Professional Documents
Culture Documents
The Ten Commandments of Treating Preschool Children Who Wheeze PDF
Uploaded by
Pablo Peña AbajoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Ten Commandments of Treating Preschool Children Who Wheeze PDF
Uploaded by
Pablo Peña AbajoCopyright:
Available Formats
South African Family Practice
ISSN: 2078-6190 (Print) 2078-6204 (Online) Journal homepage: http://www.tandfonline.com/loi/ojfp20
The “Ten Commandments” of treating preschool
children who wheeze
RJ Green , A Halkas & E Weinberg
To cite this article: RJ Green , A Halkas & E Weinberg (2012) The “Ten Commandments” of
treating preschool children who wheeze, South African Family Practice, 54:4, 316-318, DOI:
10.1080/20786204.2012.10874242
To link to this article: https://doi.org/10.1080/20786204.2012.10874242
© 2012 SAAFP. Published by Medpharm.
Published online: 15 Aug 2014.
Submit your article to this journal
Article views: 206
View related articles
Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=ojfp20
Review Article: The “Ten Commandments” of treating preschool children who wheeze
The “Ten Commandments” of treating preschool
children who wheeze
Green RJ, PhD, FRCP, Director and Head
Department of Paediatrics and Child Health, University of Pretoria
Halkas A, FC Paed(SA), MMed, FCCP, Director
Children’s Chest and Allergy Clinic, Krugersdorp Hospital
Weinberg E, FCPaeds, FAAAAI, Consultant, Allergy Unit, UCT Lung Institute
Correspondence to: Robin Green, e-mail: robin.green@up.ac.za
Keywords: recurrent wheezing, preschool, asthma
Abstract
Wheezing in young children is problematic for most practitioners. Difficulties arise in both the diagnosis and management
of this clinical phenotype. Not all preschool children who wheeze have asthma. Therefore, we suggest that the “Ten
Commandments” of managing preschool wheezing include thinking that in very young infants (< 1 year) wheezing is likely
to be viral in origin; realising that allergy testing is mandatory to diagnose the cause of early wheezing; taking a history of
asthma and allergy in family members; noting that chronic coughing is a pointer to asthma; using the term “asthma” if that
is the diagnosis; ensuring that the environmental avoidance of triggers is addressed; using a short course of montelukast for
virus-induced wheezing episodes; avoiding steroids to treat virus-induced wheezing; treating associated nasal symptoms;
and making sure that the follow-up of children addresses the issue of stopping therapy if it is not working.
Peer reviewed. (Submitted: 2011-11-04. Accepted: 2012-02-08.) © Medpharm S Afr Fam Pract 2012;54(4):316-318
Introduction to avoid the unnecessary side-effects from drugs. These
“commandments” promote the idea of identifying various
Recurrent wheezing is very common in preschool children.
phenotypes in order to label the condition, and treat it
There have been many attempts to classify wheezing in
correctly.
preschool children,1,2 but the most useful classification
seems to be that published by the European Respiratory The “Ten Commandments” of treating
Society, in which wheeze phenotypes are described as
preschool children who wheeze
“episodic viral-induced” or “multi-trigger”.3 In the former
group, children wheeze predominantly in response to viral 1. Wheezing that has a very early age of onset (< 1 year) is
infections of the airway, while in the latter group, they also likely to be viral in origin.
wheeze due to exposure to factors associated with airway 2. All preschool children who wheeze must undergo an
hyper-responsiveness, such as cold air, emotions, exercise, allergy test, preferably a skin-prick test (SPT).
pollutants, strong odours, and allergens. This latter group 3. A family history of asthma suggests that the child has
closely resembles the classic description of asthma. asthma.
It is often difficult to diagnose the cause of wheezing in 4. The presence of a cough is important in the diagnosis of
preschool children, and to manage it correctly. Asthma is asthma.
a common problem that should be controlled, but often, it 5. Use the term “asthma” if it fits.
is not well managed. However, not all wheezing preschool 6. Environmental control, and patient and parent educa-
children have asthma. It should be determined whether or tion are necessary for all asthmatics, and controller
not the wheezing is due to asthma, or another cause. In
medication may be required [inhaled corticosteroids
essence, we are taught that asthma should be controlled
(ICS) or montelukast].
to the point that symptoms and impairment of quality of
7. Treat virus-induced wheezing with montelukast for
life disappear, but that virus-induced wheezing should not
14 days.
be treated in the same way as asthma. Generally, most
preschool children who wheeze have ongoing and frequent 8. Avoid the use of oral corticosteroids when treating virus-
symptoms that might not be improved by controller induced wheezing exacerbations.
medication. We propose using these “Ten Commandments” 9. It is important to treat nasal symptoms.
when treating preschool children who wheeze. This will 10. Follow-up is important. Stop treatment that does not
make the condition less difficult to manage, and will help work.
