Professional Documents
Culture Documents
Pathophysiology of Kidneys
Uploaded by
Лариса ТкачеваOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology of Kidneys
Uploaded by
Лариса ТкачеваCopyright:
Available Formats
Topic. Pathophysiology of kidneys.
Pathogenesis of the main clinical syndromes of the
renal diseases
1. Characteristic changes in diuresis (poly-, oligo-, anuria), etiology, pathogenesis.
2. Urinary syndrome (proteinuria, hematuria, leukocyturia, cylindruria; their types, causes
and diagnostic significance).
3. Extrarenal symptoms and syndromes in renal diseases. Pathogenesis of renal
hypertension, edema, azotemia and anemia.
4. Glomerulonephritis (etiology, pathogenesis and clinical manifestations).
5. Nephrotic syndrome, pathogenesis and clinical manifestations.
6. Nephrolithiasis: etiology, pathogenesis, clinical manifestations, consequences.
7. Syndrome of acute renal failure (ARF): forms, etiology, pathogenesis, stages, principles
of treatment. The importance hemodialysis in the treatment of ARF; principles of
hemodialysis.
8. Syndrome of chronic renal failure (CRF): etiology, stages, features of pathogenesis.
Uremia; principles of its treatment.
CASE№1
Patient K., 28 years old, was admitted to hospital 3 weeks after having tonsilitis, with complaints
of dull pain in the loin, headache, frequent urination, face edema (especially in the morning),
dyspnea, thirst.
Examination findings: The patient is pale, with edema on the legs and especially on the face. BP
is 180/100 mm Hg; HR – 100; on ECG – signs of diffuse lesion of the myocardium.
Blood test: Hb – 100 g/l; ESR – 26 mm/h; BUN (blood urea nitrogen) – 70-85 mmol/l; increased
level of globulin fractions in the blood. Diurnal diuresis is 1litre; relative urine density – 1029;
concentration index – 3.3. The urine is cloudy, looks like “meat slops” and contains large quantities
of erythrocytes as “shadows”; leukocytes - 6-8 in the vision field, hyaline casts – 3 – 4 in the
vision field; protein – 1.5 – 2 g/l (molecular mass < 70, 000). Creatinine clearance is less than 50%
of the norm. In the needle bioptate of the kidneys deposits of immune complexes are detected.
1. What disease are these clinical features and laboratory findings typical of? Justify your
conclusion.
2. Explain the etiology and pathogenesis of this nephropathy.
3. Assess the filtration and concentration function of the kidneys.
4. Explain the mechanism of the patient’s symptoms and syndromes.
CASE№2
A 46-year-old woman suffering from lipoid nephrosis was admitted to an internal disease
department with complaints of marked edema, weakness, bad appetite.
Examination findings: The patient is extremely pale, edematous, having ascites. The heart
sounds are muffled. HR is 96; the heart boundaries are extended.
Blood test: albumins – 15g/l; dysproteinemia, hyperlipidemia, hypercholesterolemia.
In the urine: protein – 20g/l daily (protein molecular mass > 70, 000); hyaline, waxy and granular
casts – up to 10 in the vision field.
1. What is this syndrome called?
2. Explain the mechanism of the edema, presence of casts in the urine and proteinuria.
3. What type of proteinuria is typical of this syndrome? Justify your answer.
4. State the most likely cause of antithrombin III, transferrin and γ-globulin deficiency in this
patient. What are the consequences of this condition?
