Professional Documents
Culture Documents
COLON ANATOMY AND SURGERY
Uploaded by
Djan Kurvie ValencerinaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COLON ANATOMY AND SURGERY
Uploaded by
Djan Kurvie ValencerinaCopyright:
Available Formats
SURGERY II
Saint Louis University School of Medicine MMXXII
M.03 COLON, RECTUM, AND ANUS (PARTS 1&2) II. ANATOMY OF THE COLON
Dr. Laygo | October 22, 2020 Large intestine extends from the ileocecal valve to the anus.
Anatomical and functional divisions: colon, rectum, and anal canal
OUTLINE 5 distinct layers
I. EMBRYOLOGY o Mucosa
II. ANATOMY o Submucosa
III. CONGENITAL ANOMALIES o Inner circular muscle
IV. NORMAL PHYSIOLOGY o Outer longitudinal muscle
V. CLINICAL EVALUATION Made up of 3 teniae coli proximally at the appendix and
VI. GENERAL SURGICAL CONSIDERATIONS distally at the rectum eventually becomes (circumferential)
In the distal rectum, the inner smooth muscle layer coalesces
internal anal sphincter
DISCLAIMER: Apologies for some unreadable labels. The quality of o Serosa – outermost
the images is fitted to the maximum capacity of the trans. Please refer Forms the intraperitoneal colon and proximal 1/3 of the rectum
to Netter or the PPT presentation for better image resolution. Mid and lower rectum are usually without peritoneum
Fig. 1. Illustration depicting the large intestine from the cecum to the
ascending colon, transverse colon, descending colon, rectum and
eventually the anus.
I. EMBRYOLOGY Fig. 2. Colon. An illustration of the large intestine showing the cecum,
4th week of gestation hepatic flexure, transverse colon, splenic flexure, descending colon,
Derived from the endoderm sigmoid colon, the rectosigmoid, the rectum and eventually the anal
Divided into three segments: canal
o Midgut and hindgut colon, rectum, and anus
A. COLON LANDMARKS
Midgut Hindgut Colon begins at the junction of the terminal ileum and cecum and
Derivative Small intestine, Distal 1/3 transverse extends approximately 3-5 feet to the rectum.
ascending colon, and colon Rectosigmoid junction
proximal transverse Descending colon o Found approximately at the level of the sacral promontory
colon Rectum o Point at which the 3 teniae coli coalesce forming the outer
Proximal anus longitudinal muscle layer of the rectum
Blood Supply Superior mesenteric Inferior mesenteric 1. Cecum
artery (SMA) artery (IMA) o Part of the colon with the widest diameter (7.5-8.5 cm)
6th week AOG Herniates out of the Cloaca (distal-most end o Thinnest muscular wall
abdominal cavity of the hindgut) is o Most vulnerable to perforation
divided by the urorectal o Least vulnerable to obstruction
Rotates 270˚ septum into the 2. Ascending colon
counterclockwise urogenital sinus (urinary o Usually is fixed to the retroperitoneum
around the SMA bladder and urethra) o Has the hepatic flexure marks transition to transverse colon
and the rectum 3. Transverse colon
Distal anal canal o Intraperitoneal
o From the ectoderm o Relatively mobile but tethered by the gastrocolic ligament and
o Blood supply: internal pudendal artery colonic mesentery
Dentate line o Greater omentum is attached to the anterior/superior edge of the
o Forms endodermal hindgut from the ectodermal distal anal canal transverse colon
o Characteristic triangular appearance of transverse colon observed
during colonoscopy
SURG II |1 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
4. Splenic flexure Marginal artery of Drummond
o Marks transition from the transverse colon to the descending o Anastomosis of inferior and superior mesenteric arteries
colon Veins of the colon parallel their corresponding arteries and bear the
o Attachments between the splenic flexure and spleen (lienocolic same terminology, and they drain towards the portal venous system
ligament) mobilization of this flexure during colectomy is
o Exception: inferior mesenteric vein
challenging because of this ligament
5. Descending colon
Ascends in the retroperitoneal plane over the psoas muscle
and continues posterior to the pancreas to join the splenic
o Relatively fixed to the retroperitoneum
vein
6. Sigmoid colon
o Narrowest part of the large intestine
o Extremely mobile
o Located in the LLQ; redundancy and mobility can result in a
portion of the sigmoid colon residing in the RLQ
Fig. 4. Blood supply to the colon and rectum. Supplied by superior and
inferior mesenteric arteries.
Fig. 3. Sigmoid colon variations in position. An illustration of the large
intestine specifically the part of the sigmoid colon where the location of
the sigmoid colon is dependent on the length of the mesosigmoid. If it
is mobile, wide, and large mesocolon, the sigmoid colon can go to the
right side of the abdomen.
B. COLON VASCULAR SUPPLY
Highly variable
Superior Mesenteric Artery Inferior Mesenteric Artery
Artery Area/s Artery Area/s
supplied supplied
Ileocolic Terminal Left colic Descending
artery ileum artery colon
(absent in up
to 20% Proximal
people) ascending
colon
Right colic Ascending Sigmoidal Sigmoid colon
artery colon branches
Middle colic Transverse Superior Proximal
artery colon rectal artery rectum
Marginal
artery of
Drummond
(complete in
only 15 to
20% of
people)
Fig. 5. Arteries of large intestine
SURG II |2 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Fig. 6. Veins of small and large intestines
Fig. 8. Lymph vessels and nodes of large intestine
Fig. 7. Portal vein. The venous drainage of the Large intestine usually
goes toward the superior and inferior mesenteric veins. They
eventually drain towards the portal venous system. The portal venous
system goes towards the liver. 75% of the blood supply to the liver
comes from the portal venous system.
C. COLON LYMPHATIC DRAINAGE
Very important when dealing with colonic malignancy Fig. 9. Lymph glands abdomen. LNs from large intestines join LNs
Originates in a network of lymphatics in the muscularis mucosa from the small intestine cisterna chyli thoracic duct junction of
Lymphatic vessels and lymph nodes follow the regional arteries left subclavian vein and left internal jugular vein
Lymph nodes:
D. COLON NERVE SUPPLY
1. Epicolic – found on the bowel wall
2. Paracolic – along the lower inner margin of the bowel adjacent to Innervated by sympathetic (inhibitory) and parasympathetic
(stimulatory) nerves
the arterial arcades
3. Intermediate – around the named mesenteric vessels Sympathetic nerves: T6–T12 and L1–L3
4. Main – at the origin of the superior and inferior mesenteric arteries Parasympathetic innervation to the right and transverse colon
vagus nerve
Drain into the cisterna chyli lymphatic system drains at
the junction of internal jugular and subclavian veins Parasympathetic nerves to the left colon arise from sacral nerves S2–
S4 to form the nervi erigentes.
5. Sentinel – first one to four lymph nodes that drain a specific
segment of the colon
SURG II |3 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Anal transition zone is surrounded by longitudinal mucosal folds
Columns of Morgagni into which the anal crypts empty source
of cryptoglandular abscesses
Fig. 10. Autonomic innervation of large intestine Fig 11. Anal canal. After the rectum terminates at the anal opening.
E. ANORECTAL LANDMARKS F. ANORECTAL VASCULAR SUPPLY
1. Rectum 1. ARTERIES
Approximately 12-15 cm in length Superior rectal artery/ Superior hemorrhoidal artery
o Valves of Houston o Arises from the terminal branch of the inferior mesenteric artery
Three distinct submucosal folds that extend into the rectal and supplies the upper rectum
lumen
Middle rectal artery
Arrangement: left – right – left o Arises from the internal iliac
o Presacral fascia
Inferior rectal artery
Located posteriorly and it separates the rectum from the
o Arises from the internal pudendal
presacral venous plexus and pelvic nerves
o Retrosacral fascia (Waldeyer’s fascia)
2. VEINS
At S4, it extends forward and downward and attaches to the
fascia propria at the anorectal junction Venous drainage of the rectum parallels the arterial supply.
o Denonvilliers’ fascia Superior rectal vein
Located anteriorly and it separates the rectum from the o Drains into the portal system via the inferior mesenteric vein
prostate and seminal vesicles in men and from the vagina in Middle rectal vein
women o Drains into the internal iliac vein
o Lateral ligaments Inferior rectal vein
Support the lower rectum o Drains into the internal pudendal vein, and subsequently into the
Traversed by the middle rectal vessels internal iliac vein
o Distal rectum A submucosal plexus deep to the columns of Morgagni forms the
Internal anal sphincter (thickened inner smooth muscle) hemorrhoidal plexus and drains into all three veins.
External anal sphincter (surrounds the internal anal sphincter)
Subcutaneous
Superficial
Deep: extension of puborectalis muscle
*Levator ani muscle: puborectalis, iliococcygeus,
pubococcygeus
2. Surgical anal canal
Measures 2 to 4 cm in length and generally is longer in men than
in women
Begins at the anorectal junction and terminates at the anal verge
Dentate or pectinate line
o Marks the transition point between columnar rectal mucosa and
squamous anoderm
Anal transition zone
o 1 to 2 cm of mucosa just proximal to the dentate line shares
histologic characteristics of columnar, cuboidal, and squamous Fig 12. Venous drainage of anal canal. Superior part superior rectal
epithelium. vein inferior mesenteric veinmiddle rectal veininternal iliac
veininferior rectal veininternal pudendal veininternal iliac vein
SURG II |4 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Fig 15. Lymphatic drainage of anal canal. Eventually drains to the
internal group of LNs while some eventually to the inguinal LNs.
Fig 13. (A) Arterial supply (B) Venous drainage of anal canal
Fig 16. Medial section
H. ANORECTAL NERVE SUPPLY
Both sympathetic and parasympathetic nerves innervate the
anorectum.
Fig 14. Venous drainage. Distal rectum and anal canal
G. ANORECTAL LYMPHATIC DRAINAGE
Lymphatic drainage of the rectum parallels the vascular supply
Area Direction of Flow Lymph Node
Upper and middle Superiorly Inferior mesenteric
rectum
Lower rectum Superiorly Inferior mesenteric
Laterally Internal iliac
Anal canal: More complex
Anal canal - Inferior mesenteric
proximal to Internal iliac
dentate line
Anal canal distal to - Inguinal eventually
dentate line to the inferior
mesenteric
Internal iliac
Fig. 17. Innervation of the distal parts specifically rectum and Anal
canal
SURG II |5 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Area Innervation Potassium is actively secreted into the colonic lumen and absorbed
Anorectum Sympathetic fibers from L1 – L3 join the by passive diffusion
preaortic plexus extends below the aorta Chloride is absorbed actively via a chloride–bicarbonate exchange.
to form hypogastric plexus below the Bacterial degradation of protein and urea produces ammonia
aorta joins the parasympathetic fibers Ammonia is subsequently absorbed and transported to the liver
S2 – S4 (nervi erigentes) join the
Absorption of ammonia intraluminal pH a decrease in colonic
sympathetic fibers to form the pelvic plexus
bacteria (e.g., broad-spectrum antibiotic usage) and/or a decrease in
Internal anal Sympathetic and parasympathetic nerve intraluminal pH (e.g., lactulose administration) NH4 absorption.
sphincter fibers inhibit sphincter contraction
External anal Innervated by inferior rectal branch of the B. SHORT-CHAIN FATTY ACIDS
sphincter and internal pudendal nerve
Short-chain fatty acids (acetate, butyrate, and propionate) are
puborectalis
produced by bacterial fermentation of dietary carbohydrates
Levator ani Internal pudendal nerve and direct branches
important source of energy for the colonic mucosa, and metabolism
of S3 – S5
by colonocytes provides energy for processes such as active transport
Anal canal (sensory Inferior rectal branch of the pudendal nerve
of sodium
innervation)
Lack of a dietary source mucosal atrophy and "diversion colitis”
Although the rectum is relatively insensate, the anal canal below the
dentate line is sensate, that is why external hemorrhoids are very
C. COLONIC MICROFLORA AND INTESTINAL GAS
painful compared to internal hemorrhoids.
1. COLONIC MICROFLORA
Approximately 30% of fecal dry weight is composed of bacteria (1011
to 1012 bacteria/g of feces)
Anaerobes are the predominant class of microorganism
Bacteroides sp. – most common (1011 to 1012 organisms/mL)
Escherichia coli is the most numerous aerobe (108 to 1010
organisms/mL).
Functions of endogenous microflora:
o Breakdown of carbohydrates and proteins in the colon
o Participate in the metabolism of bilirubin, bile acids, estrogen, and
cholesterol
o Suppress the emergence of pathogenic microorganisms, such as
Clostridium difficile (colonization resistance)
2. INTESTINAL GAS
Arises from swallowed air, diffusion from the blood, and intraluminal
production
Major components:
o Nitrogen, oxygen, carbon dioxide, hydrogen, and methane are the
major components of intestinal gas
o Nitrogen and oxygen are largely derived from swallowed air
o Carbon dioxide is produced by the reaction of bicarbonate and
hydrogen ions, and by the digestion of triglycerides to fatty acids
Fig 18. Anal sphincter o Hydrogen and methane are produced by colonic bacteria;
production of methane is highly variable
III. CONGENITAL ANOMALIES GI tract 100 and 200 mL of gas and 400 to 1200 mL per day are
(not extensively discussed in the presentation) released as flatus, depending upon the type of food ingested.
Perturbation of the embryologic development of the midgut and
hindgut anatomic abnormalities of the colon, rectum, and anus D. MOTILITY, DEFECATION, AND CONTINENCE
Intestinal malrotation and colonic non-fixation 1. MOTILITY
o Failure of midgut to rotate and return to the abdominal cavity by Does not demonstrate cyclic motor activity characteristic of the
10th week AOG migratory motor complex. Instead, the colon displays intermittent
Colonic duplication contractions of either low or high amplitude.
o Failure of canalization of the primitive gut o Low-amplitude, short-duration contractions
Imperforate anus and genitourinary fistulas Occur in bursts
o Incomplete descent of the urogenital septum Move colonic contents both anterograde and
Septum imperforate anus retrograde
Fistulas to the genitourinary tract Delays colonic transit more time for water absorption and
electrolyte exchange
Many infants with congenital anomalies of the hindgut have
associated abnormalities in the genitourinary tract
o High-amplitude, prolonged-duration, propagated
contractions (HAPCs)
IV. NORMAL PHYSIOLOGY
Coordinated
A. FLUID AND ELECTROLYTE EXCHANGES “Mass movements”
4-10 times per day, mostly after meals and awakening
Colon: major site for water absorption and electrolyte exchange
Bursts of “rectal motor complexes”
Approx. 90% of the water contained in ileal fluid is absorbed in the
colon (1000 to 2000 mL/d) Cholinergic activation increases colonic motility
5000 mL of fluid absorbed in colon daily
2. DEFECATION
Na is absorbed actively via a Na-K ATPase
Complex, coordinated mechanism involving colonic mass movement,
400 mEq of Na per day-absorb in colon increased intra-abdominal and rectal pressure, and relaxation of the
Water accompanies the transported sodium and is absorbed passively pelvic floor
along an osmotic gradient
SURG II |6 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Distention of the rectum causes a reflex relaxation of the internal anal 8 cm in length
sphincter (the rectoanal inhibitory reflex) that allows the contents to Larger anoscope: rubber band ligation or sclerotherapy of
make contact with the anal canal hemorrhoids
o "Sampling reflex" allows the sensory epithelium to distinguish Perform with anesthesia if patient complains of perianal pain and
solid stool from liquid stool and gas. If defecation does not occur, cannot tolerate DRE
the rectum relaxes and the urge to defecate passes
(accommodation response)
Defecation proceeds by coordination of increasing intra-abdominal
pressure via the Valsalva maneuver, increased rectal contraction,
relaxation of the puborectalis muscle, and opening of the anal canal.
