Professional Documents
Culture Documents
Piezosurgery Versus Conventional Method Alveolopla
Uploaded by
mirah indrianiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Piezosurgery Versus Conventional Method Alveolopla
Uploaded by
mirah indrianiCopyright:
Available Formats
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.
71]
Original Article ‑ Comparative Study
Piezosurgery Versus Conventional Method Alveoloplasty
Khushal D. Gangwani, Lakshmi Shetty, Deepak Kulkarni, Ratnadeepika Seshagiri, Ratima Chopra
Department of Oral and Maxillofacial Surgery, Dr. D. Y. Patil Vidyapeeth’s, Dr. D. Y. Patil Dental College and Hospital, Pune, Maharashtra, India
Abstract
Purpose: Conventional alveoloplasty procedure using manual instruments results in higher resorption of the residual alveolar ridge,
which is unsuitable for denture construction. The purpose of this study was to evaluate the effect of piezosurgery‑assisted alveoloplasty
using minimally invasive technique compared to that of the conventional technique. Materials and Methods: This was a comparative
in vivo study. The study sample consisted of 35 edentulous patients with bilateral bony spicules requiring alveoloplasty. The primary
outcome variables assessed were time required for alveoloplasty, postoperative pain using visual analogue scale (VAS), and postoperative
healing using Landry, Turnbull, and Howley healing index. The differences between the outcome variables were statistically analyzed
using paired t‑test. Results: The participants consisted of 35 patients (25 men and 10 women; age range: 38–83 years) diagnosed
with bilateral bony spicules on the edentulous alveolar ridge. There was a statistically highly significant difference between both
groups with respect to the outcome variables such as time required, VAS at 2nd day, and healing index at 7th day with higher mean of
time required (in sec), higher mean of VAS, and lower healing index for conventional group as compared to piezo group (P < 0.05).
Conclusion: Alveoloplasty done using piezosurgery not only reduces patient’s postoperative discomfort but also maintains the alveolar
bone integrity by not disturbing the soft‑tissue and hard‑tissue architecture, allowing faster healing of tissues, which makes the future
prosthesis replacement easier
Keywords: Alveoloplasty, minimally invasive, piezoelectric surgery, piezosurgery
Introduction O. T. Dean first described “Intra‑septal alveoloplasty” in the
American Dental Association journal in 1936. Hence, this
A well‑contoured smooth alveolar ridge is crucial for
procedure also came to be known as Dean’s alveoloplasty.[3]
appropriate fabrication of complete or partial denture. While
contouring the ridge, it is highly essential to remember Technological advancement boldly gives the options to step
that greater the excision of bone, higher will be resultant aside, lead, or follow. Piezosurgery or piezoelectric bone
resorption.[1] Therefore, the procedure of contouring should be surgery is a new innovative, assuring, precise system for
limited to excision of the irregular sharp ridges and unfavorable removal of hard tissue, sparing the soft tissues. It works on
undercuts which are unsuitable for denture construction. the principle of ultrasonic vibrations.
Hence, the goal of alveoloplasty is to gain favorable tissue Reports have been published of the use of this technology
support for the designed prosthesis, while conserving as much in dentistry in maxillary sinus elevation procedures,[4,5]
soft tissue and hard tissue as possible. bone harvesting, [6,7] expansion of alveolar crest, [8]
Alveoloplasty is a term for preprosthetic surgical procedure implantology, [9,10] periodontal surgery, [11] orthognathic
that involves smoothening of rough alveolar bone following and maxillofacial surgery,[12‑14] and dental exposure and
extractions on the edentulous area or trimming of bulbous
tuberosities, which creates deep undercuts. It is one of the
Address for correspondence: Dr. Khushal D. Gangwani,
most common surgical techniques used to prepare the alveolar
Sonigara Aangan Society, F‑508, Near ISKCON Temple, Ravet,
ridges to procure a prosthesis. Historically, the procedure has Pune ‑ 412 101, Maharashtra, India.
