Professional Documents
Culture Documents
SWS 1 PDF
Uploaded by
dzhzrnOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SWS 1 PDF
Uploaded by
dzhzrnCopyright:
Available Formats
Review Article
Clinical Features of Sturge-Weber Syndrome
Francisco Xavier Palheta Neto*, Milton Alencar Vieira Junior**, Lorena Souza Ximenes**,
Celidia Cristina de Souza Jacob**, Adilson Góes Rodrigues Junior***,
Angélica Cristina Pezzin Palheta****.
* Master’s Degree in Otorhinolaryngology at the Federal University of Rio de Janeiro. In course for Doctor’s Degree in Neurosciences at the Federal University of Pará.
Assistant Professor of the Federal University of Pará and the University of the State of Pará.
** Student in the 3rd year of the Course of Medicine. University of the State of Pará.
** Student in the 2nd year of the Course of Medicine. Federal University of Pará.
**** Master’s Degree in Otorhinolaryngology at the Federal University of Rio de Janeiro. In course for Doctor’s Degree in Neurosciences at the Federal University of
Pará. Assistant Professor of the University of the State of Pará.
Institution: Centro de Otorrinolaringologia do Pará - COP.
Belém / PA - Brazil.
Mail address: Francisco Xavier Palheta Neto - Avenida Conselheiro Furtado, 2391, sala 1608 - Bairro: Cremação - Belém / PA - Brazil - Zip code:
66040-100 - Phone nos.: (+55 91) 3249-9977 or 3249-7161 and (91) 9116-0508 - E-mail: franciscopalheta@hotmail.com
Article received on June 12, 2008. Approved on November 23, 2008.
SUMMARY
Introduction: The Syndrome of Sturge-Weber is a rare condition of congenital development, and is characterized by a
neurocutaneous disorder with angiomas wrapping the leptomeninges and the face skin, mainly in the course
of ophthalmic (V1) and maxillary (V2) branches of the trigeminal nerve.
Objective: To review the literature about the Sturge-Weber Syndrome with emphasis on the current aspects.
Method: The following databases were searched: EMedicine, Encyclopedia of Medicine, FindArticles, LILACS, MEDLINE,
Merck Manuals On-Line Medical Library and Scielo, and the searches applied the terms: Sturge-Weber Syndrome,
neurocutaneous syndromes, encephalo-trigeminal angiomatosis, nevus flammeus, in articles published between
1991 and 2007.
Literature’s Review: The most characteristic clinical statement is the presence, since the birth, of nevus flammeus, that generally
reaches one half of the face and may stretch out up to the neck; in addition, other clinical manifestations may
be present, like the corticocerebral angiomatosis, cerebral calcifications, epilepsy, ocular and buccal affections
and mental retardation. The diagnosis is established by means of the inquiry of neurological and ophthalmic
alterations in patients with a characteristic nevus flammeus, allied to the clinical data of complementary exams
such as Computerized Tomography. The treatment consists basically of controlling the already confirmed clinical
manifestations and preventing from the appearing of other alterations, mainly buccal and ocular.
Conclusion: This syndrome is not much frequent, but it needs to be early diagnosed, since it brings a series of complications
to its carriers when not treated, specially because of reaching the Nervous Central System. The health professionals
have to be suitably able to recognize its characteristic signs and symptoms, and so improve the quality of life
of these patients.
Keywords: Sturge-Weber syndrome, congenital, angiomatosis, otorhinolaryngology.
Intl. Arch. Otorhinolaryngol., 565
São Paulo, v.12, n.4, p. 565-570, 2008.
Palheta Neto FX
INTRODUCTION LITERATURE REVIEW
The Sturge-Weber Syndrome (SWS) or Etiopathogenesis
encephalotrigeminal angiomatosis, or even craniofacial
angiomatosis, is specifically congenital, non-hereditary The Sturge-Weber Syndrome was initially
condition of rare development (1,2), although the described by SCHIRMER , in 1860, and was then specified
literature presents case reports inherited in an by STURGE (1878), who associated the dermatological and
autosomal recessive and dominant manner (3), namely ophthalmic changes to the disease’s neurological
of unknown etiology, marked by angiomas involving manifestations. In 1992, WEBER complemented it through
the leptomeninges and the facial skin, preferably in the documentation of these patients cerebral radiologic
the first and second trigeminal division course: the alterations (8).
ophthalmic and maxillary branches, respectively (4),
and therefore an association in which the cerebral, Although its etiology is unknown, we believe the
cutaneous and ocular hemangiomas prevail (3). SWS’s clinical manifestations derive from a common
embryologic base. Some authors say it’s from a congenital
In spite of being uncommon, this is the most malformation resulting from changes in the ectoderm,
frequent disease among the neurocutaneous mesoderm and neural crest derivates, in which we observe
syndromes - specially with vascular predominance -, the persistence of a vascular plexus around the cephalic
and its proportion is of 1/50.000 births (1,2). neural tube portion, that characterizes the leptomeninge
and face angiomatosis (9), between the fourth and the
Clinically, the most specific finding of the SWS eighth intra-uterine life (7,10).
