Professional Documents
Culture Documents
Borderline Personality Disorder Diagnosis and 2017 The Journal For Nurse PR
Uploaded by
racm890 ratings0% found this document useful (0 votes)
47 views2 pagesyjyhk
Original Title
Borderline Personality Disorder Diagnosis and 2017 the Journal for Nurse Pr
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentyjyhk
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
47 views2 pagesBorderline Personality Disorder Diagnosis and 2017 The Journal For Nurse PR
Uploaded by
racm89yjyhk
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Borderline Personality
Disorder: Diagnosis and
Common Comorbidities
Patients in inpatient and outpatient settings DIAGNOSIS: HISTORY AND EXAM
who have a previous diagnosis of anxiety, Of those diagnosed with borderline personality
depression, or bipolar disorder may also have a disorder, 85% have one or more additional
coexisting diagnosis of borderline personality mental health disorders, including substance
disorder (BPD). This condition is character- abuse/addiction, eating disorders, somatoform
ized by mood swings, inappropriate anger, disorders, anxiety, depression, and bipolar dis-
instability in relationships and employment, order. When patients present with an estab-
fear of abandonment, and impulsive lished mental health disorder, comorbid BPD
decisions.1,2 should be considered.
While assessing the patient’s history, the
EPIDEMIOLOGY diagnosis may become apparent from 3 primary
BPD has a lifetime prevalence in up to 6% in criteria: (a) a history of failed relationships and a
the population, and is apparent in 20% of feeling of “emptiness”; (b) affective dysregula-
patients hospitalized due to mental health tion including excessive mood lability and fear
conditions. Women and men have similar of abandonment; and (c) behavioral dysregula-
incidence, with women seeking treatment tion, including impulsivity, suicidality, or other
more often than men. The frequency of self-injurious behaviors.1,3 A history of excessive
psychiatric comorbidities with BPD varies anger, mood lability, and avoidance of
between genders (see Table); the incidence of
BPD between ethnic groups is inconclusive.1,2
The onset of BPD occurs in late adolescence
or early adulthood with prodromal symptoms
often occurring even earlier. A final diagnosis,
DIAGNOSTIC
however, should be delayed until early TIPS
adulthood.1,3
PATHOPHYSIOLOGY Mellisa A. Hall, DNP, and
The cause of BPD is not clear, but there is Katherine M. Riedford, PhD
evidence of genetic susceptibility, as well as
neurobiologic dysfunction in the frontal abandonment (affective dysregulation) is the
lobe, altered neuropeptide function, and most sensitive screening for BPD. Extreme
neurotransmitter alterations.1 Studies link mood swings may occur several times a day over
dysfunctional environmental influences to the meaningless triggers. Euthymia may instantly
development of BPD, which may explain change to severe distress leading to outbursts
some of the aforementioned influences. against the patient’s closest contacts.1 Mood
Childhood trauma is associated with the instability is associated with feelings of guilt,
development of BPD, including sexual failure, and self-harm. Because there is often
trauma, severe physical and verbal abuse, lack of insight, contributions from family
witnessing domestic abuse, neglect, and members provide essential information to
abandonment.1,2 support the diagnosis.
www.npjournal.org The Journal for Nurse Practitioners - JNP e455
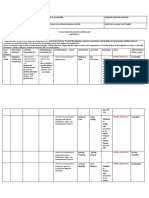
Table. Variance Between Genders of Borderline more of the following criteria should be met,
Personality Disorder With Comorbid Mental Health but patients often have all 9 of the DSM 5
Disorders diagnostic criteria: affective instability (95%);
Diagnosis Females Males inappropriate anger (87%); impulsivity (81%);
Depression No variance No variance
unstable relationships (79%); feelings of
emptiness (71%); paranoia or dissociation
Posttraumatic 51% 31%
stress disorder
(68%); identity disturbance (61%); abandon-
ment fears (60%); and suicidality or self-
Eating disorder 42% 19%
injury (60%).1,3
Identity disturbance 67% 48%
BPD shares clinical features with antisocial,
Substance use 58% 85% histrionic, narcissistic, paranoid, schizotypal, and
disorder
dependent personality disorders.3 Because BPD
Antisocial personality 10% 30% patients may share similar traits with these other
disorder
personality disorders, a mental health referral is
Narcissistic personality 5% 22% essential in confirming all diagnoses and
disorder
appropriate treatment recommendations.4
Schizotypal personality 10% 25%
disorder CONCLUSION
Alcohol use disorder No variance No variance Timely diagnosis is vital in identifying suicidal
Data from Ellison. 1
thoughts or plans. Approximately 10% of pa-
tients with BPD have committed suicide.1
Referral to a mental health specialist to confirm
The feeling of chronic emptiness has the the diagnosis of BPD is recommended, with
highest correlation with suicidality.1,3 follow-up therapy essential to improve
Assessment of early personal relationships may symptomatology.
