Professional Documents
Culture Documents
Challenges in Health Care of Rural Area
Uploaded by
Karan TrivediOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Challenges in Health Care of Rural Area
Uploaded by
Karan TrivediCopyright:
Available Formats
PROBLEMS WITH DELIVERING HEALTHCARE IN RURAL INDIA
Health is an important component for ensuring better quality of life. Large masses of the
Indian poor continue to fight hopeless and constantly losing the battle for survival and health.
The war begins even before birth, as malnourishment of the mother reduces life chances of
the foetus.
In rural India, where over 50 percent of families are living in poverty, it is not only food
security but also ill-health, which causes serious distress. Even after 50 years of
Independence, we have an infant mortality of 87 per 1,000 with most babies dying due to
diarrhoea and other minor diseases related to portable water, hygiene and sanitation.
Presently, over 25 percent of villages do not have assured source of drinking water for at least
4-5 months in a year and about 75 percent of the water sources are polluted and do not meet
the World Health Organization Standards.
Less than 10 percent of the rural population uses toilets and such lack of sanitary conditions
and shortage of clean drinking water are directly affecting the health of most of the rural
people. While the world is concerned with emerging diseases like AIDS, rural India is still
highly affected by the age-old problems of TB, malaria and diarrhoea on the one hand, and
facing new challenges posed by environmental pollution mainly due to contamination of air
by automobiles and industries, and water by agro-chemicals on the other. In such situations, it
is difficult to ensure progress and sustainable living without additional problems related to
community health.
Also the biggest problem is lack of awareness. People in rural areas are habituated to
domestic cures for their ailments and are very apprehensive about using medicines. They only
visit a doctor as the last resort after having tried everything they have been advised by
relatives and neighbours. Sometimes, this leads to worsening of their condition and the doctor
prescribing surgery or expensive medicine. This leads them to conclude a fear of going to a
fancy hospital, rather than getting an education about the disease.
Poor health in rural people suppresses their energy and enthusiasm to work hard for earning
their livelihood. In the absence of primary healthcare, it is difficult to initiate any
development programme. Inspite of this, because of the sectorial approach, health is not
considered as an integral part of the development programme.
In case of Piramal-E Swasthya, the healthcare services landscape in the state of Rajasthan
reflected the reality in India. Despite having public medical services villagers were still
following self-medication, traditional healers or private practitioners as they sought to heal
patients by balancing body’s three humors through herbs, massage and exercise. Purists
claimed that modern medicines have more harmful side effects compared to natural remedies.
Although the public facility was cheaper, lower income patients chose not to use it because it
was often closed or inconvenienced the patients who had to travel to get care. Villagers were
willing to pay a premium for more convenient access to providers, although the quality of the
care may have been suspect. Despite their small size, these communities were a complex
quilt of languages, religions and culture with intricate caste, class, age and gender
differences.
Many villages were lacking on basic infrastructure facilities and were disconnected from
urban centers due to poor transport as there were few doctors available for people. Due to
which health indicator in India were worse in rural areas where life expectancy was 12 years
because of limited access to licensed medical care. Even at higher salary doctors were not
ready to serve in rural area as they were looking at the life style of their family which was in
bad condition comparing with cities. One major problem is that average rural Indian spent as
much as 10% of income on healthcare, with medicines accounting for 15% and travel to
providers 20% of total expenditures.
For ensuring good health, there is a need to change the mindset of the donors and extension
workers involved in rural development programmes. Primary healthcare should become the
necessity for every individual, rather than treating it as a separate component of development.
