Professional Documents
Culture Documents
Risk of 2nd Malig in NHL
Uploaded by
সোমনাথ মহাপাত্রCopyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentRisk of 2nd Malig in NHL
Uploaded by
সোমনাথ মহাপাত্রVOLUME 24 䡠 NUMBER 10 䡠 APRIL 1 2006
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Risk of Second Malignancy After Non-Hodgkin’s
Lymphoma: A British Cohort Study
Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins, Paul Smith, Zongkai Qiao, Barry W. Hancock,
Peter J. Hoskin, and David C. Linch
From the Section of Epidemiology,
Institute of Cancer Research, Sutton,
A B S T R A C T
Surrey; British National Lymphoma
Investigation, Cancer Trials Centre, Purpose
London; Department of Haematology, To assess long-term site-specific risks of second malignancy following non-Hodgkin’s lymphoma
University College London Medical (NHL) in relation to treatment and demographic factors.
School, London; Academic Unit of
Clinical Oncology, Cancer Research Patients and Methods
Centre, Weston Park Hospital, Shef- A cohort of 2,456 patients with NHL who were first treated from 1973 to 2000 and were younger
field; Clinical Oncology, Mount Vernon than 60 years from centers in the British National Lymphoma Investigation were observed, and
Hospital, Northwood, Middlesex, occurrences of second malignancy was compared with expectations based on general population
United Kingdom. cancer rates in England and Wales.
Submitted September 29, 2005;
accepted January 23, 2006.
Results
In total, 123 second malignancies occurred. Relative risks (RRs) were significantly elevated for all
Supported by The Lymphoma Research malignancies combined (RR ⫽ 1.3; 95% CI, 1.1 to 1.6) and for leukemia (RR ⫽ 8.8; 95% CI, 5.1
Trust.
to 14.1) and lung cancer (RR ⫽ 1.6; 95% CI, 1.1 to 2.3). RRs of malignancy overall diminished
Authors’ disclosures of potential con- significantly with increasing age at first treatment. Leukemia risk was significantly increased after
flicts of interest and author contribu- chemotherapy (RR ⫽ 10.5; 95% CI, 5.0 to 19.3) and mixed-modality treatment (RR ⫽ 13.0; 95%
tions are found at the end of this
CI, 5.2 to 26.7). Relative risks of lung (RR ⫽ 1.9; 95% CI, 1.1 to 3.1) and colorectal (RR ⫽ 2.1; 95%
article.
CI, 1.1 to 3.6) cancers were significantly raised following chemotherapy.
Address reprint requests to N.Y. Mudie,
MD, PhD, Section of Epidemiology, Conclusion
Institute of Cancer Research, Sutton, NHL patients are at elevated risk of developing second malignancy, particularly leukemia and lung
Surrey SM2 5NG, United Kingdom; cancer. The relative risk is greater with patients who are younger at first treatment. Chemotherapy
e-mail: nadejda.mudie@icr.ac.uk. predisposes patients toan increased risk of leukemia, and possibly lung and colorectal cancers. The role
© 2006 by American Society of Clinical of specific drug treatments in the etiology of solid cancers after NHL deserves further investigation.
Oncology
0732-183X/06/2410-1568/$20.00 J Clin Oncol 24:1568-1574. © 2006 by American Society of Clinical Oncology
DOI: 10.1200/JCO.2005.04.2200
bladder cancer has been linked to cumulative
INTRODUCTION
doses of cyclophosphamide and, to a lesser extent,
The incidence of non-Hodgkin’s lymphoma (NHL) to radiotherapy.20,21 There have been sporadic
has been increasing for the past 40 years in most reports of raised risk of several other solid can-
Western countries.1,2 With better treatment, life cers5,6,8,9,13,20,21 and Hodgkin’s disease,9,22 but in-
expectancy of NHL patients has been improving,3 consistently and without an established relationship
and hence the risk of iatrogenic malignancy is be- to treatment.
coming an important concern in long-term survi- Reports on cancer risks in NHL survivors
vors. Whereas considerable attention has focused on beyond 15 years are limited to an international
late sequelae of Hodgkin’s disease,4 relatively little study conducted by Travis et al7 that demon-
information is available about second malignancies strated a persistent significantly elevated risk of all
in NHL, as there have been few large studies with malignancies, as well as of cancers of several indi-
prolonged and complete follow-up. vidual sites. With the exception of leukemia, blad-
Several studies,5-9 but not all,10-14 have re- der, and kidney cancer risks, few studies have
ported an elevated risk of second malignancy overall examined the risk of specific second malignancies in
following NHL. Most studies have found increased relation to treatment12 and these studies usually only
risks of leukemia, especially acute nonlymphocytic used data on the initial treatment in their analy-
leukemia (ANLL),6,9,11,14-17 associated with alkylat- sis.6,14 The effect of age at first treatment on the risk
ing chemotherapy, alone or in combination with of second malignancy has rarely been examined and
total nodal/body irradiation.18,19 Raised risk of has produced conflicting results.7,9,23
1568
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Second Cancer After Non-Hodgkin’s Lymphoma
To evaluate the risk of second malignancy arising from different
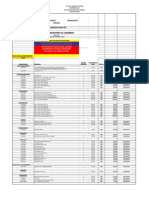
Table 1. Descriptive Characteristics of the Cohort
types of treatment for NHL, we assembled a retrospective cohort of
2,456 United Kingdom patients first treated at ages younger than 60 No. of Person-Years of
Characteristic Patients Follow-Up
years, and observed them for up to 26 years.
Year of first treatment
1973-1979 460 4,727
PATIENTS AND METHODS 1980-1984 504 4,445
1985-1989 705 5,420
1990-1994 566 3,249
The British National Lymphoma Investigation (BNLI) maintains a database
1995-2000 221 589
on the treatment and follow-up of all patients with NHL from clinical trials
Age at first treatment, years
treated in its participating hospitals. From this database, we extracted infor-
⬍ 45 932 7,658
mation on all patients first treated at ages younger 60 years, between June 1,
45-54 937 6,868
1973, and March 31, 2000, except for those who were foreign residents. The
55-59 587 3,904
data on treatments, cancers, deaths, and follow-up to March 31, 2000, were
Follow-up, yearsⴱ
then updated from case notes as necessary. Based on comparison of the BNLI
2 months† to ⬍ 5 2,456 8,728
files with case notes and other sources, we believe that the BNLI data have a
5-9 1,406 5,565
high level of completeness regarding second malignancy.24 Sites of second
10-14 795 2,713
cancer were coded according to the International Classification of Diseases
ⱖ 15 336 1,424
(ICD),25 using the editions that were applicable in England and Wales at the
Stage at diagnosis
time of diagnosis: ICD8 for 1968 through 1978, and ICD9 for 1979 through
I 500 4,992
2000. We bridge-coded the data to ICD9 categories.
II 489 4,007
For each patient in the cohort, person-years at risk of second cancer were
III 499 3,979
calculated by 5-year age group, sex, and calendar year, from 2 months after the
IV 917 5,306
date of first treatment (cancers and person-years in the first 2 months of
Not known 51 146
follow-up were excluded from the analysis to avoid inadvertent inclusion of
Histology
synchronous tumors6) to the date of the end of follow-up, or of second cancer
Follicular 771 7,062
incidence, death, or loss to follow-up, if earlier. Thirty-one patients were
Lymphocytic 168 1,245
excluded from the study because less than 2 months of follow-up was available
Lymphoblastic/Burkitt-type 106 505
for them and a further six patients were excluded due to insufficient treatment
Diffuse large cell‡ 1,163 8,064
data available. For analyses of time since first treatment and type of treatment,
Unclassified or other§ 193 1,389
case subjects were allocated at each point in their follow-up to the analytic cat-
Unknown 55 165
egory applicable at that time. Type of treatment was categorized into chemo-
Sex
therapy, radiotherapy, and mixed-modality treatment. Sub-analyses were also
Male 1,413 10,140
conducted for the two most common chemotherapy regimens: CHOP (cyclo-
Female 1,043 8,290
phosphamide, doxorubicin, vincristine, and prednisolone) and chlorambucil,
Treatment㛳
whether or not the patient had received radiotherapy or any other chemother-
Radiotherapy 328 4,165
apy. It was not practical for us to obtain more detailed therapeutic information
Chemotherapy 1,274 9,392
for the total cohort, and this will be addressed elsewhere by nested case-control
Mixed modalities 854 4,873
studies. Expected numbers of cancers incident in the cohort were calculated for
Total 2,456 18,430
each cancer site by multiplying age-, sex-, and calendar year–specific person-
ⴱ
years at risk in the cohort by the corresponding cancer registration rates in the No. of patients refers to number at the beginning of each follow-up category;
general population of England and Wales. Completeness of cancer registration person-years refer to time accumulated when in these categories (individuals
could contribute to more than one category).
in England and Wales has been assessed to be 90%1; however, cases of non- †Because first 2 months after first treatment was excluded; see Methods.
melanoma skin cancer were excluded from the analysis as their registration is ‡Including diffuse mixed cell lymphoma.
seriously incomplete.1 The ratio of observed to expected numbers of inci- §Other lymphomas include lymphocytic intermediate differentiation and
dent cancers, the standardized incidence ratio (SIR, referred to in the text plasma cell lymphomas.