been recognized from more than a century. A. T. Willard in E‑mail: khushalhkhr@gmail.com
1853 advocated reduction of the alveolar ridge to bring about
the complete proximity of soft tissues over the alveolus.[2] Sir
This is an open access journal, and articles are distributed under the terms of the
Creative Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which
Access this article online allows others to remix, tweak, and build upon the work non‑commercially, as long
Quick Response Code: as appropriate credit is given and the new creations are licensed under the identical
Website: terms.
www.amsjournal.com
For reprints contact: reprints@medknow.com
DOI: How to cite this article: Gangwani KD, Shetty L, Kulkarni D, Seshagiri R,
10.4103/ams.ams_162_18 Chopra R. Piezosurgery versus conventional method alveoloplasty. Ann
Maxillofac Surg 2018;8:181-7.
© 2018 Annals of Maxillofacial Surgery | Published by Wolters Kluwer - Medknow 181
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
extractions. [15] However, to the best of our knowledge, On the other contralateral side of the arch, a stab incision was
no studies until now have been published for the use of placed mesial or distal to the bony spicule using a surgical
piezosurgery with the minimally invasive technique for blade (No. 15) [Figure 4]. A small‑sized tip periosteal elevator
alveoloplasty procedure. was passed underneath the stab incision, and subperiosteal
tunneling was done until the prominent bony spicule was
Therefore, this study aims at evaluating the efficacy of
reached [Figure 5]. A Piezo blade of Rhomboid shape
alveoloplasty done with piezosurgery system compared with
(EX‑03, Dmetec Surgystar®, Korea) was then inserted through
that of the conventional technique. The parameters to be
the subperiosteal tunnel up to the bony spicule. The piezo
compared between the two systems will be – the time required
unit was switched on with frequency set at of 25–29 kHz in
for the procedure, postoperative pain, and healing of the soft “boosted” mode with saline flow of 60 ml/min [Figure 6].
tissues. The bony spicule was shaved off carefully in a unidirectional
motion of the piezo blade [Figure 7]. The motion was continued
Materials and Methods until the bony spicule was no longer digitally palpated. The
Study design and sample time from the start of the incision till the end of alveoloplasty
To address the research purpose, the authors designed was noted.
and implemented a split‑mouth in vivo study after Both the surgical procedures, conventional alveoloplasty, and
receiving approval from the Institutional Review Board alveoloplasty using piezosurgery were performed in the same
and Ethics Committee. The study was conducted in surgical session.
accordance with the Declaration of Helsinki. Written
Postoperatively, patients were prescribed an analgesic
informed consent was obtained from all patients after they
(500 mg of Aceclofenac 8 h for 5 days) and antibiotic
were given full written and verbal information regarding the
(250 mg of amoxicillin every 8 h for 5 days). In case of
study.
amoxicillin allergy, erythromycin (250 mg every 8 h for 5 days)
The study population comprised all edentulous patients was prescribed. Choice of analgesic and antibiotic was based
with bilateral bony spicules on the alveolar ridge indicated on the standard institutional protocol.
for alveoloplasty who presented to the institute’s dentistry
The postoperative pain at the operated site was assessed
outpatient department between January 1, 2016, and
by visual analog scale (VAS)[16] [Figure 8] on the second
January 1, 2017. Patients with bilateral bony spicules with
postoperative day (POD). Sutures were removed on the
2‑mm maximal diameter on either side were included in
7th POD and the healing was assessed using Landry et al.
this study. Patients with bleeding disorders, uncontrolled
index[17] [Table 1].
systemic comorbidities, unilateral bony spicules, and
maximal bony spicule diameter exceeding 2 mm were The obtained values were recorded, tabulated, and statistically
excluded from the study. evaluated.
