Professional Documents
Culture Documents
2010 - Validation of A New Device To Measure Postsurgical Scar Adherence
2010 - Validation of A New Device To Measure Postsurgical Scar Adherence
Uploaded by
Naisla CarolineOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2010 - Validation of A New Device To Measure Postsurgical Scar Adherence
2010 - Validation of A New Device To Measure Postsurgical Scar Adherence
Uploaded by
Naisla CarolineCopyright:
Available Formats
Validation of a New Device to Measure Postsurgical
Scar Adherence
Giorgio Ferriero, Stefano Vercelli, Ludovit Salgovic,
Valeria Stissi and Francesco Sartorio
PHYS THER. 2010; 90:776-783.
Originally published online March 11, 2010
doi: 10.2522/ptj.20090048
The online version of this article, along with updated information and services, can be
found online at: http://ptjournal.apta.org/content/90/5/776
Online-Only Material http://ptjournal.apta.org/content/suppl/2010/04/30/90.5.77
6.DC1.html
Collections This article, along with others on similar topics, appears
in the following collection(s):
Tests and Measurements
Wound Care
e-Letters To submit an e-Letter on this article, click here or click on
"Submit a response" in the right-hand menu under
"Responses" in the online version of this article.
E-mail alerts Sign up here to receive free e-mail alerts
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Research Report
Validation of a New Device to
Measure Postsurgical Scar Adherence
Giorgio Ferriero, Stefano Vercelli, Ludovit Salgovic, Valeria Stissi,
Francesco Sartorio
G. Ferriero, MD, is Physiatrist,
Fondazione Salvatore Maugeri,
Istituto Scientifico di Veruno,
Background and Purpose. Scarring after surgery can lead to a wide range of
Servizio di Fisiatria Occupazionale disorders. At present, the degree of scar adhesion is assessed manually and by ordinal
ed Ergonomia, Via per Revislate scales. This article describes a new device (the Adheremeter) to measure scar
13, I-28010, Veruno (NO), Italy. adhesion and assesses its validity, reliability, and sensitivity to change.
Address all correspondence to Dr
Ferriero at: giorgio.ferriero@fsm.it.
Design. This was a reliability and validity study.
S. Vercelli, PT, is Physical Thera-
pist, Unit of Occupational Rehabil- Setting. The study was conducted at the Scientific Institute of Veruno.
itation and Ergonomics, Instituto
Scientifico di Veruno, Fondazione
Salvatore Maugeri, Clinica del La-
Participants and Methods. Two independent raters, a physical therapist and
voro e della Riabilitazione. a physical therapist student, used the Adheremeter to measure scar mobility and
contralateral normal skin in a sample of 25 patients with adherent postsurgical scars
L. Salgovic, MD, CSc, is Lecturer in
Surgery, Univerzita sv Cyrila a Me-
before (T1) and after (T2) physical therapy. Two indexes of scar mobility, the
toda, Trnava, Slovak Republic. adherence’s surface mobility index (SMA) and the adherence severity index (AS),
were calculated. Their correlation with the Vancouver Scar Scale (VSS) and its
V. Stissi, PT, is Physical Therapist,
Unit of Occupational Rehabilita-
pliability subscale (PL-VSS) was assessed for the validity analysis.
tion and Ergonomics, Instituto Sci-
entifico di Veruno, Fondazione Results. Both the SMA and the AS showed good-to-excellent intrarater reliability
Salvatore Maugeri, Clinica del La- (intraclass correlation coefficient [ICC]!.96) and interrater reliability (SMA: ICC!.97
voro e della Riabilitazione. and .99; AS: ICC!.87 and .87, respectively, at T1 and T2), correlated moderately with
F. Sartorio, PT, is Physical Thera- the VSS and PL-VSS only at T1 (rs!".58 to ".66), and were able to detect changes
pist, Unit of Occupational Rehabil- (physical therapist/physical therapist student): z score!"4.09/"3.88 for the SMA
itation and Ergonomics, Instituto and "4.32/"4.24 for the AS; effect size!0.6/0.4 for the SMA and 1.4/1.2 for the AS;
Scientifico di Veruno, Fondazione
standard error of measurement!4.59/4.79 mm2 for the SMA and 0.05/0.06 for the AS;
Salvatore Maugeri, Clinica del La-
voro e della Riabilitazione. and minimum detectable change!12.68/13.23 mm2 for the SMA and 0.14/0.17 for
the AS.
[Ferriero G, Vercelli S, Salgovic L,
et al. Validation of a new device
to measure postsurgical scar ad- Limitations. The measurement is based on the rater’s evaluation of force to
herence. Phys Ther. 2010;90: stretch the skin and on the patient’s judgment of comfort.
776 –783.]
© 2010 American Physical Therapy
Discussion and Conclusions. The Adheremeter showed a good level of
Association reliability, validity, and sensitivity to change. Further studies are needed to confirm
these results in larger cohorts and to assess the device’s validity for other types of
scars.
