brand K. cell niche. Nat Biotechnol 2007; 25: 238-243 [PMID: 17237769
4-Hydroxynonenal prevents NF-kappaB activation and tumor DOI: 10.1038/nbt1281]
necrosis factor expression by inhibiting IkappaB phosphorylation 165 Saito Y, Uchida N, Tanaka S, Suzuki N, Tomizawa-Murasawa M,
and subsequent proteolysis. J Biol Chem 1999; 274: 11611-11618 Sone A, Najima Y, Takagi S, Aoki Y, Wake A, Taniguchi S, Shultz
[PMID: 10206970 DOI: 10.1074/jbc.274.17.11611] LD, Ishikawa F. Induction of cell cycle entry eliminates human
152 Siow RC, Ishii T, Mann GE. Modulation of antioxidant gene leukemia stem cells in a mouse model of AML. Nat Biotechnol
expression by 4-hydroxynonenal: atheroprotective role of the Nrf2/ 2010; 28: 275-280 [DOI: 10.1038/nbt.1607]
ARE transcription pathway. Redox Rep 2007; 12: 11-15 [PMID: 166 Löwenberg B, van Putten W, Theobald M, Gmür J, Verdonck
17263901 DOI: 10.1179/135100007X162167] L, Sonneveld P, Fey M, Schouten H, de Greef G, Ferrant A,
153 Allegretti M, Ricciardi MR, Licchetta R, Mirabilii S, Orecchioni S, Kovacsovics T, Gratwohl A, Daenen S, Huijgens P, Boogaerts
Reggiani F, Talarico G, Foà R, Bertolini F, Amadori S, Torrisi MR, M. Effect of priming with granulocyte colony-stimulating factor
Tafuri A. The pan-class I phosphatidyl-inositol-3 kinase inhibitor on the outcome of chemotherapy for acute myeloid leukemia. N
NVP-BKM120 demonstrates anti-leukemic activity in acute Engl J Med 2003; 349: 743-752 [PMID: 12930926 DOI: 10.1056/
myeloid leukemia. Sci Rep 2015; 5: 18137 [PMID: 26674543 DOI: NEJMoa025406]
10.1038/srep18137] 167 Estey EH, Thall PF, Pierce S, Cortes J, Beran M, Kantarjian H,
154 Lannutti BJ, Meadows SA, Herman SE, Kashishian A, Steiner Keating MJ, Andreeff M, Freireich E. Randomized phase II study of
B, Johnson AJ, Byrd JC, Tyner JW, Loriaux MM, Deininger M, fludarabine + cytosine arabinoside + idarubicin +/- all-trans retinoic
Druker BJ, Puri KD, Ulrich RG, Giese NA. CAL-101, a p110delta acid +/- granulocyte colony-stimulating factor in poor prognosis
selective phosphatidylinositol-3-kinase inhibitor for the treatment of newly diagnosed acute myeloid leukemia and myelodysplastic
B-cell malignancies, inhibits PI3K signaling and cellular viability. syndrome. Blood 1999; 93: 2478-2484 [PMID: 10194425]
Blood 2011; 117: 591-594 [PMID: 20959606 DOI: 10.1182/ 168 Milligan DW, Wheatley K, Littlewood T, Craig JI, Burnett AK.
blood-2010-03-275305] Fludarabine and cytosine are less effective than standard ADE
155 Lu JW, Lin YM, Lai YL, Chen CY, Hu CY, Tien HF, Ou DL, chemotherapy in high-risk acute myeloid leukemia, and addition of
Lin LI. MK-2206 induces apoptosis of AML cells and enhances G-CSF and ATRA are not beneficial: results of the MRC AML-HR
the cytotoxicity of cytarabine. Med Oncol 2015; 32: 206 [PMID: randomized trial. Blood 2006; 107: 4614-4622 [PMID: 16484584
26087957 DOI: 10.1007/s12032-015-0650-7] DOI: 10.1182/blood-2005-10-4202]
156 Konopleva MY, Walter RB, Faderl SH, Jabbour EJ, Zeng Z, 169 Tavor S, Petit I, Porozov S, Avigdor A, Dar A, Leider-Trejo L,
Borthakur G, Huang X, Kadia TM, Ruvolo PP, Feliu JB, Lu H, Shemtov N, Deutsch V, Naparstek E, Nagler A, Lapidot T. CXCR4
Debose L, Burger JA, Andreeff M, Liu W, Baggerly KA, Kornblau regulates migration and development of human acute myelogenous
SM, Doyle LA, Estey EH, Kantarjian HM. Preclinical and early leukemia stem cells in transplanted NOD/SCID mice. Cancer Res
clinical evaluation of the oral AKT inhibitor, MK-2206, for the 2004; 64: 2817-2824 [PMID: 15087398 DOI: 10.1158/0008-5472.