is the presence, in the birth, of the nevus flameus, also
known as port wine stain (3); in addition to this, other We depart from the understanding that between
clinical manifestations may be present, mainly those the fifth and the eighth uterine life, the optic vesicle and
regarding changes to the central nervous system, such the occipital lobe visual cortex are anatomically close to
as convulsive crises and mental retardation, resulting each other, and allow the prevalence of the association of
from the leptomeningeal angioma (1). the nevus flameus, along the ophthalmic branch of pair V
of cranial nerves, with the choroid hemangioma and the
The diagnosis is frequently defined by the involvement of the occipital lobe, and a failure in the
syndrome characteristic nevus; however, we remark development of superficial cortical veins would support
besides such lesion is not an essential condition for the occurrence of the event and thus the venous superficial
the diagnosis, in spite the disease rarely occurs draining loss would deviate the blood to the meninges in
without the port wine stain (5), it’s also necessary to development, causing the formation of abnormal vascular
make differential diagnosis with other syndromes of channels and originating the leptomeningeal angiomatosis
similar affection, hence the importance of the (10).
complimentary exams performance, such as Magnetic
Resonance (MR) and Computerized Tomography Recent studies indicate the absence of normal
(CT) (6). cortical veins cause stasis and thrombosis of the angiomatous
bed with hypoxia and chronic ischemia of the cerebral
Due to the wide spectrum of its symptomatology, tissue, and a progressive deposition of calcium in the more
the SWS treatment primarily depends on its clinical external cortical layers and in the subintimal space of
features, but it’s basically related to the convulsive capillaries and small vessels of the second, third and fourth
crises control, and ranges from a possible medication cortical layers, so that the venous leptomeningeal angioma
therapy to a surgical intervention (7). on the cortical surface interferes with the normal supply of
oxygen to the subjacent cortex, which affects the intima-
Before these facts and the condition of being a pia. Therefore, the SWS anatomopathological lesion is
multifactor character syndrome, and of etiology still progressive and prevails in the parietal and parieto-occipital
strictly known and therefore of difficult prevention, it lobes. The ipsilateral brain hemisphere is thus atrophic in
presents the need to perform a literature review, a great part of the cases (11, 12).
aiming at clarifying its specific signs and symptoms in
order to alert the scientific community as for its Some authors also believe there may be a somatic
research and knowledge, both for its relevance and for mutation in the ectoderm, mesoderm and neural crest, that
the importance of its early diagnosis, by means of all is, a dominant autossomal hereditary disorder that may lead
its unique diagnosis. to the overproduction of angiogenic factors (5).
566 Intl. Arch. Otorhinolaryngol.,
São Paulo, v.12, n.4, p. 565-570, 2008.
Palheta Neto FX
Clinical Manifestations (14). Vascular malformation problems in conjunctive,
episcleral vein, choroid and retina, in addition to glaucoma
The SWS presents with neurological (brain anomaly), - present in about 30% to 70% of the ophthalmic affections
cutaneous, ocular and oral manifestations that may (or not) - represent the SWS syndrome ocular clinical manifestations
be associated with one another; however the most evident (7).
clinical manifestation is the presence of the nevus flameus
or port wine stain on the face, which normally follows the Such ocular manifestations result from the pressure
course of branches V1 and V2 of the trigeminal serve (11). increase, lead to glaucoma and buftalmia, and the latter is
more common than glaucoma, due to prenatal intraocular
Some authors classify the SWS in three types: Type hypertension. The homonymous hemianopia, another
I, relative to the appearing of cerebral, leptomeningeal neurological complication that affects the visual field,
angiomas and glaucoma, forming the disease’s classical occurs invariably when the occipital lobe is affected. Other
form; Type II, regarding the appearing of facial angioma congenital ocular anomalies are present, such as coloboma
and glaucoma, without evidence of intracranial disease; of the iris and deformities in the lens of the eye. Clinically
and Type III, relative to the presence of isolated we have retroorbitary pains and visual deterioration (5).
leptomeningeal angioma and absence of glaucoma,
considered to be a rare condition (13). It’s recommended that children with SWS are
reevaluated constantly, due to the strong relationship
Despite it’s not an essential condition of the between the upper eyelid and glaucoma, even in the
syndrome, the Port wine stain is the most frequent finding normal intraocular pressure measurements (6).
of the disease, generally present since the birth, and affects
half of the face, and may expand to the neck with a Oral manifestations are also present in approximately
characteristic to darken with age, ranging from reddish in 38% of the cases, and they may involve hemangiomatous
the beginning to purple in time. It’s worth remarking that lesion in the lip, oral mucosa, gum, tongue and palatine
only carriers of the nevus flameus, along the ophthalmic region (10).
branch, develop the syndrome in its classical form (7).