Post a Rapid Response to
this article at:
ptjournal.apta.org
776 f Physical Therapy Volume 90 Number 5 May 2010
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
S
carring after surgery can lead to
a wide range of disorders such
as pain, movement limitation,
functional impairment, and aesthetic
or psychological disturbance.1,2 The
assessment of pathological postsur-
gical scars is crucial for planning
their treatment.3– 6 It usually includes
evaluation of physical characteristics
(eg, height, pliability, relief, adhesion),
cosmetic appearance (color, cosmetic
defects), and the patient’s symptoms
(pain, itching). In particular, scar ad-
herence (defined as the failure of the
tissues to successfully establish inde-
pendent layering)7 may produce sev-
eral clinical problems, limiting range
of motion and muscle strength (force-
Figure 1.
generating capacity) and altering the
The Adheremeter. The diameter of the largest concentric ring is 28 mm, and the
local proprioceptive input.6,7 external edge of the device is 17.5 mm from the center.
To date, most clinicians assess ad-
herent scars only by simple manual
evaluation.8 None of the available scar experienced in treating patients with Vancouver Scar Scale
rating scales9,10 have been proved postsurgical scars. The student was The VSS is the most widely used out-
valid for measuring scar adherence.6 in the third year of study for a phys- come scale for scars. Four physical
Moreover, there are many devices for ical therapy degree and had no spe- characteristics are rated: vascularity,
measuring different aspects of scars,11,12 cific experience in assessing postsur- pigmentation, height, and pliability.
but none for scar adherence. gical scars. Both raters were briefly In the original version, each variable
taught how to use the device. Neither includes ordinal subscales that are
Due to the lack of assessment tools rater was involved in the patients’ summed to obtain a total score rang-
for scar adherence and the clinical treatment. ing from 0 to 13, with 0 representing
impact of this disturbance for physi- normal skin. A different weight is
cal therapist practice, we focused Adheremeter given to each item (eg, the pliability
our attention on developing a simple The Adheremeter is a new device subscale [PL-VSS] ranges from 0 to 5
new device for scar adhesion assess- designed to measure adherence of points). Scar characteristics are de-
ment: the Adheremeter. The aim of postsurgical scar, which is defined fined not only by a numerical score,
this study was to validate the Adher- as the restriction of scar mobility but also by descriptors to increase
emeter in assessment of postsurgical with respect to underlying tissue of the potential for objective rating and
scars by analyzing its reliability, con- the worst adherent point when facilitate the training process for ob-
current validity with the Vancouver stretched in 4 orthogonal directions. servers.6 Although the literature on
Scar Scale (VSS), and sensitivity to It is an inexpensive and easy-to-use the VSS focuses predominantly on
change. instrument with an ergonomic shape,
consisting of 9 concentric rings with
Materials and Method radii of 1, 2, 4, 6, 8, 10, 12, 14, and Available With
Examiners 15 mm, respectively (Fig. 1), printed This Article at
After a pilot study, 2 raters—a phys- on flexible transparency film for ptjournal.apta.org
ical therapist and a physical therapist copiers (product no. PP2500)* to en-
student—were selected as represen- • The Bottom Line Podcast
sure maximum adaptability to differ-
tatives of 2 hypothetical categories ent anatomical surfaces. • Audio Abstracts Podcast
of interest among raters: expert and
This article was published ahead of
inexpert, respectively. The physical print on March 11, 2010, at
therapist was an employee of the Sci- * 3M, Corporate Headquarters, 3M Center, ptjournal.apta.org.
entific Institute of Veruno, who was St Paul, MN 55144-1000.
May 2010 Volume 90 Number 5 Physical Therapy f 777
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
Table 1. gery. The exclusion criteria were:
Main Characteristics of the Study Participants and of the Scars scars on the face, head, or trunk; pre-
Patient or Scar Characteristic Data
vious surgery in the same area; other
local problems reducing skin elasticity
Sex, male/female 8/17
(eg, hyperkeratosis) in the affected or
Age (y), X (SD) 38.3 (14.3)
contralateral limb at the correspond-
Scars, linear/arthroscopic 21/4 ing site of the adherence, considered a
Body region, upper arm/leg 8/17 reference measure of normal skin mo-
Location, over a joint/not over a joint 13/12 bility. Twenty-five patients between
Linear scar length (mm), X (SD) 5 (3.3)
the ages of 21 and 79 years were en-
rolled in the study. Causes for surgical
Suture material, needles/staples/adhesive skin closure strips 11/11/3
interventions were: fractures (n!10),
Time from surgical treatment (d), X (SD) 72 (49.2)
ligament (n!4) and tendon (n!4) re-
pairs, entrapment syndromes at the
wrist (n!3), joint prosthesis (n!1),
burn scars, the scale also has been increase the reliability and the valid-
arthrodesis (n!1), Dupuytren disease
validated for rating postsurgical ity of the scale, but, to our knowl-
(n!1), and traumatic injury of the
scars.13,14 In this study, we used the edge, its psychometrical properties
hand (n!1). Table 1 shows the main
modified version proposed by Ned- have never been analyzed.
