Professional Documents
Culture Documents
Primary Hyperparathyroidism, Nature
Primary Hyperparathyroidism, Nature
Uploaded by
Juanita GonzálezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Primary Hyperparathyroidism, Nature
Primary Hyperparathyroidism, Nature
Uploaded by
Juanita GonzálezCopyright:
Available Formats
REVIEWS
Primary hyperparathyroidism
Marcella D. Walker and Shonni J. Silverberg
Abstract | In this Review, we describe the pathogenesis, diagnosis and management of primary
hyperparathyroidism (PHPT), with a focus on recent advances in the field. PHPT is a common
endocrine disorder that is characterized by hypercalcaemia and elevated or inappropriately
normal serum levels of parathyroid hormone. Most often, the presentation of PHPT is
asymptomatic in regions of the world where serum levels of calcium are routinely measured. In
addition to mild hypercalcaemia, PHPT can manifest with osteoporosis and hypercalciuria as well
as with vertebral fractures and nephrolithiasis, both of which can be asymptomatic. Other clinical
forms of PHPT, such as classical disease and normocalcaemic PHPT, are less common.
Parathyroidectomy, the only curative treatment for PHPT, is recommended in patients with
symptoms and those with asymptomatic disease who are at risk of progression or have subclinical
evidence of end-organ sequelae. Parathyroidectomy results in an increase in BMD and a
reduction in nephrolithiasis. Various medical therapies can increase BMD or reduce serum levels
of calcium, but no single drug can do both. More data are needed regarding the
neuropsychological manifestations of PHPT and the pathogenetic mechanisms leading to
sporadic PHPT, as well as on risk factors for complications of the disorder. Future work that
advances our knowledge in these areas will improve the management of the disorder.
Primary hyperparathyroidism (PHPT) was first described Before the routine measurement of serum levels of cal-
approximately 90 years ago, almost simultaneously in cium in the 1970s, PHPT was a rare and symptomatic dis-
Europe and the USA1. Since that time, the clinical pres- order. When routine evaluation of serum levels of calcium
entation in the USA and Western Europe has evolved became widespread, cases of unrecognized, asympto-
from a severe and symptomatic disease, characterized matic PHPT were identified, leading to an initial fivefold
by ‘stones, bones and groans’ to one that is typically increase in the incidence of the disorder 5. Thereafter, the
asymptomatic and incidentally discovered. Advances in incidence of PHPT declined in the USA until 1998, at
diagnostics now enable us to accurately measure levels of which time another sharp increase was noted3,6,7, which
parathyroid hormone (PTH) and image the parathyroid has been attributed to the introduction of osteoporosis
glands; surgical techniques have also improved. Despite screening guidelines and targeted testing in those with
these advances and the availability of medical therapies osteoporosis7. The incidence of PHPT increases with age
that address some of the complications of the disease, and is higher in women and African Americans than
parathyroidectomy remains the only curative treatment, in men and other racial groups, respectively 2. Half of
as was the case 90 years ago. This Review describes the all patients with PHPT are postmenopausal women,
pathogenesis, diagnosis and management of PHPT, with although the disorder can occur at any age8. PHPT is
a focus on recent advances in the field. often diagnosed in the first decade after menopause, con-
sistent with the known skeletal actions of oestrogen that
Epidemiology and pathogenesis counter the hypercalcaemic effects of excess PTH in bone.
Division of Endocrinology, PHPT is a common endocrine disorder that is charac- The underlying cause of sporadic PHPT is unknown
Department of Medicine, terized by hypercalcaemia and elevated or inappropri- in most cases. Ionizing radiation, especially in childhood,
Columbia University, College
ately normal levels of PTH. PHPT results from excessive is a risk factor 9. Chronic lithium use, which decreases the
of Physicians and Surgeons,
New York, New York 10032, secretion of PTH from one or more of the parathyroid sensitivity of the parathyroid glands to calcium, is also
USA. glands. PHPT is caused by a solitary parathyroid ade- associated with the development of PHPT10. The genetic
Correspondence to S.J.S. noma in 80% of cases, whereas four-gland hyperplasia pathogenesis of PHPT is unclear in most patients. Genes
sjs5@cumc.columbia.edu accounts for 10–15%, multiple adenomas for 5% and par- regulating the cell cycle are thought to be important
doi:10.1038/nrendo.2017.104 athyroid cancer for <1% of cases. Incidence estimates for given the clonal nature of sporadic parathyroid ade-
Published online 8 Sep 2017 PHPT vary from ~0.4 to 82 cases per 100,000 (REFS 2–4). nomas. Two such genes documented as contributing to
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 115
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Key points On repeat laboratory testing, serum levels of calcium
can intermittently fall into the normal range; this find-
• Primary hyperparathyroidism (PHPT), a common endocrine disorder characterized ing is compatible with the diagnosis of PHPT as long as
by hypercalcaemia and elevated or inappropriately normal levels of parathyroid a ‘recurrent pattern’ of hypercalcaemia is evident. Levels
hormone, is diagnosed based upon biochemical evaluation of PTH that are inappropriately normal (>20 pg/ml) in a
• Over the past 50 years, the clinical profile of PHPT has evolved from a highly patient with hypercalcaemia are consistent with a diagno-
symptomatic disease to one that is most often asymptomatic, albeit with evidence sis of PHPT. Non-parathyroid causes of hypercalcaemia
of subclinical target organ involvement
(such as malignancy or granulomatous disease) are
• Even ‘asymptomatic’ patients can have skeletal deterioration (evident upon imaging; associated with suppressed levels of PTH. Ectopic PTH
for example, dual-energy X‑ray absorptiometry), and subclinical manifestations can
secretion from a non-parathyroid tumour is extremely
include osteoporosis and hypercalciuria as well as clinically silent vertebral fractures
and nephrolithiasis
rare although occasionally documented in late-stage
malignancies21,22.
• The diagnosis of normocalcaemic PHPT can be made after eliminating secondary
causes of hyperparathyroidism; however, data are limited on its natural history and
When assessing for PHPT, PTH levels should be meas-
appropriate criteria for and response to surgery ured with either an ‘intact’ second-generation PTH assay
• Parathyroidectomy by an experienced parathyroid surgeon is recommended for
or a third-generation assay. Second-generation assays
patients with symptomatic disease or subclinical end-organ involvement, as no single detect PTH(1–84), PTH(7–84) and other long C‑terminal
medical therapy addresses hypercalcaemia and the skeletal and renal consequences fragments, which are inactive fragments and/or are
of PHPT thought to oppose the activity of intact PTH. Unless renal
failure is present, the contribution of fragments to the
measured PTH value is negligible. The intact assays do
the development of PHPT are CCND1 (which encodes not cross-react with PTH-related peptide and can reli-
cyclin D1) and MEN1 (which encodes menin). Somatic ably distinguish PHPT from hypercalcaemia of malig-
mutations in MEN1 occur in 12–35% of sporadic ade- nancy, in contrast to first-generation assays. The newer
nomas, whereas rearrangement or overexpression of third-generation PTH assays detect the main circulating
CCND1 can occur in 20–40%11,12. Recent studies have also form of whole PTH(1–84) and a second PTH(1–84)
implicated CDC73, CTNNB1, CDKN1B and AIP (which molecule not detected by second-generation assays that
encodes the aryl hydrocarbon (AH) receptor-interacting is thought to have a post-translational modification23.
protein) in a small percentage of adenomas13,14. Other than in renal failure, these assays do not increase
In inherited or familial forms of PHPT, which repre- the diagnostic sensitivity over second-generation assays24.
sent about 5–10% of cases, germline mutations in several Parathyroid imaging has no role in the diagnosis of
causal genes have been identified15,16. The clinical fea- PHPT. Imaging studies assist the parathyroid surgeon in
tures, gene products and inheritance of familial forms identifying the anatomic position of abnormal gland(s)
of PHPT are shown in TABLE 1. The following genes have when planning parathyroidectomy. Negative imaging,
been associated with familial PHPT: the tumour sup- which is frequent in multi-glandular PHPT, is not incon-
pressor MEN1 in multiple endocrine neoplasia type 1 sistent with the diagnosis of PHPT and does not preclude
syndrome and familial isolated primary hyperparathy- surgical cure25. Further, positive imaging is not needed
roidism (FIHP); the proto-oncogene RET in MEN 2A to confirm the diagnosis, and false-positive tests occur
syndrome; CDKN1B in MEN 4 syndrome; inactivating often in those with concurrent nodular thyroid disease.
mutations in CASR (which encodes the calcium-sensing To differentiate PHPT from FHH, which has a similar
receptor) in FIHP; GCM2 in FIHP17 and CDC73 in serum biochemical profile, calculation of the fractional
hyperparathyroidism–jaw tumour syndrome, which is excretion of calcium (FeCa; calculated using a 24‑hour
also associated with an increased risk of parathyroid urine sample collected off diuretics) has traditionally
carcinoma. Mutations in PRUNE2 (which encodes been used. Values below 1% are consistent with FHH,
protein prune homologue 2) have also been associated but overlap of FeCa values in FHH and PHPT occurs.
with the development of parathyroid cancer 18. Other As FeCa values can also be low in patients with PHPT
work indicates that microRNA 296 might be a novel who have coexisting vitamin D deficiency, the diagno-
tumour-suppressor gene in parathyroid carcinoma19. sis of FHH should not be made until vitamin D stores
The genetics and characteristics of familial hypocalciuric are replete. FeCa can also be misleading in patients with
hypercalcaemia (FHH), which is not considered a form impaired renal function (due to advanced age or renal
of PHPT, are discussed in the following section. disease). In these patients, obtaining past serum calcium
levels (which should be consistently elevated) and fam-
Pathophysiology and (differential) diagnosis ily history of hypercalcaemia is helpful. Ultimately, if
In all forms of PHPT, there is loss of normal feedback suspicion of FHH is high, mutational analysis of CASR
suppression of serum levels of calcium upon the synthe- for FHH1, as well as mutational analysis of GNA11 and
sis and secretion of PTH, due to increased parathyroid AP2S1 for the diagnosis of FHH2 and FHH3, respec-
cell mass and/or a reduction in the number of CASR tively, can be performed26–28. Differentiation of PHPT
proteins on parathyroid cells20. As a result, increased from FHH is important, as surgical intervention is not
levels of calcium are needed to suppress PTH levels indicated or curative in FHH.