treatment of acute myelogenous leukemia. Clin Cancer Res 2014; CAN-03-3693]
20: 2226-2235 [PMID: 24583795 DOI: 10.1158/1078-0432. 170 Zeng Z, Shi YX, Samudio IJ, Wang RY, Ling X, Frolova O,
CCR-13-1978] Levis M, Rubin JB, Negrin RR, Estey EH, Konoplev S, Andreeff
WJSC|www.wjgnet.com 330 October 26, 2016|Volume 8|Issue 10|
Stahl M et al . AML stem cells
M, Konopleva M. Targeting the leukemia microenvironment by 175 Naugler WE, Karin M. NF-kappaB and cancer-identifying targets
CXCR4 inhibition overcomes resistance to kinase inhibitors and and mechanisms. Curr Opin Genet Dev 2008; 18: 19-26 [PMID:
chemotherapy in AML. Blood 2009; 113: 6215-6224 [PMID: 18440219 DOI: 10.1016/j.gde.2008.01.020]
18955566 DOI: 10.1182/blood-2008-05-158311] 176 Guzman ML, Rossi RM, Karnischky L, Li X, Peterson DR,
171 Uy GL, Rettig MP, Motabi IH, McFarland K, Trinkaus KM, Hladnik Howard DS, Jordan CT. The sesquiterpene lactone parthenolide
LM, Kulkarni S, Abboud CN, Cashen AF, Stockerl-Goldstein KE, Vij induces apoptosis of human acute myelogenous leukemia stem and
R, Westervelt P, DiPersio JF. A phase 1/2 study of chemosensitization progenitor cells. Blood 2005; 105: 4163-4169 [PMID: 15687234
with the CXCR4 antagonist plerixafor in relapsed or refractory acute DOI: 10.1182/blood-2004-10-4135]
myeloid leukemia. Blood 2012; 119: 3917-3924 [PMID: 22308295 177 Liesveld JL, Rosell KE, Lu C, Bechelli J, Phillips G, Lancet JE,
DOI: 10.1182/blood-2011-10-383406] Abboud CN. Acute myelogenous leukemia--microenvironment
172 Kuhne MR, Mulvey T, Belanger B, Chen S, Pan C, Chong C, Cao F, interactions: role of endothelial cells and proteasome inhibition.
Niekro W, Kempe T, Henning KA, Cohen LJ, Korman AJ, Cardarelli Hematology 2005; 10: 483-494 [PMID: 16321813 DOI: 10.1080/10
PM. BMS-936564/MDX-1338: a fully human anti-CXCR4 antibody 245330500233452]
induces apoptosis in vitro and shows antitumor activity in vivo in 178 Mohty M, Duarte RF, Croockewit S, Hübel K, Kvalheim G, Russell
hematologic malignancies. Clin Cancer Res 2013; 19: 357-366 N. The role of plerixafor in optimizing peripheral blood stem cell
[PMID: 23213054 DOI: 10.1158/1078-0432.CCR-12-2333] mobilization for autologous stem cell transplantation. Leukemia
173 Zohren F, Toutzaris D, Klärner V, Hartung HP, Kieseier B, Haas 2011; 25: 1-6 [PMID: 21224858 DOI: 10.1038/leu.2010.224]
R. The monoclonal anti-VLA-4 antibody natalizumab mobilizes 179 Broxmeyer HE, Orschell CM, Clapp DW, Hangoc G, Cooper
CD34+ hematopoietic progenitor cells in humans. Blood 2008; 111: S, Plett PA, Liles WC, Li X, Graham-Evans B, Campbell TB,
3893-3895 [PMID: 18235044 DOI: 10.1182/blood-2007-10-120329] Calandra G, Bridger G, Dale DC, Srour EF. Rapid mobilization of
174 Hsieh YT, Jiang E, Pham J, Kim HN, Abdel-Azim H, Khazal S, murine and human hematopoietic stem and progenitor cells with
Bug G, Spohn G, Bonig H, Kim YM. VLA4 Blockade In Acute AMD3100, a CXCR4 antagonist. J Exp Med 2005; 201: 1307-1318
Myeloid Leukemia. Blood 2013; 122: 3944 [PMID: 15837815 DOI: 10.1084/jem.20041385]
P- Reviewer: Kita K, Li ZJ, Ramírez M, Shao R S- Editor: Ji FF
L- Editor: A E- Editor: Wu HL
WJSC|www.wjgnet.com 331 October 26, 2016|Volume 8|Issue 10|
Published by Baishideng Publishing Group Inc
8226 Regency Drive, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx
http://www.wjgnet.com