characteristics of the study sample and
elec et al,9 which takes into account
of the scars. The mean (SD) duration
the concept of scar adherence de- Participants
of treatment was 10 (2) sessions,
fined as firmness.11 Global adher- The participants in this study repre-
with a frequency of 2 to 3 sessions
ence in local structures surrounding sented a convenience sample of pa-
per week. During each session, pa-
the scar is assessed with the PL-VSS, tients who were recruited with a con-
tients underwent a physical therapy
in which Nedelec et al changed the secutive sampling method over a
program including scar manual ther-
term “banding” to “adherent” and period of 10 months. All participants
apy plus stretching, joint mobiliza-
eliminated the term “contracture,” were patients referred to the Scientific
tion, muscle strengthening, and
reducing the score for this item to a Institute of Veruno, Salvatore Maugeri
functional exercises, depending on
maximum of 4 points. They also Foundation, for rehabilitation assess-
the goal of rehabilitation and their
slightly adjusted some other sub- ment and treatment. They were as-
injury. The study was approved by
scales, increasing the possible total sessed by a physiatrist and recruited if
the local institutional review board,
score to a maximum of 14 points. they had an adherent scar on one limb
and written informed consent was
This version has been proposed to as a consequence of orthopedic sur-
obtained from all participants in ac-
cordance with institutional review
board guidelines.
The Bottom Line
Procedure
What do we already know about this topic? The Adheremeter and the VSS were
administered simultaneously before
Assessment of skin adherence postsurgical scaring is crucial prior to (T1) and at the end (T2) of the phys-
planning treatment. Clinicians need tools to reliably measure scar adhe- ical therapy intervention. Only the
sion rather than estimating it or using less reliable methods. physical therapist administered the
VSS. The 2 raters performed the mea-
What new information does this study offer? surement on the same day (in the
This study reports on the Adheremeter: a new and easy-to-use device for morning), one 10 minutes after the
other, in random order. During test-
measuring scar adhesion in clinical practice.
ing, each examiner was alone with
If you’re a patient, what might these findings mean the patient in the room. Each rater
for you? was blinded to the other’s assess-
ment and their own previous results
Quantification of the extent of scar adhesion with the Adheremeter (at T2).
makes it possible to reliably assess changes at follow-up, and, secondarily,
to make better judgments of the effects of your treatment. Each rater identified as landmarks the
worst adherent point and the skin on
778 f Physical Therapy Volume 90 Number 5 May 2010
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
Figure 2.
Scar adherence (marked with a black fine-point pen) in original position (O) at rest (left) and at maximal caudal excursion (C) (right)
when stretched with maximal force within a comfort range for the patient. Red arrow shows stretching direction. In this example,
maximal caudal excursion of the adherence (from O to C) is 3 mm.
the contralateral anatomic position landmark returned to the Adhereme- rostro-caudal) and 1 represents com-
of the adherence and marked them ter’s center and, if not, repeated the pletely normal scar mobility. In both
with a fine-line pen. Both surfaces measurement. Markers on the skin indexes, an increase of values means
were cleaned. In linear scars, the were cleaned at the end of each mea- a better scar condition (ie, a higher
rater reported on the patient record surement. The whole procedure surface mobility for the SMA and a
the position of the worst adherent generally took a few minutes per scar surface mobility approaching
point by measuring its distance from landmark. that of normal skin for the AS).
the 2 extremities of the scar. The
Adheremeter was positioned so that Data Analysis
the rings were centered on the land- The 4 measurements (ie, caudal, ros-
mark. Skin was relaxed, and nearby tral, and the 2 side maximal land-
joints were in a loose-packed posi- mark excursions from the rest posi-
tion. The rater held the device in the tion), taken both for the scar and for
hand, supporting the hand on the the normal contralateral skin, were
patient’s body in such a way that used to obtain a couple of indexes of
there was no contact between the surface mobility: the adherence’s
Adheremeter and the patient’s skin. surface mobility index for the scar
The other thumb was positioned (SMA) and the surface mobility index
close to the external edge of the de- for the normal contralateral skin
vice (17.5 mm from the center) (SMN). The score of each index of
(Fig. 2). Before stretching the skin surface mobility was obtained by cal-
with the thumb with maximal force culating the area of the quadrilateral
within a comfortable range for the whose diagonals, which are orthog- Figure 3.
