Professional Documents
Culture Documents
Pediatric Concept Map
Uploaded by
api-507427888Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Concept Map
Uploaded by
api-507427888Copyright:
Available Formats
Concept Mapping
4832 Nursing Care of Children and Families
Key Problem 2: Alteration in nutrition/fluid
volume
Supporting Data:
-dehydration d/t nausea and vomiting
-chemotherapy side effects Key Problem 3: Risk for Impaired skin
Key Problem 1: Risk for infection integrity
-poor skin turgor
-dry mucous membranes
Supporting Data: Supporting Data:
-tachycardia (HR 130)
-bone marrow suppression d/t -effects of chemotherapy and radiation
-polyuria
chemotherapy -altered nutritional state
-dry/cracked lips
-central venous access port -fecal and urinary incontinence
-neutropenic -immobility and inactivity r/t pain and
-poor nutrition malaise
-skin ulcers -dec. albumin level
-invasive procedures -impaired circulation
Reason For Needing Health Care:
Antineoplastic Chemotherapy
Key Assessments:
-vital signs: HR, RR, temp, BP
-CBC -I&O -skin assessment
-lab values -skin turgor
-capillary refill -weight -pulse oximetry
Key Problem 4: Risk for Altered Oral Key Problem 5: Fatigue Key Problem 6: Caregiver Role Strain
Mucous Membranes
Supporting Data: Supporting Data:
Supporting Data: -lack of energy -single mother
-side effects of chemo treatment -lethargy/listlessness -part time job
-dehydration -disinterest in surroundings -financial responsibilities
-dec. platelets -chemo tx. -expressed concern about losing job
-malnutrition -anemia -knowledge deficit
-immunocompromised -physical inactivity -no time for self-care
-inadequate oral hygiene -anxiety/stress communicated about
child’s illness
Problem #1: Risk for infection
General Goal: Identify and participate in interventions to prevent/reduce risk of infection
Predicted Behavioral Outcome Objective (s):
The patient will remain afebrile and show no signs/symptoms of infection during shift
Nursing Interventions Patient Responses
1. Emphasize personal hygiene 1. Pt’s mother acknowledged importance of performing proper
2. Monitor temperature hygiene techniques
3. Promote adequate rest 2. Pt temperature was not elevated during time of care
4. Avoid/limit invasive procedures 3. Pt slept for about two hours during shift
5. Check central line dressing for signs 4. No invasive procedures were performed
of infection 5. Central line showed no signs of infection such as drainage,
6. Monitor CBC erythema, burning or stinging
7. Administer antibiotics as indicated 6. WBC remained 4.6 which indicates no sign of infection
8. Encourage fluid intake 7. Pt received Bactrim (120mg PO M-W-F)
8. Pt drank about 320mL of juice during shift
Evaluation of outcomes objectives:
Pt remained free from infection, as evidenced by normal vital signs and absence of signs and symptoms of
infection.
Problem # 2: Alteration in nutrition/fluid volume
General Goal: Pt will display adequate fluid balance evidenced by moist mucous membranes,
good skin turgor, and adequate urinary output
Predicted Behavioral Outcome Objective (s):
The patient will have decreased nausea and increase PO intake at end of shift
Nursing Interventions Patient Responses
1. Monitor I&O 1. Pt output was 800mL and PO intake was 620mL during shift
2. Monitor VS (pulses, skin turgor, 2. Pt had 2+ pulses, normal BP, elevated HR, normal skin turgor,
mucous membranes) and dry mucous membranes
3. Inc. fluid intake (2,000ml day) 3. Pt began drinking more throughout the day
4. Monitor CBC, electrolytes, 4. CBC, electrolytes, and albumin remained normal
serum albumin 5. Pt food intake was poor; ate a couple crackers during shift
5. Monitor daily food intake 6. Inc. in calories and protein was discussed with mother
6. Encourage high calorie and 7. Pt showed no signs of nausea during shift
high protein diet
7. Assess pt. for nausea (give antiemetics)
Evaluation of outcomes objectives:
Pt showed slight increase in PO intake but was still dehydrated according to his I&O. Mucous membranes
Problem # 3: Risk for impaired skin integrity
were dry at end of shift, skin turgor was normal and vitals remained stable.