S Afr Fam Pract 2012 316 Vol 54 No 4
Review Article: The “Ten Commandments” of treating preschool children who wheeze
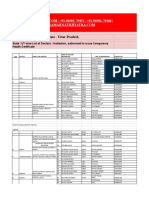
1. Wheeze that has a very early age of onset Table II: The Asthma Prediction Index5
(< 1 year) is likely to be viral in origin Major criteria Minor criteria
Very young children experience multiple viral respiratory tract Family history of asthma Eosinophilia > 4%
infections that may result in lower airway involvement and Positive history of atopic eczema Positive history of allergic rhinitis
wheezing. Although asthmatics experience exacerbations Positive skin-prick test Wheeze without viral infections
that are also largely triggered by viruses, asthma is not The diagnosis of asthma can be made if one major or two minor
common before the age of one year. criteria are satisfied.
2. All preschool children who wheeze must specificity of the term ‘wheezing’, and coughing correlates
undergo an allergy test, preferably an SPT
with lung function and atopy in preschoolers, similar to, and
Recent guidelines for the diagnosis and management of independent of, wheezing”.6
asthma in preschool children attest to the importance of
5. Use the term “asthma” if it fits
proving allergy. The recent Global Initiative for Asthma (GINA)
guideline4 for the diagnosis and management of asthma Despite a recent pronouncement by the European Task
in children who are five years old and younger, contains Force on wheezing3 in preschool children, that “the majority
clear pointers for the diagnosis of asthma in preschoolers of the task force agreed not to use the term ‘asthma’
(Table I). The use of the Asthma Prediction Index (API), as to describe preschool wheezing illness, since there is
a measure of atopy, is recommended. In addition, a set insufficient evidence showing that the pathophysiology of
of symptoms that indicate that asthma is likely should be preschool wheezing illness is similar to that of asthma in
identified in the child. older children and adults”, this is unhelpful. It also threatens
A clear message is that asthma is diagnosis-based, on the to undermine the goals of managing asthma. The term
finding of atopy or allergy. In this regard, an SPT is best. “asthma” should be used when it is applicable. A child who
has multiple wheezing triggers, including, but not limited
Table I: GINA guideline for the diagnosis of asthma in preschool
children to, viral infections, can be considered to have asthma,
Strong support for diagnosis rather than multi-trigger wheezing. Such triggers include
allergens, environmental pollutants (especially cigarette
• Wheezing: Most common asthma symptom
• Coughing: Recurrent or persistent smoke), exercise, cold air, night-time, and laughter.
• Coughing accompanied by wheezing
6. Environmental control and patient and parent
• Nocturnal coughing (occurring when the child is asleep)
• Exercise-induced coughing education, are necessary for all asthmatics, and
• In the absence of respiratory infection. controller medication may be required
Supportive evidence Essentially, two therapies may control symptoms in a
Therapeutic trial young child with asthma. If used, inhaled corticosteroids
• Strong-acting bronchodilators and inhaled glucocorticosteroids (ICS) should be administered at the lowest dose to control
(eight to 12 weeks) (Evidence D)
• Tests for atopy (Asthma Prediction Index)
symptoms. Increasing the dose usually makes no difference
• Chest X-ray. to symptom control, but increases the possibility of side-
effects. Montelukast has a weaker anti-inflammatory
3. A family history of asthma suggests that the effect, but has the advantage of being given orally, thereby
child has asthma enhancing adherence to therapy. Although the best form
of treatment is still under debate, there is no doubt that
An important feature of the atopic label is a family history of
environmental triggers, especially cigarette smoke, should
asthma, or another allergic condition. This is built into the
be avoided, and that parents should be educated about the
API (Table II).
disease. Education should encompass a description of the
4. The presence of a cough is important in the disease, the need for regular controller therapy, device co-
diagnosis of asthma ordination, and avoidance of triggers.