© 2016 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- Cancer Stem Cells ThesisDocument8 pagesCancer Stem Cells Thesisafknekkfs100% (1)
- Luna 2016Document34 pagesLuna 2016Jocilene Dantas Torres NascimentoNo ratings yet
- Cancer Stem Cells in Basic Science and in Translational Oncology: Can We Translate Into Clinical Application?Document21 pagesCancer Stem Cells in Basic Science and in Translational Oncology: Can We Translate Into Clinical Application?Raedy SusantoNo ratings yet
- Cancer Stem Cell Scientific Literature ReviewDocument5 pagesCancer Stem Cell Scientific Literature Reviewc5r3aep1100% (1)
- Cancer Stem Cell Hypothesis: Implication For Cancer Prevention and TreatmentDocument16 pagesCancer Stem Cell Hypothesis: Implication For Cancer Prevention and TreatmentlaurentiaNo ratings yet
- Mesenchymal Stem Cell Mediated Cancer Therapy CryovidaDocument8 pagesMesenchymal Stem Cell Mediated Cancer Therapy CryovidaJob MonobeNo ratings yet
- Fimmu 11 01280Document33 pagesFimmu 11 01280arifudin_achmadNo ratings yet
- Cancer Stem Cell Niche The Place To BeDocument7 pagesCancer Stem Cell Niche The Place To BeAlejandra Isabel Juarez JimenezNo ratings yet
- Stem Cell CancerDocument33 pagesStem Cell CancerRobby Rajatul AswadNo ratings yet
- Cancer Stem Cells and Evolving Novel Therapies: A Paradigm ShiftDocument6 pagesCancer Stem Cells and Evolving Novel Therapies: A Paradigm Shifttarry girothNo ratings yet
- Cancer Stem CellsDocument9 pagesCancer Stem CellsBasant Hamdy AbuZaidNo ratings yet
- Cancer Stem Cell ThesisDocument6 pagesCancer Stem Cell ThesisBestPaperWritingServiceReviewsToledo100% (2)
- Cancer Stem Cells Theories and PracticeDocument472 pagesCancer Stem Cells Theories and PracticeIndera VyasNo ratings yet
- Breast Cancer Stem CellsDocument6 pagesBreast Cancer Stem CellsTri Cahya MettaNo ratings yet
- CD96 Is A Leukemic Stem Cell-Specific Marker in HuDocument7 pagesCD96 Is A Leukemic Stem Cell-Specific Marker in HuLuis Alberto Sanchez VilelaNo ratings yet
- Stem Cell Concepts Renew Cancer Research: ASH 50th Anniversary ReviewDocument15 pagesStem Cell Concepts Renew Cancer Research: ASH 50th Anniversary ReviewbloodbenderNo ratings yet
- Neuro-Oncology: Stem Cell-Based Therapies For Tumors in The Brain: Are We There Yet?Document13 pagesNeuro-Oncology: Stem Cell-Based Therapies For Tumors in The Brain: Are We There Yet?Vinnie Juliana YonatanNo ratings yet
- The Biology and Clinical Potential of Circulating Tumor CellsDocument18 pagesThe Biology and Clinical Potential of Circulating Tumor CellssmakinpanglinkNo ratings yet
- Cancer 1Document8 pagesCancer 1JoseRodrigoSuarezCamposNo ratings yet
- Frontiers in Bioscience E4, 2502-2514, June 1, 2012Document13 pagesFrontiers in Bioscience E4, 2502-2514, June 1, 2012ginocolaciccoNo ratings yet
- Myeloid Cell Origins, Differentiation, and Clinical ImplicationsDocument18 pagesMyeloid Cell Origins, Differentiation, and Clinical ImplicationsWendy PNo ratings yet
- Cancer Stem Cells: Targeting the Roots of Cancer, Seeds of Metastasis, and Sources of Therapy ResistanceFrom EverandCancer Stem Cells: Targeting the Roots of Cancer, Seeds of Metastasis, and Sources of Therapy ResistanceHuiping LiuNo ratings yet
- Cancer Stem CellsDocument9 pagesCancer Stem CellsDaniel PricopNo ratings yet
- Articulo 1Document17 pagesArticulo 1Andrea NeriaNo ratings yet