General Goal: Pt will participate in techniques to prevent complications/promote healing as
appropriate
Predicted Behavioral Outcome Objective (s):
The patient will have no new signs of impaired skin integrity (ulcer formation, lesions) at end of
shift
Nursing Interventions Patient Responses
1. Assess skin frequently for signs of 1. Pt had pressure ulcer on left buttocks but no sign of worsening
skin breakdown or new locations of skin breakdown
2. Encourage fluid intake 2. Pt was encouraged to drink fluids throughout day; drank total
3. Turn/reposition pt q 2hrs of 620mL during shift
4. Apply moisture barrier 3. Pt was repositioned every hour
5. Assess skin and IV site for edema, 4. Antibiotic cream was applied to left buttocks where skin
tenderness or erythema breakdown was evident
6. Pat skin instead of rub when drying 5. Skin/IV site showed no signs of infection or potential breakdown
6. Patting rather than rubbing was done while cleansing patient
Evaluation of outcomes objectives:
Pt’s skin remained intact and no new signs of skin breakdown or impaired skin integrity were evident.
Problem #4: Risk for Altered Oral Mucous Membranes
General Goal: Pt. will demonstrate techniques to maintain/restore integrity of oral mucosa
Predicted Behavioral Outcome Objective (s):
Pt will display intact mucous membranes that are pink, moist, and free of
inflammation/ulcerations at end of shift
Nursing Interventions Patient Responses
1. Assess dental/oral hygiene 1. Pt showed no signs of poor oral hygiene
2. Note changes in mucous membrane 2. Mucous membranes were dry, but intact
integrity 3. Glycerin swabs were used when performing oral hygiene for pt
3. Initiate oral hygiene (mouthwash or 4. Soft toothbrush was used during oral care
glycerin swabs) 5. Lip balm was applied to prevent further cracking/dryness of lips
4. Brush w/soft toothbrush 6. No signs of thrush were present during assessment
5. Keep lips moist w/lip balm to prevent 7. Fluid intake was encouraged throughout entire shift (pt drank
drying/cracking 620mL during shift)
6. Monitor for signs of thrush
7. Encourage fluid intake
Evaluation of outcomes objectives:
Pt continued to have dry mucous membranes, but showed no signs of thrush or cracked lips.
Problem #5: Fatigue
General Goal: Pt will have an overall inc. level of energy throughout day
Predicted Behavioral Outcome Objective (s):
The patient will have improved energy and participate in ADLs during shift
Nursing Interventions Patient Responses
1. Assist w/self-care needs 1. Pt was assisted with doing ADLs
2. Encourage pt to do ADLs (self-bathing, 2. Pt was able to feed self but needed assistance walking and bathing
sitting in chair, walking) self
3. Monitor physiological response to 3. Pt’s vitals did not significantly change d/t inc in activity
activity (HR, BP, RR) 4. Pt showed no signs of pain (grimacing, guarding)
4. Perform pain assessment 5. SpO2 was normal; pt did not need oxygen
5. Provide oxygen as needed 6. Pt was encouraged to sit up but unable to do so d/t extreme fatigue
6. Inc. activity level if pt is able
Evaluation of outcomes objectives:
Pt remained fatigued throughout the day but showed slight increase in level of energy towards the end of shift.
Problem # 6: Caregiver Role Strain
General Goal: Caregiver shows confidence in performing the caregiver role by meeting patient’s
physical and psychosocial needs
Predicted Behavioral Outcome Objective (s):
The caregiver will exhibit less stress and improved knowledge of care necessary for patient at
end of shift
Nursing Interventions Patient Responses
1. Assess family resources and 1. Pt’s cousins visited and mother was always at bedside
support systems 2. Mother seemed emotionally drained but expressed importance
2. Evaluate caregiver’s physical and of caring and being there for her son
mental health status 3. Mother was encouraged to take some time for herself and received
3. Encourage rest/alone time of caregiver massage at the hospital courtesy of staff
4. Assess sleep pattern of caregiver 4. Caregiver stated she gets adequate amount of sleep (about 6 hours)
5. Evaluate caregiver’s knowledge of pt 5. Mother is aware and knowledgeable about pt’s needs
needs 6. Mother was encouraged to take care of herself mentally and
6. Encourage self-care physically before taking care of the pt
7. Assess for neglect and abuse of pt 7. No signs of neglect or abuse of the pt were observed
8. Evaluate the caregiver’s willingness 8. Mother stated she is very willing to take care of her son
to assume the caregiver role
Evaluation of outcomes objectives:
Mother acknowledged the importance of caring for herself and stated she would rest/have more alone time.