patient, the rater said to the patient, onal to each other, are the side-to- Graphic representation of the surface mo-
“Now, I’m beginning to stretch the side and rostro-caudal landmark max- bility index. O is the original position of
skin; if you feel any discomfort, tell imal excursions (Fig. 3). Then, the the evaluation point, S1 and S2 represent
the 2 maximal lateral excursions, and C
me immediately.” Traction was ap- SMA was compared with the SMN, and R represent the maximal caudal and
plied centrifugally in 4 directions: thus giving an index of adherence rostral excursions. Because the diagonals,
caudal, rostral, right side, and left severity (AS). The AS estimates the S1S2 (side-to-side, red) and RC (rostro-
side. For every traction, the rater ratio between the SMA and the SMN: caudal, blue), intersect at right angles, the
read on the Adheremeter the posi- AS!SMA/SMN (Fig. 4). Its values thus area of the quadrilateral (yellow) is com-
puted as: (S1S2 # RC)/2. In this example,
tion of the landmark at the maximal calculated range from 0 to 1, where S1S2!7$5!12 mm, RC!8$2!10 mm,
excursion. Once the tension was re- 0 represents scar immobility in at and, consequently, the surface mobility
leased, the rater verified that the least one diagonal (side-to-side or index is scored as 12 # 10/2!60 mm2.
May 2010 Volume 90 Number 5 Physical Therapy f 779
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
mined on the basis of the pilot study 3. The standard error of measure-
expecting to obtain ICC values of ment (SEM) at T1, reflecting the
about .90, with a 95% confidence extent of expected errors in dif-
interval (CI) close to .2.16 The in- ferent raters’ scores, computed
trarater reliability of the SMN (T1 ver- as follows: SEM!SD # &1 " R,
sus T2) was calculated for both rat- where SD is the standard devia-
ers. Interrater reliability was analyzed tion of test scores and R is the
by comparing the SMA, SMN, and AS test-retest reliability coefficient,
at both T1 and T2 for both raters. which in this study was the ICC18;
and
Given the sample size of 25 pa-
tients15 and the link between scar 4. The minimum detectable change
adherence, pliability, and general in single subjects (MDC), com-
scar healing,5 to provide evidence of puted from the SEM, to indicate
Figure 4. concurrent validity, we tested our the amount of change required to
Graphic representation of the surface mo-
a priori hypothesis, which was to be adequately confident that the
bility index (patient 7) showing differ-
ences between the adherence’s surface find at least a moderate correlation change that has occurred is not
mobility index for the scar (SMA) (patho- (r %.50) between the SMA and the AS attributable to measurement error
logical condition, red quadrilateral) and and both VSS and PL-VSS. Correlation or chance variation. The MDC
the surface mobility index for the normal coefficients (rs) were calculated us- was estimated using a previously
contralateral skin (SMN) (normal skin con-
ing the Spearman rank method, cor- described method (1.96 # SEM
dition, black quadrilateral) at the initial
examination (T1) and the SMA at the end rected for ties. Data were analyzed # &2, where 1.96 is the 2-sided
of treatment (T2) (outcome, blue quadri- using SPSS statistical software.† tabled z value for a 95% CI).18
lateral). The figure clearly shows, in this
patient, an improvement in scar mobility The sensitivity to change (ie, the abil- Results
after the treatment (the blue quadrilateral
ity to detect change in general, re- The mean duration of the rehabilita-
is larger than the red quadrilateral), but
also that maximal rostral excursion did gardless of whether the change was tion intervention was 17 days (inter-
not change. In this example: at T1, clinically relevant) of the SMA and quartile range!12–30 days). No pa-
SMA!10 mm2, SMN!60 mm2, and, con- the AS was determined by: tient reported discomfort during
sequently, AS is scored as 10/60!0.17; measurement with the Adheremeter.
at T2, SMA!12 mm2, SMN!60 mm2,
1. Wilcoxon signed rank tests; Table 2 shows the mean values for
and, consequently, AS is scored as 12/
60!0.20. the SMA and the AS at T1 and T2.
2. The effect size, defined as mean Both scores increased significantly
change score (T2"T1) divided by during the testing period (for all,
the standard deviation of the T1 P'.001). Figure 5 shows the corre-
Intrarater and interrater reliability
(admission) scores (values around lation between the AS values at T1
were calculated by computing the
0.2, 0.5, and 0.8 are considered, and changes that occurred after the
intraclass correlation coefficient
respectively, small, moderate, treatment period, calculated for each
(ICC [2,1]) at T1 and T2. Intraclass
and good)17; patient with the following formula:
correlation coefficient values higher
than .75 were considered good, and [(AS score at T2)"(AS score at T1)].
those above .90 were considered ex- Table 3 shows the mean values for
cellent.15 The sample size of 25 pa- the VSS and the PL-VSS at T1 and T2.
tients assessed by 2 raters was deter- †
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
Table 2.