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mini VET GuideDocument186 pagesMini VET GuideemitibiNo ratings yet
- Top 100 Pathology Secrets List W/ NotesDocument6 pagesTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- Russian Neuropsychology After Luria by Janna M. Glozman PDFDocument12 pagesRussian Neuropsychology After Luria by Janna M. Glozman PDFTernassNo ratings yet
- 1st Prof Examination 2023Document12 pages1st Prof Examination 2023Masoom IgNo ratings yet
- Feline Asthma: Laura A. Nafe, DVM, MS, Dacvim (Saim)Document5 pagesFeline Asthma: Laura A. Nafe, DVM, MS, Dacvim (Saim)Miruna ChiriacNo ratings yet
- Immune System 14Document61 pagesImmune System 14Лариса ТкачеваNo ratings yet
- Drugs Affecting Myometrium1 PDFDocument9 pagesDrugs Affecting Myometrium1 PDFЛариса ТкачеваNo ratings yet
- Diseases of The Gastrointestinal TractDocument87 pagesDiseases of The Gastrointestinal TractЛариса ТкачеваNo ratings yet
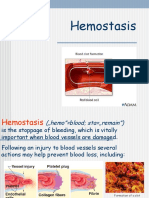
- Lecture HemostasisDocument28 pagesLecture HemostasisЛариса ТкачеваNo ratings yet
- Leukocytosis. Leukopenia.: Lecture PresentationDocument23 pagesLeukocytosis. Leukopenia.: Lecture PresentationЛариса ТкачеваNo ratings yet
- Lecture LeukemiaDocument21 pagesLecture LeukemiaЛариса ТкачеваNo ratings yet
- PLT & Heamostasis (Autosaved)Document35 pagesPLT & Heamostasis (Autosaved)Лариса ТкачеваNo ratings yet
- Autoimmunity: 1 Semester DMLTDocument11 pagesAutoimmunity: 1 Semester DMLTTepfi TepsNo ratings yet
- NLR As Biomarker of DeleriumDocument9 pagesNLR As Biomarker of DeleriumbrendaNo ratings yet
- Pancreatic Cystic Lesions English 2019Document25 pagesPancreatic Cystic Lesions English 2019Worku KifleNo ratings yet
- Drugs For The Geriatric PatientDocument1,413 pagesDrugs For The Geriatric Patientjulio.testi698295100% (1)
- Cutaneous Manifestations of GIT and Liver DiseasesDocument48 pagesCutaneous Manifestations of GIT and Liver DiseasesSippy Iqbal MemonNo ratings yet
- Bleeding (Haemorrhagia)Document63 pagesBleeding (Haemorrhagia)hatirebNo ratings yet
- SP8 Lumbar PunctureDocument5 pagesSP8 Lumbar PunctureAgeng RestiNo ratings yet
- Keep Safe Everyone. God Bless 2C.: 3. Deadline For This Activity Will Be On Sunday March 29, 2020 11:59PMDocument10 pagesKeep Safe Everyone. God Bless 2C.: 3. Deadline For This Activity Will Be On Sunday March 29, 2020 11:59PMJœnríčk AzueloNo ratings yet
- Notes AtherosclerosisDocument1 pageNotes AtherosclerosisElizabeth de GuzmanNo ratings yet
- Standard Operating Procedure (SOP) For On-Call Emergency Out of Hours Haemodialysis For Renal PatientsDocument23 pagesStandard Operating Procedure (SOP) For On-Call Emergency Out of Hours Haemodialysis For Renal PatientsShahriar MohammodNo ratings yet
- Medical Student Guide For Dermatology489Document89 pagesMedical Student Guide For Dermatology489Mojtaba Andalib AzarNo ratings yet
- Normal Pressure Hydrocephalus Neurophysiological.14Document6 pagesNormal Pressure Hydrocephalus Neurophysiological.14dewi najiraNo ratings yet
- Basic Pharmacology of Anesthesia DrugDocument47 pagesBasic Pharmacology of Anesthesia DrugAkma KamaruddinNo ratings yet
- Daily Practice Test-14 (Zoology) Questions: Excretory SystemDocument7 pagesDaily Practice Test-14 (Zoology) Questions: Excretory SystemDarshan DarshuNo ratings yet
- Seminar 9-ITPDocument22 pagesSeminar 9-ITPanon_67984147No ratings yet
- Reaction PaperDocument2 pagesReaction PaperLinzie CariquetanNo ratings yet
- Article 1522477582Document5 pagesArticle 1522477582RaoNo ratings yet
- Pharmacology Obat Lepra Dan TBC Kutis: Dharma Permana, PHD, AptDocument33 pagesPharmacology Obat Lepra Dan TBC Kutis: Dharma Permana, PHD, AptanggiNo ratings yet
- Transient Tachypnea of NewbornDocument4 pagesTransient Tachypnea of NewbornloraineNo ratings yet
- Program Plan - AlzheimersDocument26 pagesProgram Plan - Alzheimersapi-599067855No ratings yet
- Anemia IntroductionDocument15 pagesAnemia IntroductionNitesh Kotian100% (1)
- UVA QuestionsDocument61 pagesUVA QuestionsjhhjjhNo ratings yet
- Drug Study: Nursing DepartmentDocument1 pageDrug Study: Nursing Departmentgiselle chloeNo ratings yet
- OCN Study GuideDocument10 pagesOCN Study GuideYadile D BenoitNo ratings yet
- Kussmaul BreathingDocument3 pagesKussmaul BreathingsakuraleeshaoranNo ratings yet