- Breast Cancer and Cancer Stem Cells: A Mini-Review: Tu Mo Ri, 100: 363-369, 2014Document7 pagesBreast Cancer and Cancer Stem Cells: A Mini-Review: Tu Mo Ri, 100: 363-369, 2014Ava BaranNo ratings yet
- Cancer y Celulas Madre 2022Document11 pagesCancer y Celulas Madre 2022Jose EdgarNo ratings yet
- LungDocument6 pagesLungWidia MeliawatiNo ratings yet
- Stem CellsDocument9 pagesStem CellsMaria Del Mar RoblesNo ratings yet
- Understanding and Targeting Cancer Stem Cells Therapeutic Implications and ChallengesDocument9 pagesUnderstanding and Targeting Cancer Stem Cells Therapeutic Implications and ChallengesMariano PerezNo ratings yet
- Cancer Stem CellsDocument14 pagesCancer Stem CellsShivani SinghNo ratings yet
- Cancer Stem CellsDocument8 pagesCancer Stem CellsAna Paula CoronelNo ratings yet
- Cancer Stem Cells Revisited: ReviewDocument8 pagesCancer Stem Cells Revisited: ReviewJoyatideb SinhaNo ratings yet
- Cancer Stem Cells PresentationDocument27 pagesCancer Stem Cells PresentationshaanbhagatNo ratings yet
- Review: Cells of Origin in CancerDocument9 pagesReview: Cells of Origin in CancerJohn TikasNo ratings yet
- Stem Cells in Solid Tumors Cancer Stem Cell (CSC)Document37 pagesStem Cells in Solid Tumors Cancer Stem Cell (CSC)MuralidharanNo ratings yet
- 3-Mesenchimal Stem Cell DevelopmentDocument10 pages3-Mesenchimal Stem Cell Developmentabdulloh suyutiNo ratings yet
- Dominici 2006Document3 pagesDominici 2006alverina odeNo ratings yet
- 1-0articulo MM, PiRNA-823 (Myeloid-Derived Suppressor Cells Endow)Document12 pages1-0articulo MM, PiRNA-823 (Myeloid-Derived Suppressor Cells Endow)Jhonathan David Guevara RamirezNo ratings yet
- 2207 14435 1 PBDocument1 page2207 14435 1 PBJuan Sebastian YakisichNo ratings yet
- Idikio 2011Document9 pagesIdikio 2011Rizka Hadian PermanaNo ratings yet
- Cancer CellsDocument4 pagesCancer CellsJeanette NarteaNo ratings yet
- Cancer Stem Cells: From Birth To DeathDocument30 pagesCancer Stem Cells: From Birth To DeathDito AnurogoNo ratings yet
- Jurnal PDFDocument12 pagesJurnal PDFJanet UngNo ratings yet
- Cytometry PT A - 2018 - Aanei - Evaluation of Bone Marrow Microenvironment Could Change How Myelodysplastic Syndromes AreDocument14 pagesCytometry PT A - 2018 - Aanei - Evaluation of Bone Marrow Microenvironment Could Change How Myelodysplastic Syndromes AreCarmen AaneiNo ratings yet
- Stem CellDocument13 pagesStem CellVinnie Juliana YonatanNo ratings yet
- Cells 10 01043 v2Document17 pagesCells 10 01043 v2marina ruzyatiNo ratings yet
- Preprints202010 0623 v1Document35 pagesPreprints202010 0623 v1JubairNo ratings yet
- Safari - 17 Okt 2019 05.51Document1 pageSafari - 17 Okt 2019 05.51dian siswojoNo ratings yet
- 2019 Article 73Document10 pages2019 Article 73Radu AvramNo ratings yet
- Nevus Melanocitico-Nevogenesis y MelanogenesisDocument16 pagesNevus Melanocitico-Nevogenesis y Melanogenesiscarmen lopezNo ratings yet
- Fphar 09 00259Document10 pagesFphar 09 00259leartaNo ratings yet
- Stem Cells, Cancer, and Cancer Stem Cells: InsightDocument7 pagesStem Cells, Cancer, and Cancer Stem Cells: InsightMekki Lazir IlhdafNo ratings yet
- Fundamental Principles of Stem Cell BankingDocument15 pagesFundamental Principles of Stem Cell BankingRizky RamadhaniNo ratings yet
- CSC Colorectal 7Document8 pagesCSC Colorectal 7dianaNo ratings yet
- Biology For EngineersDocument15 pagesBiology For Engineerskoushikmondal4507No ratings yet