The oral manifestations are generally unilateral and
The ipsilateral leptomeninge angiomatosis also finish abruptly in the middle line. We observe ipsilateral
represents one of the main signs of the syndrome, may gingival hyperplasia, characterized by an increase in the
present with a progressive nature and commonly leads to vascular component and gingival hemorrhage at minimal
cerebral calcifications, epileptic convulsive crises, traumatisms. The accumulation of food and the presence
contralateral hypertrophy and hemiparesis and mental of bacterial plates may intensify inflammation and gingival
retardation (10). hyperplasia (15).
The epilepsy is the most common neurologic The macroglossia and the maxillary bone
manifestation that occurs as a result of the angiomatosis, hypertrophy found in some patients may cause a bad
and affects from 75% to 90% of the cases. In the patients occlusion and facial asymmetry. Other factors, such as
with unilateral involvement, the convulsive attacks dilantinic therapy, used by the patients in the treatment of
correspond to 72% of the neurological disorders, while in convulsive crises, may exacerbate the gingival increase
patients with bilateral neurologic affection, this number picture (16).
increases to 93%. The generalized tonicoclonic motor focal
convulsions occur more frequently in the initial phase of
live, in 45% of these patients; the crises begin before the Diagnosis and Complimentary Exams
first year of life, with a peak of incidence between 4 and
6 months of age; however, in older children and adults, we Although it’s not present in all cases and isn’t
may also observe a complex partial convulsion (13,14). pathognomonic in the syndrome, the diagnosis is based on
the presence of the nevus flameus in the face, and,
Hemiplegia and other neurological disorders affect according to some authors, the association between
the opposite side of the nevus flameus. Mental retardation convulsion and the nevus, irrespectively of the neurological
corresponds to 50% and hemiparesis to 30% of the loss, is sufficient for the syndrome’s clinical diagnosis (5),
neurologic disorders (6). although others defend the idea that, besides both these
findings, it’s also necessary one of the following
The ocular angioma, also present in the syndrome, manifestations to be present: Contralateral hemiparesis
appears in 30% of the cases, affects the choroids and the and hemiatrophy, mental retardation and glaucoma or
ocular sclerotic, and is ispilateral to the cutaneous angioma buftalmia findings. However, taking into account the other
Intl. Arch. Otorhinolaryngol., 567
São Paulo, v.12, n.4, p. 565-570, 2008.
Palheta Neto FX
existing systemic manifestations, there’s the need for the We still have the Rendu-Osler-Weber’s Syndrome
use of other diagnostic methods (1). or hereditary hemorrhage telangiectasis - an uncommon,
dominant autosomal condition - whose features are abnormal
As for the cerebral disturbances, for example, the vascular dilatation of the skin terminal vessels, mucosae
Computerized Tomography documents the intracranial and viscera. The disease involves the lips, buccal mucosa,
calcifications and unilateral cerebral atrophy; while the cere- pharynx, conjunctives and face, in addition to
bral vascular malformations are more easily viewed through neurofibromatosis, elliptocytosis and arteriovenous
Magnetic Resonance (1). A few cases of syndrome without aneurysm (6).
the nevus flameus were diagnosed by Magnetic Resonance,
Computerized Tomography and angiography (5). We also consider the Maffuci’s syndrome, which
presents with vascular malformations in the skin and
The MR exam is a better characterizer of the mucosae (lips and palate), dyschondroplasia, and may also
leptomeningeal angiomatosis, as well as the cerebral lead to long bones pathological deformities or fractures and
parenchyma and parenchimal venous abnormalities. While cause chondrosarcomas (6).
the CT technique represents the best diagnostic means
compared to the MR in the cortical calcifications detection Another situation is the occurrence of occipital
(17), since the studies demonstrate the cranial radiographies calcification in the absence of the nevus flameus; such fact
may reveal giriform calcifications in “rail line” in the requires the research of celiac disease associated with
affected side, and remark the location of the leptomeningeal epilepsy and brain calcifications to differ from SWS (17).
angiomas above the cerebral cortex ipsilateral to the nevus
flameus (7). However, it’s worth remarking that some The Beckwith-Wiedmann’s Syndrome requires
traces indicate such giriform calcifications are invisible to differential diagnosis, because such capillary malformation
the conventional radiographic exam, even after two years in the central region of the forehead or upper eyelids
of age (6). presents with a lesion similar to the Port wine stain,
associated with macroglossia and some risk associated to
The ophthalmologic changes may be observed visceral neoplasms due to the visceral overgrowth (18).
through the retinal examination (14) and also ocular
ultrasonography, which showed to be an important method
for diagnostic complementation, and contributed for valuable Treatment
data concerning the diagnosis and the location of the
choroid hemangiomas (16). The treatment of the Surge-Weber’s Syndrome is
variable, and depends on the nature or intensity of its
Important findings were also described of the possible clinical features.
ultrasonic biomicroscopy (UBM) in patients with the Sturge-
Weber Syndrome associated or not with glaucoma. Such Usually, the Port wine nevus in the face may be
study comments the UBM not only as a diagnostic method, improved by the use of new techniques of laser therapy or
but also as a promissory method in the study of the through the use of cosmetics (7,18).
syndrome ocular lesions (2).