Methodology
In the recruited patients, using Sequentially Numbered Opaque
Results
Sealed Envelopes randomization technique, a site on which the The participants consisted of 35 patients (25 men and 10
piezo alveoloplasty to be performed was selected. women; age range: 38–83 years, mean age: 60.8 years)
diagnosed with bilateral bony spicules on the edentulous
All the surgical procedures and postoperative assessments alveolar ridge.
were performed by the same surgeon. Preoperatively,
patients were required to gargle with 0.12% chlorhexidine Statistical package for the (SPSS) version 21.0 (SPSS,
mouthwash (Oradex) for a minute. After performing Inc, Mumbai, India) was used for the statistical analysis.
standard painting and draping of the site, local anesthetic There was no significant difference in patient age and
(2% lignocaine hydrochloride with 1:200,000 Adrenaline) size of the bony spicules. However, gender was noted
was injected in the mucobuccal fold over the prominent bony to be a confounding factor because the male population
spicule region. predominated [Figure 9].
Once complete anesthesia of the planned surgical area was Descriptive statistics such as mean, standard deviation,
achieved, crestal and releasing incisions were taken, and the frequency, and percentage of independent variables
full thickness flap was reflected [Figure 1]. Bony contouring have been expressed. Intergroup comparison of outcome
was accomplished with bone files, rongeurs forceps, or variables, such as time required for surgery, VAS score for
burs [Figure 2]. Digital palpation was used to determine pain assessment, and the healing index, was done using
paired t‑test where P < 0.05 was considered statistically
the uniformity of the ridge. The flap was approximated
significant.
and secured with nonresorbable suture (3‑0 silk suture,
Monodek®) [Figure 3]. The surgical procedure was timed from There was a statistically highly significant difference
the first incision to the last suture. between both groups with respect to outcome variables such
182 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
Figure 1: Crestal incision along with releasing incisions Figure 2: Excision of bony spicule using rongeurs forceps
Figure 3: Closure with interrupted 3‑0 black silk Figure 4: Stab incision adjacent to the bony spicule
Figure 5: Subperiosteal tunneling
Figure 6: Piezo unit
as time required in seconds, VAS at 2 day, and healing
nd
index at 7th day. It was observed that mean time required (in Pain
sec), and mean VAS was higher and mean healing index The patients in the piezo subgroup reported a significantly
was lower for the conventional group as compared to piezo lower VAS score at the surgery site on POD 1, compared to the
group [Table 2]. conventional subgroup. The mean VAS score was 2.74 for the
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018 183
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
conventional method and 0.94 for the piezosurgery method with 255.20 s and for the procedure by piezosurgery technique
the standard deviation of 1.2 and 0.7, respectively [Figure 10]. was 132.37 s with a standard deviation of 109.8 and 78.2,
respectively [Figure 11].
Operative time
The reported operative time in the piezosurgery Healing index
alveoloplasty subgroup was significantly less compared The operative site in piezosurgery subgroup showed
to the conventional site subgroup. The mean time required significantly better and faster healing compared to that in the
for the alveoloplasty by conventional method was conventional subgroup. The healing index by Landry et al.[17] on
the 7th POD for the conventional method was 3.11 and for the
piezosurgery method was 4.31 with standard deviations being
0.71 and 0.67, respectively [Figure 12].
Discussion
Except for the extraction of natural teeth, the most commonly
performed preprosthetic surgical procedure is alveolectomy
or alveoloplasty.