㛳No. of patients refers to numbers in the treatment categories at the end of
as relative risk [RR]) was calculated with likelihood-based 95% CI from follow-up; person-years refer to time accumulated when in these categories
Poisson models.26 Absolute excess risks of second cancer were calculated (individuals could contribute to more than one category).
by subtracting the expected from the observed number of cases and divid-
ing by the person-years at risk. Cumulative (actuarial) probabilities of
second cancer were calculated by the Kaplan-Meier method.27 Tests for
trend and heterogeneity were calculated as described in Breslow and Day.28
All significance levels cited are two-sided. mon forms of chemotherapy were CHOP, received by 1,219 patients
(mean age, 46 years; 61% male, mainly treated from 1980 to 1994) and
chlorambucil, received by 752 patients (mean age, 48 years; 54% male,
RESULTS
mainly treated from 1973 to 1989).
During follow-up, 123 patients (5.0%) developed a second ma-
The cohort consisted of 2,456 patients (Table 1), 58% (n ⫽ 1,413) of lignancy, 1,230 others died, seven emigrated, 37 patients (1.5%) were
whom were male. The average age at first treatment was 46.5 years lost to follow-up in other ways, and the remaining 1,059 patients
(range, 3 to 59 years), with more than a third of the cohort (n ⫽ 932) survived without second cancer to the end of the study period. No
younger than 45 years. The mean age at first treatment was not signif- patients developed a third primary cancer during the follow-up pe-
icantly different between calendar periods of the study (P ⫽ .20). The riod. Total follow-up was 18,430 person-years, a mean of 7.7 years
majority of patients were treated with chemotherapy, either alone (maximum 26.8 years) per cohort member. The mean length of
(52%) or in combination with radiotherapy (35%). The most com- follow-up was slightly longer for those patients who were younger
www.jco.org 1569
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Mudie et al
when first diagnosed with NHL than those who were older, ranging nosed with stage III disease (RR ⫽ 9.4; 95% CI, 2.6 to 24.1) and
from 8.4 years for those younger than 45 years to 6.8 years for those stage IV disease (RR ⫽ 18.7; 95% CI, 9.0 to 34.4; data not shown).
patients ages 55 to 59 years (data not shown). This trend was not apparent for all malignancies overall or for any
The risk of second malignancy overall was significantly increased individual solid cancer sites.
(RR ⫽ 1.3; 95% CI, 1.1 to 1.6; P ⬍ .01; Table 2). The risks of lung The relative risk of malignancy overall was raised for each histo-
cancer (RR ⫽ 1.6; 95% CI, 1.1 to 2.3) and leukemia (RR ⫽ 8.8; 95% logic subtype of NHL, although it was significant for only the most
CI, 5.1 to 14.1) were also significantly raised. The risks of several common type, diffuse large cell NHL (RR ⫽ 1.4; 95%CI, 1.0 to 1.8;
gastrointestinal and genitourinary cancers, bone and soft tissue can- data not shown). Similarly, the risk of leukemia was raised for each
cers, and Hodgkin’s disease were also raised, albeit not significantly. histologic subtype, and was raised significantly for follicular NHL
Lung cancer and leukemia were the main contributors to the raised (RR ⫽ 10.4; 95% CI, 4.5 to 20.5), lymphocytic NHL (RR ⫽ 19.5; 95%
absolute excess risk. Five of the cases of lung cancer were squamous CI, 4.0 to 56.9), and diffuse NHL (RR ⫽ 6.2; 95% CI, 2.0 to 14.5).
cell, three were adenocarcinoma, two were oat/small cell, one was The relative risk of second cancer overall diminished with in-
hurtle cell, one was non–small-cell, four were poorly differentiated creasing age at first treatment (Ptrend ⬍ .05; Table 3), and significant
carcinomas, and 12 were of unknown histology. diminution of relative risk with age was also apparent for cancers of the
The raised risk of second cancers overall was confined to men mouth and pharynx, stomach (data not shown), and bladder and
(RR ⫽ 1.6, 95% CI, 1.3 to 2.0 for men; RR ⫽ 1.0, 95% CI, 0.7 to 1.3 for urethra. For second cancers overall, absolute excess risk per 10,000
women; Pheterogeneity [lt] .05). There were significantly increased risks person-years (AER) diminished with age, though the opposite was
in men for leukemia (RR ⫽ 9.7; 95% CI, 5.0 to 16.9) and oropharyn- true for lung and colorectal cancers and leukemia. Breast cancer risk
geal cancer (RR ⫽ 3.6; 95% CI, 1.2 to 8.3; data not shown). Significant was significantly reduced in women first treated at ages 45 to 54 years,
raised risks of leukemia (RR ⫽ 7.2; 95% CI, 2.3 to 16.8) and soft tissue but not for those women who were younger or older than this range.
cancer (RR ⫽ 10.4; 95% CI, 1.3 to 36.5) occurred in women. The risk of second malignancies overall was raised up to 15 years
Relative risk of leukemia increased with stage of NHL at from diagnosis, but not thereafter, although with wide confidence
diagnosis (Ptrend ⬍ .05) and was only significant in patients diag- intervals (Table 4). The relative risk of leukemia was elevated during
Table 2. Risks of Second Primary Malignancy by Site
Absolute Excess
No. of Risk per 10,000
ICD9 Code Site Cases SIR 95% CI Person-Years
141-149 Mouth and pharynx 5 2.6 0.8 to 6.0 1.7
150 Esophagus 2 0.8 0.1 to 3.0 ⫺0.2
151 Stomach 6 1.5 0.6 to 3.3 1.1
153 Colon 10 1.4 0.7 to 2.6 1.6
154 Rectum 7 1.4 0.6 to 2.9 1.1
157 Pancreas 4 1.6 0.4 to 4.2 0.8
162 Lung 28 1.6ⴱ 1.1 to 2.3 5.8
170 Bone 1 6.8 0.2 to 37.9 0.5
171 Soft tissue 2 4.1 0.5 to 14.7 0.8
172 Melanoma 3 1.4 0.3 to 4.0 0.4
174 Breast (female) 11 0.7 0.3 to 1.2 ⫺5.9
179, 182 Corpus uteri 0 0.0 0.0 to 1.6 ⫺2.9
180 Cervix 2 1.2 0.1 to 4.3 0.4
183 Ovary 1 0.4 0.01 to 2.0 ⫺2.2
185 Prostate 3 0.6 0.1 to 1.6 ⫺2.3
188, 189.3-189.9 Bladder and urethra 8 1.6 0.7 to 3.2 1.7
189.0-189.2 Kidney and ureter 3 1.3 0.3 to 3.8 0.4
191-192, 225.0-225.9, 237.5, 237.6, 237.9, 239.6 Nervous system 3 1.0 0.2 to 3.0 0.3
196-199 Unspecified primary 2 0.4 0.1 to 1.5 ⫺1.5
201 Hodgkin’s disease 2 4.2 0.5 to 15.2 0.8
203 Myeloma 1 0.9 0.0 to 4.8 ⫺0.1
204-208 Leukemia 17 8.8† 5.1 to 14.1 8.2
205 Acute myeloid leukemia‡ 9 13.1† 6.0 to 24.9 4.5
140-172, 174-199 All solid cancers except nmsc§ 103 1.1 0.9 to 1.4 6.5
140-172,174-199, 201, 203-208 All malignancies, except nmsc and NHL§ 123 1.3㛳 1.1 to 1.6 15.4
Abbreviations: SIR, standardized incidence ratio; ICD9, International Classification of Diseases 9th Edition; nmsc, non-melanoma skin cancer; NHL,
non-Hodgkin’s lymphoma.