3. CONTINENCE
(not extensively discussed in the presentation)
Requires adequate
o Rectal wall compliance to accommodate the fecal bolus
o Appropriate neurogenic control of the pelvic floor and sphincter
mechanism
o Functional internal and external sphincter muscles
Puborectalis muscle creates a "sling" around the distal rectum,
forming a relatively acute angle that distributes intra-abdominal
forces onto the pelvic floor
With defecation, this angle straightens, allowing downward force to
be applied along the axis of the rectum and anal canal
Internal and external sphincters are tonically active at rest
Resting pressure (involuntary) – internal sphincter
Squeeze pressure (voluntary) – external sphincter
Internal sphincter is responsible for most of the resting, involuntary
sphincter tone (resting pressure)
The external sphincter is responsible for most of the voluntary Fig. 19. Anoscope
sphincter tone (squeeze pressure)
Pudendal nerve innervates both the internal and external sphincter 2. Proctoscopy
Hemorrhoidal cushions mechanically block the anal canal Rigid, 25 cm in length
Formed stool maintains continence Examination of rectum and distal sigmoid colon
Liquid stools exacerbate abnormalities with these anatomic and Occasionally therapeutic
physiologic mechanisms Diameter:
Causes of impaired continence: 11 mm for pediatrics and patients with anal stricture
o Poor rectal compliance 15 or 19 mm for diagnostic examination
o Injury to the internal and/or external sphincter or puborectalis 25 mm for polypectomy, electrocoagulation, and detorsion of
o Neuropathy a sigmoid volvulus
It is diagnostic and therapeutic.
V. CLINICAL EVALUATION Requires suction for adequacy
Transanal endoscopic microsurgery (TEM) uses wide diameter
CASE 1 proctoscope for excision of large polyps and tumors
A 60-yr-old businessman was brought to the hospital because of left
Transanal minimally invasive surgery (TAMIS) uses insufflation
lower quadrant abdominal pain associated with hematochezia, instead of proctoscope
alternating diarrhea and constipation and loss of weight. P.E.
findings showed a slightly distended abdomen, hypoactive bowel
sounds, with direct and rebound tenderness over the left lower
quadrant area, rectal examination is unremarkable. X-ray of the
abdomen showed distention of the small and large intestines with
paucity of rectal gas.
A. CLINICAL ASSESSMENT
Complete history and physical examination
Special attention to patient’s past medical and surgical history
o Prior intestinal surgery resultant gastrointestinal anatomy Fig. 20. Proctoscope
o Prior anorectal surgery abdominal or anorectal complaints
Obstetric history in women occult pelvic floor and/or anal sphincter 3. Flexible Sigmoidoscopy
damage Excellent visualization up to the splenic flexure
Family history of colorectal disease, inflammatory bowel disease Diagnostic and therapeutic
(IBD), polyps, and colorectal cancer 60 cm in length
History of other malignancies genetic syndrome Partial prep
Medication use gastrointestinal symptoms No sedation
Examine abdomen, visual inspection of anus and perineum, digital
rectal exam (DRE)
B. ENDOSCOPY
1. Anoscopy
Examination of anal canal
SURG II |7 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
appearance
o Volvulus. Segmental distension
b. Contrast studies
Obstruction
Fistulous tracts
Perforations or anastomotic leaks
Gastrografin – perforation/leak
Double-contrast barium enema – mass lesions >1cm
Fig22. Video/Fiberoptic Colonoscope
4. Flexible colonoscopy
100 to 160 cm in length
Capable of examining the entire colon & terminal ileum
Complete bowel prep
Sedation necessary
Diagnostic and therapeutic
Fig. 24. Plain x-ray shows Fig. 25. Contrast Study.
incomplete large bowel Coming from the anal canal going up
obstruction with towards the rectum and then the
distension of the small sigmoid colon occupying the right side
bowels with the abdomen going to the
descending colon, the splenic flexure,
Fig. 23. Colonoscope
transverse colon, hepatic flexure,
ascending colon and ends at the cecum
5. Capsule endoscopy
Small indigestible camera
Indication: small bowel lesions 2. Computed Tomography (CT)
Dissolvable capsule for obstruction lesions For extraluminal diseases such as:
Advantages: o Intra-abdominal masses
o Painless o Pericolic inflammation
o No sedation CRCA staging
o 3D color images without surgery Perforation or anastomotic leak
o Early, accurate diagnosis Inflammatory bowel disease
Colitis
Ischemia
Fig. 26.CT contrast showing uncomplicated diverticulitis with fat
stranding of the mesentery and thickening of the sigmoid colon
C. IMAGING 3. Virtual colonoscopy/CT colography
1. Plain X-rays and Contrast Studies Helical CT & 3-D
a. Plain X-rays (supine, upright, diaphragmatic views) Reconstruction to detect intraluminal colonic lesion
Detection of:
o Free intra-abdominal air a sign of perforation
o Bowel gas patterns: bowel obstruction. Step ladder
SURG II |8 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
6. Angiography
Bleeding within colon
Bleeding must be relatively brisk (approx. 0.5-1.0 mL/min)
Fig. 27. Computerized Virtual Colography
4. Magnetic Resonance Imaging (MRI) Fig. 30. Normal angiography of colonic vessels
Pelvic lesions
Bony involvement or rectal tumors extension pelvic sidewall and 7. Endorectal and Endoanal Ultrasound
mesorectum Depth of invasion of rectal CA
Differentiates most benign polyps from invasive tumors based
upon the integrity of submucosal layer (normal rectal wall appears
as a 5-layer structure)
Fig. 28. MRI of colon showing a foreign body at the transverse colon
5. Positron Emission Tomography (PET)
Imaging tissues with high levels of anaerobic glycolysis (e.g.
malignant tumors)
Adjunct to CT in colorectal cancer staging
Discriminates recurrent cancer from fibrosis Fig. 31. Normal endoanal ultrasound of the rectum
D. LABORATORY STUDIES
1. Fecal Occult Blood Testing (FOBT) and Fecal
Immunohistochemical Testing (FIT)
a. FOBT
Screening for colonic neoplasms
Efficacy is based upon serial testing
Majority of CRCA will bleed intermittently
Restrict diet for 2-3 days prior to the test
False positive result with consumption of:
Red meat
Some fruits and vegetables
Vitamin C
b. FIT
Relies on monoclonal or polyclonal antibodies to react with
the intact globin of hemoglobin
2. Stool Studies
Evaluation of etiology of diarrhea
a. Wet-mount examination
Fecal leukocytes suggest colonic inflammation
Fig. 29. PET scan for colon ca surveillance. Note that the black areas b. Stool culture
increased on the lower image, suggestive of metastases. Bacteria, ova, and/or parasites
c. Bacterial toxin
SURG II |9 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Clostridium difficile colitis
d. Sudan red stain
Steatorrhea
3. Serum Tests
CBC, electrolyte panel, coagulation studies, liver function tests,
blood typing
4. Tumor Markers
Carcinoembryonic antigen (CEA) is elevated in 60-90% of patients
with colorectal cancer
5. Genetic Testing
Mutation on adenomatous polyposis coli (APC) gene familial
adenomatous polyposis (FAP)
Mismatch repair genes hereditary nonpolyposis colon cancer Fig. 32. Hematochezia
(HNPCC)
3. Constipation and obstructed defecation
E. EVALUATION OF COMMON SYMPTOMS Extremely common complaint
1. Pain
Lack of agreement about an appropriate definition: infrequent
a. Abdominal pain
bowel movement, hard stool, excessive straining
Related to colon and rectum
Can result from: Causes of constipation:
o Anatomic
Obstruction (Inflammatory or Ca) o Metabolic
Inflammation o Pharmacologic
Perforation o Endocrine
Ischemia o Psychological
Evaluation: o Neurogenic
Plain x-ray, CT scan, or contrast studies to confirm diagnosis Stricture vs mass exclude by colonoscopy
Gentle retrograde contrast studies (Gastrografin enema) to
delineate degree of colonic obstruction Transit Studies
Sigmoidoscopy and/or colonoscopy are contraindicated in Slow-transit Outlet obstruction
perforation and near complete obstruction Constipation
b. Pelvic pain Retention of ≥20% Congregation of markers
Originates from the distal colon, rectum, or adjacent urogenital markers in colon in the rectosigmoid colon and
structures
rectum
Tenesmus proctitis, rectal/retrorectal mass, fecal impaction
Cyclical pain endometriosis
Mainstay of therapy: medical management (fiber, increase fluid
Evaluation: intake, laxatives), exercise
CT scan, MRI Sigmoidoscopy or colonoscopy are used to diagnose
Proctoscopy inflammatory bowel disease or ischemia.
Laparoscopy Endoscopy is contraindicated if the patient has abdominal
c. Anorectal pain tenderness, particularly with peritoneal signs from perforation, or
Secondary to anal fissure, perirectal abscess and/or fistula, or those with acute surgical abdomen.
thrombosed hemorrhoid
Evaluation: 4. Irritable bowel syndrome
Examine under anesthesia Common symptom
MRI Usually a self-limited symptom of infectious gastroenteritis
Colitis: bloody diarrhea and pain
2. Lower gastrointestinal bleeding o Infection stool wet mount and culture
1st goal: adequate resuscitation o IBD
2nd goal: identify source: o Ischemia
o May insert nasogastric tube/NGT (indicate upper GI bleeding), Chronic diarrhea stool culture, test for malabsorption, metabolic
or do EGD (to rule out upper GI bleed), GI scope (to view lower investigation, biopsy
GI bleed) Irritable bowel syndrome (IBS)
Most common sources: esophageal, gastric, duodenal o Troubling constellation of symptoms: crampy abdominal pain,
99mTc-tagged red blood cell scan: extremely sensitive (detects as bloating, constipation, urgent diarrhea
little as 0.1 mL/h bleeding) o Management: dietary restriction, avoidance of caffeine, alcohol,
If positive, angiography is both diagnostic and therapeutic and tobacco, antispasmodics and fiber helps alleviate symptoms
Occult GI bleeding FOBT/FIT
Unexplained anemia colonoscopy 5. Incontinence
Hematochezia due to either a/an: Ranges from occasional leakage of gas and/or liquid stool to daily
o Fissure: sharp, knife-like pain and bright red rectal bleeding loss of solid stool
with bowel movement Neurogenic causes:
o Internal hemorrhoid: painless, bright red rectal bleeding with o Diseases of central nervous system and spinal cord
bowel movement o Pudendal nerve injury
o Rectal bleeding without pain and fissure DRE, anoscopy, Anatomic causes:
proctosigmoidoscopy o Congenital abnormalities
Refer to the appendix for the diagnostic pathway. o Procidentia
o Overflow incontinence secondary to cancer, feces, or trauma
(pelvic fractures), iatrogenic
SURG II |10 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
CASE 1 continuation:
Examination of above patient revealed a rectosigmoid tumor almost
completely obstructing the bowel lumen with biopsy showing
adenocarcinoma. Which of the following colonic operations is the
best choice for this case?
A. Left hemicolectomy
B. Anterior colonic resection (Tumor is in the rectosigmoid)
C. Abdominoperineal resection (Miles’ operation)
E. Sigmoidectomy
VI. GENERAL CONSIDERATIONS
Extent of colonic resection is determined by:
o Nature of primary pathology (benign or malignant)
o Intent of resection (curative or palliative)
o Precise location/s of the primary pathology
o Condition of the mesentery (thin & soft or thick & indurated)
EMERGENCY RESECTION Fig. 34. Ileocolic resection
o Bowel is almost always unprepared
o Patient may be unstable CASE 2
o Resect involved segment with lymphovascular supply A 65-year old government employee sought consultation because of
an on and off melena associated with a right lower quadrant
A. MINIMALLY INVASIVE (Laparoscopic) abdominal mass. Colonoscopy showed a cecal mass with a
Potential advantages: histopathology finding of an adenocarcinoma. Which is the surgical
o Improved cosmetic result treatment of choice for this clinical condition?
o Decreased postoperative pain Ans: Right Hemicolectomy(For a cecal tumor)
o Earlier return of bowel function 2. RIGHT HEMICOLECTOMY
o Less immunosuppressive impact on the patient For lesions/disease in the right colon
In resections: Ileocolic vessels, right colic vessels and right branches of the middle
o Technically demanding colic vessels are ligated.
o Requires longer operative time than open procedures A primary ileal-transverse colon anastomosis
o Improved short term quality of life
Robotics/Telemanipulation
o Surgeon operates from a console away from the patient
o Easier to learn (shorter learning curve)
o Ergonomically better for the surgeon
Fig. 35. Right hemicolectomy. Resected from distal ileum up to the
hepatic flexure.
Fig. 33. Laparoscopic resection of the transverse colon. A very
minimally invasive procedure.
B. COLECTOMIES
1. ILEOCOLIC RESECTION
Limited resection of the terminal ileum, cecum, and appendix
Used to remove benign lesions or incurable cancers arising in the
terminal ileum, cecum, and appendix
Ileocolic vessels are ligated and divided
Primary anastomosis is created between the distal SI and ascending
colon
Fig. 36. (Left) Tumor on ascending colon so do right hemicolectomy;
(Right) Tumor on descending colon so do Left hemicolectomy
SURG II |11 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
3. EXTENDED RIGHT HEMICOLECTOMY CASE 3
Lesions located at the hepatic flexure or proximal transverse colon A 50-yr old male professor was subjected to a colonoscopy and was
Include ligation of the middle colic vessels at their base found out to have a mass at the splenic flexure of the colon. Biopsy
A primary anastomosis between the ileum and distal transverse colon result showed colonic adenocarcinoma. Which colonic operation is
Anastomosis relies on the marginal artery of Drummond ideal for this patient?
Ans: Left hemicolectomy
5. LEFT HEMICOLECTOMY
For lesions in the distal transverse colon, splenic flexure, or
descending colon
Left branches of the middle colic vessels, left colic vessels and first
branches or the sigmoid vessels are ligated.
