Professional Documents
Culture Documents
Human Microbiome in Health and Disease
Uploaded by
AcengHamudinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Human Microbiome in Health and Disease
Uploaded by
AcengHamudinCopyright:
Available Formats
HUMAN MICROBIOME IN HEALTH AND DISEASE
Patrick Murray
Up until the time of birth, the human fetus lives in a remarkably protected and for the most part
sterile environment; however, this rapidly changes as the infant is exposed to bacteria, archaea,
fungi, and viruses from the mother, other close contacts, and the environment. Over the next
few years, communities of organisms (microbiota or normal flora [Table 2-1]) form on the
surfaces of the skin, nares, oral cavity, intestines, and genitourinary tract. The focus of this
chapter is to gain an understanding of the role these communities play in the metabolic and
immunologic functions of healthy individuals, factors regulating the com-position of these
communities, and how disruption of these communities can result in disease states.
Human Microbiome Project
Our current knowledge of the microbiome is rooted in the successful completion of the Human
Genome Project, a 13-year international effort initiated in 1990 that determined the sequences
of the approximately 3 billion nucleotides that make up the 23,000 protein-encoding genes in
human DNA. Much like efforts to send a man to the moon, the greatest legacy of this work was
the development of technologies and informatic solutions that allow the generation and analysis
of tremendous amounts of DNA and messenger RNA sequencing data.The Human Microbiome
Project was a 5-year multina-tional study to analyze the genetic composition (microbi-ome) of
the microbial populations that live in and on healthy adults. To put the complexity of this
program into perspec-tive, it is estimated that bacterial cells outnumber human cells in the host
by 10:1, and the bacterial population con-tributes at least 300-fold more protein genes.The
Human Microbiome Project was launched in 2007 with the collection of samples from the nose,
mouth, skin, gut, and vagina from healthy adult volunteers. The microbes were identified by
sequencing targeted regions of the 16S ribosomal RNA gene, and information about the gene
content of the entire population was determined by sequenc-ing the whole genome of a subset
of specimens. These analy-ses showed that there is substantial variation in the species and
gene composition for individuals and at different body sites. For example, bacteria colonizing
the gut are different from those in the mouth, skin, and other body sites. The body site with the
greatest taxonomic and genetic diversity was the intestine, and the vagina was the least
complex. Microenvironments such as different regions of the mouth, gut, skin surface, and
vagina also had their own unique microbiome (Figure 2-1).
• Core Microbiome
Most individuals share a core microbiome, arbitrarily defined as the species that are present at a
specific site in 95% or more of individuals. The greatest numbers of shared species are present
in the mouth, followed by the nose, intes-tine, and skin, and the fewest shared species are
found in the vagina. Additionally, the small numbers of species that com-prise the core
microbiome are the most numerous, repre-senting the majority of the total population, whereas
the remaining portion of the population (secondary microbi-ome) consists of small numbers of
many species that may not be widely shared by individuals. This would imply that the members
of the core microbiome are critically impor-tant, providing essential functions that must be
retained for normal metabolic and immunologic activities, and the func-tions provided by the
secondary microbiome are also criti-cally important but can be provided by a variety of
organisms. In other words, although there is tremendous variation of species among individuals,
there is less variation in the genetic composition at each site. The taxonomic diversity of a
population is great, but the functional properties are highly conserved (functional redundancy) in
microbiomes associ-ated with health. This is not surprising if we consider that the microbiome is
a community that exists in a symbiotic relationship with its host, providing needed metabolic
func-tions, stimulating innate immunity, and preventing coloniza-tion with unwanted pathogens.
Thus interpersonal variations of the microbiome can exist in healthy individuals as long as the
needed functions are satisfied.• Evolution of the Microbiome and Normal FloraThe normal flora
of a particular site of the body consists of a unique community of core and secondary microbiota
that evolved through a symbiotic relationship with the host and a competitive relationship with
other species. The host pro-vides a place to colonize, nutrients, and some protection from
unwanted species (innate immune responses). The microbes provide needed metabolic
functions, stimulate innate and regulatory immunity, and prevent colonization with unwanted
pathogens (Figure 2-2). The ability to tolerate the amount of oxygen or lack thereof (redox state)
and the pH and salt concentration, as well as to scavenge essential minerals and harvest and
metabolize the available nutrients, determines the numbers and nature of the species that popu-
late a site of the body. Anaerobic or facultative anaerobic bacteria colonize most of the sites of
the body because of the lack of oxygen in sites such as the mouth, intestine, and genitourinary
tract.The composition of the microbiota is influenced by per-sonal hygiene (e.g., use of soap,
deodorants, mouthwash, skin peels, enemas, vaginal douches), diet, water source, medicines
(especially antibiotics), and exposure to environ-mental toxins. Drinking well water versus
chlorinated city water or a diet consisting of more or less fiber, sugar, or fats can select for
different intestinal bacteria based on their ability to utilize the essential minerals (e.g., iron) and
nutri-ents. Alteration of the environment with foods or medicines can also alter the microbiota
(Figure 2-3). These changes can be acceptable if the core microbiome and critical functional
properties of the microbiome are maintained but can result in disease if these functions are lost.
