Professional Documents
Culture Documents
F.05 Approach To Menstrual Abnormalities and Menstrual Pain (Dr. Lucas) (04-29-19)
Uploaded by
Djan Kurvie ValencerinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
F.05 Approach To Menstrual Abnormalities and Menstrual Pain (Dr. Lucas) (04-29-19)
Uploaded by
Djan Kurvie ValencerinaCopyright:
Available Formats
F.
05 APPROACH TO MENSTRUAL ABNORMALITIES Copper IUD
AND MENSTRUAL PAIN o Increases menstrual flow
Dr. Lucas | April 29, 2019 o Increases incidence of intermenstrual bleeding, reasons
why this is not really used
Levonorgestrel IUD
OUTLINE
o Typically cause an initial period of irregular spotting or
I. History
bleeding, followed by a gradual decrease in menstrual
II. Physical Examination
flow and possible amenorrhea.
III. FIGO Classification of AUB
2. RISK FACTORS FOR ENDOMETRIAL CANCER
I. HISTORY Any agent/factor that rises the level or time of
The relevant medical history in non-pregnant reproductive- exposure to estrogen is a risk factor
age women with abnormal uterine bleeding (AUB) includes One of the most common symptom of endometrial cancer
the following: is Abnormal uterine bleeding
o Older age - >35 years old
A. GENERAL HISTORY o Early menarche – average menarche in the Philippines is
1. GYNECOLOGIC AND OBSTETRIC HISTORY around 10 years old, if she has menarche earlier that
a. MENSTRUAL HISTORY that then it is a risk factor
Ask for the patient’s age at menarche (first menstruation) o Late menopause – Average is 49 years old
Ask the patient to describe her first menses as to how many o Nulliparity – never been pregnant
days? How many pads did she use? Were there any associated o Unopposed estrogen (Obesity, PCOS, HRT)
signs and symptoms? o Chronic Tamoxifen use – Tamoxifen is stimulatory to the
Also ask the patient to describe the subsequent menses endometrial lining though inhibitory to the breast that’s
The menarche could be the basis of how the patient’s menses why it is a treatment for breast cancer.
would be, the regularity of the menses afterwards. If a patient with breast cancer that is on tamoxifen
Subsequent menses: suddenly develops abnormal uterine bleeding it is
o Interval then an indication for diagnostic curettage
Ask if the patient’s menses is monthly or regular, if o Previous pelvic irradiation
irregular, ask why o Hypertension, Diabetes mellitus
More often than not patients would say it’s What do they have in common? They are all exposed to
irregular because it does not fall on the same day estrogen for a longer period
every month o If a patient can’t get pregnant she is exposed to
If for example, her last menses was January 1 st and unopposed estrogen
her next is February 8, it is still considered regular
because there is a normal interval for the interval B. OTHER MEDICAL HISTORY
It is then your responsibility to educate your 1. BLEEDING DISORDERS
patient Symptoms, risk factors (anticoagulant therapy,
o LMP thrombocytopenia, liver or renal disease), or a family history
1st day of the patient’s last menses of a bleeding disorder.
Women with a hematologic malignancy may present with AUB
b. SEXUAL HISTORY especially with the adolescent age group
This information may help determine the patient's risk for o 3.6 per 1000 in one study
pregnancy and STI. o Associated symptoms include fatigue, dyspnea or SOB,
o Could present as abnormal vaginal bleeding bruising or petechiae, fever
c. HISTORY OF OBSTETRIC OR GYNECOLOGIC SURGERY
2. THYROID DISEASE
A prior cesarean delivery, particularly multiple prior
Symptoms or family history of thyroid disease
abdominal deliveries, raises the possibility that cesarean
Associated with heavy menstrual bleeding or oligomenorrhea
scar defect may be responsible for AUB.
Hypothyroidism causes heavy menstrual bleeding because of
A prior myomectomy raises the possibility that uterine
an increase TSH
fibroids are responsible for AUB.
