Professional Documents
Culture Documents
10 23736@S1973-9087 17 04992-9
Uploaded by
FadhilannisaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 23736@S1973-9087 17 04992-9
Uploaded by
FadhilannisaCopyright:
Available Formats
not permitted.
It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
© 2017 EDIZIONI MINERVA MEDICA European Journal of Physical and Rehabilitation Medicine 2017 December;53(6):975-80
Online version at http://www.minervamedica.it DOI: 10.23736/S1973-9087.17.04992-9
SPECIAL ARTICLE
MANAGEMENT OF NEUROGENIC LOWER URINARY TRACT DYSFUNCTION
Diagnosis and clinical evaluation of neurogenic bladder
Gerard AMARENCO *, Samer SHEIKH ISMAËL, Camille CHESNEL,
Audrey CHARLANES, Frederique LE BRETON
Sorbonne Universities,
UTenon Hospital, Paris, France
*Corresponding author: Gerard Amarenco, Department of Neurourology, Tenon Hospital, Paris, France. E-mail: gerard.amarenco@aphp.fr
ABSTRACT
Neurologic diseases lead to urinary dysfunctions. The aim of this article was to present an overview of diagnosis and evaluation of neurogenic
bladder with a special focus on urodynamic tests. Overactive bladder, with high detrusor pressure associated with detrusor sphincter dyssynergia,
can lead to severe complications with renal failure, upper urinary tract dilatation and infectious complications. Underactive bladder with voiding
dysfunction and urinary retention, is also a risk factor of urological alterations. Full clinical examinations, including urodynamics and selective
radiographic imaging studies, are essential to best manage these patients.
(Cite this article as: Amarenco G, Sheikh Ismaël S, Chesnel C, Charlanes A, Le Breton F. Diagnosis and clinical evaluation of neurogenic bladder.
Eur J Phys Rehabil Med 2017;53:975-80. DOI: 10.23736/S1973-9087.17.04992-9)
Key words: Urinary bladder, neurogenic - Urinary bladder, overactive - Urodynamics.
M ost of neurologic diseases can be revealed or ac-
companied by urinary symptoms.
Indeed, bladder coordination centers and conduction
postvoid residual, can lead to severe complications with
renal failure, upper urinary tract dilatation and infec-
tious complications.
pathways are widely scattered in the whole central and Full clinical examinations, including urodynam-
peripheral somatic nervous system.1-5 Autonomic ner- ics and selective radiographic imaging studies, are
vous systems is also involved in the bladder control. essential in every case of neurogenic bladder to best
Thus, a lesion of those systems can lead to bladder manage these patients since these investigations allow
dysfunction: focal lesions (stroke, tumor, traumatic spi- to choose the right treatments and control their effi-
nal cord injury, myelopathies due to cervico-arthrosis, cacy.6-9
spina bifida), disseminated lesions (Parkinson disease,
brain trauma, multiple sclerosis, meningo-encephalitis) Diagnosis and evaluation
and peripheral neuropathies (diabetes mellitus), lead to
various and numerous urinary symptoms. These symp- Neurogenic bladder can lead to permanent urologi-
toms range from overactive bladder with urgency and cal alterations, such as hydronephrosis, reflux, recur-
urge incontinence to underactive bladder with urinary rent urinary tract infections, stones, renal alteration,
or other proprietary information of the Publisher.
retention or difficulties to empty the bladder. These and it always inevitably leads to diminished patient
symptoms, and particularly symptoms secondary to quality of life. Overactive bladder (OAB), combined
overactive detrusor with high bladder pressure and with urgency, frequency, nocturia and urge inconti-
detrusor external sphincter dyssynergia (DESD) with nence, is the most common syndrome, which is some-
Vol. 53 - No. 6 European Journal of Physical and Rehabilitation Medicine 975
not permitted. It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
AMARENCO DIAGNOSIS AND CLINICAL EVALUATION OF NEUROGENIC BLADDER
times also associated with voiding dysfunction and uri- DESD was hypothesized to be an abnormal flexor re-
nary retention. Clinical evaluation is always necessary. sponse of the perineal musculature to bladder contrac-
Urodynamic investigations may contribute to a better tion and considered as a continence reflex exaggerated
understanding of the pathophysiology of these symp- owing to the loss of supraspinal influences.
