Professional Documents
Culture Documents
Heart Transplant
Heart Transplant
Uploaded by
John Christopher Asilo AsiloCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Heart Transplant
Heart Transplant
Uploaded by
John Christopher Asilo AsiloCopyright:
Available Formats
KIDNEY
TRANSPLANTATION
JOHN CHRISTOPHER A. ASILO, RPH
Masters of Science in Pharmacy with specialization in Clinical
Pharmacy and Research
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 1 of 22
Kidney Transplantation
■ It is the renal replacement therapy of choice for suitable patients with advanced Chronic
Kidney Disease or END-Stage Renal Disease.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 2 of 22
Kidney Transplantation: Timing of
Referral
■ Survival after transplant is worse the longer a patient is on dialysis.
■ Patient and Graft survival are improved in patients transplanted preemptively.
■ The pretransplant evaluation and testing can take several months to complete,
potentially delaying addition to the waiting list, and therefore especially in diabetics,
early referral is essential.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 3 of 22
Pre-Transplant Evaluation
■ The goal of the evaluation:
– To identify any contraindications to transplantation
– To determine immunologic factors impacting donor kidney options
– To screen for comorbid conditions that need to be identified and managed prior to
transplantation
– To assess psycosocial factors that could affect the success of the transplant
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 4 of 22
Pre-Transplant Evaluation
■ The greatest morbidity and mortality from transplantation occurs in the first year after
transplant and consist both cardiovascular and infectious complications.
■ Patients with high near term mortality
■ Patients with histories of medication non-adherence or psychiatric illness that may limit
their ability to adhere to post-transplantation care need to properly address these
concerns prior to transplantation.
■ Patients with primary oxalosis should be considered carefully.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 5 of 22
Pre-Transplant Evaluation
■ Immunology
■ Panel Reactive Antibody
■ Cardiovascular Disease
– Ischaemic Heart Disease
– Structural Heart Disease
– Peripheral Vascular Disease
– Tobacco Use
– Hypercoagulable State
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 6 of 22
Pre-Transplant Evaluation
■ Infection
– Hepatitis B Virus
– Hepatitis C Virus
– HIV
– Tuberculosis
– Bacterial Infection
– Prophylactic Vaccination
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 7 of 22
Pre-Transplant Evaluation
■ Malignancy
– Depending on the malignancy, a disease-free period of between 2 to 5 years is
generally accepted as adequate.
– All transplant candidates must undergo appropriate cancer screening prior to
transplantation.
■ If the cancerous lesion is less than 3 cm, the patient can proceed to transplantation. For
lesions greater than 3 cm, transplantation should be deferred for the requisite 2- 5 years
period to ensure remission prior to transplantation.
■ Urologic Disease
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 8 of 22
TRANSPLANTATION OPTIONS FOR
HIGHLY SENSITIZED INDIVIDUALS
■ Human Leukocyte antigen is performed in response to exposure to foreign HLA
molecules.
■ Options include:
– Paired- Donations Program
– Acceptable mismatch Programs
– Desensitization
** In order for optimal treatment to be offered to highly sensitized patients, all three in
combination probably provide the optimal solution.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 9 of 22
Liver Donor Kidney Donation
■ Patients with CKD need to make two important decisions:
– Whether to proceed with transplantation or dialysis as primary therapy
– Whether to proceed with living donation or to go on the waiting list for a deceased
donor transplant
■ Transplant results are significantly better for recipients who undergo transplant before
initiating dialysis or after a short course of dialysis versus recipients who undergo
transplant after a prolonged dialysis course.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 10 of 22
Kidney Transplantation
■ Regarding on choosing between living donation or deceased donor transplantation,
there is no doubt that a living donor transplant is the best option.
■ However, donation from living and deceased donor is almost identical.
■ Note that living unrelated transplant have the same olutcome as non identical living
related transplant.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 11 of 22
Donor Surgical Risk
■ Laparoscopic Donor Nephrectomy has been associated with less pain and a faster
recovery for the donor than conventional open nephrectomy.