READING ASSIGNMENT: In hypothyroidism, gonadotropin
o The risk of recurrence from uterine fibroids are quite
levels are usually normal. TSH, which is markedly increased
high
in hypothyroidism, has a small FSH- and LH-like effect
d. CONTRACEPTIVE HISTORY because of the shared alpha subunit. The mid-cycle FSH and
Estrogen-progestin LH surge may thus be blunted or absent. Menorrhagia is a
o May develop unscheduled bleeding frequent complaint and is probably due to estrogen
o Used in the management of AUB but misuse of this could breakthrough bleeding secondary to anovulation, which is
also lead to AUB so it is important to ask how does she frequent in severe hypothyroidism
take the pills Hyperthyroidism causes oligomenorrhea or amenorrhea
Progestin only
o Irregular uterine bleeding or amenorrhea CELIAC DISEASE
o Known for spotting, minimal vaginal bleeding May develop secondary amenorrhea.
MED 1 | 1 of 7 BOLEYLEY, CAI, ROBANCHO
MEDICATIONS B. CURRENT UTERINE BLEEDING
Anticoagulants - heavy or prolonged uterine bleeding The presence and volume of bleeding from the cervical
A variety of medications can cause hyperprolactinemia os should be noted.
resulting in oligomenorrhea or amenorrhea Blood or blood clots in the vaginal vault should be noted.
Patients who present with a complaint of heavy vaginal
bleeding should be assessed for acute bleeding.
Patients who are hemodynamically unstable or who have
copious, ongoing blood flow form the uterus or other genital
tract site should be evaluated and managed in an
urgent care facility.
C. ADDITIONAL QUESTIONS
Were there precipitating factors, such as trauma (such as
post-coital lacerations) Upper picture: Endocervical Polyp that causes bleeding
o Suggests a vaginal or cervical, rather than uterine Lower picture: Post-coital bleeding; the cervix is edematous and
source of bleeding. friable; it easily bleeds after coitus
Are there any associated symptoms?
o Lower abdominal pain C. SIZE AND CONTOUR OF THE UTERUS
o Fever An enlarged uterus may be due to pregnancy, uterine
o Vaginal discharge leiomyomas, adenomyosis, or uterine malignancy.
Could indicate infection such as pelvic Limited uterine mobility (difficulty in moving the uterus)
inflammatory disease and endometritis should be noted, if present, this finding suggests that pelvic
o Dysmenorrhea, dyspareunia, or infertility suggests adhesions (especially if the patient has undergone recent
endometriosis and/or adenomyosis pelvic surgery or previous infection or PID) or a pelvic mass
Endometriosis manifests as increasing severity of is present.
dysmenorrhea Pelvic adhesions may be due to prior infections, surgery, or
o Changes in bladder or bowel function suggest endometriosis, and also may impact surgical planning if
extrauterine bleeding or a mass effect from an enlarged surgical treatment is indicated.
fibroid uterus or a neoplasm. A boggy, globular, tender uterus is typical of
o Galactorrhea, heat or cold intolerance, hirsutism, or hot adenomyosis.
flashes suggest an endocrinologic issue. Uterine tenderness (pain illicited when the uterus is
Has there been a recent illness, stress, excessive exercise, or palpated) is present in women with pelvic inflammatory
possible eating disorder? disease (PID), but is not consistently found in those with
o Suggests hypothalamic dysfunction chronic endometritis.
II. PHYSICAL EXAMINATION
A. VITAL SIGNS
Should be assessed and a complete pelvic exam should be
performed with a particular focus on:
o Potential sites of bleeding from the vulva, vagina,
cervix, urethra, anus, or perineum.
o Any abnormal findings along the genital tract (eg.
Mass, laceration, ulceration, friable area, vaginal or
cervical discharge, foreign body).