toms that are generally related to overactive detrusor This incoordination between detrusor smooth muscle
and DESD.10, 11 and external urethral sphincter and/or bladder neck,
induces an obstruction which determines excessive
The different patterns of neurogenic lower urinary tract bladder pressures during voiding and residual volume.
dysfunction Thereby, the risk of recurrent urinary tract infections,
ureteral reflux, hydronephrosis and pyelonephritis, in-
Overactive bladder and voiding dysfunction with a creases.
risk of urinary retention are the most common symptom Discoordination between bladder and urethra during
patterns in neurogenic lower urinary tract dysfunction voiding, determines a weak stream and/or urinary re-
(NLTUD). tention. Urinary flow can be low during all the voiding
Urge incontinence is one of the main symptoms of (tonic dyssynergia) or can be irregularly interrupted by
overactive bladder. Some cases of overactive bladder perineal muscle spasms (clonic dyssynergia). Symp-
can be attributed to specific conditions, such as acute toms are often variable and can be influenced by general
or chronic urinary tract infection, and bladder stones, fatigue, subject position, bladder repletion, concomitant
but most cases result from neurologic dysfunction anorectal dysfunction, urinary tract infection, urinary li-
with inability to suppress detrusor contractions. This thiasis, orthopedic complications, and generally by any
neurogenic detrusor overactivity (NDO) can be due factor inducing spasticity increase.
to suprapontine lesions or spinal cord lesions (above
the lumbosacral level). NDO is likely to be mediated Clinical evaluation
by capsaicin-sensitive C-fiber afferents. In addition to
changes in reflex pathways, it has been demonstrated Urinary tract dysfunction during the course of neu-
that a functional outlet obstruction resulting from de- rogenic bladders requires full clinical evaluation since
trusor sphincter dyssynergia may alter the properties these urinary disorders represent a considerable psy-
of bladder afferent neurons. Decreased afferents due to chosocial burden and a real risk of upper urinary tract
pelvic floor deficiency can lead to involuntary detrusor involvement and kidney disease.
contraction and can be observed in neurogenic patients. A thorough history is always the first step in the eval-
Recently, a role of the urothelium in afferent activation uation of urinary dysfunction in neurogenic population.
has been strongly suggested. It has been demonstrated Onset, duration of complaint, precipitants (position
that the transduction mechanisms can be altered with change, urinary tract infection), frequency, severity,
modification of the activation of sensory afferent fibers quantity, number of pads, constipation, associated dis-
during bladder filling. eases (diabetes, surgeries, obesity), medications (e.g.,
Voiding dysfunction and particularly urinary reten- anticholinergics, calcium channel blockers, diuretics,
tion can be observed in NLUTD. Underactive detrusor sedatives, alpha-agonists, alpha-antagonists) must be
can be one of the mechanisms, especially in peripheral précised.
nervous system lesions (radiculopathies, peripheral Quantitative evaluation of urinary symptoms can be
neuropathies) but in fact the main cause is a detrusor- done by means of specific symptoms scores.
external sphincter dyssynergia (DESD). DESD is char- The 24-hour bladder diary can provide an accurate
acterized by involuntary contractions of the external record of urinary output, average voided volume, fre-
urethral sphincter during an involuntary detrusor con- quency of voiding, and frequency and nature of incon-
or other proprietary information of the Publisher.
traction. It is caused by neurological lesions between tinent episodes, as well as type and volume of fluid in-
the brainstem (pontine micturition center) and the sacral take. Patients are asked to measure their urine output in
spinal cord (sacral micturition center). This is the case a measuring cup during any “normal” 24-hour period
in multiple sclerosis and spinal cord injuries patients. they choose. Since urinary dysfunction can have a ma-
976 European Journal of Physical and Rehabilitation Medicine December 2017
not permitted. It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
DIAGNOSIS AND CLINICAL EVALUATION OF NEUROGENIC BLADDER AMARENCO
jor impact on all aspects of well-being in neurogenic tive predictive value for confirming infection is only
patients with urinary disorders, this impact can be as- 50%.