(FIG. 1). The diagnosis of PHPT is established biochem- PHPT can be distinguished from secondary and
ically and can be confirmed by documenting hypercal- tertiary hyperparathyroidism by its different biochem-
caemia with a simultaneously elevated intact PTH level. ical profile (TABLE 2). Secondary hyperparathyroidism
116 | FEBRUARY 2018 | VOLUME 14 www.nature.com/nrendo
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 | Inherited forms of PHPT16,17
Familial syndrome Clinical manifestations Gene (protein) Inheritance
MEN 1 PHPT (95%), anterior pituitary adenomas (30%), pancreatic MEN1 (menin) Autosomal
neuroendocrine tumours (40%); other features can include adrenal dominant
adenomas, carcinoid, lipomas, angiofibromas and collagenomas
MEN 2A Medullary thyroid cancer (90%), pheochromocytoma (50%), PHPT (20%) RET (proto-oncogene c-Ret) Autosomal
dominant
MEN 4 PHPT (~80%), anterior pituitary tumours (~40%), pancreatic CDKN1B (p27) Autosomal
neuroendocrine tumours; other features can include carcinoid, dominant
adrenocorticoid tumours, thyroid tumours, reproductive organ
tumours and renal angiomyolipomas
FIHP Isolated PHPT • MEN1 (menin) Autosomal
• CASR (CASR) dominant
• GCM2 (GCM motif protein 2,
also known as hGCMb)
Hyperparathyroid– PHPT (80%), often parathyroid carcinoma (>15%), jaw tumours (>30%); CDC73 (also known as HRPT2; Autosomal
jaw tumour syndrome other features can include renal abnormalities, uterine tumours, parafibromin) dominant
pancreatic adenocarcinoma, testicular mixed germ cells and Hürthle
cell thyroid adenomas
FIHP, familial isolated primary hyperparathyroidism; MEN, multiple endocrine neoplasia; PHPT, primary hyperparathyroidism.
is associated with an appropriate elevation in PTH to a symptomatic, multi-system disorder characterized
in response to a hypocalcaemic stimulus and either a by skeletal, renal, gastrointestinal, neurological and psy-
frankly low or normal serum calcium level. Most com- chiatric manifestations as well as increased mortality 1.
monly, secondary hyperparathyroidism is due to vita- Descriptions of PHPT from the early to mid‑20th cen-
min D deficiency, malabsorption, kidney disease or tury include marked hypercalcaemia (11.5–16.8 mg/dl)
hypercalciuria. In our experience, a subset of patients and frequent reports of osteitis fibrosa cystica, a skele-
with secondary hyperparathyroidism will become tal condition characterized clinically by bone pain and
hypercalcaemic and will ultimately be found to have fractures (particularly vertebral) and radiographically
PHPT, when the underlying condition (for example, by demineralization, fibrosis, brown tumours and bone
vitamin D deficiency) is corrected. In these cases, the cysts1,30. Nephrolithiasis, nephrocalcinosis, polyuria
hypercalcaemia of PHPT is said to have been ‘masked’ and polydipsia as well as renal impairment were also
by the coexisting hypocalcaemic stimulus. Tertiary common presenting signs and symptoms1,30; other fea-
hyperparathyroidism describes a condition in which tures of classical PHPT include anorexia, constipation,
prolonged, severe secondary hyperparathyroidism (as in peptic ulcer disease and pancreatitis, muscle weakness
end-stage renal disease) evolves into a hypercalcaemic and associated type 2 muscle fibre atrophy, and mental
state due to autonomous functioning of hyperplastic disturbances as well as fatigue or lasstitude1,30.
parathyroid glands. Although this effect can be observed Classical PHPT is uncommon today in the USA,
in patients on dialysis, it can also occur after renal trans- Western Europe and Turkey 8,31,32. In the USA, <2% of
plant. Tertiary hyperparathyroidism is typically obvious patients have osteitis fibrosa cystica, and rates of overt
from the history of the patient. nephrolithiasis have steadily declined over the past
In distinction, normocalcaemic primary hyperpara 70 years from 60% to <20%1,8,33. Classical PHPT, however,
thyroidism (NPHPT) is a term used for those patients remains the predominant mode of presentation in most
with normal serum albumin-corrected calcium levels of the Middle East, Asia and South Africa34–38. In Latin
and ionized calcium values with an elevated PTH level America, a 2015 report indicated that >50% of patients
in whom all known causes of secondary hyperpara present with osteitis fibrosa cystica or nephrolithiasis39;
thyroidism have been excluded. NPHPT was thought other reports confirmed high rates of nephrolithia-
to be an early form of PHPT. Although data regarding sis (>40%)40,41. This more severe form of the disease is
the natural history of NPHPT are limited, a 2007 study thought to be more common in areas where severe vita-
found that ~19% became hypercalcaemic within 3 years min D deficiency is endemic, although lack of routine
of follow-up29. Thus, the term NPHPT can describe calcium screening in these regions might also have a role
more than one natural history, with some patients in this presentation.
maintaining the biochemical pattern of NPHPT over
many years and perhaps even indefinitely. Asymptomatic PHPT
Today, the vast majority (>80%) of patients with PHPT
Clinical manifestations and complications in the USA and Western Europe are ‘asymptomatic’,
Classical PHPT a term used to describe those lacking the skeletal and
Classical PHPT was the disease presentation almost renal manifestations described in classical PHPT.
exclusively observed before the routine measurement of Although this term was introduced in the 1970s and
serum calcium levels in the 1970s. Classical PHPT refers 1980s to differentiate it from classical PHPT, over the
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 117
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
in the latter cohort. Further, many cross-s ectional
100 Normal PHPT
studies have suggested an inverse correlation between
PTH, % of maximal secretion
serum levels of 25OHD and PTH, which indicates that
low vitamin D levels might heighten PTH elevations
in PHPT43,44,47–51. Additional evidence of worse hyper-
parathyroidism in those with vitamin D deficiency is
50 reflected in increased serum levels of calcium, reduced
levels of phosphate and increased 1,25(OH)2D levels as
well as increased alkaline phosphatase levels, in some
but not all studies42,43,48,49,51–57. Vitamin D treatment in
PHPT is also associated with a lowering of PTH levels
0 in observational studies and randomized controlled tri-
Calcium
als (RCTs)58,59. Thus, vitamin D deficiency, particularly
Nature Reviews | Endocrinology when marked and prolonged, might be a risk factor for
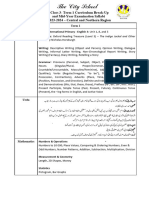
Figure 1 | Relationship between serum levels of calcium
and PTH. Depicted is the relationship between serum more biochemically severe PHPT.
levels of calcium and PTH in patients with primary hyper-
parathyroidism (PHPT; red line) and normal individuals Skeletal manifestations. Although osteitis fibrosa cyst-
(blue line). PHPT results in a shift of the curve to the right. ica is rare, ample evidence exists for subclinical bone
Increased levels of calcium are needed to suppress PTH disease in PHPT. Dual-energy X‑ray absorptiometry
levels in PHPT.
(DXA) demonstrates preferential loss of BMD at cor-
tical sites such as the distal one-third of the forearm,
years, we have come to realize that many patients with whereas cancellous sites such as the lumbar spine are rel-
this form of the disease do indeed have manifestations atively spared60. This pattern reflects the catabolic versus
of PHPT. Many have clinical complaints, whereas oth- anabolic effects of PTH on different skeletal compart-
ers have characteristic findings on testing of the target ments61. Iliac crest bone biopsy studies show a similar
organs of the hyperparathyroid process. pattern with a reduction in cortical thickness but more
favourable or similar trabecular indices in patients with
Biochemical profile. Most patients with PHPT are inci- PHPT versus controls61.
dentally discovered when routine laboratory work reveals Estimates of the prevalence of osteoporosis in PHPT
hypercalcaemia. Serum levels of calcium are mildly ele- have varied in recent studies (39–62.9%)50,51,62, likely influ-
vated, often within 1 mg/dl of the upper limit of normal8. enced by bias as a diagnosis of osteoporosis might have led
PTH levels are typically within two times the upper limit to screening for PHPT. Mean T‑scores in most studies are
of normal. Serum phosphate is often in the lower half of in the osteopenic range50,51. Risk factors for osteoporosis in
the normal range and less frequently frankly low due to the PHPT, as in the general population, include older age and
phosphaturic effects of PTH8. Alkaline phosphatase levels lower weight62. In contrast, vitamin D deficiency seems to
can be elevated, a reflection of increased bone resorp- have minimal effect on BMD, with only slightly reduced
tion and compensatory formation, but most often remain BMD at the one-third radius in those with low vitamin D
within the normal range8. levels; vitamin D repletion, however, might improve
The storage form of vitamin D, 25‑hydroxyvitamin D BMD, particularly at the spine50,51,59.