ⴱ
P ⬍ .05.
†P ⬍ .001.
‡Other leukemias were: four cases acute lymphoid leukemia, one case lymphoblastic leukemia of unspecified chronicity, one case chronic myeloid leukemia,
one case acute leukemia of unspecified type, and one case leukemia not further specified.
§Including, in addition to the cancers detailed above, one cancer of the pleura and one cancer of the testis.
㛳P ⬍ .01.
1570 JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Second Cancer After Non-Hodgkin’s Lymphoma
Table 3. Relative Risks of Second Primary Malignancy of Selected Sites, by Age at First Treatment
Age (years)
⬍ 45 45-54 55-59
No. of No. of No. of
Cancer Site Cases SIR 95% CI AER Cases SIR 95% CI AER Cases SIR 95% CI AER
Mouth and pharynx 4 10.2ⴱ 2.8 to 26.2 4.7 1 1.1 0.03 to 6.2 0.2 0 0.0 0.0 to 5.6† ⫺1.7
Colon and rectum 2 1.4 0.2 to 4.9 0.7 8 1.5 0.7 to 3.0 4.0 7 1.3 0.5 to 2.8 4.6
Lung 1 0.6 0.02 to 3.6 ⫺0.7 13 1.7 0.9 to 3.0 8.1 14 1.7 0.9 to 2.9 14.8
Breast (female) 5 1.1 0.4 to 2.6 0.7 1 0.1‡ 0.004 to 0.8 ⫺8.5 5 1.1 0.3 to 2.5 0.8
Bladder and urethra 2 4.0 0.5 to 14.3 2.0 5 2.3 0.7 to 5.4 4.1 1 0.4 0.01 to 2.4§ ⫺3.3
Leukemia 5 14.4㛳 4.7 to 33.7 6.1 7 8.6㛳 3.4 to 17.6 9.0 5 6.5ⴱ 2.1 to 15.2 10.8
All solid cancers except nmsc 24 1.6‡ 1.0 to 2.4 12.0 45 1.1 0.8 to 1.5 8.2 34 0.9 0.6 to 1.3§ ⫺7.2
All malignancies except nmsc 30 1.9㛳 1.3 to 2.8 18.9 53 1.3 1.0 to 1.7 16.2 40 1.1 0.8 to 1.5§ 7.1
and NHL
Abbreviations: SIR, standardized incidence ratio; AER, Absolute excess risk per 10,000 person-years; nmsc, non-melanoma skin cancer; NHL, non-Hodgkin’s lymphoma.
ⴱ
P ⬍ .01.
†Ptrend ⬍ .01.
‡P ⬍ .05.
§Ptrend ⬍ .05.
㛳P ⬍ .001.
the first 10 years of follow-up, but then diminished, and no cases of significantly only in the chemotherapy-treated group (RR ⫽ 2.1; 95%
leukemia were diagnosed beyond 15 years. The relative risk of lung CI, 1.1 to 3.6), particularly in those patients who were treated with
cancer was raised significantly only during the period 5 to 9 years CHOP (RR ⫽ 2.4; 95% CI, 1.1 to 4.3), but not those treated with
following first treatment. chlorambucil (RR ⫽ 1.4; 95% CI, 0.5 to 3.2).
Relative risk of second malignancies overall was raised for each Risk of female breast cancer was significantly reduced (P ⬍ .01)
treatment modality (Table 5), but not significantly. Significantly in- in the chemotherapy-only group. Risk of lung cancer was significantly
creased risk of leukemia was confined to patients who had received increased (P ⬍ .05) in patients treated with only radiotherapy (nine
chemotherapy, with or without radiotherapy. No cases of leukemia cases, seven of whom received radiotherapy above and two below the
were observed in patients treated with radiotherapy only. The relative diaphragm). The risk was also increased in those patients treated with
risk of leukemia in the patients who were treated with CHOP was 14.2 only chemotherapy, but based on small numbers it was not increased
(95% CI, 6.8 to 26.2) and in the RR for those treated with chlorambucil in those with mixed-modality treatment (three cases, for whom site of
was 19.2 (95% CI, 9.6 to 34.3; data not shown). radiotherapy is not known). The relative risk of lung cancer was
The relative risk of mouth and pharynx cancers was significantly significantly raised in the CHOP subcohort (RR ⫽ 2.1; 95% CI, 1.1 to
increased in patients treated with mixed modalities and not signifi- 3.7), but not in those patients treated with chlorambucil (RR ⫽ 1.1;
cantly after radiotherapy alone. Risk of colorectal cancer was increased 95% CI, 0.4 to 2.4). The risk of bladder and urethra cancers was
Table 4. Relative Risks of Second Primary Malignancy of Selected Sites, by Time Since First Treatment
Time Since First Treatment (years)
⬍5 5-9 10-14 ⱖ 15
No. of No. of No. of No. of
Cancer Site Cases SIR 95% CI Cases SIR 95% CI Cases SIR 95% CI Cases SIR 95% CI
ⴱ
Mouth and pharynx 1 1.4 0.03 to 7.7 2 3.3 0.4 to 11.8 0 0.0 0.0 to 9.9 2 8.6 1.0 to 31.2
Colon and rectum 6 1.6 0.6 to 3.6 3 0.8 0.2 to 2.5 4 1.5 0.4 to 3.9 4 1.9 0.5 to 5.0
Lung 9 1.6 0.7 to 3.0 11 2.1ⴱ 1.1 to 3.8 6 1.6 0.6 to 3.5 2 0.7 0.1 to 2.7
Breast (female) 2 0.3 0.04 to 1.2 3 0.6 0.1 to 1.8 4 1.3 0.4 to 3.3 2 1.0 0.1 to 3.7
Bladder and urethra 1 0.6 0.02 to 3.5 2 1.3 0.2 to 4.9 3 2.8 0.6 to 8.1 2 2.4 0.3 to 8.7
Leukemia† 9 14.0‡ 6.4 to 26.6 6 10.4‡ 3.8 to 22.7 2 5.0 0.6 to 17.9 0 0.0 0.0 to 11.9§
All solid cancers except nmsc㛳 27 0.9 0.6 to 1.3 34 1.2 0.9 to 1.7 27 1.4 0.9 to 2.1 15 1.1 0.6 to 1.8
All malignancies except nmsc 38 1.2 0.9 to 1.6 41 1.4ⴱ 1.0 to 2.0 29 1.5 1.0 to 2.1 15 1.0 0.6 to 1.7
and NHL¶
Abbreviations: SIR, standardized incidence ratio; nmsc, non-melanoma skin cancer; NHL, non-Hodgkin’s lymphoma; AER, absolute excess risks per 10,000
person-years.
ⴱ
P ⬍ .05.
†AERs: 9.6 for ⬍ 5 years, 9.7 for 5-9 years, 5.9 for 10-14 years, and ⫺2.2 for ⱖ 15 years.
‡P ⬍ .001.
§Ptrend ⫽ .01.
㛳AERs: ⫺3.9 for ⬍ 5 years, 12.0 for 5-9 years, 6.3 for 10-14 years, and 6.3 for ⱖ 15 years.
¶AERs: 7.3 for ⬍ 5 years, 22.6 for 5-9 years, 33.6 for 10-14 years, and 2.4 for ⱖ 15 years.
www.jco.org 1571
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Mudie et al
Table 5. Relative Risks of Second Primary Malignancy of Selected Sites, by Treatment Modality
Chemotherapy Mixed Modalities Radiotherapy
No. of No. of No. of
Cancer Site Cases SIR 95% CI Cases SIR 95% CI Cases SIR 95% CI
ⴱ
Mouth and pharynx 0 0.0 0.0 to 3.8 3 5.7 1.2 to 16.6 2 4.6 0.6 to 16.5
Colon and rectum 12 2.1ⴱ 1.1 to 3.6 5 1.5 0.5 to 3.5 0 0.0 0.0 to 1.3
Lung 16 1.9ⴱ 1.1 to 3.1 3 0.6 0.1 to 1.7 9 2.3ⴱ 1.1 to 4.5
Breast (female) 1 0.12† 0.003 to 0.7 7 1.7 0.7 to 3.6 3 0.8 0.2 to 2.4
Bladder and urethra 3 1.2 0.3 to 3.6 0 0.0 0.0 to 2.6 5 4.5ⴱ 1.5 to 10.4
Leukemia 10 10.5‡ 5.0 to 19.3 7 13.0‡ 5.2 to 26.7 0 0.0 0.0 to 8.3
All solid cancers except nmsc 46 1.0 0.7 to 1.4 30 1.2 0.8 to 1.7 27 1.3 0.9 to 1.9
All malignancies except nmsc 58 1.3 0.9 to 1.6 37 1.4 1.0 to 2.0 28 1.3 0.9 to 2.0
and NHL
Abbreviations: SIR, standardized incidence ratio; nmsc, non-melanoma skin cancer; NHL, non-Hodgkin’s lymphoma.