help identify a pattern of dysfunctional
References
relationships, including instability in
1. Ellison WD, Rosenstein L, Chelminskil I, Dalrymple K, Zimmerman M.
employment. Active listening and keen skin The clinical significance of single features of borderline personality
inspection can identify previous nonsuicidal disorder; anger, affective instability, impulsivity, and chronic
emptiness in psychiatric outpatients. J Pers Disord. 2016;30:261-270.
self-injury such as cutting, burning, or injecting 2. US Department of Health and Human Services. Report to Congress on
Borderline Personality Disorder. HHS Publication No. SM 11-4644; 2012.
with needles. Suicidal risk increases during 3. American Psychiatric Association. Diagnostic and Statistical Manual of
periods of worsening depression, recent loss, and Mental Disorders. 5th ed. Arlington, VA: American Psychiatric
Association; 2013.
increased patterns of substance abuse.1,3 4. Zimmerman M, Multach MD, Dalrymple K, Chelminski I. Clinically
useful screen for borderline personality disorder criteria in psychiatric
outpatients. Br J Psychiatry. 2017;210:165-166.
DIAGNOSIS: DSM 5 and Screening Tools
The McLean Instrument for Borderline Per-
sonality disorder helps with initial diagnostic
Both authors are affiliated with the University of Southern
screening. The instrument has a sensitivity of Indiana. Mellisa A. Hall, DNP, is an associate professor, and
0.81 and a specificity of 0.85. Criteria for BPD, Column Editor for Diagnostic Tips. She can be reached at
mhall@usi.edu. Katherine M. Riedford, PhD, is an associate
as described in the Diagnostic and Statistical professor of nursing.
Manual of Mental Disorders (DSM 5), include an
ongoing pattern of instability in interpersonal
relationships, lower self-image, and impul- 1555-4155/17/$ see front matter
© 2017 Elsevier Inc. All rights reserved.
sivity, beginning in early adulthood. Five or http://dx.doi.org/10.1016/j.nurpra.2017.07.012
e456 The Journal for Nurse Practitioners - JNP Volume 13, Issue 9, October 2017
You might also like
- Borderline Personality Disorder (Lieb Et Al, 2004) PDFDocument10 pagesBorderline Personality Disorder (Lieb Et Al, 2004) PDFGokushimakNo ratings yet
- Borderline Personality DisorderDocument9 pagesBorderline Personality Disordernaila syawalita tsaniNo ratings yet
- BPD, DiagnosisDocument5 pagesBPD, DiagnosisMArkoNo ratings yet
- Cluster BDocument62 pagesCluster BAshish DootNo ratings yet
- Borderline Personality Disorder: Dialectical Behavior Therapy Workbook, Complete DBT Guide to Recovering from Borderline Personality DisorderFrom EverandBorderline Personality Disorder: Dialectical Behavior Therapy Workbook, Complete DBT Guide to Recovering from Borderline Personality DisorderNo ratings yet
- Borderline Personality Disorder and SuicidalityDocument17 pagesBorderline Personality Disorder and SuicidalityFranciscaFernandaRubioRamírezNo ratings yet
- Valencia (2015) Potential Biomarkers in Personality DisordersDocument15 pagesValencia (2015) Potential Biomarkers in Personality DisordersJulieht RodriguezNo ratings yet
- Bordeline Personality DisorderDocument6 pagesBordeline Personality DisorderWilliam Donato Rodriguez PacahualaNo ratings yet
- Crossmark: Psychiatry ResearchDocument6 pagesCrossmark: Psychiatry ResearchAndrei BăcanuNo ratings yet
- Borderline Personality Disorder Write Up 2Document8 pagesBorderline Personality Disorder Write Up 2Sreejita GhoshNo ratings yet
- Review Jurnal Bahasa InggrisDocument16 pagesReview Jurnal Bahasa InggrisDay EnNo ratings yet
- Why Learn A New Treatment?: Why Dialectical Behavior Therapy (DBT) ?Document22 pagesWhy Learn A New Treatment?: Why Dialectical Behavior Therapy (DBT) ?Doomimummo100% (2)