sessed by using validated condition-specific quality of In all the cases, it is necessary to track down uri-
life instruments (e.g. Qualiveen questionnaire). nary retention. A measure of postvoid residual urine by
Physical examination is necessary to detect contribu- supra-pubic ultrasonography or in-out catheterization
tory factors and any underlying serious medical condi- must be done.
tions. Evaluations should always consider associated When micturitional symptoms are discovered or
urogynecologic alterations (benign prostatic hypertro- spontaneously reported during this minimal evalu-
phy in male, associated stress urinary incontinence in ation, other evaluations must be performed with a
female patients) since these alterations may modify three-day voiding chart, an ultrasound scan of the uri-
pathophysiology of the different symptoms and thera- nary tract, a urine bacteriology, a urodynamic study,
peutic strategies. The sacral dermatomes should be a urinary creatinine clearance, and finally an evalua-
tested by assessing anal tone, perineal sensation and the tion of the impact of urinary symptoms on a quality-
bulbocavernosus reflex. of-life scale (which may be based on the specific and
Postvoid residual (PVR) urine volume is assessed validated Qualiveen Questionnaire in MS and spinal
by catheterizing and measuring residual urine within 5 cord injury). When risk factors are observed, e.g. high
minutes after voiding (or by means of ultrasonography). vesical pressure during the filling phase or during mic-
Numerous and various symptoms can be observed in turition, specific radiologic investigations must be per-
NLUTD. formed (CT-scan, cystourethrography and sometimes
Overactive bladder syndrome characterized by ur- renal scintigraphy when urinary creatinine clearance is
gency, urinary frequency and/or urge incontinence is altered).
very frequent. Obstructive symptoms with voiding dys-
function, urinary retention are also frequently reported. Urodynamic evaluation
Overactive bladder and voiding dysfunction often coex-
ist in many cases. Urodynamic explorations allow a precise evaluation
The clinical presentation of vesicourethral dysfunc- of pathophysiology of urinary dysfunction and of risk
tion is variable over time and there is little correlation factors for urinary tract damage in neurogenic patients
between the clinical and urodynamic symptomatology. with urinary dysfunction, thus helping to plan their
Two factors are often associated with presence and se- optimal management. Indeed, diagnosis of urinary in-
verity of vesicourethral dysfunction: the duration of the continence and more generally of urinary dysfunction,
neurologic disease and the severity of the neurological is complex with intricate pathophysiologic factors.
deficiencies and disabilities. The prevalence of urinary Thus, in many cases, urodynamic investigations are
dysfunction is correlated with the severity of the overall necessary to better understand symptoms pathophysi-
deficiencies especially in MS patients. ology and choose the best therapeutic strategies. But
The first line evaluation is based on simple param- in all the cases, urodynamic must be considered as a
eters. complementary investigation and always interpreted in
A specific questionnaire about voiding must be used conjunction with clinical data and the results of the
in all the patients (frequency, number and easiness of others morphological and/or radiological investiga-
voiding, appraising voiding volume, sensation of com- tions.
plete emptying or not), continence (number and ap- Measurement of the urinary flow rate (uroflowmetry)
praising volume of leakage, use of pads), symptoms of is used to confirm the presence of bladder outlet ob-
urinary tract infection (and associated fever) and ano- struction and more precisely the presence of a DESD.
rectal symptoms (constipation, fecal incontinence). Urinary flow rate is measured with a flowmeter that
or other proprietary information of the Publisher.
Combined rapid tests of urine, ‘‘dipstick’’ test, is measures a quantity of fluid passed per unit time, ex-
advisable for all patients presenting with new bladder pressed in mL/s. Uroflow depends on detrusor contrac-
symptoms. Negative predictive value for ruling out uri- tility and urethra-sphincter resistance. Voided volume
nary tract infection is excellent (0.98%) but the posi- should be greater than 150 mL. Patients are instructed
Vol. 53 - No. 6 European Journal of Physical and Rehabilitation Medicine 977
not permitted. It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
AMARENCO DIAGNOSIS AND CLINICAL EVALUATION OF NEUROGENIC BLADDER
to void normally as in usual conditions, with a comfort- measurement of both the intravesical and intra-abdom-
ably full bladder, which is sometimes difficult in these inal pressure simultaneously. Electronic subtraction
neurogenic patients with neurogenic detrusor overactiv- of the intra-abdominal pressure from the intravesical
ity leading to a reduced bladder capacity. Measurement pressure enables detrusor pressure measurements. In
of residual urine volume (by means of ultrasounds or current practice intra-abdominal pressure is estimated
catheterization) is necessary to properly interpret the from rectal pressure (or vaginal pressure in female).