Alveolectomy has been defined by Boucher in 1974 as
“removal of a part of the alveolus by surgery.”[1] In recent
Figure 7: Alveoloplasty using piezo blade EX‑03
Figure 8: Visual analog score
Figure 10: Comparison of visual analog scale
Figure 9: Gender distribution
Figure 11: Comparison of operative time Figure 12: Comparison of postoperative healing
184 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
years, the term “Alveoloplasty” has been adopted to signify revolutionized the process of alveoloplasty by introducing
recontouring of the alveolar process rather than its removal. intraseptal alveoloplasty, a procedure he had been using for
Thoma has stated that there is requirement of alveoloplasty in 20 years.[3] Since then, there has not been any improvement
almost every patient who has undergone multiple extractions or change in the procedure. Dean differed from other pioneers
and may also be needed in those with single extraction.[18] The in the field of preprosthetic surgery in that he advocated the
goal for contouring the alveolar ridge is to gain favorable tissue preservation of the labial cortex, preferring instead to sacrifice
support for the designed prosthesis while conserving as much the interradicular medullary bone to achieve optimal alveolar
soft tissue and hard tissue as possible.[19] ridge contour. Dean’s intraseptal alveoloplasty was particularly
Historically, alveoloplasty is known to the field of surgery well suited for immediate denture surgery. For the cases of
for the past few decades. W. G. Beers in 1976 coined the extreme premaxillary protrusion, Obwegeser in 1966 suggested
phrase “heroic treatment of alveolectomy” in which large a modification of Dean’s technique wherein both the palatal
portions of alveolus were removed with cutting forceps. In and labial cortices were fractured and repositioned.
1905, W. Shearer advocated and elaborated on alveolectomy In 1976, Michael and Barsoum[1] studied the amount and
to eradicate gingival and alveolar pathosis and to serve as a duration of postoperative bone resorption and ridge contour
foundation for the prosthodontist to prepare a denture.[20] The changes in immediate denture patients using various surgical
problems of excessive bone resorption after alveolectomy techniques such as: (1) simple extractions without additional
were addressed when in 1936 Sir O. T. Dean published and surgery, (2) extractions with labial cortical alveolectomy,
and (3) extractions with Dean’s intraseptal alveolectomy. Using
serial sagittal contour photographs of study casts and serial
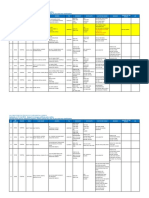
Table 1: Healing index (Landry, Turnbull and Howley) cephalometric radiographs of patients, they showed that the
HEALING INDEX CRITERIA three techniques produced almost the same amount of bone
VERY POOR 1 Tissue color: more than 50% of gingivae red resorption at the end of 3 months, but thereafter, the differences
Response to palpation :bleeding were noteworthy (with statistical significant difference). At
Granulation tissue: present the end of 6 and 12 months, the nonsurgical extractions had
Incision margin: not epithelialised, with loss produced the least amount of bone resorption with a marked
of epithelium beyond margins slowing of the rate by 6 months, whereas both alveoloplasty
Suppuration: present
techniques resulted in continuing bone resorption.
POOR 2 Tissue color: more than 50% of gingivae red
Response to palpation: bleeding Piezoelectric technique was introduced in oral surgery during
Granulation tissue: present the 1970s when Horton examined the recovery process of dogs
Incision margin: not epitheliased with that had undergone osteotomy.[21] It works on the principle of
connective tissue exposed.
piezoelectric effect, first reported in 1880 by Marie and Jean
GOOD 3 Tissue color: less than 50% of gingivae red
Curie that asserts that some crystals and ceramics change their
Response to palpation: no bleeding
Granulation tissue: none
shape when an electric current is sent across them, producing
Incision margin: no connective tissue oscillations of ultrasonic frequency. There is amplification
exposed of vibrations with minimum pressure on hard tissue, which
VERY GOOD 4 Tissue color: less than 25% of gingivae red produces cavitation phenomenon, which is a mechanical
Response to palpation: no bleeding cutting phenomenon occurring particularly on hard tissues.
Granulation tissue: none
Incision margin: no connective tissue The piezoelectric instrument develops a regulated ultrasonic
exposed frequency of 24–29 kHz, and a microvibration amplitude of
EXCELLENT 5 Tissue color: all gingivae pink 60–200 mm/s. Soft tissues remain unharmed at this frequency,
Response to palpation: no bleeding but may also be damaged at frequencies above 50 kHz.
Granulation tissue: none Microstreaming and cavitation phenomenon are peculiar
Incision margin: no connective tissue exposed features of piezosurgery.