A colocolonic anastomosis
Fig. 36. Example of extended right colectomy. Resection of the distal
ileum, the cecum and appendix, the ascending colon, the hepatic
flexure and proximal two third of the transverse colon
4. TRANSVERSE COLECTOMY Fig. 39. Left hemicolectomy. Resect the distal transverse colon, splenic
For lesions in the mid and distal transverse colon flexure and part of the sigmoid colon then do colocolonic anastomosis
Ligating the middle colic vessel
Colo-colonic anastomosis
Fig. 40. Left hemicolectomy
6. EXTENDED LEFT HEMICOLECTOMY
For lesions in the distal transverse colon
Include the right branches of the middle colic vessels
Fig. 37. Resect entire transverse colon and anastomose proximal and 7. SIGMOID COLECTOMY
distal end Lesions in the sigmoid colon
Ligation of the sigmoid branches of IMA
Sigmoid is resected to the level of the peritoneal reflection and
anastomosis between the descending colon and upper rectum
Fig. 38. Transverse colectomy Fig 41. Sigmoid Colectomy. Anastomose the upper part of the
LEFT HEMICOLECTOMY rectum to the descending colon
SURG II |12 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
D. ANTERIOR RESECTION
1. HIGH ANTERIOR RESECTION
Resection of the distal sigmoid colon and upper rectum
Operation for benign lesions at the rectosigmoid junction
(diverticulitis)
Upper rectum is mobilized but the pelvic peritoneum is not divided
Rectum is not mobilized fully form the concavity of the sacrum
Anastomosis between the colon and rectal stump
2. LOW ANTERIOR RESECTION
Lesions in the upper and mid rectum
3. EXTENDED LOW ANTERIOR RESECTION
Lesions in the distal rectum, and several centimeters above the
sphincter
Fig. 42. Sigmoid colectomy
8. TOTAL AND SUBTOTAL COLECTOMY
Fulminant colitis, attenuated familial adenomatous polyposis or
synchronous colon carcinomas
Ileocolic, right colic, middle colic and left colic vessels are ligated.
Superior rectal vessels are preserved.
Fig. 44. Low anterior resection. Anastomosis between the proximal
colon and the remaining rectum are usually done by hand sewing but
more ideal to do with a stapler device
Fig. 42. Subtotal colectomy
C. PROCTOCOLECTOMIES
1. TOTAL PROCTOCOLECTOMY
Entire colon, rectum, and anus are removed
Ileum is brought to the skin as ileostomy
2. RESTORATIVE PROCTOLECTOMY (Ileal Pouch-Anal
Anastomosis)
Fig. 45. Low anterior resection showing the stapled or sutured distal
Entire colon and rectum are resected colon to the remaining distal part of the rectum
Anal sphincter muscles and a portion of the distal anal canal are
E. ABDOMINOPERINEAL RESECTION (APR)/MILES’
preserved
OPERATION
Anastomosis of an ileal reservoir to the anal canal restores bowel
Removal of the entire rectum, anal canal, and anus
continuity
Permanent colostomy from the descending or sigmoid colon
Fig. 43. Proctocolectomies
Fig. 46. Abdominoperineal Resection (APR)
SURG II |13 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
VII. CHECKPOINT
Identify what is asked.
1. Outermost layer of the colon
2. The outer longitudinal muscle of the colon is made up of how
many teniae coli?
3. At what AOG is the cloaca divided by the urorectal septum into
the urogenital sinus and the rectum?
4. Part of the colon with the widest diameter
5. Has the characteristic triangular appearance observed during
colonoscopy
True or False:
6. The ascending colon has the thinnest muscular wall.
7. The ascending colon has the splenic flexure.
8. The lesser omentum is attached to the anterior/superior edge
of the transverse colon.
9. The attachment between the hepatic flexure and spleen is
Fig. 47. Abdominoperineal Resection (APR). Resect entire colon, known as the lienocolic ligament.
sigmoid, rectum and anus. Then put out remaining distal portion as 10. The sigmoid colon is the narrowest part of the large intestine.
permanent colostomy. 11. The surgical anal canal is longer in men than in women.
12. The predominant class of microorganisms in the colon is
F. HARTMANN’S PROCEDURE aerobes.
Colon or rectal resection without anastomosis 13. The puborectalis muscle creates a sling around the distal
Colostomy and ileostomy is created rectum.
Distal colon or rectum is left as a blind pouch 14. The major site of water absorption and electrolyte exchange is
For those with ruptured tumors or cancer in the sigmoid colon. Resect the small intestine.
part of the tumor and have a blind pouch. 15. E. coli is the most numerous aerobe in the colon.
Identify the procedure asked.
16. Anastomosis relies on the marginal artery of Drummond
17. Indicated for benign lesions of the terminal ileum, cecum, or
appendix
18. Indicated for lesions on the distal transverse colon
19. If sigmoid is preserved, this procedure is indicated together
with ileosigmoid anastomosis.
20. If sigmoid is resected, this procedure is indicated together with
ileorectal anastomosis.
colectomy, (20) Total colectomy
Ileocolic resection, (18) Extended left hemicolectomy, (19) Subtotal
T, (14) F – colon, (15) T, (16) Extended right hemicolectomy, (17)
omentum, (9) F – splenic flexure, (10) T, (11) T, (12) F – anaerobes, (13)
Transverse colon, (6) F – cecum, (7) F – hepatic flexure, (8) F – greater
ANSWERS: (1) Serosa, (2) Three, (3) 6th week, (4) Cecum, (5)
Fig. 47. Hartmann’s procedure
G. MUCUS FISTULA
Done if the distal colon is long enough to reach the abdominal wall
Created by opening the defunctioned bowel and suturing the open
lumen to the skin
SURG II |14 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
APPENDIX
SURG II |15 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
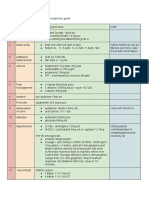
SUMMARY OF THE COLECTOMIES
Type Indication / Vessels ligated Anastomosis
Location of lesion
Ileocolic resection Benign lesions of Ileocolic vessels Between distal small intestine
A to C terminal ileum, cecum, and ascending colon
appendix
Right hemicolectomy Right colon Ileocolic vessels Ileal-transverse colon
A to D For proximal colon Right colic vessels
carcinoma Right branches of the middle colic
vessels
Extended right Hepatic flexure Middle colic vessels at their base Between ileum and distal
hemicolectomy Proximal transverse transverse colon
A to G colon Relies on the marginal artery of
Drummond
Transverse colectomy Mid and distal Middle colic vessel Colocolonic
E to H transverse colon
Left hemicolectomy Distal transverse colon Left branches of the middle colic Colocolonic
G to I Splenic flexure vessels
Descending colon Left colic vessels
First branches of the sigmoid vessels
Extended left hemicolectomy Distal transverse colon Right branches of the middle colic -
F to I vessels
Sigmoid colectomy Sigmoid colon Sigmoid branches of the inferior Between descending colon and
J to K mesenteric artery upper rectum
o Sigmoid is resected to
the level of the peritoneal
reflection
Total colectomy Fulminant colitis Ileocolic vessels If sigmoid is preserved:
A to K Attenuated FAP Right colic vessels Subtotal colectomy with
Synchronous colon Middle colic vessels ileosigmoid anastomosis
& carcinomas Left colic vessels
If sigmoid is resected: Total
Subtotal colectomy *Superior rectal vessels are preserved abdominal colectomy with
A to J ileorectal anastomosis
*Subtotal: Preserve sigmoid and
distal sigmoid vessels
SURG II |16 of 16 [ WONG, M.C., EZEUDEH, DELA CRUZ]
SURGERY II
Saint Louis University School of Medicine MMXXII
M.03 COLON, RECTUM, AND ANUS (PARTS 3 & 4)
Dr. Laygo | October 22, 2020
I. General Considerations
II. Operative Preliminaries
III. Diseases of the Colon
IV. Colorectal Diseases
V. Screening and Surveillance
VI. Colon Cancer Staging
VII. Routes of Spread and Natural History
VIII. Staging of Colorectal Cancer
IX. Therapy for Colonic Cancer
X. Therapy for Rectal Cancer
XI. Appendix (from 2021) ● These are your resected bowels, eventually they are
anastomosed with each other
I. GENERAL CONSIDERATIONS (continuation)
A. ANASTOMOSES
● Created between two segments of bowel
● may be end-to-end, end-to-side, side-to-end, or side-to-side
● the submucosal layer of the intestine provides the strength of
the bowel wall, must be incorporated in the anastomosis to
assure healing
GEOMETRY OF ANASTOMOSES
TYPE DESCRIPTION APPLICATION
Performed when two 1. Rectal resections
segments of the bowel 2. Colocostomy
End-to-end1
are roughly the same 3. Small bowel
caliber (diameter) anastomoses
Useful when one limb of
End-to-side2 the bowel is larger than Chronic obstruction Figure 1. Examples of Anastomoses
the other ● Anastomosis of small intestine to the side of the ascending
Used when the colon
proximal bowel is of B. OSTOMIES
Side-to-end3 Ileorectal anastomoses ● Usually temporary or permanent
smaller caliber than the
distal bowel ● Located within the rectus muscle to minimize parastomal
Allows a large, well- hernia
vascularized connection ● Placed where the patient can see & manipulate easily
to be created on the Ileocolic and small ● Surrounding abdominal soft tissue should be as flat as
Side-to-side4 possible to ensure a tight seal & prevent leak
anti-mesenteric side bowel anastomoses
of two segments of the ● As small as possible without compromising the intestinal blood
intestine supply
1
Connection between the proximal and the distal end of the colon CHARACTERISTICS OF A GOOD OSTOMY
2
Often employed where the ileum is connected to the colon, which has 1. Located within the rectus muscle, to minimize parastomal
a wider diameter; the ileum is connected to the side of the colon hernia1
3
Often applied when a portion of the small intestine is distended, 2. Ideally placed in a location where the patient can easily see
and you want to bypass an obstruction; the dilated bowel is then and manipulate it2
connected to the distal end of the colon or to the end of the intestine 3. The surrounding abdominal soft tissue should be as flat as
4
Usually performed when the end of the intestines is edematous possible to ensure a tight seal and prevent leak3
or swollen; it is anastomosed side-to-side; the bowel that will be 4. It must be as small as possible without compromising the
anastomosed to must not be edematous, since it will be at risk for intestinal blood supply, usually the width of two to three fingers4
1
leakage when the edema subsides The rectus muscle will act as a sphincter
2
In the preparation of the patient, the area where the ostomy will be
ANASTOMOSES AT HIGH placed is already marked; the location is usually between the
CHARACTERISTICS OF A umbilicus to the iliac crest or to the ASIS
RISK OF LEAK OR
GOOD ANASTOMOSIS 3
The ostomy should not be near the iliac crest or the ASIS because the
STRICTURE
1. High in the distal rectum or colostomy bag cannot be placed
4
anal canal If the ostomy is wide, there will be a higher risk for leakage
1. Well-vascularized, healthy 2. Irradiated or diseased
limbs of bowel intestine, including ● In order to make appliance use easier, a protruding nipple
2. Bowel without tension1 perforation with peritoneal is fashioned by everting the bowel
3. Normotensive, well- spoilage
nourished patient 3. Malnourished,
immunosuppressed, or very
ill patients2
SURG II |1 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
○ Prolapse of the stoma
○ Rare: Dehydration & skin irritation
Figure. Different ostomies: colostomy and ileostomy
CASE
This is a case of a 45-year-old miner who accidentally sustained multiple
injuries secondary to a blasting injury inside a mine tunnel. He was
rushed immediately to the Mines’ Hospital where emergency measures
were done and was referred to SLU Hospital of Sacred Heart for further
evaluation and management. In the minor OR-ER, PE findings include a
BP 80/60mmHg CR 110/min RR 25/min Temp 37.8C with second and
third degree burns on the head and neck, abdomen, and upper
extremities. Abdominal wall defect was noted in the left lower quadrant
area with left colonic perforation and fecal materials scattered in the
peritoneal cavity. He was scheduled for Emergency Exploratory
Laparotomy.
● What is the most practical operation that could be done for
this particular patient?
