Professional Documents
Culture Documents
Calcified Pseudoneoplasm of The Neuraxis Capnon A Lesson Learnt From A Rare Entity PDF
Uploaded by
Kisspetre PetreOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Calcified Pseudoneoplasm of The Neuraxis Capnon A Lesson Learnt From A Rare Entity PDF
Uploaded by
Kisspetre PetreCopyright:
Available Formats
Case Report
iMedPub Journals JOURNAL OF NEUROLOGY AND NEUROSCIENCE 2016
http://www.imedpub.com/ Vol.7 No.3:121
ISSN 2171-6625
DOI: 10.21767/2171-6625.1000121
Calcified Pseudoneoplasm of the Neuraxis (CAPNON): A Lesson Learnt from a
Rare Entity
Merola J, Jain A, Ziad F and Hussain Z
Neurosurgery Department, Waikato Hospital, Hamilton, New Zealand
Corresponding author: Dr. Joseph Merola, Neurosurgery Department, Waikato Hospital, Hamilton, New Zealand, 3210, Tel: 02920814000; E-
mail: merola.joe@gmail.com;merolaj@doctors.org.uk
Received: May 27, 2016; Accepted: Jun 21, 2016; Published: Jun 24, 2016
Abstract
We present the case of a 39-year-old female with an
exceptional rare entity of the neural axis located in the
perisylvian region. We discuss the unique features and the
subsequent management of this interesting case.
Keywords: Calcified pseudoneoplasm of the neuraxis;
CAPNON; Oedema; Brain stone
Case Report
A 39-year-old, right hand dominant, female presented with
tingling sensation in her right arm followed by a first-time, self-
terminating generalized tonic-clonic seizure. There was no
previous medical history and no regular medications. Detailed
neurological examination was unremarkable and there were
no signs elicited from cardiorespiratory or abdominal
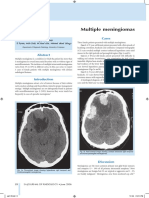
examination. Computed tomography (CT) of the brain revealed
a hyper dense calcified mass in the left perisylvian region
(Figure 1). Magnetic Resonance Imaging (MRI) showed Figure 1 CT Axial (A) and coronal (B) views showing
hypointense signal on T1 and T2-weighted images in the region hyperdense lesion in perisylvian region with extensive
of calcification as seen on CT. Extensive vasogenic oedema was surrounding vasogenic oedema within the frontal, parietal
also noted in adjacent lobes and extended into the external and temporal lobes. Indicated by yellow arrow in (A) C & D
capsule and lentiform nucleus. Prominent vessels were seen show MRI T1 weighted imaging. A lobular lesion involving
surrounding the lesion but no vascular anomaly was noted on the cortex and subcortical white matter of the superior left
Magnetic Resonance Angiography (MRA). A Digital Subtraction temporal lobe, posterior aspect of the left insular cortex,
Angiogram (DSA) ruled out aneurysm or arterio-venous posterior left frontal lobe and anterior left parietal lobe. On
malformation (AVM). The differential diagnosis remained low- T1 (and T2 not seen here) this lesion demonstrates hypo-
grade astrocytoma versus oligodendroglioma. intense signal corresponding with the calcification seen on
Following multidisciplinary discussion surgical intervention CT. Thin rim of enhancement was seen following contrast
was recommended. The patient underwent a left fronto- administration. Vasogenic oedema extended into the
temporal craniotomy and gross total resection of the calcified adjacent frontal, parietal and temporal lobes and also
mass. The sylvian fissure was noted to be wide open and involved the left external capsule and lentiform nucleus.
surrounded by prominent vessels. The calcified mass was
removed in three pieces and abnormal looking surrounding Post-operatively the patient was noted to be significantly
brain was biopsied; it had a rubbery consistency with grey- weak in the right upper and lower limbs. MRI confirmed
yellow appearance. restricted diffusion in the parietal lobe. Histological diagnosis
confirmed a calcified pseudoneoplasm of the neural axis
(Figure 2).
© Copyright iMedPub | This article is available from: http://www.jneuro.com/
1
JOURNAL OF NEUROLOGY AND NEUROSCIENCE 2016
ISSN 2171-6625 Vol.7 No.3:121
Figure 2 surgical specimens as seen macroscopically (A) and under the microscope (B-E). A – macroscopic specimens showing
three pieces with the largest measuring 25 mm. B – low power view C- High power view; Rosenthal fibres; D-F basophilic
nodules, peripheral rim of radially arranged cells.