(25OHD), is often in the insufficient (20–29 ng/ml) or Given the BMD patterns observed with DXA, one
deficient range (<20 ng/ml), whereas activated vita- would anticipate an increased risk of peripheral fractures
min D (1,25‑dihydroxyvitamin D; 1,25(OH)2D) is near but a reduction in vertebral fractures in modern PHPT.
the upper end of normal and sometimes frankly ele- Epidemiological data, however, suggest an increased risk
vated8,42. In fact, vitamin D deficiency has been reported of both vertebral and peripheral fractures63–66. The para-
to be more common in patients with PHPT than in the dox of increased vertebral fracture risk despite preserved
general population43,44. Potential pathophysiological lumbar spine BMD in PHPT has remained unclear until
mechanisms for vitamin D deficiency in PHPT include recently. New technologies for non-invasively imaging
the following: PTH enhances the conversion of 25OHD the skeletal microarchitecture, such as high-resolution
to 1,25(OH)2D by inducing the renal 1α‑hydroxylase peripheral quantitative CT (HRpQCT) and the tra-
enzyme45, the half-life of 25OHD might also be shortened becular bone score (TBS), demonstrate that trabecular
due to enhanced hepatic inactivation46, and chronic vita- deterioration occurs at the spine as well as the radius
min D deficiency could result in parathyroid hyperplasia and tibia67–69 (FIG. 2). Deteriorated microarchitecture has
and autonomous adenomatous change. not yet been shown to be a risk factor for fracture in
Whereas the biochemical profile in modern PHPT PHPT, but studies have implicated traditional risk fac-
is clearly milder than in descriptions from the early and tors such as older age, lower BMD and vitamin D levels,
mid‑20th century, recent work suggests even further higher levels of bone turnover markers and higher PTH
evolution within the modern era42. A comparison of levels62,70. Recent work suggesting that clinically silent
two PHPT cohorts recruited in the same region of the vertebral fractures are a common feature of PHPT led
USA 20 years apart (1984–1991 and 2010–2014) revealed experts in the 2014 guidelines for the management of
increased mean serum levels of 25OHD and decreased asymptomatic PHPT to recommend screening for ver-
PTH levels due to self-supplementation with vitamin D tebral fractures and parathyroidectomy if present 62,71.
118 | FEBRUARY 2018 | VOLUME 14 www.nature.com/nrendo
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 2 | Biochemical features of various forms of hyperparathyroidism and FHH
Form of hyperparathyroidism Calcium levels PTH levels Phosphate levels Urinary calcium excretion
Primary hyperparathyroidism Increased Increased or Low or low–normal FeCA typically >1–2%
inappropriately normal
Secondary hyperparathyroidism Normal or low Increased Dependent on cause; low or Dependent on cause; low
low–normal in vitamin D in vitamin D deficiency or
deficiency or malabsorption; high malabsorption; high in renal
or high–normal in renal failure calcium leak
Tertiary hyperparathyroidism Increased Increased Variable; dependent on before or Low before renal transplant
after renal transplant
Normocalcaemic primary Normal (total & Increased Normal <350 mg per 24 h29
hyperparathyroidism ionized)
FHH Increased Increased or Normal FeCa typically <1%
inappropriately normal; the
majority have normal PTH
FeCa, fractional excretion of calcium; FHH, familial hypocalciuric hypercalcaemia; PTH, parathyroid hormone
This recommendation is supported by recent RCT data PHPT as well as the exact mechanisms underlying them
that suggest parathyroidectomy might reduce the risk of is unclear. The muscle weakness and atrophy observed in
vertebral fractures compared with observation72. classical PHPT are not seen today. A number of studies
suggest, however, that even ‘mild PHPT’ (serum calcium
Renal manifestations. Today, the main renal manifes- <12 mg/dl) is associated with nonspecific symptoms such
tations of PHPT are hypercalciuria and nephrolithia- as depression, anxiety, fatigue, decreased quality of life
sis73. Symptomatic nephrolithiasis is present in about (QoL), sleep disturbance and cognitive dysfunction.
10–20% of patients8,73. Screening for asymptomatic Many, but not all, observational studies have indicated
nephrolithiasis, as recommended by the most recent these features improve after parathyroidectomy 87. Three
(2014) guidelines for the management of asymptomatic RCTs have investigated the reversibility of reduced QoL
PHPT, indicates that the prevalence is actually much and psychiatric symptoms82,83,88. Despite being of similar
higher 62,71,73,74. Risk factors for nephrolithiasis include design and using similar assessment tools, all three RCTs
younger age and male sex, whereas degree of hyper came to different conclusions: one RCT suggested para
calcaemia and hypercalciuria, PTH levels and other uri- thyroidectomy prevents worsening of QoL and improves
nary factors have shown less consistent associations73–76. psychiatric symptoms88, another RCT indicated no ben-
Limited data are available regarding nephrocalcinosis, efit and the third RCT demonstrated improvement in
but it seems to be an uncommon feature of modern QoL82,83. One RCT investigated changes in cognition after
PHPT, as are polyuria and polydipsia73. The prevalence parathyroidectomy, but its small size precluded defini-
of renal dysfunction (estimated glomerular filtration rate tive conclusions being drawn89. At present, most experts
(eGFR) <60 ml/min) is low, with recent studies suggest- do not recognize cognitive or psychiatric symptoms as a
ing rates of 15–17%77–79. Neither the severity of PHPT sole indication for parathyroidectomy. Reasons for this
nor having a history of nephrolithiasis was a risk factor include the failure to clearly demonstrate reversibility
for reduced eGFR in a 2014 study; instead, traditional in RCTs, the inability to predict which patients might
risk factors, such as age, hypertension, use of antihyper- improve and the lack of a clear mechanism71.
tensive medication and fasting glucose levels, were asso-
ciated with poorer kidney function78. Longitudinal data Cardiovascular manifestations. Increased cardiovascu-
are reassuring in this regard, as renal function remains lar mortality in patients with moderate to severe PHPT
stable in PHPT over long periods of follow-up8,80. Further, has been documented in studies from Scandinavia90.
parathyroidectomy has not been shown to improve Data on those with asymptomatic PHPT are limited,
renal function, although one small study suggested an but several studies suggest no increase in mortality in
improvement in concentrating capacity 8,80–83. those with mild hypercalcaemia91,92. Hypertension has
long been associated with PHPT but is not reversible
Neuropsychological features. Increased serum calcium with parathyroidectomy 90. Recent studies have inves-
and PTH concentrations, the biochemical hallmarks tigated subclinical cardiovascular findings in PHPT,
of PHPT, could affect neuropsychological function. including asymptomatic coronary artery disease (CAD),
Calcium has a key role in regulating the release of neuro valve calcification, left ventricular hypertrophy (LVH),
transmitters at synapses, and hypercalcaemia could carotid disease and vascular stiffness. When CAD is
interfere with that process. On the other hand, the present in PHPT, it is most likely due to traditional
long-known vascular effects of PTH could also affect risk factors rather than the disease itself 93–95. Valve cal-
cognition and mood by altering cerebrovascular func- cification, which is present in severe PHPT, has been
tion84–86. Descriptions of classical PHPT do indeed indi- shown to be more extensive (greater valve area) when
cate neuropsychological features1,30. The extent to which present in those with mild PHPT than in controls96–98
these features remain a part of the modern picture of and is associated with increased PTH levels, but it is
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 119
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
PHPT Control calcium levels (within the normal range) and higher uri-
nary calcium excretion as well as older age are reported
to be risk factors for the development of hypercalcaemia
in some studies29,113.
Skeletal, renal and other manifestations. Although the
clinical manifestations of NPHPT would be anticipated
to be milder than those of hypercalcaemic PHPT, most
case series suggest this is not the case, with high rates of
osteoporosis, fractures and kidney stones29,114,115. This
difference is likely due to selection bias, as NPHPT is
often diagnosed after a clinical event such as a fracture
or nephrolithiasis. Data from community cohorts sug-
Nature Reviews | Endocrinology gest no differences in BMD between those with NPHPT
Figure 2 | Trabecular deterioration in PHPT. High-resolution peripheral quantitative CT
images of the radius in a patient with primary hyperparathyroidism (PHPT; left) and a and those with normal PTH levels, although more data
normal control (right). Trabecular deterioration is evident in PHPT. Reproduced with are needed111. Almost no data exist regarding non-clas-
permission from REF. 67, John Wiley and Sons. sical manifestations (such as neuropsychological and
cardiovascular manifestations) in NPHPT.
not reversible with parathyroidectomy 98. LVH has been Evaluation and management
associated with PHPT in many, but not all, studies90. A Surgery
2015 meta-analysis indicated that parathyroidectomy Parathyroidectomy remains the only cure for PHPT
is associated with a decline in left ventricular mass and and is recommended in all symptomatic patients. The
that higher levels of PTH predict a greater cardiovascu- Fourth International Workshop for the Management of
lar benefit; however, dissociating disease severity from Asymptomatic PHPT recommended surgical intervention
study design (RCTs included individuals with lower lev- in patients with asymptomatic PHPT in whom evidence of
els of calcium and PTH than those included in observa- subclinical end-organ (skeletal or renal) effects or risk
tional studies) was not possible99. Conflicting data exist of disease progression exists71 (TABLE 3). This recommen-
regarding whether intima–media thickness is increased dation includes those with serum calcium ≥1 mg/dl above
in PHPT86,100–103. Multiple studies have reported increased the upper limit of normal; those with osteoporosis (T‑score
vascular stiffness, sometimes associated with PTH levels, ≤-2.5) or vertebral fractures on imaging; those with
in mild PHPT, but its reversibility with parathyroidec- eGFR <60 ml/min, severe hypercalciuria (>400 mg/day),
tomy is inconsistent86,104–106. Given conflicting data, most increased risk of stones on a stone risk profile or evidence
experts do not consider cardiovascular disease to be an of occult nephrolithiasis or nephrocalcinosis on imag-
indication for parathyroidectomy 71. ing; and those aged <50 years. Although evidence-based
recommendations are lacking in NPHPT, surgery is sug-
Other manifestations. Gastrointestinal symptoms, such gested if patients become hypercalcaemic and have other
as pancreatitis and peptic ulcer disease, do not seem to indications for parathyroidectomy and should be consid-
be a feature of modern PHPT, although conflicting data ered in those who have disease progression regardless of
exist concerning an association of PHPT with constipa- hypercalcaemia (that is, worsening of BMD, fracture or
tion107,108. Patients with coeliac disease are at increased risk kidney stones)71.