- Prescribing in Borderline Personality Disorder - The Clinical Guidelines - Yadav - 2020 - Progress in Neurology and Psychiatry - Wiley Online LibraryDocument17 pagesPrescribing in Borderline Personality Disorder - The Clinical Guidelines - Yadav - 2020 - Progress in Neurology and Psychiatry - Wiley Online Librarydo leeNo ratings yet
- Psychotic Disorders: Heidi Combs, MDDocument60 pagesPsychotic Disorders: Heidi Combs, MDmariaNo ratings yet
- Psychotic Symptoms As A Continuum Between Normality and PathologyDocument12 pagesPsychotic Symptoms As A Continuum Between Normality and PathologyOana OrosNo ratings yet
- Affective Instability and Suicidal Ideat20160629 23040 WFCGFH With Cover Page v2Document16 pagesAffective Instability and Suicidal Ideat20160629 23040 WFCGFH With Cover Page v2Clarice Almeida da SilvaNo ratings yet
- Bipolar Versus Borderline Difference Matter Acta PsychDocument2 pagesBipolar Versus Borderline Difference Matter Acta PsychSalud Mental SantiagoNo ratings yet
- DSM V Clinical Cases - Chapter 8 Dissociative DisordersDocument12 pagesDSM V Clinical Cases - Chapter 8 Dissociative DisordersIzzyinOzzieNo ratings yet
- Borderline Personality DisorderDocument6 pagesBorderline Personality DisorderPetrovecNo ratings yet
- Evidence-Basedcareofthe Patientwithborderline PersonalitydisorderDocument10 pagesEvidence-Basedcareofthe Patientwithborderline PersonalitydisorderMoonyNo ratings yet
- Careplan 1Document8 pagesCareplan 1api-509642710No ratings yet
- Evidence-Based Guideline: Assessment and Management of Psychiatric Disorders in Individuals With MSDocument9 pagesEvidence-Based Guideline: Assessment and Management of Psychiatric Disorders in Individuals With MSChon ChiNo ratings yet
- Assessment and Management of Late-Life DepressionDocument8 pagesAssessment and Management of Late-Life DepressionIzza Aliya KennedyNo ratings yet
- Borderline Vs BipolarDocument2 pagesBorderline Vs BipolarStefany GómezNo ratings yet
- Clinical Diagnosis For PD'SDocument5 pagesClinical Diagnosis For PD'SNgobYehsNo ratings yet
- Borderline Personality DisorderDocument128 pagesBorderline Personality Disorderعمر الحدادNo ratings yet
- Personality Disorders and Crime (Lecture Notes)Document8 pagesPersonality Disorders and Crime (Lecture Notes)Nadia MuhammadNo ratings yet
- Trastorno Depresivo en Edades TempranasDocument15 pagesTrastorno Depresivo en Edades TempranasManuel Dacio Castañeda CabelloNo ratings yet
- Scholarly Paper: DELUSION1: Dow University of Health Sciences Institute of Nursing (ION) BSN Generic (Semester VI)Document7 pagesScholarly Paper: DELUSION1: Dow University of Health Sciences Institute of Nursing (ION) BSN Generic (Semester VI)Ambreen ArshadNo ratings yet
- Geriatric Depression: The Use of Antidepressants in The ElderlyDocument7 pagesGeriatric Depression: The Use of Antidepressants in The ElderlyBilly D. Justia WahidNo ratings yet
- Personality DisordersDocument16 pagesPersonality Disorderssomebody_ma100% (1)
- Borderline Personality Disorder Implications in Family and Pediatric Practice 2161 0487.1000122Document6 pagesBorderline Personality Disorder Implications in Family and Pediatric Practice 2161 0487.1000122Farida DurotulNo ratings yet
- Borderline Personality Disorder Implications in Family and Pediatric Practice 2161 0487.1000122 PDFDocument6 pagesBorderline Personality Disorder Implications in Family and Pediatric Practice 2161 0487.1000122 PDFFarida Durotul100% (1)
- Borderline Personality DisorderDocument7 pagesBorderline Personality DisorderRobert Sebastian ConstantinescuNo ratings yet
- Histrionic Personality Disorder JhonyDocument17 pagesHistrionic Personality Disorder Jhonyjhony c. benedictaNo ratings yet
