Professional Documents
Culture Documents
Gyygg
Uploaded by
Yaumil AqsaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gyygg
Uploaded by
Yaumil AqsaCopyright:
Available Formats
Clinical Neurology: Research Article
Eur Neurol Received: August 11, 2019
Accepted: November 10, 2019
DOI: 10.1159/000504704 Published online: December 11, 2019
Hypertension with Hyperhomocysteinemia
Increases the Risk of Early Cognitive Impairment
after First-Ever Ischemic Stroke
Zhen-Hui Lu a, b Jia Li b Xin-Ling Li b Mei Ding b Cheng-Jie Mao a
Xiang-Yang Zhu b Chun-Feng Liu a
a Department
of Neurology, Second Affiliated Hospital of Soochow University, Suzhou, China;
b Department
of Neurology, Second Affiliated Hospital of Nantong University, Nantong, China
Keywords showed that hypertension with HHcy (OR 7.797; 95% CI
Cognitive impairment · Hypertension · 2.917–20.843; p = 0.000), the level of serum Hcy (OR 1.063;
Hyperhomocysteinemia · Ischemic stroke 95% CI 1.109–1.109; p = 0.005), education years (OR 0.797;
95% CI 0.722–0.880; p = 0.000), and Fazekas scale of leuko-
araiosis (OR 1.648; 95% CI 1.239–2.191; p = 0.001) were inde-
Abstract pendent influencing factors of early PSCI; however, simple
Background: Hypertension and hyperhomocysteinemia hypertension (OR 1.183, 95% CI 0.208–6.737; p = 0.850) and
(HHcy) are independent risk factors of stroke and are associ- simple HHcy (OR 1.112, 95% CI 0.181–6.810; p = 0.909) were
ated with each other. Although evidence suggests that they not. Conclusion: Patients with both hypertension and HHcy
are related to cognitive impairment, the relationship be- are at an increased risk of early cognitive impairment after
tween hypertension accompanied with HHcy and post- acute first-ever ischemic stroke. © 2019 S. Karger AG, Basel
stroke cognitive impairment (PSCI) is unclear. Objective: To
define the relationship between hypertension with HHcy
and early cognitive impairment after acute cerebral infarc-
tion. Materials and Methods: Our study enrolled 232 pa- Introduction
tients with acute first-ever ischemic stroke. Patients were as-
signed to 3 groups by blood pressure and homocysteine A previous study has shown an acute decline in cogni-
(Hcy) levels: hypertension with HHcy, simple hypertension, tive function after incident stroke and persistent cogni-
or control. Cognition was assessed by the Montreal cognitive tive decline over years [1]. However, early cognitive im-
assessment at admission and at 3- and 6-month follow-ups. pairment (at 3 months after onset) has a greater effect on
Results: The hypertension with HHcy group exhibited the neurological recovery than delayed cognitive impairment
highest incidence of early cognitive impairment (simple hy- thus that deserves our more attention. Cognitive impair-
pertension: p = 0.000; control: p = 0.000). This group also had
lower visual space/executive scores than the simple hyper-
tension group (p = 0.000) and lower delayed recall scores Chun-Feng Liu
Department of Neurology
than the control group (p = 0.011). Multivariate analysis Second Affiliated Hospital of Soochow University
1055 Sanxiang Road, Suzhou 215004 (China)
193.51.85.197 - 12/12/2019 5:33:15 PM
E-Mail liuchunfeng @ suda.edu.cn
Université René Descartes Paris 5
© 2019 S. Karger AG, Basel Xiang-Yang Zhu
Department of Neurology
Second Affiliated Hospital of Nantong University
E-Mail karger@karger.com
6 Haier-xiang North Road, Nantong 226001 (China)
www.karger.com/ene
Downloaded by:
E-Mail zhuxxyy @ 163.com
ment after stroke is common. A previous investigation Sociodemographic, Clinical, Biochemical, and Neuroimaging
found that the prevalence of poststroke cognitive impair- Parameters
The following sociodemographic data were collected for all
ment (PSCI) in China is approximately 81% while that of participants by electronic medical records at admission: age, gen-
nondementia PSCI is 48.91% and poststroke dementia is der, level of education, smoking status, alcohol drinking status,
32.05% [2]. PSCI worsens quality of life, slows recovery and a history of hypertension, diabetes, and cardiac disease.
of function, and increases mortality. Despite of the prev- We monitored blood pressure during hospitalization and col-
alence of PSCI, cognitive assessment after stroke is often lected fasting venous blood samples within 1 day of hospitaliza-
tion. Homocysteine (Hcy), uric acid, cystatin C, total cholesterol,
neglected. Once PSCI progresses to poststroke dementia, triglyceride, HDL-C, LDL-C, C-reactive protein, and lipoprotein
the curative effect will be poor, so it is urgent to recognize phospholipase 2 were detected. Hypertension was defined as sys-
and prevent PSCI. tolic blood pressure (SBP) > 140 mm Hg and/or diastolic blood
Hypertension and hyperhomocysteinemia (HHcy) are pressure >90 mm Hg for 3 times in a quiet condition 1 week after
independent risk factors of stroke. Evidence suggests they onset of stroke or having a history of hypertension. HHcy was de-
fined as Hcy level ≥10 μmol/L [8, 9]. Patients were assigned to
are also associated with each other [3] and appear to be groups by blood pressure and Hcy levels: hypertension with HHcy
related to cognitive impairment [4, 5]. However, no stud- group, patients with hypertension and HHcy; simple hypertension
ies have investigated whether (and by what mechanism) group, patients with hypertension but without HHcy; and control
hypertension accompanied with HHcy is related to PSCI. group, patients without hypertension regardless of Hcy level.
In China, the prevalence of hypertension accompanied Ischemic stroke was classified by the following the Trial of Org
10172 in Acute Stroke Treatment classification [10] subtypes: large-
with HHcy was estimated at 50.2% among elderly persons artery atherosclerosis, small-artery occlusion, cardioembolism, oth-
aged ≥60 years [6]. In Chinese patients with first-ever er determined cause, and undetermined cause. Cerebral infarction
acute cerebral infarction, this study aimed to explore clinical subtypes were categorized according to the Oxfordshire
whether those with both hypertension and HHcy exhib- Community Stroke Project (OCSP) classification [11]: total anterior
ited earlier cognitive impairment and a higher incidence circulation infarction, partial anterior circulation infarction, lacu-
nar cerebral infarction, and posterior circulation infarction.
of PSCI after stroke than those without hypertension or Brain MRI was performed on a 3.0T Verio MRI system (Verio,
HHcy. Siemens, Germany), with a 16-channel head coil. The scanning
sequences included diffusion weighted imaging, T1WI, T2WI, T2-
fluid-attenuated inversion recovery, and coronal images of T1WI.
All scans covered the entire brain parenchyma.
Materials and Methods The severity of cerebral leukoaraiosis was evaluated by Fazekas
scale based on fluid-attenuated inversion recovery sequence im-
Study Design and Participants ages of brain MRI [12]. The degree of hippocampal atrophy was
From April to December 2018 in neurology department of Sec- evaluated by medial temporal lobe atrophy (MTA) score based on
ond Affiliated Hospital of Nantong University, 232 patients eligi- the coronal images of brain MRI [13].
ble for inclusion were enrolled in this study. All patients received
routine treatment of acute cerebral infarction during hospitaliza- Cognitive and Neurological Functional Assessment and
tion and secondary prevention during follow-up and did not use Follow-Up
drugs or rehabilitation training that may affect cognitive function. In our study, the Montreal cognitive assessment (MoCA) was
Inclusion criteria for participants in this study were the follow- used to evaluate all participants’ cognition during hospitalization
ing: (1) onset of first-ever acute ischemic stroke within 7 days of and at 3 and 6 months after onset. Patients with an MoCA score
enrollment; (2) the ability to undergo a brain MRI examination to less than 26 (if years of education ≤12 years, the final score plus 1)
confirm acute infarct of brain, and (3) willingness to undergo a were considered cognitively impaired. The MoCA is a brief and
cognitive functional examination. Patients were excluded from the effective tool for assessing cognitive function, and its specificity
study for the following reasons: (1) preexisting cognitive impair- and sensitivity to detect mild cognitive injury are better than those
ment, and the prestroke functional status was determined by the of the Mini-Mental State Examination [14]. When the cutoff score
IQCODE [7]; (2) anxiety or depression examined by the anxiety/ is 26, MoCA has been found to have good specificity and sensitiv-
depression self-rating scale; (3) aphasia or uncooperative patients ity [15].
who could not perform a cognitive functional examination; (4) The National Institutes of Health Stroke Scale (NIHSS) [16]
strategic infarction that may affect cognition, such as frontal and score was used to assess all participants’ neurological function at
temporal lobe, hippocampus, thalamus, and corpus callosum; (4) admission. Modified Rankin Scale (mRS) was used to assess neu-
venous/arterial thrombolysis, interventional thrombectomy, or rological prognosis at 3 months after onset. An mRS score ≤2 was
other cerebral diseases such as tumor and hydrocephalus; (5) ce- considered a good outcome, and an mRS score >2 was considered
rebral hemorrhage transformation; and (6) recurrence of stroke a poor outcome.