of developing PHPT, possibly due to chronic vitamin D Surgical guidelines from other societies are more lib-
deficiency 109. eral than those of the Fourth International Workshop
for the Management of Asymptomatic PHPT25. The
Normocalcaemic PHPT American Association of Endocrine Surgeons Guidelines
Biochemical profile. Both the Third and Fourth additionally recommend surgery in those with cognitive
International Guidelines for the Management of or psychiatric symptoms attributable to PHPT, suggest
Asymptomatic PHPT recognized NPHPT as a phenotype offering parathyroidectomy to those with cardiovascular
of PHPT24,31,110. NPHPT has a prevalence of 0.4–3.1% disease (other than hypertension) and consider symp-
in community-based cohorts 111. Although calcium toms of muscle weakness, impaired functional capac-
levels are normal in this entity, PTH levels are similar ity and abnormal sleep patterns. Patient preference has
or slightly lower than in the hypercalcaemic form of an important role in decision-making; surgery is never
PHPT29,112. Phosphate levels have been reported to be inappropriate even in those who do not meet surgical
higher and 1,25(OH)2D levels lower than in the hyper- criteria, as long as the diagnosis is secure. Finally, access
calcaemic variant 112. By definition, ionized calcium, to an experienced parathyroid surgeon has a role in the
vitamin D levels, urinary calcium excretion and renal decision, as data suggest that surgeon volume inversely
function must be normal to distinguish this entity from correlates with complications, cost and length of stay
secondary hyperparathyroidism29. NPHPT can precede in hospital116,117.
the development of typical hypercalcaemic PHPT, but Preoperative localization is necessary if a minimally
patient series have suggested only 0.6–19% of patients invasive parathyroidectomy (MIP) is contemplated25.
go on to develop hypercalcaemia29,111,113. Higher serum Imaging accuracy has improved vastly, but there remains
120 | FEBRUARY 2018 | VOLUME 14 www.nature.com/nrendo
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 3 | Evaluation and indications for surgery in asymptomatic PHPT
Measure Criteria for surgery at initial Schedule for follow‑up Criteria for surgery at
evaluation evaluation follow up
Age <50 years NA <50 years
Serum level of calcium ≥1 mg/dl above upper limit Yearly ≥1 mg/dl above upper limit
eGFR <60 ml/min Yearly Reduction in eGFR <60 ml/min
24 h urinary calcium level >400 mg per day Repeat if kidney stone suspected >400 mg per day
Biochemical stone profile Increased risk Repeat if kidney stone suspected Increased risk
Renal imaging Presence of nephrolithiasis or Repeat if kidney stone suspected Development of kidney stone
nephrocalcinosis
DXA (spine, hip and forearm) T‑Score ≤−2.5 Every 1–2 years T‑Score ≤−2.5 or reduction in BMD
Vertebral imaging Presence of a vertebral fracture Repeat if vertebral fracture is Development of vertebral fracture
suspected
DXA, dual-energy X‑ray absorptiometry; eGFR, estimated glomerular filtration rate; NA, not applicable; PHPT, primary hyperparathyroidism.
wide variation in the sensitivity and specificity of different normalize, and urinary calcium levels decline120. RCTs
modalities across institutions. Cervical ultrasonography and nonrandomized studies indicate that BMD improves
can localize parathyroid disease and assess for concom- robustly over the first year after parathyroidectomy with
itant thyroid pathology. Technetium (99mTc) sestamibi is further increases over time, even in those with normal
the dominant radioisotope in parathyroid scintigraphy. BMD8,72,83,121; limited data suggest fracture risk might
Sestamibi protocols vary (dual phase, I131 subtraction, also decline72. Risk of nephrolithiasis also decreases after
single-photon emission CT (SPECT) or SPECT–CT); successful parathyroidectomy 122.
a review of the individual strengths and weaknesses Postoperatively, most patients are discharged on cal-
of these protocols can be found elsewhere25. Sestamibi cium and vitamin D supplementation. Some patients
protocols have low sensitivity in multi-gland disease. remain persistently hyperparathyroid after successful
Combined ultrasonography and sestamibi imaging parathyroid surgery (as evidenced by normalization of
increases localization accuracy and improves sensitiv- serum calcium levels) if they have untreated vitamin D
ity. Although traditional CT imaging has little utility, the deficiency or inadequate calcium intake (a form of ‘hun-
4D CT protocol has emerged as a useful modality even gry bones’). Correction of the underlying cause of their
though once again, it has limited sensitivity in multi- secondary hyperparathyroidism should lead to normali-
gland disease. Other technologies are recommended in zation of all indices. Patients with normocalcaemic PHPT
more limited settings. MRI and venous sampling can cannot be considered to be cured until and unless their
be considered in cases of reoperation or difficult local- PTH levels normalize, as their calcium levels were never
ization or when ionizing radiation is contraindicated. abnormal. Patients who are not cured (those with both
Although PET is costly and not widely available, recent calcium and PTH levels that remain elevated after sur-
data support incremental value of 18F-fluorocholine PET gery) are said to have persistent PHPT25. A small subset of
with CT (PET–CT) in the localization of pathologic par- patients will be cured (with normalization of calcium and
athyroid glands118. Preoperative fine-needle aspiration PTH levels) for a period of 6 months or more (up to many
biopsy (FNAB) preoperatively is generally not recom- years) and then develop biochemical evidence of PHPT
mended in PHPT and is absolutely contraindicated if once again. These patients are said to have recurrent
parathyroid cancer is a diagnostic consideration, as PHPT25. The incidence of recurrent PHPT is not known.
FNAB can seed the operative site, leading to spread of
disease. In the 5–10% of patients in whom surgery is per- Non-surgical monitoring and management
formed for persistent or recurrent disease, two or more The surgical guidelines developed by various groups
concordant studies should be obtained before surgery. imply that it is safe to monitor those who do not meet
A success rate of up to 95% can be achieved when this surgical guidelines25,71. Additionally, monitoring is rec-
rule is followed, but no agreement exists as to which two ommended for those who refuse surgery and those who
studies are best in these cases119. have significant comorbidities and are deemed poor
Bilateral neck exploration was the traditional sur- surgical candidates. Very few patients fall into the lat-
gical approach and has cure rates of >95% with a low ter category given the recent advances in parathyroid
risk of complications25. Improvements in imaging and surgery, including MIP, which can be performed with
the availability of intraoperative PTH monitoring allow local anaesthesia. However, those who have poor over-
for MIP in many centres, which reduces the extent of all health that prohibits use of general anaesthesia and
surgery, incision length, discomfort and recovery time who are not good candidates for local anaesthesia due to
and is associated with high cure rates as well25. MIP is aspiration risk or sleep apnoea might fall into this group.
appropriate for those with single adenomas in whom Long-term observational studies indicate that biochem-
preoperative imaging has localized the culprit gland. istries and BMD remain stable for many years in those
With surgical cure of PHPT, serum biochemistries followed non-operatively 8. However, 15‑year data suggest
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 121
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
that BMD starts to decline at cortical sites after 10 years of Hydrochlorothiazide. A retrospective analysis of
observation, and almost 40% of patients developed one or 72 patients in 2016 suggested that thiazides might not
more indications for parathyroidectomy over 15 years of increase serum levels of calcium in PHPT as they can do
follow-up123. Regular monitoring of biochemistries and in normal individuals. Hydrochlorothiazide (12.5–50 mg
of BMD with DXA is recommended (TABLE 3) for those daily for 3.1 years on average) was associated with a
who choose to be observed; repeat imaging of the spine decrease in urinary calcium excretion but no change in
and kidney is advised when vertebral fractures or nephro serum levels of calcium129. Smaller and cross-sectional
lithiasis is suspected71. Guidelines for surgery during studies have suggested similar results, although it is
monitoring are similar to those at baseline (TABLE 3). unclear if hydrochlorothiazide reduces the risk of
Some data suggest surgery is more cost-effective than nephrolithiasis130,131. Given the heterogeneity of doses
medical treatment or observation of PHPT in patients used and the absence of data from larger, (preferably)
who do not meet guidelines for parathyroidectomy 124. randomized trials, recommending thiazide use routinely
However, some patients prefer observation and/or med- in PHPT is premature. However, thiazides could be con-
ical therapy to parathyroidectomy, even when meeting sidered in those who refuse surgery or are poor surgical
criteria for surgery. All patients who are observed should candidates but at high risk of nephrolithiasis, as long as
be advised to stay adequately hydrated and not to restrict serum levels of calcium are monitored regularly.
dietary calcium intake. Liberal dietary calcium intake
does not worsen hypercalcaemia. Conversely, restric- Oestrogen and selective oestrogen receptor modulators.
tion could exacerbate hyperparathyroidism125,126. The An RCT of conjugated oestrogen (0.625 mg daily plus
Fourth International Workshop recommends follow- medroxyprogesterone at 5 mg daily) versus placebo
ing the Institute of Medicine guidelines with regard to indicated that hormone-replacement therapy effectively
calcium intake127. Although calcium supplements are increases BMD at all skeletal sites in patients with PHPT,
not specifically recommended in those with PHPT and with the greatest increases at the lumbar spine132. This
osteoporosis, small doses do not seem to exacerbate RCT, however, did not confirm the calcium-lowering
hypercalcaemia or hypercalciuria if the diet is deficient128. effect of earlier uncontrolled studies127. Currently, no data
Recent guidelines recommend restoring vitamin D to regarding the ability of oestrogen to lower fracture risk in
levels of 21–30 ng/ml with conservative doses of vita- patients with PHPT are available. In an RCT, raloxifene
min D (600–1000 IU daily) on the basis of data showing (60 mg daily compared with placebo; n = 18) decreased
that vitamin D repletion lowers PTH levels127. Higher serum levels of bone markers and serum calcium levels
levels of vitamin D might be beneficial. A 2014 RCT of after 8 weeks of treatment; BMD data were not available127.