Mean (SD) Values for the Adherence’s Surface Mobility Index for the Scar (SMA) and the Index of Adherence Severity (AS) at the
Initial Examination (T1) and at the End of Treatment (T2)
Physical Therapist Physical Therapist Student
Index T1 T2 T1 T2
SMA 20.82 (26.51) 37.96 (47.96) 22.64 (32.31) 37.18 (47.96)
AS 0.22 (0.15) 0.44 (0.25) 0.25 (0.18) 0.44 (0.25)
a
SMA!the adherence’s surface mobility index for the scar, AS!index of adherence severity.
780 f Physical Therapy Volume 90 Number 5 May 2010
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
In normal skin, measurement of in-
trarater reliability showed excellent
and reliable values in both raters
(ICC!.96; 95% CI!.91, .98). Interra-
ter reliability values for the SMN,
SMA, and AS are shown in Table 4.
Correlations between both the Ad-
heremeter’s indexes (SMA and AS)
and the VSS and PL-VSS are shown in
Table 5. The z values were "4.09
and "3.88 for the SMA and "4.32
and "4.24 for the AS, for the physi-
cal therapist and the physical thera-
pist student, respectively (P'.001).
The effect size was 0.6 and 0.4 for
the SMA index and 1.4 and 1.2 for the
AS. The SEM was 4.59 and 4.79 mm2
for the SMA and .05 and .06 for Figure 5.
the AS. The MDC was 12.68 and Correlation between the index of adherence severity (AS) at the initial examination
13.23 mm2 for the SMA and 0.14 and (T1) and the AS change after treatment (T2"T1), based on the physical therapist’s
0.17 for the AS. The MDC for the AS measurements.
was met or exceeded by more than
50% (13/25) of this cohort.
VSS. We chose the version proposed bility is more closely related to con-
Discussion by Nedelec et al9 because this is the traction and pliability when scar con-
Assessment of skin adherence is cru- only one that considers scar adher- dition is worse, and they suggest a
cial to obtain outcome measurements ence. The 2 Adheremeter indexes possible use of the Adheremeter to
regarding treatment of pathological (SMA and AS) showed a better corre- measure not only adherent scars but
scars and to quantify compensation in lation with the VSS and the PL-VSS at also scar pliability in general. Unfor-
medico-legal settings. To our knowl- the initial examination than after re- tunately, the PL-VSS assesses general
edge, the only scale developed for ad- habilitation. These results could be scar adhesion and is not focused on
herent scars is the Skin Glide Grade explained by the fact that scar mo- the worst adherent point.
scale, a nonvalidated 5-point Likert
scale for grading the amount of scar
restriction.10 In addition, a complex Table 3.
technological device has been pro- Mean (SD) Values of the Vancouver Scar Scale (VSS, Range!0 –14) and Its Pliability
Subscale (PL-VSS, Range!0 – 4) at the Initial Examination (T1) and at the End of
posed, but its validity has not been Treatment (T2)
demonstrated.19
Index T1 T2
The Adheremeter showed excellent VSS 5.04 (1.77) 4.44 (1.58)
intrarater reliability, both with the PL-VSS 2.08 (.81) 1.52 (.77)
expert and the inexpert examiner,
and good-to-excellent interrater reli-
Table 4.
ability for both normal skin and post-
Interrater Reliabilitya for the Surface Mobility Index for the Normal Contralateral Skin
surgical scar. Confidence intervals (SMN), the Adherence’s Surface Mobility Index for the Scar (SMA), and the Index of
for the AS were larger than for the Adherence Severity (AS) at the Initial Examination (T1) and at the End of Treatment (T2)
SMA because the AS is the ratio of 2
ICC ICC
random variables and thus has more Index (95% CI) at T1 (95% CI) at T2
variability. In fact, the greater the SMN .98 (.96, .99) .98 (.95, .99)
variability, the larger the CI.
SMA .97 (.93, .99) .99 (.98, .99)
To verify the validity of the Adher- AS .88 (.75, .94) .87 (.72, .94)
emeter, we compared it with the a
ICC!intraclass correlation coefficient, 95% CI!95% confidence interval.
May 2010 Volume 90 Number 5 Physical Therapy f 781
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
Table 5. passed between the original exami-
Correlations Among Variablesa at the Initial Examination (T1) and at the End of nation and the end of treatment. The
Treatment (T2) Adheremeter showed an adequate
SMA AS sensitivity to change, but in future
Index T1 T2 T1 T2
studies it would be interesting to
b b b
evaluate the Adheremeter’s ability to
VSS !.58 ".50 !.59 ".41c
detect minimal clinical important
b b
PL-VSS !.58 ".39 !.66 ".32
changes using anchor-based meth-
a
SMA!the adherence’s surface mobility index for the scar, AS!index of adherence severity, ods (eg, patients’ or clinicians’ judg-
VSS!Vancouver Scar Scale, PL-VSS!Pliability Subscale of the Vancouver Scar Scale. Bold values indicate
moderate correlation. ments about the changes that oc-
b
c
P'.01. curred). In this study, we did not
P'.05.