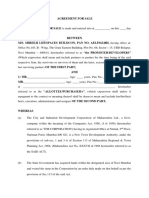
during follow-up. After 6 months of follow-up, 19 patients were excluded: 9 pa-
Second Affiliated Hospital of Nantong University Ethics Com- tients were lost to follow-up, 6 patients had cerebral hemorrhage
mittee (2018003) approved our study. All participants or autho- transformation after stroke, 3 patients had a recurrence of cerebral
rized agents signed written informed consent. infarction, and 1 patient died of severe pneumonia (Fig. 1).
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
2 Eur Neurol Lu/Li/Li/Ding/Mao/Zhu/Liu
DOI: 10.1159/000504704
Downloaded by:
(p > 0.05, Table 1). However, the differences in level of
Baseline: 232 patients with Hcy and cystatin C, the Trial of Org 10172 in Acute Stroke
first-ever acute ischemic stroke
Treatment subtype, and Fazekas scale of leukoaraiosis
were statistically significant (p < 0.05, Table 1). The hy-
Follow-up for 6 months pertension with HHcy group had higher cystatin C levels
than the simple hypertension (p = 0.000) and normal
19 patients were excluded:
blood pressure (p = 0.042) groups. The hypertension with
• Lost to follow-up (n = 9) HHcy group had more small-artery occlusion than the
• Hemorrhage transformation (n = 6) control group (p = 0.028). The hypertension with HHcy
• Recurrence of stroke (n = 3)
• Died of pneumonia (n = 1)
group had a more severe scale of leukoaraiosis than the
control group (p = 0.013).
213 patients completed study
MoCA Score and Incidence of Early PSCI after
Ischemic Stroke
Fig. 1. Flowchart of study participant selection. Repetitive ANOVA showed there were statistically sig-
nificant changes in MoCA scores of all study participants
within 6 months after stroke (Fig. 2). MoCA scores de-
Statistical Analysis creased within 3 months and then slowly increased at 6
SPSS 19.0 was used to perform the statistical analysis. Differ- months after stroke. However, no statistically significant
ences in baseline characteristics and neurological prognosis among difference was found in the incidence of PSCI during the
the 3 groups were tested by the χ2 test, one-way ANOVA, or Krus- follow-up period (Fig. 2).
kal-Wallis test. The incidence of PSCI and MoCA scores among 3
groups were compared by χ2 test or Kruskal-Wallis test. Repetitive
ANOVA was used to analyze the change of MoCA score during Incidence of Early PSCI and Cognitive Function at 3
follow-up, and χ2 test was used to analyze the change of PSCI in- Months after Stroke
cidence after ischemic stroke during follow-up. As indicated in Table 2, the hypertension with HHcy
Then, patients were resorted into 1 of 2 groups: PSCI group, group showed a higher incidence of early PSCI than the
presence of PSCI; and no PSCI group, absence of PSCI. Differ-
ences in baseline characteristics and neurological prognosis be- simple hypertension (p = 0.000) and control (p = 0. 000)
tween the PSCI group and the no PSCI group were tested by the χ2 groups. Participants with both hypertension and HHcy
test, Student’s t test, or Mann-Whitney U test. Statistical signifi- had lower MoCA scores than those with simple hyperten-
cance was set at a p value <0.05. sion. No statistically significant differences were found in
Finally, we used logistic regression analysis to explore indepen- the subscores of naming, language, abstraction, and orien-
dent influencing factors of early PSCI after first-ever acute isch-
emic stroke. tation. However, statistically significant differences were
demonstrated in visual space/executive (p = 0.000), atten-
tion (p = 0.003), and delayed recall (p = 0.034) subscores.
Further comparisons indicated that the hypertension with
Results HHcy group had lower visual space/executive scores than
the simple hypertension group (p = 0.000) and control
Clinical Characteristics group (p = 0.011) and also had lower attention scores than
Of the 232 patients who were initially enrolled in our the simple hypertension group (p = 0.002) and lower de-
study, 19 were excluded during follow-up and 213 com- layed recall scores than the control group (p = 0.020).
pleted the study. The differences in baseline characteris-
tics (gender, age, years of education, a history of diabetes Correlation between Clinical Characteristics and PSCI
mellitus and cardiac disease, smoking status, and alcohol at 3 Months after Stroke
drinking status, time from onset to admission, uric acid, All participants were divided into 2 groups according
total cholesterol, triglyceride, HDL-C, LDL-C, C-reactive to whether they were with or without PSCI at 3 months
protein, lipoprotein phospholipase 2, OCSP type, loca- after stroke. Comparisons between these 2 groups showed
tion, MTA score of hippocampal volume, National Insti- that participants with PSCI were older and had less years
tutes of Health Stroke Scale score at admission) and prog- of education than those without PSCI (p < 0.05; Table 3).
nosis among hypertension with HHcy, simple hyperten- The PSCI group had higher cystatin C and serum Hcy
sion, and control groups were not statistically significant levels than the no PSCI group (p < 0.05; Table 3). Signifi-
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
Hypertension with HHcy Increases the Eur Neurol 3
Risk of Early Cognitive Impairment DOI: 10.1159/000504704
Downloaded by:
Table 1. Baseline clinical characteristics of participants by group
Characteristicsa Hypertension with Simple Control group F value p value
HHcy group hypertension (n = 41) or
(n = 128) group (n = 44) χ2 value
Gender, males, n (%) 86 (67.2) 22 (50.0) 30 (73.2) 5.804 0.055
Age, years 66.3 (11.2) 62.8 (10.0) 65.5 (13.4) 1.487 0.229
Education, years 9.2 (4.1) 9.2 (4.1) 8.3 (4.2) 0.740 0.478
Time from onset to admission, days 2.6 (1.7) 2.7 (2.0) 2.4 (1.7) 0.483 0.618
Diabetes mellitus, n (%) 38 (29.7) 21 (47.7) 13 (31.7) 4.862 0.088
Coronary heart disease, n (%) 13 (10.2) 7 (15.9) 6 (14.6) 1.290 0.525
Atrial fibrillation, n (%) 16 (12.5) 2 (4.5) 2 (4.9) 3.650 0.161
Smoking, n (%) 30 (23.4) 9 (20.5) 8 (19.5) 0.362 0.834
Alcohol drinking, n (%) 22 (17.2) 7 (15.9) 7 (17.1) 0.039 0.981
Homocysteine, μmol/L 16.1 (9.6)b 8.6 (0.9)c 14.5 (13.4) 10.025 0.000
UA, μmol/L 334.1 (98.1) 300.4 (105.2) 307.7 (89.0) 2.473 0.087
Cystatin C, mg/L 1.1 (0.3)b,c 0.9 (0.2) 1.0 (0.3) 9.487 0.000
TC, mmol/L 4.3 (0.9) 4.4 (1.0) 4.1 (1.0) 1.280 0.280
TG, mmol/L 1.9 (1.4) 2.0 (1.1) 1.6 (0.9) 1.358 0.259
HDL-C, mmol/L 1.2 (0.3) 1.2 (0.3) 1.2 (0.2) 0.032 0.968
LDL-C, mmol/L 2.7 (0.8) 2.8 (0.9) 2.6 (0.8) 0.514 0.599
CRP, mg/L 4.4 (3.8) 5.2 (5.0) 3.9 (3.5) 1.092 0.337
Lp-PLA2, ng/mL 131.0 (110.7) 116.2 (104.8) 143.2 (118.1) 0.635 0.531
TOAST type, n (%) 16.893 0.010
Large-artery atherosclerosis 38 (29.7)c 17 (38.6) 21 (51.2)
Small-artery occlusion 83 (64.8)c 26 (59.1) 17 (41.5)
Cardioembolism 7 (5.5) 0 3 (7.3)
Other determined cause 0 1 (2.3) 0
OCSP type, n (%) 7.160 0.128
TACI 0 0 0
PACI 34 (26.6) 12 (27.3) 13 (31.7)
LACI 60 (46.8) 19 (43.2) 10 (24.4)
POCI 34 (26.6) 13 (29.5) 18 (43.9)
Location, n (%) 4.511 0.341
Left side 59 (46.1) 18 (40.9) 19 (46.3)
Right side 61 (47.7) 25 (56.8) 17 (41.5)
Bilateral 8 (6.2) 1 (2.3) 5 (12.2)
Fazekas scale of leukoaraiosis, median (IQR) 3 (2)c 2 (2) 2 (2) 7.091 0.029
MTA score of hippocampal volume, median (IQR) 1 (1) 1 (1) 1 (1) 0.808 0.668
NIHSS score 3.7 (2.8) 3.6 (2.8) 3.3 (2.7) 0.328 0.721
Good outcome, n (%) 94 (73.4) 38 (86.4) 36 (87.8) 5.714 0.057
a Data
are expressed as mean (SD) unless otherwise noted.