Figure 3. Colostomy
COMPLICATIONS OF COLOSTOMY
● The patient was subjected to exploratory laparotomy to clean the Colostomy May occur in the early post-operative period, as a
peritoneal cavity and repair the damage, but the most important necrosis1 result of impaired vascular supply
thing is to divert the intestinal contents by doing ileostomy. Less problematic with a colostomy than with an
● An example of ostomy where it shows the opening/stoma which ileostomy, because the stool is less irritating to the
shows the diversion Retraction skin than succus entericus
Skin irritation is less common than with ileostomy
Herniation at the area of the colostomy
Parastomal
hernia Most common late complication of colostomy,
and requires repair if it is symptomatic
Often seen in patients with high abdominal
Prolapse
pressure or coughing
Rare after colostomy; it is more common in
Dehydration
ileostomy
1
A quite common complication, especially when one places numerous
sutures around the colostomy; as much as possible, avoid placing
numerous sutures, as it causes devascularization
Figure 2. Examples of Ostomies
● You have to properly care for the stoma of your ileostomy, so you 2. ILEOSTOMY
apply your colostomy bag. a. TEMPORARY ILEOSTOMY
● A temporary ileostomy is often used to “protect” an
1. COLOSTOMY anastomosis that is at the risk for leak
● End or loop colostomy ○ In this setting, the stoma is often constructed as a
● Most colostomies are created as end colostomies, rather loop ileostomy, where a segment of a distal ileum
than loop colostomies is brough
○ Most colostomies are created on the left side of ● Loop ileostomy closure can often be done without a formal
the colon; an abdominal defect is created and the laparotomy
end of the colon is mobilized through it ● The timing of ileostomy closure should take into account
● Closure of a colostomy usually requires laparotomy anastomotic healing, as well as the patient’s overall condition
● Complication of colostomy: ● Takedown of ileostomy should be delayed until chemotherapy
○ Necrosis due to impaired vascular supply is completed
○ Retraction of the stoma
○ Parastomal hernia
SURG II |2 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Less common after an ileostomy than after a
Parastomal
colostomy, but can cause poor appliance fitting,
hernia
pain, obstruction or strangulation
II. OPERATIVE PRELIMINARIES
A. BOWEL PREPARATION
● Decreasing the bacterial load
● Decreasing the incidence of post op infection
● Polyethylene glycol (PEG) solutions or sodium phosphate
● Antibiotic prophylaxis
Figure 4. Example of Temporary Ileostomy ● Mechanical bowel preparation refers to the use of
Ideal location of ileostomy cathartics to rid the colon of solid stool the night before
b. PERMANENT ILEOSTOMY surgery
● Required after total proctocolectomy or in patients with ○ The most commonly used regimens include
obstruction polyethylene glycol (PEG) or sodium phosphate, or
○ Performed when the distal bowels (rectum, anal any laxatives and enema
opening) are removed ● Chemical bowel preparation refers to the use of
● An end ileostomy is the preferred configuration for a antibiotics as prophylaxis
permanent ileostomy ○ Broad-spectrum parenteral antibiotic(s) with
○ The end of the small intestine is brought through activity against aerobic and anaerobic enteric
the abdominal wall defect and matured pathogens should be administered prior to skin
c. END ILEOSTOMY incision and re-dosed as needed, depending on
● Preferred configuration for a permanent ileostomy the length of the operation
B. STOMA PLANNING
● Ideal placed in a location that can easily be seen &
manipulated, within the rectus muscle, & below the belt line,
away from both the costal margin & iliac crest
III. DISEASES OF THE COLON
INFLAMMATORY BOWEL DISEASE
● Ulcerative colitis vs. Crohn’s disease [see Appendix]
IV. COLORECTAL DISEASES
A. DIVERTICULAR DISEASE
● Diverticular disease is a clinical term used to describe the
Figure. Types of ileostomy presence of symptomatic diverticula
COMPLICATIONS OF ILEOSTOMY CLINICAL SPECTRUM OF DIVERTICULAR DISEASE
1. Stoma necrosis - caused by skeletonizing the distal small DIVERTICULOSIS DIVERTICULITIS
bowel or an overly tight fascial defect Refers to inflammation and
2. Stroma retraction Presence of diverticula
infection associated with
3. Bypass of fluid absorbing capability of the colon without inflammation
diverticula
4. Dehydration with fluid and electrolyte imbalance TRUE DIVERTICULA FALSE DIVERTICULA
● Ileostomy output: <1,500mL/day Only the mucosa and the
5. Skin irritation Sac-like herniation involving muscularis mucosa have
6. Obstruction all layers of the bowel herniated through the colonic
wall
COMPLICATIONS OF ILEOSTOMY ● 5% of patients with complicated diverticulitis develop fistulas
May occur in the early post-operative period, as between the colon and an adjacent organ
a result of skeletonizing the distal small ● Colovesical fistulas are most common, followed by
bowel and/or creating an overly tight colovaginal and coloenteric fistulas
fascial defect ● Colocutaneous fistulas are a rare complication of diverticulitis
● Results from the devascularization of
Stoma necrosis
the intestine 1. BLEEDING DIVERTICULUM
● Limited mucosal necrosis above the fascia ● Results from erosion of the periventricular arteriole
may be treated expectantly, but necrosis which results to massive hemorrhage
below the level of the fascia requires ● Bleeding stops spontaneously in 80% of patients
surgical revision
May occur early or late and may be exacerbated
Stoma retraction
by obesity
The creation of an ileostomy bypasses the
Dehydration & fluid-absorbing capacity of the colon, and
fluid and dehydration with fluid and electrolyte
electrolyte abnormalities is common
abnormalities ● Ileostomy output should be maintained at
less than 1500 mL/day
Associated with the intestinal juice (succus
Skin irritation
entericus)
May occur intra-abdominally, or at the site
Obstruction
where the stoma exits the fascia Figure 5. Bleeding Diverticulum
SURG II |3 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
B. ADENOCARCINOMA AND COLONIC POLYPS Obesity and sedentary lifestyle dramatically
1. COLORECTAL CARCINOMA (CRCA) increase cancer-related mortality in a number of
● Most common malignancy of the GIT malignancies, including CRCA
● >150,000 new cases are dx per year in the US Patients with long-standing colitis from IBD are
● Similar incidence in men & women Inflammatory
at increased risk for the development of
bowel disease
colorectal cancer
1. Cigarette smoking is associated with an
increased risk of colonic adenomas,
especially after more than 35 years of use
Other risk 2. Acromegaly is associated with increased
factors levels of circulating human growth
hormone and IGF-1, which increases risk
3. Pelvic irradiation may increase the risk
of developing rectal carcinoma
● Pathogenesis
○ Colorectal cancer is associated with genetic defects
and molecular abnormalities, and includes the
following:
1. Activation of oncogenes (K-ras)
2. Inactivation or loss of tumor
suppressor genes
▪ Defects in the APC gene were first
described in patients with familial
adenomatous polyposis
▪ DCC - mutation seen in >70% of
CRCA
▪ p53 mutations in 75% of cases
Figure 7. CRCA Pathogenesis
2. COLORECTAL POLYPS
● Polyp is a non-specific clinical term that describes any
projection from the surface of the intestinal mucosa,
Figure 6. Examples of CRCA. Not only does it cause
regardless of its histologic nature
obstruction, but can ulcerate the colon, and cause lower GI
bleeding
SUMMARY OF THE HISTOLOGIC CLASSIFICATION
COLORECTAL POLYPS
RISK FACTORS FOR COLORECTAL CARCINOMA
1. Tubular adenoma
Aging is the dominant risk factor for
Neoplastic 2. Villous adenoma
colorectal cancer, with incidence rising steadily
3. Tubulovillous adenoma
Aging after the age of 50
1. Familial Juvenile polyposis
● More than 90% of cases are diagnosed in
Hamartomatous 2. Peutz-Jeghers syndrome
people older than 50 years old
(Juvenile) 3. Cronkhite-Canada syndrome
Approximately 80% of cases occur
Hereditary risk 4. Cowden’s syndrome
sporadically, while 20% arise in patients with
factors 1. Pseudopolyp
a known family history of colorectal cancer Inflammatory
2. Benign Lymphoid Polyp
Diet high in saturated or
Hyperplastic -
High risk polyunsaturated fats- high
animal fat, low fiber diet
Diet high in oleic acid (olive
Environmental No risk
oil, coconut oil and fish oil)
and dietary
Diet high in vegetable fiber,
factors
and ingestion of calcium,
Decrease risk
selenium, vitamins A, C, E,
(protective)
carotenoids and plant
phenols
Figure 8. Colorectal Polyp
SURG II |4 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
a. NEOPLASTIC POLYPS
● Adenomatous polyps are common, occurring in up to 25% of the
population older than 50 years of age
● These lesions are dysplastic
● The risk of malignant degeneration is related to both the size
and the type of polyp
o Tubular adenoma: 5%
o Villous adenoma: 40%
o Tubulovillous adenoma: 22%
o Rare in <1 cm polyp; the incidence increases with size
o The risk of carcinoma in a polyp larger than 2 cm is 35% to
50%
NEOPLASTIC POLYPS
LOCATION
ADENOMA TYPE
DESCRIPTION
Tubular1 Figure 10. Peutz-Jeghers syndrome. Histopathology reveals the
Throughout the large intestine
Tubulovillous arborizing pattern of smooth muscle proliferation
Villous 2
Rectum
1
Tubular adenoma is the most common of the three types
2
Villous adenoma carries the highest morbidity and mortality rates
b. HAMARTOMATOUS (JUVENILE) POLYPS
● Hamartomatous polyps are usually not premalignant
o These lesions are the characteristic polyps of
childhood, but may occur at any age
● Bleeding is a common symptom
● intussusception and/or obstruction may occur
● These lesions are often associated with mutation in PTEN
FAMILIAL JUVENILE POLYPOSIS
● Autosomal dominant disorder, in which the patient develops
hundreds of polyps in the colon and rectum
○ These lesions may degenerate into adenomas, and Figure 11. Melanin spots on the lips
eventually carcinoma ● Treatment:
● Treatment: Surgery 1. Surgery for symptoms such as obstruction or
○ If rectum is spared: Total abdominal colectomy with bleeding
ileorectal anastomosis 2. Screening: baseline colonoscopy & upper
○ Involvement of rectum: Total proctocolectomy endoscopy at the age of 20, followed by annual
flexible sigmoidoscopy thereafter
Figure 9. Familial juvenile polyposis
• Polyps are usually scattered into the entire large intestine
and may involve the small intestines
•
PEUTZ-JEGHERS SYNDROME
● Characterized by polyposis of the small intestine, and to a Figure 12. Hematoma screening
lesser extent, the colon and rectum
o Melanin spots: buccal mucosa & lips CRONKHITE-CANADA SYNDROME
o Carcinoma may occasionally develop from these ● Disorder in which patients develop gastrointestinal polyposis +
polyps alopecia, cutaneous pigmentation and atrophy of the
fingernails and toenails
● Diarrhea is a prominent syndrome, accompanied by vomiting,
malabsorption and protein-losing enteropathy
SURG II |5 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
o APC mutation testing is positive in 75% of cases
● Clinically, patients develop hundreds and thousands of
adenomatous polyps shortly after puberty
● The lifetime risk of colorectal cancer in FAP patients approaches
100% by age 50
● At risk for developing duodenal adenomas but can occur anywhere
in the GIT, particularly in the duodenum
● Risk of Periampullary carcinoma
● Upper endoscopy is therefore recommended for surveillance every
1-3 years beginning age 25-30 years old.
Figure 13. Cronkhite-Canada Syndrome
COWDEN’S SYNDROME
● An autosomal dominant disorder with hamartomas of all three
embryonal cell layers
● Facial trichilemmomas, breast carcinoma, thyroid disease and
gastrointestinal polyps are typical of his syndrome
Figure 17. FAP
SCREENING FOR FAMILIAL ADENOMATOUS POLYPOSIS
APC testing is done in relatives of patients who
are known to be APC testing positive
APC testing
● If APC testing is negative, the relative can
be screened starting at age 50 years
First degree relatives of FAP patients, beginning
Annual Flexible
Figure 14. Cowden’s Syndrome at age 10 to 15 years of age until polyps are
sigmoidoscopy
identified
c. INFLAMMATORY POLYPS (PSEUDOPOLYPS) Periampullary Upper endoscopy for surveillance every 1 to 3
● These lesions are multiple and not premalignant carcinoma years, beginning at age 25 to 30 years
● Inflammatory polyps occur most commonly in the context of TREATMENT FOR FAMILIAL ADENOMATOUS POLYPOSIS
inflammatory bowel disease, but may also occur after Once the diagnosis of FAP has been made, and
amebic colitis, ischemic colitis and schistosomal colitis polyps are developing
● Factors affecting the choice of operation:
1. Age of the patient
2. Presence and severity of symptoms
3. Extent of rectal polyposis
4. Presence and location of cancer or
desmoid tumors
Surgery
● Operative procedures considered:
Figure 15. Pseudopolyps in inflammatory bowel disease 1. Total proctocolectomy with end
ileostomy
d. HYPERPLASTIC POLYPS 2. Total abdominal colectomy with
● Usually small (<5mm) ileorectal anastomosis
● Histology: hyperplasia without dysplasia 3. Restorative proctocolectomy with ileal
● Not premalignant except for polyps >2cm pouch-anal anastomosis with or without
a temporary ileostomy
COX-2 May slow or prevent the development of polyps
inhibitors (celecoxib, sulindac)
b. ATTENUATED FAMILIAL ADENOMATOUS POLYPOSIS
● The mutation is located at the 3’ to 5’ end of the APC gene
● APC gene mutations are present only in about 30% of patients
● When present, it is usually expressed in an autosomal dominant
pattern
● Variant of FAP, which patients present later in life, with fewer
polyps (usually 10 to 100)
Figure 16. Histology of Hyperplastic Polyps
● Predominantly located in the right colon (cecum, ascending colon,
hepatic flexure, and proximal two-thirds of the transverse colon)
3. INHERITED COLORECTAL CARCINOMA
a. FAMILIAL ADENOMATOUS POLYPOSIS (FAP) ● Colorectal cancer develops in more than 50% of these patients, but
occurs later (average age of 55 years)
● Rare autosomal dominant condition, accounting for 1% of all
colorectal adenocarcinomas ● Patients are also at risk for duodenal polyposis
● Mutation in the APC gene, located on chromosome 5q
SURG II |6 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
SCREENING FOR ATTENUATED FAMILIAL ADENOMATOUS Yearly proctoscopy -
POLYPOSIS Prophylactic TAHBSO
Screening colonoscopy is recommended beginning (Total Abdominal Should be considered in women who
Colonoscopy age 13 to 15 years, then every 4 years at 28 Hysterectomy Bilateral have completed childbearing
years, and then every 3 years Salphingoopherectomy
TREATMENT FOR ATTENUATED FAMILIAL ADENOMATOUS
POLYPOSIS d. FAMILIAL COLORECTAL CANCER
Patients are often candidates for a total ● Non-syndromic familial colorectal cancer accounts for 10% to
Surgery abdominal colectomy with ileorectal 15% of patients with colorectal cancer
anastomosis o The lifetime risk of developing colorectal cancer increases
COX-2 Prophylaxis with COX-2 inhibitors may also be with a family history of the disease
inhibitors appropriate ▪ 6% in patients with no family history
▪ 12% if one first-degree relative is affected
c. HEREDITARY NON-POLYPOSIS COLON CANCER (LYNCH’S ▪ 35% if two first-degree relatives are affected
SYNDROME) ● Age of onset also impacts risk, and a diagnosis before the age of
● Lynch’s syndrome (HNPCC) is more common than FAP, but still 50 is associated with a higher incidence in family members
extremely rare
● It is an autosomal dominant syndrome, and arise from errors in SCREENING FOR FAMILIAL COLORECTAL CANCER
mismatch repairs Recommended every 5 years, beginning age
● It is characterized by the development of colorectal cancer at an Colonoscopy 40, or beginning 10 years before the age of
early age (average age of 40-45 years) earliest diagnosed patient in the pedigree
● Approximately 70% of affected individuals will develop colorectal
cancer V. SCREENING AND SURVEILLANCE
● Cancers appear in the proximal colon more often than in sporadic A. FECAL OCCULT BLOOD TESTING (FOBT)
colorectal cancer, and have a better prognosis regardless of ● Reduces colorectal CA mortality by 33% and metastasis by
stage 50%
o The risk of synchronous or metachronous colorectal ● Low sensitivity, low specificity
carcinoma is 40% ● Positive test should be followed by colonoscopy
● HNPCC may also be associated with extracolonic malignancies, B. FLEXIBLE SIGMOIDOSCOPY
including the following: ● Screening every 5 years: 60 to 70% reduction in mortality
1. Endometrial carcinoma (most common) from CRCA
2. Ovarian carcinoma ● Require colonoscopy if with findings
3. Pancreatic carcinoma C. FOBT + FLEXIBLE SIGMOIDOSCOPY
4. Stomach carcinoma ● FOBT Annually + flexible sigmoidoscopy every 5 years is
5. Small bowel carcinoma preferred than FOBT or Flexible Sigmoidoscopy alone
6. Biliary carcinoma D. COLONOSCOPY
7. Urinary tract carcinoma ● Most accurate and most complete method for examining the
large bowl
● Highly sensitive or detecting even small polyps (<1 cm)
● Allows biopsy, polypectomy, control of hemorrhage, and
dilation of strictures
● Colonoscopy is both diagnostic and Therapeutic
● Requires mechanical bowel preparation and sedation as the
procedure is associated with discomfort
● Risk of major complication (perforation/hemorrhage) is
extremely low (0.2-0.3%)
E. AIR-CONTRAST BARIUM ENEMA
● Good sensitivity for polyps >1cm (90% sensitivity)
● Accuracy is greatest at the proximal colon, but may be
compromised in the sigmoid colon if there is significant
diverticulosis
● Requires bowel prep
● Positive results require colonoscopy
SCREENING FOR HEREDITARY NON-POLYPOSIS COLON
CANCER
Screening colonoscopy is recommended
beginning either age 20 to 25 years or 10
Colonoscopy
years younger than the youngest age at
diagnosis in the family, whichever comes first
Transvaginal UTZ
Recommended annually after age 25 to 35
+
years because of risk of endometrial
Endometrial
carcinoma
aspiration biopsy
Annual proctoscopy is necessary because the
Proctoscopy
risk of developing rectal cancer remains high
Figure 18. Air-contrast barium enema
TREATMENT FOR HEREDITARY NON-POLYPOSIS COLON
CANCER F. CT COLONOGRAPHY (VIRTUAL COLONOSCOPY)
Done once adenomas or a colon CA is ● Examines the entire colon
Total colectomy with ● Non-invasive
diagnosed because of a 40% risk of
ileorectal anastomosis ● Makes use of helical CT technology & 3D reconstruction
developing a second colon cancer
SURG II |7 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
● Sensitivity may be as good as colonoscopy (but still VI. COLON CANCER STAGING
insensitive for small polyps)
● Colonoscopy required for positive results
● It is also useful for imaging the proximal colon in cases of
obstruction or if a colonoscopy cannot be completed
Figure 20. Stages of Colon CA
STAGING AND EXTENT OF COLON CARCINOMA
Figure 19. Virtual colonoscopy vs CT colography I Within the mucosa
SCREENING AND SURVEILLANCE II Involves up to the muscularis propria
ADVANTAGES DISADVANTAGES Extends up to the serosa, and involves
III
the surrounding structures
FOBT Ease of use and May not detect most
noninvasive polyps VII. ROUTES OF SPREAD AND NATURAL HISTORY
Low cost Low specificity CASE: This is a case of a 40-year-old female patient who consulted
Good sensitivity with Colonoscopy in the ER of the SLU hospital because of hematochezia and small
repeated testing requires to positive caliber stools. The condition started about 3 months prior to
result admission as on-off anorectal pain associated with alternating
Poor compliance constipation and diarrhea. She sought consultation and after
with serial testing fecalysis, she prescribed antiamoebic drugs. One month PTA, the
symptoms recurred and on rectal examination, a partially
SIGMOIDOSCOPY Examines colon Invasive obstructing mass was palpated so she was advised colonoscopy.
most at risk Uncomfortable Colonoscopic findings revealed an ulcerating mass about 2-3cms in
Very sensitive for Slight risk of diameter, about 6cms from the anal verge. A biopsy revealed a
polyp detection in perforation or rectal adenocarcinoma. Which colonic operation would be ideal for
left colon bleeding this patient?
