Professional Documents
Culture Documents
Review Anti Core VHB
Uploaded by
Alejandro de la RosaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Review Anti Core VHB
Uploaded by
Alejandro de la RosaCopyright:
Available Formats
1780 CLINICAL AND SYSTEMATIC REVIEWS
CME
Isolated anti-HBc: The Relevance of Hepatitis B Core
REVIEW
Antibody—A Review of New Issues
Tiffany Wu, MD1, Ryan M. Kwok, MD2 and Tram T. Tran, MD3
Hepatitis B core antibody (anti-HBc) is considered the most sensitive serological marker for history of hepatitis B virus
(HBV) infection. In a subset of anti-HBc carriers, anti-HBc is present in the absence of hepatitis B surface antigen
and hepatitis B surface antibody—a serological pattern known as “isolated anti-HBc” (IAHBc). IAHBc has been of
clinical interest over the past several years, with growing data to suggest its role as a serological marker for occult HBV
infection (OBI). This article reviews the clinical significance and association of IAHBc with hepatitis C virus (HCV)
co-infection, risk of HBV reactivation during direct-acting antiviral therapy for HCV as well as immune suppression,
and development of hepatocellular carcinoma (HCC). Hepatitis B core-related antigen is also highlighted as an
emerging laboratory assay that may identify OBI and predict HCC development in non-cirrhotic patients receiving
nucleoside/nucleotide analog therapy.
Am J Gastroenterol 2017; 112:1780–1788; doi:10.1038/ajg.2017.397; published online 31 October 2017
INTRODUCTION Occult HBV infection
Hepatitis B core antibody (anti-HBc) is recognized as an The persistence and detection of serum or liver HBV DNA in
important serological marker in identifying patients infected the absence of serum HBsAg is defined as occult HBV infec-
or exposed to hepatitis B virus (HBV). Increasing interest has tion (OBI) (2). Most studies identifying OBI among cohorts of
focused on patients positive for anti-HBc and negative for both chronically infected HBV patients have been positive for anti-
hepatitis B surface antigen (HBsAg) and antibody (anti-HBs)— HBc with or without concomitant anti-HBs positivity. Status
a serological pattern called “isolated anti-HBc” (IAHBc) (1). of occult infection has primarily been associated with the sup-
Traditionally, this pattern is considered to be evidence of prior pression of viral replication and gene expression; however, it
infection; however, recent findings suggest a greater clinical sig- has also been seen in patients with mutant forms of HBV with
nificance. Herein, we elaborate on several clinical implications of undetectable HBsAg. OBI is recognized among patients with
potential future tests and strategies for management of patients prior HBV exposure and is significant in various clinical con-
with IAHBc. texts including viral transmission, reactivation, and progression
of liver disease (3).
DEFINITIONS/TERMS
Isolated anti-HBc HEPATITIS B CORE ANTIGEN AND ANTIBODY:
The presence of anti-HBc in the absence of HBsAg and anti-HBs CLINICAL IMPLICATIONS
is known as IAHBc, also defined in some studies as “anti-HBc Hepatitis B core antigen (HBcAg), a viral nucleocapsid protein, is
alone.” Current literature has used the “isolated anti-HBc” nomen- the most immunogenic component of HBV. Typically contained
clature to refer specifically to HBsAg-negative, anti-HBc-positive within the viral envelope, HBcAg in liver tissue is poorly acces-
patients, often stratifying this population into anti-HBs-positive sible to host B cells until infected hepatocytes are damaged and
and -negative subgroups. In this review, we report only findings lyse, stimulating B-cell antibody production (4). High T-cell
relevant to the IAHBc serological profile as defined by absence of immunogenicity of HBcAg also enhances humoral response
both HBsAg and anti-HBs. (1). During acute infection, IgM class antibodies to HBcAg pre-
1
Department of Medicine, Cedars-Sinai Medical Center, Los Angeles, California, USA; 2Division of Gastroenterology and Hepatology, Walter Reed National Military
Medical Center, Bethesda, Maryland, USA; 3Comprehensive Transplant Center, Cedars-Sinai Medical Center, Los Angeles, California, USA. Correspondence:
Tram T. Tran, MD, Cedars-Sinai Medical Center, 8900 Beverly Boulevard, Los Angeles, California 90048, USA. E-mail: Tram.Tran@cshs.org
Received 25 May 2017; accepted 19 September 2017
The American Journal of GASTROENTEROLOGY VOLUME 112 | DECEMBER 2017 www.nature.com/ajg
The Relevance of Hepatitis B Core Antibody 1781
dominate. Over time, IgM levels decline although total IgG levels of normal, factors other than anti-HBV T-cell response may
persist with slowly decreasing titers for 10–20 years or more (4). contribute to elevations in ALT (4).
If reactivated, IgM re-emerges confirming a chronic hepatitis B
REVIEW
(CHB) exacerbation (5). Antibody to HBcAg is only produced in
the presence of viral infection and is not a serological response to ISOLATED ANTI-HBC
HBV vaccination. As such, anti-HBc is considered the most sensi- IAHBc may represent several clinical entities including a false
tive marker for a history of HBV infection, given its persistence positive test result, the window phase of acute HBV when anti-
even after viral clearance (4). Assays for serum levels of HBcAg HBs is not yet detected, the late stage of prior infection after anti-
are not currently available in the United States and circulating HBs has fallen to undetectable levels, or OBI (1,2).
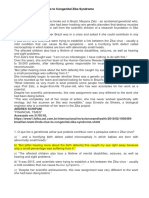
HBcAg is not routinely detected in any phase of HBV infection. See Figure 1 for a proposed algorithm to evaluate a patient with
In contrast, anti-HBc is readily obtainable and may be quanti- IAHBc.
fied through various types of immunoassays. Currently available Depending on the type of assay used as well as the prevalence
assays use human or mouse-monoclonal core antibodies, detec- of infection, false positives may occur in patients with a finding
tion systems involving enzymes, fluorescence, or chemilumines- of IAHBc. Although modifications have been made to improve
cence, as well as variable reaction kinetics differing in incubation test specificity, confirming anti-HBc status may be appropriate in
steps, temperature, and time (1). certain clinical scenarios (1). Alternatively, it is important to con-
Hepatitis B envelope antigen (HBeAg) and hepatitis B envelope sider the window phase of acute infection as anti-HBs and hepa-
antibody, HBV DNA, and serum alanine aminotransferase (ALT) titis B envelope antibody immune complexes and their antigen
help to classify patients into phases correlating with the natural counterparts may not be detectable by conventional assays. Repeat
history of CHB and associated changes on liver histology (5,6). anti-HBc testing several months later may be indicated wherein
Previous studies have quantified the values of anti-HBc among HBsAg, anti-HBs, HBeAg, and hepatitis B envelope antibody
the four phases of CHB infection. Anti-HBc levels are highest in would be detectable. Patients who have undergone viral clearance
the immune active and immune reactivation phases and lowest may also lose the ability to produce anti-HBs after long periods
in immune tolerant and inactive phases. Elevation of anti-HBc of time. Reasons for this chronic decline are unclear, although it
during immune active and reactive phases suggests a role for this has been previously hypothesized to result from a waning T-cell
antibody in the immune response to chronic HBV infection (5). response (1).