b p
value <0.05 for comparisons with the simple hypertension group.
c p value <0.05 for comparisons with the control group.
UA, uric acid; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, high-density lipoprotein
cholesterol; CRP, C-reactive protein; Lp-PLA2, lipoprotein phospholipase 2; TOAST, the Trial of Org 10172 in Acute Stroke Treatment;
OCSP, Oxfordshire Community Stroke Project; TACI, total anterior circulation infarction; PACI, partial anterior circulation infarction;
POCI, posterior circulation infarction; LACI, lacunar cerebral infarction; IQR, interquartile range; MTA, medial temporal lobe atrophy;
NIHSS, National Institutes of Health Stroke Scalect.
cant difference in OCSP type was identified between the without PSCI. In addition, patients with PSCI had higher
2 groups, and the PSCI group had more partial anterior Fazekas scale and MTA scores than patients without PSCI
circulation infarction than the control group (p < 0.05; (p < 0.05; Table 3). Furthermore, participants without
Table 3). Participants with PSCI had higher incidences of PSCI had a better prognosis at 3 months after stroke than
hypertension and hypertension with HHcy than those those with PSCI (p < 0.05; Table 3).
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
4 Eur Neurol Lu/Li/Li/Ding/Mao/Zhu/Liu
DOI: 10.1159/000504704
Downloaded by:
100 35
PSCI MoCA
90 30
80 25
Incidence of PSCI, %
MoCA score, point
70 20
24.03 (5.05) 23.66 (5.05) 23.81 (5.09)
60 15
Fig. 2. Changes in MoCA scores and early
PSCI incidence after ischemic stroke. AA, 50 10
53.1
at admission. There were statistically sig-
nificant changes in MoCA scores (Fb = 46.5
40 5
21.454; pb = 0.000), but no statistically sig- 41.3
nificant change in the incidence of PSCI
(χ2a = 5.919, pa = 0.052). PSCI, poststroke 30 0
AA 3m 6m
cognitive impairment; MoCA, Montreal
cognitive assessment.
Table 2. Comparison of MoCA score and the incidence of PSCI at 3 months after stroke among patients with both hypertension and
HHcy, with simple hypertension and without hypertension
Characteristicsa Hypertension with Simple Control group F value p value
HHcy group hypertension (n = 41) or
(n = 128) group (n = 44) χ2 value
PSCI, n (%) 86 (67.2)b,c 13 (29.5) 14 (34.1) 25.914 0.000
MoCA scores, mean (SD) 22.7±4.8b 25.6±4.3 24.5±5.8 6.042 0.003
Visual space/executive 3 (2)b,c 5 (1.75) 4 (2) 21.787 0.000
Naming 3 (0) 3 (0) 3 (0) 0.424 0.809
Attention 4.5 (3)b 5 (1) 5 (1) 11.653 0.003
Language 3 (1) 3 (1) 3 (0.5) 0.639 0.727
Abstraction 2 (0.75) 2 (0) 2 (0) 0.387 0.824
Delayed recall 3 (4)c 4 (2) 4 (1) 6.736 0.034
Orientation 6 (1) 6 (1) 5 (1) 3.358 0.187
a
Data expressed as median (interquartile range) unless otherwise noted.
b p value <0.05 for comparisons with the simple hypertension group.
c p value <0.05 for comparisons with the control group.
MoCA, Montreal cognitive assessment; PSCI, poststroke cognitive impairment; HHcy, hyperhomocysteinemia.
Independent Influencing Factors of Early PSCI at 3 and found that hypertension with HHcy (OR 7.797; 95%
Months after Ischemic Stroke CI 2.917–20.843; p = 0.000) was an independent risk fac-
In multivariate logistic regression, we found both hy- tor of early PSCI after ischemic stroke with normal blood
pertension (OR 4.841; 95% CI 1.921–12.196; p = 0.001) pressure group as the reference while simple hyperten-
and the level of serum Hcy (OR 1.063; 95% CI 1.109– sion (OR 1.097, 95% CI 0.345–3.495; p = 0.875) was not
1.109; p = 0.005) were independent risk factors of early (Table 5, Model 2). Furthermore, we divided normal
PSCI after adjusting for the factors with p < 0.1 in a uni- blood pressure group in Model 2 into normal blood pres-
variate logistic regression (Table 4, Model 1). Then we sure and Hcy group and simple HHcy group in Model 3
replaced the factors (hypertension and Hcy level) in and found that hypertension with HHcy (OR 8.453; 95%
Model 1 with the factor (grouping [normal blood pres- CI 1.542–46.347; p = 0.014) was an independent risk fac-
sure, simple hypertension, and hypertension with HHcy]) tor of early PSCI with normal blood pressure and Hcy
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
Hypertension with HHcy Increases the Eur Neurol 5
Risk of Early Cognitive Impairment DOI: 10.1159/000504704
Downloaded by:
Table 3. Comparison of clinical characteristics between participants with and without PSCI
Characteristicsa PSCI No PSCI t value, p value
(n = 113) (n = 100) U value, χ2
Gender, males, n (%) 67 (59.3) 71 (71.0) 3.188 0.074
Age, years 68.7 (9.1) 61.7 (12.8) −4.587 0.000
Education, years 7.7 (4.6) 10.4 (3.1) 5.156 0.000
Time from onset to admission, days 2.5 (1.6) 2.6 (1.9) 0.372 0.710
Hypertension, n (%) 99 (87.6) 73 (73.0) 7.286 0.007
Homocysteine, μmol/L 15.5 (10.1) 12.8 (9.5) –2.050 0.042
Diabetes mellitus, n (%) 36 (31.9) 36 (36.0) 0.407 0.529
Coronary heart disease, n (%) 10 (8.8) 16 (16.0) 2.531 0.112
Atrial fibrillation, n (%) 12 (10.6) 8 (8.0) 0.428 0.513
Smoking, n (%) 22 (19.5) 25 (25.0) 0.944 0.331
Alcohol drinking, n (%) 16 (14.2) 20 (20.0) 1.289 0.256
UA, μmol/L 324.5 (100.1) 319.2 (97.5) –0.387 0.699
Cystatin C, mg/L 1.1 (0.3) 1.0 (0.2) –2.863 0.005
TC, mmol/L 4.3 (1.0) 4.3 (0.9) –0.115 0.909
TG, mmol/L 1.8 (1.3) 2.0 (1.2) 0.804 0.422
HDL-C, mmol/L 1.2 (0.3) 1.1 (0.3) –1.435 0.153
LDL-C, mmol/L 2.7 (0.8) 2.7 (0.8) 0.459 0.647
CRP, mg/L 4.5 (4.0) 4.4 (4.0) –0.091 0.928
Lp-PLA2, ng/mL 133.8 (112.2) 126.3 (109.5) –0.496 0.621
Grouping 1, n (%) 25.914 0.000
Hypertension with HHcy 86 (76.1) 42 (42.0)
Simple hypertension 13 (11.5) 31 (31.0)
Normal blood pressure 14 (12.4) 27 (27.0)
Grouping 2, n (%) 25.943 0.000
Hypertension with HHcy 86 (76.1) 42 (42.0)
Simple hypertension 13 (11.5) 31 (31.0)
Simple HHcy 10 (8.8) 20 (20.0)
Normal blood pressure and Hcy 4 (3.6) 7 (7.0)
TOAST type, n (%) 2.796 0.424
Large-artery atherosclerosis 45 (39.8) 31 (31.0)
Small-artery occlusion 63 (55.8) 63 (63.0)
Cardioembolism 5 (4.4) 5 (5.0)
Other determined cause 0 1 (1.0)
OCSP type, n (%) 7.274 0.026
TACI 0 0
PACI 40 (35.4) 19 (19.0)
LACI 41 (36.3) 48 (48.0)
POCI 32 (28.3) 33 (30.0)
Location, n (%) 1.572 0.456
Left side 47 (41.6) 49 (49.0)
Right side 57 (50.4) 46 (46.0)
Bilateral 9 (8.0) 5 (5.0)
Fazekas scale of leukoaraiosis, median (IQR) 3 (2) 2 (2) −4.665 0.000
MTA score of hippocampal volume, median (IQR) 1 (1) 0 (1) −3.163 0.002
NIHSS score, mean (SD) 3.8 (2.7) 3.5 (2.9) –0.827 0.409
Good outcome, n (%) 79 (70.0) 90 (90.0) 14.005 0.000
a Dataare expressed as mean (SD) unless otherwise noted.