You might also like
- Current Status Trends and Challenges of CHNDocument41 pagesCurrent Status Trends and Challenges of CHNangayarkanni98% (45)
- Project Proposal On Advancing Health and Sexual & Reproductive Rights of Tribal Women in OdishaDocument19 pagesProject Proposal On Advancing Health and Sexual & Reproductive Rights of Tribal Women in OdishaMinatiBindhani75% (4)
- MGT-521 Human Resource Management: HRM: End Term Evaluation AssignmentDocument8 pagesMGT-521 Human Resource Management: HRM: End Term Evaluation AssignmentKaran TrivediNo ratings yet
- Project Report On Plastic Ban1Document15 pagesProject Report On Plastic Ban1Silas Wilson67% (3)
- Error Code Copier CanonDocument7 pagesError Code Copier Canonkaka_afie100% (12)
- "It Is Health That Is Real Wealth and Not Pieces of Gold and Silver" Mahatma GandhiDocument8 pages"It Is Health That Is Real Wealth and Not Pieces of Gold and Silver" Mahatma GandhishivamNo ratings yet
- Health Sector of Pakistan Term PaperDocument14 pagesHealth Sector of Pakistan Term PaperNelum Shehzade100% (1)
- Health Care Industry in India: Dr.R.KavithaDocument4 pagesHealth Care Industry in India: Dr.R.KavithakavitagotheNo ratings yet
- Group 7 Proposal FSRRDocument3 pagesGroup 7 Proposal FSRRAusmiita SarkarNo ratings yet
- Reasons For Development of Health Care in IndiaDocument5 pagesReasons For Development of Health Care in IndiasnehapriyaNo ratings yet
- Project Proposal JheelpurDocument14 pagesProject Proposal JheelpurAftab Uddin100% (2)
- Situation of Indigenous Peoples and Rights To HealthDocument8 pagesSituation of Indigenous Peoples and Rights To Healthshubham vermaNo ratings yet
- Health CareDocument3 pagesHealth CareJhanvi SharmaNo ratings yet
- PBH101 Assignment 02Document6 pagesPBH101 Assignment 02Siam AhmedNo ratings yet
- Health Development in PakistanDocument3 pagesHealth Development in PakistanMazher Hussain SyalNo ratings yet
- Public Health Care System in IndiaDocument5 pagesPublic Health Care System in IndiaPela KqbcgrlaNo ratings yet
- Apa Determinants of HealthDocument7 pagesApa Determinants of Healthapi-446692943No ratings yet
- Ambulansiyang de PaaDocument2 pagesAmbulansiyang de PaaAlliahNo ratings yet
- CBSE Class 7 Political Science (Civics) Chapter 2 Notes - Role of The Government in HealthDocument13 pagesCBSE Class 7 Political Science (Civics) Chapter 2 Notes - Role of The Government in HealthPriya SinghNo ratings yet
- Subject Submitted To Sir. Muzammal Submitted by Naz Javaid 0004 Asna Waheed 0011 Roshina Tanveer 0012 Aamna Khan 0013Document6 pagesSubject Submitted To Sir. Muzammal Submitted by Naz Javaid 0004 Asna Waheed 0011 Roshina Tanveer 0012 Aamna Khan 0013muzammal555No ratings yet
- MH0051 - Health Administration (4 Credits) : Mbahcs Semester 3Document11 pagesMH0051 - Health Administration (4 Credits) : Mbahcs Semester 3Rajesh SinghNo ratings yet
- Fpubh 03 00245Document13 pagesFpubh 03 00245Tanushree S RaoNo ratings yet
- ProjDocument7 pagesProjAnonymous 6Xoh1YWIDeNo ratings yet
- Geriatric Care JournalDocument10 pagesGeriatric Care JournalPrincyFernandoNo ratings yet
- Tribal Population in India: A Public Health Challenge and Road To FutureDocument2 pagesTribal Population in India: A Public Health Challenge and Road To FutureMlbb GameplaysNo ratings yet
- Rural Medicine by Tunika, I.Document14 pagesRural Medicine by Tunika, I.terhemenmoavegaNo ratings yet
- HealthCareFacilitiesinRuralAreas Paper5Document18 pagesHealthCareFacilitiesinRuralAreas Paper5shiNo ratings yet
- Origins of Ayurveda Have Been Traced To Around 6,000Document13 pagesOrigins of Ayurveda Have Been Traced To Around 6,000PriyankaNo ratings yet