- Stem Cells in Breast Tumours - Are They Ready For The Clinicď Ą, 2012Document13 pagesStem Cells in Breast Tumours - Are They Ready For The Clinicď Ą, 2012Daniela GologanNo ratings yet
- Histological, Molecular and Functional SubtypesDocument7 pagesHistological, Molecular and Functional SubtypesCristopherJairEstupiñanVirúNo ratings yet
- Mesenchymal Stromal Cells as Tumor Stromal ModulatorsFrom EverandMesenchymal Stromal Cells as Tumor Stromal ModulatorsMarcela BolontradeNo ratings yet
- Nilai Respon FARMAKOKINETIK Kelas C 2018Document5 pagesNilai Respon FARMAKOKINETIK Kelas C 2018Mini Bekti NingsihNo ratings yet
- Absen Kelas C 2017-1Document3 pagesAbsen Kelas C 2017-1Mini Bekti NingsihNo ratings yet
- Comparative Studies On Povidone-Iodine Ointment and Gel: IJPSR (2012), Vol. 3, Issue 11 (Research Article)Document7 pagesComparative Studies On Povidone-Iodine Ointment and Gel: IJPSR (2012), Vol. 3, Issue 11 (Research Article)Mini Bekti NingsihNo ratings yet
- Ijpr 14 1015Document16 pagesIjpr 14 1015jackeiNo ratings yet
- Comparative Studies On Povidone-Iodine Ointment and GelDocument8 pagesComparative Studies On Povidone-Iodine Ointment and GelMini Bekti NingsihNo ratings yet
- Daftar Pustaka No. 1 Bagian ADocument1 pageDaftar Pustaka No. 1 Bagian AMini Bekti NingsihNo ratings yet
- Sample Chapter PDFDocument12 pagesSample Chapter PDFMini Bekti NingsihNo ratings yet
- Sibbald RG Et All, 2011Document6 pagesSibbald RG Et All, 2011safiraNo ratings yet
- 2015 Article 1030 PDFDocument15 pages2015 Article 1030 PDFMini Bekti NingsihNo ratings yet
- Drug Repurposing For The Treatment of Acute Myeloid LeukemiaDocument11 pagesDrug Repurposing For The Treatment of Acute Myeloid LeukemiaMini Bekti NingsihNo ratings yet
- F1000research 7 15353 PDFDocument14 pagesF1000research 7 15353 PDFMini Bekti NingsihNo ratings yet
- Post-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyDocument8 pagesPost-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyMini Bekti NingsihNo ratings yet
- Hoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFDocument9 pagesHoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFMini Bekti NingsihNo ratings yet
- 15.shelke Usha Y. Mahajan Ashish A.Document23 pages15.shelke Usha Y. Mahajan Ashish A.Mahdhun ShiddiqNo ratings yet
- Formulasi Dan Evaluasi Sediaan Lotion Dari Ekstrak PDFDocument7 pagesFormulasi Dan Evaluasi Sediaan Lotion Dari Ekstrak PDFMini Bekti NingsihNo ratings yet
- Pone 0119497 PDFDocument11 pagesPone 0119497 PDFMini Bekti NingsihNo ratings yet
- Salep Daun NangkaDocument5 pagesSalep Daun NangkaDianti Yuni Lestari IINo ratings yet
- PVP Iodine 10%Document1 pagePVP Iodine 10%Trần Văn LộcNo ratings yet
- Hajaratumar DoddamaniDocument82 pagesHajaratumar DoddamaniMini Bekti NingsihNo ratings yet
- Acute Myeloid LeukemiaDocument11 pagesAcute Myeloid LeukemiaAndi SusiloNo ratings yet
- Ijh 05 143 PDFDocument22 pagesIjh 05 143 PDFMini Bekti NingsihNo ratings yet
- O1a1 17 103 Mini Bekti NingsihDocument9 pagesO1a1 17 103 Mini Bekti NingsihMini Bekti NingsihNo ratings yet
- Schena EJPP2004Document16 pagesSchena EJPP2004Mini Bekti NingsihNo ratings yet
- Arrival Guide To MalaysiaDocument2 pagesArrival Guide To Malaysiaamanu092No ratings yet
- Midterm Requirement-Green BuildingDocument7 pagesMidterm Requirement-Green BuildingJo-anne RiveraNo ratings yet