Initially the foreign body would be the cause of
infection and abnormal discharge but later on
because of necrosis at the tissue surrounding the Bimanual Examination: To examine the uterus and adnexa (ovary
foreign body would then result to vaginal bleeding. and fallopian tubes)
MED 1 | 2 of 7 BOLEYLEY, CAI, ROBANCHO
D. GENERAL EXAMINATION Mainly, the term DUB has been used as a
Should be performed to look for signs of systemic illness, diagnosis of exclusion in women with AUB in
such as fever, ecchymoses, an enlarged thyroid gland, or whom the structural pathology has not been
evidence of hyperandrogenism which is seen in Polycystic identified.
ovarian syndrome (PCOS) (hirsutism, acne, clitoromegaly, or
male pattern balding). A. NORMAL MENSES
Acanthosis nigricans may be seen in women with PCOS NOTE: Refer to table at the end for summary
o Also seen in diabetics
Galactorrhea (bilateral milky nipple discharge) suggests the 1. FREQUENCY
presence of hyperprolactinemia. Interval
24-38 days
Oligomenorrhea – more than 38 days
Regularity - variation ≤ 7 to 9 days
NMT (mean variation) 7-9 days difference between the
shortest to longest cycles; cycle length is the number of days
from the 1st day of one menstrual cycle to the 1st day of the
next.
For some young girls who have occasional or frequent long
cycles, typically, but not always, the cycle length evolves
spontaneously to fit norms. For others, such an evolution may
not occur.
2. DURATION
≤ 8 days
Upper picture (left): Hyperthyroidism usually coupled with a Number of days of bleeding in a single menstrual period.
complaint of oligomenorrhea There are no specific clinical entities that are associated with
Upper picture (right): Galactorrhea reduced duration below 4 days, with the exception of
Lower picture: Hirsutism and acne associated with Polycystic amenorrhea.
ovarian syndrome
3. QUANTITY
NOTE: Refer to table at the end for evaluation of abnormal
Volume
uterine bleeding in non-pregnant reproductive-age women.
o Clinical definition is subjective and defined as a volume
III. FIGO CLASSIFICATION OF AUB that does not interfere with a woman's physical, social,
Based on concerns about the confusing nature of AUB emotional, and/or material quality of life.
terminology raised by a multinational group of experts in Research definition is ≤ 80 ml vaginal “blood” loss per
gynecology, an international workshop was convened in cycle.
Washington, DC in 2005. Normal amount of blood is just 35mL.
The workshop addressed the most obvious and confusing If greater than 80mL = heavy
issues regarding AUB terminology, definitions, and 1 regular pad is about 60mL if fully soaked
classifications. Light if she is only able to use 1 pad for the entire day
As a result of this workshop, an international working group
was set up with oversight from the International Federation
of Gynecology and obstetrics via a Menstrual Disorders
Working Group (FIGO MDWG), and since 2012, this working
group has become a standing committee of FIGO, the FIGO
Menstrual Disorders Committee (MDC).
The process of developing new definitions and
terminology has included:
o Identifying terms describing AUB symptoms that should
no longer be used because they are confusing and
poorly defined
o Among the most commonly used terms were
menorrhagia and metrorrhagia.
MENORRHAGIA METRORRHAGIA
Heavy menstrual bleeding at REGULAR heavy menstrual
IRREGULAR intervals bleeding
o The experts group also recommended abandonment B. ABNORMAL UTERINE BLEEDING
of the term dysfunctional uterine bleeding (DUB), AUB is the overarching term used to describe any
which is another poorly defined term. symptomatic variation from normal menstruation and
This term has been used with variability as both also includes intermenstrual bleeding.
a vague symptom and/or a poorly defined This term covers the full range of symptoms of abnormal
diagnosis. bleeding.
MED 1 | 3 of 7 BOLEYLEY, CAI, ROBANCHO
1. ACUTE AUB 1. AUB-P (ENDOMETRIAL POLYPS)
An episode of uterine bleeding in a woman of reproductive Polyps are localized epithelial tumors that include those in
age, who is not pregnant, that is of sufficient quantity to the endometrial cavity and the cervical canal.
require immediate intervention to prevent further Overgrowth of endometrial tissue, containing glands, stroma
blood loss. and blood vessels, covered with epithelium.
Difference between acute and chronic would be the urgency Most commonly found in reproductive age women, rare
of the situation before menarche.
Estrogen stimulation is thought to play a key role in its
2. CHRONIC AUB
development.