UA, uric acid; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, high-density lipoprotein
cholesterol; CRP, C-reactive protein; Lp-PLA2, lipoprotein phospholipase 2; TOAST, the Trial of Org 10172 in Acute Stroke Treatment;
OCSP, Oxfordshire Community Stroke Project; TACI, total anterior circulation infarction; PACI, partial anterior circulation infarction;
POCI, posterior circulation infarction; LACI, lacunar cerebral infarction; IQR, interquartile range; MTA, medial temporal lobe atrophy;
NIHSS, National Institutes of Health Stroke Scale; PSCI, post-stroke cognitive impairment.
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
6 Eur Neurol Lu/Li/Li/Ding/Mao/Zhu/Liu
DOI: 10.1159/000504704
Downloaded by:
Table 4. Risk factors associated with PSCI in multivariate logistic panied with HHcy is an independent risk factor of stroke
regression Model 1 and maybe correlated with PSCI. Recently, the high pro-
portion of Chinese patients with both hypertension and
OR 95% CIs p value
HHcy has been garnering increased attention from cardi-
Hypertension 4.841 1.921–12.196 0.001 ologists and neurologists. Our study showed that patients
Homocysteine 1.063 1.019–1.109 0.005 with both hypertension and HHcy have a higher Fazekas
Education years 0.797 0.722–0.880 0.000 score of leukoaraiosis and an increased incidence of early
Fazekas scale of leukoaraiosis 1.648 1.239–2.191 0.001
PSCI after first-ever acute ischemic stroke. Hypertension
Model 1: Factors (hypertension history, homocysteine, gender, with HHcy was an independent risk factor of early PSCI.
age, education years, Cystatin C, OCSP type, Fazekas scale of leu- In addition, we found that patients with both hyperten-
koaraiosis, and MTA score of hippocampal volume) were included sion and HHcy experience the most severe cognitive im-
in multivariate logistic regression. pairments in visual space/executive, attention, and de-
PSCI, poststroke cognitive impairment; OCSP, Oxfordshire
Community Stroke Project; MTA, medial temporal lobe atrophy.
layed recall functions.
Hcy, an amino acid primarily derived from food, is an
important intermediate of methionine and cysteine me-
tabolism. HHcy participates in the formation of hyper-
Table 5. Risk factors associated with PSCI in multivariate logistic tension, and there is synergy between HHcy and hyper-
regression Model 2 tension. For example, a previous study found that indi-
viduals with hypertension and HHcy are more likely to
OR 95% CIs p value have a stroke [17]. We found that patients with both hy-
pertension and HHcy were more susceptible to small-ves-
Grouping 1
Normal blood pressure 1 (ref.) 0.000 sel cerebral infarction and had the most severe cases of
Simple hypertension 1.097 0.345–3.495 0.875 leukoaraiosis. Also called white matter changes and
Hypertension with HHcy 7.797 2.917–20.843 0.000 white-matter hyperintensity, leukoaraiosis is a clinical
Education years 0.791 0.715–0.876 0.000 syndrome characterized by imaging terms proposed by
Fazekas scale of leukoaraiosis 1.559 1.171–2.077 0.002 Hachinski et al. [18]. Its pathological basis primarily in-
Model 2: Factors (grouping 1 [normal blood pressure, simple cludes loss of the myelin sheath, abnormity of the axon,
hypertension, and hypertension with HHcy], gender, age, educa- arteriosclerosis and lacunar infarction, microinfarction,
tion years, Cystatin C, OCSP type, Fazekas scale of leukoaraiosis, microhemorrhage, and changes in the perivascular sep-
and MTA score of hippocampal volume) were included in multi- tum [19]. Long-term hypertension can damage blood
variate logistic regression. vessels by degrading elastic fibers and increasing cellular/
PSCI, post-stroke cognitive impairment; HHcy, hyperhomo-
cysteinemia; OCSP, Oxfordshire Community Stroke Project; connective tissue components [20, 21]. Arterial stiffness
MTA, medial temporal lobe atrophy. or arteriosclerosis could occlude small perforating arter-
ies, leading to small-vessel lesions [22], and make the self-
regulation of cerebral blood vessels become worse, result-
ing in the brain being more sensitive to hypoperfusion.
group as the reference while simple hypertension (OR White matter is more susceptible to hypoperfusion be-
1.183, 95% CI 0.208–6.737; p = 0.850) and simple HHcy cause its blood supply primarily comes from the water-
(OR 1.112, 95% CI 0.181–6.810; p = 0.909) were not (Ta- shed arteries. Nasrallah et al. [23] also showed that higher
ble 6, Model 3). In the 3 models, it was shown that both SBP caused a larger increase in mean white matter change
of education years and Fazekas scale of leukoaraiosis were volume than lower SBP. However, the data concerning
independent influencing factors of early PSCI. the relationship between HHcy and leukoaraiosis are in-
consistent. Kloppenborg et al. [24] found that HHcy pro-
motes the progression of leukoaraiosis, and Feng et al.
Discussion [25] found that HHcy has a greater effect on cerebral
small vessel disease than large vessel disease. In contrast,
Globally, the prevalence of stroke remains high. A Yu et al. [26] demonstrated that leukoaraiosis is related to
stroke can result in motor and nonmotor disability. The hypertension but not serum Hcy. In our study, we showed
latter has become a research hotspot in the field of neurol- that the combination of hypertension and HHcy had
ogy, especially cognitive function. Hypertension accom- more damage to cerebral white matter and small blood
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
Hypertension with HHcy Increases the Eur Neurol 7
Risk of Early Cognitive Impairment DOI: 10.1159/000504704
Downloaded by:
Table 6. Risk factors associated with PSCI in multivariate logistic regression Model 3
OR 95% CIs p value
Grouping 2
Normal blood pressure and Hcy 1 (ref.) 0.000
Simple HHcy 1.112 0.181–6.810 0.909
Simple hypertension 1.183 0.208–6.737 0.850
Hypertension with HHcy 8.453 1.542–46.347 0.014
Education years 0.791 0.714–0.876 0.000
Fazekas scale of leukoaraiosis 1.559 1.171–2.076 0.002
Model 3: Factors (grouping 2 [normal blood pressure and Hcy, simple HHcy, simple hypertension, and hy-
pertension with HHcy], gender, age, education years, Cystatin C, OCSP type, Fazekas scale of leukoaraiosis, and
MTA score of hippocampal volume) were included in multivariate logistic regression.