cholecalciferol (2,800 IU daily versus placebo) indicated
that treatment increased 25OHD levels from 20 ng/ml to Bisphosphonates and denosumab. Several small RCTs
37.8 ng/ml, lowered levels of PTH, and increased lumbar have indicated that alendronate increases BMD at the
spine BMD without having a deleterious effect on serum lumbar spine and hip in patients with PHPT, but most
or urinary calcium levels59. studies suggest there is no change in serum biochemis-
Ideal medical therapy of PHPT would provide the tries127. No data exist regarding fracture risk reduction
equivalent to a medical parathyroidectomy. Such an with alendronate, and no BMD data are available in
agent would normalize serum calcium and PTH lev- PHPT for other bisphosphonates including zoledronic
els as well as urinary calcium excretion, increase BMD acid, pamidronate or ibandronate. One small nonrand-
and lower fracture risk, and reduce the risk of kidney omized study of risedronate plus calcium and vitamin D
stones. Unfortunately, no currently available single drug versus parathyroidectomy suggested that risedronate
meets all these criteria. The following medications can increases BMD at the spine compared with baseline in
achieve some of these goals and might be considered patients with PHPT but that surgery is more effective133;
in patients not having surgery in whom it is desirable no data regarding fracture risk reduction were availa-
to lower serum or urinary calcium levels or increase ble. No published data are available regarding the use of
BMD (TABLE 4). denosumab in PHPT. In summary, anti-resorptives can
be considered in patients not undergoing parathyroid-
ectomy who have osteoporosis, a history of fragility frac-
Table 4 | Response to medication in patients with PHPT* ture or high fracture risk, though none are specifically
approved for the treatment of PHPT.
Drug Serum calcium Serum PTH Urinary calcium BMD
level level excretion
Cinacalcet. Cinacalcet is a type 2 calcimimetic that binds
HCTZ No change No change Decreases No data
to the CASR and increases its sensitivity. Cinacalcet
Oestrogen No change No change No change Increases effectively reduces serum levels of calcium in patients
Raloxifene Decreases** No change No change No data with PHPT. Cinacalcet was approved for PHPT by the
Alendronate No change No change No change Increases European Medicines Agency in 2008 and by the FDA
in 2011 for the treatment of severe hypercalcaemia in
Cinacalcet Decreases Minimal No change No
decrease change
patients with PHPT who are unable to undergo para
thyroidectomy 127. Cinacalcet maintains long-term
*We are not recommending the use of these agents in PHPT (the changes described are
occasionally based on small numbers of individuals). **At 8 weeks of treatment. HCTZ, normocalcaemia across a wide spectrum of disease
hydrochlorothiazide. severity 127. Unfortunately, neither BMD nor urinary
122 | FEBRUARY 2018 | VOLUME 14 www.nature.com/nrendo
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
calcium excretion improves with cinacalcet treatment, and a reduction in nephrolithiasis. Medical therapy
and there are currently no data regarding reduction in for those who cannot undergo parathyroidectomy can
the risk of nephrolithiasis127. Cinacalcet is also frequently increase BMD (for example, oestrogen and bisphospho-
associated with headache, nausea and vomiting. nates) or reduce serum levels of calcium (calcimimetics),
but no single drug can do both.
Conclusions and future directions Looking to the future, more data are needed on the
In summary, PHPT has evolved into a disorder that is neuropsychological manifestations of PHPT to help direct
typically asymptomatic in regions of the world where surgical recommendations for patients with specific com-
serum levels of calcium are routinely measured. plaints, as well as on the cardiovascular effects of mild
Manifestations of PHPT include mild hypercalcaemia, disease. Data are also needed to enable evidence-based
osteoporosis, hypercalciuria as well as vertebral fractures decisions about current renal guidelines for surgery
and nephrolithiasis, both of which can be subclinical. and on the applicability of current surgical criteria to
Classical PHPT and normocalcaemic disease are less NPHPT. Secular trends in the measurement of calcium
common. Earlier detection of PHPT and vitamin D levels, which might increase in the developing world and
supplementation might have contributed to the changes decrease in the developed world, could alter the clinical
in PHPT presentation in recent decades. Further evolu- profile of the disease internationally. Finally, as the cause
tion might continue to occur with secular trends in the of most cases of sporadic PHPT is unknown, we do not
measurement of serum levels of calcium and vitamin D understand why some patients develop skeletal, renal or
supplementation, as well as with advances in disease other complications while others do not. Owing to the
detection and management. limited data regarding these mechanisms, a ‘personalized’
Surgery, the only curative treatment for PHPT, is rec- approach to tailor monitoring, surgical recommendations
ommended for those with symptoms and is suggested or medications to individual patients with PHPT has a
for those with asymptomatic disease who are at risk of limited role in the management of PHPT today. Future
progression or have subclinical evidence of end-organ work that advances our knowledge in these areas will
effects. Parathyroidectomy leads to an increase in BMD clearly improve the management of the disorder.
1. Cope, O. The study of hyperparathyroidism at the 15. Marx, S. J. et al. Hyperparathyroidism in hereditary 26. Eastell, R. et al. Diagnosis of asymptomatic primary
Massachusetts General Hospital. N. Engl. J. Med. syndromes: special expressions and special hyperparathyroidism: proceedings of the third
274, 1174–1182 (1966). managements. J. Bone Miner. Res. 17 (Suppl. 2), international workshop. J. Clin. Endocrinol. Metab.
2. Yeh, M. W. et al. Incidence and prevalence of primary N37–N43 (2002). 94, 340–350 (2009).
hyperparathyroidism in a racially mixed population. 16. Thakker, R. V. Genetics of parathyroid tumours. 27. Nesbit, M. A. et al. Mutations affecting G‑protein
J. Clin. Endocrinol. Metab. 98, 1122–1129 (2013). J. Intern. Med. 280, 574–583 (2016). subunit α11 in hypercalcemia and hypocalcemia.
3. Wermers, R. A. et al. Incidence of primary 17. Guan, B. et al. GCM2‑activating mutations in familial N. Engl. J. Med. 368, 2476–2486 (2013).
hyperparathyroidism in Rochester, Minnesota, isolated hyperparathyroidism. Am. J. Hum. Genet. 99, 28. Nesbit, M. A. et al. Mutations in AP2S1 cause familial
1993–2001: an update on the changing epidemiology 1034–1044 (2016). hypocalciuric hypercalcemia type 3. Nat. Genet. 45,
of the disease. J. Bone Miner. Res. 21, 171–177 (2006). 18. Yu, W. et al. Whole-exome sequencing studies of 93–97 (2013).
4. Press, D. M. et al. The prevalence of undiagnosed and parathyroid carcinomas reveal novel PRUNE2 29. Lowe, H., McMahon, D. J., Rubin, M. R.,
unrecognized primary hyperparathyroidism: mutations, distinctive mutational spectra related to Bilezikian, J. P. & Silverberg, S. J. Normocalcemic
a population-based analysis from the electronic APOBEC-catalyzed DNA mutagenesis and primary hyperparathyroidism: further characterization
medical record. Surgery 154, 1232–1237 (2013). mutational enrichment in kinases associated with of a new clinical phenotype. J. Clin. Endocrinol. Metab.
5. Heath, H. 3rd, Hodgson, S. F. & Kennedy, M. A. cell migration and invasion. J. Clin. Endocrinol. 92, 3001–3005 (2007).
Primary hyperparathyroidism. Incidence, morbidity, Metab. 100, E360–E364 (2015). 30. Albright, F., Aub, J. & Bauer, W. Hyperparathyroidism:
and potential economic impact in a community. 19. Corbetta, S. et al. Differential expression of common and polymorphic condition as illustrated by
N. Engl. J. Med. 302, 189–193 (1980). microRNAs in human parathyroid carcinomas seventeen proven cases in one clinic. JAMA 102,
6. Wermers, R. A. et al. The rise and fall of primary compared with normal parathyroid tissue. Endocr. 1276 (1934).
hyperparathyroidism: a population-based study in Relat. Cancer 17, 135–146 (2010). 31. Silverberg, S. J. et al. Current issues in the
Rochester, Minnesota, 1965–1992. Ann. Intern. Med. 20. Brown, E. M. Role of the calcium-sensing receptor presentation of asymptomatic primary
126, 433–440 (1997). in extracellular calcium homeostasis. Best Pract. hyperparathyroidism: proceedings of the Fourth
7. Griebeler, M. L. et al. Secular trends in the incidence of Res. Clin. Endocrinol. Metab. 27, 333–343 International Workshop. J. Clin. Endocrinol. Metab.
primary hyperparathyroidism over five decades. Bone (2013). 99, 3580–3594 (2014).
73, 1–7 (2015). 21. Mahoney, E. J., Monchik, J. M., Donatini, G. & De 32. Usta, A., Alhan, E., Cinel, A., Turkyilmaz, S. &
8. Silverberg, S. J., Shane, E., Jacobs, T. P., Siris, E. & Lellis, R. Life-threatening hypercalcemia from a Erem, C. A 20‑year study on 190 patients with
Bilezikian, J. P. A 10‑year prospective study of primary hepatocellular carcinoma secreting intact primary hyperparathyroidism in a developing
hyperparathyroidism with or without parathyroid parathyroid hormone: localization by sestamibi country: Turkey experience. Int. Surg. 100, 648–655
surgery. N. Engl. J. Med. 341, 1249–1255 (1999). single-photon emission computed tomographic (2015).