At one month follow up the patient remained densely Rodriguez et al. support this theory in their description of an
monoplegic in the right upper limb but now able to move anti- unusual case of co-existing CAPNON and a low-grade
gravity in the right lower limb. She remained on anti-seizure cerebellar ependymoma associated with marked piloid gliosis
medication and continued intensive Neuro-rehabilitation. on histology. The authors conclude that CAPNON is a result of
tumefactive reaction rather than metaplasia [3]. The
Discussion histological descriptions from our case are typical of those for
CAPNON and are shown in Figure 2.
Calcified pseudoneoplasm of the neuraxis (CAPNON) is a There is widespread acceptance that while surgical resection
rare entity and is considered benign. Review of previous may provide symptom relief, histological diagnosis and
reports suggests similar incidence in both sexes occurring in prevention of recurrence, it does not come without risk. In our
different locations intra-and extra-axially [1]. To our knowledge case there was significant postoperative right upper limb
none have previously been reported in the perisylvian region. weakness as a result of infarction-postoperative MRI
Presentation varies depending on location but can involve, as demonstrates an area of restricted diffusion extending
seen in this case, sensorimotor deficit or seizures [2]. postero-laterally from the surgical resection site to the left
CAPNON is typically mistaken for more common neoplastic posterior parietal lobe.
or non-neoplastic lesions and CT/MRI helps to distinguish
between the different types. On CT, CAPNON is classically Conclusion
hyper dense given the calcification while on MRI imaging
lesions tend to show hypo-intense signal on T1 and T2 CAPNON must be considered in the differential diagnosis of
weighted sequences [1]. Surrounding vasogenic oedema is not calcified lesions in the brain. The decision to proceed with
commonly reported and would not typically be expected from surgical intervention must be influenced by the clinical
a benign lesion. Grabowski et al. reported vasogenic oedema presentation. The type of approach (e.g. biopsy versus total
in their case report and suggest seizures as the possible cause resection) should be discussed at a multidisciplinary level to
[2]. Similarly our patient presented with seizures although the mitigate the inherent risks of surgical intervention.
cerebral oedema was more extensive.
Histologically CAPNON contains variable portions of fibrous Conflicts of Interest
stroma, bone, palisading spindle and epithelioid cells and a
chondromyxoid-like matrix [1]. The etiology and natural history None declared
of CAPNON is unclear and thought to result from a reactive
process. This is suggested by associated granulomatous
inflammation typically surrounding the calcified mass [3].
2 This article is available from: http://www.jneuro.com/
JOURNAL OF NEUROLOGY AND NEUROSCIENCE 2016
ISSN 2171-6625 Vol.7 No.3:121
References callosum: A case report and review of the literature Clinical
Neuropathology 32: 515-521.
1. Aiken AH, Akgun H, Tihan T, Barbaro N, Glastonbury C (2009) 3. Rodriguez FJ, Scheithauer BW, Fourney DR, Robinson CA (2008)
Calcifying pseudoneoplasms of the neuraxis: CT, MR Imaging Ependymoma and intraparenchymal calcifying pseudoneoplasm
and Histologic features AJNR 30: 1256-1260. of the neural axis: Incidental collision or unique reactive