calculate the measure of a minimal
clinically important difference be-
cause it is said to be sample specif-
Figure 5 shows that AS scores The results showed that both in- ic20 and a larger sample would have
changed during the testing period dexes have adequate psychometric been necessary to obtain a universal
and that there was a greater improve- characteristics, but the AS seems the cut-point measure useful for clinical
ment in scar mobility in participants more interesting index due to the decision making.
with the highest initial scores. Both fact that differences between scar
of the Adheremeter’s indexes were and normal skin, or different anatom- Finally, the measurement is based on
able to detect these changes after ical sites, are normalized. the rater’s evaluation of force to
rehabilitation. The SEM and the MDC stretch the skin and on the patient’s
were calculated to enhance the mea- In this study, we assessed the reliabil- judgment of comfort. The experi-
sure’s interpretation. The results of ity, validity, and sensitivity to change mental protocol required a brief
this study demonstrate that a clini- of the Adheremeter in a sample of training of the raters in the assess-
cian should be confident (95%) that patients affected by orthopedic post- ment method, allowing landmark de-
an AS change score greater than 0.17 surgical pathological scars. Further termination and end-range stretch-
in individuals is not likely to be at- studies are needed to assess its valid- ing force to vary among raters.21 The
tributable to measurement error or ity for other types of scars, such as results of this study demonstrate that
chance variation, whereas for a large traumatic and burn scars, or after the method is valid, so that minimal
sample, a change greater than 0.06 surgery in specific clinical fields, differences in the intensity of force
could be sufficient. Considering that such as plastic and reconstructive (not measured in the study and thus
the MDC values obtained from each surgery. a potential source of error) probably
rater were different, we suggest tak- are not relevant. Complex and ex-
ing into account a prudent value for Limitations pensive electronic equipment that
MDC equal to 0.20 as a change value Intrarater reliability was assessed would be necessary for a more pre-
not likely to be attributable to mea- only on normal skin (SMN) because cise measurement of the intensity of
surement error or chance variation. different measuring sessions of scar stretching strength is not required
In our sample, more than 50% of the adherence on different days might with this method, making the
patients had an AS score increase have been less valid due to a possible Adheremeter feasible for use in any
greater than 0.20 (the MDC value maturation effect, and 2 or more rehabilitation setting or consulting
suggested). Moreover, most of these measuring sessions of scar adher- room. Finally, examiners were not
individuals had at admission the ence, conducted on the same day, completely masked, in that they
highest AS scores of the overall sam- could have been biased by the fact were aware of the Adheremeter
ple. These results might suggest that that the rater could have been influ- reading during the stretching (as is
the AS score could represent a pos- enced by the memory of the first the case with other common clinical
sible prognostic indicator of the final scores (rater bias). measures, such as a universal goni-
outcome after rehabilitation aimed ometer). These limitations are due
also at treating scar adhesions. In Nevertheless, there is a chance that to the nature of the study and to the
fact, patients affected by a less se- such a systematic error could have partially standardized approach used,
vere adherent postsurgical scar had a been present in the intrarater reli- chosen precisely to reflect the reali-
better improvement in scar mobility ability of the SMA and AS scores, ties of the clinic.
than the others. even if nearly 3 weeks, on average,
782 f Physical Therapy Volume 90 Number 5 May 2010
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical Scar Adherence
The Adheremeter might not be reli- This article was received February 18, 2009, 11 Cleary C, Sanders AK, Nick TG. Reliability
and was accepted December 20, 2010. of the skin compliance device in the as-
able for measuring scars situated in sessment of scar pliability. J Hand Ther.
highly concave or convex anatomi- DOI: 10.2522/ptj.20090048 2007;20:232–237.
cal zones. In the absence of a con- 12 Draaijers LJ, Botman YA, Tempelman FR,
et al. Skin elasticity meter or subjective
tralateral landmark (eg, amputation
References evaluation in scars: a reliability assess-
or scar on the midsagittal axis), we 1 van de Kar AL, Corion LU, Smeulders MJ,
ment. Burns. 2004;30:109 –114.
suggest comparing the adherence et al. Reliable and feasible evaluation of 13 Truong PT, Lee JC, Soer B, et al. Reliability
linear scars by the Patient and Observer and validity testing of the Patient and Ob-
with the nearest healthy skin. Scar Assessment Scale. Plast Reconstr server Scar Assessment Scale in evaluating
Surg. 2005;116:514 –522. linear scars after breast cancer surgery.
Plast Reconstr Surg. 2007;119:487– 494.
Conclusions 2 Moran M, Khan A, Sochart DH, Andrew G.
Evaluation of patient concerns before total 14 Truong PT, Abnousi F, Yong CM, et al.
