Professional Documents
Culture Documents
Bratton 2008
Uploaded by
Mariska Regina RannuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bratton 2008
Uploaded by
Mariska Regina RannuCopyright:
Available Formats
Tinea capitis is a common pediatric infection most frequently 2. Friedlander SF, et al. Pediatrics. 2002;109:602-607.
caused by T tonsurans in the US.1-3 Systemic treatment is required 3. Fleece D, et al. Pediatrics. 2004;114:1312-1315.
to eradicate the infection and griseofulvin has traditionally been 4. Lamasil oral granules [package insert]. East Hanover, NJ: Novar-
the antifungal therapy of choice.3 In clinical practice, effective tis Pharmaceuticals Corp; 2007.
treatment with griseofulvin often requires higher doses and a lon-
ger duration of therapy than recommended on the package label-
ing.1,2 Effective alternative antifungal therapies that have good oral
tolerability and require a shorter course of treatment are therefore
likely to be advantageous. CRITICAL CARE
This is the largest pediatric trial of terbinafine to date. Similar to
other prior studies that evaluated terbinafine tablets, terbinafine
hydrochloride granules appear to be efficacious and well-tolerated
Clinical Practice
in the treatment of tinea capitis.1-3 This new pediatric formulation,
which can be sprinkled on non-acidic food (such as pudding), may
Guidelines for
be easier for children to consume than the tablet formulation.
A previous meta-analysis of comparative, randomized trials Management of
of griseofulvin versus terbinafine tablets also found that terbi-
nafine was at least as effective as griseofulvin in the treatment
of Trichophyton species infections.3 However, the dosing and
Encephalitis
duration of treatment of griseofulvin in that study were less than Source: Tunket AR, Glaser CA, Bloch KC, et al. The management
what is often used in clinical practice, and the overall cure rate of of encephalitis: clinical practice guidelines by the Infectious
terbinafine in that trial was lower than those found in other prior Diseases Society of America. Clin Infect Dis. 2008;47(3):303-327;
studies.1,2 doi:10.1086/589747
Contrary to usual clinical practice, no adjunctive therapy, such
PICO
as antifungal shampoo, was utilized in the current study, which
may have affected cure rates. Question: In patients with suspected encephalitis, what is the
Terbinafine oral granules received US approval in September most appropriate diagnostic evaluation and empiric therapy?
2007 to treat tinea capitis in children age four years and older.4 Question type: Intervention
Recommended six-week dosing is based on body weight (<25 kg:
125 mg/day; 25-35 kg: 187.5 mg/day; >35 kg: 250 mg/day) and the Study design: Practice guideline
granules are available in 125 mg and 187.5 mg packets.4 Since T ton-
T
surans is the most common dermatophyte causing tinea capitis in he objective of this practice guideline is to provide clinicians
the US, terbinafine granules are a potential alternative antifungal with evidence-based recommendations in the approach to
therapeutic option to treat tinea capitis caused by Trichophyton patients with encephalitis. The work is a consensus state-
species. However, if Microsporum species are identified on fungal ment by a panel of pediatric and internal medicine infectious
culture, griseofulvin is probably a better choice. Performing a fun- disease specialists and neurologists with expertise in encephalitis
gal culture on patients suspected to have tinea capitis is therefore who reviewed the literature published since 1996 regarding the
highly recommended to not only confirm infection, but also to diagnosis and treatment of encephalitis.
help guide appropriate therapy. In the approach to the patient with encephalitis, an attempt
Shorter duration of therapy and the ease of administration should be made to establish an etiologic diagnosis. The panel
of terbinafine hydrochloride granules are potential advantages recommends cerebrospinal fluid (CSF) analysis in all cases of sus-
compared to griseofulvin. Cost of terbinafine granules may be pected encephalitis. Culture for bacteria and fungus is indicated,
less since the duration of therapy is potentially shorter than stan- but since CSF cultures are generally of limited value in the deter-
dard treatment with griseofulvin; however, the package insert for mination of the viral causes of encephalitis, CSF should be tested
terbinafine granules recommends baseline liver function studies by PCR for herpes simplex virus (HSV), Epstein-Barr virus (EBV),
prior to treatment (baseline lab work is not usually performed in varicella zoster virus (VZV), the enteroviruses, and Mycobacterium
healthy children treated with griseofulvin) which may increase the tuberculo. In patients with clinical evidence of HSV encephalitis
overall cost of therapy.4 but negative results on initial CSF HSV PCR, repeat testing in 1-3
days may be positive.