- Sociology Sem 2Document16 pagesSociology Sem 2cjksdbvjkcsbNo ratings yet
- ArticleDocument5 pagesArticleAnnie AsgharNo ratings yet
- 002 Class 7 Social FinalDocument4 pages002 Class 7 Social Finalpoorni9No ratings yet
- Rural Health ProjectDocument7 pagesRural Health ProjectSashaNo ratings yet
- Definition of PovertyDocument5 pagesDefinition of PovertySamy ShahNo ratings yet
- Health, EducationDocument47 pagesHealth, EducationdiljitgippyNo ratings yet
- Research IntroductionDocument1 pageResearch IntroductionBungar, Daniel Luis, Edades.No ratings yet
- Best Movement in My LifeDocument4 pagesBest Movement in My LifePujaSinghNo ratings yet
- Health in PakistanDocument3 pagesHealth in PakistanUmair ShafiqNo ratings yet
- Poverty 1Document1 pagePoverty 1Harriet SalvoNo ratings yet
- Population ExplosionDocument2 pagesPopulation ExplosionRupesh GuptaNo ratings yet
- Challenges of Home Nursing Sector A Kerala ExperienceDocument5 pagesChallenges of Home Nursing Sector A Kerala ExperienceInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Factors Associated With Nutritional Status of WomeDocument7 pagesFactors Associated With Nutritional Status of WomeMd Junayeth BhuiyanNo ratings yet
- Final Position Paper Group 8Document3 pagesFinal Position Paper Group 8secretNo ratings yet
- The Philippine Health Situation May 2017Document22 pagesThe Philippine Health Situation May 2017Amil P. Tan IINo ratings yet
- Presentation 16Document20 pagesPresentation 16siddhjain91No ratings yet
- MAC (Mother and Child) Health Project Concept: Identifying The Problems: Root Cause AnalysisDocument4 pagesMAC (Mother and Child) Health Project Concept: Identifying The Problems: Root Cause AnalysisMuhammad SajidNo ratings yet
- Health Inequities by Rama Baru PDFDocument6 pagesHealth Inequities by Rama Baru PDFwrit majumdarNo ratings yet
- Impact of Malnutrition On Health 24Document12 pagesImpact of Malnutrition On Health 24fatomNo ratings yet
- The Primary Barriers To An Accessible Quality Healthcare in The Philippines Are The Shortage of Hospitals and Surgical EquipmentDocument3 pagesThe Primary Barriers To An Accessible Quality Healthcare in The Philippines Are The Shortage of Hospitals and Surgical Equipmentartrei09No ratings yet
- Universal Health Care: The Barriers and The Way ForwardDocument2 pagesUniversal Health Care: The Barriers and The Way Forward@nshu_theachieverNo ratings yet
- The Focus of Healthcare Is Increasingly Getting Skewed Towards TheDocument4 pagesThe Focus of Healthcare Is Increasingly Getting Skewed Towards TheNitish KumarNo ratings yet
- Untitled DocumentDocument4 pagesUntitled DocumentRohit MakwanaNo ratings yet
- Nsth06 22.Rs - BalgirDocument16 pagesNsth06 22.Rs - Balgirjeyakar.mz8442No ratings yet
- Anup Kumar MishraDocument11 pagesAnup Kumar MishraMahila Pratishtha JournalNo ratings yet
- Health Problems in India: Anamika Ramawat M.Sc. Nursing Prev. BATCH 2017-18 Gcon, JodhpurDocument52 pagesHealth Problems in India: Anamika Ramawat M.Sc. Nursing Prev. BATCH 2017-18 Gcon, JodhpurFarha AamirNo ratings yet
- Asia Market Insights - India Disease Prevalence 2010Document2 pagesAsia Market Insights - India Disease Prevalence 2010Clearstate Pte LtdNo ratings yet
- Reproductive Health Status of Rural Scheduled Caste Women of Uttar PradeshDocument7 pagesReproductive Health Status of Rural Scheduled Caste Women of Uttar PradeshMariaNo ratings yet
- SSC C206 Midterm Module - PPT2Document4 pagesSSC C206 Midterm Module - PPT2Vinnie GognittiNo ratings yet