In our sample, this new method to knee and hip arthroplasty. J Arthroplasty. Standardized assessment of breast cancer
measure adherent scars showed an 2003;18:442– 445. surgical scars integrating the Vancouver
Scar Scale, Short Form McGill Pain Ques-
adequate level of reliability, validity, 3 Roques C. Massage applied to scars. tionnaire, and patients’ perspective. Plast
and sensitivity to change. The Adher- Wound Repair Regen. 2002;10:126 –128. Reconstr Surg. 2005;116:1291–1299.
emeter could be considered a useful 4 Roques C, Téot L. A critical analysis of 15 Portney LG, Watkins MP. Foundations of
measurements used to assess and manage Clinical Research: Applications to Prac-
device for clinicians working with scars. Lower Extremity Wounds. 2007;6: tice. Upper Saddle River, NJ: Prentice Hall
patients with scars. Caution should 249 –253. Health; 2000.
be applied in generalizing the results 5 Idriss N, Maibach HI. Scar assessment 16 Bonett DG. Sample size requirements for
scales: a dermatologic overview. Skin Res estimating intraclass correlations with de-
of this study because further studies Technol. 2009;15:1–5. sired precision. Stat Med. 2002;21:1331–
are needed to confirm our results in 6 Vercelli S, Ferriero G, Sartorio F, et al. 1335.
larger cohorts and for other types of How to assess postsurgical scars? A review 17 Kazis LE, Anderson JJ, Meenan RF. Effect
of outcome measures. Disabil Rehabil. sizes for interpreting changes in health
scars. 2009;31:2055–2063. status. Med Care. 1989;27(suppl 3):S178 –
7 Kobesova A, Morris CE, Lewit K, Safarova S189.
M. Twenty-year-old pathogenic “active” 18 Taylor R, Jayasinghe UW, Koelmeyer L,
Dr Ferriero and Dr Vercelli provided concept/ postsurgical scar: a case study of a patient et al. Reliability and validity of arm volume
idea/project design. All authors provided with persistent right lower quadrant pain. measurements for assessment of lymph-
J Manipulative Phys Ther. 2007;30:234 – edema. Phys Ther. 2006;86:205–214.
writing. Dr Vercelli, Dr Stissi, and Dr Sartorio 238.
provided data collection. Dr Ferriero, Dr Ver- 19 Zhang Y, Goldgof DB, Sarkar S, Tsap LV. A
8 Sutton GS, Bartel MR. Soft-tissue mobiliza- modeling approach for burn scar assess-
celli, and Dr Salgovic provided data analysis. tion techniques for the hand therapist.
Dr Ferriero provided project management ment using natural features and elastic
J Hand Ther. 1994;7:185–192. property. IEEE Trans Med Imaging. 2004;
and institutional liaisons. Dr Salgovic pro- 9 Nedelec B, Shankowsky HA, Tredget EE. 23:1325–1329.
vided consultation (including review of Rating the resolving hypertrophic scar: 20 Copay A, Subach B, Glassman S, et al. Un-
manuscript before submission). The authors comparison of the Vancouver Scar Scale derstanding the minimum clinically impor-
thank Dr Franco Franchignoni for his con- and scar volume. J Burn Care Rehabil. tant difference: a review of concepts and
2000;21:205–212. methods. Spine J. 2007;7:541–546.
tinuing guidance and advice.
10 Silverberg R, Johnson J, Moffat M. The ef- 21 Domholdt E. Rehabilitation Research:
The research reported in this article was un- fects of soft tissue mobilization on the im- Principles and Applications. 3rd ed. Phil-
dertaken in compliance with the Helsinki mature burn scar: results of a pilot study. adelphia, PA: Elsevier Saunders; 2005.
J Burn Care Rehabil. 1996;17:252–259.
Declaration and the international principles
governing research on animals.
May 2010 Volume 90 Number 5 Physical Therapy f 783
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
Validation of a New Device to Measure Postsurgical
Scar Adherence
Giorgio Ferriero, Stefano Vercelli, Ludovit Salgovic,
Valeria Stissi and Francesco Sartorio
PHYS THER. 2010; 90:776-783.