References CSF and serum antigen tests are useful in diagnosing Cryptococ-
1. Gonzalez U, et al. Cochrane Database Syst Rev. (4):CD004685, cus neoformans while CSF and urine antigen tests are useful for
2007. diagnosing histoplasmosis. Spirochetes such as Treponema pal-
lidum and Borrelia burgdorferi infections can be detected using
non-specific (VDRL) as well as specific antibody tests in the CSF
and serum. In the appropriate season or clinical setting, CSF can be
sent for IgM to West Nile virus, St. Louis encephalitis, and VZV.
AAP Grand Rounds™ is published monthly by the American Academy of Testing of sites outside of the nervous system may be helpful
Pediatrics, 141 Northwest Point Blvd., Elk Grove Village, IL 60007. Copy- in establishing cause for the encephalitis. While viral cultures of
right © 2008 American Academy of Pediatrics. All rights reserved. Post- the CSF are rarely useful, sputum can be sent for viral antigen
master: Send address changes to AAP Grand Rounds, American Academy testing and culture. Biopsy of specific tissues for culture, antigen
of Pediatrics, Customer Service Center, 141 Northwest Point Blvd., Elk
Grove Village, IL 60007-0198.
detection, nucleic acid amplification tests (such as PCR), and his-
topathologic examination should be performed. Serologic testing
ISSN Numbers
Print: 1099-6605 for HIV, EBV, and Mycoplasma pneumonia may be useful. In cer-
Online: 1556-362X tain seasons, serologic testing should be considered for St. Louis
Customer Service and Renewals: (866) 843-2271. encephalitis virus, Eastern equine encephalitis virus, Venezuelan
Email Address: grandrounds@aap.org equine encephalitis virus, La Crosse virus, and West Nile virus as
Subscription Rates: AAP member $91/year; non-member $114/year (12 well as Rickettsia rickettsii, Ehrlichia chaffeensis, and Anaplasma
issues), including up to 18 AMA PRA Category 1 credit(s)™. phagocytophilum.
Senior Managing Editor: Joseph Puskarz CT and MRI are most frequently used to evaluate patients with
Managing Editor: Joseph Puskarz encephalitis, MRI is more sensitive and specific. MRI may show
Editorial Assistant: Megan Lenz
Production: Michael Hayes classic findings of specific infections such as HSV encephalitis or
Editorial Associates: Nancy Cochran, Seattle, WA; Nancy Moreland, may be useful to exclude conditions with a clinical presentation
Burlington, VT similar to that of encephalitis, such as acute disseminated en-
50 AAP Grand Rounds
Downloaded from http://aapgrandrounds.aappublications.org/ at University of Michigan on June 17, 2015
cephalomyelitis (ADEM), a disease mediated by an immunologic
response to an antigenic stimulus. Identifying ADEM is particularly Weighing the Evidence:
important as therapy includes high-dose steroids. Clinical Practice Guidelines
Although EEG is rarely useful in identifying a pathogen, it has
a role in identifying patients with nonconvulsive seizure activity M. Paulina Velasquez, MD
who are confused, obtunded, or comatose. In 80% of patients with Virgina A. Moyer, MD, MPH, FAAP
HSV encephalitis, a temporal lobe focus demonstrates lateralizing
periodic discharges. Where you live or which doctor you choose should not be the
Initial treatment of encephalitis should always include acyclovir primary determinant of what specific tests and treatment you get
and empiric antibiotic therapy in patients with suspected bacterial — but often is.1 While care should vary according to the patient’s
meningitis, including doxycycline if risk factors for Rickettsia or condition and values, it should not vary based on physician “style.”