Bleeding from the uterine body present for at least the
Increases overall surface area of the endometrium leading to
majority of the past 6 months.
heavier blood loss
Does not need urgent intervention
More friable and edematous compared to leiomyomas
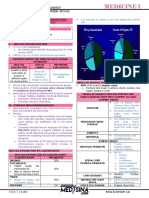
C. PALM-COIEN CLASSIFICATION
2. AUB-A (ADENOMYOSIS)
Adenomyosis is the presence of endometrial-type glands
and stroma within the myometrium, a diagnosis that
traditionally requires a histopathologic diagnosis.
However, it is now apparent that transvaginal ultrasound
or MRI may be used to make a clinical diagnosis of
adenomyosis.
The presence of ectopic endometrial tissue leads to
hypertrophy of surrounding epithelium.
Endometriosis if the ectopic endometrial tissue is seen outside
of the uterus (ovary, fallopian tube, posterior cul de sac)
If ectopic tissue seen inside the myometrial tissue –
adenomyosis
If localized at one area it is called adenomyoma
Peak incidence in the 5th decade.
Multiparity: most significant risk factor, but any process
that allows penetration of endometrial glands and stroma past
the basalis layer is thought to contribute (dilatation and
curettage, cesarean delivery, abortion).
It is a result of altered uterine contractility and
associated with profound dysmenorrhea.
PALM COEIN The ectopic endometrial tissue is interspersed between the
Non-Structural causes of muscle fibers allowing it to contract leading to more blood loss
Structural causes of AUB
AUB
Measurable visually using 3. AUB-L (LEIOMYOMAS)
AKA myomas or uterine fibroids are benign neoplasms of
imaging techniques Not defined by imaging or
and/or with histopathology smooth muscle
histopathology Leiomyomas vs Adenomyosis:
o Leiomyomas – smooth muscle within the myometrium
o Adenomyosis – endometrial-type glands and stroma
within the myometrium
While the diagnosis of leiomyomas can be suggested by pelvic
exam, pelvic imaging is necessary for a more accurate
diagnosis.
Pathogenesis is thought to initiate from myometrial injury
leading to cellular proliferation, decreased apoptosis and
increased production of extracellular matrix.
Causes AUB by: Intracavitary, submucous increase of overall
surface area of endometrium, altering uterine contractility.
Locations: (nice to know only)
o Submucous – most associated with heavier menstrual
bleeding
o Intramural and subserous, “other” or outside the
endometrial cavity
o Hybrid (transmural)
Like polyps, increases overall surface area of the
endometrium and since myometrium is involved then it alters
contractility leading to bleeding
MED 1 | 4 of 7 BOLEYLEY, CAI, ROBANCHO
FIGO LEIOMYOMA CLASSIFICATION (BASED ON 5. AUB-C (COAGULOPATHY)
LOCATION) Coagulopathy encompass the spectrum of systemic disorders
0 Pedunculated Intracavity of hemostasis.
Submucosal: Such disorders are identifiable in up to 24% of women with
1 <50% intramural
Primary Type the symptom of heavy menstrual bleeding, most
2 >50% Intramural
Contacts endometrium, 100% commonly mild Von Willebrand disease.
3 The approach to identifying these patients starts with
intramural
Other: 4 Intramural structured history to assess symptoms or risk factors for
Secondary 5 Subserosal, >50% intramural coagulation disorders.
Type 6 Subserosal, <50% intramural Confirmation requires lab testing.
7 Subserosal pedunculated Platelet disorders, hemophilia, leukemia, severe
sepsis, ITP, hypersplenism.
8 Others (Specify if cervical, parasitic)
Routine screening indicated for:
Two numbers are listed separated
o Adolescent with prolonged menses beginning at
by hyphen
menarche.
Hybrid By convention, the first refers to
o Adults with heavy menstrual bleeding with clinical signs
Leiomyomas the relationship with
such as bleeding gums, epistaxis or ecchymosis.