However, we remark the first direction for treatment
The oral manifestations are observed in radiographies must focus the control of the convulsive crises, with
through the identification of horizontal and vertical bone administration of suitable medication. In case the convulsive
re-absorptions with loss of the hard lamina, which commit crises become uncontrollable, several neurosurgical
the teeth of the side involved by the lesion and obviously procedures have been used - for instance lobectomy or
by the clinical observation of other changes, such as hemispherectomy - aiming at diminishing such crises and
gingival hyperplasia (5). make the patients more sensitive to the medication
treatment. Nevertheless, the great limitation to the surgical
intervention is its high morbimortality (7).
Differential Diagnosis
In addition, physiotherapies to mitigate the motor
The Sturge-Weber Syndrome differential diagnosis difficulties resulting from hemiparesis and reeducation to
includes the angio-osseous-hypertrophic Syndrome, also increase the intellectual level are also recommended (7, 18).
known as Klippel-Trénaunay-Weber’s syndrome that
presents with Port wine stains in the face ends, soft and The annual monitoring as for glaucoma is
osseous tissues hypertrophy, in addition to other features recommended for all patients, specially children and, if
of the SWS (10). applicable, it deserves an aggressive treatment (19).
568 Intl. Arch. Otorhinolaryngol.,
São Paulo, v.12, n.4, p. 565-570, 2008.
Palheta Neto FX
The patients with oral changes must be submitted Weber syndrome without facial nervus. Pediatr. Nerol. 2000,
to oral cavity exams periodically and perform a detailed 22:400-402.
control of the bacterial plate, since it may aggravate the
vascular picture and extreme cares are also crucial with 6. Marinho AS, Cherubini K. Síndrome de Sturge-Weber.
surgical procedures in the oral cavity, due to its trend to Revista de Odontologia da Universidade Cidade de São
flow with intense hemorrhage (1). Paulo. 2006, 18:167-173. Disponível em: http://
www.ciadadesp.edu.br/old/arquivos/publicacoes/
revsita_odontologia/maio_agoso/9_sindrome_sturge.pdf.
FINAL COMMENTS
7. Neville et al. Patologia Oral e Maxilofacial. Rio de Janeiro:
The large spectrum of clinical manifestations of the Guanabara Koogan, 1998, 87-89.
Sturge-Weber Syndrome shows its multifactor nature and
therefore its difficult early diagnosis. Even the classical 8. Freitas TMC, Amorim RFB, Galvão HC, Freitas RA.
manifestations, such as facial nevus flameus, convulsive Síndrome de Sturge-Weber: Relato de caso com
crises, glaucoma and gingival changes, contribute for the manifestações orais. Revista do Conselho Regional de
late diagnosis before their differential diagnoses, which also Odontologia de Pernambuco. 2004, 3:143-146. Disponível
form uncommon and not much known syndromes (1). em: http://bases.bireme.br/cgibin/wxislind.exe/iah/online/
?IsisScript=iah/iah.xis&base=LILACS&lang=
As the SWS’s etiopathogenesis is not strictly known, p&nextAction=lnk&exprSearch=sturge%20and%20
its prevention is then hardened and its early diagnosis is weber&label=sturge%20and%20weber.
critical, since it allows the control of future complications,
mainly those relating to the Central Nervous System, 9. Castroviejo IP, Gonzales CD, Garciamalian RM, Gonzalez-
considering the inexistence of specific treatments for such Casado I, Muñozhiraldo E. Sturge-Weber syndrome: Study of
pathology (18). 40 pacients. Journal of Pediatric Neurology. 1993, 9:283-287.
The Sturge’s disease requires major cares in the 10. Fontenelle LMC, Silva ES, Kreimer VS. Síndrome de
performance of invasive procedures, which improves the Sturge-Weber: Relato de um caso com hemangioma de retina
surgical planning and the therapeutic proposal to be e outras alterações incomuns. Rev Bras de Neurologia. 1991,
instituted, and prevents the significant intercurrences arising 27:161-163.
out of hemorrhages that elevate so much this disease’s
morbimortality (20). 11. Yacubin EMT. Síndromes Epilépticas Hemisféricas.
Sociedade Portuguesa de Neurologia. 2002, 2:10-16.