- Octavia Tour BrochureDocument9 pagesOctavia Tour BrochureOvidiuIONo ratings yet
- Kaos PriaDocument133 pagesKaos PriaUrieNo ratings yet
- Bio 2Document3 pagesBio 2ganchimeg gankhuuNo ratings yet
- Slender Quest DetailsDocument1 pageSlender Quest Detailsparents021No ratings yet
- DAFTARRUJUKANDocument4 pagesDAFTARRUJUKANIndahNo ratings yet
- Aerobic ActivitiesExercises PDFDocument14 pagesAerobic ActivitiesExercises PDFPalma, Arrabela M.No ratings yet
- Elecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationDocument5 pagesElecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationIsmael CulquiNo ratings yet
- Substation Basic PDFDocument6 pagesSubstation Basic PDFSaraswatapalitNo ratings yet
- 1978 - Behavior Analysis and Behavior Modification - Mallot, Tillema & Glenn PDFDocument499 pages1978 - Behavior Analysis and Behavior Modification - Mallot, Tillema & Glenn PDFKrusovice15No ratings yet
- Alabama Religious Exemption AdvisoryDocument1 pageAlabama Religious Exemption AdvisoryABC 33/40No ratings yet
- List of Grocery Importers in Austria Europe PDF FreeDocument11 pagesList of Grocery Importers in Austria Europe PDF FreeEmpy SumardiNo ratings yet
- Dr. Ashraf Sayeed: Department of OphthalmologyDocument49 pagesDr. Ashraf Sayeed: Department of Ophthalmologysaiful haque100% (1)
- (Nikolaj Wolfson, Alexander Lerner, Leonid Roshal (B-Ok - CC)Document589 pages(Nikolaj Wolfson, Alexander Lerner, Leonid Roshal (B-Ok - CC)Andi sutandi100% (1)
- Goat Science and Production PDFDocument446 pagesGoat Science and Production PDFRiyaz Khan100% (1)
- 2 TABLE 1.1. Key Events in The Development of Cell and Tissue CultureDocument1 page2 TABLE 1.1. Key Events in The Development of Cell and Tissue CultureCatalina ColoradoNo ratings yet
- Invoice, packing list mẫuDocument2 pagesInvoice, packing list mẫuPHI BUI MINHNo ratings yet
- First Quarter Examination For AP 10Document4 pagesFirst Quarter Examination For AP 10Reynan Orillos HorohoroNo ratings yet
- Glare CompositeDocument10 pagesGlare Compositewsjouri2510No ratings yet
- Oedipus SummaryDocument1 pageOedipus SummaryReynold FrancoNo ratings yet
- Aaron Magana's Resume, Business AnalystDocument3 pagesAaron Magana's Resume, Business AnalystEmiNo ratings yet
- Bộ Đề Ôn Tập HK1 (Kèm Lời Giải Chi Tiết)Document51 pagesBộ Đề Ôn Tập HK1 (Kèm Lời Giải Chi Tiết)Lê Thị Ngọc AnhNo ratings yet
- JSLHR Author InstructionsDocument14 pagesJSLHR Author InstructionsChanyanit CharoenpholNo ratings yet
- Problem 21-02 Wright Company Spreadsheet For The Statement of Cash Flows Dec. 31 Changes Dec. 31 2020 Debits Credits 2021 Balance SheetDocument17 pagesProblem 21-02 Wright Company Spreadsheet For The Statement of Cash Flows Dec. 31 Changes Dec. 31 2020 Debits Credits 2021 Balance SheetVishal P RaoNo ratings yet
- Batch Records HandoDocument39 pagesBatch Records HandoNiranjan SinghNo ratings yet
- Torts and Damages Lecture NotesDocument42 pagesTorts and Damages Lecture NotesMaeNo ratings yet
- Soiltac Safety Data Sheet: Section 1 - IdentificationDocument9 pagesSoiltac Safety Data Sheet: Section 1 - IdentificationSameh AhmedNo ratings yet
- Mineral Resources, Uses and Impact of MiningDocument4 pagesMineral Resources, Uses and Impact of MiningShakti PandaNo ratings yet
- Reading ComprehensionDocument9 pagesReading Comprehensionxifres i lletres xifres i lletres100% (1)