Professional Documents
Culture Documents
Case Traumatic Brain Injury - 0
Uploaded by
Dw Ipha Ma HaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Traumatic Brain Injury - 0
Uploaded by
Dw Ipha Ma HaCopyright:
Available Formats
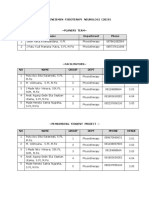
TRAUMATIC BRAIN INJURY
Ketut Widyastuti
AIMS : Able to understand of traumatic brain injury
LEARNING OUTCOME :
1. Able to describe pathobiology of Traumatic Brain Injury
2. Able to describe how to implement a neurological assessment for patient with
traumatic brain injury
3. Able to describe management of patient with Traumatic Brain Injury
4. Able to describe the prognosis patient with Traumatic Brain Injury
ABSTRACT
Traumatic Brain Injury (TBI) also known as acquired brain injury, head injury or brain injury
causes substantial disability and mortality. It occurs when a sudden trauma damages the brain
and disrupts normal brain function.
Pathophysiology of TBI: Classified as primary and secondary or focal and diffuse injury.
a.The Primary Mechanism
The two main mechanism that cause primary injury are contact and acceleration-
deceleration. As primary mechanisms of injury; in rapid acceleration/deceleration forces,
brain contusions most commonly occurs in the frontal and temporal poles and the inferior
surfaces of the frontal and temporal lobes, where bony protuberances at the skull base serve
as a less than friendly cushion for the brain moving the cranium.
b.The Secondary Mechanism
Injury may result from impairment or local declines in cerebral blood flow (CBF) after a TBI.
Decreases in CBF are result of local edema, hemorrhage, or increased intracranial pressure
(ICP). As a result of inadequate perfusion, cellular ion pumps may fail, causing a cascade
involving intracellular calcium and sodium. The metabolic cascades involves molecular and
cellular events that have multiple consequences. These include breakdown of the blood-brain
barrier and cerebral autoregulation, edema formation, impairment of energy metabolism,
changes in cerebral perfusion, disruption of ionic homeostasis, activation of autodestructive
neurochemicals, generation of free radicals and genomic changes, which all are considered
secondary mechanism of neural dysfunction and cell death. Clinical conditions associated with
the risk of a decreased CBF are arterial hypotension, hypoxemia, intracranial hemorrhage and
malignant brain edema and hyperthermia.
Prognosis of head injury depend on :
1. The anatomical area involved
The outcome and complications of frontal , lateral and occipital impacts are to some
extent dictated by the local anatomy, e. g. precense of air sinuses, large blood
vessels, etc.
2. The type of injury
Injury forces applied to particular anatomical areas produce a patetern of injury for
the individual, e. g.
- Acceleration/ Deceleration : - applied to entire head, evident as disordered
consciousness from the time of impact resulting from concussion, often with
diffuse axonal injury and /or cerebral contusions [coup or contrecoup].
- Local impact : - coup injuries to scalp, skull, meninges, brain.
- Penetrating : - pathway of injury velocity and nature of projectile
- Crush injury : - scalp, skull, and cranial nerve injuries.
3. The pathology of injury
Primary :
Scalp : - contusion, abrasion, laceration
Skull fracture : open, close, linear, depressed, comminuted
Meningeal injury : - contusion, laceration
Brain injury: concussion, diffuse axonal, focal contusion, laceration and penetration
Secondary: Intracranial haemorrhage, Cerebral swelling, Cerebral hypoxia, C.S.F.
leakage and pneumocephalus, Metabolic disorders, Infection, Epilepsy
4. The evolution of the injury
The rate of deterioration will influence the time available for specific treatment..
Cognitive impairments after TBI include difficulty concentrating, difficulty remembering,
forgetting recent events, confusion, answering slowly and amnesia. Duration of post traumatic
amnesia (PTA) can also provide of injury severity ranging from very mild (<5 minutes) to
extremely severe (>4 weeks). Retrograde amnesia involving minutes or more rarely days,
immediately preceding the accident frequently accompanies PTA.
The TBI severity spectrum ranges from mild impact with no behavioral syndromes, resulting
in no lasting structural injury and producing only transient and temporary changes in
neurologic function to patients in prolonged coma/ vegetative state from catastrophic brain
injury. Cognitive impairments after a concussion can include difficulty concentrating, difficulty
remembering, feeling slowed down, forgetting recent events, confusion, repeating question,
answering slowly and amnesia.
Retrograde Amnesia is characterized by memory loss for events before brain trauma. This
likely results from inability to retrieve those memories from our memory storage with related
to an inability appropriate cues for memory retrieval.
Anterograde Amnesia is an inability to form a new memories or new information following brain
trauma, likely as a result of damage to the temporal or frontal lobes and the white matter
connecting them.
SCENARIO
A 23-year-old woman was taken to the hospital with a decrease in consciousness after a head
hit due to falling from a motorbike during a traffic accident. Head CT was performed and a
cerebral frontotemporal hemorrhage and cerebral edema were found. Decompression
craniectomy was performed in patients by neurosurgeons. On the third day postoperatively,
the patient was well aware of the weakness in the left side of the body. Patients do not
remember chronologically when the event took place.