- Personality DisorderDocument33 pagesPersonality DisorderIulia Moldovan100% (1)
- BPD Literature ReviewDocument19 pagesBPD Literature ReviewMary Winston DozierNo ratings yet
- Personality DisordersDocument21 pagesPersonality DisordersRumaNo ratings yet
- Abnormal PersonalityDisordersDocument13 pagesAbnormal PersonalityDisorderscurtisbogettiNo ratings yet
- Psychotherapy and Pharmacotherapy For DIDDocument8 pagesPsychotherapy and Pharmacotherapy For DIDAnh NguyênNo ratings yet
- Personality Disorders: General SymptomsDocument6 pagesPersonality Disorders: General Symptomsiqra kanwalNo ratings yet
- Outline Chapter 5!Document5 pagesOutline Chapter 5!razbythewayNo ratings yet
- Suicidal Thought or Behavior in BPD Literature ReviewDocument9 pagesSuicidal Thought or Behavior in BPD Literature ReviewzianaNo ratings yet
- Borderline Personality Disorder in Late Life - A Medication Adherence VariableDocument7 pagesBorderline Personality Disorder in Late Life - A Medication Adherence VariableResidentes PsiquiatríaNo ratings yet
- Wellways Fact Sheet BPDDocument4 pagesWellways Fact Sheet BPDJonty ArputhemNo ratings yet
- Paranoid Personality DisorderDocument3 pagesParanoid Personality Disorderayan_edrianNo ratings yet
- Jamapsychiatry Hasin 2018 Oi 170112Document11 pagesJamapsychiatry Hasin 2018 Oi 170112Willy SvdNo ratings yet
- BPD Case StudyDocument6 pagesBPD Case StudySabina İsmayılovaNo ratings yet
- The Frustrating NoDocument11 pagesThe Frustrating NoLu LarNo ratings yet
- Emerson Fletcher - Psych Case Study - Final 2Document14 pagesEmerson Fletcher - Psych Case Study - Final 2api-660321588No ratings yet
- Outline and Evaluate The Classification and Diagnosis of SchizophreniaDocument1 pageOutline and Evaluate The Classification and Diagnosis of SchizophreniasophiabalkizovaNo ratings yet
- CLC - Research Paper 1Document13 pagesCLC - Research Paper 1api-549337583No ratings yet
- SchizophreniaDocument46 pagesSchizophreniaEmilyne Joy Mendoza CabayaNo ratings yet
- LiteraturereviewDocument5 pagesLiteraturereviewkristinaNo ratings yet
- Ijrtsat 11 2 6Document7 pagesIjrtsat 11 2 6amritaNo ratings yet
- Borderline Personality Disorder: Presented By: Nurul Syazwani Binti Ramli 080100315 K5Document11 pagesBorderline Personality Disorder: Presented By: Nurul Syazwani Binti Ramli 080100315 K5Nurul Syazwani Ramli100% (1)
- Personality DisordersDocument34 pagesPersonality DisordersKelvin kipkuruiNo ratings yet
- Schizoaffective Disorder - Emedicine SourceDocument25 pagesSchizoaffective Disorder - Emedicine SourcenarseeNo ratings yet
- SchizophreniaDocument14 pagesSchizophreniaBEA RADANo ratings yet
- Personality Disorder and Management Block 2.4: Carla R MarchiraDocument38 pagesPersonality Disorder and Management Block 2.4: Carla R MarchiraadystiNo ratings yet
- TLP Wpa 2024Document22 pagesTLP Wpa 2024Juan ParedesNo ratings yet
- Emotions and Thoughts Move So Quickly That It Can Be Hard ToDocument6 pagesEmotions and Thoughts Move So Quickly That It Can Be Hard Toracm89No ratings yet
- Garca-Escaleraetal 2017 StudyprotocolUP-ADocument19 pagesGarca-Escaleraetal 2017 StudyprotocolUP-Aracm89No ratings yet
- Is A Nervous System Necessary For Learning?: Perspectives On Behavior Science (2018) 41:343 - 368Document26 pagesIs A Nervous System Necessary For Learning?: Perspectives On Behavior Science (2018) 41:343 - 368MiguelNo ratings yet
- The Neural Correlates of Trauma Related Autobiographical Memory in Posttraumatic Stress Disorder: A Meta AnalysisDocument25 pagesThe Neural Correlates of Trauma Related Autobiographical Memory in Posttraumatic Stress Disorder: A Meta Analysisracm89No ratings yet