Disponível em: http://www.cefaleiasspc.com/sinapse/
BIBLIOGRAPHICAL REFERENCES Sinapse_Vol2_N1_Maio02.pdf.
1. Gomes ACA, Silva EDO, Albert DGM. Síndrome de Sturge- 12. Sem Y et al. Sturge-Weber syndrome in a 14-year-old
Weber: Relato de caso clínico. Revista de Cirurgia e girl without facial naevus. European Journal Pediatric. 2002,
Traumatologia Buco-Maxilo-Facial. 2004 4: 01-71. Disponível 161:505-507. Disponível em: http://
em: http://www.revistacirurgiabmf.com/2004/v4n1/pdf/ www.springerlink.com/content/wc3ua06q2rwq/
v4n1.6.pdf. ?p=db61e0b742f240298bd3a42c48890557&pi=69.
2. Cronemberger S, Calixto N, Assunção DAM, Milhomens 13. Roach ES. Neurocutaneous syndromes. Pediatric clinical
EG. Síndrome de Sturge-Weber: estudo ultrabiomicros- north am. 1992, 39:591-620.
cópico. Arquivo Brasileiro de Oftalmologia. 2004, 67:211-
217. 14. Raquel IH. Avaliação psico-educacional de uma
adolescente portadora de Síndrome de Sturge-Weber. São
3. Concepción OF, García AG, Sardiñaz NH. Síndrome de Paulo, 2007, p. 20-23, (Tese de Mestrado - Universidade
Sturge-Weber, revisión. Revista Cubana de Pediatria. 1999, Estadual Paulista, campus de Bauru).
71:153-159.
15. Santos MCM, Alleman N, Cha SB, Erwenue CM. Ultra-
4. Takeoka M. Sturge-Weber Syndrom. The Mediscape som ocular na síndrome de Sturge-Weber. Arquivo Brasileiro
Journal. 2006. Disponível em: http://www.emedicine.com/ de Oftalmologia. 1998, 61:271-275. Disponível em:http:/
neuro/topic356.htm. /www.abonet.com.br/abo/abo613.htm#Ultra-som.
5. Aydin A, Cakmakçi H, Kovanlikaya A, Dirik E. Sturge- 16. Huang JS, Chen CC, Wu YM. Periodontal Manifestations
Intl. Arch. Otorhinolaryngol., 569
São Paulo, v.12, n.4, p. 565-570, 2008.
Palheta Neto FX
and Treatment of Sturge-Weber Syndrome- report of two 19. Pereira CM, Vedrano APG, Naclério-Homem MG.
cases. Kao J Med Sci. 1997, 3:127-135. Síndrome de Sturge-Weber: Revisão de Literatura e Relato
de Dois Casos Clínicos. Revista Brasileira de Patologiageral.
17. Dilber C et al. Sturge-Weber syndrome involved 2003: 2:1. Disponível em: http://www.patologiaoral.com.br/
frontoparietal region without facial nervus. Pediatr Neurol. texto18.asp.
2002, 26:387-390.
20. Gontijo B, Pereira LB, Silva CMR. Malformações
18. Caizzo A. The use of preoperative percuraneous Vasculares. An. Bras. Dermatol., Rio de Janeiro. 2004, 79:7-
transcatherer vascular occlusive therapy in the managemenr 25. Disponível em: http://www.scielo.br/pdf/abd/v79n1/
of Srurge- Weber syndrome; report of a case. Oral Maxillofac. en_19990.pdf.
Sarg. 1998, 56:775-778.
570 Intl. Arch. Otorhinolaryngol.,
São Paulo, v.12, n.4, p. 565-570, 2008.