uroflowmetry results. The precise shape of the flow Urinary tract infection should always be checked be-
curve is decided by detrusor contractility, the presence fore urodynamic investigation. Artificial bladder fill-
of any abdominal straining and by the bladder outlet. ing is used, via a catheter, with sterile water or normal
A normal flow curve is a smooth curve without any saline. In current practice the filling rate is usually 50
rapid changes in amplitude. Rapid changes in flowrate mL/min. Different events must be analyzed during fill-
may evoke detrusor sphincter dyssynergia with lack ing and voiding phases: first sensation of bladder fill-
of urethral sphincter relaxation during micturition and ing (feeling of the bladder filling), first desire to void,
sometimes involuntary flow interruption and abdominal strong desire to void. Increased bladder sensation is
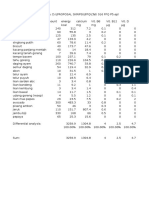
straining (Figure 1). defined as an early first sensation of bladder filling (or
Cystometry is the method used to measure the pres- an early desire to void) and/or an early strong desire to
sure-volume relationships of the bladder. The intravesi- void, which occurs at low bladder volume and which
cal pressure is measured while the bladder is filled, but persists. Reduced bladder sensation is defined as dimin-
this simple technique is not accurate because intravesi- ished sensation throughout bladder filling. This fact is
cal pressure does not represent in all the cases the true always observed in peripheral lesions (lesions of sacral
detrusor pressure: as the bladder is an intra-abdominal roots or plexus injury, peripheral neuropathy). Absent
organ, the intravesical pressure is subjected to changes bladder sensation means that, during filling cystometry,
(during cough, patient movements, …) and not rep- the individual has no bladder sensation. Urgency, dur-
resent the real detrusor pressure. Thus, it is more ap- ing filling cystometry, is a sudden compelling desire to
propriate to use subtracted cystometry which involves void.
Assessment of the detrusor function during filling
cystometry is one of the major goals of the urodynamic
investigation in neurogenic patients with urinary dys-
function. All detrusor activity before the “permission
Upper motor
to void” is defined as “involuntary detrusor activity”.
neuron
lesions
Normal detrusor function is defined as bladder filling
with little or no change in pressure. No involuntary pha-
Sacral sic contractions occur despite provocation (rapid filling,
parasym-
pathetic ice water, postural changes, hand washing). Detrusor
center
overactivity is a urodynamic observation characterized
by involuntary detrusor contractions during the fill-
Lower motor ing phase which may be spontaneous or provoked. In
neuron
lesions central disease (upper motor neuron lesions), there are
certain patterns of detrusor overactivity: phasic detru-
sor overactivity, defined by a characteristic wave form
and may or may not lead to urinary and often observed
Figure 1.—Upper motor neuron lesions (lesions of neural pathway in spinal cord lesions; terminal detrusor overactivity,
above the anterior horn cell of the spinal cord): lead to overactive de- defined as a single, involuntary detrusor contraction,
or other proprietary information of the Publisher.
trusor with uninhibited detrusor contraction associated with detrusor
sphincter dyssynergia and high detrusor pressure during micturition (top occurring at cystometric capacity, which cannot be sup-
curve); lower motor neuron lesions (lesions are either in the anterior pressed and results in incontinence usually resulting in
horn cell or distal to the anterior horn cell): lead to underactive detrusor
with high compliance, decreased filling sensation and absence of detru- bladder emptying (voiding) and often observed in corti-
sor contraction (lower curve). cal lesions (stroke, tumor).