ⴱ
P ⬍ .05.
†P ⬍ .01.
‡P ⬍ .001.
significantly raised only after radiation treatment (five cases, of ence in relative risk of malignancy overall between NHL patients aged
whom two received radiotherapy below and two above the dia- younger and older than 40 years at diagnosis, whereas a Swedish
phragm, and for one patient the site of radiotherapy was un- study9 found greater relative risks at younger ages. Similar to the
known). All three cases of bladder and urethra cancer among the Swedish study, we found that risk decreased significantly with increas-
chemotherapy-treated patients occurred within the CHOP subco- ing age at first treatment.
hort (RR ⫽ 1.7; 95% CI, 0.3 to 4.9). Long-term risk of second malignancy after NHL has been exam-
Overall, the risk of all malignancy was significantly raised in the ined previously by Travis et al,7 who found raised risks beyond 15 years
CHOP subcohort (RR ⫽ 1.6; 95% CI, 1.2 to 2.1), mainly due to the of follow-up. In this study, with a similar mean length of follow-up,
raised risks of leukemia, lung, and colorectal cancers. The risk of RRs of second malignancy were raised for the first 15 years, with no
second malignancy overall in the chlorambucil subcohort was border- evident raised risk thereafter. The 15-year cumulative risk of all second
line significantly raised (RR ⫽ 1.4; 95% CI, 1.0 to 1.9), primarily due to malignancies in our study was a little lower than the one found in the
the high risk of leukemia in this group. study by Travis et al7 (11% v 15%), probably reflecting the younger
The 15-year cumulative risk of second malignancy in the total mean age of our cohort (46.6 v 56.1 years).
cohort was 11.2% (95% CI, 9.1 to 13.7). Cumulative risks were Raised relative risks (two- to eight-fold) of leukemia among NHL
greater for males (13.6%; 95% CI, 10.5 to 17.5) than females (8.3%; patients have been demonstrated previously in adult cohort
95% CI, 5.8 to 11.3), and were much greater in patients who were first studies.6,7,9,11-13 The relative risk was even greater (200-fold) in chil-
treated at 50 years of age and older (17.5%; 95% CI, 13.6 to 22.3) than dren.23 High relative risks have been linked to alkylating chemother-
for those who were treated at a younger age (7%; 95% CI, 5.0 to 9.9).
apy, including chlorambucil and cyclophosphamide specifically,17
The main contributors to the overall 15-year risk were lung cancer
which were associated with raised risk in our data, and have been
(2.8%), leukemia (1.5%), colorectal cancer (1.5%), and breast cancer
shown to be leukemogenic when used to treat Hodgkin’s disease and
(1.2%; data not shown).
other malignancies.30-32 Involved-field radiation treatment did not
materially increase the risk of leukemia in previous studies of patients
DISCUSSION treated for NHL12,17 and Hodgkin’s disease,4,32other than the risk
conferred by alkylating chemotherapy, but low-dose total-body irra-
This cohort of British NHL patients had a 30% higher rate of second diation did.15-18,33,34 In our study, radiotherapy-treated patients pre-
malignancy than in the general population of England and Wales, dominantly received involved-field treatments, and no cases of
primarily due to elevated risks of leukemia and lung cancer. The leukemia occurred in the group treatedwith radiation only. The rela-
results may have been biased slightly upwards, because cancer regis- tive risks of leukemia were similarly raised in the chemotherapy- and
tration in England and Wales is only approximately 90% complete,1 mixed-modality–treated groups. The high relative risk of leukemia
however, the results are comparable to the raised risks of 18% to 37% seen after CHOP and chlorambucil chemotherapies is of a similar
in other large cohort studies.5-9 Also similar to previous reports among order of magnitude to the risks observed following treatment with
NHL patients,5-7 the raised relative risk was greater in male than alkylating regimens such as MOPP (mechlorethamine, vincristine,
female patients. Only a few studies have examined age at first treat- procarbazine, prednisone) in Hodgkin’s disease patients.4
ment in relation to risk of second malignancy following NHL, and the As in previous reports,15-17 we found that patients who presented
evidence has been conflicting. An American study of childhood with advanced stages of NHL were more likely to develop leukemia.
NHL,23 based on 497 cases, reported a much higher relative risk of This reflects their treatment; it has been found that NHL stage was
malignancy overall (RR ⫽ 10.8; 95% CI, 6.1 to 16.9) than in adult not associated with leukemia after the risks were adjusted for the effect
cohorts, whereas a smaller Italian study29 of children with NHL re- of alkylating agents.17 The relative risk of leukemia in our study dimin-
ported no raised risk. An international cohort study7 found no differ- ished with patient age at first treatment, as has been observed after
1572 JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Second Cancer After Non-Hodgkin’s Lymphoma
chemotherapy for Hodgkin’s disease.24 As is usual in chemotherapy- following chemotherapy, specifically CHOP. To our knowledge, the
induced leukemia,34 including leukemia after NHL,7 the risk of leuke- risk of colorectal cancer following chemotherapy in NHL has not been
mia was raised significantly during the 10 years after first treatment, reported before. A multicenter study of second malignancy after
and then diminished. Hodgkin’s disease showed a large significant risk of digestive and
In a large case-control study of bladder cancer after NHL, peritoneal cancers following treatment with doxorubicin (RR ⫽ 23),
Travis et al21 demonstrated that risk of this cancer is strongly which is part of the CHOP regimen, but did not report the specific
associated with cumulative dose of cyclophosphamide, with the cancer sites associated with this treatment.39 Two components of
lowest doses (up to 20g) having a nonsignificant two-fold in- CHOP, namely cyclophosphamide and doxorubicin, have been
creased risk. In this cohort, we found a not significantly increased shown to cause solid tumors in rodent models.40 The risk of colorectal
risk of bladder cancer in patients treated with CHOP, who were cancer in relation to chemotherapy for NHL, specifically CHOP,
generally administered between 6 to 9 cycles of treatment with no needs further investigation.
long-term maintenance, which would give a cumulative cyclophosph- Several NHL cohort studies have noted a reduction in breast
amide dose of about 20g or less. We observed a significantly raised risk cancer risk,6-9,14 though only two studies found the diminution to
of bladder cancer in the radiotherapy-only treated group, in accor- be statistically significant.6,9 Where examined, no significant rela-
dance with the elevated bladder cancer risks shown in radiotherapy- tion was found to any specific type of treatment.6,12,14 We found a
treated NHL patients6 and other radiation-exposed cohorts.35,36 significant diminution of risk for women treated with chemother-
Several studies have shown lung cancer as the most common apy. A significantly reduced risk of breast cancer has been shown
second malignancy among NHL patients, with risks raised by 36% to repeatedly in Hodgkin’s disease patients treated with alkylating
90%.5-7 We found a 60% raised risk of this cancer, and a significantly chemotherapy; the effect was greater with an increasing number of
raised risk after radiotherapy. Although previous studies6,12 of NHL cycles, and related to premature menopause as a consequence of
patients have not found a significantly increased risk of lung cancer treatment.34 Drugs used to treat NHL are capable of causing pre-
following radiation treatment, it is well established that exposure to mature menopause. Ovarian failure following treatment with cy-
ionizing radiation can increase the risk of lung cancer.36 We do not clophosphamide is well documented, with most studies showing a
have comprehensive data on field of radiotherapy for the overall linear correlation between cumulative dose of cyclophosphamide
cohort, and an additional limitation of our study is that data on and reduction in age at menopause.41 It may therefore be the case
smoking was also unavailable. that for NHL, as for Hodgkin’s disease, chemotherapy can cause
Raised risks of lung cancer after chemotherapy for NHL have reduced breast cancer risk via induction of premature menopause.