Ehrlichia infections are present. Once an etiologic agent is identi- This is ever more important in the era of frequent patient handoffs.
fied, therapy should be targeted to that agent and other antimicro- A clinical practice guideline is a set of recommendations whose
bial treatment discontinued. main objective is to standardize medical practice regarding a specific
health condition. The creation of such sets promotes cost-effective
practice while helping minimize the occurrence of medical errors
Commentary by Susan L. Bratton, MD, MPH, FAAP and inappropriate variation in care. Guidelines are not rules set in
Pediatric Critical Care Medicine, Primary Children’s Medical Center, University
stone; they have to be flexible enough to allow for individualized
of Utah Health Sciences Center, Salt Lake City, UT
changes based on clinical judgment. The aim of a good guideline
Dr. Bratton has disclosed no financial relationship relevant to this commentary. This commentary does not contain
a discussion of an unapproved/investigative use of a commercial product/device. is always to improve quality of care and promote optimal health
outcomes for patients.2
Encephalitis is defined as an inflammatory process of the brain But…what makes a guideline “good”? This question has to be
associated with acute neurologic dysfunction. This management answered whether you are looking to write a new guideline or evalu-
ating an existing guideline before introducing it into daily practice.
guideline is a useful and concise reference for the approach to
First, the process of creating a guideline should involve a multidis-
patients with encephalitis. Although a wide variety of agents have
ciplinary team including all relevant stakeholders in order to get
been reported to cause encephalitis, most are viral. The underly- adequate input from different points of view. A rigorous method of
ing cause, however, remains uncertain in approximately 50-60% development, including a thorough search, systematic review, and
of cases despite extensive testing.1 A thorough history is needed grading of scientific evidence related to the topic is required. This is
to reveal risk factors such as travel, exposure to mosquito or tick accomplished by extracting data on the benefits, harms, and even
bites, animal exposure, vaccination status, and patient immune costs of different interventions from all important studies.3 The
status. The season of the year and prevalence of disease in the lo- information obtained is then categorized according to its quality,
cal community are helpful in targeting the diagnostic work-up for and linked to each of the recommendations in the guideline. When
encephalitis. However, no specific treatment is currently available the evidence is limited, expert opinion often fills in the gaps so that
for most infectious causes of encephalitis. guidelines can be comprehensive.
The expert guidelines emphasize that treatment with acyclovir As long as this process is transparent, the reader can indepen-
be started in all patients with suspected encephalitis pending dently analyze the recommendations provided, and then decide if
diagnostic studies. Such treatment is associated with improved they are applicable to any specific case.4 Keep in mind that the qual-
survival and decreased morbidity from HSV and VZV but not EBV ity of the evidence is not the sole determinant of the strength of the
recommendation: very good evidence might exist but the trade-off
encephalitis. Although PCR testing is very specific for HSV, it is not
between benefits and harms may be so close that an evidence-based
100% sensitive, and for patients with clinical features suggestive of
recommendation one way or the other cannot be made.5
HSV infection, repeat testing of the CSF with PCR may be indicated Another issue that has to be considered is the presence of edito-
if the initial testing is negative. Patients with temporal lobe findings rial independence and conflicts of interest. In some instances, ex-
on MRI or seizure foci typical for HSV should be treated despite an tensive ties between guideline committees and the pharmaceutical
initial negative PCR, and expert consultation should be sought to industry have been revealed.6 As complete avoidance of corporate
guide final treatment duration. sponsorship and exclusion of experts with financial ties may be
The practicing pediatrician must remain particularly vigilant very difficult to achieve, public disclosure of all potential conflicts of
regarding neonates with fever and signs of sepsis. Among febrile interest should be a minimal requirement to assure that those using
neonates with a CSF pleocytosis (either mononuclear or poly- the guideline can ascertain where bias might exist.4
nuclear) approximately 1-2% have documented HSV encephalitis2 Finally, a good guideline should not be static; it should be
and require prompt treatment with high dose acyclovir. Reported reviewed and updated regularly, and a mechanism should be in
risk factors for neonatal HSV include maternal factors (maternal place to trigger a review if new evidence becomes available before
primary HSV infection, maternal fever, vaginal delivery) and infant the scheduled update.
factors (prematurity, postnatal HSV contact, vesicular rash, hypo- A guideline that has been rigorously developed by a multidisci-
thermia, lethargy, seizures, respiratory distress, or CSF pleocyto- plinary group should be characterized by clarity, validity, and re-
producibility. Tools that can help you assess guidelines include the
sis).3 Pediatric patients with encephalitis are at risk for brain injury
AGREE instrument, the SIGN process, and the CASP tools.6-8 These
and neuropsychologic follow-up is appropriate. checklists can help you determine whether the goal of moving from
best evidence to best practice is likely to be achieved. When you see
Editors’ Note
guidelines for clinical care, use the criteria discussed here to deter-
The authors of this practice guideline meet the standard out- mine whether you will incorporate them into your practice.
lined in Weighing the Evidence. The important role of head MRI
to help distinguish an infectious from post-infectious etiology of References
encephalitis and the automatic administration of acyclovir upon 1. Wennberg JE, et al. Geography and the Debate Over Medicare Reform.