(impacts endometrium while 2nd refers to
2-5
both the relationship with serosa,
endometrium submuscosal, and serosal, each
and Serosa) less than half the diameter in the
endometrium and peritoneal
cavities
NOTE: No need to Memorize! Just know the hierarchy
6. AUB-O (OVULATORY DYSFUNCTION)
Occurs when a woman is not ovulating, has infrequent
ovulation, or especially in the late reproductive years (when
Written as: E.g. AUB-Lsm-1 – Submucosal under 1 wherein it patient transitions from reproductive age to menopause),
is <50% intramural experiences luteal out-of-phase events.
Alterations in neuroendocrine function.
4. AUB-M (MALIGNANCY AND HYPERPLASIA)
A luteal out-of-phase event occurs when there is early,
Endometrial hyperplasia with cytological atypia and
luteal phase recruitment of a follicle that then matures
carcinoma, including endometrial stromal sarcomas, are
precociously, resulting in high circulating levels of estradiol
epithelial neoplasms of the endometrium that are usually
making the endometrium thick leading to heavy menses and
diagnosed with transcervical endometrial sampling.
associated increased menstrual volume.
Diagnosed after a diagnostic curettage
Proliferating endometrium may outgrow its blood supply
Endometrial hyperplasia has a risk of turning into a
leading to various degrees of necrosis.
malignancy
o Pattern is irregular heavy bleeding; heavy-spotting-
Unopposed estrogen stimulation of the endometrium:
heavy again
o Obesity - increased estrone levels due to peripheral
o There is no normal uniform sloughing off of the
conversion by aromatase in adipose tissue.
endometrium
o Impaired ovulation, absence of progesterone withdrawal
Occurs in extremes of reproductive life (1st few years after
- sustained estrogen production and endometrial
menarche, perimenopause).
stimulation.
Adolescent - cause of anovulation is immaturity of HPO axis,
o Lynch syndrome (hereditary non-polyposis colorectal
failure of positive feedback of estradiol to cause LH surge.
cancer) - 40-50% risk for endometrial cancer;
o Allows 2-3 years of adjustment for the HPO axis to
therefore, immediately referred
mature
o Estrogen producing ovarian tumors (granulosa cell
o If still irregular or oligomenorrhea has become heavy
tumors).
MED 1 | 5 of 7 BOLEYLEY, CAI, ROBANCHO
menstrual bleeding after 2-3 years, patient should seek PGF2 alpha
for further consultation o Promotes uterine contractility.
o Anovulation is caused by immaturity of HPO axis which o Together with formation of the platelet plug are the
causes failure of positive feedback of estradiol to cause primary line of defense to excessive bleeding during
LH surge which is an important prerequisite to ovulation normal menses.
o No ovulation = no production of progesterone Excessive production of prostacyclin - Vasodilatory
Perimenopausal - lack of synchronization between prostaglandin, opposes platelet adhesion.
components of the HPO axis as the woman approaches
9. AUB-N (NOT OTHERWISE CLASSIFIED)
ovarian decline.
These have been poorly defined, inadequately
Other causes of anovulation:
examined, and/or are extremely rare.
o PCOS because of the hyperandrogenism
Wastebasket
o Hypothalamic dysfunction – may be caused by Bulimic,
E.g. - arteriovenous malformation and AUB in the context of
anorexic, extreme exercise, stress
a uterine isthmocele (there would be necrosis surrounding the
o Abnormalities in other hormones like TSH, prolactin,
isthmocele that would affect the shedding of the endometrium
cortisol
lining producing heavy menstrual bleeding) secondary to a
7. AUB-I (IATROGENIC) lower segment cesarean section.
AUB due to medical devices, mainly intrauterine Foreign body
contraception systems, or pharmaceutical therapy. Trauma
Medications that can cause AUB include:
D. DOCUMENTATION
o Gonadal steroids (estrogen, progestins, androgens)
Following appropriate investigation, a woman with AUB
o Gonadal steroid-related therapy (GnRH analogues,
symptoms may be found to have 1 or multiple potential
aromatase inhibitors, selective estrogen receptor
causes or contributors. The FIGO systems have been
modulators, selective progesterone receptor
designed to allow both categorization and
modulators)
documentation.