Does not require full May miss proximal
bowel prep (enemas lesions
only) Colonoscopy
required if polyp
identified
COLONOSCOPY Examines the entire Most invasive;
colon uncomfortable and
Highly sensitive and requires sedation
specific Requires bowel
Therapeutic preparation
Risk of perforation or
bleeding
Costly
Figure 21. Colon CA Route of Spread
Important factors:
● Regional Lymph Node Involvement: most common form
DOUBLE- Examines the entire Requires bowel
of spread
CONTRAST colon preparation
● Tumor size
BARIUM ENEMA Good sensitivity for Less sensitivity for
● Poorly differentiated histology
polyps >1 cm polyps <1 cm
● Lymphovascular invasion
May miss lesions in
● Depth of invasion
the sigmoid colon
Colonoscopy
VIII. STAGING OF COLORECTAL CANCER
required for positive
TNM STAGING OF CRCA
result
TUMOR STAGE (T)
TUMOR
COMPUTED Non-invasive Requires bowel DEFINITION
STAGE
TOMOGRAPHY Sensitivity may be as preparation
Tx Cannot be assessed
COLONOGRAPHY good as colonoscopy Insensitive for small
T0 No evidence of cancer
polyps
Minimal experience Tis Carcinoma in situ
and date T1 Tumor invades submucosa
Colonoscopy T2 Tumor invades muscularis propria
required for positive Tumor invades through muscularis propria into
result T3 subserosa or into non peritonealized pericolic or
perirectal tissues.
SURG II |8 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
Tumor directly invades other organs or tissues or ○ Tx: segmental colectomy
T4
perforates the visceral peritoneum of specimen. ● Stage I and II (T1-3, N0, M0)
NODAL STAGE (N) ○ Localized Colonic Cancer
NODAL STAGE DEFINITION ○ Tx: surgical resection
○ Adjuvant chemotherapy has been suggested for
Nx Regional lymph nodes cannot be assessed
selected patients with Stage II disease (young
N0 No lymph nodes metastasis
patients, tumors with “high risk” histologic findings
Metastasis to 1-3 pericolic or perirectal lymph ● Stage III (Tany, N1, M0)
N1
nodes ○ Tumor with any size but LN metastasis
Metastasis to 4 or more pericolic or perirectal ○ Adjuvant chemotherapy is usually routine before
N2
lymph nodes doing any surgery
Metastasis to any lymph node along a major ● Stage IV (Tany, Nany, M1)
N3 named vascular trunk e.g. in the inferior ○ Distant Metastasis
mesenteric trunk or superior mesenteric trunk ○ Most common site: Liver
DISTANT METASTASIS (M) ■ 20% are potentially resectable for cure
DISTANT ■ 20-40% 5yr survival
DEFINITION
METASTASIS ■ All patients require adjuvant
chemotherapy
Mx Presence of distant metastasis cannot be assessed ○ Second MC site: Lungs
M0 No distant metastasis ■ 20% of patients with Colorectal CA
○ The remainder of patients with Stage IV disease
M1 Distant metastasis present
cannot be cured surgically
■ The focus of the treatment should be
STAGING AND EXTENT OF COLON CARCINOMA palliative
Stage TNM 5-yr Survival
I T1-2, N0, M0 70-95% IX. THERAPY FOR RECTAL CA
II T3-4, N0, M0 54-65% A. PRINCIPLES OF RESECTION
III Tany, N1-3, M0 39-60% ● The principles of complete resection of primary tumor, its
IV Tany, Nany, M1 0-16% lymphatic bed, and any other involved organ apply
● Tany – tumor of any size ● Anatomy of the pelvis and proximity of other structures
● Nany – any nodes (ureters, bladder, prostate, vagina, iliac, vessels, and
● In colorectal carcinoma, the most common site of metastasis of sacrum) make resection more challenging and often require
cancer is the liver due to its rich blood supply. a different approach than for colonic adenocarcinoma
o After which distant metastasis to the lungs may also occur. ● Difficult to achieve negative margins due to anatomic
It can also go high in your brain. limitations of the pelvis
● Local recurrence is higher
IX. THERAPY FOR COLONIC CA ● Relative paucity of SI and other radiation-sensitive structures
A. PRINCIPLES OF RESECTION in the pelvis makes it easier to treat with radiation therapy
● Objective: Remove the primary tumor and lymphovascular B. LOCAL THERAPY
supply (Radical dissection) ● Transanal excision (full thickness/mucosal) approach for
● Any adjacent organ that has been invaded should be non-circumferential, benign villous adenomas of the rectum -
resected en bloc with the tumor. If it reaches the uterus, do for distal 10cm
hysterectomy (consult a gynecologic surgeon) ● Does not allow pathologic exam of the LNs -> understage
● If all the tumor cannot be removed, a palliative procedure CA
should be considered (Diverting colostomy or distal end C. RADICAL RESECTION
colostomy/ Hartmann’s procedure) ● Preferred for most rectal carcinoma
● Others have suggested that the # of negative LN and/or the ● Removal of the involved segment of the rectum along with
LN ratio (+LN:total LN) may further improve staging its lymphovascular supply
● If unexpected metastatic disease is encountered at the time ● Total mesorectal excision (TME)
of a laparotomy, the primary tumor should be resected if ○ Sharp dissection along anatomic planes to ensure
technically feasible and safe. complete resection of the rectal mesentery during
LARs
B. STAGE-SPECIFIC THERAPY ○ Decreases local recurrence rates and improves
● Stage 0 (Tis, N0, M0) long-term survival rates
○ Polyps containing carcinoma in-situ ○ Less blood loss and less risk pelvic nerves and
○ Pedunculated & sessile polyps may be completely presacral plexus than blunt dissection
removed endoscopically ● Pelvic Exenteration
○ If the polyps cannot be removed entirely, a ○ Done when other pelvic organs are involved
segmental resection is done ○ APR (Abdominoperineal resection) plus en bloc
● Stage 1 (T1, N0, M0) resection of the ureters, bladder, prostate, or
○ The malignant polyp uterus and vagina
○ The risk of LN metastasis depends primarily on the ○ A permanent colostomy and ileal conduit to drain
depth of invasion the urinary tract
○ Invasive CA in the head of pedunculated polyp
without involvement of the stalk may be
completely resected endoscopically
○ Lymphovascular invasion poorly differentiated
histology tumor within 1mm of the resection
margin
○ Greatly increases the risk for local recurrence and
metastatic spread
○ Invasive cancer in a sessile polyp Figure 22. Pelvic Exenteration
SURG II |9 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
• An example of radical resection with an establishment of
ileal conduit after pelvic exenteration
D. STAGE-SPECIFIC THERAPY
● Pre-treatment staging often relies on endorectal ultrasound
(determine the T & N status of a rectal cancer)
● Ultrasound is accurate in assessing tumor depth, but less
accurate in diagnosis nodal involvement
● MRI is useful to assess mesorectal involvement
● Stage 0 (Tis [tumor in-situ], N0, M0)
○ Local excision
○ 1cm margin
Figure 25. Stage II and II Algorithm
Figure 23. Rectal Adenocarcinoma work-up
Figure 26. Stage IV Algorithm
● Advantage of pre-op chemo RT:
○ Tumor shrinkage (reduce the size of tumor with
chemoradiation)
○ Increase likelihood of resection and sphincter-
sparing procedure
○ Tumor downstaging by treating locally involved
LNs
○ Decrease risk to systemic involvement
E. FOLLOW-UP AND SURVEILLANCE
● A COLONOSCOPY should be performed within 12 months after the
Figure 24. Stage I Algorithm. diagnosis of the original cancer
Invasive CA confined to the head of the pedunculated polyp = low risk ● If normal, colonoscopy should be repeated every 3-5 years
mets = POLYPECTOMY WITH CLEAR MARGIN thereafter
Radical resection is done for later stages ● CEA is often followed every 2-3 months for 2 years.
● Locally advanced Rectal CA F. RECURRENT COLORECTAL CARCINOMA
○ Stage II: Localized Rectal CA ● 20-40% of patients who have undergone curative intent surgery
○ Stage III: LN Metastasis for CRCA will eventually develop recurrent disease, usually within
○ Preoperative chemoradiation - most 2 years of the initial diagnosis
appropriate therapy for locally advanced rectal CA ● Recurrence after colon CA resection usually occurs at the local site
within the abdomen, or in the liver or lungs
● Adjuvant therapy should be administered before salvage surgery
(resect the tumor to relieve symptoms like compression on ovary
etc.)
● Radical resection may require extensive resection of pelvic organs
SURG II |10 of 10 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
CHECKPOINT!!! Matching Type
1. Erosions of periventricular arteriole
2. Activation of kras and inactivation/loss of dcc, apc
and p53 genes
3. Causes bleeding and intussusception &/or
obstruction
4. Polyposis of small intestines causing melanin on the
lips
5. Gastrointestinal polyps with associated atrophy of
nails and alopecia
6. Autosomal dominant causing early malignancy in
proximal colon
A. Peutz Jeghers Syndrome B. Lynch’s Syndrome
C. Hamartomatous Polyps D. Diverticulum
E. Colorectal cancer
F. Cronkhite-Canada Syndrome
(6) B. (5). F (4). A (3). C (2) E (1) D
Figure 27. Rectal Adenocarcinoma Algorithm
APPENDIX LIFTED FROM 2021
A. ULCERATIVE COLITIS VERSUS CROHN’S DISEASE
Note. Not discussed
COMPARISON OF ULCERATIVE COLITIS AND CROHN’S DISEASE
BASIS ULCERATIVE COLITIS CROHN’S DISEASE
Site of origin, localization Rectum Terminal ileum
Proximally contiguous (diffuse ‘Skip’ lesions (segmental,
Pattern of progression
involvement of the GI tract) discontinuous)
Involvement of the:
● Colon Left > right Right > left
● Rectum Commonly involved Typically spared
Aphtoid ulcers, confluent deep linear
Ulcers Superficial ulcers
ulcers
Pseudopolyps Common Uncommon
Cobblestone-pattern Absent Present
Deep fissures Absent, except in fulminant colitis Present
Fistulae Absent, except in fulminant colitis Present
Thickness of inflammation Submucosa or mucosa Transmural
Fat wrapping Absent Present
Lead pipe colon or barium x-ray String sign on barium x-ray
Radiologic findings
Risk of colon cancer Marked increase Slight increase
B. PATHOGENESIS OF COLORECTAL CARCINOMA
Figure 13. Schematic diagram showing the progression from normal colonic epithelium to carcinoma of the colon
SURG II |11 of 1 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
C. SCREENING MODALITIES FOR ASYMPTOMATIC INDIVIDUALS
ADVANTAGES AND DISADVANTAGES OF SCREENING MODALITIES FOR ASYMPTOMATIC INDIVIDUALS
MODALITY ADVANTAGES DISADVANTAGES
1. May not detect most polyps
1. Ease of use and non-invasive
2. Low specificity
Fecal occult blood 2. Low cost
3. Colonoscopy required for positive results
3. Good sensitivity with repeat testing
4. Poor compliance with serial testing
1. Invasive and uncomfortable
1. Examines colon most at risk
2. Slight risk of perforation or bleeding
Sigmoidoscopy 2. Very sensitive for polyp detection in the left colon
3. May miss proximal lesions
3. Does not required full bowel preparation (enema only)
4. Colonoscopy required if polyp identified
1. Most invasive; uncomfortable and requires sedation
1. Examines the entire colon
2. Requires bowel preparation
Colonoscopy 2. Highly sensitive and specific
3. Risk of perforation or bleeding
3. Therapeutic
4. Costly
1. Requires bowel preparation
1. Examines the entire colon 2. Less sensitivity for polyps <1 cm
Double-contrast barium enema
2. Good sensitivity for polyps >1 cm 3. May miss lesions in the sigmoid colon
4. Colonoscopy required for positive result
1. Requires bowel preparation
1. Non-invasive 2. Insensitive for small polyps
Computed tomography colonography
2. Sensitivity may be as good as colonoscopy 3. Minimal experience and date
4. Colonoscopy required for positive result
D. SUMMARY FOR SCREENING GUIDELINES FOR COLORECTAL CANCER
SCREENING GUIDELINES FOR COLORECTAL CANCER
POPULATION INITIAL AGE RECOMMENDED SCREENING TEST
1. Annual FOBT, or
2. Flexible sigmoidoscopy every 5 years, or
Average risk 50 years old 3. Annual FOBT + flexible sigmoidoscopy every 5 years, or
4. Air-contrast barium enema every 5 years, or
5. Colonoscopy every 10 years
• Colonoscopy at first detection, then colonoscopy in 3 years
Adenomatous polyp 50 years old
• If no further polyps, colonoscopy every 5 years
• If polyps, colonoscopy every 3 years
• Annual colonoscopy for >5 adenomas
• Pretreatment colonoscopy, then at 12 months after curative resection; then
Colorectal cancer At diagnosis • Colonoscopy after 3 years; then
• Colonoscopy every 5 years, if no new lesions
At diagnosis; then after 8 years for pancolitis; after
Ulcerative colitis, Crohn’s disease Colonoscopy with multiple biopsies every 1 to 2 years
15 years for left-sided colitis
1. Annual flexible sigmoidoscopy
FAP 10 to 12 years old
2. Upper endoscopy every 1 to 3 years after polyps appear
1. Annual flexible sigmoidoscopy
Attenuated FAP 20 years old
2. Upper endoscopy every 1 to 3 years after polyps appear
1. Colonoscopy every 1 to 2 years
HNPCC 20 to 25 years
2. Endometrial aspiration biopsy every 1 to 2 years
40 years old, or
Familial colorectal cancer, first- 1. Colonoscopy every 5 years
10 years before the age of the youngest affected
degree relative 2. Increase frequency if multiple family members are affected, especially before 50 years old
relative
SURG II |12 of 1 [ NAVA, LUCABEN, PACLEB ]
SURGERY II
Saint Louis University School of Medicine MMXXII
M.08 COLON, RECTUM, AND ANUS (PARTS 5 & 6) metastasis
Dr. Lagyo | October 22, 2020 • Carcinoid tumors in the proximal colon are less common and are
more likely to be malignant.