You might also like
- Paris Concept MapDocument3 pagesParis Concept Mapapi-663568963No ratings yet
- Concept MapDocument5 pagesConcept Mapapi-546503916No ratings yet
- Diabetis MelitusDocument25 pagesDiabetis MelitusIrma0% (1)
- Module F Endocrine Roy Model-Protection, Rest, and ActivityDocument8 pagesModule F Endocrine Roy Model-Protection, Rest, and ActivityJeff ZhouNo ratings yet
- Problem # 2: Anxiety Related To Rashes (Petechiae) Assessmen T Nursing Diagnosi S Planning Nursing Interventio N Rational E Evaluatio NDocument1 pageProblem # 2: Anxiety Related To Rashes (Petechiae) Assessmen T Nursing Diagnosi S Planning Nursing Interventio N Rational E Evaluatio NnymphaaugustusNo ratings yet
- Peds Concept MapDocument5 pagesPeds Concept Mapapi-496323326No ratings yet
- Concept Map PedsDocument6 pagesConcept Map Pedsapi-498759347No ratings yet
- Test Bank For Saunders Comprehensive Review For The Nclex RN Examination 7th Edition Linda Anne SilvestriDocument73 pagesTest Bank For Saunders Comprehensive Review For The Nclex RN Examination 7th Edition Linda Anne SilvestriRobert Taylor100% (28)
- NCP and Drug Study For Case in SleDocument34 pagesNCP and Drug Study For Case in SlePaolo Vittorio Perdigueros GonzalesNo ratings yet
- Pir 2018 Teaching Slides Atopic Dermatitis Pir-2016-0169Document16 pagesPir 2018 Teaching Slides Atopic Dermatitis Pir-2016-0169bentoeNo ratings yet
- Concept MapDocument5 pagesConcept Mapapi-544322316No ratings yet
- critical care concept map template final 2Document6 pagescritical care concept map template final 2api-740444719No ratings yet
- Peds Concept MapDocument6 pagesPeds Concept Mapapi-663024375No ratings yet
- Malnutrition Protein Energy ProblemsDocument33 pagesMalnutrition Protein Energy ProblemsDwi AgustinaNo ratings yet
- Pediatric Concept MapDocument6 pagesPediatric Concept Mapapi-593213381No ratings yet
- Pruritusani:Etiology Andmanagement: Katharine W. Markell,, Richard P. BillinghamDocument11 pagesPruritusani:Etiology Andmanagement: Katharine W. Markell,, Richard P. BillinghamSinue PumaNo ratings yet
- Epigastric Pain Case StudyDocument19 pagesEpigastric Pain Case StudyYana PotNo ratings yet
- Brooke Baker Concept Map 4840 Complex Care: P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002Document10 pagesBrooke Baker Concept Map 4840 Complex Care: P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002api-546799391No ratings yet
- ND - Impaired Skin IntegrityDocument3 pagesND - Impaired Skin IntegrityHu DawiNo ratings yet
- Care Plan Number 2Document5 pagesCare Plan Number 2Teddy mc Bones100% (1)
- pediatric 4832 concept mapDocument4 pagespediatric 4832 concept mapapi-740642728No ratings yet
- Physical Examination - RedactedDocument52 pagesPhysical Examination - RedactedFelix FwsNo ratings yet
- Case Study (Iph) Amoebiasis Diarrhea With Mild DHNDocument9 pagesCase Study (Iph) Amoebiasis Diarrhea With Mild DHNLance_Joshua_7907No ratings yet
- Pre-Reading Supplementary Materials 5.1 Immune and Inflammatory DisordersDocument25 pagesPre-Reading Supplementary Materials 5.1 Immune and Inflammatory DisordersAndrea Love PalomoNo ratings yet
- Concept Map PedsDocument7 pagesConcept Map Pedsapi-545001894No ratings yet
- Gastritis Case Study Table of ContentsDocument27 pagesGastritis Case Study Table of ContentsNur IstiqamahNo ratings yet
- DIABETES Nursing ManagementDocument11 pagesDIABETES Nursing ManagementKaloy KamaoNo ratings yet
- 4832 Concept Map On Failure To Thrive-Desktop-1dptoe6Document11 pages4832 Concept Map On Failure To Thrive-Desktop-1dptoe6api-603346045No ratings yet
- Cebu Institute of Technology University College of Nursing Course OutlineDocument7 pagesCebu Institute of Technology University College of Nursing Course OutlineKimberly Abella CabreraNo ratings yet