Bisgaard et al recently commented on the importance 7. Treat virus-induced wheezing with montelukast
of the presence of a cough in diagnosing asthma: “The
for 14 days
term ‘wheezing’ is often misclassified. Control of asthma
symptoms correlates best with composite scores of There is evidence from three well-controlled studies that,
symptoms, rather than wheezing. Audible wheezing occurs during an exacerbation, giving young children montelukast
late in airway obstruction. There is no data on sensitivity or for 14 days is useful in treating viral-induced wheezing.7-9
S Afr Fam Pract 2012 317 Vol 54 No 4
Review Article: The “Ten Commandments” of treating preschool children who wheeze
8. Avoid the use of oral corticosteroids when of medication and treatment, is required. Medication should
treating virus-induced wheezing exacerbations not be prescribed regularly to any child with asthma if it
The treatment of wheezing in preschool children presents does not control the child’s symptoms.11
many challenges. Oral corticosteroids are often used.
References
However, there is no clear evidence that they are effective in
these children. Oral corticosteroids have been subjected to 1. Martinez FD, Wright AL, Taussig LM, et al. Asthma and wheezing in the first six
years of life. N Engl J Med. 1995;332(3):133-138.
a clinical study, and have been shown to have no effect on
symptom scores, duration of hospitalisation, and numbers 2. Lowe LA, Simpson A, Woodcock A, et al. Wheeze phenotypes and lung function
in preschool children Am J Respir Crit Care Med. 2005;171(3):231-237.
of readmissions, in children with episodic viral wheezing.10
3. Brand PLP, Baraldi E, Bisgaard H. Definition, assessment and treatment of
In preschool children, who have wheezing exacerbations
wheezing disorders in preschool children: an evidence-based approach. Eur
due to asthma, there is no evidence to support the use Respir J. 2008;32(4):1096-1110.
of oral corticosteroids, but a trial of such therapy may be 4. Diagnosis and management of asthma in children 5 years and younger, 2009.
beneficial regarding more severe exacerbations. Global Initiative for Asthma [homepage on the Internet]. c2011. Available from:
http://www.ginasthma.org
9. It is important to treat nasal symptoms 5. Castro-Rodriguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to
Both asthma and allergic rhinitis are defined as inflammatory define risk of asthma in young children with recurrent wheezing. Am J Respir Crit
Care Med. 2000;162(4 Pt 1):1403-1406.
conditions. The epidemiological relationship between upper
6. Bisgaard H, Pipper CB, Bønnelykke K. Endotyping early childhood asthma by
and lower airway disease (rhinitis and asthma) demonstrates
quantitative symptom assessment. J Allerg Clin Immunol. 2011;127(5):1155-1164.
that 58-78% of asthmatics also have allergic rhinitis. There
7. Bisgaard H, Zielen S, Garcia-Garcia ML, et al. Montelukast reduces asthma
is now clear evidence that uncontrolled allergic rhinitis exacerbations in 2- to 5-year-old children with intermittent asthma. Am J Respir
worsens asthma, and makes it more difficult and expensive Crit Care Med. 2005;171(4):315-322.
to treat. The opposite is true of treating rhinitis in asthmatics, 8. Robertson CF, Price D, Henry R, et al. Short-course montelukast for intermittent
in which case, their asthma is also better controlled, while asthma in children. A randomized controlled trial. Am J Respir Crit Care Med.
2007;175(4):323-239.
costs are lower. Therefore, allergic rhinitis therapy is truly
9. Johnston NW, Mandhane PJ, Dal J, et al. Attenuation of the September epidemic
cost-effective in asthmatics.
of asthma exacerbations in children: a randomised, controlled trial of montelukast
10. Follow-up is important: stop treatment that does added to usual therapy. Pediatrics. 2007;120(3):e702-e712.
not work 10. Panickar J, Lakhanpaul M, Lambert PC, et al. Oral prednisone for preschool
children with acute virus-induced wheezing. N Eng J Med. 2009;360(4):329-338.
Since asthma is often difficult to define and treat in 11. Motala C, Green RJ, Manjra A, et al. Guideline for the management of chronic
preschool children, regular review, especially of the success asthma in children: 2009 update. S Afr Med J. 2009;99(Part 2):877-912.