Historically, the greatest concern with the use of broad-spectrum antibiotics was the selection of
resistant bacteria; however, a greater concern should be the disruption of the microbiome and
loss of essential functions.Of the approximately 200 unique species of bacteria that colonize the
gut, most are members of the Actinobacteria (e.g., Bifidobacterium), Bacteroidetes (e.g.,
Bacteroides), and Firmicutes (e.g., Eubacterium, Ruminococcus, Faecalibacte-rium, Blautia).
Interestingly, the importance of many of these bacteria was not appreciated before gene
sequencing was used to identify and quantitate the gut microbiota.
Within the colon, some bacteria wage interspecies warfare to establish their niche with
bacteriocins (e.g., colicins pro-duced by Escherichia coli), other antibacterial proteins, and
metabolites that deter other species from growing. These molecules also benefit the host by
eliminating invading bac-teria including Salmonella, Shigella, Clostridium difficile, Bacillus
cereus, and other pathogens. The bacteria must also resist antimicrobial peptides and
immunoglobulin (Ig)A produced by the host and released into the bowel.Metabolism of nutrients
plays a major role in the symbiotic relationship between the human host and microbe. Bacteria
in the human gut are responsible for metabolizing complex carbohydrates (including cellulose)
to provide small-chain fatty acids such as acetate, propionate, and butyrate that can be readily
transported and used by the cells of our body. These acids also limit the growth of undesirable
bacteria. Other bacteria graze on the carbohydrates, the mucins that line the epithelium, or the
oils released in our sweat. Bacteroidetes and Firmicutes are more efficient than others at
breaking down complex carbohydrates, including plant cell wall com-pounds (cellulose, pectin,
xylan) as well as host-derived carbohydrates, including those attached to the mucins or
chondroitin sulfates of the protective mucous layer of the intestine. Increases in the ratio of
these bacteria in the gut microbiome can lead to a higher efficiency in storage of the metabolic
byproducts. This can be a benefit for malnourished populations or patients with debilitating
diseases such as cancer, or can lead to obesity in well-nourished populations.
• Role of the Microbiome in Disease
If the normal microbiome characterizes health, alterations in the microbiome can signify
disease, a relationship we are only beginning to understand. In 1884 Robert Koch and Friedrich
Loeffler defined the relationship between an organ-ism and infection. The Koch postulates were
based on the concept of one organism: one disease. Microbiome research has introduced a
new concept—disease caused by a com-munity of organisms rather than a single species of
bacteria, and the influence extends beyond traditional “infectious” diseases to include
immunologic and metabolic disorders such as inflammatory bowel disease, obesity, type 2
diabetes, and celiac disease. We are now at the forefront of a new era of defining infectious
diseases.Disruption of the normal microflora (commonly referred to as dysbiosis) can lead to
disease by the elimination of needed organisms or allowing the growth of inappropriate bacteria.
For example, following exposure to antibiotics and suppression of the intestinal normal flora, C.
difficile is able to proliferate and express enterotoxins, leading to inflamma-tion of the colon
(antibiotic-associated colitis). Another disease of the colon, ulcerative colitis, is associated with
an increased level of bacteria producing mucin-degrading sul-fatases, leading to degradation of
the protective mucosal lining of the intestinal wall and stimulation of inflammatory immune
responses. Individuals with an intestinal microbiota that is more efficient at breaking down
complex carbohy-drates internalize rather than void these nutrients and are therefore
susceptible to obesity and a predisposition to metabolic syndromes such as type 2 diabetes. Not
all patients genetically predisposed to celiac disease, an
Glossary of Terms
Term Definition
Microbiota Community of microbes that live in and on an individual; can vary
substantially between environmental sites and host niches in health and
disease
Normal flora Microbiota
Microbiome Aggregate collection of microbial genomes in the microbiota
Core microbiome Commonly shared microbial species among individuals at specific body
sites; although typically represented by a limited number of species, these
comprise the largest proportion of the microbial population
Secondary Microbial species that contribute to the unique diversity of individuals at
microbiome specific body sites; typically present in proportionately small numbers
Functional Required functions (e.g., metabolism of nutrients, regulation of the immune