been demonstrated in one US cohort,6 but not in another.12 A recent Significantly reduced risk of endometrial malignancy (RR ⫽ 0.51)
French study14 found a significantly raised risk of this malignancy in was found in a recent Swedish study of NHL patients,9 and we also
men following the CHOP-like regimen ACVBP (doxorubicin, cyclo- noted a deficit, which might perhaps relate to treatment-induced
phosphamide, vindesine, bleomycin, prednisone). Raised risks of lung premature menopause.
cancer have also been seen after alkylating chemotherapy for In conclusion, long-term follow-up of this cohort of British
Hodgkin’s disease.37,38 Risk of lung cancer in our cohort was signifi- NHL patients treated under the age of 60 years revealed an in-
cantly elevated after CHOP but was not evident in chlorambucil- creased risk of second malignancy, with a 15-year cumulative prob-
treated patients. This warrants more detailed investigation, which we ability of 11.2%. After chemotherapy there was an elevated risk of
plan to do with a nested case-control approach. leukemia, as would be expected, but also of lung and colorectal
Modest nonsignificant increases in the risk of colorectal cancer cancers and there was a diminution of the risk of breast cancer.
after NHL have been observed in some previous studies,6-8 but not all.9 These potential effects of treatment need to be taken into account
In our study, the raised risk was only statistically significant when during clinical follow-up.
6. Travis LB, Curtis RE, Boice JD Jr, et al: 12. Lavey RS, Eby NL, Prosnitz LR: Impact on
REFERENCES Second cancers following non-Hodgkin’s lym- second malignancy risk of the combined use of
phoma. Cancer 67:2002-2009, 1991 radiation and chemotherapy for lymphomas. Cancer
1. Swerdlow AJ, dos Santos Silva I, Doll R: 7. Travis LB, Curtis RE, Glimelius B, et al: Sec- 66:80-88, 1990
Cancer incidence and mortality in England and ond cancers among long-term survivors of non- 13. Lishner M, Slingerland J, Barr J, et al: Second
Wales: Trends and risk factors. Oxford, United King- Hodgkin’s lymphoma. J Natl Cancer Inst 85:1932- malignant neoplasms in patients with non-Hodgkin’s
dom, Oxford University Press, 2001 1937, 1993 lymphoma. Hematol Oncol 9:169-179, 1991
2. Swerdlow AJ: Epidemiology of Hodgkin’s dis- 8. Brennan P, Coates M, Armstrong B, et al: 14. Andre M, Mounier N, Leleu X, et al: Second
ease and non-Hodgkin’s lymphoma. Eur J Nucl Med Second primary neoplasms following non-Hodgkin’s cancers and late toxicities after treatment of aggres-
Mol Imaging 30:S3-S12, 2003 (suppl 1) lymphoma in New South Wales, Australia. Br J sive non-Hodgkin lymphoma with the ACVBP regi-
3. National Cancer Institute: SEER Cancer Sta- Cancer 82:1344-1347, 2000 men: A GELA cohort study on 2837 patients. Blood
tistics Review, 1975-2001. http://seer.cancer.gov/ 9. Dong C, Hemminki K: Second primary neo- 103:1222-1228, 2004
csr/1975_2001/ plasms among 53 159 haematolymphoprolifera- 15. Greene MH, Young RC, Merrill JM, et al:
4. Swerdlow AJ, Van Leeuwen FE: Late effects tive malignancy patients in Sweden, 1958-1996: A Evidence of a treatment dose response in acute
after treatment for Hodgkin lymphoma, in Dembo search for common mechanisms. Br J Cancer nonlymphocytic leukemias which occur after ther-
AJ, Linch DC, Lowenberg B (eds): Textbook of 85:997-1005, 2001 apy of non-Hodgkin’s lymphoma. Cancer Res 43:
Malignant Hematology. Abingdon, United Kingdom, 10. MacDougall BK, Weinerman BH, Kemel S: 1891-1898, 1983
Taylor & Francis, 2005, pp 753-768 Second malignancies in non-Hodgkin’s lymphoma. 16. Pedersen-Bjergaard J, Ersboll J, Sorensen
5. Greene MH, Wilson J: Second cancer fol- Cancer 48:1299-1301, 1981 HM, et al: Risk of acute nonlymphocytic leukemia
lowing lymphatic and hematopoietic cancers in 11. Storm HH, Prener A: Second cancer following and preleukemia in patients treated with cyclophos-
Connecticut, 1935-82. Natl Cancer Inst Monogr lymphatic and hematopoietic cancers in Denmark, phamide for non-Hodgkin’s lymphomas: Compari-
68:191-217, 1985 1943-80. Natl Cancer Inst Monogr 68:389-409, 1985 son with results obtained in patients treated for
www.jco.org 1573
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Mudie et al
Hodgkin’s disease and ovarian carcinoma with other 25. World Health Organisation.Manual of the In- cer: Principles and Practice of Oncology. Philadel-
alkylating agents. Ann Intern Med 103:195-200, ternational Statistical Classification of Diseases, In- phia, PA, Lippincott Williams & Wilkins, 2005, pp
1985 juries, and Causes of Death (ed 9). Geneva, 2575-2602
17. Travis LB, Curtis RE, Stovall M, et al: Risk of Switzerland, World Health Organisation, 1978 35. Boice JD Jr, Land CE, Preston DL: Ionizing
leukemia following treatment for non-Hodgkin’s 26. Clayton D, Hills M: Statistical Models in Epi- radiation, in Schottenfeld D, Fraumeni JF Jr (eds):
lymphoma. J Natl Cancer Inst 86:1450-1457, 1994 demiology. Oxford, Oxford University Press, 1993 Cancer Epidemiology and Prevention. New York,
18. Travis LB, Weeks J, Curtis RE, et al: Leukemia 27. Kaplan E, Meier P: Non-parametric estimation NY, Oxford University Press, 1996, pp 319-354
following low-dose total body irradiation and chemo- from incomplete observations. J Am Stat Assoc 36. UNSCEAR: Sources and effects of ionizing
therapy for non-Hodgkin’s lymphoma. J Clin Oncol 53:457-481, 1958 radiation. UNSCEAR 2000 Report to the General
14:565-571, 1996 28. Breslow N, Day N: Statistical methods in Assembly, with scientific annexes. New York, NY,
19. Hosing C, Munsell M, Yazji S, et al: Risk of cancer research. Lyon, France, International Agency United Nations, 2000
therapy-related myelodysplastic syndrome/acute leuke- for Research on Cancer, 1987 37. Swerdlow AJ, Schoemaker MJ, Allerton R, et
mia following high-dose therapy and autologous bone 29. Pillon M, Di Tullio MT, Garaventa A, et al:
al: Lung cancer after Hodgkin’s disease: A nested
marrow transplantation for non-Hodgkin’s lymphoma. Long-term results of the first Italian Association of
case-control study of the relation to treatment. J Clin
Ann Oncol 13:450-459, 2002 Pediatric Hematology and Oncology protocol for the
Oncol 19:1610-1618, 2001
20. Pedersen-Bjergaard J, Ersboll J, Hansen VL, treatment of pediatric B-cell non-Hodgkin lymphoma
38. Travis LB, Gospodarowicz M, Curtis RE, et al:
et al: Carcinoma of the urinary bladder after treat- (AIEOP LNH92). Cancer 101:385-394, 2004
Lung cancer following chemotherapy and radiother-
ment with cyclophosphamide for non-Hodgkin’s 30. Haas JF, Kittelmann B, Mehnert WH, et al: Risk of
apy for Hodgkin’s disease. J Natl Cancer Inst 94:
lymphoma. N Engl J Med 318:1028-1032, 1988 leukaemia in ovarian tumour and breast cancer patients
182-192, 2002
21. Travis LB, Curtis RE, Glimelius B, et al: Blad- following treatment by cyclophosphamide. Br J Cancer
der and kidney cancer following cyclophosphamide 55:213-218, 1987 39. Boivin JF, Hutchison GB, Zauber AG, et al:
therapy for non-Hodgkin’s lymphoma. J Natl Cancer 31. Kaldor JM, Day NE, Pettersson F, et al: Leu- Incidence of second cancers in patients treated for
Inst 87:524-530, 1995 kemia following chemotherapy for ovarian cancer. Hodgkin’s disease. J Natl Cancer Inst 87:732-741,
22. Travis LB, Gonzalez CL, Hankey BF, et al: N Engl J Med 322:1-6, 1990 1995
Hodgkin’s disease following non-Hodgkin’s lym- 32. Kaldor JM, Day NE, Clarke EA, et al: Leukemia 40. IARC working group on the evaluation of
phoma. Cancer 69:2337-2342, 1992 following Hodgkin’s disease. N Engl J Med 322:7- carcinogenic risks to humans: Overall evaluation of
23. Leung W, Sandlund JT, Hudson MM, et al: Sec- 13, 1990 carcinogenicity: An updating of IARC Monographs
ond malignancy after treatment of childhood non- 33. Gomez GA, Aggarwal KK, Han T: Post-therapeutic volumes 1-42. Lyon, France, IARC, 1987
Hodgkin lymphoma. Cancer 92:1959-1966, 2001 acute malignant myeloproliferative syndrome and acute 41. Meistrich ML, Vassilopoulou-Sellin R, Lipshultz LI:
24. Swerdlow AJ, Barber JA, Hudson GV, et al: nonlymphocytic leukemia in non-Hodgkin’s lymphoma. Gonadal disfunction, in DeVita VT, Hellman S, Rosenberg
Risk of second malignancy after Hodgkin’s disease Cancer 50:2285-2288, 1982 SA (eds): Cancer: Principles and Practice of Oncolgy.