You might also like
- Aspectos Clinicos NmoDocument11 pagesAspectos Clinicos NmoOlga Manco GuzmánNo ratings yet
- 1 s2.0 S152550500500185X MainDocument10 pages1 s2.0 S152550500500185X MainmarleneNo ratings yet
- The Clinical Syndrome Cerebral MalariaDocument14 pagesThe Clinical Syndrome Cerebral Malaria1130120017 ALI ANTONO TANNo ratings yet
- Camargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Document6 pagesCamargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Rizki Muhammad RanandaNo ratings yet
- Neuropathology Autopsy Practice Post Mortem Examination in Cerebrovascular Disease StrokeDocument15 pagesNeuropathology Autopsy Practice Post Mortem Examination in Cerebrovascular Disease Strokelisboa_rodriNo ratings yet
- Posterior Circulation Stroke: Advances in Understanding and ManagementFrom EverandPosterior Circulation Stroke: Advances in Understanding and ManagementJong S. KimNo ratings yet
- Cerebellar MutismDocument4 pagesCerebellar MutismDwi Puja SetiawanNo ratings yet
- Status Epilepticus in Critically Ill PatientsDocument11 pagesStatus Epilepticus in Critically Ill PatientsAkbal Nur KarimNo ratings yet
- Handbook of Medical Neuropsychology: Applications of Cognitive NeuroscienceFrom EverandHandbook of Medical Neuropsychology: Applications of Cognitive NeuroscienceNo ratings yet
- An Algorithm For The Evaluation of Peripheral Neuropathy - American Family PhysicianDocument9 pagesAn Algorithm For The Evaluation of Peripheral Neuropathy - American Family PhysicianAnonymous vnv6QFNo ratings yet
- Sturge Weber SyndromeDocument14 pagesSturge Weber SyndromeAnumeha JindalNo ratings yet
- Empty Sella Syndrome: Continuing Education ActivityDocument8 pagesEmpty Sella Syndrome: Continuing Education Activityn2763288No ratings yet
- Malaria and StrokeDocument3 pagesMalaria and StrokeRia Septi HarmiaNo ratings yet
- Neuromyelitis Optica: Mark J. Morrow, MD, Dean Wingerchuk, MD, MSC, FRCP (C)Document13 pagesNeuromyelitis Optica: Mark J. Morrow, MD, Dean Wingerchuk, MD, MSC, FRCP (C)sidogra100% (1)
- Heart Valve Disease: State of the ArtFrom EverandHeart Valve Disease: State of the ArtJose ZamoranoNo ratings yet
- Aicardi Goutieres SyndromeDocument7 pagesAicardi Goutieres Syndromezloncar3No ratings yet
- 2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryDocument20 pages2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryLéo VidoniNo ratings yet
- Clinical and Genetic Basis of Familial Amyotrophic Lateral Sclerosis (Revisión)Document12 pagesClinical and Genetic Basis of Familial Amyotrophic Lateral Sclerosis (Revisión)Francisco Ahumada MéndezNo ratings yet
- Highlights in Neuro OphthalmologyDocument2 pagesHighlights in Neuro OphthalmologyShruthi VMNo ratings yet
- Semiology of Insular Lobe Seizures: SciencedirectDocument6 pagesSemiology of Insular Lobe Seizures: SciencedirectViviana Torres BallesterosNo ratings yet
- Semiology of Insular Lobe Seizures: SciencedirectDocument6 pagesSemiology of Insular Lobe Seizures: SciencedirectViviana Torres BallesterosNo ratings yet
- CNS Diseases and UveitisDocument25 pagesCNS Diseases and UveitisHabib G. Moutran BarrosoNo ratings yet
- E RefdDocument13 pagesE RefdGabriella TjondroNo ratings yet
- Pseudo 1Document20 pagesPseudo 1giant nitaNo ratings yet
- Investigatory Project inDocument31 pagesInvestigatory Project inrchandralega2205100% (1)
- Wernicke Korsakoff SyndromeDocument19 pagesWernicke Korsakoff Syndrometerry2wa100% (4)
- Motor Neuron DiseaseDocument7 pagesMotor Neuron DiseasegeraldineongNo ratings yet
- What Can Mimic Multiple Sclerosis?Document29 pagesWhat Can Mimic Multiple Sclerosis?Ankita ShahNo ratings yet
- The Expanded Spectrum of Neuromyelitis oDocument7 pagesThe Expanded Spectrum of Neuromyelitis oFlavia ChNo ratings yet
- Tolosa HuntDocument10 pagesTolosa HuntRoxana StanciuNo ratings yet
- Facomatosis Pubmed PDFDocument8 pagesFacomatosis Pubmed PDFKevin ChaucaNo ratings yet
- Neurological Assessment of ComaDocument5 pagesNeurological Assessment of Comapanda7100No ratings yet
- Central Ocular Motor Disorders, Including Gaze Palsy and NystagmusDocument17 pagesCentral Ocular Motor Disorders, Including Gaze Palsy and NystagmusAnonymous vnv6QFNo ratings yet