redundancy response) that are provided by the diverse members of the microbiota
Taxonomic The diverse number of species that comprise the microbiota
diversity
Prebiotic Food ingredient that supports the growth of one or more members of the
microbiota
Probiotic Live organism that when ingested is believed to provide benefit to the host
You might also like
- Antioxidants: Zeaxanthin: Metabolism, Properties, and Antioxidant Protection of Eyes, Heart, Liver, and SkinDocument18 pagesAntioxidants: Zeaxanthin: Metabolism, Properties, and Antioxidant Protection of Eyes, Heart, Liver, and SkinAcengHamudinNo ratings yet
- Skin Microneedling Plus Platelet-Rich PlasmaDocument7 pagesSkin Microneedling Plus Platelet-Rich PlasmaAcengHamudin100% (1)
- Uas Penuaan Seluler: Dosen Pengampu: Edhyana K.S, DR., PHDDocument57 pagesUas Penuaan Seluler: Dosen Pengampu: Edhyana K.S, DR., PHDAcengHamudinNo ratings yet
- Immuno Senescence PublishedDocument5 pagesImmuno Senescence PublishedAcengHamudinNo ratings yet
- Conceiving The Research QuestionDocument16 pagesConceiving The Research QuestionAcengHamudinNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Parboiled RiceDocument38 pagesParboiled RiceArpit RohillaNo ratings yet
- OTC-26068-MS Wettability Alteration of Heavy-Oil/Bitumen Containing Carbonates Using Solvents, High PH Solutions and Nano/Ionic LiquidsDocument18 pagesOTC-26068-MS Wettability Alteration of Heavy-Oil/Bitumen Containing Carbonates Using Solvents, High PH Solutions and Nano/Ionic Liquidsjose floresNo ratings yet
- Surgeon ListDocument6 pagesSurgeon Listkaushal shahNo ratings yet
- Helicopter LiftingDocument11 pagesHelicopter LiftingWidya Ningrum100% (1)
- Types of CompressorsDocument44 pagesTypes of Compressorsjezreeleda.limNo ratings yet
- BHB SandeepDocument2 pagesBHB SandeepAbzad HussainNo ratings yet
- Aipmt-Neet Cutoff 2012Document178 pagesAipmt-Neet Cutoff 2012rahuldayal90No ratings yet
- Chapter 9 - Firewalls and Intrusion Detection SystemDocument8 pagesChapter 9 - Firewalls and Intrusion Detection SystemJasminNo ratings yet
- FMS 55 1050 LD Spec REV1.0.3 1Document5 pagesFMS 55 1050 LD Spec REV1.0.3 1E ShNo ratings yet
- Current AffairsDocument20 pagesCurrent AffairsugoobiokaforNo ratings yet
- DOPE Personality TestDocument8 pagesDOPE Personality TestMohammed Hisham100% (1)
- Using SSPC Coating Material Standards 1Document18 pagesUsing SSPC Coating Material Standards 1achusanachu100% (1)
- 20mpe18 Aeor Assignment 3Document9 pages20mpe18 Aeor Assignment 3Shrinath JaniNo ratings yet
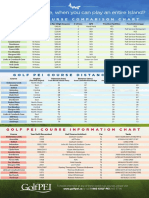
- Golf Pei Course Comparison ChartDocument1 pageGolf Pei Course Comparison ChartSteve DimondNo ratings yet
- Fire Protection MethodsDocument3 pagesFire Protection MethodsEquilibrium EngineersNo ratings yet
- Chapter - IDocument60 pagesChapter - IAnil ThakurNo ratings yet
- Trauma Informed Care Information From Allison Sampson Jackson PDFDocument14 pagesTrauma Informed Care Information From Allison Sampson Jackson PDFMirjana StevanovicNo ratings yet
- Don Honorio Ventura Technological State University Bacolor, PampangaDocument10 pagesDon Honorio Ventura Technological State University Bacolor, PampangaAnonymous Xwd7uWe0YUNo ratings yet
- Quality Control Inspection ReportDocument5 pagesQuality Control Inspection ReportjaymarNo ratings yet
- Assignment 2Document2 pagesAssignment 2Aishwarrya NanthakumarNo ratings yet
- Eudrabook - Epub - en - European Commission - HealthDocument826 pagesEudrabook - Epub - en - European Commission - Healthpr1asdNo ratings yet
- DPPH (1,1-Diphenyl-2-Picrylhydrazyl) Radical Scavenging Activity of Flavonoids Obtained From Some Medicinal PlantsDocument4 pagesDPPH (1,1-Diphenyl-2-Picrylhydrazyl) Radical Scavenging Activity of Flavonoids Obtained From Some Medicinal PlantsEtika Ayu LestariNo ratings yet
- Chemistry Notes On The Periodic Table: Syllabus 5070 O' LevelDocument8 pagesChemistry Notes On The Periodic Table: Syllabus 5070 O' LevelNancy Mohamed100% (1)
- Bio 11.1 LE 2 NotesDocument7 pagesBio 11.1 LE 2 NotesCode BlueNo ratings yet
- Insect Milk: VocabularyDocument3 pagesInsect Milk: VocabularyChris Mae Vinson DalumpinesNo ratings yet
- (Susan Aldridge) The Thread of Life The Story ofDocument272 pages(Susan Aldridge) The Thread of Life The Story ofsergioNo ratings yet
- Likes and DislikesDocument4 pagesLikes and DislikesgabysoteloNo ratings yet
- Journal of Drug Delivery Science and TechnologyDocument11 pagesJournal of Drug Delivery Science and TechnologyNguyen PhuongNo ratings yet
- Simply Put - ENT NOSE LECTURESDocument38 pagesSimply Put - ENT NOSE LECTURESCedric KyekyeNo ratings yet
- Grade 5 Health Most Essential Learning Competencies MELCsDocument6 pagesGrade 5 Health Most Essential Learning Competencies MELCsSaldi VitorilloNo ratings yet