Health Affairs. February 13, 2002. http://content.healthaffairs.org/cgi/
suspicion of the diagnosis are just two of the recommendations
content/abstract/hlthaff.w2.96v1
that head up the new guidelines for this serious inflammatory 2. AAP Steering Committee on Quality Improvement and Management.
process. Pediatrics. 2004;114:874-877.
3. Shekelle PG, et al. BMJ. 1999;318:593-596.
References 4. AAP Steering Committee on Quality Improvement and Management.
1. Glaser CS, et al. Clin Infect Dis. 2003;36:731-742. Pediatrics. 2008;121:643-646.
5. Guyatt GH, et al. BMJ. 2008;924-926.
2. Caviness AC, et al. J Pediatr. 2008;153:164-169. 6. The AGREE Collaboration. Agree Instrument. September 2001. http://
3. Caviness AC, et al. Pediatr Infect Dis J. 2000;27:425-430. www.agreecollaboration.org/instrument/
7. Harbour R, et al. BMH. 2001;323:334-336.
8. Public Health Resource Unit. Critical Appraisal Skills Programme.
http://www.phru.nhs.uk/Pages/PHD/CASP.htm
November 2008 Downloaded
from http://aapgrandrounds.aappublications.org/ at University of Michigan on June 17, 2015 51
Clinical Practice Guidelines for Management of Encephalitis
AAP Grand Rounds 2008;20;50
DOI: 10.1542/gr.20-5-50
Updated Information & including high resolution figures, can be found at:
Services http://aapgrandrounds.aappublications.org/content/20/5/50
References This article cites 4 articles, 1 of which you can access for free at:
http://aapgrandrounds.aappublications.org/content/20/5/50#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the following
collection(s):
Critical Care
http://aapgrandrounds.aappublications.org/cgi/collection/critical_care_sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or in its
entirety can be found online at:
http://aapgrandrounds.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://aapgrandrounds.aappublications.org/site/misc/reprints.xhtml
Downloaded from http://aapgrandrounds.aappublications.org/ at University of Michigan on June 17, 2015
Clinical Practice Guidelines for Management of Encephalitis
AAP Grand Rounds 2008;20;50
DOI: 10.1542/gr.20-5-50
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://aapgrandrounds.aappublications.org/content/20/5/50
AAP Grand Rounds is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1999. AAP Grand Rounds is owned, published, and
trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove
Village, Illinois, 60007. Copyright © 2008 by the American Academy of Pediatrics. All rights reserved.
Print ISSN: 1099-6605.
Downloaded from http://aapgrandrounds.aappublications.org/ at University of Michigan on June 17, 2015
You might also like
- Case Study: Patient Presents With Influenza-Like IllnessDocument3 pagesCase Study: Patient Presents With Influenza-Like IllnessAlin DragosNo ratings yet
- Literature Review On Typhoid FeverDocument4 pagesLiterature Review On Typhoid Feverc5h4drzjNo ratings yet
- Case Study: PharyngitisDocument3 pagesCase Study: PharyngitisRestian Rony SaragiNo ratings yet
- 625-Article Text-3497-1-10-20200207Document6 pages625-Article Text-3497-1-10-20200207zeyla.riveros.29No ratings yet
- Serologic Diagnosis of Tuberculosis Using A Simple Commercial Multiantigen AssayDocument6 pagesSerologic Diagnosis of Tuberculosis Using A Simple Commercial Multiantigen AssayTanveerNo ratings yet
- 1 s2.0 S1526054219300235 MainDocument4 pages1 s2.0 S1526054219300235 MainBruno SantosNo ratings yet
- Can Tey 2015Document4 pagesCan Tey 2015irenesmbNo ratings yet