- Health Care Challenges in IndiaDocument8 pagesHealth Care Challenges in IndiaKailash NagarNo ratings yet
- Blue and White Illustrated Medical Healthcare in The 21st Century Education Presentation - 20230925 - 110030 - 0000Document8 pagesBlue and White Illustrated Medical Healthcare in The 21st Century Education Presentation - 20230925 - 110030 - 0000Janix MagbanuaNo ratings yet
- Yojana October Issue: Health and Nutrition Article1Document3 pagesYojana October Issue: Health and Nutrition Article1Ritika SinghalNo ratings yet
- UntitledDocument8 pagesUntitledifaans16No ratings yet
- Asl 1Document2 pagesAsl 1Aadab HussainNo ratings yet
- Occupational Diseases and Health Awareness Through Multimedia: A Case Study Among Women at Risk Employed in Coir Retting in Kerala, IndiaFrom EverandOccupational Diseases and Health Awareness Through Multimedia: A Case Study Among Women at Risk Employed in Coir Retting in Kerala, IndiaNo ratings yet
- CC ProjectDocument6 pagesCC ProjectKaran TrivediNo ratings yet
- Corporate Communication (COM-501) : Faculty Name: Sections: Contact: Office HoursDocument3 pagesCorporate Communication (COM-501) : Faculty Name: Sections: Contact: Office HoursKaran TrivediNo ratings yet
- Oba0: Stad Solution: MGT 511: Organization BehaviourDocument8 pagesOba0: Stad Solution: MGT 511: Organization BehaviourKaran TrivediNo ratings yet
- SpeechDocument2 pagesSpeechKaran TrivediNo ratings yet
- Are To Carry On A Real War Against War, We Shall Have To Begin With The Children"Document2 pagesAre To Carry On A Real War Against War, We Shall Have To Begin With The Children"Karan TrivediNo ratings yet
- Assignment of Problem Solving and Social Change On Background On MYBYKDocument4 pagesAssignment of Problem Solving and Social Change On Background On MYBYKKaran TrivediNo ratings yet
- PSSC Background Group-4Document6 pagesPSSC Background Group-4Karan TrivediNo ratings yet
- MatchedDocument1 pageMatchedKaran TrivediNo ratings yet
- PSSC Background Group-3Document4 pagesPSSC Background Group-3Karan TrivediNo ratings yet
- PSSC Background Group-2Document4 pagesPSSC Background Group-2Karan TrivediNo ratings yet
- Problem Solving Report On Child Labour: Group-5Document2 pagesProblem Solving Report On Child Labour: Group-5Karan TrivediNo ratings yet
- Racing BicyclesDocument1 pageRacing BicyclesKaran TrivediNo ratings yet
- PSCC Background Group-6Document4 pagesPSCC Background Group-6Karan TrivediNo ratings yet
- Golf ScoresDocument1 pageGolf ScoresKaran TrivediNo ratings yet
- MatchedDocument1 pageMatchedKaran TrivediNo ratings yet
- Expansion Strategy For Mary's Poop: X-Culture ProjectDocument13 pagesExpansion Strategy For Mary's Poop: X-Culture ProjectKaran TrivediNo ratings yet
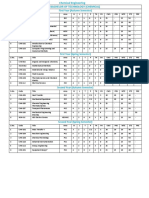
- Observation Salary ($) Position ExperienceDocument3 pagesObservation Salary ($) Position ExperienceKaran TrivediNo ratings yet
- Respondent Plan Company Total Result 69 58 53 Total Result 72 108 180Document5 pagesRespondent Plan Company Total Result 69 58 53 Total Result 72 108 180Karan TrivediNo ratings yet
- Current Mins New MinsDocument2 pagesCurrent Mins New MinsKaran TrivediNo ratings yet
- Karan RegressionDocument10 pagesKaran RegressionKaran TrivediNo ratings yet
- Regression StatisticsDocument3 pagesRegression StatisticsKaran TrivediNo ratings yet
- Range Frequency Midpoint Cumulative Freqquency (X - ) 2Document1 pageRange Frequency Midpoint Cumulative Freqquency (X - ) 2Karan TrivediNo ratings yet
- Business Engineering Arts and Sciences 3-Hour Review 1-Day Program 10-Week CourseDocument6 pagesBusiness Engineering Arts and Sciences 3-Hour Review 1-Day Program 10-Week CourseKaran TrivediNo ratings yet