9. Rao, S. D. et al. Hyperparathyroidism following head imaging. Endocr. Pract. 12, 302–306 33. Mallette, L. E., Bilezikian, J. P., Heath, D. A. &
and neck irradiation. Arch. Intern. Med. 140, (2006). Aurbach, G. D. Primary hyperparathyroidism: clinical
205–207 (1980). 22. Nussbaum, S. R., Gaz, R. D. & Arnold, A. and biochemical features. Med. (Baltimore) 53,
10. Bendz, H., Sjodin, I., Toss, G. & Berglund, K. Hypercalcemia and ectopic secretion of parathyroid 127–146 (1974).
Hyperparathyroidism and long-term lithium therapy — hormone by an ovarian carcinoma with rearrangement 34. Liu, J. M. et al. Primary hyperparathyroidism: a tale of
a cross-sectional study and the effect of lithium of the gene for parathyroid hormone. N. Engl. J. Med. two cities revisited — New York and Shanghai. Bone
withdrawal. J. Intern. Med. 240, 357–365 (1996). 323, 1324–1328 (1990). Res. 1, 162–169 (2013).
11. Newey, P. J. et al. Whole-exome sequencing studies of 23. D’Amour, P. et al. Amino-terminal form of parathyroid 35. Malabu, U. H. & Founda, M. A. Primary
nonhereditary (sporadic) parathyroid adenomas. hormone (PTH) with immunologic similarities to hyperparathyroidism in Saudi Arabia: a review of 46
J. Clin. Endocrinol. Metab. 97, E1995–E2005 (2012). hPTH(1–84) is overproduced in primary and cases. Med. J. Malaysia 62, 394–397 (2007).
12. Costa-Guda, J. & Arnold, A. Genetic and epigenetic secondary hyperparathyroidism. Clin. Chem. 49, 36. Paruk, I. M., Esterhuizen, T. M., Maharaj, S., Pirie, F. J.
changes in sporadic endocrine tumors: parathyroid 2037–2044 (2003). & Motala, A. A. Characteristics, management and
tumors. Mol. Cell. Endocrinol. 386, 46–54 (2014). 24. Eastell, R. et al. Diagnosis of asymptomatic primary outcome of primary hyperparathyroidism in South
13. Pardi, E. et al. Aryl hydrocarbon receptor interacting hyperparathyroidism: proceedings of the Fourth Africa: a single-centre experience. Postgrad. Med. J.
protein (AIP) mutations occur rarely in sporadic International Workshop. J. Clin. Endocrinol. Metab. 89, 626–631 (2013).
parathyroid adenomas. J. Clin. Endocrinol. Metab. 98, 99, 3570–3579 (2014). 37. Shah, V. N., Bhadada, S., Bhansali, A., Behera, A. &
2800–2810 (2013). 25. Wilhelm, S. M. et al. The American Association of Mittal, B. R. Changes in clinical and biochemical
14. Arnold, A. M. & Levine, M. A. in The Parathyroids: Endocrine Surgeons Guidelines for definitive presentations of primary hyperparathyroidism in India
Basic and Clinical Concepts (ed. Bilezikian, J. P.) management of primary hyperparathyroidism. over a period of 20 years. Indian J. Med. Res. 139,
279–297 (Academic Press, 2015). JAMA Surg. 151, 959–968 (2016). 694–699 (2014).
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 123
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
38. Zhao, L. et al. The changing clinical patterns of 60. Silverberg, S. J. et al. Skeletal disease in primary hyper- 83. Bollerslev, J. et al. Medical observation, compared
primary hyperparathyroidism in Chinese patients: parathyroidism. J. Bone Miner. Res. 4, 283–291 (1989). with parathyroidectomy, for asymptomatic primary
data from 2000 to 2010 in a single clinical center. 61. Parisien, M. et al. The histomorphometry of bone in hyperparathyroidism: a prospective, randomized trial.
J. Clin. Endocrinol. Metab. 98, 721–728 (2013). primary hyperparathyroidism: preservation of J. Clin. Endocrinol. Metab. 92, 1687–1692 (2007).
39. Bandeira, F. & Cassibba, S. Hyperparathyroidism and cancellous bone structure. J. Clin. Endocrinol. Metab. 84. Ogino, K., Burkhoff, D. & Bilezikian, J. P. The
bone health. Curr. Rheumatol. Rep. 17, 48 (2015). 70, 930–938 (1990). hemodynamic basis for the cardiac effects of
40. Oliveira, U. E. et al. Analysis of the diagnostic 62. Cipriani, C. et al. Prevalence of kidney stones and parathyroid hormone (PTH) and PTH-related protein.
presentation profile, parathyroidectomy indication and vertebral fractures in primary hyperparathyroidism Endocrinology 136, 3024–3030 (1995).
bone mineral density follow‑up of Brazilian patients using imaging technology. J. Clin. Endocrinol. Metab. 85. Collip, J. B. & Clark, E. P. Further studies on the
with primary hyperparathyroidism. Braz. J. Med. Biol. 100, 13091315 (2015). physiological action of a parathyroid hormone. J. Biol.
Res. 40, 519–526 (2007). 63. Khosla, S. et al. Primary hyperparathyroidism and the Chem. 64, 4485–507 (1925).
41. Spivacow, F. R., Martinez, C. & Polonsky, A. [Primary risk of fracture: a population-based study. J. Bone 86. Walker, M. D. et al. Carotid vascular abnormalities in
hyperparathyroidism: postoperative long-term Miner. Res. 14, 1700–1707 (1999). primary hyperparathyroidism. J. Clin. Endocrinol.
evolution]. Medicina (B. Aires) 70, 408–414 64. Vignali, E. et al. Morphometric vertebral fractures in Metab. 94, 3849–3856 (2009).
(in Spanish) (2010). postmenopausal women with primary 87. Walker, M. D. & Silverberg, S. J. Parathyroidectomy in
42. Walker, M. D. et al. Low vitamin D levels have become hyperparathyroidism. J. Clin. Endocrinol. Metab. 94, asymptomatic primary hyperparathyroidism: improves
less common in primary hyperparathyroidism. 2306–2312 (2009). “bones” but not “psychic moans”. J. Clin. Endocrinol.
Osteoporos. Int. 26, 2837–2843 (2015). 65. Mosekilde, L. Primary hyperparathyroidism and the Metab. 92, 1613–1615 (2007).
43. Moosgaard, B. et al. Vitamin D status, seasonal skeleton. Clin. Endocrinol. (Oxf.) 69, 1–19 (2008). 88. Talpos, G. B. et al. Randomized trial of
variations, parathyroid adenoma weight and bone 66. De Geronimo, S., Romagnoli, E., Diacinti, D., D’Erasmo, E. parathyroidectomy in mild asymptomatic primary
mineral density in primary hyperparathyroidism. & Minisola, S. The risk of fractures in postmenopausal hyperparathyroidism: patient description and effects
Clin. Endocrinol. (Oxf.) 63, 506–513 (2005). women with primary hyperparathyroidism. Eur. on the SF‑36 health survey. Surgery 128, 1013–1020
44. Boudou, P., Ibrahim, F., Cormier, C., Sarfati, E. & J. Endocrinol. 155, 415–420 (2006). (2000).
Souberbielle, J. C. A very high incidence of low 25 67. Stein, E. M. et al. Primary hyperparathyroidism is 89. Perrier, N. D. et al. Prospective, randomized,
hydroxy-vitamin D serum concentration in a French associated with abnormal cortical and trabecular controlled trial of parathyroidectomy versus
population of patients with primary microstructure and reduced bone stiffness in observation in patients with “asymptomatic” primary
hyperparathyroidism. J. Endocrinol. Invest. 29, postmenopausal women. J. Bone Miner. Res. 28, hyperparathyroidism. Surgery 146, 1116–1122
511–515 (2006). 1029–1040 (2013). (2009).
45. Clements, M. R. et al. The role of 68. Walker, M. D. et al. Effect of concomitant vitamin D 90. Walker, M. D. & Silverberg, S. J. Cardiovascular
1,25‑dihydroxyvitamin D in the mechanism of deficiency or insufficiency on lumbar spine volumetric aspects of primary hyperparathyroidism.
acquired vitamin D deficiency. Clin. Endocrinol. (Oxf.) bone mineral density and trabecular bone score in J. Endocrinol. Invest. 31, 925–931 (2008).
37, 17–27 (1992). primary hyperparathyroidism. Osteoporos. Int. 27, 91. Soreide, J. A. et al. Survival after surgical treatment
46. Clements, M. R. et al. Metabolic inactivation of 3063–3071 (2016). for primary hyperparathyroidism. Surgery 122,
vitamin D is enhanced in primary 69. Hansen, S., Hauge, E. M., Rasmussen, L., Jensen, J. E. 1117–1123 (1997).
hyperparathyroidism. Clin. Sci. (Lond.) 73, 659–664 & Brixen, K. Parathyroidectomy improves bone 92. Wermers, R. A. et al. Survival after the diagnosis of
(1987). geometry and microarchitecture in female patients hyperparathyroidism: a population-based study.
47. Rao, D. S. et al. Effect of vitamin D nutrition on with primary hyperparathyroidism. A 1‑year Am. J. Med. 104, 115–122 (1998).
parathyroid adenoma weight: pathogenetic and prospective controlled study using high resolution 93. Vestergaard, P. et al. Cardiovascular events before and
clinical implications. J. Clin. Endocrinol. Metab. 85, peripheral quantitative computed tomography. after surgery for primary hyperparathyroidism. World
1054–1058 (2000). J. Bone Miner. Res. 27, 1150–1158 (2012). J. Surg. 27, 216–222 (2003).