- Ciab 187Document4 pagesCiab 187Nguyễn Lê BằngNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofFransisca PekertiNo ratings yet
- Childhood Community Acquired Pneumonia A Review of Etiology and Antimicrobial Treatment Studies.Document10 pagesChildhood Community Acquired Pneumonia A Review of Etiology and Antimicrobial Treatment Studies.Andry Wahyudi AgusNo ratings yet
- Streptococcal PharyngitisDocument28 pagesStreptococcal PharyngitissylviaNo ratings yet
- Efficacy of Extract of Pelargonium Sidoides in Children With Acute Non-Group A Beta-Hemolytic Streptococcus Tonsillopharyngitis: A Randomized, Double-Blind, Placebo-Controlled TrialDocument11 pagesEfficacy of Extract of Pelargonium Sidoides in Children With Acute Non-Group A Beta-Hemolytic Streptococcus Tonsillopharyngitis: A Randomized, Double-Blind, Placebo-Controlled TrialInnoVision Health Media100% (1)
- Uso de TTPA para Diagnostico de SCDocument7 pagesUso de TTPA para Diagnostico de SCdrirrazabalNo ratings yet
- Detection of Typhoid CarriersDocument6 pagesDetection of Typhoid CarriersClarestaNo ratings yet
- Atorvastatin Improves Sputum Conversion and Chest X-Ray Severity ScoreDocument6 pagesAtorvastatin Improves Sputum Conversion and Chest X-Ray Severity Scorecharmainemargaret.parreno.medNo ratings yet
- A Multicenter Study Evaluating Ceftriaxone and Benzathine Penicillin G As Treatment Agents For Early Syphilis in Jiangsu, ChinaDocument6 pagesA Multicenter Study Evaluating Ceftriaxone and Benzathine Penicillin G As Treatment Agents For Early Syphilis in Jiangsu, ChinaSuryaNo ratings yet
- 2010 - Consensus Statement On Childhood TuberculosisDocument15 pages2010 - Consensus Statement On Childhood TuberculosisTammy Utami DewiNo ratings yet
- Entericfever 201810061138061823280Document4 pagesEntericfever 201810061138061823280Cindy HerwitiNo ratings yet
- Vih Actualizacion en OportunistasDocument18 pagesVih Actualizacion en Oportunistassamuro625No ratings yet
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesDocument11 pagesEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidNo ratings yet
- Tuberculosis Research Paper ExampleDocument4 pagesTuberculosis Research Paper Exampled1fytyt1man3100% (1)
- Jurnal PD Convert 2Document14 pagesJurnal PD Convert 2Anonymous G9gfz4No ratings yet
- Dxto de Infecciones en El SNCDocument17 pagesDxto de Infecciones en El SNCcarlos ballestasNo ratings yet
- Nej Mo A 1511812Document10 pagesNej Mo A 1511812anggiNo ratings yet
- Anti-NMDA Receptor Encephalitis and Nonencephalitic HSV-1 InfectionDocument6 pagesAnti-NMDA Receptor Encephalitis and Nonencephalitic HSV-1 Infectionmjbb1310No ratings yet
- CPG On CAPDocument29 pagesCPG On CAPAngeline Zamoras-ToledoNo ratings yet
- Jurnal DudiDocument15 pagesJurnal DudidudihadinegoroNo ratings yet
- Pneumonia Research PaperDocument5 pagesPneumonia Research Paperhbzqwpulg100% (1)
- JAH3 7 E010223Document22 pagesJAH3 7 E010223Dede MarizalNo ratings yet
- Pyrexia of Unknown Origin AfpDocument6 pagesPyrexia of Unknown Origin Afpabdul qayyumNo ratings yet
- PPT HiponatremiDocument9 pagesPPT HiponatremiArini NurlelaNo ratings yet
- Marais Criteria MTBDocument5 pagesMarais Criteria MTBAdhadi IsranurhaqNo ratings yet
- Ijpedi2021 1544553Document6 pagesIjpedi2021 1544553Naresh ReddyNo ratings yet
- Usefulness of Tumor Marker CA-125 Serum Levels For The Follow-Up of Therapeutic Responses in Tuberculosis Patients With and Without SerositisDocument6 pagesUsefulness of Tumor Marker CA-125 Serum Levels For The Follow-Up of Therapeutic Responses in Tuberculosis Patients With and Without Serositishumayun kabirNo ratings yet