978 European Journal of Physical and Rehabilitation Medicine December 2017
not permitted. It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
DIAGNOSIS AND CLINICAL EVALUATION OF NEUROGENIC BLADDER AMARENCO
Bladder compliance describes the relationship be- stenosis, prostatic hypertrophy). However, recognizing
tween change in bladder volume and change in detrusor DESD is not the main problem in the management of
pressure. Compliance (C) is calculated by dividing the neurogenic bladder. The real challenge is not to prove
volume change (∆V) by the change in detrusor pres- absolutely DESD with urodynamic tests, but to evalu-
sure (∆pdet) during any change in bladder volume (C= ate its consequences, especially high detrusor pressure
∆V/∆pdet). Cystometric capacity is the bladder volume during storage and/or micturition, which can determine
at the end of the filling cystometry, when “permission to bladder or renal complications.
void” is usually given. Alteration of bladder compliance
can be observed in congenital lesions (spina bifida) or in Conclusions
spinal cord lesions.
Urodynamic investigations allow the diagnosis of Urinary incontinence, overactive bladder and more
DESD in neurogenic patients with voiding dysfunc- generally urinary dysfunction is a major clinical prob-
tion. The classic test to recognize DESD is combined lem and a significant cause of disability in neurogenic
cystometry and external sphincter electromyography. patients. Indeed, the bothersome symptom of urinary
Meanwhile, DESD can be suggested if a uroflowmetry dysfunction may adversely affect social relationships
examination is possible to perform, when an interrupt- and activities in these patients. Since many causes of
ed urine flow with residual volume observed. urinary dysfunction are described, a thorough evalua-
Cystometry may be recorded with a rectal pres- tion including history, clinical examination and evalua-
sure measurement to analyze abdominal pressure si- tion of quality of life is necessary.
multaneously with bladder pressure to eliminate ar- Clinical evaluation is still the main step in the man-
tifacts due to abdominal muscle contraction. Indeed, agement of urinary disorders in neurogenic patients.
the diagnosis of DESD requires a detrusor contrac- Questionnaires are highly recommended and signifi-
tion. However, many patients are unable to initi- cantly improve symptoms comprehension and thera-
ate such a contraction, particularly in severe DESD. peutic decision. Investigations, biological, radiological
Furthermore, in moderate DESD, some patients will or urodynamic are indicated in all symptomatic patients.
strain to try to urinate, which causes a simultaneous Specific algorithms can be used in order to track down
increase in sphincter activity, bladder and rectal pres- any complications and help to a better follow-up of the
sure. Sphincter dyssynergia is diagnosed by increased patients.12, 13
EMG activity during an involuntary detrusor contrac-
tion. DESD is further suggested by a high voiding
References
pressure, persistent elevated MUP (maximal urethral
pressure). Smooth sphincter dyssynergia is more dif- 1. Panicker JN, Fowler CJ, Kessler TM. Lower urinary tract dysfunc-
ficult to confirm. Video imaging techniques allow the tion in the neurological patient: clinical assessment and management.
Lancet Neurol 2015;14:720-32.
diagnosis of bladder neck dyssynergia. Fluoroscopic 2. Chan YY, Sandlin SK, Kurzrock EA. Urological Outcomes of
imaging during an involuntary contraction objectifies Myelomeningocele and Lipomeningocele. Curr Urol Rep 2017;
18:35.
persistent narrowing of the internal sphincter and /or 3. Wyndaele JJ. The management of neurogenic lower urinary tract dys-
of the bladder neck. function after spinal cord injury. Nat Rev Urol 2016;13:705-14.
4. Sturm RM, Cheng EY. The Management of the Pediatric Neurogenic
When the micturition is possible, combined uroflow Bladder. Curr Bladder Dysfunct Rep 2016;11:225-33.
and sphincter EMG (possibly with a single rectal pres- 5. Tudor KI, Sakakibara R, Panicker JN. Neurogenic lower uri-
nary tract dysfunction: evaluation and management. J Neurol
sure record) allow DESD screening. 2016;263:2555-64.
In fact, a very common and important question, is 6. Drake MJ, Apostolidis A, Cocci A, Emmanuel A, Gajewski JB, Har-
rison SC, et al. Neurogenic lower urinary tract dysfunction: Clinical
whether dyssynergia can be diagnosed in the absence of management recommendations of the Neurologic Incontinence com-
a bladder contraction. Even if the DESD rigorous defi- mittee of the fifth International Consultation on Incontinence 2013.
or other proprietary information of the Publisher.