- Yeti Manual - EnglishDocument20 pagesYeti Manual - Englishracm89No ratings yet
- Bush Francis Scale With A Few References 4 18 19Document4 pagesBush Francis Scale With A Few References 4 18 19USM San IgnacioNo ratings yet
- Safety of Psychotropic Medications in People With COVID-19: Evidence Review and Practical RecommendationsDocument14 pagesSafety of Psychotropic Medications in People With COVID-19: Evidence Review and Practical Recommendationsracm89No ratings yet
- Davison 39 S 20 Articles 200320 BM20 Psychology 20 ShouldDocument14 pagesDavison 39 S 20 Articles 200320 BM20 Psychology 20 Shouldracm89No ratings yet
- 10.1016/j.cbpra.2017.06.002: Cognitive and Behavioral PracticeDocument37 pages10.1016/j.cbpra.2017.06.002: Cognitive and Behavioral Practiceracm89No ratings yet
- Predicting Engagement in Psychotherapy, Pharmacotherapy, or Both Psychotherapy and Pharmacotherapy Among Returning Veterans Seeking PTSD TreatmentDocument8 pagesPredicting Engagement in Psychotherapy, Pharmacotherapy, or Both Psychotherapy and Pharmacotherapy Among Returning Veterans Seeking PTSD Treatmentracm89No ratings yet
- Acceptance and Commitment Therapy For Individuals With DisabilitiesDocument11 pagesAcceptance and Commitment Therapy For Individuals With Disabilitiesjoao1504No ratings yet
- The Phenomenology of Between: An Intersubjective Epistemology For Psychological ScienceDocument29 pagesThe Phenomenology of Between: An Intersubjective Epistemology For Psychological Scienceracm89No ratings yet
- E024104 FullDocument14 pagesE024104 Fullracm89No ratings yet
- Uso de Sustancias y EsquizofreniaDocument10 pagesUso de Sustancias y Esquizofreniaracm89No ratings yet
- Using Behavioural Science To Help Fight The Coronavirus: Working Paper No. 656 March 2020Document25 pagesUsing Behavioural Science To Help Fight The Coronavirus: Working Paper No. 656 March 2020racm89No ratings yet
- WheelofAwareness Guided Meditation PDFDocument3 pagesWheelofAwareness Guided Meditation PDFgustavogknNo ratings yet
- Social Support and The Outcome of Major Depression.: References ReprintsDocument9 pagesSocial Support and The Outcome of Major Depression.: References Reprintsracm89No ratings yet
- Prolonged Exposure and Sertraline Treatments For Posttraumatic Stress Disorder Also Improve Multiple Indicators of Social FunctioningDocument12 pagesProlonged Exposure and Sertraline Treatments For Posttraumatic Stress Disorder Also Improve Multiple Indicators of Social Functioningracm89No ratings yet
- FACE COVID - How To Respond Effectively To The Corona Crisis - by Russ HarrisDocument6 pagesFACE COVID - How To Respond Effectively To The Corona Crisis - by Russ HarrisJuan Alberto GonzálezNo ratings yet
- BJMP 2016 9 1 A909 PDFDocument7 pagesBJMP 2016 9 1 A909 PDFracm89No ratings yet
- (Lauren Slater) Opening Skinner's Box Great PsyDocument262 pages(Lauren Slater) Opening Skinner's Box Great Psystragusrj100% (3)
- Do The WorkDocument57 pagesDo The WorknikNo ratings yet
- Guias NICE DMDocument64 pagesGuias NICE DMracm89No ratings yet
- Canmat 2013Document44 pagesCanmat 2013Lucas GmrNo ratings yet
- PIIS221503661930416XDocument14 pagesPIIS221503661930416Xracm89No ratings yet
- BJMP 2016 9 1 A909 PDFDocument7 pagesBJMP 2016 9 1 A909 PDFracm89No ratings yet
- Starcevic 2017Document5 pagesStarcevic 2017racm89No ratings yet
- S. Faubel and J. Topf 4 Volume RegulationDocument24 pagesS. Faubel and J. Topf 4 Volume RegulationJoel TopfNo ratings yet
- What's Next A Clinical OverviewDocument6 pagesWhat's Next A Clinical Overviewracm89No ratings yet
- 25th European Congress of Psychiatry / European Psychiatry 41S (2017) S405-S464 S407Document1 page25th European Congress of Psychiatry / European Psychiatry 41S (2017) S405-S464 S407miyaeeeeeNo ratings yet