- Orofacial Reflex Myocloni. Definition, Relation To Epilepsy Syndromes, Nosological and Prognosis Significance. A Focused ReviewDocument5 pagesOrofacial Reflex Myocloni. Definition, Relation To Epilepsy Syndromes, Nosological and Prognosis Significance. A Focused ReviewJuliana AparcanaNo ratings yet
- JURNALDocument10 pagesJURNALLuses Shantia HaryantoNo ratings yet
- Multiple Sclerosis - The Disease and Its ManifestationsDocument8 pagesMultiple Sclerosis - The Disease and Its ManifestationsCecilia FRNo ratings yet
- Infantile Spasms: Review of The Literature and Personal ExperienceDocument10 pagesInfantile Spasms: Review of The Literature and Personal ExperienceDianMuliasariNo ratings yet
- 3rd Taccone MSDocument18 pages3rd Taccone MSDouglasNo ratings yet
- Focal Epilepsy Causes and Clinical Features - UpToDateDocument44 pagesFocal Epilepsy Causes and Clinical Features - UpToDateBenjamínGalvanNo ratings yet
- Espectro Neuromielitis Óptica 2022 NejmDocument9 pagesEspectro Neuromielitis Óptica 2022 NejmOscar BushNo ratings yet
- FS007v1 RasmussensDocument4 pagesFS007v1 Rasmussensbilly2107No ratings yet
- Finding (Neurology)Document12 pagesFinding (Neurology)Ayu NoviantiNo ratings yet
- Encefalite Herpética 4 Casos Rev Neurol 2002Document6 pagesEncefalite Herpética 4 Casos Rev Neurol 2002Ana SopaNo ratings yet
- 10.1007@s00381 020 04746 9Document12 pages10.1007@s00381 020 04746 9Alvaro Perez HenriquezNo ratings yet
- Status Epilepticus in ChildrenDocument73 pagesStatus Epilepticus in ChildrenvelasquezcamposmaximoNo ratings yet
- Seizure and EpilepsyDocument9 pagesSeizure and EpilepsyAien LeeNo ratings yet
- Pathogenesis of Opsoclonus MyoclonusDocument2 pagesPathogenesis of Opsoclonus MyoclonusIRENA GENINo ratings yet
- Facial Nerve Palsy: Dr. Saud AlromaihDocument74 pagesFacial Nerve Palsy: Dr. Saud AlromaihChandra ManapaNo ratings yet
- Nejmra 1904655Document9 pagesNejmra 1904655silviaNo ratings yet
- Acute Dizziness, Vertigo, and Unsteadiness 2021 NCDocument17 pagesAcute Dizziness, Vertigo, and Unsteadiness 2021 NCLaura A M MNo ratings yet
- Differential Diagnosis of Cardiogenic Syncope and Seizure DisordersDocument6 pagesDifferential Diagnosis of Cardiogenic Syncope and Seizure DisordersganangahimsaNo ratings yet
- Si Gede Teguh Surya Negara 011.06.0043: 28/08/2017 1 FK Unizar Mataram 2017Document50 pagesSi Gede Teguh Surya Negara 011.06.0043: 28/08/2017 1 FK Unizar Mataram 2017'aac' JujuuNo ratings yet
- Central Vertigo PDFDocument6 pagesCentral Vertigo PDFarlinieNo ratings yet
- Multiple SclerosisDocument4 pagesMultiple SclerosisMarwan M.No ratings yet
- Current Concept of Neuromyelitis Optica (NMO) and NMO Spectrum DisordersDocument10 pagesCurrent Concept of Neuromyelitis Optica (NMO) and NMO Spectrum DisordersGabriella TjondroNo ratings yet
- C R C S: Urrent Eview in Linical CienceDocument7 pagesC R C S: Urrent Eview in Linical CienceAdriel Chandra AngNo ratings yet
- Central Pontine Myelinolysis and The Osmotic Demyelination 2021Document10 pagesCentral Pontine Myelinolysis and The Osmotic Demyelination 2021Nicolas RodriguezNo ratings yet
- Non Breathing Related Sleep Disorders Following StrokeDocument6 pagesNon Breathing Related Sleep Disorders Following StrokeRizqan Fahlevvi AkbarNo ratings yet
- Posterior Reversible Encephalopathy SyndDocument7 pagesPosterior Reversible Encephalopathy SyndasasakopNo ratings yet
- Brachii - Google SearchDocument1 pageBrachii - Google SearchdzhzrnNo ratings yet
- Disc & Motivators Report For: Diaz SetiadiDocument14 pagesDisc & Motivators Report For: Diaz SetiadidzhzrnNo ratings yet
- Spotify Top Track Generator: Last 6 MonthsDocument1 pageSpotify Top Track Generator: Last 6 MonthsdzhzrnNo ratings yet
- Significantly Increased Risk of All-Cause Mortality Among Cardiac Patients Feeling LonelyDocument7 pagesSignificantly Increased Risk of All-Cause Mortality Among Cardiac Patients Feeling LonelydzhzrnNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Sturge-Weber Syndrome. Study of 55 PatientsDocument7 pagesSturge-Weber Syndrome. Study of 55 PatientsdzhzrnNo ratings yet