Neurourol Urodyn 2016;35:657-65.
nition is not applicable, we can consider that DESD is 7. Phe V, Chartier-Kastler E, Panicker JN. Management of neuro-
the only mechanism of urinary retention in a neurogenic genic bladder in patients with multiple sclerosis. Nat Rev Urol
2016;13:275-88.
patient who complains of overactive bladder without 8. Lee B, Featherstone N, Nagappan P, McCarthy L, O’Toole S.
bladder neck or urethral organic obstruction (urethral British Association of Paediatric Urologists consensus statement
Vol. 53 - No. 6 European Journal of Physical and Rehabilitation Medicine 979
not permitted. It is not permitted to remove, cover, overlay, obscure, block, or change any copyright notices or terms of use which the Publisher may post on the Article. It is not permitted to frame or use framing techniques to enclose any trademark, log
means which may allow access to the Article. The use of all or any part of the Article for any Commercial Use is not permitted. The creation of derivative works from the Article is not permitted. The production of reprints for personal or commercial use i
This document is protected by international copyright laws. No additional reproduction is authorized. It is permitted for personal use to download and save only one file and print only one copy of this Article. It is not permitted to make additional copies
(either sporadically or systematically, either printed or electronic) of the Article for any purpose. It is not permitted to distribute the electronic copy of the article through online internet and/or intranet file sharing systems, electronic mailing or any other
©
COPYRIGHT 2017 EDIZIONI MINERVA MEDICA
AMARENCO DIAGNOSIS AND CLINICAL EVALUATION OF NEUROGENIC BLADDER
on the management of the neuropathic bladder. J Pediatr Urol G. Diagnosis and therapy for neurogenic bladder dysfunctions in
2016;12:76-87. multiple sclerosis patients. Neurol Sci 2008;29:S352-355.
9. Stoffel JT. Detrusor sphincter dyssynergia: a review of physi- 12. De Ridder D, Vermeulen C, De Smet E, Van Poppel H, Ketelaer P,
ology, diagnosis, and treatment strategies. Transl Androl Urol Baert L, et al. Clinical assessment of pelvic floor dysfunction in mul-
2016;5:127-35. tiple sclerosis: urodynamic and neurological correlates. Neurourol
10. Allio BA, Peterson AC. Urodynamic and physiologic patterns associ- Urodyn 1998;17:537-42.
ated with the common causes of neurogenic bladder in adults. Transl 13. Fowler CJ, Panicker JN, Drake M, Harris C, Harrison SC, Kirby M,
Androl Urol 2016;5:31-8. et al. A UK consensus on the management of the bladder in multiple
11. Del Popolo G, Panariello G, Del Corso F, De Scisciolo G, Lombardi sclerosis. J Neurol Neurosurg Psychiatr 2009;80:470-7.
Conflicts of interest.—The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Article first published online: October 25, 2017. - Manuscript accepted: October 25, 2017. - Manuscript received: September 17, 2017.
or other proprietary information of the Publisher.