PSCI, poststroke cognitive impairment; Hcy, homocysteine; HHcy, hyperhomocysteinemia; OCSP, Oxfords-
hire Community Stroke Project; MTA, medial temporal lobe atrophy.
vessels than simple hypertension. Hcy promotes extracel- PSCI while simple HHcy was not. This result is not self-
lular matrix proliferation [27] and may cause the overex- contradictory, probably due to the low value of HHcy set
pression of matrix metalloproteinase-2 in vascular endo- in the study. In our future study, we will stratify serum
thelium that leaded to vascular matrix damage [28]. Hcy Hcy at different levels and further explore its association
also could increase free oxygen radicals production that with PSCI. In addition, education years and Fazekas scale
contributed to impaired vascular endothelial function by of leukoaraiosis were independent influencing factors of
oxidative injury [29, 30]. In a study on hypertension by early PSCI after ischemic stroke. In a previous study, a
Guo et al. [31], HHcy was suggested to aggravate oxida- higher education level as a reasonable indicator of knowl-
tive stress, thus promoting vascular impairment. Im- edge reserves was found to reduce the risk of PSCI, which
paired endothelial function of cerebral small vessels re- is consistent with our findings [36]. Leukoaraiosis has
sulting in cerebral hypoperfusion and ischemia is expect- been suggested as a mediator in the association between
ed to further aggravate white matter leukoaraiosis. Our hypertension accompanied with HHcy and PSCI. Stroke
study also showed that patients with both hypertension patients with preexisting leukoaraiosis were more vulner-
and HHcy had highest cystatin C levels. Cystatin C is se- able to cognitive impairment regardless of the ischemic
creted from microglia, astrocytes and neurons, and its lesions [37]. A possible explanation was that widespread
level in the brain parenchyma rises as neurons degenerate leukoaraiosis impaired cognitive resilience of stroke pa-
[32]. Cystatin C is upregulated in degenerative astrocytes tients by diffusive damaging to brain’s network, thus pre-
in a self-defense response to the process of white matter disposing cognitive impairment once after ischemic
degeneration [33]. Lee et al. [34] also reported that Cys- stroke occurred [38]. The mechanism by which leukoara-
tatin C level was significantly correlated with white-mat- iosis causes cognitive impairment is still unclear. Previ-
ter hyperintensity volume. Thus, Cystatin C might be a ous studies have confirmed that cognitive impairment is
mediator in the association between hypertension ac- correlated with the degree of white matter loss [39] and
companied with HHcy and leukoaraiosis. remote white matter is related to cognitive function with-
This study indicated that hypertension accompanied in a long period after ischemic stroke [40]. There is evi-
with HHcy was an independent risk factor of early PSCI dence that it may be related to the damage of long joint
after first-ever acute ischemic stroke; however, simple hy- fibers that play a role in cognitive function, such as demy-
pertension and simple HHcy were not. Our findings fur- elination, loss of oligodendrocytes, and axonal injury
ther support the viewpoint that HHcy and hypertension [41]. Yuan et al. [42] also provided further evidence that
have a strong synergistic effect with each other. Hyper- leukoaraiosis may result in the impairment of subcortical
tension accompanied with Hcy accelerates endothelial and cortical-cortical connections and then leading to cog-
impairment and atherosclerosis, which are major patho- nitive dysfunction, especially in executive function.
logical processes in dementia [35]. We also found the lev- Further analysis of MoCA subscores indicated that pa-
el of serum Hcy was an independent risk factor of early tients with both hypertension and HHcy have the lowest
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
8 Eur Neurol Lu/Li/Li/Ding/Mao/Zhu/Liu
DOI: 10.1159/000504704
Downloaded by:
visual space/executive, attention, and delayed recall hypertension accompanied with HHcy and measure se-
scores. Recent studies showed that early cognitive impair- rum Hcy routinely in patients with hypertension. Once
ment of patients with leukoaraiosis may be most obvious acute cerebral infarction occurs in patients with both hy-
in visual space/executive function, delayed recall, abstrac- pertension and HHcy, we recommend assessing cognitive
tion, and orientation [43], and that cerebral small vessel function, monitoring the patient closely, and treating
disease is related to delayed recall dysfunction [44]. The cognitive impairments as soon as possible.
hippocampus and the cerebral cortex are vulnerable to
ischemia and anoxia [45], which may be a potential mech-
anism of PSCI. It would also explain why patients with Acknowledgment
PSCI are most impaired in visual space/executive and de-
I would like to express my gratitude to all those who helped me
layed recall functions.
during the writing of this thesis. A special acknowledgement
The prevalence of PSCI increased to 53.1% at 3rd should be shown to Prof. Chun-Feng Liu, from whose lectures I
month and then decreased to 46.5% at 6th month in our benefited greatly. I am particularly indebted to Prof. Xiang-Yang
study. The trend of PSCI incidence is consistent with pre- Zhu, who gave me kind encouragement and useful instructions all
vious study [46]. However, incidence of PSCI in our study through my writing.
was lower than previous studies, which perhaps be attrib-
uted to the exclusion of strategic infarction. In addition,
statistically significance changes in MoCA scores were Statement of Ethics
found within 6 months after stroke. Furthermore, we will The study was approved by Second Affiliated Hospital of Nan-
extend the observational time to acknowledge the regu- tong University Ethics Committee (2018003). All participants or
larity and characteristics of long-term PSCI after acute authorized agents signed written informed consent.
ischemic stroke.
Our study has some limitations. First, only patients
with first-ever ischemic stroke were included while those Disclosure Statement
who developed venous thrombolysis were excluded.
However, in clinical practice, there will be more and more The authors have no conflicts of interest to disclose.
patients with several times of stroke, and more and more
patients develop venous thrombolysis, so we can analyze
the factors such as number of strokes and venous throm- Funding Sources
bolysis in the future research. Second, this study did not This work was supported by Jiangsu Provincial Medical Key
involve the correlation between intervention of hyperten- Discipline Project (ZDXKB2016022) and Suzhou Clinical Re-
sion with HHcy and PSCI. Third, other factors that may search Center of Neurological Disease (Szzx201503).
be associated with PSCI, such as the level and rhythm of
blood pressure, blood pressure variability, blood glucose,
cerebral microbleed, and obstructive sleep apnea syn- Author Contributions
drome, were not measured in our current study. In future
Z.-H.L., X.-Y.Z., and C.-F.L. conceived and designed the study.
research, we can include these factors in the analysis.
Z.-H.L., J.-L., X.-L.L., and M.D. performed collection of medical
records and follow-up. Z.-H.L. analyzed the data and wrote the
paper. C.-J.M. and C.-F.L. reviewed and edited the manuscript. All
Conclusion authors read and approved the manuscript.
Hypertension accompanied with HHcy was found to
increase the risk of early PSCI after first-ever acute isch-
emic stroke, especially in visual space/executive, atten- References 1 Levine DA, Galecki AT, Langa KM, Unver-
tion, and delayed recall functions. Patients with PSCI af- zagt FW, Kabeto MU, Giordani B, et al. Tra-
jectory of cognitive decline after incident
ter first-ever ischemic stroke have worse prognosis at 3 stroke. JAMA. 2015 Jul;314(1):41–51.
months. Although simple hypertension and simple HHcy 2 Qu Y, Zhuo L, Li N, Hu Y, Chen W, Zhou Y,
are not independent risk factors of PSCI, hypertension et al. Prevalence of post-stroke cognitive im-
pairment in china: a community-based,
accompanied with HHcy and the level of serum Hcy are. cross-sectional study. PLoS One. 2015 Apr;
This suggests neurologists should pay more attention to 10(4):e0122864.
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
Hypertension with HHcy Increases the Eur Neurol 9
Risk of Early Cognitive Impairment DOI: 10.1159/000504704
Downloaded by:
3 Virdis A, Ghiadoni L, Cardinal H, Favilla S, in mild cognitive impairment (MCI) detec- but not other etiologic subtypes of ischemic
Duranti P, Birindelli R, et al. Mechanisms re- tion among people aged over 60? Meta- stroke. Stroke. 2000 May;31(5):1069–75.
sponsible for endothelial dysfunction in- analysis. Psychiatr Pol. 2016 Oct; 50(5): 30 Tian X, Zhao L, Song X, Yan Y, Liu N, Li T, et
duced by fasting hyperhomocystinemia in 1039–52. al. Hsp27 inhibits homocysteine-induced en-
normotensive subjects and patients with es- 16 Goldstein LB, Samsa GP. Reliability of the dothelial apoptosis by modulation of ros pro-
sential hypertension. J Am Coll Cardiol. 2001 National Institutes of Health Stroke Scale. duction and mitochondrial caspase-depen-
Oct;38(4):1106–15. Extension to non-neurologists in the context dent apoptotic pathway. BioMed Res Int.