- Bandal 3bsna Parotidectomy Pleomorophic AdenomaDocument25 pagesBandal 3bsna Parotidectomy Pleomorophic AdenomasharedNo ratings yet
- Ocne 9 SupportDocument8 pagesOcne 9 Supportapi-349380871No ratings yet
- Skin Soft Tissue Infections 1 - 27 - 2019Document14 pagesSkin Soft Tissue Infections 1 - 27 - 2019Muhammad Azhar ImranNo ratings yet
- Case Study of AppendicitisDocument14 pagesCase Study of AppendicitisArvin Ian Penaflor89% (27)
- Pedia Module Preschooler PDFDocument11 pagesPedia Module Preschooler PDFRegine CuntapayNo ratings yet
- E51.full 2Document22 pagesE51.full 2Diana AndriucNo ratings yet
- NUR 205-Week 5 Pre Class Assignment WI 21Document6 pagesNUR 205-Week 5 Pre Class Assignment WI 21Oliver Namyalo100% (3)
- Nursing Care Plan For Diabetes MellitusDocument5 pagesNursing Care Plan For Diabetes MellitusAgronaSlaughter67% (6)
- A. Background of The StudyDocument43 pagesA. Background of The StudyJohn Robert CruzNo ratings yet
- Lecture-3: Dermatitis. Toxicoderma. Eczema. Psoriasis. Lichenplanus. Bullous DermatosisDocument75 pagesLecture-3: Dermatitis. Toxicoderma. Eczema. Psoriasis. Lichenplanus. Bullous DermatosisLatika ChoudhuryNo ratings yet
- Type 1 Diabetes Mellitus PP pth617Document10 pagesType 1 Diabetes Mellitus PP pth617api-621438645No ratings yet
- Dengue Hemorhagic Fever (DHF)Document30 pagesDengue Hemorhagic Fever (DHF)Octa VianiNo ratings yet
- M3. Nursing DiagnosisDocument18 pagesM3. Nursing DiagnosisRezalNo ratings yet
- PhChem 421 ManualDocument70 pagesPhChem 421 ManualSomethingSomething SomethingNo ratings yet
- 65 DDB 7 CF 79183Document11 pages65 DDB 7 CF 79183marisa araujoNo ratings yet
- NCM 114 Lec NotesDocument6 pagesNCM 114 Lec NotesJustine Claire M. NamocatcatNo ratings yet
- Pediatric Nursing Process RecordDocument14 pagesPediatric Nursing Process RecordHeidi Heffelfinger67% (3)
- Askep PENYAKIT HIVDocument27 pagesAskep PENYAKIT HIVFildzah TamimiNo ratings yet
- Slides AllDocument76 pagesSlides AllKassu KanaNo ratings yet
- Disease Condition:: Hyperemsis Gravidarum: DefinitionDocument4 pagesDisease Condition:: Hyperemsis Gravidarum: DefinitionPriyanka JohnNo ratings yet
- NCS-DM Type 2 For Case PresentationDocument49 pagesNCS-DM Type 2 For Case Presentationadnelg0771% (7)
- Week 13Document6 pagesWeek 13Sal MiahNo ratings yet
- NUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Document4 pagesNUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Oliver NamyaloNo ratings yet
- Vitamins & NutritionDocument56 pagesVitamins & Nutritionahmed abd elazizNo ratings yet
- Nursing Care for Varicella PatientDocument3 pagesNursing Care for Varicella Patienteka pionitaNo ratings yet
- Concept MapDocument3 pagesConcept Mapapi-401961702No ratings yet
- Geriatric Nursing Care PlanDocument4 pagesGeriatric Nursing Care PlanHarjotBrarNo ratings yet
- Integrative Dermatology: Practical Applications in Acne and RosaceaFrom EverandIntegrative Dermatology: Practical Applications in Acne and RosaceaReena N. RupaniNo ratings yet
- Thiamine Deficiency Disease, Dysautonomia, and High Calorie MalnutritionFrom EverandThiamine Deficiency Disease, Dysautonomia, and High Calorie MalnutritionRating: 4.5 out of 5 stars4.5/5 (5)
- Letter To The EditorDocument3 pagesLetter To The Editorapi-507427888No ratings yet
- Critical Care Concept MapDocument5 pagesCritical Care Concept Mapapi-507427888No ratings yet
- Senior Capstone Clinical Nursing JudgmentDocument5 pagesSenior Capstone Clinical Nursing Judgmentapi-507427888No ratings yet
- Nursing Research PaperDocument14 pagesNursing Research Paperapi-507427888No ratings yet
- Kimberly Reinhart ResumeDocument1 pageKimberly Reinhart Resumeapi-507427888No ratings yet
- Clean and Healthy IndiaDocument2 pagesClean and Healthy IndiaMeenakshi SinghNo ratings yet
- NCM 104 Final Exam NotesDocument8 pagesNCM 104 Final Exam NotesJADE MAIKHA A. MIERGASNo ratings yet