48. Silverberg, S. J., Shane, E., Dempster, D. W. & 70. Nordenstrom, E., Westerdahl, J., Lindergard, B., 94. Streeten, E. A. et al. Coronary artery calcification in
Bilezikian, J. P. The effects of vitamin D insufficiency in Lindblom, P. & Bergenfelz, A. Multifactorial risk profile patients with primary hyperparathyroidism in
patients with primary hyperparathyroidism. for bone fractures in primary hyperparathyroidism. comparison with control subjects from the multi-ethnic
Am. J. Med. 107, 561–567 (1999). World J. Surg. 26, 1463–1467 (2002). study of atherosclerosis. Endocr. Pract. 14, 155–161
49. Tassone, F. et al. Vitamin D status in primary 71. Bilezikian, J. P. et al. Guidelines for the management (2008).
hyperparathyroidism: a Southern European of asymptomatic primary hyperparathyroidism: 95. Kepez, A. et al. Evaluation of subclinical coronary
perspective. Clin. Endocrinol. (Oxf.) 79, 784–790 summary statement from the Fourth International atherosclerosis in mild asymptomatic primary
(2013). Workshop. J. Clin. Endocrinol. Metab. 99, hyperparathyroidism patients. Int. J. Cardiovasc.
50. Viccica, G., Cetani, F., Vignali, E., Miccoli, M. & 3561–3569 (2014). Imag. 25, 187–193 (2009).
Marcocci, C. Impact of vitamin D deficiency on the 72. Lundstam, K. et al. Effects of parathyroidectomy 96. Stefenelli, T. et al. Primary hyperparathyroidism:
clinical and biochemical phenotype in women with versus observation on the development of vertebral incidence of cardiac abnormalities and partial
sporadic primary hyperparathyroidism. Endocrine 55, fractures in mild primary hyperparathyroidism. J. Clin. reversibility after successful parathyroidectomy.
256–265 (2017). Endocrinol. Metab. 100, 1359–1367 (2015). Am. J. Med. 95, 197–202 (1993).
51. Walker, M. D. et al. Vitamin D in primary 73. Rejnmark, L., Vestergaard, P. & Mosekilde, L. 97. Iwata, S. et al. Aortic valve calcification in mild primary
hyperparathyroidism: effects on clinical, biochemical, Nephrolithiasis and renal calcifications in primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 97,
and densitometric presentation. J. Clin. Endocrinol. hyperparathyroidism. J. Clin. Endocrinol. Metab. 96, 132–137 (2012).
Metab. 100, 3443–3451 (2015). 2377–2385 (2011). 98. Walker, M. D. et al. Effect of parathyroidectomy on
52. Yamashita, H. et al. Vitamin D status in Japanese 74. Cassibba, S. et al. Silent renal stones in primary subclinical cardiovascular disease in mild primary
patients with hyperparathyroidism: seasonal changes hyperparathyroidism: prevalence and clinical features. hyperparathyroidism. Eur. J. Endocrinol. 167,
and effect on clinical presentation. World J. Surg. 26, Endocr. Pract. 20, 1137–1142 (2014). 277–285 (2012).
937–941 (2002). 75. Odvina, C. V. et al. Biochemical characterization of 99. McMahon, D. J. et al. Effect of parathyroidectomy
53. Ozbey, N. et al. Correlations between vitamin D status primary hyperparathyroidism with and without kidney upon left ventricular mass in primary
and biochemical/clinical and pathological parameters stones. Urol. Res. 35, 123–128 (2007). hyperparathyroidism: a meta-analysis. J. Clin.
in primary hyperparathyroidism. World J. Surg. 30, 76. Berger, A. D. et al. Patients with primary Endocrinol. Metab. 100, 4399–4407 (2015).
321–326 (2006). hyperparathyroidism — why do some form stones? 100. Nilsson, I. L., Aberg, J., Rastad, J. & Lind, L.
54. Jayasena, C. N. et al. Associations of serum J. Urol. 181, 2141–2145 (2009). Endothelial vasodilatory dysfunction in primary
25‑hydroxyvitamin D with circulating PTH, phosphate 77. Tassone, F., Gianotti, L., Emmolo, I., Ghio, M. & hyperparathyroidism is reversed after
and calcium in patients with primary Borretta, G. Glomerular filtration rate and parathyroid parathyroidectomy. Surgery 126, 1049–1055 (1999).
hyperparathyroidism. Clin. Endocrinol. (Oxf.) 78, hormone secretion in primary hyperparathyroidism. 101. Kosch, M. et al. Studies on flow-mediated vasodilation
838–843 (2013). J. Clin. Endocrinol. Metab. 94, 4458–4461 (2009). and intima–media thickness of the brachial artery in
55. Inoue, Y. et al. Vitamin D status affects osteopenia in 78. Walker, M. D. et al. Predictors of renal function in patients with primary hyperparathyroidism.
postmenopausal patients with primary primary hyperparathyroidism. J. Clin. Endocrinol. Am. J. Hypertens. 13, 759–764 (2000).
hyperparathyroidism. Endocr. J. 55, 57–65 (2008). Metab. 99, 1885–1892 (2014). 102. Lumachi, F. et al. Intima-media thickness
56. Moosgaard, B. et al. Plasma 25‑hydroxyvitamin D and 79. Walker, M. D. et al. Effect of renal function on skeletal measurement of the carotid artery in patients with
not 1,25‑dihydroxyvitamin D is associated with health in primary hyperparathyroidism. J. Clin. primary hyperparathyroidism. A prospective case–
parathyroid adenoma secretion in primary Endocrinol. Metab. 97, 1501–1507 (2012). control study and long-term follow‑up. In Vivo 20,
hyperparathyroidism: a cross-sectional study. 80. Rao, D. S., Wilson, R. J., Kleerekoper, M. & 887–890 (2006).
Eur. J. Endocrinol. 155, 237–244 (2006). Parfitt, A. M. Lack of biochemical progression or 103. Fallo, F. et al. Ultrasound evaluation of carotid artery
57. Moosgaard, B. et al. Vitamin D metabolites and continuation of accelerated bone loss in mild in primary hyperparathyroidism. J. Clin. Endocrinol.
skeletal consequences in primary asymptomatic primary hyperparathyroidism: evidence Metab. 88, 2096–2099 (2003).
hyperparathyroidism. Clin. Endocrinol. (Oxf.) 68, for biphasic disease course. J. Clin. Endocrinol. Metab. 104. Rosa, J. et al. Pulse wave velocity in primary
707–715 (2008). 67, 1294–1298 (1988). hyperparathyroidism and effect of surgical therapy.
58. Shah, V. N., Shah, C. S., Bhadada, S. K. & Rao, D. S. 81. Kristoffersson, A., Backman, C., Granqvist, K. & Hypertens. Res. 34, 296–300 (2011).
Effect of 25 (OH) D replacements in patients with Jarhult, J. Pre- and postoperative evaluation of renal 105. Schillaci, G. et al. Large-artery stiffness: a reversible
primary hyperparathyroidism (PHPT) and coexistent function with five different tests in patients with primary marker of cardiovascular risk in primary
vitamin D deficiency on serum 25(OH) D, calcium and hyperparathyroidism. J. Intern. Med. 227, 317–324 hyperparathyroidism. Atherosclerosis 218, 96–101
PTH levels: a meta-analysis and review of literature. (1990). (2011).
Clin. Endocrinol. (Oxf.) 80, 797–803 (2014). 82. Ambrogini, E. et al. Surgery or surveillance for mild 106. Rubin, M. R., Maurer, M. S., McMahon, D. J.,
59. Rolighed, L. et al. Vitamin D treatment in primary asymptomatic primary hyperparathyroidism: Bilezikian, J. P. & Silverberg, S. J. Arterial stiffness in
hyperparathyroidism: a randomized placebo controlled a prospective, randomized clinical trial. J. Clin. mild primary hyperparathyroidism. J. Clin. Endocrinol.
trial. J. Clin. Endocrinol. Metab. 99, 1072–1080 (2014). Endocrinol. Metab. 92, 3114–3121 (2007). Metab. 90, 3326–3330 (2005).
124 | FEBRUARY 2018 | VOLUME 14 www.nature.com/nrendo
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
107. Ragno, A. et al. Chronic constipation in 117. Stavrakis, A. I., Ituarte, P. H., Ko, C. Y. & Yeh, M. W. 128. Jorde, R., Szumlas, K., Haug, E. & Sundsfjord, J.
hypercalcemic patients with primary Surgeon volume as a predictor of outcomes in The effects of calcium supplementation to patients
hyperparathyroidism. Eur. Rev. Med. Pharmacol. Sci. inpatient and outpatient endocrine surgery. Surgery with primary hyperparathyroidism and a low calcium
16, 884–889 (2012). 142, 887–899 (2007). intake. Eur. J. Nutr. 41, 258–263 (2002).
108. Pepe, J. et al. The effect of parathyroidectomy on 118. Kluijfhout, W. P. et al. Fluorine‑18 fluorocholine 129. Tsvetov, G. et al. Thiazide treatment in primary
chronic constipation in patients affected by primary PET–CT localizes hyperparathyroidism in patients with hyperparathyroidism — a new indication for an old
hyperparathyroidism. J. Bone Miner. Metab. 31, inconclusive conventional imaging: a multicenter study medication? J. Clin. Endocrinol. Metab. 102,
690–694 (2013). from the Netherlands. Nucl. Med. Commun. 37, 1270–1276 (2017).
109. Ludvigsson, J. F. et al. Primary 1246–1252 (2016). 130. Riss, P. et al. The influence of thiazide intake on
hyperparathyroidism and celiac disease: 119. Udelsman, R. & Donovan, P. I. Remedial parathyroid calcium and parathyroid hormone levels in patients
a population-based cohort study. J. Clin. surgery: changing trends in 130 consecutive cases. with primary hyperparathyroidism. Clin. Endocrinol.