In addition, anti-HBc levels correlate with serum ALT levels and If IAHBc is confirmed, consideration of subsequent testing
individuals with higher ALT tend to have higher anti-HBc levels. should be pursued to evaluate for OBI. Kang et al, described rates
However, this correlation only applies to values of ALT less than of occult infection ranging from 0% to 22.5% though source of
five times the upper limit of normal. In ALT >5 times upper limit HBV DNA sampling may contribute to differences among studies
Isolated anti-HBc
Repeat with different immunoassay
for confirmatory testing
Negative
Positive
Likely false
positive result
Check anti-HBs in 1–3 months
Anti-HBs positive Anti-HBs negative
Likely window phase of Evaluate for occult HBV
acute HBV infection infection with assay for
HBV DNA PCR
Figure 1. Methodology to evaluate a patient initially found with isolated hepatitis B core antibody (anti-HBc). Adapted from “The underlying mechanisms
for the ‘anti-HBc alone’ serological profile,” by RA Ponde, DD Cardoso, and MO Ferro, 2010, Archives of Virology, 155, p. 154.
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
1782 Wu et al.
(2). Table 1 provides an updated range of 1.7% to 41%, report- phase and 11 patients were found to be false positive. Of the 351
ing on subjects who are HBsAg negative, anti-HBc positive, and IAHBc patients, 10 were positive for HBV DNA, whereas the other
HBV DNA positive among a sample of studies from 2001 to 2015. 341 did not have detectable HBV DNA in serum. Of these 10 HBV
REVIEW
Methods of HBV DNA quantification may vary given differences DNA-positive subjects, 6 had high levels of viremia. This particular
in measurement of DNA in serum vs. liver tissue. Variation may study cited a prevalence of 2.8% of occult HBV among patients
also result from differences in sample size or virological features of with IAHBc. The authors hypothesized this may have been an
studied patient populations including co-morbidities, prevalence underestimate since only one data point was gathered, potentially
or endemicity of populations, and assay sensitivity (7). excluding patients with intermittent viremia. In addition, screen-
A study by Launay et al. (8) retrospectively categorized 362 ing assays may not have been sensitive enough to detect very
patients with IAHBc sera into the clinical entities described in the low levels of viremia. Notably, HBsAg was detected in two of
algorithm. Only one patient was found to be within the window these patients when retested using a different, multivalent assay.
Table 1. Summary of studies of IAHBc (HBsAg negative and anti-HBc positive) HBV DNA-positive patients (2,47–61)
Study (year of publication) HBV DNA positive (%) HBV DNA detection ALT, if available High-risk Clinically relevant
(serum or liver) limit (copies per ml) comorbidities outcomes
Jilg et al. (47) Germany 5/65 (7.7) Serum 100 to 10,000 Nested Not reported Yes (HCV)
PCR
Kleinman et al. (48) USA 4/107 (3.7) Serum 10–100 Enzymatic Not reported NA
detection of amplified
DNA
Alhababi et al. (49) UK 6/151 (4) Serum 100–400 Nested PCR Not reported No HBV DNA+ pts were not
identified among co-infected
HIV+ or HCV+ patients within
the study population
García-Montalvo et al. (50) 13/158 (8.2) Serum 30–300 Nested PCR Not reported NA
Mexico
Knoll et al. (51) Germany 16/39 (41) Liver 50–100 Quantitative Normal to 2× ULN Yes (HCV) HBV DNA+ less often
PCR by Taqman detected in IAHBc patients
with cirrhosis or HCC
Banerjee et al. (52) India 39/171 (22.8) Serum 100–1000 Quantitative Not reported NA
PCR by Taqman
El-Zaatari et al. (53) Lebanon 11/203 (5.4) Serum <400 Nested PCR Not reported No
Vitale et al. (54) Italy 5/119 (4.2) Serum 100 Nested PCR Not reported No
Gibney et al. (55) Australia 1/35 (3) Serum 100 Nested PCR Not reported No Lower rate than expected of
HBV DNA positivity among a
highly endemic population
Kang et al. (2) Korea 4/230 (1.7) Serum <60 to 110 Quantitative 18–33 No
PCR by Taqman
Ramezani et al. (7,56) Iran 12/40 (30) Serum Not reported Not reported Yes (HD, HIV+) HBV DNA+ more prevalent in
high-risk patients (HIV+ and
hemodialysis)
Tramuto et al. (57) Italy 3/58 (5.2) Serum Not reported 22 Yes (HIV) HIV+identified as a risk factor
for HBV DNA+
Rios-Ocampo et al. (58) 6/302 (1.9) Serum 18–224 IU ml−1 Nested Not reported No
Columbia PCR
Jutavijittum et al. (59) Laos 12/75 (16) Serum 1110 Quantitative PCR Not reported No
by Taqman
Antar, et al. (60) Egypt 5/80 (6.2) Serum 3–11481 IU ml−1 Not reported No
Enzymatic detection of
amplified DNA
Kishk et al. (61) Egypt 5/27 (18.5) Serum <2.0–4.5 log Enzymatic 9–22 No
detection of amplified
DNA
ALT, alanine aminotransferase; Anti-HBc, hepatitis B core antibody; HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus; HCV, hepatitis C virus; HCC, hepato-
cellular carcinoma; HIV, human immunodeficiency virus; IAHBc, isolated hepatitis B core antibody; NA, not available; ULN, upper limit of normal.