– As a result, laparoscopic nephrectomy has become the procedure of choice at many
transplant centers.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 12 of 22
Donor Quality of Life
■ In general, Living donor report a similar or better quality of life.
■ Donors negative effects on recovery and future health:
– The amount of time to return to routine daily activities and commitment
– The financial consequences and implications
– The potential penalization by life or health insurance companies
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 13 of 22
Surgical Procedure
■ Procedures:
– Cadaveric Donor Nephrectomy (En Bloc Technique)
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 14 of 22
Pediatric Kidney Transplantation
■ Many children requiring renal transplantation will receive an adult organ.
■ This has of course an implications with regards to the size match of kidney to recipient
that is why it is necessary to place the kidney within the peritoneal cavity.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 15 of 22
DONATION AFTER CARDIAC DEATH
CADAVERIC DONORS
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 16 of 22
Complications
■ Bleeding and Thrombosis
■ Hemorrhage
■ Hematoma
■ Arterial Thrombosis and Renal Vein Thrombosis
■ Uteric Complications
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 17 of 22
Perioperative care and Early
Complications
■ Examination
– A full physical examination of patient should be performed including the
observation of fluid status, peripheral pulses and abdominal scars/hernias.
Examine also signs of infection.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 18 of 22
Perioperative Management
■ Dialysis
– Hemodialysis is indicated before transplantation if serum potassium is greater than
5.5 mmol/l or significantly having a fluid overload
■ Drug Therapy
– Antihypertensive Medications
■ This should all be reviewed during perioperative evaluation.
– Antiplatelt and Anticoagulation therapy
■ Aspirin therapy can be continued peri-operatively, as it has not been shown to increase
the risk of postoperative hemorrhage.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 19 of 22
Long Term Management and Outcomes
■ Advanced donor age is the strongest predictor of poor long –term graft survival.
■ Transplant glomerulopathy is an alloimmune-mediated lesion that is strongly linked to
an anti-human leukocyte antigen class II antibodies.
■ Proteinuria is common after renal transplantation and is an important marker of graft
injury.
■ Renal Transplant recipients are at 3 to 5 fold higher risk of cancer than the general
population.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 20 of 22
Long Term Management and Outcomes
■ Urinary Tract Infection is the most common infection in kidney transplant recipients
and usually occurs in the first year following transplantation.
■ Chronic allograft nephropathy remains the most common cause of chronic graft
dysfunction, where the mainstay if treatment is calcineurin inhibitor reduction or
withdrawal.
Klein, A. (2011). Organ Transplantation: A Clinical Guide.
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 21 of 22
**End of Kidney Transplantation**
https://cdn.fbsbx.com/v/t59.2708-21/61568067_472646476803337_6884395133068902400_n…ZkRes&_nc_ht=cdn.fbsbx.com&oh=a4cda20fe1b388129f8bdbe878292ddd&oe=5D1043C1&dl=1 23/06/2019, 02J28
Page 22 of 22
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Govt SchemesDocument144 pagesGovt SchemesGorakhnath MethreNo ratings yet
- EBM-Diagnosis & SkriningDocument37 pagesEBM-Diagnosis & SkriningIndah MaulidawatiNo ratings yet
- Rabia Ali Complete Errata, 4th Edition. by Fazli RashidDocument31 pagesRabia Ali Complete Errata, 4th Edition. by Fazli RashidAsma Saleem100% (1)