4 Levine DA, Wadley VG, Langa KM, Unver- of a clinical trial. Stroke. 1997 Feb;28(2):307– 2016;2016:4847874.
zagt FW, Kabeto MU, Giordani B, et al. Risk 10. 31 Guo G, Sun W, Liu G, Zheng H, Zhao J. Com-
Factors for Poststroke Cognitive Decline: The 17 Towfighi A, Markovic D, Ovbiagele B. Pro- parison of oxidative stress biomarkers in hy-
REGARDS Study (Reasons for Geographic nounced association of elevated serum homo- pertensive patients with or without hyperho-
and Racial Differences in Stroke). Stroke. cysteine with stroke in subgroups of individu- mocysteinemia. Clin Exp Hypertens. 2018;
2018 Apr;49(4):987–94. als: a nationwide study. J Neurol Sci. 2010 40(3):262–6.
5 Smith AD, Refsum H. Homocysteine, B vita- Nov;298(1-2):153–7. 32 Wada M, Nagasawa H, Kawanami T, Kurita
mins, and cognitive impairment. Annu Rev 18 Hachinski VC, Potter P, Merskey H. Leuko- K, Daimon M, Kubota I, et al. Cystatin C as an
Nutr. 2016 Jul;36(1):211–39. araiosis. Arch Neurol. 1987 Jan;44(1):21–3. index of cerebral small vessel disease: results
6 Ma L, Li L, Tang Z. Epidemiological charac- 19 Wallin A, Román GC, Esiri M, Kettunen P, of a cross-sectional study in community-
teristics of hyperhomocysteinemia and H- Svensson J, Paraskevas GP, et al. Update on based Japanese elderly. Eur J Neurol. 2010
type hypertension in the elderly in Beijing, vascular cognitive impairment associated Mar;17(3):383–90.
China. Clin Exp Hypertens. 2017; 39(7): 640– with subcortical small-vessel disease. J Al- 33 Umegae N, Nagai A, Terashima M, Watanabe
4. zheimers Dis. 2018;62(3):1417–41. T, Shimode K, Kobayashi S, et al. Cystatin C
7 Park MH. Informant questionnaire on cogni- 20 Mahmud A, Feely J. Arterial stiffness is relat- expression in ischemic white matter lesions.
tive decline in the elderly (IQCODE) for clas- ed to systemic inflammation in essential hy- Acta Neurol Scand. 2008 Jul;118(1):60–7.
sifying cognitive dysfunction as cognitively pertension. Hypertension. 2005 Nov; 46(5): 34 Lee WJ, Jung KH, Ryu YJ, Kim JM, Lee ST,
normal, mild cognitive impairment, and de- 1118–22. Chu K, et al. Cystatin C, a potential marker
mentia. Int Psychogeriatr. 2017 Sep; 29(9): 21 Sun Z. Aging, arterial stiffness, and hyperten- for cerebral microvascular compliance, is
1461–7. sion. Hypertension. 2015 Feb;65(2):252–6. associated with white-matter hyperintensi-
8 McCully KS. Homocysteine, vitamins, and 22 Nam KW, Kwon HM, Jeong HY, Park JH, ties progression. PLoS One. 2017 Sep; 12(9):
vascular disease prevention. Am J Clin Nutr. Kim SH, Jeong SM, et al. Cerebral white mat- e0184999.
2007 Nov;86(5):1563S–8S. ter hyperintensity is associated with intracra- 35 Yarchoan M, Xie SX, Kling MA, Toledo JB,
9 Qin X, Huo Y. H-Type hypertension, stroke nial atherosclerosis in a healthy population. Wolk DA, Lee EB, et al. Cerebrovascular ath-
and diabetes in China: opportunities for pri- Atherosclerosis. 2017 Oct;265:179–83. erosclerosis correlates with Alzheimer pa-
mary prevention. J Diabetes. 2016 Jan; 8(1): 23 Nasrallah IM, Pajewski NM, Auchus AP, thology in neurodegenerative dementias.
38–40. Chelune G, Cheung AK, Cleveland ML, et al.; Brain. 2012 Dec;135(Pt 12):3749–56.
10 Adams HP Jr, Bendixen BH, Kappelle LJ, SPRINT MIND Investigators for the SPRINT 36 Ojala-Oksala J, Jokinen H, Kopsi V, Lehtonen
Biller J, Love BB, Gordon DL, et al. Classifi- Research Group. Association of intensive vs K, Luukkonen L, Paukkunen A, et al. Educa-
cation of subtype of acute ischemic stroke. standard blood pressure control with cerebral tional history is an independent predictor of
Definitions for use in a multicenter clinical white matter lesions. JAMA. 2019 Aug; cognitive deficits and long-term survival in
trial. TOAST. Trial of Org 10172 in Acute 322(6):524–34. postacute patients with mild to moderate
Stroke Treatment. Stroke. 1993 Jan; 24(1): 24 Kloppenborg RP, Geerlings MI, Visseren FL, ischemic stroke. Stroke. 2012 Nov; 43(11):
35–41. Mali WP, Vermeulen M, van der Graaf Y, et 2931–5.
11 Bamford J, Sandercock P, Dennis M, Burn J, al.; SMART Study Group. Homocysteine and 37 Kliper E, Ben Assayag E, Tarrasch R, Artzi M,
Warlow C. Classification and natural history progression of generalized small-vessel dis- Korczyn AD, Shenhar-Tsarfaty S, et al. Cog-
of clinically identifiable subtypes of cerebral ease: the SMART-MR Study. Neurology. 2014 nitive state following stroke: the predominant
infarction. Lancet. 1991 Jun;337(8756):1521– Mar;82(9):777–83. role of preexisting white matter lesions. PLoS
6. 25 Feng C, Bai X, Xu Y, Hua T, Huang J, Liu XY. One. 2014 Aug;9(8):e105461.
12 Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Hyperhomocysteinemia associates with small 38 Mok VC, Lam BY, Wong A, Ko H, Markus
Zimmerman RA. MR signal abnormalities at vessel disease more closely than large vessel HS, Wong LK. Early-onset and delayed-onset
1.5 T in Alzheimer’s dementia and normal ag- disease. Int J Med Sci. 2013;10(4):408–12. poststroke dementia – revisiting the mecha-
ing. AJR Am J Roentgenol. 1987 Aug; 149(2): 26 Yu X, Wang G, Zhan J, Zhang Z, Feng T, Xu nisms. Nat Rev Neurol. 2017;13(3):148–59.
351–6. J. Risk factors of pure leukoaraiosis and the 39 Lampe L, Kharabian-Masouleh S, Kynast J,
13 Scheltens P, Launer LJ, Barkhof F, Weinstein association with preclinical carotid athero- Arelin K, Steele CJ, Löffler M, et al. Lesion lo-
HC, van Gool WA. Visual assessment of me- sclerosis. Atherosclerosis. 2018 Aug;275:328– cation matters: the relationships between
dial temporal lobe atrophy on magnetic reso- 32. white matter hyperintensities on cognition in
nance imaging: interobserver reliability. J 27 Spence JD. Homocysteine-lowering therapy: the healthy elderly. J Cereb Blood Flow Metab.
Neurol. 1995 Sep;242(9):557–60. a role in stroke prevention? Lancet Neurol. 2019 Jan;39(1):36–43.
14 Nasreddine ZS, Phillips NA, Bédirian V, 2007 Sep;6(9):830–8. 40 Schaapsmeerders P, Tuladhar AM, Arntz
Charbonneau S, Whitehead V, Collin I, et al. 28 Liu J, Jin X, Liu KJ, Liu W. Matrix metallopro- RM, Franssen S, Maaijwee NA, Rutten-Jacobs
The Montreal Cognitive Assessment, MoCA: teinase-2-mediated occludin degradation and LC, et al. Remote lower white matter integrity
a brief screening tool for mild cognitive im- caveolin-1-mediated claudin-5 redistribution increases the risk of long-term cognitive im-
pairment. J Am Geriatr Soc. 2005 Apr; 53(4): contribute to blood-brain barrier damage in pairment after ischemic stroke in young
695–9. early ischemic stroke stage. J Neurosci. 2012 adults. Stroke. 2016 Oct;47(10):2517–25.
15 Ciesielska N, Sokołowski R, Mazur E, Pod- Feb;32(9):3044–57. 41 Kalaria RN. Neuropathological diagnosis of
horecka M, Polak-Szabela A, Kędziora- 29 Eikelboom JW, Hankey GJ, Anand SS, Loft- vascular cognitive impairment and vascular
Kornatowska K. Is the Montreal Cognitive house E, Staples N, Baker RI. Association be- dementia with implications for Alzheimer’s
Assessment (MoCA) test better suited than tween high homocyst(e)ine and ischemic disease. Acta Neuropathol. 2016 May;131(5):
the Mini-Mental State Examination (MMSE) stroke due to large- and small-artery disease 659–85.