2. Grabowski M, Recinos P, Chen T, Prayson R, Vogelbaum M (2013) phenomenon? Acta Neuropathol 115: 363-366.
Calcifying pseudoneoplasm of the neuraxis overlying the corpus
© Copyright iMedPub 3
You might also like
- 5 5 5 Pontine Atypical Neurocytoma Case Report 副本Document8 pages5 5 5 Pontine Atypical Neurocytoma Case Report 副本singhNo ratings yet
- Magnetic Resonance Spectroscopy A Noninvasive Diagno - 2006 - Magnetic ResonancDocument3 pagesMagnetic Resonance Spectroscopy A Noninvasive Diagno - 2006 - Magnetic Resonanctejas1578No ratings yet
- Hemangioma of The Cavernous Sinus: A Case SeriesDocument5 pagesHemangioma of The Cavernous Sinus: A Case SerieshamdanNo ratings yet
- Challenging Neurological Manifestations in Large Cell Neuroendocrine Carcinoma Lcnec A Case Study of Extensive Intracranial and Intradural MetastasesDocument3 pagesChallenging Neurological Manifestations in Large Cell Neuroendocrine Carcinoma Lcnec A Case Study of Extensive Intracranial and Intradural MetastasesHerald Scholarly Open AccessNo ratings yet
- Cordom Clivus Case Report Plus Review 2017Document6 pagesCordom Clivus Case Report Plus Review 2017Ionela DumitriuNo ratings yet
- Unusual Brain StoneDocument5 pagesUnusual Brain StonekucingNo ratings yet
- Hon 2005Document2 pagesHon 2005Andana TrisaviNo ratings yet
- 1009 Case 2Document4 pages1009 Case 2willygopeNo ratings yet
- A Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientDocument3 pagesA Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- Combined Treatment of Surgery and Sclerotherapy For Sinus PericraniiDocument5 pagesCombined Treatment of Surgery and Sclerotherapy For Sinus Pericranii相壮壮No ratings yet
- Recurrent Intracranial Neurenteric Cyst With Malignant Transformation: A Case Report and Literature ReviewDocument8 pagesRecurrent Intracranial Neurenteric Cyst With Malignant Transformation: A Case Report and Literature ReviewWildaHanimNo ratings yet
- Subtemporal approach to large cranial base tumorsDocument12 pagesSubtemporal approach to large cranial base tumorsRamses OrtizNo ratings yet
- Lawrence Et Al 2021 Contralateral Transmaxillary Approach For Resection of Chondrosarcoma of The Petrous Apex A CaseDocument4 pagesLawrence Et Al 2021 Contralateral Transmaxillary Approach For Resection of Chondrosarcoma of The Petrous Apex A CaseSourabh PatroNo ratings yet
- Cerebral Edema Associated With MeningiomaDocument3 pagesCerebral Edema Associated With MeningiomaEstefania Ramirez CardonaNo ratings yet
- AsianJNeurosurg102126-4310714 115827 PDFDocument3 pagesAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNo ratings yet
- Syndromes of The Orbital Fissure, Cavernous Sinus, Cerebello-Pontine Angle, and Skull BaseDocument10 pagesSyndromes of The Orbital Fissure, Cavernous Sinus, Cerebello-Pontine Angle, and Skull BaseMarlene Arbeu ReyesNo ratings yet
- Gliomatose CerebriDocument6 pagesGliomatose CerebrijoaquinNo ratings yet
- 1208 Case 1Document2 pages1208 Case 1willygopeNo ratings yet
- Late Recurrence of A Brain Tumor: Michael N. Needle,, Lucy B. Rorke,, and Peter WinklerDocument5 pagesLate Recurrence of A Brain Tumor: Michael N. Needle,, Lucy B. Rorke,, and Peter WinklerantonioopNo ratings yet
- 2019 - Chung Et Al-AnnotatedDocument6 pages2019 - Chung Et Al-AnnotatedCemal GürselNo ratings yet
- Herniation of Uncus and Parahippocampal Gyrus: An Accidental Finding On Magnetic Resonance Imaging of CerebrumDocument3 pagesHerniation of Uncus and Parahippocampal Gyrus: An Accidental Finding On Magnetic Resonance Imaging of CerebrumDanaAmaranducaiNo ratings yet
- Bulbo-Medullary Ependymoma in An Adult: Case ReportDocument6 pagesBulbo-Medullary Ependymoma in An Adult: Case ReportIJAR JOURNALNo ratings yet
- Abducens Nerve Palsy as Initial Symptom of Trigeminal SchwannomaDocument8 pagesAbducens Nerve Palsy as Initial Symptom of Trigeminal SchwannomaLinius CruzNo ratings yet
- Original Research Paper: Schwannomatosis: A Case Report and Literature ReviewDocument4 pagesOriginal Research Paper: Schwannomatosis: A Case Report and Literature ReviewEarthjournal PublisherNo ratings yet