Table 2: Comparison of outcome variables
Outcome variables Groups n Mean Std. deviation Std. error mean P of t-test
Time required (Sec) Conventional 35 255.20 109.854 18.569 0.000**
Piezo 35 132.37 78.258 13.228
VAS 2d Conventional 35 2.74 1.221 0.206 0.000**
Piezo 35 0.94 0.765 0.129
Healing Index 7d Conventional 35 3.11 0.718 0.121 0.000**
Piezo 35 4.31 0.676 0.114
**=Statistically highly significant difference (P<0.01)
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018 185
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
In bone microsurgery, two fundamental concepts principally controlling the inflammatory process better, and stimulating
govern the philosophy behind the development of piezoelectric bony remodeling as early as 56 days after treatment. There are
bone surgery. The first being minimally invasive surgery in few limitations also which include slightly longer osteotomy
which the postoperative pain and swelling is much lower time and increasing heat transmission due to increasing
as compared to traditional techniques because of improved working pressure which can lead to tissue damage unless
tissue healing, ultimately reducing patient discomfort. The used carefully.
second concept which increases the effectiveness of the
treatment is surgical predictability. The development of Conclusion
piezoelectric bone surgery has indeed optimized the surgical
Among the various instruments and techniques used for
results even in the most complex and unfavorable anatomical
alveoloplasty, piezosurgery using the minimally invasive
cases due to ease of controlling the instrument leading to
incision has proved to be a better alternative by minimizing the
reduced hemorrhages, precise cuts eventually producing
operative time, reducing patient’s discomfort, and accelerating
excellent tissue healing.
the healing process. Therefore, this study justifies the use of
Subperiosteal tunneling, a minimally invasive access piezosurgery in atraumatic alveoloplasty in all patients.
procedure, was a technique used by Kim et al. in horizontal
There are few limitations to this study. The sample size in the
ridge augmentation procedure in which the authors prepared a
study is small. However, the findings were consistent across
subperiosteal cavity with a periosteal elevator, and a selection
all patients. Studies using larger sample size are needed to
of bone graft materials was placed into the tunnel to augment
establish the findings with higher statistical significance.
the deficient alveolar ridge.[22] A similar technique is used
in this study to get access to the bony spicule and perform Declaration of patient consent
alveoloplasty using the contrangled piezo blade. The advantage The authors certify that they have obtained all appropriate
of this minimally invasive sutureless technique is reduced patient consent forms. In the form the patient(s) has/have
healing time with lesser postoperative discomfort. given his/her/their consent for his/her/their images and other
clinical information to be reported in the journal. The patients
According to a prospective study by Waite and Cherala, the
understand that their names and initials will not be published
authors stated that tight closure over a large bony socket
and due efforts will be made to conceal their identity, but
or defect does not facilitate drainage and oral hygiene.[23]
anonymity cannot be guaranteed.
Suturing may create a one‑way valve that allows food debris
to enter the socket but not easily escape which may lead to Financial support and sponsorship
local infection, inflammation, edema, clot necrosis, alveolar Nil.
osteitis, and pain. A small flap left open without suturing may
facilitate drainage, improve hygiene, and reduce the risk of Conflicts of interest
pain associated with alveolar osteitis. Hence, we performed a There are no conflicts of interest.
sutureless alveoloplasty technique in our study.
In studies conducted by Sortino et al.[15] and Goyal et al.[24]
References
1. Michael CG, Barsoum WM. Comparing ridge resorption with
comparing the efficacy of piezosurgery and conventional various surgical techniques in immediate dentures. J Prosthet Dent
rotatory instruments for impacted mandibular third molar 1976;35:142‑55.
removal, the authors concluded that there was a reduction in 2. Hayward JR, Thompson S. Principles of alveolectomy. J Oral
postoperative pain, facial swelling, and trismus in piezosurgery Surg (Chic) 1958;16:101‑8.