OUTLINE • Size also correlates with risk of malignancy, and tumors less than
I. Therapy for rectal caner 2 cm in diameter rarely metastasize.
II. Other neoplasms • Treatment:
III. Anal canal and perianal tumors o Local resection: Small carcinoids
IV. Benign conditions o Radical surgery: Larger tumors and tumors with obvious
V. Anorectal sepsis and cryptoglandular disease invasion into the muscularis
VI. Fistula in ano o Symptoms of carcinoid syndrome are treated with
VII. Necrotizing soft tissue infection of the perineum somatostatin analogues (Octreotide), and/or interferon-
alpha
VIII. Rectovaginal fistula
IX. Pilonidal disease
2. ADENOCARCINOIDS
X. Trauma
• Have histologic features of both carcinoid tumors and
XI. Foreign body entrapment adenocarcinoma
I. THERAPY FOR RECTAL CANCER: STAGE-SPECIFIC • Natural history: Parallel adenocarcinoma > carcinoid tumors
THERAPY • Regional and systemic metastasis are common
STAGE IV (DISTANT METASTASIS) • Treated according to the same oncologic principles as followed
• Radical resection may be required to control pain, bleeding, or for management of adenocarcinoma
tenesmus.
• Local therapy (usual requires cautery, endocavitary radiation 3. LIPOMAS
or laser ablation) may be adequate to control bleeding or • Occur most commonly in the submucosa of colorectum
prevent obstruction • Benign
• Survival is limited in patients with distant metastasis from rectal • Treatment:
carcinoma. Some patients will require palliative procedures. o Small and asymptomatic: no treatment required
• Intraluminal stents may be useful in the uppermost rectum but o Larger:
often cause pain and tenesmus lower in the rectum. § Resection through colonoscopy
§ Enucleation
ADVANTAGES OF PRE-OPERATIVE CHEMORADIATION § Limited colectomy
THERAPY
• Tumor shrinkage
• Increase likelihood of resection and sphincter-sparing procedure
• Tumor downstaging by treating locally involved LNs
• Decreases risk of systemic involvement
FOLLOW-UP AND SURVEILLANCE
• A colonoscopy should be performed within 12 months after the
diagnosis of the original cancer
• If normal, colonoscopy should be repeated every 3-5 years
thereafter
• Carcinoembryonic Antigen (CEA) is often followed every 2-3
months for 2 years
• The goal of close follow- up observation is to detect resectable
recurrence and to improve survival.
RECURRENT COLORECTAL CARCINOMA (CRCA)
• 20-40% of patients who have undergone curative intent
surgery for CRCA will eventually develop recurrent disease Figure 1. Lipomas
• Recurrence after colon CA resection usually occurs at the local
site within the abdomen, or in the liver or lungs 4. LYMPHOMA
• Rare (10% of all gastrointestinal lymphomas)
TREATMENT OF RECURRENT CRCA • Most often involves the cecum (result of spread from the
• Adjuvant therapy should be administered before salvage ileum)
surgery (resect the tumor to relieve symptoms like compression • Symptoms include bleeding and obstruction
on ovary etc.) • Treatment: Bowel resection
• Radical resection may require extensive resection of pelvic
organs
II. OTHER NEOPLASMS
1. CARCINOID TUMORS
• Occur most commonly in the GI tract (25% of which:
rectum)
• Most small rectal carcinoid tumors are benign
• Risk of malignancy increases with size
• >60% of tumors >2 cm are associated with distant
metastases
• Carcinoid syndrome: uncommon in the absence of liver
Figure 2. Lymphoma in the large intestine
SURG II |1 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
5. LEIOMYOMA 3. VERRUCOUS CARCINOMA (BUSCHKE-LOWENSTEIN TUMOR;
• Benign smooth muscle tumor GIANT CONDYLOMA ACUMINATA)
• Most common in the upper GI tract • Locally aggressive form of condyloma acuminata
• Mostly asymptomatic • Do not metastasize
• Larger lesions bleed or obstruct • Cause extensive local tissue destruction
• Treatment: Resection (difficult to differentiate leiomyoma • Treatment:
o Wide local excision
from malignant leiomyosarcoma)
o Radical resection
4. BASAL CELL CARCINOMA (BCCA)
• Rare
• Resembles BCCA elsewhere
• Raised, pearly edges with central ulceration
• Slow growing
• Rarely metastasize
• Treatment:
o Wide local excision
o Radical resection and/ or radiotherapy (RT) for large lesions
• 30% recurrence
Figure 3. Leiomyoma
6. LEIOMYOSARCOMA
• Rare in the GI tract
• Rectum is the most common site in the large intestine
• Symptoms: Bleeding and obstruction
• Treatment: Radical Resection
III. ANAL CANAL AND PERIANAL TUMORS
CARCINOMA OF THE ANAL CANAL
• 2% of all colorectal malignancies Figure 5. Basal Cell Carcinoma (BCCA) of the colon
• Anal margin (distal to the dentate line)
5. ADENOCARCINOMA
• Anal canal (proximal to the dentate line)
• Extremely rare
1. ANAL INTRAEPITHELIAL NEOPLASIA (BOWEN’S DISEASE) • Usually represents downward spread with a low rectal
• Squamous cell carcinoma in situ (CIS) adenocarcinoma
• Precursor to an invasive squamous cell carcinoma (epidermoid • Arise from anal glands or may develop in a chronic fistula
carcinoma) • Treatment: Radical resection with or without
• Associated with human papilloma virus (HPV types 16 and 18) adjuvant chemoradiation
• Perianal Paget’s Disease
2. EPIDERMOID CARCINOMA o Extramammary
• Slow growing tumor, usually presenting as anal or perianal mass o Adenocarcinoma in situ from the apocrine glands of the
perianal area
• Pain and bleeding
o Treatment: Wide local excision
• Anal margin CA:
o Resection with adequate surgical margins
6. MELANOMA
• Anal canal CA or invading the sphincter: • Rare: <1% of all anorectal CA; 1-2% of melanomas
o Chemo and radiation (Nigro protocol)
• Poor prognosis
• Radical resection or abdominoperineal resection (APR) for
recurrence • 5-year survival is less than 10%, and many patients present
with systemic metastasis and/or deeply invasive tumors at the
• Metastasis to inguinal lymph nodes is a poor prognostic sign. time of diagnosis.
• Treatment:
o Wide local excision
o Radical resection (APR)
o Adjuvant chemotherapy and radiotherapy
• Recurrence is common and usually occurs systemically
regardless of the initial surgical procedure.
Figure 4. Epidermoid Carcinoma in perianal area: preoperative
appearance
Figure 6. Melanoma
SURG II |2 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
IV. BENIGN COLORECTAL CONDITIONS
A. COLORECTAL
1. RECTAL PROLAPSE
• Circumferential, full-thickness protrusion of the rectum through
the anus
• Also been called “first-degree” prolapse, “complete”
prolapse, or procidentia.
• Female:Male ratio of 6:1
• Internal prolapse occurs when the rectal wall intussuscepts but
does not protrude and is probably more accurately described as
internal intussusception.
• Mucosal prolapse is a partial-thickness protrusion often
associated with hemorrhoidal disease and is usually treated with
Figure 8. Sigmoid Volvulus
banding or hemorrhoidectomy.
• Symptoms: • Treatment:
o Resuscitation followed by endoscopic detorsion (rigid
o Tenesmus
proctoscope)
o Sensation of tissue protruding from the anus that may or
o 40% recurrence
may not spontaneously reduce
o Elective sigmoid colectomy should be performed
o Sensation of incomplete evacuation
o Gangrene or perforation mandates immediate ex-lap
o Incontinence
(sigmoid colectomy w/ end colostomy) – safest
o Diarrhea/constipation
o Outlet obstruction • Transverse Colon Volvulus: Extremely rare, non-fixation of
the colon and chronic constipation with megacolon
• Prior to surgery:
o Colonic transit studies
o Anorectal manometry
o Tests of pudendal nerve
o Terminal motor latency
o Electromyography
o Cinedefecography
o Colonoscopy or air-contrast BE to exclude neoplasms or
diverticular disease
o CP evaluation
• Treatment: Usually surgical
o Abdominal Rectopexy
§ With or without sigmoid resection
§ Most durable repair
§ <10% recurrence
§ Fixes the rectum to the pelvic area
o Perianal Rectosigmoidectomy Figure 9. Transverse Colon Volvulus
§ No abdominal operation • Radiographic appearance of transverse colon volvulus
§ For high-risk patients resembles sigmoid volvulus, but Gastrografin enema will reveal
a more proximal obstruction
3. MEGACOLON
• A chronically dilated, elongated, hypertrophied large bowel
• May be congenital or acquired
• Evaluation must always include examination of the colon and
rectum (either endoscopically or radiographically) to exclude a
surgically correctable mechanical obstruction.
Figure 7. Rectal Prolapse
2. VOLVULUS
• Occurs when an air-filled segment of the colon twists about its Figure 10. Toxic Megacolon
mesentery
A. CONGENITAL MEGACOLON
• The symptoms of volvulus are those of acute bowel obstruction.
Patients present with abdominal distention, nausea, and • Caused by Hirschsprung’s disease; failure of migration of
neural crest cells to the distant Large Intestine
vomiting. Symptoms rapidly progress to generalized abdominal
pain and tenderness. • Absence of ganglion cells in the distal colon results in a failure of
• Sigmoid colon: 90% of cases relaxation causing a functional obstruction
• Sigmoid Volvulus: Characteristic bent inner tube or coffee • Treatment: Resection of the aganglionic segment
bean appearance on plain X-ray
SURG II |3 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
is out of proportion to P.E.
o Fever and leukocytosis
o Diagnosis: History and P.E.
o Plain films: Thumb printing (results from mucosal edema
and submucosal hemorrhage)
• Treatment:
o Bowel rest and broad spectrum antibiotics
o Indications for surgical exploration:
Figure 11. Congenital Megacolon § Failure to improve after 2-3 days of medical
management
B. ACQUIRED MEGACOLON § Progression of symptoms: deterioration of clinical
• Results from infection or chronic constipation condition
• Trypanosima cruzi destroys ganglion cells § All necrotic bowel should be resected
• Chronic constipation from slow transit or secondary to § Primary anastomosis should be avoided
medications or neurologic disorders § A second-look operation may be necessary
• Treatment: Diverting ileostomy or subtotal colectomy
Figure 14. Ischemic Colitis
Figure 12. Megacolon
6. INFECTIOUS COLITIS
4. OGILVIE’S SYNDROME PSEUDOMEMBRANOUS COLITIS
• Colonic pseudo-obstruction • AKA: Clostridium difficile Colitis
• Functional disorder in which the colon becomes massively • Leading cause of nosocomially-acquired diarrhea
dilated in the absence of mechanical obstruction
• Overgrowth of Clostridium difficile after depletion of the normal
• Most common in hospitalized patients and is associated with the commensal flora of the gut with the use of antibiotics
use of narcotics, sedentary lifestyle, and comorbid diseases • The pathogenic changes associated with C. difficile colitis result
• Results from autonomic dysfunction and severe adynamic ileus in further production of 2 toxins:
• Diagnosis is made based on the presence of massive dilatation of o Toxin A (An enterotoxin)
the colon (usually predominantly the right and transverse colon) o Toxin B (A cytotoxin)
in the absence of a mechanical obstruction. • Diagnosis:
• Treatment: o Cytotoxic assays or immunoassays
o Cessation of narcotics, anticholinergics, and medications that § Detects one or both toxins
contribute to ileus § Most sensitive and specific
o Strict bowel rest and IV hydration o Characteristic ulcers, plaques, and pseudomembranes seen
o Colonoscopic decompression endoscopically
o Recurrence in up to 40% • Treatment:
o Neostigmine effective in decompressing the dilated colon o Cessation of all offending antimicrobial agents
o Bowel rest for more severe infections
o 10 days oral Metronidazole
o Vancomycin if patient is allergic
o Hydration
o Probiotics added if condition is recurrent
to reintroduce normal flora
o Surgery for fulminant colitis (septicemia and/or evidence of
perforation)
Figure 13. Ogilvie’s Syndrome presenting with dilated segments
5. ISCHEMIC COLITIS
• Result from low flow and/or small-vessel occlusion
• Risk factors:
o Vascular Disease
o Diabetes Mellitus Figure 15. Gross pathology of florid pseudomembranous colitis due
o Vasculitis to Clostridium difficile
o Hypotension
• In addition, ligation of the inferior mesenteric artery during B. BENIGN ANORECTAL DISEASES
aortic surgery predisposes to colonic ischemia. 1. HEMORRHOIDS
• Splenic flexure: most common site of ischemic colitis • Cushions of submucosal tissue containing venules, arterioles,
• Rectum is spared because of its rich collateral circulation and smooth-muscle fibers located at the anal canal
• Signs and Symptoms: • Hemorrhoidal cushions (positions):
o Bloody diarrhea without abdominal pain o Left lateral or 3 o’clock
o Severe ischemia produces more intense abdominal pain that o Right anterior or 7 o’clock
o Right posterior or 11 o’clock
SURG II |4 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
• Excessive straining, increased abdominal pressure, and hard
stools cause increased venous engorgement of the hemorrhoidal
plexus leading to prolapse of hemorrhoidal tissue
Figure 19. Internal Hemorrhoids
INTERNAL HEMORRHOID GRADING
• FIRST DEGREE:
o Bulges into anal canal, may prolapse beyond dentate line
on straining
Figure 16. Hemorrhoids. External hemorrhoids outside and internal • SECOND DEGREE:
hemorrhoids above the dentate line o Prolapse into the anus but reduce spontaneously
• THIRD DEGREE:
EXTERNAL HEMORRHOIDS o Prolapse into the anal canal, requires manual reduction
• Distal to the dentate line • FOURTH DEGREE:
• Covered with anoderm o Prolapse but cannot be reduced, at risk for strangulation
• Thrombosis may cause significant pain (the anoderm is richly • Combined internal and external hemorrhoids straddle the
innervated) dentate line and have characteristics of both internal and
• Should not be ligated or excised without adequate local external hemorrhoids.