Usually given to patients with adenomyosis,
The full documentation might be considered to be
endometriosis to preserve their fertility
cumbersome, abbreviating the notation to only the positive
They do not have menses while on these
findings can be considered.
medications
o For example, a patient with adenomyosis, irregular
o Anticoagulants
bleeding, and a type 6 leiomyoma could be recorded as
o Systemic agents that can contribute to disorders of
AUB-A1, -Lo1, -O
ovulation, for example, those that interfere with
o First write the OB score then the day of cycle
dopamine metabolism or cause hyperprolactinemia
o The 0 subscript would mean she does not have that
(Refer to Table 2 on Page 1 for drugs that cause
pathology
Hyperprolactinemia)
o 1 would mean that it is the culprit
o IUD devices, such may be inert, are frequently
o It is written this way because a patient could have
composites of copper and plastic, or take the form of a
multiple pathologies
local progesterone-releasing system.
o Alternative way of writing it would be if multiple
o OCP WITH antibiotics and anticonvulsants
pathologies: AUB-P, AUB-M
Cephalosporins, chloramphenicol, macrolide,
o Although the right way of documenting would be the
barbiturates.
image below
Some drugs react with OCP leading to decreased
efficacy of the OCP even if she takes the OCP
religiously leading to abnormal uterine bleeding
Alter circulating levels of steroids
increased endogenous levels of estrogen
Common cause of irregular bleeding in
contraceptive users.
8. AUB-E (ENDOMETRIAL)
In women with predictable and cyclic menses suggestive of
normal ovulation who have AUB, particularly the symptom of
heavy menstrual bleeding (HMB) compared to previous ones
but can also include intermenstrual bleeding, and absent
other definable causes, the patient is classified having AUB-E.
Most often, the cause of such bleeding is a primary
disorder of the endometrium.
If the symptom is HMB, the patient may have a primary
disorder of mechanism regulating local endometrial
hemostasis (Prostaglandin producing function of the
endometrium) (A) Single entity
At the present time, there are no available tests for these (B) Multiple entity
disorders, so AUB-E is assigned after excluding other NOTE: Please focus on HISTORY AND PHYSICAL
etiologies of AUB in women of reproductive years. EXAMINATION for the quiz
MED 1 | 6 of 7 BOLEYLEY, CAI, ROBANCHO
ADDENDUM
EVALUATION OF ABNORMAL UTERINE BLEEDING IN NONPREGNANT REPRODUCTIVE-AGE WOMEN
COMMENTS: (AUDIO)
Missed Period/Amenorrhea – ALWAYS CONSIDER PREGNANCY! Even if the patient denies contact.
Do not limit yourself to just obstetrics or gynecologic causes
NORMAL MENSTRUATION PARAMETERS
CLINICAL DIMENSIONS OF
NORMAL LIMITS (5TH TO 95TH
MENSTRUATION AND MENSTRUAL DESCRIPTIVE TERMS
CENTILES)
CYCLE
Absent
Infrequent >38
Frequency of Menses (Days)
Normal 24-38
Frequent <24
Regularity of menses (variation Regular Variation 7 to 9 days*
defined as shortest to longest cycle
Irregular Variation >7 to 9 days*
length, in days)
Normal 8 days
Duration of flow (days)
Prolonged >8 days
Heavy >80
Volume of monthly blood loss
Normal 5 to 80
(objective)
Light <5
Clinical Definition of heavy menstrual
bleeding (HMB): based on the patient’s
Volume of monthly blood loss
Heavy, Normal, and Light perception of volume (refer to UpToDate
(subjective)
topic on Abnormal Uterine Bleeding in
reproductive-age women)
*Normal variation depends on age; these data are calculated excluding short and long outliers
NOTE: THIS WILL COME OUT IN THE QUIZ/EXAM!