in a collaborative British cohort: The relation to age 34. Van Leeuwen FE, Travis LB: Second cancers, Philadelphia, PA, Lippincott Williams & Wilkins, 2005, pp
at treatment. J Clin Oncol 18:498-509, 2000 in DeVita VT, Hellman S, Rosenberg SA (eds): Can- 2560-2574
■ ■ ■
Acknowledgment
We thank the collaborators at the British National Lymphoma Investigation (BNLI) whose patients are included in this cohort.
Authors’ Disclosures of Potential Conflicts of Interest
Although all authors completed the disclosure declaration, the following author or immediate family members indicated a financial interest. No conflict exists for drugs
or devices used in a study if they are not being evaluated as part of the investigation. For a detailed description of the disclosure categories, or for more information about
ASCO’s conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Authors Employment Leadership Consultant Stock Honoraria Research Funds Testimony Other
Anthony J. Swerdlow GlaxoSmithKline (A)
Dollar Amount Codes (A) ⬍ $10,000 (B) $10,000-99,999 (C) ⱖ $100,000 (N/R) Not Required
Author Contributions
Conception and design: Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins
Administrative support: Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins, Zongkai Qiao
Provision of study materials or patients: Barry W. Hancock, Peter J. Hoskin, David C. Linch
Collection and assembly of data: Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins, Paul Smith, Zongkai Qiao, David C. Linch
Data analysis and interpretation: Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins
Manuscript writing: Nadejda Y. Mudie, Anthony J. Swerdlow, David C. Linch
Final approval of manuscript: Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins, Paul Smith, Zongkai Qiao, Barry W. Hancock, Peter J. Hoskin,
David C. Linch
Other: Anthony J. Swerdlow [Grant application], David C. Linch [Grant application]
1574 JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
JOURNAL OF CLINICAL ONCOLOGY
Official Journal of the American Society of Clinical Oncology
Vol 24, No 10 C O N T E N T S April 1, 2006
Editorials
Promise of New Vascular-Disrupting Agents Balanced With Cardiac Toxicity: Is It Time
for Oncologists to Get to Know Their Cardiologists?
Willem J. van Heeckeren, Shyam Bhakta, Jose Ortiz, Jeff Duerk, Matthew M. Cooney, Afshin Dowlati,
Keith McCrae, and Scot C. Remick (see article on page 1491) ................................................................................................................... 1485
Developing a New Framework for Dose Calculation
Howard Gurney (see article on page 1499) ............................................................................................................................................................... 1489
Original Reports
PHASE I AND CLINICAL PHARMACOLOGY
Phase I Clinical Evaluation of Weekly Administration of the Novel Vascular-Targeting
Agent, ZD6126, in Patients With Solid Tumors
Laurens V. Beerepoot, Sandra A. Radema, Els O. Witteveen, Tawnie Thomas, Catherine Wheeler,
Sanford Kempin, and Emile E. Voest (see editorial on page 1485) ......................................................................................................... 1491
Evaluation of an Alternate Dosing Strategy for Cisplatin in Patients With Extreme Body
Surface Area Values
Walter J. Loos, Felix E. de Jongh, Alex Sparreboom, Ronald de Wit, Desiree M. van Boven-van Zomeren,
Gerrit Stoter, Kees Nooter, and Jaap Verweij (see editorial on page 1489) ..................................................................................... 1499
PEDIATRIC ONCOLOGY
High WT1 Expression After Induction Therapy Predicts High Risk of Relapse and Death
in Pediatric Acute Myeloid Leukemia
Hélène Lapillonne, Aline Renneville, Anne Auvrignon, Cyril Flamant, Annick Blaise, Christine Perot,
Jean-Luc Lai, Paola Ballerini, Françoise Mazingue, Sylvie Fasola, Axelle Dehée, Françoise Bellman,
Mircéa Adam, Myriam Labopin, Luc Douay, Guy Leverger, Claude Preudhomme,
and Judith Landman-Parker .................................................................................................................................................................................................. 1507
White Race As a Risk Factor for Hypothyroidism After Treatment for Pediatric
Hodgkin’s Lymphoma
Monika L. Metzger, Melissa M. Hudson, Grant W. Somes, Ron I. Shorr, Chin-Shang Li, Matthew J. Krasin,
John Shelso, Ching-Hon Pui, and Scott C. Howard ............................................................................................................................................ 1516
(continued on following page)
Journal of Clinical Oncology (ISSN 0732-183X) is published 36 times a year, three times monthly, by American Society of Clinical Oncology, 1900 Duke St, Suite 200, Alexandria,
VA 22314. Periodicals postage is paid at Alexandria, VA, and at additional mailing offices. Publication Mail Agreement Number 863289.
Editorial correspondence should be addressed to Daniel G. Haller, MD, Journal of Clinical Oncology, 330 John Carlyle St, Suite 300, Alexandria, VA 22314. Telephone: (703)
797-1900; Fax: (703) 684-8720. E-mail: jco@asco.org. Internet: www.jco.org.
POSTMASTER: ASCO members send change of address to American Society of Clinical Oncology, 1900 Duke St, Suite 200, Alexandria, VA 22314. Nonmembers send change
of address to Journal of Clinical Oncology Customer Service, 330 John Carlyle St, Suite 300, Alexandria, VA 22314.
2006 annual subscription rates, effective September 1, 2005: United States and possessions: individual, $435; single issue, $35. International: individual, $605; single issue, $45.
Institutions: Tier 1: $615 US, $870 Int’l; Tier 2: $715 US, $970 Int’l; Tier 3: $1,035 US, $1,290 Int’l; Tier 4: $1,140 US, $1,395 Int’l; Tier 5: contact JCO for a quote. See
http://www.jco.org/subscriptions/tieredpricing.shtml for descriptions of each tier. Student and resident: United States and possessions: $215; all other countries, $300. To receive
student/resident rate, orders must be accompanied by name of affiliated institution, date of term, and the signature of program/residency coordinator on institution letterhead.
Orders will be billed at individual rate until proof of status is received. Current prices are in effect for back volumes and back issues. Back issues sold in conjunction with a
subscription rate are on a prorated basis. Subscriptions are accepted on a 12-month basis. Prices are subject to change without notice. Single issues, both current and back, exist in limited
quantities and are offered for sale subject to availability. JCO Legacy Archive (electronic back issues from January 1983 through December 1998) is also available; please inquire.