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
10 Eur Neurol Lu/Li/Li/Ding/Mao/Zhu/Liu
DOI: 10.1159/000504704
Downloaded by:
42 Yuan JL, Wang SK, Guo XJ, Teng LL, Ji- imaging data detects microstructural damage 45 Ishibashi S, Kuroiwa T, LiYuan S, Katsumata
ang H, Gu H, et al. Disconnections of in mild cognitive impairment and alzheimer’s N, Li S, Endo S, et al. Long-term cognitive and
cortico-subcortical pathways related to
disease patients. J Magn Reson Imaging. 2018; neuropsychological symptoms after global
cognitive impairment in patients with
48(3):767–79. cerebral ischemia in Mongolian gerbils. Acta
leukoaraiosis: A preliminary diffusion tensor 44 van Es AC, van der Grond J, de Craen AJ, Neurochir Suppl (Wien). 2006;96:299–302.
imaging study. Eur Neurol. 2017; 78(1-2): Westendorp RG, Bollen EL, Blauw GJ, et al.; 46 He M, Wang J, Liu N, Xiao X, Geng S, Meng
41–7. PROSPER Study Group. Cerebral micro- P, et al. Effects of blood pressure in the early
43 Giulietti G, Mario T, Laura S, Barbara S, Ca- bleeds and cognitive functioning in the phase of ischemic stroke and stroke subtype
millo M, Carlo C, et al. Whole brain white PROSPER study. Neurology. 2011 Oct; on poststroke cognitive impairment. Stroke.
matter histogram analysis of diffusion tensor 77(15):1446–52. 2018 Jul;49(7):1610–7.
193.51.85.197 - 12/12/2019 5:33:15 PM
Université René Descartes Paris 5
Hypertension with HHcy Increases the Eur Neurol 11
Risk of Early Cognitive Impairment DOI: 10.1159/000504704
Downloaded by:
You might also like
- Initial Diagnosis and Management of Acutely Elevated Intracranial PressureDocument8 pagesInitial Diagnosis and Management of Acutely Elevated Intracranial PressureGlessin MurilloNo ratings yet
- Retinopatia HipertensivaDocument14 pagesRetinopatia HipertensivaPaito MartinezNo ratings yet
- Head Position in Acute Stroke Trial Statistical Analysis PlanDocument5 pagesHead Position in Acute Stroke Trial Statistical Analysis PlanNurul AzmiyahNo ratings yet
- Fneur 11 00071Document10 pagesFneur 11 00071Nurvia AndrianiNo ratings yet
- Hipertensi EnsefalopatiDocument6 pagesHipertensi EnsefalopatiLeonardo JeversonNo ratings yet
- Jamaneurology Topcuoglu 2017 Oi 170047Document8 pagesJamaneurology Topcuoglu 2017 Oi 170047LadycherryNo ratings yet
- Accepted Manuscript: Journal of The Neurological SciencesDocument31 pagesAccepted Manuscript: Journal of The Neurological SciencesZelNo ratings yet
- Juraschek Et Al, 2020Document28 pagesJuraschek Et Al, 2020Rahmi LubisNo ratings yet
- Cerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Document40 pagesCerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Reny Wane Vieira dos SantosNo ratings yet
- Brain and Behavior - 2020 - Feng - Reduced Thiamine Is A Predictor For Cognitive Impairment of Cerebral InfarctionDocument8 pagesBrain and Behavior - 2020 - Feng - Reduced Thiamine Is A Predictor For Cognitive Impairment of Cerebral InfarctionJasna BuhariNo ratings yet
- Ischemic StrokeDocument13 pagesIschemic StrokearthurbaidoodouglasNo ratings yet
- Cardiogenic VertigoDocument6 pagesCardiogenic VertigoHappy PramandaNo ratings yet
- Psychogenic Stroke A Case ReportDocument4 pagesPsychogenic Stroke A Case Reporteditorial.boardNo ratings yet
- Altered Mental Status in Cirrhosis: Etiologies and Outcomes: Riginal RticleDocument7 pagesAltered Mental Status in Cirrhosis: Etiologies and Outcomes: Riginal RticleTheRainMelodyNo ratings yet
- In Hospital Cardiac Complications After Intracerebral HemorrhageDocument6 pagesIn Hospital Cardiac Complications After Intracerebral HemorrhageIdrianaNo ratings yet
- Paroxysmal SympatheticDocument9 pagesParoxysmal Sympatheticluis argasNo ratings yet
- HIE and CVSDocument11 pagesHIE and CVSakshayajainaNo ratings yet
- The Pathogenesis Based On The Glymphatic System Diagnosis and Treatment of Idiopathic Normal Pressure Hydrocephalus-2Document16 pagesThe Pathogenesis Based On The Glymphatic System Diagnosis and Treatment of Idiopathic Normal Pressure Hydrocephalus-2dewi najiraNo ratings yet
- Missed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesDocument7 pagesMissed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesReyhansyah RachmadhyanNo ratings yet
- Clinical Neurology and NeurosurgeryDocument6 pagesClinical Neurology and NeurosurgeryNurul Azmi Rosmala PutriNo ratings yet
- Accepted Manuscript: 10.1016/j.neuint.2017.01.005Document42 pagesAccepted Manuscript: 10.1016/j.neuint.2017.01.005Irvin MarcelNo ratings yet
- Overview of Hemorrhagic Stroke Care in The Emergency Unit: Natalie Kreitzer and Daniel WooDocument11 pagesOverview of Hemorrhagic Stroke Care in The Emergency Unit: Natalie Kreitzer and Daniel WooIstiqomahsejatiNo ratings yet
- Lattanzi2019 Article Neutrophil To LymphocyteRatioIDocument9 pagesLattanzi2019 Article Neutrophil To LymphocyteRatioISusanyi ErvinNo ratings yet
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- Cerebrovascular Manifestations of Herpes Simplex Virus Infection of The Central Nervous System A Systematic ReviewDocument10 pagesCerebrovascular Manifestations of Herpes Simplex Virus Infection of The Central Nervous System A Systematic ReviewPau PuenteNo ratings yet
- Gallstone Disease and The Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Observational StudiesDocument7 pagesGallstone Disease and The Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Observational StudiesAfkar30No ratings yet
- Laske2015Document18 pagesLaske2015Paco SaavedraNo ratings yet
- Neutrophil To Lymphocyte Ratio at Admission Prognostic Factor in Patients With Acute Ischemic StrokeDocument7 pagesNeutrophil To Lymphocyte Ratio at Admission Prognostic Factor in Patients With Acute Ischemic StrokeUtari UbNo ratings yet
- EEG N StrokeDocument7 pagesEEG N StrokeNona Suci rahayuNo ratings yet
- Ensefalitis Dan PsikosisDocument15 pagesEnsefalitis Dan PsikosisLhia PrisciliiaNo ratings yet
- 1-s2.0-S1525505013004186 TUGAS INDAH-mainDocument5 pages1-s2.0-S1525505013004186 TUGAS INDAH-mainRendi Er PratamaNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument5 pagesIschemic Cerebral Stroke Case Report, Complications and Associated Factorsfaradilla wiyandaNo ratings yet
- Rossetti 2016Document13 pagesRossetti 2016Alexandra MoraesNo ratings yet
- Jurnal KimiaDocument5 pagesJurnal Kimiatrisna amijayaNo ratings yet
- 2018 Book CerebralIschemicReperfusionInjDocument269 pages2018 Book CerebralIschemicReperfusionInjVictor M TorresNo ratings yet
- postgradmedj-96-525Document5 pagespostgradmedj-96-525Huda TrisenaNo ratings yet
- Effect of Diabetes On The Prognosis of Sudden Sensorineural Hearing Loss: Propensity Score Matching AnalysisDocument8 pagesEffect of Diabetes On The Prognosis of Sudden Sensorineural Hearing Loss: Propensity Score Matching AnalysisRizki AdhinugrohoNo ratings yet