The American Journal of GASTROENTEROLOGY VOLUME 112 | DECEMBER 2017 www.nature.com/ajg
The Relevance of Hepatitis B Core Antibody 1783
This suggests a mutant form of HBsAg initially undetected on chronic HCV had detectable HBV DNA in serum (14). It is pro-
conventional screening. This may represent “false occult HBV,” for posed that simultaneous HCV infection downregulates synthesis
which IAHBc may be a significant risk factor (8). of HBsAg and induces mutations, making it undetectable by con-
REVIEW
ventional assay (2,15). If this mechanism holds true, then total
anti-HBc level may be used as a surrogate biomarker for occult
ISOLATED CORE ANTIBODY-POSITIVE HEPATITIS B HBV or liver damage in HCV co-infection.
AND HEPATITIS C CO-INFECTION
Patients with IAHBc are more frequently co-infected with hepa-
titis C virus (HCV) when compared with patients with positive REACTIVATION RISK OF HEPATITIS B WITH ISOLATED
anti-HBs (9). Moreover, anti-HBc positive patients have been CORE ANTIBODY
associated with more active hepatitis C. A study by Wedemeyer Although HBV reactivation has been studied extensively, charac-
et al. (10) found that IAHBc occurred more frequently when com- teristics of reactivation among IAHBc patients is less well defined.
paring HCV RNA-positive and negative patients (22% vs. 13%, Table 2 provides a summary of reactivation risk in IAHBc patients
P<0.0001). The authors suggested mechanisms of increased HCV receiving therapies specific to gastrointestinal and hepatic diseases.
replication in patients with IAHBc, including the cross-reactivity Further research needs to be done to define risk among IAHBc
of immune response. For instance, the presence of anti-HBs and patients in other medical and surgical interventions such as loco-
partial resolution of HBV may have implied a stronger immune regional therapies and hepatectomy for hepatocellular carcinoma.
response to both viruses, allowing for HCV suppression. Subse-
quent loss of anti-HBs may then allow for increased viremia and HCV direct-acting antiviral therapy
activity of HCV. HCV treatment and the alteration of immune synergy in co-infec-
An alternative explanation for HCV co-infection and IAHBc tion must take into consideration the risk of HBV reactivation. In
suggests that chronic HCV dominates immune response over October of 2016, the US Food and Drug Administration issued
HBV. HCV core protein may directly suppress transcription of a drug safety Boxed Warning after identifying 29 cases of HBV
HBV RNA (11). HCV proteins may also limit HBsAg expres- reactivation in hepatitis B and C co-infected patients undergoing
sion, resulting in lower level of viremia, as well as enhance clear- treatment with HCV direct-acting antiviral (DAA) therapies. Of
ance of HBsAg (12). Sheen et al. (13) observed a rate of HBsAg the 29 cases, two patients died and one required liver transplanta-
clearance 2.5 times faster in co-infected patients vs. patients with tion. Notably, HBV co-infected individuals were excluded from
HBV mono-infection. Thus, the serological pattern of IAHBc may clinical trials evaluating the safety of DAA medications. There-
actually result from increased HCV viremia. fore, HBV reactivation had not been reported as an adverse drug
IAHBc may represent potential for OBI among patients event (16).
with chronic HCV, who are already at high-risk for related liver Joint American Association for the Study of Liver Diseases and
injury (2). In one cohort study, up to 22.5% of IAHBc patients with Infectious Diseases Society of America guidelines recommend all
Table 2. Summary of HBV reactivation risk in IAHBc (HBsAg negative and anti-HBc positive) individuals receiving therapies specific to
gastrointestinal and hepatic diseases
Therapy GI/liver indication Reactivation risk Prophylaxis
a,b,c
DAA therapy HCV treatment Low Monitor for reactivation and treat
if clinically evident
Traditional immunosuppressive agents (azathioprine, Inflammatory bowel disease Lowd Monitor for reactivation and treat
6-mercaptopurine, methotrexate) if clinically evident
TNF-α inhibitors (etanercept, adalimumab, infliximab) Inflammatory bowel disease Moderate (1–10%)d Recommendedd,e
Anthracycline derivatives (doxorubicin) Hepatocellular carcinoma Moderate (1–10%)d Recommendedd,e
d
B-cell-depleting agents (rituximab) Extrahepatic manifestations of Hepatitis C High (>10%) Recommendedd,f
virus infection
Autoimmune hepatitis
Anti-HBc, hepatitis B core antibody; DAA, direct-acting antiviral; GI, gastrointestinal; HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus; HCV, hepatitis C virus;
IAHBc, isolated hepatitis B core antibody; TNF-α , tumor necrosis factor-α .
a
Tang et al. (19).
b
Loggi et al. (20).
c
Yeh et al. (21).
d
Reddy et al. (22).
e
Prophylaxis to continue at least 6 months after discontinuation of therapy. Patients may reasonably opt out of prophylaxis if they value avoiding long-term antiviral use
and cost over the risk of reactivation.
f
Prophylaxis to continue at least 12 months after discontinuation of therapy.
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
1784 Wu et al.
patients undergoing HCV DAA therapy be evaluated for HBV factor (TNF)-α inhibitors, other cytokine and integrin inhibi-
coinfection by measuring HBsAg, anti-HBs, and anti-HBc levels tors, tyrosine kinase inhibitors, and use of corticosteroids for
(17). For patients with positive HBsAg, HBV DNA level should more than 4 weeks. High reactivation risk is defined as ≥10% and
REVIEW
be measured prior to starting DAA therapy. For patients meeting includes B-cell-depleting agents (22).
treatment criteria for HBV treatment, therapy should be given Two notable classes of immune suppression agents that have
before or at the same time as treatment for HCV. Among patients been associated with HBV reactivation in the setting of IAHBc
with IAHBc serology, there is currently insufficient data to pro- patients include: rituximab and anti-tumor necrosis factor inhibi-
vide clear recommendations for monitoring during or after DAA tors.
therapy (17). Rituximab, the monoclonal antibody against CD20 antigen of B
Since the release of recommendations by US Food and Drug cells, has well-known complications of use including HBV reacti-
Administration and American Association for the Study of Liver vation (23). Retrospective studies describe reactivation rates rang-
Diseases, several independent investigators have sought to identify ing from 8.9 to 23.8% among IAHBc patients, with reactivation
the overall risk of HBV reactivation in the setting of DAA therapy. occurring up to one year after completion of therapy (24,25). How-
Belperio et al. (18) performed a retrospective evaluation of over ever, one prospective study among patients undergoing rituximab-
62,000 HCV-infected patients. Data were considerably limited containing chemotherapy for lymphoma reported up to 41.5%
by availability of testing results, with HBV DNA values provided cumulative 2-year reactivation rate (26). More recently, rituximab
for 0.9% of patients with ALT elevation. The study identified nine has been used in the setting of desensitization for transplantation
unique patients who demonstrated HBV reactivation during DAA and immune suppression in this context has also been associated
treatment, most of whom had normal or less than 2 times the with HBV reactivation with a median time to reactivation at 11
upper limit of normal ALT with rare occurrence of severe hepa- months. Cases have included severe hepatitis and death due to
titis. Only one of the nine cases was known to have IAHBc (18). hepatic failure (27). Other reports of reactivation have similarly
Several retrospective studies have reported no HBV reactiva- carried poor prognoses during rituximab use (28). Ofatumumab,
tion events among IAHBc patients during DAA treatment. Tang another B-cell-depleting agent similar to rituximab, has limited
et al. (19) found no reactivations among 68 patients from the data on HBV reactivation; however, it is also deemed high risk
Baltimore Veterans Affairs Medical Center database, who had given the analogous mechanism of action (23).