END
MED 1 | 7 of 7 BOLEYLEY, CAI, ROBANCHO
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Saint Louis University School of Medicine Mmxxii: Dr. Laygo - October 22, 2020Document37 pagesSaint Louis University School of Medicine Mmxxii: Dr. Laygo - October 22, 2020Djan Kurvie ValencerinaNo ratings yet
- Apgar ScoreDocument5 pagesApgar ScoreDjan Kurvie ValencerinaNo ratings yet
- Apgar ScoreDocument5 pagesApgar ScoreDjan Kurvie ValencerinaNo ratings yet
- DYSMENORRHEADocument12 pagesDYSMENORRHEAsanthiyasandyNo ratings yet
- Bleeding in Early PregnancyDocument39 pagesBleeding in Early PregnancyIdiAmadouNo ratings yet
- Obstetric and Gynecology: A. ColpotomyDocument44 pagesObstetric and Gynecology: A. ColpotomyAloah122346100% (1)
- Update in Sexually Transmitted Infections Free IssueDocument147 pagesUpdate in Sexually Transmitted Infections Free IssuefeiliciaNo ratings yet
- Chronic Pelvic PainDocument18 pagesChronic Pelvic PainWilliam Alfonso Parada VecinoNo ratings yet
- Kehamilan Ektopik TergangguDocument31 pagesKehamilan Ektopik TergangguAnonymous al0G68RwjJNo ratings yet
- FLUVOXAMINE and COVID19Document9 pagesFLUVOXAMINE and COVID19Petra JobovaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument2 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument4 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Baldovino - October 13, 2020Document11 pagesSaint Louis University School of Medicine Mmxxii: Dr. Baldovino - October 13, 2020Djan Kurvie ValencerinaNo ratings yet
- Group-2 - Fluvoxamine 1stDocument10 pagesGroup-2 - Fluvoxamine 1stDjan Kurvie ValencerinaNo ratings yet
- Group-2 - Fluvoxamine 1stDocument10 pagesGroup-2 - Fluvoxamine 1stDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument6 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- Ethical Guidelines For The Use of Animals in ResearchDocument9 pagesEthical Guidelines For The Use of Animals in ResearchDjan Kurvie ValencerinaNo ratings yet
- F.02 Approach To Lower Urinary Tract Symptoms (Dr. Dominguez) (04-12-19)Document3 pagesF.02 Approach To Lower Urinary Tract Symptoms (Dr. Dominguez) (04-12-19)Djan Kurvie ValencerinaNo ratings yet
- EssayDocument1 pageEssayDjan Kurvie ValencerinaNo ratings yet
- TAENIASPP RevisedDocument3 pagesTAENIASPP RevisedDjan Kurvie ValencerinaNo ratings yet
- F.03 Approach To Scrotal Pain, Swelling, and Lesions (Dr. Dominguez) (04-12-19)Document5 pagesF.03 Approach To Scrotal Pain, Swelling, and Lesions (Dr. Dominguez) (04-12-19)Djan Kurvie ValencerinaNo ratings yet
- Pharmacology and Therapeutics LabDocument20 pagesPharmacology and Therapeutics LabDjan Kurvie ValencerinaNo ratings yet
- F.01 Approach To Sexual Dysfunction (Dr. Dominguez) (04-10-19)Document4 pagesF.01 Approach To Sexual Dysfunction (Dr. Dominguez) (04-10-19)Djan Kurvie ValencerinaNo ratings yet
- Ea ComparisonDocument1 pageEa ComparisonDjan Kurvie ValencerinaNo ratings yet
- Google Deepmind Alphazero Chess, As HavingDocument1 pageGoogle Deepmind Alphazero Chess, As HavingDjan Kurvie ValencerinaNo ratings yet
- Teaching Plan On Electrolyte Imbalance22Document2 pagesTeaching Plan On Electrolyte Imbalance22Djan Kurvie ValencerinaNo ratings yet
- SCREEMDocument4 pagesSCREEMDjan Kurvie ValencerinaNo ratings yet