- Flat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialDocument12 pagesFlat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialNaufal HilmiNo ratings yet
- In-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackDocument15 pagesIn-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackferrevNo ratings yet
- Mayoclinproc 85-5-004Document6 pagesMayoclinproc 85-5-004Alain SánchezNo ratings yet
- ClinicalCharacteristicsAndProgrognostic AstrocytomaDocument12 pagesClinicalCharacteristicsAndProgrognostic AstrocytomaDesty PurnamasariNo ratings yet
- Comparison of Characteristics of Stroke-Associated Pneumonia in Stroke Care Units in Indonesia and JapanDocument6 pagesComparison of Characteristics of Stroke-Associated Pneumonia in Stroke Care Units in Indonesia and JapanMaulana DimasNo ratings yet
- 6-Diagnosis and Treatment of Nonepileptic Seizures.11Document16 pages6-Diagnosis and Treatment of Nonepileptic Seizures.11مجاهد إسماعيل حسن حسينNo ratings yet
- 5 Pre Diagnosis of Hypertension Using Artificial Neural Network PDFDocument7 pages5 Pre Diagnosis of Hypertension Using Artificial Neural Network PDFMartin AlcarazNo ratings yet
- Stress Mediators and Immune Dysfunction in Patients With Acute Cerebrovascular DiseasesDocument10 pagesStress Mediators and Immune Dysfunction in Patients With Acute Cerebrovascular DiseasesBian Rahmadi MedikantoNo ratings yet
- Intracerebral Haemorrhage: Disease PrimersDocument18 pagesIntracerebral Haemorrhage: Disease PrimersMarlon VillanuevaNo ratings yet
- Zhao 2014Document8 pagesZhao 2014AzkiaNo ratings yet
- Icbt10i12p1409 2 PDFDocument9 pagesIcbt10i12p1409 2 PDFakshayajainaNo ratings yet
- Prevalence and Prognosis of Atrial Fibrillation in A HypertensiveDocument8 pagesPrevalence and Prognosis of Atrial Fibrillation in A HypertensiveSyadzwina Putri salsabilaNo ratings yet
- Aspirin and Aspilet Compared PDFDocument18 pagesAspirin and Aspilet Compared PDFEfrianti Viorenta HutapeaNo ratings yet
- 10 1684@epd 2020 1159Document12 pages10 1684@epd 2020 1159rsu malahayatiNo ratings yet
- HSA Controversias 2016Document9 pagesHSA Controversias 2016Ellys Macías PeraltaNo ratings yet
- Paroxysmal Sympathetic Hyperactivity: The Storm After Acute Brain InjuryDocument25 pagesParoxysmal Sympathetic Hyperactivity: The Storm After Acute Brain InjuryaimanNo ratings yet
- E1512 FullDocument16 pagesE1512 Fullamilkar morunoNo ratings yet
- Y Yyy Y Yyy Y YY Y Yy Yyy Y ! YY"Y#Y$Y# Y Y % Y &Y'Y (Y) +#Y"Y Y Y, Yyyy-Yyy Y.Y Y Y/Y "Y.Y Y Y YDocument15 pagesY Yyy Y Yyy Y YY Y Yy Yyy Y ! YY"Y#Y$Y# Y Y % Y &Y'Y (Y) +#Y"Y Y Y, Yyyy-Yyy Y.Y Y Y/Y "Y.Y Y Y Ydoni007No ratings yet
- International Journal of Gerontology: Gwo-Chi Hu, Yi-Min ChenDocument5 pagesInternational Journal of Gerontology: Gwo-Chi Hu, Yi-Min Chenluthfia ayu az zahraNo ratings yet
- The Relationship Between Neurogenic Dysphagia, Stroke-Associated Pneumonia and Functional Outcome in A Cohort of Ischemic Stroke Patients Treated With Mechanical ThrombectomyDocument8 pagesThe Relationship Between Neurogenic Dysphagia, Stroke-Associated Pneumonia and Functional Outcome in A Cohort of Ischemic Stroke Patients Treated With Mechanical Thrombectomypalmaputri pinantiNo ratings yet
- 2.the Causes Analysis of Ischemic Stroke Transformation Into Hemorrhagic Stroke Using PLS Partial Least Square-GA and Swarm AlgorithmDocument10 pages2.the Causes Analysis of Ischemic Stroke Transformation Into Hemorrhagic Stroke Using PLS Partial Least Square-GA and Swarm AlgorithmgeethaNo ratings yet
- Ts Jurnal Batak SarapDocument6 pagesTs Jurnal Batak SarapAdityaNo ratings yet
- Seminar: Jan Claassen, Soojin ParkDocument17 pagesSeminar: Jan Claassen, Soojin ParkRaul DoctoNo ratings yet
- OrlDocument186 pagesOrlMuli MaroshiNo ratings yet
- SR. NO. Capacity/Descirption of Machine Client: A.C. Generator StatorsDocument5 pagesSR. NO. Capacity/Descirption of Machine Client: A.C. Generator Statorsmtj4uNo ratings yet
- Hero LetterDocument3 pagesHero LetterArunachalam Muthiah0% (1)
- Mohair FiberDocument33 pagesMohair FiberMuhammad Ahsan AftabNo ratings yet
- Mitsubishi Motors: Service ManualDocument29 pagesMitsubishi Motors: Service ManualCristobalNo ratings yet
- Studyguide TracksDocument75 pagesStudyguide TracksAnonymous FabB2WJl485% (13)
- 14-Friedel Crafts Acylation FerroceneDocument10 pages14-Friedel Crafts Acylation FerroceneNguyen Minh Duc100% (1)
- STP1236 Eb.1415051 1 PDFDocument208 pagesSTP1236 Eb.1415051 1 PDFpaolaNo ratings yet
- Sampling and Field Testing at Wastewater Treatment FacilitiesDocument11 pagesSampling and Field Testing at Wastewater Treatment FacilitiesSundarapandiyan SundaramoorthyNo ratings yet
- Rate AnalysisDocument46 pagesRate AnalysisbulganinganguliNo ratings yet
- Understanding The Nature of ReligionDocument41 pagesUnderstanding The Nature of Religioneden l. abadNo ratings yet
- Demonstration POSTNATAL EXAMINATION Easy WayDocument9 pagesDemonstration POSTNATAL EXAMINATION Easy Wayjyoti singhNo ratings yet
- Dsa 5300Document8 pagesDsa 5300Nguyen Van ToanNo ratings yet
- Iot PresentationDocument9 pagesIot PresentationAbdul Majid ShaikhNo ratings yet
- AABB Accredited DNA Testing FacilitiesDocument2 pagesAABB Accredited DNA Testing Facilitiesjosueduran75No ratings yet
- Hydraulic Excavator RH 200 1,568 kW 30.5 m3Document8 pagesHydraulic Excavator RH 200 1,568 kW 30.5 m3mchan1965100% (1)
- Eutelsat 12 West A Satellite FootprintDocument2 pagesEutelsat 12 West A Satellite FootprintSkybrokersNo ratings yet
- Comparative Study of Organic Solvents For Extraction of Copper From Ammoniacal Carbonate Solution Hu2010Document6 pagesComparative Study of Organic Solvents For Extraction of Copper From Ammoniacal Carbonate Solution Hu2010mtanaydinNo ratings yet
- yudaturana,+Manajer+Jurnal,+dr +nelson+rev+2+ (162-172)Document12 pagesyudaturana,+Manajer+Jurnal,+dr +nelson+rev+2+ (162-172)Fath TiaraNo ratings yet
- 1 Proforma of Allotment LetterDocument32 pages1 Proforma of Allotment LetterGovind SandhaNo ratings yet
- Bio Sem2 EssayDocument2 pagesBio Sem2 EssayEileen WongNo ratings yet
- Fault Codes: STO U AndriivDocument3 pagesFault Codes: STO U AndriivAtochkavNo ratings yet
- PT2E-1723 Gas Detector Operating ManualDocument54 pagesPT2E-1723 Gas Detector Operating ManualAsad Raza QureshiNo ratings yet
- Textiles and Clothing SustaninabilityDocument134 pagesTextiles and Clothing Sustaninabilitydike100% (1)
- Barney's Great Adventure - Barney Wiki - WikiaDocument2 pagesBarney's Great Adventure - Barney Wiki - WikiachefchadsmithNo ratings yet
- Astm D2467-2013Document8 pagesAstm D2467-2013Renato CorrêaNo ratings yet
- BrosurDocument68 pagesBrosurKiki Xhui7No ratings yet
- Rules For The CertificationDocument84 pagesRules For The CertificationhdelriovNo ratings yet
- Auomotivr Fuel TanksDocument9 pagesAuomotivr Fuel Tankscolumba_mcNo ratings yet
- 0610 m16 QP 62Document12 pages0610 m16 QP 62faryal khanNo ratings yet