IAHBc and chronic HCV for which DAA treatment was initiated Tumor necrosis factor -α inhibitors (anti-tumor necrosis fac-
between December 2014 and August 2016. Two patients demon- tor), such as etanercept, infliximab, and adalimumab, have also
strated a rise in ALT above the upper limit of normal, however both been associated with HBV reactivation. Rates of reactivation have
normalized without intervention (19). Loggi et al. (20) similarly been much lower than that in rituximab, with retrospective stud-
reported no reactivation events in a study of 42 IAHBc patients ies citing as low as 1.7% in IAHBc patients (29). A recent multi-
undergoing DAA treatment between January 2015 and January center, observational study of patients with spondyloarthritis and
2016. Yeh et al. (21) also found no episodes of HBV reactivation previously resolved HBV infection showed no reactivation among
among 57 IAHBc patients on DAA treatment between December IAHBc patients. After 75 months of follow-up, HBV DNA was
2013 and August 2016. undetectable and HBsAg remained negative (30).
Although these studies reveal minimal to no risk of reactivation Separate from immunosuppressive drugs, hematopoietic stem
among IAHBc patients undergoing DAA therapy, identifying such cell transplant has also been linked to HBV reactivation among
patients through evaluation of HBV DNA level, prior to initiation IAHBc patients. Retrospective studies describe a range of reacti-
remains essential. Providers should recognize the potential risk vation rates from 6.5 to 19.7% (31–33). Yet, a prospective study
and monitor for signs of HBV reactivation as currently suggested showed a much higher upper limit at 40.8% cumulative 2-year
in guidelines and initiate treatment as appropriate (17). reactivation rate, with two important determinants of reactivation
being chronic graft-vs.-host disease and age >50 years old (34).
Immune suppressive therapy Regarding screening before initiation of therapy, both the
HBV reactivation is a key consideration when initiating immuno- American Gastroenterological Association and American Asso-
suppressive medications. The 2015 American Gastroenterological ciation for the Study of Liver Diseases agree on recommendations
Association guidelines summarized the prevention and treatment to screen for HBV, specifically in patients at moderate or high risk,
of HBV reactivation during immunosuppressive therapy. When before immunosuppressive therapy (35). Screening with HBsAg
considering IAHBc patients, the use of antiviral prophylaxis is and anti-HBc, however, is not recommended among patients at
categorized by level of risk of reactivation, with types of immu- low risk (22).
nosuppression categorized into low-, moderate-, and high-risk
groups depending on perceived intensity of therapy and associ-
ated risk. Low reactivation risk is defined as <1% and includes HCC RISK WITH ISOLATED CORE ANTIBODY
traditional immunosuppressive agents such as azathioprine, CHB is associated with a significant increased risk for develop-
6-mercaptopurine, and methotrexate, as well as use of corticos- ment of HCC. HBV accounts for up to 60% of total HCC
teroids for up to one week. Moderate reactivation risk is higher cases in developing countries and 23% of cases in developed
at 1–10% and includes anthracycline derivatives, tumor necrosis countries (36). Various mechanisms are described in HBV-related
The American Journal of GASTROENTEROLOGY VOLUME 112 | DECEMBER 2017 www.nature.com/ajg
The Relevance of Hepatitis B Core Antibody 1785
carcinogenesis including integration of HBV DNA into host dependent on HBV DNA formation, and is detected altogether by
genome, viral protein expression, chronic inflammation, and antibodies to HBcrAg in the assay (41,42).
cytokine induction of fibrosis and liver cell proliferation (36). HBcrAg has been found to correlate significantly with HBV
REVIEW
In addition, patients with CHB may have additional risk factors covalently closed circular DNA (cccDNA), the template for
associated with HCC development including sex, age, tobacco HBV RNA transcription within hepatocyte nuclei. Direct meas-
and alcohol use, chemical carcinogens, hormonal factors, and urement of cccDNA requires liver biopsy and is therefore not a
genetic susceptibility (37). practical marker for infection. Similar correlation has been iden-
Previous studies have shown that anti-HBc is more common tified between HBcrAg-cccDNA and HBV DNA-cccDNA. How-
than HBeAg or HBV DNA in patients with HCC (38). As previ- ever, HBV DNA is not a useful surrogate for cccDNA, as it often
ously mentioned, anti-HBc has been examined as a surrogate for becomes undetectable with nucleos (t)ide analog treatment (41).
OBI. In this setting, investigators sought to identify an association Currently, assays for HBcrAg are available in Asia and Europe but
between OBI and HCC. In a prospective study of IAHBc patients not yet commercially available in the United States or Canada.
with non-HBV, non-HCV cirrhosis, carcinogenesis rates in patients HBcrAg has been studied for distribution patterns across the
with positive HBV DNA and negative HBV DNA were 27% and phases of HBV infection. High levels of HBcrAg have correlated
11.8%, respectively, at 5-year follow-up, and 100% and 17.6%, with HBeAg-positive phases of infection, which is expected given
respectively, at 10-year follow-up (P=0.0078, log-rank test). HBV the shared components of the amino acid sequence. HBcrAg levels
DNA positivity increased rate of carcinogenesis by a hazard ratio correlate strongly with serum HBV DNA during immune clear-
of 8.25 (95% confidence interval 2.01–33.93, P=0.003). During the ance and HBeAg-negative reactivation, suggesting its role in sign-
observational period, the median time from diagnosis of cirrhosis aling viral replication (43).
to HCC was 5.6 years. Despite being a single cohort study, these HBcrAg thereby can assist in differentiating between HBeAg-
findings suggested OBI to be an independent risk factor for hepa- negative active and quiescent disease. Studies have reported
tocarcinogenesis (39). patients initially classified as quiescent infection by HBV DNA,
Another study examined patients with non-HBV, non-HCV ALT, or liver biopsy, who also expressed higher levels of HBcrAg
HCC, in an area endemic to HBV. Over 40% of the cohort popu- and demonstrated an increased chance for HBV reactivation
lation were IAHBc, further suggesting OBI as a potential link to (43). As such, HBcrAg may serve a role as a surrogate marker for
HCC development (40). These findings may suggest a benefit to immune activation.