- Instructional PlanDocument6 pagesInstructional PlanShaina Mae ParicoNo ratings yet
- Ies RDocument3 pagesIes RIvana OzzNo ratings yet
- Emotional IntelligenceDocument9 pagesEmotional Intelligencedhrona g100% (1)
- Competency Based HRMDocument33 pagesCompetency Based HRMDino DinoNo ratings yet
- Lab RubricsDocument2 pagesLab RubricsHasnain KhanNo ratings yet
- Friends Can Be of The Same or Different AgeDocument1 pageFriends Can Be of The Same or Different AgeDaisy Ann Cariaga SaccuanNo ratings yet
- QMS Assignment 4Document2 pagesQMS Assignment 4John Michael PadillaNo ratings yet
- Annotation TemplateDocument7 pagesAnnotation TemplateMargiebel Daano100% (1)
- 4as and IPP Format Lesson PlanDocument10 pages4as and IPP Format Lesson PlanMarry Ann MendozaNo ratings yet
- Theory of Mind and Selective Attention, Response Inhibition, CognitiveDocument7 pagesTheory of Mind and Selective Attention, Response Inhibition, CognitiveSilvanilla PiliNo ratings yet
- Tutorial Letter 101/0/2021: Child Development (0-9)Document33 pagesTutorial Letter 101/0/2021: Child Development (0-9)Simoné NelsonNo ratings yet
- Psychological Resilience in Sport Performers - A Review of Stressors and Protective Factors - Fletcher-SarkarDocument17 pagesPsychological Resilience in Sport Performers - A Review of Stressors and Protective Factors - Fletcher-SarkarJavier BardemNo ratings yet
- Assessing Emotional IntelligenceDocument16 pagesAssessing Emotional IntelligenceabayabayaNo ratings yet
- PT 1Document2 pagesPT 1Pedimor Dolor CabansagNo ratings yet
- Aids To Effective Teaching-Sir Sagge Maam BustamanteDocument12 pagesAids To Effective Teaching-Sir Sagge Maam BustamanteMC Lopez Aguilar100% (2)
- Behavioural Interview PDFDocument33 pagesBehavioural Interview PDFDeepthi VasanthakumarNo ratings yet
- Assessment of Poor Learning Strategies and Their Effects On Academic Performance of Senior Secondary School Students in Sokoto StateDocument6 pagesAssessment of Poor Learning Strategies and Their Effects On Academic Performance of Senior Secondary School Students in Sokoto StateIjahss JournalNo ratings yet
- Professionalism and Career Networking: Authors: Susan S. Stratton Dorothy I. MitstiferDocument13 pagesProfessionalism and Career Networking: Authors: Susan S. Stratton Dorothy I. Mitstiferwicak_spNo ratings yet
- The Learners Demonstrate An Understanding of The Learners Shall Be Able To Learners Are Expected ToDocument6 pagesThe Learners Demonstrate An Understanding of The Learners Shall Be Able To Learners Are Expected ToMartie AvancenaNo ratings yet
- CLILDocument14 pagesCLILabuclauNo ratings yet
- A Pilot Study Examining The Test-Retest and Internal Consistency Reliability of The Ablls-RDocument6 pagesA Pilot Study Examining The Test-Retest and Internal Consistency Reliability of The Ablls-RSimona TintaNo ratings yet
- Ocd Research PaperDocument13 pagesOcd Research Paperapi-582440798No ratings yet
- Reflection Piece HL 440Document2 pagesReflection Piece HL 440api-252456939No ratings yet
- Open Book Examinations The Need of The HDocument13 pagesOpen Book Examinations The Need of The Hasurana29459No ratings yet
- 4 Instructional MethodsDocument23 pages4 Instructional MethodsNhial AbednegoNo ratings yet
- Coaching For Behavioral ChangeDocument5 pagesCoaching For Behavioral ChangeMoroxo ParraNo ratings yet
- DSM 5 - DSM 5Document7 pagesDSM 5 - DSM 5Roxana ClsNo ratings yet
- Chapter 4 - Work-Related AttitudesDocument12 pagesChapter 4 - Work-Related AttitudesSteffany RoqueNo ratings yet
- Differentiation For Groups of StudentsDocument11 pagesDifferentiation For Groups of Studentsapi-421042053No ratings yet