Originally published online March 11, 2010
doi: 10.2522/ptj.20090048
References This article cites 19 articles, 1 of which you can access
for free at:
http://ptjournal.apta.org/content/90/5/776#BIBL
Subscription http://ptjournal.apta.org/subscriptions/
Information
Permissions and Reprints http://ptjournal.apta.org/site/misc/terms.xhtml
Information for Authors http://ptjournal.apta.org/site/misc/ifora.xhtml
Downloaded from http://ptjournal.apta.org/ by guest on February 10, 2013
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The 15 Most Homeless Cities in The WorldDocument16 pagesThe 15 Most Homeless Cities in The WorldGennaro ThiagoNo ratings yet
- SH Libro CompletoDocument80 pagesSH Libro CompletoMickel Caballero100% (1)
- Piping Class: PROJ: 2963 REV: 1 DOC: PPAG-100-ET-C-009Document5 pagesPiping Class: PROJ: 2963 REV: 1 DOC: PPAG-100-ET-C-009Santiago GarciaNo ratings yet
- Bemco Steel Industries Co. LTD.: Qp10-Q-6764 - Typicalsteelwatertower1500MDocument12 pagesBemco Steel Industries Co. LTD.: Qp10-Q-6764 - Typicalsteelwatertower1500MhgagNo ratings yet
- Hydraulic Rock Drill He 122: Serial NumberDocument6 pagesHydraulic Rock Drill He 122: Serial NumberElizabeth OctagonNo ratings yet
- Kenmore 385.17624 Sewing Machine Instruction ManualDocument109 pagesKenmore 385.17624 Sewing Machine Instruction ManualiliiexpugnansNo ratings yet
- Wasonga's PaperDocument13 pagesWasonga's PaperWillis WasongaNo ratings yet
- Textbook Marina Carr Pastures of The Unknown Melissa Sihra Ebook All Chapter PDFDocument53 pagesTextbook Marina Carr Pastures of The Unknown Melissa Sihra Ebook All Chapter PDFcharles.valle114100% (10)
- Mechanical Engineering Syllabus at The Amrita Vishwa Vidyapeetham, Coimbatore CampusDocument3 pagesMechanical Engineering Syllabus at The Amrita Vishwa Vidyapeetham, Coimbatore CampusMathan76No ratings yet
- XTRACT Fall2012 Manual PDFDocument15 pagesXTRACT Fall2012 Manual PDFJuan Pablo PeñalosaNo ratings yet
- Canon Option Platen Cover Type S PC Rev0 100312Document16 pagesCanon Option Platen Cover Type S PC Rev0 100312Jaime RiosNo ratings yet
- Ch. 5 - No Future For White MenDocument29 pagesCh. 5 - No Future For White MenEleanora LawrenceNo ratings yet
- Balochistan Public Procurement Rules 2014Document41 pagesBalochistan Public Procurement Rules 2014Muhammad AzamNo ratings yet
- Clio2 Groupen en PDFDocument57 pagesClio2 Groupen en PDFAlexandru TerciuNo ratings yet
- Project ApolloDocument174 pagesProject ApolloSpil_vv_IJmuiden100% (1)
- 9a L5 Vocab NotesDocument7 pages9a L5 Vocab NotesCindy NguyenNo ratings yet
- Chapter 1 Practice Quiz PrintoutDocument2 pagesChapter 1 Practice Quiz PrintoutlisajleanbalNo ratings yet
- Customize Your Parfait Pen National Pen PDFDocument1 pageCustomize Your Parfait Pen National Pen PDFMary MptNo ratings yet
- Nguyen Thi Thu Thao: ExperienceDocument2 pagesNguyen Thi Thu Thao: ExperienceThao NguyenNo ratings yet
- Switchgear Vs SwitchboardDocument20 pagesSwitchgear Vs SwitchboardJuan MoralesNo ratings yet
- Interactive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768Document32 pagesInteractive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768CarlosNo ratings yet
- Ime 100l Mcaxr0100eab LowDocument4 pagesIme 100l Mcaxr0100eab LowVictorNo ratings yet
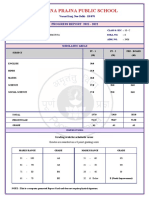
- Poorna Prajna Public School: Progress Report 2021 - 2022Document1 pagePoorna Prajna Public School: Progress Report 2021 - 2022SwagBeast SKJJNo ratings yet
- E3-282 MidSemPaper Aug2021Document3 pagesE3-282 MidSemPaper Aug2021Wiluam Rutherford BondNo ratings yet
- SG-CR01: Contact Person: Mr. Wonder Mobile: +86 15158106703 Tel: +86 571 63131356 Skype: WonderofficeworksDocument2 pagesSG-CR01: Contact Person: Mr. Wonder Mobile: +86 15158106703 Tel: +86 571 63131356 Skype: WonderofficeworksШеф ОтрисовкаNo ratings yet
- Hypnosis OusbyDocument51 pagesHypnosis OusbyRazvan Popadiuc100% (8)
- III AssociateDocument2 pagesIII Associateagupta_118177No ratings yet
- Congruence Model: Submitted By-SyndicateDocument9 pagesCongruence Model: Submitted By-SyndicateKrishnakant NeekhraNo ratings yet
- Overcoming Apathy and Classroom Disconnect in Marketing Courses: Employing Karaoke Jeopardy As A Content Retention ToolDocument7 pagesOvercoming Apathy and Classroom Disconnect in Marketing Courses: Employing Karaoke Jeopardy As A Content Retention ToolNATALY MISHELLE ROSERO HERRERANo ratings yet
- Sor - WRD Gob - 01 - 10 - 12Document383 pagesSor - WRD Gob - 01 - 10 - 12Abhishek sNo ratings yet