anesthetic HEMORRHOID TREATMENT
• Treatment: Indicated for symptomatic relief • Medical Therapy
o Dietary fiber, stool softeners, increased fluid intake and
avoidance of straining
• Rubber Band Ligation
o For persistent bleeding from first and second degree
hemorrhoids
o Rubber band strangulates the tissue, causing scarring
and preventing further bleeding or prolapse
o Complications: Urinary retention, infection, bleeding
Figure 17. External Hemorrhoids
ANAL SKIN TAGS
• Redundant fibrotic skin at the anal verge
• Often persist as residua of thrombosed external hemorrhoids
• Treatment: Indicated for symptomatic relief
Figure 20. Rubber Band Ligation
• Infrared Photocoagulation
o For small first and second degree hemorrhoids
o Instrument is applied to the apex of each hemorrhoid to
coagulate the underlying plexus
Figure 18. Anal Skin Tag
• Sclerotherapy
INTERNAL HEMORRHOIDS o For first, second, and some third degree hemorrhoids
o Sclerosing solution (phenol in olive oil, sodium morrhuate,
• Located proximal to the dentate line and covered by insensate
or quinine urea) is injected into the submucosa of each
anorectal mucosa
hemorrhoid
• May prolapse or bleed, but rarely become painful
o Complications: Infection, fibrosis
SURG II |5 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
o 2% lidocaine jelly
o Nitroglycerin ointment
§ Used locally to improve blood flow
§ Adverse effect: Throbbing headache
o Oral/topical calcium channel blockers (Diltiazem/Nifedipine)
o Arginine
o Topical Bethanechol
o Botulinum toxin (Botox)
§ Causes temporary muscle paralysis by preventing
acetylcholine release from presynaptic nerve terminals
o Surgical therapy
§ For chronic fissures that have failed to heal during
medical therapy
Figure 21. Sclerotherapy § Lateral internal sphincterotomy: procedure of choice
• Operative Hemorrhoidectomy V. ANORECTAL SEPSIS AND CRYPTOGLANDULAR
o Elective resection of symptomatic hemorrhoids ABSCESS
o Based on decreasing blood flow to the hemorrhoidal
plexuses and excising redundant anoderm and mucosa
o Complications:
§ Urinary retention (10-50%)
§ Fecal impaction (post-op pain)
§ Bleeding
§ Long term: Incontinence, anal stenosis, ectropion
(Whitehead’s deformity)
2. ANAL FISSURE
• Also called fissure in ano
• A tear in anoderm distal to the dentate line
• Trauma from either passage of hard stool or prolonged diarrhea Figure 23. Anal Abscess
• Presence of abscess either in the anal canal or outside the anal
• You’ll have to examine the inner aspect of anal canal to see the
opening
fissures
RELEVANT ANATOMY
• Majority of anorectal suppurative disease results from infections
of the anal glands (cryptoglandular infection) found in the
intersphincteric plane
• The perianal space surrounds the anus and laterally becomes
continuous with the fat of the buttocks
• The intersphincteric space separates the internal and external
anal sphincters
• The ischiorectal space (ischiorectal fossa) is located
lateral and posterior to the anus
Figure 22. Anal Fissure o Borders:
§ Medial: External sphincter
• Tear causes spasm of the internal anal sphincter § Lateral: Ischium
o Pain, increased tearing, decreased blood supply § Superior: Levator ani
• Majority: Posterior midline § Inferior: Transverse septum
o 10-15%: Anterior midline • The ischiorectal space contains the inferior rectal vessels and
o <1%: Off midline lymphatics
• Symptoms and Findings: • The two ischiorectal spaces connect posteriorly above the
o Tearing pain with defecation and hematochezia (blood on anococcygeal ligament and below the levator ani muscle
toilet paper) forming the deep post anal space
o Sensation of intense and painful anal spasms lasting for • The supralevator spaces lie above the levator ani on either
several hours after a bowel movement side of the rectum and communicate posteriorly
o PE: often seen in the anoderm by gently separating • The anatomy of these spaces influences the location and
buttocks; too tender (digital rectal exam cannot be spread of cryptoglandular infections
tolerated) • Surgical drainage as soon as the diagnosis is established
• Acute Fissure • Antibiotics alone are ineffective.
o Superficial tearing of the distal anoderm and heals with
medical management DIAGNOSIS
• Chronic Fissure • Severe anal pain is the most common presenting complaint
o Develop ulceration and heaped up edges with the • Walking, coughing, or straining can aggravate the pain
white fibers of the internal anal sphincter visible at the • A palpable mass is often detected by inspection of the perianal
base of the ulcer area or by digital rectal examination (DRE)
• Treatment: Surgery • Patients may present with fever, urinary retention, and life-
o Focus: Break the cycle of pain, spasm, and ischemia threatening sepsis
o First line: TREATMENT
§ Minimize anal trauma • Surgical drainage as soon as the diagnosis is established
§ Bulk agents, stool softeners, warm sitz bath • Antibiotics alone are ineffective
SURG II |6 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
VI. FISTULA IN ANO
• Usually originates in the infected crypt (internal opening) and
tracks to the external opening, usually the site of a previous
abscess
• The course of the fistula often can be predicted by the
anatomy of the previous abscess
Figure 26. Fistulotomy
• Resect the fistulous tract and apply the seton to the fistulous
tract and eventually there would be a fistulotomy. The tract will
close with fibrosis.
VII. NECROTIZING SOFT TISSUE INFECTION OF THE
PERINEUM
• Also known as Fourniere’s Gangrene is a rare but lethal
condition
• Polymicrobial and synergistic
• Source of sepsis: Undrained or inadequate drained
cryptoglandular abscess or a urogenital infection
• Usually seen in immunocompromised patients and
diabetic patients are at increased risk
Figure 24. Fistula in ano
• Diagnosis: Persistent drainage from the internal and/or external
openings
• An indurated tract is often palpable Figure 27. Necrotizing Soft Tissue Infection of the Perineum
• Although the external opening is often easily identifiable,
identification of the internal opening may be more challenging. • P.E.: Necrotic skin, bullae, or crepitus
• GOODSALL’S RULE: • Surgical debridement of all nonviable tissue: mainstay of
o In general fistulas with an external opening anteriorly therapy
connect to the internal opening by a short, radial tract • Broad-spectrum antibiotics
o Fistulas with an external opening posteriorly track in • The mortality of necrotizing perineal soft-tissue infections
curvilinear fashion to the posterior midline remains approximately 50% despite early recognition and
o Exception: If an anterior external opening is >3 cm from adequate surgical therapy
the anal margin, the fistula usually tracks to the posterior
midline VIII. RECTOVAGINAL FISTULA
• Connection between the vagina and the rectum or the anal
canal proximal to the dentate line
Figure 25. Goodsall’s rule to identify the internal opening of fistulas
in ano. Figure 28. Rectovaginal Fistula and repair of the fistula
• Treatment:
o Goal: Eradication of sepsis without sacrificing • Classification:
urinary incontinence o LOW:
o Fistulotomy § Rectal opening close to the dentate line and
o Curettage vaginal opening in the fourchette
o Healing by secondary intention § Commonly caused by obstetric injuries or trauma from
o Seton placement a foreign body
§ A seton is a drain placed through a fistula to maintain o MIDDLE:
drainage and/or induce fibrosis. § Vaginal opening between the fourchette and
cervix
SURG II |7 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
§ Causes: • Factors for management:
- Severe obstetric injury o Delay between injury and surgery
- Can occur after surgical resection of midrectal o Overall condition and stability of the patient
neoplasm o Degree of peritoneal contamination
- Radiation injury o Condition of the injured colon
- Extension of an undrained abscess
o HIGH: PRIMARY REPAIR
§ Vaginal opening near the cervix INDICATIONS CONTRAINDICATIONS
§ Result from operative or radiation injury • Hemodynamically stable § Shock
patients § Injury to >2 other organs
DIAGNOSIS • Few additional injuries § Mesenteric vascular damage
• Symptoms: • Minimal contamination § Extensive fecal
o Sensation of passing flatus in vagina • Otherwise healthy contamination
o Passage of solid stool from vagina colon § > 6 hours delay between
o Fecal incontinence injury and operation
o Vaginitis
o Speculum exam PENETRATING RECTAL INJURY
o Barium enema • Treatment: Proximal fecal diversion and copious irrigation of
o Endorectal ultrasound the rectum (distal rectal washout)
• Treatment: • Presacral drains - if w/ extensive fecal contamination
o Depends on the size, location, condition of the surrounding • Primary repair for small, clean injuries in stable patients
tissues
o 50% of fistulas caused by obstetric injury heal BLUNT COLORECTAL INJURY
spontaneously • Primary repair vs fecal diversion
o Fistula secondary to cryptoglandular abscess: • Crush injuries with pelvic fracture:
drainage may allow spontaneous closure o Often associated with significant rectal damage and
o For low and midrectovaginal fistula: Endorectal contamination
advancement flap o Debridement of all nonviable tissue, proximal fecal
o If with sphincter injury: Overlapping sphincteroplasty diversion, distal rectal washout, with or without
o For high rectovaginal, colovaginal, enterovaginal drain placement
fistula: Transabdominal
o Secondary to Chron’s disease, radiation injury or malignancy:
§ Adequate drainage of perianal sepsis
and nutritional support
§ Endorectal Advancement Flap
§ Tumor resection
§ All fistulas caused by radiation should be biopsied to
rule out CA
IX. PILONIDAL DISEASE
• Consists of hair-containing sinus or abscess occurring in the
intergluteal cleft (cyst, infection)
• Cleft creates a suction that draws hair into the midline pits Figure 31. Blunt Trauma of the transverse colon after multiple
when the patient sits —>becomes infected —> abscess vehicular accident (MVA), note the feces on the upper right side
formation
• Treatments IATROGENIC INJURY
o ACUTE: Incision and Drainage A. INTRAOPERATIVE INJURY
o CHRONIC: Unroofing, curettage, marsupialization • Key to management: early recognition
• Primary repair: if there is little contamination
• Late recognition of injury results in significant peritonitis and
sepsis
o Treatment: Fecal diversion
B. INJURY FROM BARIUM ENEMA
• If recognized early:
o Primary repair
o Abdominal irrigation: removal of stool and barium
Figure 29. Pilonidal disease o (+) Sepsis: Fecal diversion
X. TRAUMA • Small mucosal injury to the extraperitoneal rectum:
PENETRATING COLORECTAL INJURY o Bowel rest
o Broad-spectrum antibiotics
o Close observation
C. COLONOSCOPIC PERFORATION
• Rare
• Most common major complication after diagnostic or
therapeutic colonoscopy
• Treatment depends on:
o Size of the perforation
Figure 30. Penetrating injury damaging parts of the colon and small
o Duration of time since injury
intestines
SURG II |8 of 9 THURS, TIBAN, PEREZ (Liza)
SURGERY II
Saint Louis University School of Medicine MMXXII
o Overall condition of the patient CHECKPOINT!
• Large perforation: Surgical exploration I. T or F
In the follow up and surveillance of rectal cancer: (1-2)
ANAL SPHINCTER INJURY AND INCONTINENCE 1. A colonoscopy should be performed within 6 months after the
• Most common cause: Obstetric trauma during vaginal delivery diagnosis of the original cancer.
• Risk increased by: 2. If normal, colonoscopy should be repeated every 3-5 years
o Fourth degree laceration thereafter.
o Episiotomy infection 3. Carcinoid tumor occur most commonly in the GI tract and
o Prolonged labor 25% of which is in the cecum.
• Other causes of anal sphincter injury: 4. Lymphoma most often involves the rectum.
o Hemorrhoidectomy 5. Leiomyoma most commonly occurs in the upper GI tract.
o Sphincterotomy 6. Medial internal sphincterotomy is the procedure of choice in
o Abscess drainage anal fissure.
o Fistulotomy 7. The goal in the treatment of fistula in ano is eradication of
o Blunt or penetrating trauma sepsis even if urinary incontinence will be sacrificed.
• Definitive repair: 8. The key to management to intraoperative colorectal iatrogenic
o Deferred until other injuries have been repaired injury is early recognition.
• Isolated sphincter injuries (no rectal involvement): May be 9. Most common cause of anal sphincter injury and incontinence
repaired primarily is hemorrhoidectomy.
10. Foreign body entrapment low in the rectum may not be
• Rectal injury + sphincter injury:
removed under conscious sedation.
o Fecal diversion, distal rectal washout, drain
11. Splenic flexure is the most common site of ischemic colitis.
placement
12. Rectum is not spared in ischemic colitis.
II. Identification
SURGICAL REPAIRS OF THE ANAL SPHINCTER
13. Adenocarcinoma in situ which is extramammary and arise from the
• Wrap-around sphincteroplasty apocrine glands of the perianal area
o Most common method of repair 14. Most durable repair of rectal prolapse that can be done with or
• Postnatal intersphincteric levatoroplasty without sigmoid resection and has <10% recurrence
o Less commonly used 15. This occurs when an air-filled segment of the colon twists
o May be used for incontinence caused by prolapse and/or about its mesentery
loss of the anorectal angle 16. Congenital megacolon is caused by this disease wherein there is
• Gracilis Muscle Transposition (w/ or w/o chronic low failure of migration of neural crest cells to the distant large
frequency electrostimulation) intestine.
o In cases of significant loss of sphincter muscle or in 17. Functional disorder in which the colon becomes massively
which prior repairs have failed dilated in the absence of mechanical obstruction
• Artificial Anal Sphincter 18. Necrotizing soft tissue infection of the perineum is also known
o In failed repairs as ____
• Sacral Nerve Stimulation 19. Surgical treatment for low and midrectovaginal fistula.
o For neurogenic incontinence: intact sphincter 20. This disease consists of hair-containing sinus or abscess
occurring in the intergluteal cleft.