- Neuro Osce Cheat Sheet LolsDocument1 pageNeuro Osce Cheat Sheet LolsDjan Kurvie ValencerinaNo ratings yet
- QuestionnaireDocument1 pageQuestionnaireDjan Kurvie ValencerinaNo ratings yet
- CrammedDocument5 pagesCrammedDjan Kurvie ValencerinaNo ratings yet
- Safety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDocument1 pageSafety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDjan Kurvie ValencerinaNo ratings yet
- Thirst in Chronic Heart FailureDocument2 pagesThirst in Chronic Heart FailureDjan Kurvie ValencerinaNo ratings yet
- Safety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDocument1 pageSafety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDjan Kurvie ValencerinaNo ratings yet
- MULHANDocument17 pagesMULHANDjan Kurvie ValencerinaNo ratings yet
- DadahsitDocument1 pageDadahsitDjan Kurvie ValencerinaNo ratings yet
- Obg LMRP 2019Document34 pagesObg LMRP 2019skNo ratings yet
- GonorreheaDocument5 pagesGonorreheaSunny OZNo ratings yet
- Usg PidDocument13 pagesUsg PidHisbulloh syarifNo ratings yet
- Differential Diagnosis of The Adnexal Mass - UpToDateDocument38 pagesDifferential Diagnosis of The Adnexal Mass - UpToDateRamackNo ratings yet
- CASE3Document5 pagesCASE3romelynNo ratings yet
- Benin LesionDocument14 pagesBenin Lesionsandeepv08No ratings yet
- 8pelvic Inflammatory Disease and Tubo-Ovarian AbscessDocument16 pages8pelvic Inflammatory Disease and Tubo-Ovarian AbscessKaye VictorianoNo ratings yet
- Clinical Chart Audit STDDocument31 pagesClinical Chart Audit STDNoureen ZawarNo ratings yet
- CONTRACEPTIONDocument38 pagesCONTRACEPTIONGopala HariNo ratings yet
- Pelvic Inflammatory DiseaseDocument5 pagesPelvic Inflammatory DiseaseRahma Rafina100% (2)
- Embarazo EctopicoDocument13 pagesEmbarazo Ectopiconautilus81No ratings yet
- Iud (Intra Uterine Device)Document10 pagesIud (Intra Uterine Device)Rani ArsopistaNo ratings yet
- DysmenorrheaDocument35 pagesDysmenorrheaAs-sifa KharismaNo ratings yet
- Risk Factors of Gonorhea Infection Among Indirect Female Sex Workers (Ifsw) in Indonesia 2015 ArticleDocument6 pagesRisk Factors of Gonorhea Infection Among Indirect Female Sex Workers (Ifsw) in Indonesia 2015 ArticleFrans LandiNo ratings yet
- Pelvic Inflammatory DiseaseDocument34 pagesPelvic Inflammatory DiseaseOhunakin AfolabiNo ratings yet
- 260 QuestionsDocument42 pages260 QuestionsMaryjoy Mertalla50% (4)
- Trusted Medical Answers-In Seconds.: GonorrheaDocument7 pagesTrusted Medical Answers-In Seconds.: GonorrheantnquynhproNo ratings yet
- Pelvic Inflammatory Disease (PID) : Basim Abu-RafeaDocument26 pagesPelvic Inflammatory Disease (PID) : Basim Abu-Rafeaedwin mudumiNo ratings yet
- Vasquez - RLE A3 - PCCR (OSMUN Ward)Document16 pagesVasquez - RLE A3 - PCCR (OSMUN Ward)Mari Sheanne M. Vasquez100% (1)
- Bacterial Vaginosis, Trichomoniasis and Yeast Infection: Who Is at Risk For BV?Document4 pagesBacterial Vaginosis, Trichomoniasis and Yeast Infection: Who Is at Risk For BV?Drashua AshuaNo ratings yet
- KET4Document7 pagesKET4Janetta RheaNo ratings yet
- Ectopic Pregnancy Kehamilan Luar RahimDocument5 pagesEctopic Pregnancy Kehamilan Luar RahimMuhamad Aminuddin Abu BakarNo ratings yet
- Treatment Guidelines GonorrheaDocument1 pageTreatment Guidelines GonorrheaJoe DettNo ratings yet
- Chapter 023Document8 pagesChapter 023Roman RoundNo ratings yet