HCC screening among IAHBc patients, although further studies HBcrAg has also been detected in up to 40% of CHB patients
are required to make this recommendation. who have achieved HBsAg seroclearance, or who are designated
Anti-HBc has also been shown to be prognostically significant in as occult carriers of HBV (42). When identified as a potential
HCC recurrence after curative resection. In a study of HBV-related marker for occult HBV, various investigators have sought to assess
HCC cases by Li et al. (36), anti-HBc positivity was found to be an HBcrAg as a surrogate of disease activity as well as HCC. In a study
independent prognostic factor for recurrence free survival. Among by Tada et al. (37) elevated levels of HBcrAg were independently
patients positive for anti-HBc, recurrence free survival rates were associated with HCC incidence (hazard ratio 5.05; 95% confidence
lower than those without anti-HBc at 1-,3-, and 5-years (77.9%, interval 2.40–10.63, P<0.001). HBcrAg was also found to be supe-
58.6%, and 46.9%, vs. 92.5%, 72.1%, and 65.9%, respectively, rior to other continuous HBV serological markers for predicting
P<0.001). However, overall survival was not significantly different HCC development among patients not receiving NA therapy (37).
between anti-HBc-positive and -negative patients. Anti-HBc In a study of HBV reactivation in IAHBc patients by Seto et al.
positivity was also associated with early intrahepatic recurrence, (44), HBcrAg-positivity was shown to be a significant risk factor for
possibly indicating a more invasive phenotype of HCC. Neverthe- reactivation events in patients undergoing high-risk immunosup-
less, among HBsAg-negative patients, anti-HBc positivity had no pression of rituximab therapy (hazard ratio 2.94, 95% confidence
prognostic significance (36). This suggests that IAHBc may not be interval 1.43–6.07, P=0.004). Of note, a separate cohort of patients
as telling as the role of anti-HBc in the presence of HBsAg. in the same study, undergoing hematopoietic stem cell transplant,
did not show a significant correlation between HBcrAg-positivity
and HBV reactivation. However, in the rituximab cohort, patients
HEPATITIS B CORE-RELATED ANTIGEN positive for HBcrAg had a significantly higher 2-year cumulative
Hepatitis B core-related antigen (HBcrAg) is emerging as a poten- reactivation rate than HBcrAg negative patients (71.8% vs. 31%,
tially clinically useful serological marker of HBV infection. This P=0.002) (44). Given its clinical significance as a risk factor for
assay detects an amino acid sequence shared collectively by the reactivation, the use of HBcrAg may be a valuable supplemental
HBcAg, HBeAg, and a 22 kDa precore protein. As described pre- test. Positive HBcrAg implies persistence of HBV infection, despite
viously, HBcAg is a structural unit of viral capsids and is trans- loss of HBsAg. As such, HBcrAg may be used as a marker to screen
lated from viral pregenomic RNA. HBeAg is a non-structural for patients with IAHBc, who are at-risk for reactivation and would
immunomodulating secretory protein and is translated from benefit from prophylaxis.
HBV precore mRNA. The 22 kDA precore protein, also desig- Among patients treated with nucleos (t)ide analog therapy,
nated as p22cr, is similarly translated from precore mRNA. The Honda et al. (45) reported that HBcrAg positivity was also inde-
three components share a 149-amino acid sequence, which is not pendently associated with HCC development. Presence of HBcrAg
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
1786 Wu et al.
Table 3. Statistical analysis of HBcrAg related to markers and outcomes of chronic hepatitis B infection
Marker Phase of infection Correlation coefficient (r) P-value
REVIEW
a
cccDNA Not reported 0.70 <0.0001
Serum HBV DNA levelb Overall 0.87 <0.0001
IT 0.45 0.0130
IC 0.66 <0.0001
ENH 0.74 <0.0001
ENQ 0.18 0.054
HBsAg levelb Overall 0.78 <0.0001
IT 0.47 0.0095
IC 0.53 <0.0001
ENH 0.40 0.0045
ENQ 0.47 <0.0001
Outcome Hazard ratio 95% CI P-value
HBV reactivation risk in setting of rituximab therapyc 2.94 1.43–6.07 0.004
d
HCC development 5.05 2.40–10.63 <0.001
HCC development in setting of nucleoside analog therapye 3.53 1.52–9.63 0.0025
cccDNA, covalently closed circular DNA; CI, confidence interval; ENH, HBeAg-negative hepatitis; ENQ, HBeAg-negative quiescent phase; HBcrAg, hepatitis B core-
related antigen; HBV, hepatitis B virus; HBeAg, hepatitis B e antigen; IC, immune clearance; IT, immune tolerance.
a
Wong et al. (41).
b
Maasoumy et al. (43).
c
Seto et al. (44).
d
Tada et al. (37).
e
Honda et al. (45).
was indicative of cccDNA activation, HBV replication in the liver, persistence in the bloodstream. The serological pattern of IAHBc
and was found to be predictive of HCC (45). In a separate study, has been of clinical interest over the past several years, with grow-
higher levels of HBcrAg, both pre- and post-nucleos (t)ide analog ing data suggesting a role as a marker for OBI. IAHBc has impor-
treatment, were associated with risk of HCC development. These tant clinical implications in the setting of co-infection with HCV,
patients had otherwise undetectable HBV DNA. When stratified HBV reactivation risk with HCV DAA therapy and immuno-
by cirrhosis status, cirrhotic patients had no significant difference suppression, as well as the progression of liver disease and HCC
in HBcrAg levels among those with and without HCC. However, development. HBcrAg is emerging as an important laboratory
for non-cirrhotic patients, median HBcrAg level was signifi- assay that may serve as a surrogate marker for infection, identify-
cantly higher in patients with HCC compared with those without ing occult cases of HBV through additional serological studies,
(P=0.030) (46). This finding may suggest the utility of HBcrAg in and, more importantly, as a potential marker for HBV clearance
predicting HCC development in non-cirrhotic patients. for future therapies.