- Safety Orientation - New EmployeeDocument4 pagesSafety Orientation - New EmployeeMattNo ratings yet
- Understanding Philippine Music History and StylesDocument15 pagesUnderstanding Philippine Music History and StylesAnne Eliver CentenaNo ratings yet
- Hospital Waste ManagementDocument40 pagesHospital Waste Managementamir khanNo ratings yet
- Disease Prevention and Control Bureau: Department of HealthDocument24 pagesDisease Prevention and Control Bureau: Department of HealthIsrael H. ZantuaNo ratings yet
- 2018 Projects Compendia IeN WiAmc7SDocument149 pages2018 Projects Compendia IeN WiAmc7Sucbscholarship officeNo ratings yet
- AstraZeneca COVID-19 vaccine informed consentDocument1 pageAstraZeneca COVID-19 vaccine informed consentJohn BNo ratings yet
- 482 839 1 SMDocument10 pages482 839 1 SMianatun Nisa'No ratings yet
- Importance of ImmunizationDocument3 pagesImportance of ImmunizationEsteban JuanNo ratings yet
- PNLE II For Community Health Nursing and Care of The Mother and ChildDocument20 pagesPNLE II For Community Health Nursing and Care of The Mother and ChildASDF ASDFNo ratings yet
- COVID-19 Patient: Institute of Public Health (IPH), LahoreDocument2 pagesCOVID-19 Patient: Institute of Public Health (IPH), LahoreFique Abdullah KhanNo ratings yet
- Advances in The Diagnosis of Preterm LabourDocument22 pagesAdvances in The Diagnosis of Preterm LabouranggialwieNo ratings yet
- Role of Print Media During CovidDocument3 pagesRole of Print Media During Coviduwu momNo ratings yet
- Polio Field and Laboratory Surveillance Requirements in The Context of nOPV2 Use 20201218Document30 pagesPolio Field and Laboratory Surveillance Requirements in The Context of nOPV2 Use 20201218francissimwinga08No ratings yet
- Social Determinants of Health Executive SummaryDocument40 pagesSocial Determinants of Health Executive Summarykingcs1100% (2)
- Updated IDSA - ATS Guidelines On Management of Adults With HAP and VAPDocument11 pagesUpdated IDSA - ATS Guidelines On Management of Adults With HAP and VAPr dwiandiniNo ratings yet
- Magna Carta of Public Health WorkersDocument7 pagesMagna Carta of Public Health Workersrural health unit-talisayanNo ratings yet
- pID - CA OVARIUMDocument21 pagespID - CA OVARIUMMaria TifaniNo ratings yet
- Application Form: Institution Name Institution Location Degree Name From (MM/YY) To (MM/YY) Degree Received (Y/N)Document6 pagesApplication Form: Institution Name Institution Location Degree Name From (MM/YY) To (MM/YY) Degree Received (Y/N)SalwiyadiNo ratings yet
- Asepsis - PPT StudentDocument21 pagesAsepsis - PPT Studentqhn9999_359999443No ratings yet
- Empiric IV RX CAP Children - UpToDateDocument3 pagesEmpiric IV RX CAP Children - UpToDateMagda Mariana Medina100% (1)
- Postpartum HTPDocument2 pagesPostpartum HTPGershom Perez AcaboNo ratings yet
- Human Diseases 8th Edition Ebook PDFDocument41 pagesHuman Diseases 8th Edition Ebook PDFchad.archuleta889100% (35)
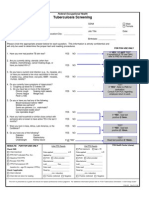
- FOH-25 Tuberculosis Screening (M.25)Document1 pageFOH-25 Tuberculosis Screening (M.25)Maria CabañasNo ratings yet
- American Needle Guard - Dental Needle Guard in NYCDocument4 pagesAmerican Needle Guard - Dental Needle Guard in NYCSyed Sajjad RazaNo ratings yet
- Sudan: African Medical Students AssociationDocument18 pagesSudan: African Medical Students AssociationAfrican Medical Students Association at IUANo ratings yet
- Manual of TB and Leprosy in TanzaniaDocument132 pagesManual of TB and Leprosy in TanzaniaYovanRivanzahNo ratings yet
- Cultural Competence or Cultural Humility Moving Beyond The DebateDocument4 pagesCultural Competence or Cultural Humility Moving Beyond The DebateEstela MedinaNo ratings yet
- TBC Who 2011 PDFDocument258 pagesTBC Who 2011 PDFdrdewdewNo ratings yet