3. Dean OT. Surgery for the denture patient. J Am Dent Assoc
group, while the operative time was higher in the same 1936;23:2124.
compared to the control group. However, in this study, the 4. Barone A, Santini S, Marconcini S, Giacomelli L, Gherlone E, Covani U,
operative time in piezo group was lesser compared to control et al. Osteotomy and membrane elevation during the maxillary
group owing to the lack of need for suturing of the minimally sinus augmentation procedure. A comparative study: Piezoelectric
device vs. conventional rotative instruments. Clin Oral Implants Res
invasive incision. 2008;19:511‑5.
5. Wallace SS, Mazor Z, Froum SJ, Cho SC, Tarnow DP. Schneiderian
Labanca et al.[25] reported the advances in piezosurgery
membrane perforation rate during sinus elevation using piezosurgery:
over the last 20 years and focused on its uses in different Clinical results of 100 consecutive cases. Int J Periodontics Restorative
surgical areas. In oral and maxillofacial surgery, it has Dent 2007;27:413‑9.
been used in orthognathic surgeries, rhinoplasties, and 6. Happe A. Use of a piezoelectric surgical device to harvest bone grafts
from the mandibular ramus: Report of 40 cases. Int J Periodontics
surgical extractions. After studying the use of piezosurgery
Restorative Dent 2007;27:241‑9.
in all these clinical scenarios, the authors concluded that 7. Sohn DS, Ahn MR, Lee WH, Yeo DS, Lim SY. Piezoelectric osteotomy
piezoelectric surgery is an innovative technique for safe and for intraoral harvesting of bone blocks. Int J Periodontics Restorative
effective osteotomy owing to the lack of macro vibrations, Dent 2007;27:127‑31.
8. Stübinger S, Landes C, Seitz O, Zeilhofer HF, Sader R. Ultrasonic
ease of use, and controlled and safe cutting. It seems to be bone cutting in oral surgery: A review of 60 cases. Ultraschall Med
more efficient in the first phases of bony healing, inducing 2008;29:66‑71.
an earlier increase in Bone Morphogenic Proteins (BMPs), 9. Sivolella S, Berengo M, Fiorot M, Mazzuchin M. Retrieval of blade
186 Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018
[Downloaded free from http://www.amsjournal.com on Wednesday, December 26, 2018, IP: 187.160.101.71]
Gangwani, et al.: Minimally invasive Piezo-alveoloplasty
implants with piezosurgery: Two clinical cases. Minerva Stomatol Med J 1990;59:149‑54.
2007;56:53‑61. 17. Landry RG, Turnbull RS, Howley T. Effectiveness of benzydamyne HCl
10. Vercellotti T. Piezoelectric surgery in implantology: A case report – A in the treatment of periodontal post‑surgical patients. Res Clin Forum
new piezoelectric ridge expansion technique. Int J Periodontics 1988;10:105.
Restorative Dent 2000;20:358‑65. 18. Thoma KH. Oral Surgery. 3rd ed. St. Louis: Mosby Company; 1958. p. 229.
11. Vercellotti T, Nevins ML, Kim DM, Nevins M, Wada K, Schenk RK, 19. Fonseca RJ, Davis WH. Reconstructive Preprosthetic Oral and
et al. Osseous response following resective therapy with piezosurgery. Maxillofacial Surgery. St. Louis: W.B. Saunders; 1986.
Int J Periodontics Restorative Dent 2005;25:543‑9. 20. Shearer WL. Alveolectomy. Chron Omaha D Soc 1953;16:247.
12. Gleizal A, Bera JC, Lavandier B, Beziat JL. Piezoelectric osteotomy: 21. Horton JE, Tarpley TM Jr., Jacoway JR. Clinical applications of
A new technique for bone surgery‑advantages in craniofacial surgery. ultrasonic instrumentation in the surgical removal of bone. Oral Surg
Childs Nerv Syst 2007;23:509‑13. Oral Med Oral Pathol 1981;51:236‑42.