980 European Journal of Physical and Rehabilitation Medicine December 2017
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Business Model Canvas TemplateDocument5 pagesBusiness Model Canvas TemplateAsraihan Raihan100% (1)
- Queen'S University Midterm Examination Department of EconomicsDocument7 pagesQueen'S University Midterm Examination Department of EconomicsAsif Ahmed NeloyNo ratings yet
- 20 Neurogenic-LUTD LR PDFDocument64 pages20 Neurogenic-LUTD LR PDFItri SyamdiahNo ratings yet
- JNC 8 Guideline Algorithm for Treating HypertensionDocument2 pagesJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- Eberting2014 Article PathophysiologicTreatmentApproDocument12 pagesEberting2014 Article PathophysiologicTreatmentApproFadhilannisaNo ratings yet
- Samuelsson 2016Document18 pagesSamuelsson 2016FadhilannisaNo ratings yet
- Leprosy Diagnosis and TreatmentDocument23 pagesLeprosy Diagnosis and TreatmentFadhilannisaNo ratings yet
- Eberting2014 Article PathophysiologicTreatmentApproDocument12 pagesEberting2014 Article PathophysiologicTreatmentApproFadhilannisaNo ratings yet
- Factors Affecting The Age in Normal Menopause and Frequency of Menopausal Symptoms in Northern IranDocument7 pagesFactors Affecting The Age in Normal Menopause and Frequency of Menopausal Symptoms in Northern IranFadhilannisaNo ratings yet
- Leprosy Diagnosis and TreatmentDocument23 pagesLeprosy Diagnosis and TreatmentFadhilannisaNo ratings yet
- Laryngopharyngeal Reflux and Functional Laryngeal Disorder: Perspective and Common Practice of The General GastroenterologistDocument9 pagesLaryngopharyngeal Reflux and Functional Laryngeal Disorder: Perspective and Common Practice of The General GastroenterologistKenzi A HasyaputraNo ratings yet
- Safety Product For PregnancyDocument3 pagesSafety Product For PregnancyneonitesNo ratings yet
- International Variability of Ages at Menarche and Menopause: Patterns and Main DeterminantsDocument20 pagesInternational Variability of Ages at Menarche and Menopause: Patterns and Main DeterminantsFadhilannisaNo ratings yet
- Laryngopharyngeal Reflux Disease - LPRD: Professional PaperDocument4 pagesLaryngopharyngeal Reflux Disease - LPRD: Professional PaperAndi Tiara S. AdamNo ratings yet
- Long-Termcomplications Oftheneurogenic Bladder: Unwanaobong Nseyo,, Yahir Santiago-LastraDocument12 pagesLong-Termcomplications Oftheneurogenic Bladder: Unwanaobong Nseyo,, Yahir Santiago-LastraFadhilannisaNo ratings yet
- Masas Cervicales AAOHNSDocument30 pagesMasas Cervicales AAOHNSchwbaccaNo ratings yet
- Rapid Sequence InductionDocument8 pagesRapid Sequence InductionAngela Mitchelle NyanganNo ratings yet
- Occupational Stress and Cardiovascular Risk Factors in High-Ranking Government Officials and Office WorkersDocument7 pagesOccupational Stress and Cardiovascular Risk Factors in High-Ranking Government Officials and Office WorkersFadhilannisaNo ratings yet
- Pinto 2015Document15 pagesPinto 2015FadhilannisaNo ratings yet
- TetanusreviewToxins2012Document12 pagesTetanusreviewToxins2012FadhilannisaNo ratings yet
- Ijms 16 18580 PDFDocument21 pagesIjms 16 18580 PDFItri SyamdiahNo ratings yet
- Comprehensive Geriatric Assessment: British Journal of Hospital Medicine (London, England: 2005) August 2014Document5 pagesComprehensive Geriatric Assessment: British Journal of Hospital Medicine (London, England: 2005) August 2014FadhilannisaNo ratings yet
- Aging, Disability and Frailty: Getting Older, Facts About A Biological ProcessDocument6 pagesAging, Disability and Frailty: Getting Older, Facts About A Biological ProcessFadhilannisaNo ratings yet
- Conjunctivitis PPP UnlockedDocument53 pagesConjunctivitis PPP UnlockedFadhilannisaNo ratings yet
- Comprehensive Geriatric Assessment: British Journal of Hospital Medicine (London, England: 2005) August 2014Document5 pagesComprehensive Geriatric Assessment: British Journal of Hospital Medicine (London, England: 2005) August 2014FadhilannisaNo ratings yet