- The Pathogenesis of Port Wine Stain and Sturge Weber Syndrome: Complex Interactions Between Genetic Alterations and Aberrant MAPK and PI3K ActivationDocument17 pagesThe Pathogenesis of Port Wine Stain and Sturge Weber Syndrome: Complex Interactions Between Genetic Alterations and Aberrant MAPK and PI3K ActivationdzhzrnNo ratings yet
- Sturge Weber SyndromeDocument6 pagesSturge Weber SyndromedzhzrnNo ratings yet
- The "Reptilian" - Triune Brain - The Origins of A Misguided Idea - Emotion & Cognition and The Brain, by Luiz PessoaDocument6 pagesThe "Reptilian" - Triune Brain - The Origins of A Misguided Idea - Emotion & Cognition and The Brain, by Luiz PessoaJ. Félix Angulo RascoNo ratings yet
- Migraine Aura - Pathophysiology, Mimics, and TratamentDocument10 pagesMigraine Aura - Pathophysiology, Mimics, and Tratamentrafael rocha novaes100% (1)
- Psy 03 Biopsychology-Ch. 8 Sensorimotor SystemDocument1 pagePsy 03 Biopsychology-Ch. 8 Sensorimotor SystemMitch Shyrelle BaclaoNo ratings yet
- Music and Brain Circuitry Strategies For StrengtheningDocument10 pagesMusic and Brain Circuitry Strategies For Strengtheningbiahonda15No ratings yet
- K8a Anatomi Sistem Saraf PusatDocument87 pagesK8a Anatomi Sistem Saraf Pusathartinissa vaniaNo ratings yet
- Human Physiology From Cells To Systems 9th Edition Sherwood Solutions ManualDocument12 pagesHuman Physiology From Cells To Systems 9th Edition Sherwood Solutions ManualSamanthaStuartijgt100% (40)
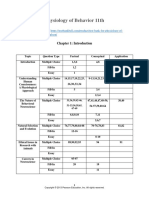
- Test Bank For Physiology of Behavior 11th Edition by CarlsonDocument45 pagesTest Bank For Physiology of Behavior 11th Edition by CarlsonThomas White100% (26)
- Fuster 2001Document15 pagesFuster 2001Jane SmithNo ratings yet
- 5 - The Visual System and Mechanisms of PerceptionDocument13 pages5 - The Visual System and Mechanisms of PerceptionElmer SalazarNo ratings yet
- Emotion, Memory and The BrainDocument9 pagesEmotion, Memory and The Brainbarrylyndon1967No ratings yet
- Biological Basis of BehaviorDocument6 pagesBiological Basis of BehaviorLyanna MormontNo ratings yet
- General NosologyDocument13 pagesGeneral Nosologyyasingada100% (1)
- Brain StudyDocument57 pagesBrain StudyJoeNo ratings yet
- Beta-Oscillations Reflect Recovery in Subacute Stroke NNR 20200511Document13 pagesBeta-Oscillations Reflect Recovery in Subacute Stroke NNR 20200511yafangNo ratings yet
- Brainsci 09 00068 v2Document20 pagesBrainsci 09 00068 v2RobertoVargasPérezNo ratings yet
- Nano BotsDocument31 pagesNano Botspradeepagarwal62No ratings yet
- Functional Areas of Cerebral CortexDocument3 pagesFunctional Areas of Cerebral CortexMatet MonjeNo ratings yet
- Adonis Quintero Linguistic DictionaryDocument20 pagesAdonis Quintero Linguistic DictionaryMax No MeloNo ratings yet
- Brain AnatomyDocument2 pagesBrain AnatomyÖzge ŞenNo ratings yet
- Need Motivates The Behaviour of A Person.: Human Needs TheoryDocument8 pagesNeed Motivates The Behaviour of A Person.: Human Needs TheoryDan Ataniel EnsaladaNo ratings yet
- Visual PathwayDocument24 pagesVisual PathwayAkshara Eye FoundationNo ratings yet
- 100 Days of Sunlight by Abbie EmmonsDocument315 pages100 Days of Sunlight by Abbie EmmonsJessie Ann Aquino100% (11)
- Motor PlanningDocument30 pagesMotor PlanningkalbaliNo ratings yet
- Identify The Part of The BrainDocument2 pagesIdentify The Part of The BrainClement Mar ClimacoNo ratings yet
- EEG-Based Emotion RecognitionDocument17 pagesEEG-Based Emotion RecognitionbmakworoNo ratings yet
- Neurological Considerations 1966 PDFDocument1 pageNeurological Considerations 1966 PDFWahyuni SusantiNo ratings yet
- Solutions Manual Ch. 11 and 12 - Test BankDocument9 pagesSolutions Manual Ch. 11 and 12 - Test BankSally RiverNo ratings yet
- N - I. A - P: Eurotransmisores DEL Sistema Límbico Mígdala Rimera ParteDocument6 pagesN - I. A - P: Eurotransmisores DEL Sistema Límbico Mígdala Rimera ParteghgfchmNo ratings yet
- Neuromodulation by Means of Electrical Brain Stimulation: AbstractsDocument5 pagesNeuromodulation by Means of Electrical Brain Stimulation: AbstractsmoiNo ratings yet
- Central Vestibular PathwayDocument22 pagesCentral Vestibular PathwayPutri Noursyarief Maharanny NasutionNo ratings yet