- Extra-Articular Phalangeal FracturesDocument65 pagesExtra-Articular Phalangeal FracturesProfesseur Christian Dumontier100% (2)
- 2009 ErskineDocument12 pages2009 ErskineAlina ComendantNo ratings yet
- Science Form 1 - Chapter 2.3 by KelvinDocument18 pagesScience Form 1 - Chapter 2.3 by KelvinKelvinNo ratings yet
- Nursing Informatics ImportanceDocument3 pagesNursing Informatics ImportanceDaniela Villanueva RosalNo ratings yet
- MM Comic by Ritualist Ddd4h4mDocument10 pagesMM Comic by Ritualist Ddd4h4mpablo donnerNo ratings yet
- Kika Prevod 3. Predmet I Celi Na IstrazuvanjetoDocument8 pagesKika Prevod 3. Predmet I Celi Na IstrazuvanjetoVlado NajdovNo ratings yet
- Rational Psychotherapy and Individual PsychologyDocument9 pagesRational Psychotherapy and Individual PsychologyDavidNo ratings yet
- Certificate in Geriatric Care Assistance DetailsDocument2 pagesCertificate in Geriatric Care Assistance DetailssuryakmrNo ratings yet
- Research Methods For Development: Week 2, Session 2 Dr. Hina KhalidDocument8 pagesResearch Methods For Development: Week 2, Session 2 Dr. Hina KhalidMarhaba RanaNo ratings yet
- Hepatic EncephalopathyDocument16 pagesHepatic Encephalopathyjh_ajjNo ratings yet
- The Drug Interaction Probability ScaleDocument2 pagesThe Drug Interaction Probability ScaleAta07No ratings yet
- Ultherapy System Instructions For UseDocument72 pagesUltherapy System Instructions For UseEmilija Minova100% (1)
- Roles Responsibility Matrix GC As Client PMC PDFDocument3 pagesRoles Responsibility Matrix GC As Client PMC PDFkavi_prakash6992100% (1)
- Complications of Labor & DeliveryDocument7 pagesComplications of Labor & DeliveryPatricia Anne Nicole CuaresmaNo ratings yet
- Effects of Vethathiri Maharishi - S Kaya Kalpa Technique and Simplified Physical Exercise Program - Aayvagam JournalDocument5 pagesEffects of Vethathiri Maharishi - S Kaya Kalpa Technique and Simplified Physical Exercise Program - Aayvagam Journalveera1491No ratings yet
- Intellectual Disability and Psychotic Disorders of Adult EpilepsyDocument0 pagesIntellectual Disability and Psychotic Disorders of Adult EpilepsyRevathi SelvapandianNo ratings yet
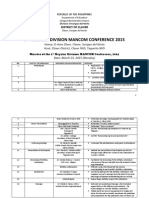
- Mancom MinutesDocument10 pagesMancom MinutesTetzie SumayloNo ratings yet
- Maintenance and Thorough Examination of Mobile CranesDocument106 pagesMaintenance and Thorough Examination of Mobile CranesKate Poole100% (2)
- CPA Burnout Berry Loranger Wong Final 101118Document80 pagesCPA Burnout Berry Loranger Wong Final 101118Sy LabthavikulNo ratings yet
- Weight Management Practices of Bachelor of Physical Education StudentsDocument32 pagesWeight Management Practices of Bachelor of Physical Education StudentsRalph Rexor Macarayan BantuganNo ratings yet
- Job Sharing - Behaviour in OrganisationDocument9 pagesJob Sharing - Behaviour in Organisationdecor17No ratings yet
- DSSQ PDFDocument12 pagesDSSQ PDFKiyo Korean StationaryNo ratings yet
- Specification Dried Oyster Mushrooms-2019Document2 pagesSpecification Dried Oyster Mushrooms-2019Manoj PatelNo ratings yet
- Periodic Test in Science 4 1st - 4thDocument17 pagesPeriodic Test in Science 4 1st - 4th엘라엘라No ratings yet
- The Antibacterial Efficacy of Tomato (Solanum Lycopersicum) Fruit Extract On Bacillus Cereus Using Varied Solvents For ExtractionDocument35 pagesThe Antibacterial Efficacy of Tomato (Solanum Lycopersicum) Fruit Extract On Bacillus Cereus Using Varied Solvents For ExtractionKoreen R.No ratings yet
- Pediatric Tracheostomy Decannulation: 11-Year ExperienceDocument8 pagesPediatric Tracheostomy Decannulation: 11-Year Experienceanitaabreu123No ratings yet
- Npiap 2019Document408 pagesNpiap 2019Militanisa ZamzaraNo ratings yet