- Month Units Sold (Xi-X) 2 (Xi-X)Document13 pagesMonth Units Sold (Xi-X) 2 (Xi-X)Karan TrivediNo ratings yet
- Mutual Funds - Load Return Mutual Funds - No Load ReturnDocument1 pageMutual Funds - Load Return Mutual Funds - No Load ReturnKaran TrivediNo ratings yet
- Excel GraphsDocument6 pagesExcel GraphsKaran TrivediNo ratings yet
- TOEIC 5 - Mini Test - NO KEYDocument4 pagesTOEIC 5 - Mini Test - NO KEYHồng Điệp LươngNo ratings yet
- Intro To ASCP PresentationDocument32 pagesIntro To ASCP PresentationSundar SeetharamNo ratings yet
- Bullying and Cyberbullying in Polish Elementary and Middle Schools Validation of Questionnaires Twardowska-Staszek2018Document37 pagesBullying and Cyberbullying in Polish Elementary and Middle Schools Validation of Questionnaires Twardowska-Staszek2018julzcat100% (1)
- AC Service Appointment and Maintenance FormDocument11 pagesAC Service Appointment and Maintenance FormRiad RahmanNo ratings yet
- ASTM - D888 Oxigeno DisueltoDocument14 pagesASTM - D888 Oxigeno DisueltoAngel MurilloNo ratings yet
- Chart of Accounts: Appendix UDocument3 pagesChart of Accounts: Appendix Ujawadr218No ratings yet
- Kasus Ke 10 (Inggris)Document5 pagesKasus Ke 10 (Inggris)Fauzan AdvantageNo ratings yet
- Department of Education: Inset Refelction Journal SY: 2020-2021Document2 pagesDepartment of Education: Inset Refelction Journal SY: 2020-2021RachelleGomezLatrasNo ratings yet
- Excessive Workload and Ung IsaDocument4 pagesExcessive Workload and Ung IsaElyssa Mae ChuaNo ratings yet
- Meaning and Scope of Supply Under GSTDocument5 pagesMeaning and Scope of Supply Under GSTRohit BajpaiNo ratings yet
- Caring Theories: Jaime R. Soriano - RN.RM - MSN.RTDocument56 pagesCaring Theories: Jaime R. Soriano - RN.RM - MSN.RTMarcelle HolderNo ratings yet
- Distillation Column 2Document6 pagesDistillation Column 2vaqifNo ratings yet
- Bảng mã lỗi Wise15Document56 pagesBảng mã lỗi Wise15Bach Nguyen XuanNo ratings yet
- Sloping Agricultural Land TechnologyDocument12 pagesSloping Agricultural Land TechnologyBe ChahNo ratings yet
- Abuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2Document48 pagesAbuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2sryh2012No ratings yet
- IIT Roorkee Programme Structure CHeDocument4 pagesIIT Roorkee Programme Structure CHeabcNo ratings yet
- Valve Identifier VI-SB13-01Document5 pagesValve Identifier VI-SB13-01jcastell100No ratings yet
- Data Sheet: DEGALAN® LP 64/12Document2 pagesData Sheet: DEGALAN® LP 64/12Akhtar aliNo ratings yet
- Prubsn Panel Hospital Updated As of 28082023 For CorpWebsite 2023Document10 pagesPrubsn Panel Hospital Updated As of 28082023 For CorpWebsite 2023m.abubaker1992No ratings yet
- Old MacDonald LyricsDocument5 pagesOld MacDonald LyricsMarieNo ratings yet
- Midterms Quiz 1Document2 pagesMidterms Quiz 1Arjay Cuh-ingNo ratings yet
- Gazi Abdur Rakib BiodataDocument2 pagesGazi Abdur Rakib Biodataগাজী আব্দুর রাকিবNo ratings yet
- 1 s2.0 S1110863017300228 MainDocument5 pages1 s2.0 S1110863017300228 Mainmaria melayantiNo ratings yet
- Mil PRF 680CDocument12 pagesMil PRF 680CfltpNo ratings yet
- Become Healthy or Extinct by Darryl DsouzaDocument281 pagesBecome Healthy or Extinct by Darryl DsouzaDip Dip DipNo ratings yet
- Letter For Feild Compressive Strength Test 1Document2 pagesLetter For Feild Compressive Strength Test 1Pja Shantha100% (1)
- Counter Affidavit SAMPLEDocument7 pagesCounter Affidavit SAMPLEChristle PMDNo ratings yet
- Case Studies-Industrial BuildingsDocument13 pagesCase Studies-Industrial Buildingsgligamsn0% (1)