S Afr Fam Pract 2012 318 Vol 54 No 4
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Apis S4hanaDocument8 pagesApis S4hanaPablo Peña AbajoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Internet of Things Architecture Iot-A Project Deliverable D7.2 - Exact Definition Use Case 1 and Use Case 2Document86 pagesInternet of Things Architecture Iot-A Project Deliverable D7.2 - Exact Definition Use Case 1 and Use Case 2Pablo Peña AbajoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Transform Your Logistics Processes With: SAP Digital Logistics SolutionsDocument76 pagesTransform Your Logistics Processes With: SAP Digital Logistics SolutionsPablo Peña AbajoNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Sap Roadmap For ManufacturingDocument20 pagesSap Roadmap For ManufacturingPablo Peña AbajoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Is XML Einvoicing Standard SPDocument26 pagesIs XML Einvoicing Standard SPPablo Peña AbajoNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Jacobi Aquasorb F23 SDSDocument10 pagesJacobi Aquasorb F23 SDSkhiemNo ratings yet
- Uttar PradeshDocument7 pagesUttar PradeshPawani Gupta100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 2018-The Relationship Between PerceivedDocument8 pages2018-The Relationship Between PerceivedFernandoCedroNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- CS Form No - 6, Revised 2020 (Application For Leave) (Fillable) - 1Document3 pagesCS Form No - 6, Revised 2020 (Application For Leave) (Fillable) - 1ben carlo ramos srNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Sacred Ash (3.5e Epic Spell) - D&D WikiDocument1 pageSacred Ash (3.5e Epic Spell) - D&D WikiJuan MonsalveNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- PCR My - Wan Nur Afiyah - 8mayDocument1 pagePCR My - Wan Nur Afiyah - 8mayEvie SuriNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Air PollutionDocument6 pagesAir PollutionJaylynn MurungiNo ratings yet
- Male Female PsychologyDocument38 pagesMale Female PsychologyParamjit SharmaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 1K Solid BasecoatDocument6 pages1K Solid BasecoatjanakaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Fluid Therapy: Route Advantages DisadvantagesDocument3 pagesFluid Therapy: Route Advantages DisadvantagesAshref BelhajNo ratings yet
- Final Draft Research EssayDocument4 pagesFinal Draft Research EssayizellahnavarroNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Chapter 10Document38 pagesChapter 10chindypermataNo ratings yet
- Iso 13485Document15 pagesIso 13485sayem.unicertNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- API BGD DS2 en Excel v2 4685979Document339 pagesAPI BGD DS2 en Excel v2 4685979Areesha KamranNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- J Clinic Periodontology - 2018 - Caton - A New Classification Scheme For Periodontal and Peri Implant Diseases andDocument8 pagesJ Clinic Periodontology - 2018 - Caton - A New Classification Scheme For Periodontal and Peri Implant Diseases andVõ Thị Mỹ NhungNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Nyvad 1999Document9 pagesNyvad 1999Felipe Maldonado ArayaNo ratings yet
- 2022 MEDICATION ERROR Without ReferenceDocument133 pages2022 MEDICATION ERROR Without ReferenceSuhaime UEMNo ratings yet
- Full Download Test Bank For Health Psychology 3rd Edition Sanderson PDF Full ChapterDocument13 pagesFull Download Test Bank For Health Psychology 3rd Edition Sanderson PDF Full Chapterrequinneologic8yzqgt100% (17)
- March/April 2002 Number 2 105-208 ©: Operative Dentistry, IncDocument108 pagesMarch/April 2002 Number 2 105-208 ©: Operative Dentistry, IncZulvan AviviNo ratings yet
- Understated 1431 1440Document34 pagesUnderstated 1431 1440Ata100% (1)
- Medical Student Assessment Form in PDFDocument4 pagesMedical Student Assessment Form in PDFDanial S. SaktiNo ratings yet
- Tanishqa Jogani - TAPMIDocument3 pagesTanishqa Jogani - TAPMITanishqa JoganiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Bottle Packing Price List 2020-21Document21 pagesBottle Packing Price List 2020-21healerharishNo ratings yet
- 2022 Benefits Enrollment GuideDocument28 pages2022 Benefits Enrollment GuideWyattNo ratings yet
- Nebosh: Management of Health and Safety Unit Ig1Document5 pagesNebosh: Management of Health and Safety Unit Ig1TFIBER PROGRESSNo ratings yet
- Hold Time Study ProtocolDocument9 pagesHold Time Study ProtocolMubarak Patel100% (1)
- ResearchDocument70 pagesResearchMagud, Jemverick Jan Leonard O.No ratings yet
- Method Statement For Installation of Telephone ManholeDocument4 pagesMethod Statement For Installation of Telephone ManholemujtiobamaliblNo ratings yet
- Effective People Management - Interpersonal Skills For ManagersDocument8 pagesEffective People Management - Interpersonal Skills For ManagersJude LarteyNo ratings yet
- CV Dr. ErwadiDocument3 pagesCV Dr. ErwadiErwadi ErwadiNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)