- The Rate of Metabolism Slows Dow Age Due To A Decrease in Lean Body Mass and Increasingly Sedentary LifestyleDocument1 pageThe Rate of Metabolism Slows Dow Age Due To A Decrease in Lean Body Mass and Increasingly Sedentary LifestyleFadhilannisaNo ratings yet
- Tati 016 FFQ P5Document1 pageTati 016 FFQ P5FadhilannisaNo ratings yet
- Lymphedema: Patient InformationDocument26 pagesLymphedema: Patient InformationFadhilannisaNo ratings yet
- History of DentistryDocument24 pagesHistory of DentistryEzhilarasi INo ratings yet
- VW Crafter 2f Component Locations EngDocument118 pagesVW Crafter 2f Component Locations EngHugo Emilio Garcia Gonzalez100% (2)
- An Engineer's Guide To Designing With Precision Amplifiers: E-BookDocument60 pagesAn Engineer's Guide To Designing With Precision Amplifiers: E-BookIan ChegeNo ratings yet
- On The Art of Fighting - A Humanist Translation of Fiore Dei Liberi's Flower of Battle Owned by Leonello D'EsteDocument37 pagesOn The Art of Fighting - A Humanist Translation of Fiore Dei Liberi's Flower of Battle Owned by Leonello D'EsteHunterSJNo ratings yet
- Wma11 01 Que 20221011Document28 pagesWma11 01 Que 20221011Maks LubasNo ratings yet
- RTR - Nonmetallic Pipng ProcedureDocument16 pagesRTR - Nonmetallic Pipng Proceduremoytabura96100% (1)
- Letter of Request For Brgy. ProfileDocument2 pagesLetter of Request For Brgy. ProfileRhea Mae MacabodbodNo ratings yet
- Oakham Surgery New Patient FormDocument7 pagesOakham Surgery New Patient FormTrần Thanh ThảoNo ratings yet
- Way Back To The BibleDocument19 pagesWay Back To The BiblePearlCladelLapidezNo ratings yet
- Eco 121 Set 2 Fundamentals of EconomicsDocument3 pagesEco 121 Set 2 Fundamentals of EconomicsShadreck CharlesNo ratings yet
- The University of QueenslandDocument2 pagesThe University of Queenslandimmanuel nauk elokpereNo ratings yet
- THICKWALL CYLINDERS AND PRESS FITSDocument10 pagesTHICKWALL CYLINDERS AND PRESS FITSankitaNo ratings yet
- SF-2012AH-QG User' S ManualDocument61 pagesSF-2012AH-QG User' S Manualkamal hasan0% (1)
- Biotensegrity and Myofascial Chains A Global Approach To An Integrated Kinetic ChainDocument8 pagesBiotensegrity and Myofascial Chains A Global Approach To An Integrated Kinetic ChainMohamed ElMeligieNo ratings yet
- Spelling Bee Word ListDocument26 pagesSpelling Bee Word Listsan_6303No ratings yet
- Analyzing Historical DocumentDocument4 pagesAnalyzing Historical DocumentChristine Joy VillasisNo ratings yet
- Intro To Rizal LawDocument61 pagesIntro To Rizal Lawnicachavez030No ratings yet
- 7306 31980 1 PBDocument10 pages7306 31980 1 PBRaihan Aditiya JuniorNo ratings yet
- Probability and Statistics. ASSIGNMENT 2Document5 pagesProbability and Statistics. ASSIGNMENT 2ByhiswillNo ratings yet
- Institute of Graduate Studies (Igs)Document46 pagesInstitute of Graduate Studies (Igs)Syara Shazanna ZulkifliNo ratings yet
- 14 Ways To Acquire KnowledgeDocument4 pages14 Ways To Acquire KnowledgeRenato MiguelNo ratings yet
- Growatt Warranty Procedure - 07-09-2020Document9 pagesGrowatt Warranty Procedure - 07-09-2020Design TeamNo ratings yet
- Form 4 Biology Chapter OverviewDocument21 pagesForm 4 Biology Chapter OverviewKar KuanNo ratings yet
- Open University of Tanzania Term PaperDocument7 pagesOpen University of Tanzania Term Paperafmzfmeeavndqe100% (1)
- Imeko WC 2012 TC21 O10Document5 pagesImeko WC 2012 TC21 O10mcastillogzNo ratings yet
- Vessel and Conveyors - VPDDocument4 pagesVessel and Conveyors - VPDAntonio Mizraim Magallon SantanaNo ratings yet
- Grade 7 Lesson: Module 4 - Acids and BasesDocument3 pagesGrade 7 Lesson: Module 4 - Acids and BasesJoedelyn Wagas100% (4)
- Stress Management Towards Employees in Reliance Life Insurance SureshDocument90 pagesStress Management Towards Employees in Reliance Life Insurance SureshSuresh Babu Reddy100% (3)