Endocrinol. Metab. 97, 897–904 (2012). Ann. Surg. 244, 471–479 (2006). (Oxf.) 85, 196–201 (2016).
110. Bilezikian, J. P., Khan, A. A. & Potts, J. T. Jr. Guidelines 120. Rao, D. S., Phillips, E. R., Divine, G. W. & Talpos, G. B. 131. Farquhar, C. W., Spathis, G. S., Barron, J. L. &
for the management of asymptomatic primary Randomized controlled clinical trial of surgery versus Levin, G. E. Failure of thiazide diuretics to increase
hyperparathyroidism: summary statement from the no surgery in patients with mild asymptomatic plasma calcium in mild primary
third international workshop. J. Clin. Endocrinol. primary hyperparathyroidism. J. Clin. Endocrinol. hyperparathyroidism. Postgrad. Med. J. 66,
Metab. 94, 335–339 (2009). Metab. 89, 5415–5422 (2004). 714–716 (1990).
111. Cusano, N. E. et al. Normocalcemic 121. Rolighed, L. et al. BMD improvements after operation 132. Grey, A. B., Stapleton, J. P., Evans, M. C., Tatnell, M. A.
hyperparathyroidism and hypoparathyroidism in for primary hyperparathyroidism. Langenbecks Arch. & Reid, I. R. Effect of hormone replacement therapy
two community-based nonreferral populations. Surg. 398, 113–120 (2013). on bone mineral density in postmenopausal women
J. Clin. Endocrinol. Metab. 98, 2734–2741 122. Mollerup, C. L. et al. Risk of renal stone events in with mild primary hyperparathyroidism. A
(2013). primary hyperparathyroidism before and after randomized, controlled trial. Ann. Intern. Med. 125,
112. Maruani, G., Hertig, A., Paillard, M. & Houillier, P. parathyroid surgery: controlled retrospective follow up 360–368 (1996).
Normocalcemic primary hyperparathyroidism: study. BMJ 325, 807 (2002). 133. Tournis, S. et al. Effect of parathyroidectomy versus
evidence for a generalized target-tissue resistance to 123. Rubin, M. R. et al. The natural history of primary risedronate on volumetric bone mineral density and
parathyroid hormone. J. Clin. Endocrinol. Metab. 88, hyperparathyroidism with or without parathyroid bone geometry at the tibia in postmenopausal women
4641–4648 (2003). surgery after 15 years. J. Clin. Endocrinol. Metab. 93, with primary hyperparathyroidism. J. Bone Miner.
113. Rejnmark, L., Amstrup, A. K., Mollerup, C. L., 3462–3470 (2008). Metab. 32, 151–158 (2014).
Heickendorff, L. & Mosekilde, L. Further insights into 124. Zanocco, K. A., Wu, J. X. & Yeh, M. W.
the pathogenesis of primary hyperparathyroidism: a Parathyroidectomy for asymptomatic primary Acknowledgements
nested case–control study. J. Clin. Endocrinol. Metab. hyperparathyroidism: A revised cost-effectiveness The authors acknowledge the National Institiutes of Health
98, 87–96 (2013). analysis incorporating fracture risk reduction. Surgery (NIH; Grants DK074457 and DK084986 to S.J.S. and
114. Tuna, M. M. et al. Normocalcemic 161, 16–24 (2017). DK104105 to M.D.W.).
hyperparathyroidism is associated with complications 125. Locker, F. G., Silverberg, S. J. & Bilezikian, J. P. Optimal
similar to those of hypercalcemic dietary calcium intake in primary hyperparathyroidism. Author contributions
hyperparathyroidism. J. Bone Miner. Metab. 34, Am. J. Med. 102, 543–550 (1997). M.D.W. and S.J.S. researched data for the article, made sub-
331–335 (2016). 126. Paik, J. M., Curhan, G. C. & Taylor, E. N. Calcium stantial contributions to discussions of the content, wrote the
115. Koumakis, E. et al. Bone mineral density evolution intake and risk of primary hyperparathyroidism in article and reviewed and/or edited the manuscript before
after successful parathyroidectomy in patients with women: prospective cohort study. BMJ 345, e6390 submission.
normocalcemic primary hyperparathyroidism. (2012).
J. Clin. Endocrinol. Metab. 98, 3213–3220 127. Marcocci, C., Bollerslev, J., Khan, A. A. & Competing interests statement
(2013). Shoback, D. M. Medical management of primary The authors declare no competing interests.
116. Abdulla, A. G., Ituarte, P. H., Harari, A., Wu, J. X. & hyperparathyroidism: proceedings of the fourth
Yeh, M. W. Trends in the frequency and quality of International Workshop on the Management of Publisher’s note
parathyroid surgery: analysis of 17,082 cases over Asymptomatic Primary Hyperparathyroidism. J. Clin. Springer Nature remains neutral with regard to jurisdictional
10 years. Ann. Surg. 261, 746–750 (2015). Endocrinol. Metab. 99, 3607–3618 (2014). claims in published maps and institutional affiliations.
NATURE REVIEWS | ENDOCRINOLOGY VOLUME 14 | FEBRUARY 2018 | 125
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- SvarDocument15 pagesSvarDanica descatamiento71% (7)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Brief Summary of The Major Problem Areas at Fireart. (80Document10 pagesA Brief Summary of The Major Problem Areas at Fireart. (80Apoorv Gupta75% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- AP World History Speed ReviewDocument3 pagesAP World History Speed ReviewAshNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- En 10268-2006 - Cold Rolled High Strength - Dual Phase SteelsDocument16 pagesEn 10268-2006 - Cold Rolled High Strength - Dual Phase SteelsSuvro ChakrabortyNo ratings yet
- Product Design at Regal MarineDocument13 pagesProduct Design at Regal Marinereshmee12340% (1)
- We LikeDocument48 pagesWe LikeRahul H.No ratings yet
- Design of A MSF Desalination Plant To Be Supplied by A New Specific 42 MW Power Plant Located in IranDocument7 pagesDesign of A MSF Desalination Plant To Be Supplied by A New Specific 42 MW Power Plant Located in Iranayman jummaNo ratings yet
- 12-3 Translation OperatorDocument16 pages12-3 Translation OperatorVAHID VAHIDNo ratings yet
- Medical Device Materials - Stainless SteelDocument5 pagesMedical Device Materials - Stainless Steelmaran.suguNo ratings yet
- Secure Architecture PrinciplesDocument67 pagesSecure Architecture Principlessalim ucarNo ratings yet
- Life Cycle of A StarDocument62 pagesLife Cycle of A StarJay Stinson Kalinani100% (1)
- AS LEVEL IT 9626 A LEVEL IT 9626 Monitoring and ControlDocument17 pagesAS LEVEL IT 9626 A LEVEL IT 9626 Monitoring and ControlTooba Farooq100% (1)
- MileIQ Ultimate Guide Mileage DeductionDocument19 pagesMileIQ Ultimate Guide Mileage DeductionjazzyzNo ratings yet
- Readingpractietest4 v9 18865116Document17 pagesReadingpractietest4 v9 18865116Hssan RiahiNo ratings yet
- Field Behaviour of Stiffened Deep Cement Mixing PilesDocument17 pagesField Behaviour of Stiffened Deep Cement Mixing PilesNguyen Quoc KhanhNo ratings yet
- Current Status and Future Strategy For Development of Medicinal Plants Sector in Uttaranchal, India PDFDocument9 pagesCurrent Status and Future Strategy For Development of Medicinal Plants Sector in Uttaranchal, India PDFAmit RoyNo ratings yet
- Centrífuga Thermo Cl40 Cl40r (Manual de Servicio)Document44 pagesCentrífuga Thermo Cl40 Cl40r (Manual de Servicio)Diego Alonso SanchezNo ratings yet
- Dentin Bonding Agents My SeminarDocument36 pagesDentin Bonding Agents My SeminarSimran UtwalNo ratings yet
- The Rape of The Sabine WomenDocument7 pagesThe Rape of The Sabine WomenAnna Wu ZhuNo ratings yet
- Why Polyphase Induction Never Attains Synchronous SpeedDocument2 pagesWhy Polyphase Induction Never Attains Synchronous SpeedKaruppu SamyNo ratings yet
- Problems On Symmetrical Parabolic Curve PDFDocument20 pagesProblems On Symmetrical Parabolic Curve PDFJoash Normie DuldulaoNo ratings yet
- Roundness Metrology (21!11!07)Document193 pagesRoundness Metrology (21!11!07)Phung TuanNo ratings yet
- Boiler TroublesDocument12 pagesBoiler TroublesHARSH CHAUHAN 20SCSE1010094No ratings yet
- Tweet Workshop ManualDocument64 pagesTweet Workshop ManualwernerNo ratings yet
- Documents - Pub - Reliance Trends Internship ProjectDocument94 pagesDocuments - Pub - Reliance Trends Internship ProjectAgney KudekarNo ratings yet
- 'Class 3 Term 1 Curriculum Break Up and MYE Syallabi CR-NRDocument2 pages'Class 3 Term 1 Curriculum Break Up and MYE Syallabi CR-NRManahil ImranNo ratings yet
- Carti Despre Tehnica PicturiiDocument147 pagesCarti Despre Tehnica Picturiidespina_mircea100% (1)
- Introduction To OpenGL ProgrammingDocument20 pagesIntroduction To OpenGL ProgrammingAyush MaheshwariNo ratings yet
- Activity 2 - Effect of Blood Viscosity On Blood Flow RateDocument4 pagesActivity 2 - Effect of Blood Viscosity On Blood Flow RateTadhg Ó MaoldhomhnaighNo ratings yet
- Alemnew Mamo SiteDocument6 pagesAlemnew Mamo SiteTilahun WoretawNo ratings yet