- 394 Full PDFDocument20 pages394 Full PDFHaltiNo ratings yet
- Avances en Sepsis Art Ing 2022Document10 pagesAvances en Sepsis Art Ing 2022roman rodriguezNo ratings yet
- Targeted Therapies for Lung CancerFrom EverandTargeted Therapies for Lung CancerRavi SalgiaNo ratings yet
- Diagnostico y Tratamiento Sindrome Antifosfolipido PediatriaDocument7 pagesDiagnostico y Tratamiento Sindrome Antifosfolipido PediatriaJavier Muñoz MartínezNo ratings yet
- Sun 2012Document6 pagesSun 2012ntnquynhproNo ratings yet
- Research Paper On Herpes ZosterDocument6 pagesResearch Paper On Herpes Zosteryquyxsund100% (1)
- Asim,+prof +1726Document6 pagesAsim,+prof +1726Zayn HNo ratings yet
- Fernandez, John Michael BSN403 Group 10: I. Clinical QuestionDocument5 pagesFernandez, John Michael BSN403 Group 10: I. Clinical QuestionJohn Michael FernandezNo ratings yet
- ImunDocument2 pagesImunleli191No ratings yet
- Streptococcal PharyngitisDocument19 pagesStreptococcal PharyngitisBimasenaNo ratings yet
- Research Paper On PneumoniaDocument6 pagesResearch Paper On Pneumoniagz8bjzmj100% (1)
- Jvim 31 901Document6 pagesJvim 31 901Muhammad Imam NoorNo ratings yet
- 8.5 Case AnalysisDocument4 pages8.5 Case AnalysisMichal VillanuevaNo ratings yet
- Enteric Fever in Mumbai - Clinical Profile, Sensitivity Patterns and Response To AntimicrobialsDocument4 pagesEnteric Fever in Mumbai - Clinical Profile, Sensitivity Patterns and Response To AntimicrobialsHaidar HanifNo ratings yet
- ContentServer AspDocument2 pagesContentServer AspDarian EnmanuelNo ratings yet
- Bhat 2016Document6 pagesBhat 2016andrian dwiNo ratings yet
- Summaries of Evidence in Support of Proposed Recommendations FinalDocument25 pagesSummaries of Evidence in Support of Proposed Recommendations FinalodyNo ratings yet
- Journal of Medical Virology Volume 57 Issue 2 1999 (Doi 10.1002/ (Sici) 1096-9071 (199902) 57:2-193::aid-Jmv18-3.0.co 2-n) Foray, Sophie Pailloud, Fabienne Thouvenot, Dani Le FlorDocument5 pagesJournal of Medical Virology Volume 57 Issue 2 1999 (Doi 10.1002/ (Sici) 1096-9071 (199902) 57:2-193::aid-Jmv18-3.0.co 2-n) Foray, Sophie Pailloud, Fabienne Thouvenot, Dani Le FlorKhupe KafundaNo ratings yet
- Al-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Document6 pagesAl-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Vincentius Michael WilliantoNo ratings yet
- 10 1016@j Ijid 2016 08 020Document2 pages10 1016@j Ijid 2016 08 020Karen BecerraNo ratings yet
- Atypical MeaslesDocument2 pagesAtypical MeaslesBagusPranataNo ratings yet
- Inappropriate Antibiotic Prescribing: A Cross-Sectional Study in SwazilandDocument6 pagesInappropriate Antibiotic Prescribing: A Cross-Sectional Study in Swazilandditof58671No ratings yet
- Gene Therapy Clinical Trials Worldwide To 2017 An UpdateDocument16 pagesGene Therapy Clinical Trials Worldwide To 2017 An UpdateLeonardo Sandi SalazarNo ratings yet
- TuberculosisDocument5 pagesTuberculosislittlecandiesNo ratings yet
- PCR Based Dagnostics Improve Outcome in Septic PtsDocument9 pagesPCR Based Dagnostics Improve Outcome in Septic Ptsfaraz.mirza1No ratings yet
- Research Paper PneumoniaDocument7 pagesResearch Paper Pneumoniawkzcoprhf100% (1)
- Jakarta Declaration PPDocument17 pagesJakarta Declaration PPvashniNo ratings yet
