Professional Documents
Culture Documents
A Schwan1983
A Schwan1983
Uploaded by
Christian HongOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Schwan1983
A Schwan1983
Uploaded by
Christian HongCopyright:
Available Formats
845
RELAPSING CLOSTRIDIUM DIFFICILE urea nitrogen 5’8mmol/l, serum creatinine 330 mol/1, and urine
ENTEROCOLITIS CURED BY RECTAL INFUSION OF analysis showing abundant proteinuria (2’5g/day) and microscopic
HOMOLOGOUS FAECES haematuria. Renal echography disclosed a symmetrical
of
enlargement both kidneys.
SIR,-Recurrent Clostridium difficile associated enterocolitis is
uncommon but troublesome for the patient. The patient described During the next 4 days symptoms regressed, whereas renal
function continued to deteriorate (serum creatinine peaked at 960
here received vancomycin treatment several times but always
relapsed with C difficile enterocolitis 2-3 weeks after mol/1 on the 1 Oth day of the disease), urinary output was 800-1000
discontinuation of treatment. ml/day with a urinary sodium below 10 mmol/day and a moderate
A 65-year-old woman with a lifelong history of irritable colon also proteinuria. On the 1 lth day diuresis occurred (3300 ml/day) and
had diverticulosis of the colon and diverticulitis of increasing persisted for 4 days, followed by a dramatic improvement of renal
function. By the l7th day serum creatinine and urinary sediment
severity. A partial colectomy was done to remove the diseased had returned to normal; proteinuria was negative. 9 months later the
part of the sigmoid colon. She was given routine preoperative
treatment with neomycin and metronidazole. 1 week patient has no clinical or biochemical abnormality. A renal
she given co-trimoxazole because of percutaneous biopsy on day 10 showed conspicuous abnormalities
postoperatively was pulmonary within the medulla, with diffuse oedema, hyperaemia, and
infection. She responded well at first but 3 weeks later she had
frequent diarrhoea and fever and C difficile enterocolitis was haemorrhages in the interstitium. There was also a pronounced
vacuolisation and swelling of tubular epithelial cells without
diagnosed. Stool cultures grew C dzfficile and its cytotoxin was necrosis. Glomerular changes were minimal. Several capillary loops
demonstrated. Vancomycin was given for 7 days and proved
were enlarged by numerous red cells; no hypercellularity was
effective. 2 weeks later, however, the patient had a relapse. C
present. Arteries and arterioles were normal. Immunofluorescence
difficile and its cytotoxin was again demonstrated in the stool. for IgG, IgM, IgA, Clq, C3, and fibrinogen was negative. The
Vancomycin was given with prompt response. The patient had
another four relapses of Cdifficile enterocolitis, also after prolonged diagnosis of HFRS, which was strongly suggested by both clinical
and histological data,2,5 was confirmed by fluorescent-antibody test
(4 month’s) vancomycin therapy. in two different laboratories. A significant increase in antibodies to
Since the patient was faced with the unattractive prospect of
vero E6 cells infected with strain 74-118 Hantaan virus (see figure)6
lifelong vancomycin treatment we decided to try to achieve a normal and to lung section of bank voles infected for nephropathia
bowel flora by infusing faeces, hoping that C difficile would be
suppressed and a normal flora established. epidemicawas detected.
Enemas were prepared in an anaerobic cabinet from fresh faeces
obtained from the patient’s husband. 4 days after the last (sixth)
course of vancomycin treatment two such enemas were given
immediately after preparation and 3 days apart. There were no
untoward reactions. The rectal infusion of normal faeces resulted in
prompt and complete normalisation of bowel function. Stools of
normal consistency, colour, and smell have thereafter been passed
daily or every other day. The follow-up period is now 9 months. The
patient feels well and has gained in weight from 41 to 47 kg.