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Human Telomere Reverse Transcriptase Expression Predicts Progression and Survival in
Pediatric Intracranial Ependymoma
Uri Tabori, Jing Ma, Michael Carter, Maria Zielenska, James Rutka, Eric Bouffet, Ute Bartels, David Malkin,
and Cynthia Hawkins .................................................................................................................................................................................................................. 1522
Translocation Carcinomas of the Kidney After Chemotherapy in Childhood
Pedram Argani, Marick Laé, Edgar T. Ballard, Mahul Amin, Carlos Manivel, Brian Hutchinson,
Victor E. Reuter, and Marc Ladanyi ................................................................................................................................................................................. 1529
Skip Metastases in Osteosarcoma: Experience of the Cooperative Osteosarcoma
Study Group
Leo Kager, Andreas Zoubek, Ulrike Kastner, Beate Kempf-Bielack, Jenny Potratz, Rainer Kotz,
G. Ulrich Exner, Christiane Franzius, Susanna Lang, Rainer Maas, Heribert Jürgens, Helmut Gadner,
and Stefan Bielack ......................................................................................................................................................................................................................... 1535
Treatment Complications in Children Diagnosed With Neuroblastoma During a
Screening Program
Stéphane Barrette, Mark L. Bernstein, Jean-Marie Leclerc, Martin A. Champagne, Yvan Samson,
Josée Brossard, and William G. Woods ...................................................................................................................................................................... 1542
Association of High-Level MRP1 Expression With Poor Clinical Outcome in a Large
Prospective Study of Primary Neuroblastoma
Michelle Haber, Janice Smith, Sharon B. Bordow, Claudia Flemming, Susan L. Cohn, Wendy B. London,
Glenn M. Marshall, and Murray D. Norris .................................................................................................................................................................. 1546
Role of Radiotherapy in Supratentorial Primitive Neuroectodermal Tumor in Young
Children: Results of the German HIT-SKK87 and HIT-SKK92 Trials
Beate Timmermann, Rolf-Dieter Kortmann, Joachim Kühl, Stefan Rutkowski, Christof Meisner,
Torsten Pietsch, Frank Deinlein, Christian Urban, Monika Warmuth-Metz, and Michael Bamberg ............................. 1554
THORACIC ONCOLOGY
Phase I to II Study of Pleurectomy/Decortication and Intraoperative Intracavitary
Hyperthermic Cisplatin Lavage for Mesothelioma
William G. Richards, Lambros Zellos, Raphael Bueno, Michael T. Jaklitsch, Pasi A. Jänne,
Lucian R. Chirieac, Beow Y. Yeap, Rene J. Dekkers, Phillip M. Hartigan, Leah Capalbo,
and David J. Sugarbaker .......................................................................................................................................................................................................... 1561
EPIDEMIOLOGY
Risk of Second Malignancy After Non-Hodgkin’s Lymphoma: A British Cohort Study
Nadejda Y. Mudie, Anthony J. Swerdlow, Craig D. Higgins, Paul Smith, Zongkai Qiao, Barry W. Hancock,
Peter J. Hoskin, and David C. Linch ................................................................................................................................................................................ 1568
HEMATOLOGIC MALIGNANCIES
Pentostatin, Cyclophosphamide, and Rituximab Is an Active, Well-Tolerated Regimen
for Patients With Previously Treated Chronic Lymphocytic Leukemia
Nicole Lamanna, Matt Kalaycio, Peter Maslak, Joseph G. Jurcic, Mark Heaney, Renier Brentjens,
Andrew D. Zelenetz, Denise Horgan, Alison Gencarelli, Katherine S. Panageas, David A. Scheinberg,
and Mark A. Weiss ........................................................................................................................................................................................................................ 1575
Improvement of Overall and Failure-Free Survival in Stage IV Follicular Lymphoma: 25
Years of Treatment Experience at The University of Texas M.D. Anderson Cancer Center
Qi Liu, Luis Fayad, Fernando Cabanillas, Fredrick B. Hagemeister, Gregory D. Ayers, Mark Hess,
Jorge Romaguera, M. Alma Rodriguez, Apostolia M. Tsimberidou, Srdan Verstovsek, Anas Younes,
Barbara Pro, Ming-Sheng Lee, Ana Ayala, and Peter McLaughlin ......................................................................................................... 1582
(continued on following page)
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Phase III Intergroup Study of Fludarabine Phosphate Compared With
Cyclophosphamide, Vincristine, and Prednisone Chemotherapy in Newly Diagnosed
Patients With Stage III and IV Low-Grade Malignant Non-Hodgkin’s Lymphoma
Anton Hagenbeek, Houchingue Eghbali, Silvio Monfardini, Umberto Vitolo, Peter J. Hoskin,
Christiane de Wolf-Peeters, Ken MacLennan, Elvira Staab-Renner, Joachim Kalmus, Astrid Schott,
Ivana Teodorovic, Anastassia Negrouk, Martine van Glabbeke, and Robert Marcus .............................................................. 1590
Prospective Study of Survival Outcomes in Non-Hodgkin’s Lymphoma Patients With
Rheumatoid Arthritis
Ted R. Mikuls, Justin O. Endo, Susan E. Puumala, Patricia A. Aoun, Natalie A. Black, James R. O’Dell,
Julie A. Stoner, Eugene C. Boilesen, Martin A. Bast, Debra A. Bergman, Kay M. Ristow, Melissa Ooi,
James O. Armitage, and Thomas M. Habermann ............................................................................................................................................... 1597
GASTROINTESTINAL CANCER
Tumor Thymidylate Synthase 1494del6 Genotype As a Prognostic Factor in Colorectal
Cancer Patients Receiving Fluorouracil-Based Adjuvant Treatment
Emma Dotor, Miriam Cuatrecases, María Martínez-Iniesta, Matilde Navarro, Felip Vilardell, Elisabeth Guinó,
Laura Pareja, Agnés Figueras, David G. Molleví, Teresa Serrano, Javier de Oca, Miguel A. Peinado,
Víctor Moreno, Josep Ramón Germà, Gabriel Capellá, and Alberto Villanueva ......................................................................... 1603
Predictive Factors for Outcome in a Phase II Study of Gefitinib in Second-Line Treatment
of Advanced Esophageal Cancer Patients
Maarten L. Janmaat, Mariëlle I. Gallegos-Ruiz, José A. Rodriguez, Gerrit A. Meijer, Walter L. Vervenne,
Dick J. Richel, Cees Van Groeningen, and Giuseppe Giaccone ................................................................................................................ 1612
SUPPORTIVE CARE AND QUALITY OF LIFE
Randomized Trial of Peer Counseling on Reproductive Health in African American Breast
Cancer Survivors
Leslie R. Schover, Rosell Jenkins, Dawen Sui, Jennifer Harned Adams, Michelle S. Marion,
and Karen Eubanks Jackson ................................................................................................................................................................................................. 1620
NEUROONCOLOGY
Survival Prediction in Patients With Glioblastoma Multiforme by Human Telomerase
Genetic Variation
Luo Wang, Qingyi Wei, Li-E Wang, Kenneth D. Aldape, Yumei Cao, M. Fatih Okcu, Kenneth R. Hess,
Randa El-Zein, Mark R. Gilbert, Shiao Y. Woo, Sujit S. Prabhu, Greg N. Fuller, and Melissa L. Bondy .................... 1627
Review Article
Peripheral Neuropathy Induced by Microtubule-Stabilizing Agents
James J. Lee and Sandra M. Swain ................................................................................................................................................................................ 1633
Art of Oncology
Deliberate Deceit of Family Members: A Challenge to Providers of Clinical
Genetics Services
Jennifer T. Loud, Nancy E. Weissman, June A. Peters, Ruthann M. Giusti, Benjamin S. Wilfond,