Learning Task:
1. What kind of history points are needed in the case?
2. How to diagnose this patient?
3. Please explain physical assessment and plan of care in this patient! I
4. Please explain the prognosis in this patient
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Game Audio - Tales of A Technical Sound Designer Volume 02Document154 pagesGame Audio - Tales of A Technical Sound Designer Volume 02Joshua HuNo ratings yet
- Aggregate Production PlanningDocument5 pagesAggregate Production PlanningSarbani SahuNo ratings yet
- (Walter Podolny, JR., John B. Scalzi) Construction PDFDocument354 pages(Walter Podolny, JR., John B. Scalzi) Construction PDFJuan Carlos CastroNo ratings yet
- 3309 19930 3 PB PDFDocument10 pages3309 19930 3 PB PDFOktania Karisma DewiNo ratings yet
- Fast Food Consumption Habits of University StudentsDocument4 pagesFast Food Consumption Habits of University StudentsDw Ipha Ma HaNo ratings yet
- Jadwal Blok Manajemen FT Neuro 2019 Revisi 13 November 2019 - 4 PDFDocument7 pagesJadwal Blok Manajemen FT Neuro 2019 Revisi 13 November 2019 - 4 PDFDw Ipha Ma HaNo ratings yet
- 1582 4356 1 PBDocument9 pages1582 4356 1 PBnurulanisa0703No ratings yet
- Cervical Traction 2Document13 pagesCervical Traction 2Dw Ipha Ma HaNo ratings yet
- Spinal Traction 1Document16 pagesSpinal Traction 1Dw Ipha Ma HaNo ratings yet
- Ultraviolet Radiaton: Made Hendra Satria Nugraha, S.FT., M.FisDocument30 pagesUltraviolet Radiaton: Made Hendra Satria Nugraha, S.FT., M.FisDw Ipha Ma HaNo ratings yet
- T-61.246 Digital Signal Processing and Filtering T-61.246 Digitaalinen Signaalink Asittely Ja Suodatus Description of Example ProblemsDocument35 pagesT-61.246 Digital Signal Processing and Filtering T-61.246 Digitaalinen Signaalink Asittely Ja Suodatus Description of Example ProblemsDoğukan TuranNo ratings yet
- English 7 q3 Week2 Daily Lesson LogDocument5 pagesEnglish 7 q3 Week2 Daily Lesson LogKILVEN MASIONNo ratings yet
- Syllabus 9701 Chemistry AS: AS or A2 UnitsDocument4 pagesSyllabus 9701 Chemistry AS: AS or A2 UnitsHubbak KhanNo ratings yet
- Module No.3 Prepare Architectual Job Requirements Architectural Working DrawingDocument23 pagesModule No.3 Prepare Architectual Job Requirements Architectural Working DrawingJay S. On100% (1)
- Hormone Replacement Therapy Real Concerns and FalsDocument13 pagesHormone Replacement Therapy Real Concerns and FalsDxng 1No ratings yet
- Toeic VocabularyDocument10 pagesToeic VocabularyBrian Niblo80% (5)
- SAP IAG Admin GuideDocument182 pagesSAP IAG Admin GuidegadesigerNo ratings yet
- A Study On Awareness of Mutual Funds and Perception of Investors 2Document89 pagesA Study On Awareness of Mutual Funds and Perception of Investors 2Yashaswini BangeraNo ratings yet
- Injection Nozzle Opening Pressure: Lmbo QFKD Fkpqor'qflkDocument1 pageInjection Nozzle Opening Pressure: Lmbo QFKD Fkpqor'qflkAlexanderNo ratings yet
- Chapter-4 Conditional and Iterative Statements in PythonDocument30 pagesChapter-4 Conditional and Iterative Statements in Pythonashishiet100% (1)
- CAKUTDocument50 pagesCAKUTsantosh subediNo ratings yet
- Law MCQ 25Document3 pagesLaw MCQ 25nonoNo ratings yet
- The Division 2 - Guide To Highest Possible Weapon Damage PvE BuildDocument18 pagesThe Division 2 - Guide To Highest Possible Weapon Damage PvE BuildJjjjNo ratings yet
- Available Online Through: International Journal of Mathematical Archive-4 (12), 2013Document4 pagesAvailable Online Through: International Journal of Mathematical Archive-4 (12), 2013Gwen WalkerNo ratings yet
- 1.2.2.5 Packet Tracer - Connecting Devices To Build IoTDocument4 pages1.2.2.5 Packet Tracer - Connecting Devices To Build IoTyayasan dharamabharataNo ratings yet
- Developing Sui-Generis System For The Protection of Trade Secret in India: An Analytical StudyDocument8 pagesDeveloping Sui-Generis System For The Protection of Trade Secret in India: An Analytical StudyVEENA T NNo ratings yet
- Sci5 q3 Module3 NoanswerkeyDocument22 pagesSci5 q3 Module3 NoanswerkeyRebishara CapobresNo ratings yet
- Fabrication Daily Progress: No DescriptionDocument4 pagesFabrication Daily Progress: No DescriptionAris PurniawanNo ratings yet
- rOCKY Dem Manual (010-057)Document48 pagesrOCKY Dem Manual (010-057)eduardo huancaNo ratings yet
- The Morning Calm Korea Weekly - August 22,2008Document24 pagesThe Morning Calm Korea Weekly - August 22,2008Morning Calm Weekly NewspaperNo ratings yet
- Business Maths Chapter 5Document9 pagesBusiness Maths Chapter 5鄭仲抗No ratings yet
- Acc 13 Februari 23 PagiDocument19 pagesAcc 13 Februari 23 PagisimbahNo ratings yet
- Portfolio Sandwich Game Lesson PlanDocument2 pagesPortfolio Sandwich Game Lesson Planapi-252005239No ratings yet
- Pinto pm5 Tif 02Document24 pagesPinto pm5 Tif 02Salem BawazirNo ratings yet
- CFA L1 Ethics Questions and AnswersDocument94 pagesCFA L1 Ethics Questions and AnswersMaulik PatelNo ratings yet
- Annual Presentation 18 19 EILDocument41 pagesAnnual Presentation 18 19 EILPartha Pratim GhoshNo ratings yet
- RRC & RabDocument14 pagesRRC & RabSyed Waqas AhmedNo ratings yet