- Para Lab Case Study 2Document6 pagesPara Lab Case Study 2jmezzmdc.mdNo ratings yet
- Atypical Atlanto Axial Subluxation - Yjocn - 4Document1 pageAtypical Atlanto Axial Subluxation - Yjocn - 4KaitlynHynes34No ratings yet
- 0209 Case 2Document4 pages0209 Case 2willygopeNo ratings yet
- Surgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year SurvivalDocument5 pagesSurgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year Survivallucasnegromonte0001No ratings yet
- Exemplu 8Document4 pagesExemplu 8Pavel SebastianNo ratings yet
- ParasiteDocument7 pagesParasiteJOAN REPOLLONo ratings yet
- Scapulothoracic Dissociation 2165 7548.1000142Document2 pagesScapulothoracic Dissociation 2165 7548.1000142Fadlu ManafNo ratings yet
- Imaging in Brain TumorDocument142 pagesImaging in Brain TumorMagrinov AzaniaNo ratings yet
- 2008 TWPRMLinDocument8 pages2008 TWPRMLinVictor_id077No ratings yet
- E110 FullDocument2 pagesE110 FullLuther ThengNo ratings yet
- Post-Craniotomy Blindness in The Supine Position UDocument6 pagesPost-Craniotomy Blindness in The Supine Position UZezo AbdullahNo ratings yet
- Orbital Metastasis of A Pediatric Nasopharyngeal Carcinoma A Rare Case ReportDocument4 pagesOrbital Metastasis of A Pediatric Nasopharyngeal Carcinoma A Rare Case ReportInternational Journal of Innovative Science and Research Technology100% (1)
- 1 Neurosurgery Cases and ReviewsDocument5 pages1 Neurosurgery Cases and ReviewsintodoieblissNo ratings yet
- Lumbar epidural hematoma case reportDocument2 pagesLumbar epidural hematoma case reportrswongym449No ratings yet
- Brainstem CysticercoseDocument4 pagesBrainstem CysticercoseDr. R. SANKAR CITNo ratings yet
- Exercise-Associated Numbness and Tingling in The Legs: For Editorial Comment See Page 1509Document4 pagesExercise-Associated Numbness and Tingling in The Legs: For Editorial Comment See Page 1509herpthederpNo ratings yet
- Ochalski 2010Document5 pagesOchalski 2010Felipe RohamNo ratings yet
- Rare Axillary Nerve Schwannoma Case ReportDocument3 pagesRare Axillary Nerve Schwannoma Case ReportMani MaranNo ratings yet
- Millar J Choksey M Case of the Month Size_is_not_importantDocument2 pagesMillar J Choksey M Case of the Month Size_is_not_importantmunchisolichokseyNo ratings yet
- Syringomyelia and Arachnoid Cysts Associated With Spinal Arachnoiditis Following Subarachnoid HemorrhageDocument5 pagesSyringomyelia and Arachnoid Cysts Associated With Spinal Arachnoiditis Following Subarachnoid Hemorrhagekomputer12No ratings yet
- Chordoma of The Corpus Callosum: Case Report: Literature SearchDocument7 pagesChordoma of The Corpus Callosum: Case Report: Literature SearchAleksandar DimovskiNo ratings yet
- SSP 1Document5 pagesSSP 1YanNo ratings yet
- Surgical Treatment For Metastatic Brain Tumor in TDocument5 pagesSurgical Treatment For Metastatic Brain Tumor in Tsneha.921530sharmaNo ratings yet
- Intracranial Epidermoid CystDocument3 pagesIntracranial Epidermoid CystWildaHanimNo ratings yet
- 0909 Case 2Document2 pages0909 Case 2willygopeNo ratings yet
- A Case of Malignant Pleural Mesothelioma With Metastasis To The OrbitDocument3 pagesA Case of Malignant Pleural Mesothelioma With Metastasis To The OrbitjamesyuNo ratings yet
- Mature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportDocument5 pagesMature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportHaribabuBabuNo ratings yet
- Multiple MeningiomasDocument3 pagesMultiple Meningiomasarun gowdaNo ratings yet
- PROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDDocument9 pagesPROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDfriiday.qNo ratings yet
- 0709 Case 2Document4 pages0709 Case 2willygopeNo ratings yet
- White Cord Syndrome After Cervical DecompressionDocument7 pagesWhite Cord Syndrome After Cervical DecompressionJosé A. RodríguezNo ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- InvestigationsDocument28 pagesInvestigationsAndrei BulgariuNo ratings yet