Table 3 summarizes the association between HBcrAg and vari-
ous markers and outcomes of CHB. CONFLICT OF INTEREST
In clinical practice, HBcrAg has many potential roles as a rel- Guarantor of the article: Tiffany Wu, MD.
evant marker for disease activity. Given its correlation to active Specific author contributions: T. Wu conducted literature review.
viral replication, high levels of HBcrAg may be used to identify T. Wu, R. Kwok, and T. Tran wrote and developed the manuscript.
occult infection when screening patients at risk of reactivation Financial support: None.
before immunosuppressive therapy. This serological marker may Potential competing interests: None.
also help to predict HCC development in the setting of nucleos (t)
ide analog therapy, especially among non-cirrhotic patients.
REFERENCES
1. Ponde RA, Cardoso DD, Ferro MO. The underlying mechanisms for the
SUMMARY ‘anti-HBc alone’ serological profile. Arch Virol 2010;155:149–58.
2. Kang SY, Kim MH, Lee WI. The prevalence of ‘anti-HBc alone’ and HBV
Anti-HBc is currently considered the most sensitive serological DNA detection among anti-HBc alone in Korea. J Med Virol 2010;82:
marker for a patient’s history of HBV infection given its long-term 1508–14.
The American Journal of GASTROENTEROLOGY VOLUME 112 | DECEMBER 2017 www.nature.com/ajg
The Relevance of Hepatitis B Core Antibody 1787
3. Raimondo G, Caccamo G, Filomia R et al. Occult HBV infection. Semin chemotherapy for lymphoma: a prospective study. J Clin Oncol
Immunopathol 2013;35:39–52. 2014;32:3736–43.
4. Song LW, Liu PG, Liu CJ et al. Quantitative hepatitis B core antibody levels 27. Lee J, Park JY, Huh KH et al. Rituximab and hepatitis B reactivation in
in the natural history of hepatitis B virus infection. Clin Microbiol Infect HBsAg-negative/anti-HBc-positive kidney transplant recipients. Nephrol
2015;21:197–203. Dial Transplant 2017;32:722–9.
REVIEW
5. Jia W, Song L-W, Fang Y-Q et al. Antibody to hepatitis B core antigen levels 28. Pei SN, Chen CH, Lee CM et al. Reactivation of hepatitis B virus following
in the natural history of chronic hepatitis B: a prospective observational rituximab-based regimens: a serious complication in both HBsAg-positive
study. Medicine 2014;93:e322. and HBsAg-negative patients. Ann Hematol 2010;89:255–62.
6. Terrault NA, Bzowej NH, Chang KM et al. AASLD guidelines for treatment 29. Lee YH, Bae SC, Song GG. Hepatitis B virus reactivation in rheumatic
of chronic hepatitis B. Hepatology 2016;63:261–83. patients with hepatitis core antigen (HBV occult carriers) undergoing
7. Ramezani A, Banifazi M, Eslamifar A et al. Serological pattern of anti-HBc anti-tumor necrosis factor therapy. Clin Exp Rheumatol 2013;31:118–21.
alone infers occult hepatitis B virus infection in high-risk individuals in 30. Giannitti C, Lopalco G, Vitale A et al. Long-term safety of anti-TNF agents
Iran. J Infect Dev Ctries 2010;4:658–61. on the liver of patients with spondyloarthritis and potential occult hepatitis
8. Launay O, Masurel J, Delmas AS et al. High levels of serum hepatitis B B viral infection: an observational multicentre study. Clin Exp Rheumatol
virus DNA in patients with ‘anti-HBc alone’: role of HBsAg mutants. J Viral 2017;35:93–7.
Hepat 2011;18:721–29. 31. Varma A, Biritxinaga L, Saliba RM et al. Impact of hepatitis B core antibody
9. Jilg W, Sieger E, Zachoval R et al. Individuals with antibodies against seropositivity on the outcome of autologous hematopoietic stem cell
hepatitis B core antigen as the only serological marker for hepatitis B transplantation for multiple myeloma. Biol Blood Marrow Transplant
infection: high percentage of carriers of hepatitis B and C virus. J Hepatol 2017;23:581–7.
1995;23:14–20. 32. Vigano M, Vener C, Lampertico P et al. Risk of hepatitis B surface antigen
10. Wedemeyer H, Cornberg M, Tegtmeyer B et al. Isolated anti-HBV core seroreversion after allogeneic hematopoietic SCT. Bone Marrow Transplant
phenotype in anti-HCV-positive patients is associated with hepatitis C 2011;46:125–31.
virus replication. Clin Microbiol Infect 2004;10:70–2. 33. Hammond SP, Borchelt AM, Ukomadu C et al. Hepatitis B virus reactiva-
11. Schuttler CG, Fiedler N, Schmidt K et al. Suppression of hepatitis B virus tion following allogeneic hematopoietic stem cell transplantation. Biol
enhancer 1 and 2 by hepatitis C virus core protein. J Hepatol 2002;37:855–62. Blood Marrow Transplant 2009;15:1049–59.
12. Chu CM, Yeh CT, Liaw YF. Low-level viremia and intracellular expression 34. Seto WK, Chan TS, Hwang YY et al. Hepatitis B reactivation in occult viral
of hepatitis B surface antigen (HBsAg) in HBsAg carriers with concurrent carriers undergoing hematopoietic stem cell transplantation: a prospective
hepatitis C virus infection. J Clin Microbiol 1998;36:2084–6. study. Hepatology 2017;65:1451–61.
13. Sheen IS, Liaw YF, Lin DY et al. Role of hepatitis C and delta viruses in the 35. Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology
termination of chronic hepatitis B surface antigen carrier state: a multivariate 2009;50:661–2.
analysis in a longitudinal follow-up study. J Infect Dis 1994;170:358–61. 36. Li T, Wang SK, Zhou J et al. Positive HBcAb is associated with higher
14. El-Sherif A, Abou-Shady M, Abou-Zeid H et al. Antibody to hepatitis B risk of early recurrence and poorer survival after curative resection of
core antigen as a screening test for occult hepatitis B virus infection in HBV-related HCC. Liver Int 2016;36:284–92.
Egyptian chronic hepatitis C patients. J Gastroenterol 2009;44:359–64. 37. Tada T, Kumada T, Toyoda H et al. HBcrAg predicts hepatocellular carci-
15. Weber B, Melchior W, Gehrke R et al. Hepatitis B virus markers in anti- noma development: an analysis using time-dependent receiver operating
HBc only positive individuals. J Med Virol 2001;64:312–9. characteristics. J Hepatol 2016;65:48–56.