Wylie Burke, and Mark H. Greene .................................................................................................................................................................................... 1643
(continued on following page)
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Correspondence
Chronic Eosinophilic Leukemia/Hypereosinophilic Syndrome and Acute Leukemia
Neil Abramson ................................................................................................................................................................................................................................. 1647
Errata .................................................................................................................................................................................................................................................... 1648
Also in This Issue
Announcements
Information for Contributors
Current Abstracts
Calendar of Oncology Events
Online supplementary information available at www.jco.org
Article was published online ahead of print at www.jco.org
www.jco.org www.asco.org
Downloaded from ascopubs.org by 106.199.123.120 on May 22, 2019 from 106.199.123.120
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Brandtzaeg 1981Document14 pagesBrandtzaeg 1981সোমনাথ মহাপাত্রNo ratings yet
- 1201020895PL IMillerDocument26 pages1201020895PL IMillerসোমনাথ মহাপাত্রNo ratings yet
- East Bank MapDocument1 pageEast Bank Mapসোমনাথ মহাপাত্রNo ratings yet
- CBT 15 1029Document13 pagesCBT 15 1029সোমনাথ মহাপাত্রNo ratings yet
- BD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood CellsDocument1 pageBD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood Cellsসোমনাথ মহাপাত্রNo ratings yet
- Chapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)Document27 pagesChapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)সোমনাথ মহাপাত্রNo ratings yet
- Account Statement As of 04-05-2020 19:48:27 GMT +0530Document11 pagesAccount Statement As of 04-05-2020 19:48:27 GMT +0530সোমনাথ মহাপাত্রNo ratings yet
- My OwnDocument1 pageMy Ownসোমনাথ মহাপাত্রNo ratings yet
- Result Sheet PDFDocument41 pagesResult Sheet PDFManohar ManuNo ratings yet
- Globalizarea Nimicului - RitzerDocument27 pagesGlobalizarea Nimicului - RitzerAlina PetreNo ratings yet
- Cell-Cell Interactions: Concept OutlineDocument18 pagesCell-Cell Interactions: Concept Outlineসোমনাথ মহাপাত্রNo ratings yet
- DHR-ICMR Workshop Funding ApplicationDocument3 pagesDHR-ICMR Workshop Funding Applicationসোমনাথ মহাপাত্রNo ratings yet
- 149 FullDocument10 pages149 Fullসোমনাথ মহাপাত্রNo ratings yet
- Immune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in AutoimmunityDocument176 pagesImmune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in Autoimmunityসোমনাথ মহাপাত্রNo ratings yet
- Icmr Talent FormDocument2 pagesIcmr Talent Formসোমনাথ মহাপাত্রNo ratings yet
- Chap1 - Units, Dimensions & Vectors PDFDocument61 pagesChap1 - Units, Dimensions & Vectors PDFসোমনাথ মহাপাত্রNo ratings yet
- DHR-ICMR Workshop Funding ApplicationDocument3 pagesDHR-ICMR Workshop Funding Applicationসোমনাথ মহাপাত্রNo ratings yet
- EBv Neg Epidemiology Leblond JCO.1998.16.6Document8 pagesEBv Neg Epidemiology Leblond JCO.1998.16.6সোমনাথ মহাপাত্রNo ratings yet
- Anxiety Disorders Treatment ProtocolDocument25 pagesAnxiety Disorders Treatment Protocolসোমনাথ মহাপাত্রNo ratings yet
- Five Content Areas and Percent of Scored Test Items (Range) in Each AreaDocument5 pagesFive Content Areas and Percent of Scored Test Items (Range) in Each Areaসোমনাথ মহাপাত্রNo ratings yet
- Griffin Observership ApplicationDocument7 pagesGriffin Observership Applicationসোমনাথ মহাপাত্রNo ratings yet
- Boards and Beyound Step 2 Cs PalpitationsDocument4 pagesBoards and Beyound Step 2 Cs Palpitationsসোমনাথ মহাপাত্রNo ratings yet
- 1 This Is System WiseDocument1 page1 This Is System Wiseসোমনাথ মহাপাত্রNo ratings yet
- Chemo For HematologyDocument1 pageChemo For Hematologyp monica aneeshaNo ratings yet
- UWORLD Biostatistics Book Review PDFDocument93 pagesUWORLD Biostatistics Book Review PDFসোমনাথ মহাপাত্র50% (2)
- Cs Info ManualDocument20 pagesCs Info Manualসোমনাথ মহাপাত্রNo ratings yet
- IMG Observership PolicyDocument3 pagesIMG Observership PolicyNilay BhattNo ratings yet
- Medical AbbreviationsDocument4 pagesMedical AbbreviationsNelly PaniaguaNo ratings yet
- Chemo For HematologyDocument1 pageChemo For Hematologyp monica aneeshaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- EMRAM Stages Model ExplainedDocument2 pagesEMRAM Stages Model ExplainedReinhard Harianja100% (1)
- Single-Step DIPSI 75g Glucose Tolerance Test-For Diagnosis of Gestational Diabetes MellitusDocument7 pagesSingle-Step DIPSI 75g Glucose Tolerance Test-For Diagnosis of Gestational Diabetes MellitusEditor ERWEJNo ratings yet
- CSF LeaksDocument3 pagesCSF LeaksDrTarek Mahmoud Abo KammerNo ratings yet
- TOP 25 RICHEST PEOPLE IN THE WORLD BY NET WORTH AND YEARLY CHANGEDocument24 pagesTOP 25 RICHEST PEOPLE IN THE WORLD BY NET WORTH AND YEARLY CHANGEEstiyak JahanNo ratings yet
- Orientation To The IVT ProgramDocument16 pagesOrientation To The IVT ProgramCrystal Mae Castrodes DaquipilNo ratings yet
- Floor Supervisor ChecklistDocument1 pageFloor Supervisor ChecklistBOOKREADER_NOW100% (1)
- The Unofficial ADHD Self-TestDocument73 pagesThe Unofficial ADHD Self-TestOmayra Sánchez González100% (1)
- Assess Patient with Suspected AppendicitisDocument6 pagesAssess Patient with Suspected AppendicitisRirin Ajeng Kartiningsih100% (1)
- dm2022 0455Document4 pagesdm2022 0455Charlemagne Sabio Galamgam100% (1)
- Gelenberg - The Practitioner's Guide To Psychoactive Drugs, 4eDocument553 pagesGelenberg - The Practitioner's Guide To Psychoactive Drugs, 4eamm90No ratings yet
- PLAUT-VINCENT ANGINA Borrelia Vincenti Tonsillitis PDFDocument2 pagesPLAUT-VINCENT ANGINA Borrelia Vincenti Tonsillitis PDFJosua MakerNo ratings yet
- NURSING RESEARCH-Questionnaire On Sexually Transmitted InfectionsDocument3 pagesNURSING RESEARCH-Questionnaire On Sexually Transmitted InfectionsEJ Cubero, R☤NNo ratings yet
- DR Carlos S. Lanting College: in Partial Fulfillment of The Requirements in N-508Document23 pagesDR Carlos S. Lanting College: in Partial Fulfillment of The Requirements in N-508Richard Ines ValinoNo ratings yet
- PARENTAL HEIGHT AND STUNTING LINKDocument24 pagesPARENTAL HEIGHT AND STUNTING LINKputri annikeNo ratings yet
- Bangladesh College of Physicians and Surgeons (BCPS)Document2 pagesBangladesh College of Physicians and Surgeons (BCPS)Faruk HossainNo ratings yet
- Couching in Ancient India: SushrutaDocument3 pagesCouching in Ancient India: SushrutaDeepak RamNo ratings yet
- OpllDocument10 pagesOpllTeofilus KristiantoNo ratings yet
- JURNALDocument64 pagesJURNALSaleh AlsadiNo ratings yet
- BING Covid-19Document9 pagesBING Covid-19tirsha tjowasiNo ratings yet
- Case Study on Using Informatics in Nursing PracticeDocument3 pagesCase Study on Using Informatics in Nursing PracticeKenzie SmithNo ratings yet
- Vaginitis: Dr. Zienab Halem Faculty of Pharmacy SCUDocument25 pagesVaginitis: Dr. Zienab Halem Faculty of Pharmacy SCUshona SharupaniNo ratings yet
- Placenta Akreta Screening and DiagnosisDocument46 pagesPlacenta Akreta Screening and DiagnosisDwiweirkepPetNo ratings yet
- B.well SwissDocument1 pageB.well SwissZumrud QafarliNo ratings yet
- 1 DUW10022-COURSE OUTLINE 1 2022 2023 (PPL-04 (2b) (21-09-21)Document5 pages1 DUW10022-COURSE OUTLINE 1 2022 2023 (PPL-04 (2b) (21-09-21)Hanie MunirahNo ratings yet
- Drug Abuse Prevention, Treatment, and RehabilitationDocument16 pagesDrug Abuse Prevention, Treatment, and RehabilitationNigel HopeNo ratings yet
- Avaxim CMI July 2019Document3 pagesAvaxim CMI July 2019walkrogNo ratings yet
- Issuance of Sick Leave Certificate Policy Final - UAEDocument12 pagesIssuance of Sick Leave Certificate Policy Final - UAEmarks2much100% (2)
- Ao 2011-0002Document7 pagesAo 2011-0002Suzette Paredes-RagosNo ratings yet
- Bibliografía Terapias Con AnimalesDocument4 pagesBibliografía Terapias Con AnimalesMiriam SerranoNo ratings yet
- Eurheartj Ehw272 FullDocument72 pagesEurheartj Ehw272 FullFabian SanabriaNo ratings yet