- (Ebook) SuperBrain Yoga by Master Choa Kok Sui PDFDocument81 pages(Ebook) SuperBrain Yoga by Master Choa Kok Sui PDFBoonyarit Huang100% (5)
- The Peat WhispererDocument85 pagesThe Peat Whispererzarrin77100% (6)
- My Family Health Portrait-DiagramDocument3 pagesMy Family Health Portrait-DiagramTaj BoydNo ratings yet
- Hba1C: Quality System CertifiedDocument4 pagesHba1C: Quality System CertifiedNonameNo ratings yet
- 1cambrigton Dave Ielts Reading 100 9 PointsDocument43 pages1cambrigton Dave Ielts Reading 100 9 PointsWit FksunNo ratings yet
- Local Anaesthetics Mcqs From LouisDocument6 pagesLocal Anaesthetics Mcqs From LouisAmreen Khan100% (1)
- Common Skin Diseases in Africa: An Illustrated GuideDocument85 pagesCommon Skin Diseases in Africa: An Illustrated GuideJohn EnioladeNo ratings yet
- List of CosmeticsDocument9 pagesList of Cosmeticsasit_m0% (1)
- Health Services in Developing CountriesDocument11 pagesHealth Services in Developing CountriesKailash NagarNo ratings yet
- Curriculum Vitae - Aditya Pratama PutraDocument3 pagesCurriculum Vitae - Aditya Pratama PutraIan SeptiantoNo ratings yet
- Moth Balls: Safety Data SheetDocument9 pagesMoth Balls: Safety Data SheethafilrediandikaNo ratings yet
- Hyoscine ButylbromideDocument2 pagesHyoscine ButylbromideKenneth ColeNo ratings yet
- UJA-Federation of New York Donor Recognition List 2022Document17 pagesUJA-Federation of New York Donor Recognition List 2022ericlkaplanNo ratings yet
- Winter Safety Toolbox TalkDocument18 pagesWinter Safety Toolbox TalkKristina100% (1)
- Science3 Q1 W4 Proper Use HandlingDocument50 pagesScience3 Q1 W4 Proper Use HandlingGina Contalba TubeoNo ratings yet
- Approach To The Patient in Shock: by James Holencik, DODocument52 pagesApproach To The Patient in Shock: by James Holencik, DOLydia MamurNo ratings yet
- Isu Dan Etika Pada Perawatan Paliatif PDFDocument17 pagesIsu Dan Etika Pada Perawatan Paliatif PDFNatasya ChieCaem FunforeverNo ratings yet
- Telescopic Handler Student ManualDocument41 pagesTelescopic Handler Student ManualingcalderonNo ratings yet
- Ims 1 10 18Document2 pagesIms 1 10 18Katherine UrregoNo ratings yet
- Xcelera Brochure Updated (English)Document24 pagesXcelera Brochure Updated (English)Pablo Rosas100% (1)
- Lesson Plan-Pregnant WomenDocument5 pagesLesson Plan-Pregnant Womenapi-270972965No ratings yet
- ECGforinternsDocument25 pagesECGforinternsusmleusmle86No ratings yet
- Chevron Thailand Employee and Contractor Handbook EngDocument200 pagesChevron Thailand Employee and Contractor Handbook EngAndré Lima100% (1)
- Power2 340-H44: Operation ManualDocument166 pagesPower2 340-H44: Operation ManualDmitrii PustoshkinNo ratings yet
- Budget of Works in Grade 7 Health: S.Y. 2019 - 2020 Quarter Topics Objectives Activites No. of HoursDocument1 pageBudget of Works in Grade 7 Health: S.Y. 2019 - 2020 Quarter Topics Objectives Activites No. of HoursRichard MarquezNo ratings yet
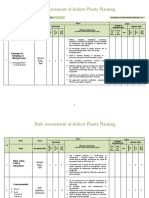
- Risk Assessment of Indoor Plants PlantingDocument5 pagesRisk Assessment of Indoor Plants Plantingطارق رضوانNo ratings yet
- Notes On Critical Areas in Labor Law Part IiDocument66 pagesNotes On Critical Areas in Labor Law Part IipaulNo ratings yet
- Policy That Implemented in Kota SamarahanDocument9 pagesPolicy That Implemented in Kota SamarahanIskandar IskandarNo ratings yet
- PERDEV DLL Unit 1 - M3 (Developmental Stages Handout)Document4 pagesPERDEV DLL Unit 1 - M3 (Developmental Stages Handout)Leonila MirandaNo ratings yet