16. Bersoff-Matcha SJ, Cao K, Jason M et al. Hepatitis B virus reactivation 38. Sjogren MH, Dusheiko GM, Kew MC et al. Hepatitis B virus infection and
associated with direct-acting antiviral therapy for chronic hepatitis C virus: hepatocellular carcinoma: correlation between IgM antibody to hepatitis B
a review of cases reported to the U.S. Food and Drug Administration core antigen, hepatitis B e antigen, and hepatitis B DNA. Am J Trop Med
Adverse Event Reporting System. Ann Intern Med 2017;166:792–8. Hyg 1988;39:582–5.
17. AASLD-IDSA. HCV Guidance: Recommendations for testing, managing, 39. Ikeda K, Kobayashi M, Someya T et al. Occult hepatitis B virus infection
and treating hepatitis C. Available at http://hcvguidelines.org/full-report/ increases hepatocellular carcinogenesis by eight times in patients with
monitoring-patients-who-are-starting-hepatitis-c-treatment-are-treatment- non-B, non-C liver cirrhosis: a cohort study. J Viral Hepat 2009;16:437–43.
or-have. Accessed 4 April 2017. 40. Lee SB, Kim KM, An J et al. Clinical characteristics and potential aetio-
18. Belperio PS, Shahoumian TA, Mole LA et al. Evaluation of hepatitis B logies of non-B non-C hepatocellular carcinoma in hepatitis B virus
reactivation among 62,920 veterans treated with oral hepatitis C antivirals. endemic area. Liver Int 2016;36:1351–61.
Hepatology 2017;66:27–36. 41. Wong DK, Seto WK, Cheung KS et al. Hepatitis B virus core-related
19. Tang L, Tolaymat M, Stonesifer E et al. Absence of hepatitis B reactivation antigen as a surrogate marker for covalently closed circular DNA. Liver Int
among veterans with serological evidence of previous hepatitis B infection 2016;37:995–1001.
receiving anti-hepatitis C direct acting antivirals. J Hepatol Abstracts of The 42. Seto WK, Wong DK, Fung J et al. Linearized hepatitis B surface antigen and
International Liver Congress 2017;66:S251–2. hepatitis B core-related antigen in the natural history of chronic hepatitis B.
20. Loggi E, Gitto S, Galli S et al. Hepatitis B virus reactivation among hepatitis Clin Microbiol Infect 2014;20:1173–80.
C patients treated with direct-acting antiviral therapies in routine clinical 43. Maasoumy B, Wiegand SB, Jaroszewicz J et al. Hepatitis B core-related
practice. J Clin Virol 2017;93:66–70. antigen levels in the natural history of hepatitis B virus infection in a large
21. Yeh ML, Huang CF, Hsieh MH et al. Reactivation of hepatitis B in patients European cohort predominantly infected with genotypes A and D. Clin
of chronic hepatitis C with hepatitis B virus infection treated with direct Microbiol Infect 2015;21:606.e1–10.
acting antivirals. J Gastroenterol Hepatol 2017;32:1754–62. 44. Seto WK, Wong DH, Chan TY et al. Association of hepatitis B core-
22. Reddy KR, Beavers KL, Hammond SP et al. American Gastroenterological related antigen with hepatitis B virus reactivation in occult viral carriers
Association Institute guideline on the prevention and treatment of hepatitis B undergoing high-risk immunosuppressive therapy. Am J Gastroenterol
virus reactivation during immunosuppressive drug therapy. Gastroenterology 2016;111:1788–95.
2015;148:215–9. 45. Honda M, Shirasaki T, Terashima T et al. Hepatitis B virus core-related
23. Perrillo RP, Gish R, Falck-Ytter YT. American Gastroenterological Association antigen during nucleos (t)ide analog therapy is related to intra-hepatic
Institute technical review on prevention and treatment of hepatitis B virus HBV replication and development of hepatocellular carcinoma. J Infect Dis
reactivation during immunosuppressive drug therapy. Gastroenterology 2016;213:1096–106.
2015;148:221–44. 46. Cheung KS, Seto WK, Wong DK et al. Relationship between HBsAg,
24. Matsue K, Kimura S, Takanashi Y et al. Reactivation of hepatitis B virus HBcrAg and hepatocellular carcinoma in patients with undetectable HBV
after rituximab-containing treatment in patients with CD20-positive B-cell DNA under nucleos (t)ide therapy. J Viral Hepat 2017;24:654–61.
lymphoma. Cancer 2010;116:4769–76. 47. Jilg W, Hottenträger B, Weinberger K et al. Prevalence of markers of
25. Yeo W, Chan TC, Leung NW et al. Hepatitis B virus reactivation in lympho- hepatitis B in the adult German population. J Med Virol 2001;63:96–102.
ma patients with prior resolved hepatitis B undergoing anticancer therapy 48. Kleinman SH, Kuhns MC, Todd DS et al. Retrovirus Epidemiology Donor
with or without rituximab. J Clin Oncol 2009;27:605–11. Study. Frequency of HBV DNA detection in US blood donors testing posi-
26. Seto WK, Chan TS, Hwang YY et al. Hepatitis B reactivation in patients tive for the presence of anti-HBc: implications for transfusion transmission
with previous hepatitis B virus exposure undergoing rituximab-containing and donor screening. Transfusion 2003;43:696–704.
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
1788 Wu et al.
49. Alhababi F, Sallam TA, Tong CY. The significance of ‘anti-HBc only’ in the 55. Gibney KB, Torresi J, Lemoh C et al. Isolated core antibody hepatitis B in
clinical virology laboratory. J Clin Virol 2003;27:162–9. sub-Saharan African immigrants. J Med Virol 2008;80:1565–9.
50. Garcia-Montalvo BM, Farfan-Ale JA, Acosta-Viana KY et al. Hepatitis B 56. Ramezani A, Banifazl M, Eslamifar A et al. Serological pattern of anti-HBc
virus DNA in blood donors with anti-HBc as a possible indicator of active alone infers occult hepatitis B virus infection in high-risk individuals in
hepatitis B virus infection in Yucatan, Mexico. Transfus Med 2005;15: Iran. J Infect Dev Ctries 2010;4:658–61.