- Diagnostic Difficulties in Fibrous Dysplasia - A 5-Case Series and A Literature ReviewDocument9 pagesDiagnostic Difficulties in Fibrous Dysplasia - A 5-Case Series and A Literature Reviewsolikin ikinNo ratings yet
- Medi 101 E28665Document5 pagesMedi 101 E28665S Francisco MotNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Owner's Manual Highlights Key Safety InfoDocument35 pagesOwner's Manual Highlights Key Safety InfoKisspetre PetreNo ratings yet
- Owner's Manual Highlights Key Safety InfoDocument35 pagesOwner's Manual Highlights Key Safety InfoKisspetre PetreNo ratings yet
- Owner's Manual Highlights Key Safety InfoDocument35 pagesOwner's Manual Highlights Key Safety InfoKisspetre PetreNo ratings yet
- CAPNONDocument4 pagesCAPNONKisspetre PetreNo ratings yet
- Ent ModuleDocument14 pagesEnt ModuleVishnu KrshNo ratings yet
- Family Violence Legal Medical and Social Perspectives 7th Wallace Test BankDocument10 pagesFamily Violence Legal Medical and Social Perspectives 7th Wallace Test BankTravis Bogan100% (35)
- Salvestrols Cures CancerDocument29 pagesSalvestrols Cures CancerJohn Tan100% (1)
- Unit 7Document3 pagesUnit 7ALIFIANo ratings yet
- Celiac Disease by DR Mohamed EbraheemDocument12 pagesCeliac Disease by DR Mohamed EbraheemFercho MedNo ratings yet
- BC USMLE Step 2 Pediatrics - KaDocument4 pagesBC USMLE Step 2 Pediatrics - KaMoonaLoveeNo ratings yet
- BHERTDocument2 pagesBHERTLei SomodioNo ratings yet
- S101 General Paper April/May, 2023: HoursDocument4 pagesS101 General Paper April/May, 2023: HoursJoseph RanksNo ratings yet
- Report Text About Covid 19Document4 pagesReport Text About Covid 19Yanti Sinaga100% (2)
- Safety Doesn't Happen by AccidentDocument77 pagesSafety Doesn't Happen by AccidentmaivieNo ratings yet
- Disease Study: A. Myasthenia GravisDocument6 pagesDisease Study: A. Myasthenia GravisMark Lemuel AbadaNo ratings yet
- Effect of Wound Care Using Robusta Coffee Powders On Diabetic Ulcer Healing in Sekarwangi Hospital SukabumiDocument10 pagesEffect of Wound Care Using Robusta Coffee Powders On Diabetic Ulcer Healing in Sekarwangi Hospital SukabumiBonita SiraitNo ratings yet
- Physiological JaundiceDocument11 pagesPhysiological Jaundiceapi-3859062No ratings yet
- Hopelessness NCPDocument5 pagesHopelessness NCPMatty JolbitadoNo ratings yet
- LITERATURE REVIEW ON ENDOSCOPY EXAMINATIONDocument29 pagesLITERATURE REVIEW ON ENDOSCOPY EXAMINATIONShenaquitaIvandraNo ratings yet
- Psychiatric Morbidity in Cancer Patients: Original ResearchDocument8 pagesPsychiatric Morbidity in Cancer Patients: Original ResearchGautami ThirumalaisamyNo ratings yet
- Jadwal Pit (Fetomaternal Room)Document3 pagesJadwal Pit (Fetomaternal Room)Dwi Adi NugrohoNo ratings yet
- Quiz 3Document2 pagesQuiz 3Abdalrahman AhmedNo ratings yet
- H 12 PlmpilukDocument7 pagesH 12 PlmpilukSofiNo ratings yet
- CBC and Widal Test ReportDocument4 pagesCBC and Widal Test ReportNeeraj KumarNo ratings yet
- Diagnosis and Treatment of Gestational Trophoblastic Disease PDFDocument11 pagesDiagnosis and Treatment of Gestational Trophoblastic Disease PDFAlexeySAgNo ratings yet
- Farmakoterapi Pada SepsisDocument36 pagesFarmakoterapi Pada SepsisNathaniaNo ratings yet
- Power Git EndoDocument170 pagesPower Git Endoapi-3735995100% (1)
- Psychogenic VertigoDocument5 pagesPsychogenic VertigoVirza Chairunnisa LatuconsinaNo ratings yet
- PEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827Document197 pagesPEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827adhytiyani putriNo ratings yet
- Vaginitis in Children (For Parents) - Nemours KidsHealthDocument1 pageVaginitis in Children (For Parents) - Nemours KidsHealthHabtamu tamiruNo ratings yet
- MCQ 2009 FMS4 - HIV, Meningitis, PneumoniaDocument18 pagesMCQ 2009 FMS4 - HIV, Meningitis, Pneumoniadanielgunawan92No ratings yet
- RV Ollero MD's Guide to Advanced Trauma Life SupportDocument18 pagesRV Ollero MD's Guide to Advanced Trauma Life SupportPrincess Cate MercadoNo ratings yet
- Acute Diabetes ComplicationsDocument13 pagesAcute Diabetes ComplicationsMark Christian M. GonzagaNo ratings yet
- Cid en AdultosDocument38 pagesCid en AdultosJosephGabrielNo ratings yet