XI. FOREIGN BODY ENTRAPMENT 20. Pilonidal disease
19. Endorectal advancement flap
18. Fourniere’s Gangrene
17. Ogilvie’s syndrome
16. Hirschsprung’s disease
15. Volvulus
14 . Abdominal Rectopexy
13. Perianal Paget’s disease
circulation
12) F - Rectum is spared because of its rich collateral
trauma during vaginal delivery 10) F - May be removed 11) T
without sacrificing urinary incontinence 8) T 9)F - Obstetric
not rectum 5) T 6)F - Lateral 7) F - Eradication of sepsis
Figure 32. Ore inside the rectum of a 54 y/o male. 1)F - 12 months 2) T 3) F - Rectum not cecum 4) F - Cecum
• Generalized abdominal pain suggests intraperitoneal perforation. ANSWERS:
• Evaluation of the patient includes inspection of the perineum and
a careful abdominal examination to detect any evidence of
perforation. Plain films of the abdomen are mandatory to detect
free intra-abdominal air
• Low in the rectum:
o May be removed under conscious sedation (w or w/o
local anesthetic block)
• Impaction higher in the rectum
o May require regional or general anesthesia for removal
SURG II |9 of 9 THURS, TIBAN, PEREZ (Liza)
You might also like
- Frcophth 400 Sbas and CrqsDocument262 pagesFrcophth 400 Sbas and CrqsZaheer Ullah Soleh100% (1)
- 4 PEDIA 8 - Bleeding DisordersDocument5 pages4 PEDIA 8 - Bleeding DisordersRainy Liony DuhNo ratings yet
- Osce Cranial Nerves PDFDocument42 pagesOsce Cranial Nerves PDFriczen vilaNo ratings yet
- Apgar ScoreDocument5 pagesApgar ScoreDjan Kurvie ValencerinaNo ratings yet
- Apgar ScoreDocument5 pagesApgar ScoreDjan Kurvie ValencerinaNo ratings yet
- Genetics Problem Key Biol 121Document13 pagesGenetics Problem Key Biol 121S0% (1)
- SURGERY - 1.5 Colon, Rectum, and Anus (Lecture)Document8 pagesSURGERY - 1.5 Colon, Rectum, and Anus (Lecture)Bianca Jane Maaliw100% (1)
- Urology: Kidneys BladderDocument26 pagesUrology: Kidneys BladderChristineGonzalesNo ratings yet
- HirschprungDocument13 pagesHirschprungfitra hayatiNo ratings yet
- Esophageal Achalasia DysphagiaDocument14 pagesEsophageal Achalasia DysphagiaTirtha Taposh100% (1)
- Approach To A Patient With Jaundice: Group A9 Cho, Chua Family, Co Family, CofrerosDocument115 pagesApproach To A Patient With Jaundice: Group A9 Cho, Chua Family, Co Family, CofrerosEunice Co100% (1)
- DISC, Drugs, Infection, Thick Basal MembraneDocument5 pagesDISC, Drugs, Infection, Thick Basal MembraneHOPENo ratings yet
- TRIVIA: Dr. Tan Is The Father/Pioneer of Laparoscopic Surgery in The PhilippinesDocument48 pagesTRIVIA: Dr. Tan Is The Father/Pioneer of Laparoscopic Surgery in The PhilippinesJüdith Marie Reyes BauntoNo ratings yet
- UROLOGY 2020 (Doc BarcenasDocument33 pagesUROLOGY 2020 (Doc BarcenasJüdith Marie Reyes BauntoNo ratings yet
- JaundiceDocument53 pagesJaundiceAbhishiktaAbhiNo ratings yet
- 1.33 (Surgery) Hepatobiliary Tract Part 2Document8 pages1.33 (Surgery) Hepatobiliary Tract Part 2Leo Mari Go LimNo ratings yet
- HS-FPH101 Foundations To Public Health: Track 2Document5 pagesHS-FPH101 Foundations To Public Health: Track 2Nerzo SongaliaNo ratings yet
- Approach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDateDocument21 pagesApproach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDatekrlotaNo ratings yet
- Peptic Ulcer DiseaseDocument14 pagesPeptic Ulcer DiseasePernel Jose Alam MicuboNo ratings yet
- Abdominal AbscessDocument3 pagesAbdominal AbscessIchalAzNo ratings yet
- Examination of the Thyroid GlandDocument49 pagesExamination of the Thyroid GlandRajhmuniran KandasamyNo ratings yet
- Postoperative Surgical Complications 2015Document26 pagesPostoperative Surgical Complications 2015AlaaGaballaNo ratings yet
- Imaging of The Reproductive SystemDocument15 pagesImaging of The Reproductive SystemAbi SulitNo ratings yet
- PCOS Diagnosis and SymptomsDocument7 pagesPCOS Diagnosis and SymptomsAlodia Razon100% (1)
- Total Abdominal HysterectomyDocument19 pagesTotal Abdominal HysterectomyMeidina Rachma Amanda100% (1)
- Anal Rectal DiseasesDocument43 pagesAnal Rectal DiseasesNikita NababanNo ratings yet
- (DERMA) 03 TineasDocument9 pages(DERMA) 03 TineasJolaine ValloNo ratings yet
- Approach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDateDocument21 pagesApproach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDateChrista OvalleNo ratings yet
- Clinical Approach to JaundiceDocument48 pagesClinical Approach to JaundiceSuranga Lakshitha PereraNo ratings yet
- Approach To Jaundice (1) .PPT ALAWAJIDocument28 pagesApproach To Jaundice (1) .PPT ALAWAJIayuNo ratings yet
- Endometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDateDocument39 pagesEndometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDatefujimeisterNo ratings yet
- Malignant Thyroid PDFDocument4 pagesMalignant Thyroid PDFOliver QuiambaoNo ratings yet
- Hematuria in ChildrenDocument26 pagesHematuria in ChildrenNovenZefanya100% (1)
- Gyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesDocument8 pagesGyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesVon HippoNo ratings yet
- Internal Medicine - Nephrology Lecture on Cystic Kidney DiseasesDocument3 pagesInternal Medicine - Nephrology Lecture on Cystic Kidney DiseasesVon HippoNo ratings yet
- Head & Neck: Most CommonDocument6 pagesHead & Neck: Most CommonJüdith Marie Reyes BauntoNo ratings yet
- Abdominal Trauma Signs, Symptoms and Nursing CareDocument24 pagesAbdominal Trauma Signs, Symptoms and Nursing CareSurgeryClassesNo ratings yet
- 5.2 Renal Masses and Congenital AnomaliesDocument9 pages5.2 Renal Masses and Congenital AnomaliesMaria roxanne HernandezNo ratings yet
- Fluids and Electrolytes Management in Surgical PatientsDocument4 pagesFluids and Electrolytes Management in Surgical PatientsJanine Maita BalicaoNo ratings yet
- Evaluation of Abdominal PainDocument7 pagesEvaluation of Abdominal PainCherry Faith Merisco LabtangNo ratings yet
- (Gyne) 2.2 Cervical Intraepithelial Neoplasia (Delos Reyes) - JTIIIDocument6 pages(Gyne) 2.2 Cervical Intraepithelial Neoplasia (Delos Reyes) - JTIIIDexter Ian100% (1)
- Surgical Oncology and Breast BiopsyDocument12 pagesSurgical Oncology and Breast Biopsybo gum parkNo ratings yet
- Urethral Stricture DiseaseDocument9 pagesUrethral Stricture DiseaseIntanAgustiFernandesNo ratings yet
- Surgery II - Pancreas 2014Document20 pagesSurgery II - Pancreas 2014Medisina101No ratings yet
- Benign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDocument83 pagesBenign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDian Permata PutraNo ratings yet
- Liver Function Tests (Sem)Document6 pagesLiver Function Tests (Sem)Francisco NiegasNo ratings yet
- Management of Acute Appendicitis in Adults - UpToDateDocument28 pagesManagement of Acute Appendicitis in Adults - UpToDateVinicius VieiraNo ratings yet
- GYNE 4.04 Pelvic Organ DisordersDocument7 pagesGYNE 4.04 Pelvic Organ DisordersGray SnellNo ratings yet
- Case 1 History & PEDocument3 pagesCase 1 History & PEcbac1990No ratings yet
- Obstructive JaundiceDocument1 pageObstructive JaundiceMattNo ratings yet
- Fammed Family Life CycleDocument3 pagesFammed Family Life CycleTMC PGI GENER MICKONo ratings yet
- 17 - Gallbladder StonesDocument71 pages17 - Gallbladder StonesRashed ShatnawiNo ratings yet
- Approach To Peritoneal Fluid AnalysisDocument10 pagesApproach To Peritoneal Fluid AnalysisLady BugNo ratings yet
- Anatomy of the SpleenDocument18 pagesAnatomy of the Spleenزين العابدين محمد عويش100% (1)
- Jaundice: Seminar Under The Guidance Of-Dr. Shiva NarangDocument47 pagesJaundice: Seminar Under The Guidance Of-Dr. Shiva NarangMiguel MansillaNo ratings yet
- Medicine 6.1b Approach To Cancer Patients - FernandoDocument7 pagesMedicine 6.1b Approach To Cancer Patients - FernandoAbigail LausNo ratings yet
- Pathophysiology of Appendicitis (RupturedDocument2 pagesPathophysiology of Appendicitis (RuptureddesireeroseNo ratings yet
- Small Bowel Obstruction - Clinical Diagnosis and TreatmentDocument11 pagesSmall Bowel Obstruction - Clinical Diagnosis and TreatmentVigariooNo ratings yet
- 0.7 Surgery Trans PDFDocument29 pages0.7 Surgery Trans PDFJoy ManzanoNo ratings yet
- Management of Acute Appendicitis in Adults - UpToDateDocument28 pagesManagement of Acute Appendicitis in Adults - UpToDateaulia rachman100% (1)
- Adnexal Torsion: Maria Giroux, HBSC, MDDocument33 pagesAdnexal Torsion: Maria Giroux, HBSC, MDMistiru TegegneNo ratings yet
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Pathology of the Digestive SystemDocument28 pagesPathology of the Digestive SystemDianNursyifaRahmahNo ratings yet
- Anatomy Large IntestineDocument4 pagesAnatomy Large IntestinetristineNo ratings yet
- Group-2 - Fluvoxamine 1stDocument10 pagesGroup-2 - Fluvoxamine 1stDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument6 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Baldovino - October 13, 2020Document11 pagesSaint Louis University School of Medicine Mmxxii: Dr. Baldovino - October 13, 2020Djan Kurvie ValencerinaNo ratings yet
- FLUVOXAMINE and COVID19Document9 pagesFLUVOXAMINE and COVID19Petra JobovaNo ratings yet
- Group-2 - Fluvoxamine 1stDocument10 pagesGroup-2 - Fluvoxamine 1stDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument2 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- Saint Louis University School of Medicine Department of OphthalmologyDocument4 pagesSaint Louis University School of Medicine Department of OphthalmologyDjan Kurvie ValencerinaNo ratings yet
- F.05 Approach To Menstrual Abnormalities and Menstrual Pain (Dr. Lucas) (04-29-19)Document7 pagesF.05 Approach To Menstrual Abnormalities and Menstrual Pain (Dr. Lucas) (04-29-19)Djan Kurvie ValencerinaNo ratings yet
- Pharmacology and Therapeutics LabDocument20 pagesPharmacology and Therapeutics LabDjan Kurvie ValencerinaNo ratings yet
- F.02 Approach To Lower Urinary Tract Symptoms (Dr. Dominguez) (04-12-19)Document3 pagesF.02 Approach To Lower Urinary Tract Symptoms (Dr. Dominguez) (04-12-19)Djan Kurvie ValencerinaNo ratings yet
- F.01 Approach To Sexual Dysfunction (Dr. Dominguez) (04-10-19)Document4 pagesF.01 Approach To Sexual Dysfunction (Dr. Dominguez) (04-10-19)Djan Kurvie ValencerinaNo ratings yet
- EssayDocument1 pageEssayDjan Kurvie ValencerinaNo ratings yet
- Ethical Guidelines For The Use of Animals in ResearchDocument9 pagesEthical Guidelines For The Use of Animals in ResearchDjan Kurvie ValencerinaNo ratings yet
- SCREEMDocument4 pagesSCREEMDjan Kurvie ValencerinaNo ratings yet
- F.03 Approach To Scrotal Pain, Swelling, and Lesions (Dr. Dominguez) (04-12-19)Document5 pagesF.03 Approach To Scrotal Pain, Swelling, and Lesions (Dr. Dominguez) (04-12-19)Djan Kurvie ValencerinaNo ratings yet
- TAENIASPP RevisedDocument3 pagesTAENIASPP RevisedDjan Kurvie ValencerinaNo ratings yet
- Neuro Osce Cheat Sheet LolsDocument1 pageNeuro Osce Cheat Sheet LolsDjan Kurvie ValencerinaNo ratings yet
- AI Examples: NLP, Machine Vision & Machine LearningDocument1 pageAI Examples: NLP, Machine Vision & Machine LearningDjan Kurvie ValencerinaNo ratings yet
- Ea ComparisonDocument1 pageEa ComparisonDjan Kurvie ValencerinaNo ratings yet
- MULHANDocument17 pagesMULHANDjan Kurvie ValencerinaNo ratings yet
- Safety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDocument1 pageSafety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDjan Kurvie ValencerinaNo ratings yet
- CrammedDocument5 pagesCrammedDjan Kurvie ValencerinaNo ratings yet
- Teaching Plan On Electrolyte Imbalance22Document2 pagesTeaching Plan On Electrolyte Imbalance22Djan Kurvie ValencerinaNo ratings yet
- Thirst in Chronic Heart FailureDocument2 pagesThirst in Chronic Heart FailureDjan Kurvie ValencerinaNo ratings yet
- QuestionnaireDocument1 pageQuestionnaireDjan Kurvie ValencerinaNo ratings yet
- DadahsitDocument1 pageDadahsitDjan Kurvie ValencerinaNo ratings yet
- Safety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDocument1 pageSafety and Immunogenicity of A Live Attenuated Tetravalent Dengue Vaccine Candidate in FlavivirusDjan Kurvie ValencerinaNo ratings yet
- Case Study TabhsoDocument7 pagesCase Study TabhsoGina Barredo Bustamante100% (1)
- Halitosis Augost 20 2015Document52 pagesHalitosis Augost 20 2015HairunnisaNo ratings yet
- Achilles Tendinitis Rehabilitation ExercisesDocument3 pagesAchilles Tendinitis Rehabilitation ExercisesAjish VijayanNo ratings yet
- Full Download Test Bank For Radiation Protection in Medical Radiography 7th Edition by Sherer PDF Full ChapterDocument36 pagesFull Download Test Bank For Radiation Protection in Medical Radiography 7th Edition by Sherer PDF Full Chaptermaryrodriguezxsntrogkwd100% (18)
- მიტოქონდრიის ფუნქცია და კიბოDocument1 pageმიტოქონდრიის ფუნქცია და კიბოEMD GROUPNo ratings yet
- Echocardiographic Anatomy in The FetusDocument14 pagesEchocardiographic Anatomy in The FetusAnonymous hOHi6TZTnNo ratings yet
- OBGYN 1st Round 2021 AnsweredDocument14 pagesOBGYN 1st Round 2021 AnsweredMuhammed Mostafa100% (4)
- Caie As Level Geography 9696 Core Human Geography v1Document13 pagesCaie As Level Geography 9696 Core Human Geography v1BrizzyNo ratings yet
- Theoretical FrameworkDocument27 pagesTheoretical Frameworkcm289867No ratings yet
- CDC 2017 0019 0010 - ContentDocument156 pagesCDC 2017 0019 0010 - ContentTrey Martin-EllisNo ratings yet
- Operating Manual Electronic Column Scale M20610Document8 pagesOperating Manual Electronic Column Scale M20610Bryan GarciaNo ratings yet
- #1 Risk For Aspirations DCDocument2 pages#1 Risk For Aspirations DCtanyav26No ratings yet
- CBG Cannabinoid Benefits and EffectsDocument10 pagesCBG Cannabinoid Benefits and EffectsjohnnemanicNo ratings yet
- 2007 4328b1 02 PrestwickDocument149 pages2007 4328b1 02 PrestwickComunidad Cetram100% (1)
- Healing Through Loss and GriefDocument3 pagesHealing Through Loss and Griefjackieob123No ratings yet
- Dho Health Science Updated 8th Edition Simmers Test BankDocument9 pagesDho Health Science Updated 8th Edition Simmers Test Bankjosephrodriguez04121993gbm100% (25)
- Alien TechnologyDocument11 pagesAlien TechnologySharvari TaklikarNo ratings yet
- ClavusDocument4 pagesClavusargie3333No ratings yet
- Pyloric StenosisDocument14 pagesPyloric Stenosisgangguan hepatobilierNo ratings yet
- Dsm-Iii at The Cinema: Madness in The MoviesDocument12 pagesDsm-Iii at The Cinema: Madness in The MoviesLiridon1804No ratings yet
- Water Is Alive Shellys House Speech PDFDocument9 pagesWater Is Alive Shellys House Speech PDFCyndi Lindenberger100% (1)
- Ts 410 420 Product Instruction ManualDocument112 pagesTs 410 420 Product Instruction ManualRosario GonzalesNo ratings yet
- Master Drug ChartDocument22 pagesMaster Drug ChartMahadhir AkmalNo ratings yet
- Gua ShaDocument41 pagesGua ShaFerencne Hanis100% (2)
- Assignment 3Document5 pagesAssignment 3Samantha PargadNo ratings yet
- Leishman-Stain Technicaldetails 72320230328.101614Document2 pagesLeishman-Stain Technicaldetails 72320230328.101614RahulNo ratings yet
- Probiotics and Preterm Infants A Position Paper.26 ShareDocument17 pagesProbiotics and Preterm Infants A Position Paper.26 Shareendy tovarNo ratings yet
- Hydrocephalus N C P BY BHERU LALDocument1 pageHydrocephalus N C P BY BHERU LALBheru LalNo ratings yet