REVIEW
371–8. 57. Tramuto F, Maida CM, Colomba GM et al. Occult hepatitis B infection in
51. Knöll A, Hartmann A, Hamoshi H et al. Serological pattern ‘‘anti-HBc the immigrant population of Sicily, Italy. J Immigr Minor Health 2013;15:
alone’’: characterization of 552 individuals and clinical significance. World J 725–31.
Gastroenterol 2006;12:1255–60. 58. Rios-Ocampo WA, Cortes-Mancera F, Olarte JC et al. Occult hepatitis B
52. Banerjee A, Chandra PK, Datta S et al. Frequency and significance of virus infection among blood donors in Colombia. Virol J 2014;11:206.
hepatitis B virus surface gene variant circulating among 'antiHBc only' 59. Jutavijittum P, Andernach IE, Yousukh A et al. Occult hepatitis B infections
individuals in Eastern India. J Clin Virol 2007;40:312–7. among blood donors in Lao PDR. Vox Sang. 2014;106:31–7.
53. El-Zaatari M, Kazma H, Naboulsi-Majzoub M et al. Hepatitis B virus 60. Antar W, El-Shokry MH, Abd El Hamid WA et al. Significance of detecting
DNA in serum of ‘anti-HBc only’-positive healthy Lebanese blood donors: anti-HBc among Egyptian male blood donors negative for HBsAg. Transfus
significance and possible implications. J Hosp Infect. 2007;66:278–82. Med 2010;20:409–13.
54. Vitale F, Tramuto F, Orlando A et al. Can the serological status of anti-HBc 61. Kishk R, Nemr N, Elkady A et al. Hepatitis B surface gene variants isolated
alone be considered a sentinel marker for detection of occult HBV infection? from blood donors with overt and occult HBV infection in north eastern
J Med Virol 2008;80:577–82. Egypt. Virol J 2015;12:153.
The American Journal of GASTROENTEROLOGY VOLUME 112 | DECEMBER 2017 www.nature.com/ajg
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Self-Assessment Colour Review of Small Animal Soft Tissue SurgeryDocument194 pagesSelf-Assessment Colour Review of Small Animal Soft Tissue Surgerymiliindianu100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Jay Wiseman's Negotiation ChecklistDocument18 pagesJay Wiseman's Negotiation ChecklistDoveAndTheCrow100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hemodynamic Disorders, Thrombosis, and Shock GWAIDocument102 pagesHemodynamic Disorders, Thrombosis, and Shock GWAIkavindukarunarathnaNo ratings yet
- Pediatrics MnemonicsDocument11 pagesPediatrics MnemonicsIndrajit Rana95% (21)
- Zoology CH 8 Animal Like Pro TistsDocument103 pagesZoology CH 8 Animal Like Pro TistsTHUNDERCLASH_SILVEREYES139100% (3)
- The Infectious Hazards of Dead BodiesDocument3 pagesThe Infectious Hazards of Dead Bodiespenn hicksNo ratings yet
- Typhoid 21Document9 pagesTyphoid 21Nanda Hikma LestariNo ratings yet
- Safety Action Bundle: Surgical Site Infections (SSI) - ColorectalDocument4 pagesSafety Action Bundle: Surgical Site Infections (SSI) - ColorectalYunita PanjaitanNo ratings yet
- Nose, Sinuses, Mouth, and LarynxDocument3 pagesNose, Sinuses, Mouth, and LarynxjottowagNo ratings yet
- Canine Distemper VirusDocument5 pagesCanine Distemper VirusDumapis RichardNo ratings yet
- 1 1 2 A Investigatingoutbreak 1Document2 pages1 1 2 A Investigatingoutbreak 1api-327503253No ratings yet
- Bean Productions Problems of Phaseolus VulgarisDocument415 pagesBean Productions Problems of Phaseolus Vulgarisherodo100% (3)
- Chapter Test # 2 Biological Classification BIO Prodigy Test SeriesDocument3 pagesChapter Test # 2 Biological Classification BIO Prodigy Test SeriesLively LipunNo ratings yet
- Piercings: Techniques and Complications: Christa de Cuyper, Maria Luisa Pérez-Cotapos S., and Roberto CullenDocument19 pagesPiercings: Techniques and Complications: Christa de Cuyper, Maria Luisa Pérez-Cotapos S., and Roberto CullenGhalyRizqiMauludinNo ratings yet
- Fungi, Viruses and ParasitesDocument31 pagesFungi, Viruses and ParasitesIraqiNo ratings yet
- C.V AfayoDocument4 pagesC.V AfayoAfayo RobertNo ratings yet
- Answer Key - Biology EOC Essential Standard Study GuideDocument26 pagesAnswer Key - Biology EOC Essential Standard Study GuideHithe60% (5)
- Vibrio and Related Species NotesDocument3 pagesVibrio and Related Species NotesYelai CarveroNo ratings yet
- MorbiliDocument43 pagesMorbiliNur AtikaNo ratings yet
- Chapter 22 Upper Respiratory DisorderDocument171 pagesChapter 22 Upper Respiratory DisorderAnnette Aquino GuevarraNo ratings yet
- 1º Atividade para Os 4º Anos - GABARITODocument3 pages1º Atividade para Os 4º Anos - GABARITOChrisNo ratings yet
- Para Lec CombinedDocument83 pagesPara Lec CombinedClent Earl Jason O. BascoNo ratings yet
- Review On Dermatomycosis Jurnal 2Document23 pagesReview On Dermatomycosis Jurnal 2Laela NurrochmahNo ratings yet
- Biology Quarter 1 Unit 2 Day 6 Immune System ArticleDocument4 pagesBiology Quarter 1 Unit 2 Day 6 Immune System ArticleTeachTappyNo ratings yet
- Contagion Film Analysis QuestionsDocument3 pagesContagion Film Analysis QuestionsAnonymous zBFTSrNo ratings yet
- Free Online Mock Test For MHT-CET BIOLOGY PDFDocument28 pagesFree Online Mock Test For MHT-CET BIOLOGY PDFBiologyForMHTCET75% (8)
- Chapter 53 - Introduction To The Respiratory SystemDocument13 pagesChapter 53 - Introduction To The Respiratory SystemJonathonNo ratings yet
- EPI and HIV 1Document5 pagesEPI and HIV 1April Ivonne Claire BatoNo ratings yet
- CH 18 Haemophilus and Other Fastidious GNBDocument37 pagesCH 18 Haemophilus and Other Fastidious GNBshericeNo ratings yet
- HPV PCRDocument34 pagesHPV PCRGuneyden GuneydenNo ratings yet