Institute of Clinical Bacteriology,
Department of Paediatrics ANNA SCHWAN
and Department of Infectious Diseases
University Hospital, STIG SJOLIN
75122 Uppsala, Sweden ULLA TROTTESTAM
National Bacteriological Laboratory,
Stockholm BO ARONSSON
MUROID VIRUS NEPHROPATHIES
SIR,-Your editorial and the subsequent correspondence drew
attention to the haemorrhagic fever with renal syndrome (HFRS)
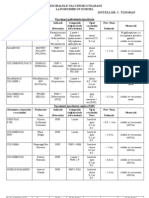
and the closely related nephropathia epidemica described by Scan- not uec. idn. ai reu. mar. Apr. may
dinavian workers.2,3 It seems that in Western Europe, outside Scan- IgG and IgM titres to strain 76 - 118 Hantaan virus.
dinavia, HFRS acquired from laboratory rats has been observed
only in Belgium (Desmyler J, personal communication). In addition This case of HFRS is the first observed in France. The patient had
antibodies to Hantaan virus, as well as antigen, have been detected in never travelled out of France or been exposed to laboratory rats.
a wild rodent, the red-backed vole (Clethrionomys glareolus), in However, he had worked for a day two weeks before onset in a barn
Belgium.4We have observed a case of HFRS in a French resident located in a small village 120 km north-east of Paris. It seems very
after exposure to wild rodents. A previously healthy 29-year-old likely that he had acquired the infection from wild rodents which
man living in Paris was admitted to hospital on Nov 16, 1982, were sometimes seen in the barn. An epidemiological survey has
because of fever, chills, profuse sweating, vomiting, and intense been undertaken in this rural area. The occurrence of an infection of
lumbar pain which had appeared 4 days earlier. The only relevant man due to an HFRS-related virus acquired in France after
signs found on initial examination were bilateral conjunctival exposure to wild rodents obviously extends the boundary of
haemorrhages and acute myopia. Blood pressure was 110/70 mm European endemic HFRS. This is not surprising, since field mice
Hg and remained normal throughout the course of the disease. (Apodemus), the reservoir of Hantaan virus, are common in France
Laboratory data included haemoglobin 7 g/dl, leucocyte count as in other Western European countries.8 HFRS should be
21 700/1, platelets 41 000/1, SGOT 65 IU/1, SGPT 67 IU/1, blood
1 Editorial Muroid virus nephropathies. Lancet 1982, ii: 1375-77. 5 Lee HW. Korean hemorrhagic fever. Prog Med Virol 1982, 28: 96-113.
2 Lähdevirta J Nephropathia epidemica in Finland. A clinical, histological and 6. McCormick JB, Sasso DR, Palmer EL, Kiley MP Morphological identification of the
epidemiological study. Ann Clin Res 1971, 3 (suppl 8). 1-154. agent of Korean haemorrhagic fever (Hantaan virus) as a member of the
3 Lee HW, Lee PW, Lähdevirta J, Brummer-Korvenkontio M. Aetiological relation Bunyaviridae Lancet 1982; i; 765-68
between Korean haemorrhagic fever and nephropathia epidemica. Lancet 1979; ii: 7 Brummer-Korvenkontio J, Vaheri A, Hovi T, et al. Nephropathia epidemica:
186-87 Detection of antigen m bank voles and serologic diagnosis of human infection J
4 Van der Groen G, Tkachenko EA, Ivanov AP, Verhagen R Haemorrhagic fever with Infect Dis 1980, 141: 131-34.
renal syndrome related virus in indigenous wild rodents in Belgium Lancet 1983; ii: 8. Nowak RM, Paradiso JL. Walker’s mammals of the world. Baltimore. Johns Hopkins
110-11 University Press, 1983
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Blood Typing - : Adapted From Figure 40.5 in Holt Biology by Johnson and RavenDocument4 pagesBlood Typing - : Adapted From Figure 40.5 in Holt Biology by Johnson and Ravenjazzmine andesonNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lateral Flow Self-Swab InstructionsDocument8 pagesLateral Flow Self-Swab InstructionsSabera KapasiNo ratings yet
- Democracy in The BalanceDocument180 pagesDemocracy in The BalanceJoe WigginsNo ratings yet
- US Trade Deficit Rises Amid Record Drop in Exports: QuotesDocument28 pagesUS Trade Deficit Rises Amid Record Drop in Exports: QuotesjayNo ratings yet
- Department of Haematology Test Name Result Unit Bio. Ref. Range MethodDocument5 pagesDepartment of Haematology Test Name Result Unit Bio. Ref. Range MethodSunil KhandekarNo ratings yet
- Enterovirus 71 Outbreaks, Taiwan: Occurrence and RecognitionDocument3 pagesEnterovirus 71 Outbreaks, Taiwan: Occurrence and RecognitionAdhi SyukriNo ratings yet
- Zombie Deer DiseaseDocument3 pagesZombie Deer DiseaseAngela CubillosNo ratings yet
- Insights: Reducing Transmission of Sars-Cov-2Document4 pagesInsights: Reducing Transmission of Sars-Cov-2epraetorianNo ratings yet
- How Long Before We Find An HIV Cure?: BENSON NASASIRA, February 4th 2021Document20 pagesHow Long Before We Find An HIV Cure?: BENSON NASASIRA, February 4th 2021Nasasira BensonNo ratings yet
- Avian Polyomavirus My ThoughtsDocument22 pagesAvian Polyomavirus My Thoughtsnasih hamadNo ratings yet
- FOSFOMYCINDocument27 pagesFOSFOMYCINDavid RamirezNo ratings yet
- Vaccinuri Porumbei EuropaDocument3 pagesVaccinuri Porumbei EuropaLeGaCykojiNo ratings yet
- Malaysian Women Suggested To Carry Condom - Health NewsDocument4 pagesMalaysian Women Suggested To Carry Condom - Health NewsDiva WidyaNo ratings yet
- Progress in Disaster Science: Invited ViewpointDocument9 pagesProgress in Disaster Science: Invited ViewpointHalidaAnNabilaNo ratings yet
- Cu-Ag Ionisation Vs ClO2Document4 pagesCu-Ag Ionisation Vs ClO2Engineering WavesNo ratings yet
- Pneumococcal VaccinesDocument38 pagesPneumococcal VaccinesKishore Chandki100% (1)
- MCQs For FridayDocument2 pagesMCQs For FridaydfngjlnNo ratings yet
- Lung AbscessDocument27 pagesLung AbscessMalueth Angui100% (1)
- Gut Health in Poultry, 2013 PDFDocument42 pagesGut Health in Poultry, 2013 PDFvetbcas100% (1)
- Micro by DR - Hesham (GIT)Document65 pagesMicro by DR - Hesham (GIT)abcde990075No ratings yet
- Tersano and Deposon PathogenSummarySheetDocument2 pagesTersano and Deposon PathogenSummarySheetNikhil C me18s303No ratings yet
- 2020 Axonal Variants of Guillain-Barré Syndrome - An Update PDFDocument18 pages2020 Axonal Variants of Guillain-Barré Syndrome - An Update PDFVladimir BasurtoNo ratings yet
- Ebola ActivityDocument7 pagesEbola Activitycory kurdapyaNo ratings yet
- Systemic Infections From GiDocument10 pagesSystemic Infections From GiJake MillerNo ratings yet
- Streptococcus Pneumoniae: PneumococciDocument1 pageStreptococcus Pneumoniae: Pneumococciridin007No ratings yet
- Mr. Rohit Raghav: 29 Years / Male Sample Location: Facility Centre: Self: COVID-26426-20: 02/12/2020 17:40Document2 pagesMr. Rohit Raghav: 29 Years / Male Sample Location: Facility Centre: Self: COVID-26426-20: 02/12/2020 17:40raghav1208No ratings yet
- POULTRY PATHO - Marek's DiseaseDocument31 pagesPOULTRY PATHO - Marek's DiseaseArooma KhalidNo ratings yet
- Food Control: Matheus S. Barbosa, Svetoslav D. Todorov, Cynthia H. Jurkiewicz, Bernadette D.G.M. FrancoDocument7 pagesFood Control: Matheus S. Barbosa, Svetoslav D. Todorov, Cynthia H. Jurkiewicz, Bernadette D.G.M. FrancoLizi SorciaNo ratings yet
- Yaws Eradication ProgrammeDocument1 pageYaws Eradication ProgrammeArchana SahuNo ratings yet
- Slapped Cheek SyndromeDocument1 pageSlapped Cheek SyndromeDavid HylandNo ratings yet