13. Robiony M, Polini F, Costa F, Zerman N, Politi M. Ultrasonic bone 22. Kim HS, Kim YK, Yun PY. Minimal invasive horizontal ridge
cutting for surgically assisted rapid maxillary expansion (SARME) augmentation using subperiosteal tunneling technique. Maxillofac Plast
under local anaesthesia. Int J Oral Maxillofac Surg 2007;36:267‑9. Reconstr Surg 2016;38:41.
14. Geha HJ, Gleizal AM, Nimeskern NJ, Beziat JL. Sensitivity 23. Waite PD, Cherala S. Surgical outcomes for suture‑less surgery in 366
of the inferior lip and chin following mandibular bilateral impacted third molar patients. J Oral Maxillofac Surg 2006;64:669‑73.
sagittal split osteotomy using piezosurgery. Plast Reconstr Surg 24. Goyal M, Marya K, Jhamb A, Chawla S, Sonoo PR, Singh V, et al.
2006;118:1598‑607. Comparative evaluation of surgical outcome after removal of impacted
15. Sortino F, Pedullà E, Masoli V. The piezoelectric and rotatory osteotomy mandibular third molars using a piezotome or a conventional handpiece:
technique in impacted third molar surgery: Comparison of postoperative A prospective study. Br J Oral Maxillofac Surg 2012;50:556‑61.
recovery. J Oral Maxillofac Surg 2008;66:2444‑8. 25. Labanca M, Azzola F, Vinci R, Rodella LF. Piezoelectric surgery:
16. Campbell WI, Lewis S. Visual analogue measurement of pain. Ulster Twenty years of use. Br J Oral Maxillofac Surg 2008;46:265‑9.
Annals of Maxillofacial Surgery ¦ Volume 8 ¦ Issue 2 ¦ July-December 2018 187
You might also like
- Ibm 5Document7 pagesIbm 5rintanfsNo ratings yet
- Sutura X Art.Document11 pagesSutura X Art.jessica5rcNo ratings yet
- Minimally Invasive Transgingival Implant Therapy: A Literature ReviewDocument6 pagesMinimally Invasive Transgingival Implant Therapy: A Literature ReviewEmilio RodríguezNo ratings yet
- ACC Soft Tissue Development Around Pontic SiteDocument5 pagesACC Soft Tissue Development Around Pontic SiteJayarti Rohmadani MarsaNo ratings yet
- Epiphora Drainage by DCR - Long-Term Results: Original ResearchDocument5 pagesEpiphora Drainage by DCR - Long-Term Results: Original ResearchSaatvik AtriNo ratings yet
- Chipalia 2014 Articulocompleto PDFDocument11 pagesChipalia 2014 Articulocompleto PDFLeid ArizaNo ratings yet
- Implante Articulo 3Document7 pagesImplante Articulo 3alessandrachumbimuneNo ratings yet
- dentistry-12-00035Document8 pagesdentistry-12-00035expertodentalboliviaNo ratings yet
- The New "Cubism" Graft Technique in Tympanoplasty - A Randomized Controlled TrialDocument9 pagesThe New "Cubism" Graft Technique in Tympanoplasty - A Randomized Controlled Trialian danarkoNo ratings yet
- Comparison of Direct vs Indirect Sinus Lift ProceduresDocument8 pagesComparison of Direct vs Indirect Sinus Lift ProceduresSooraj SNo ratings yet
- Letter To The Editor: Adenoidectomy: Our ApproachDocument1 pageLetter To The Editor: Adenoidectomy: Our Approachdr.hungsonNo ratings yet
- Esthetic and Functional Reconstruction of Large Mandibular Defects Using Free Fibula Flap and Implant-Retained Prosthetics - A Case Series With Long-Term Follow-UpDocument7 pagesEsthetic and Functional Reconstruction of Large Mandibular Defects Using Free Fibula Flap and Implant-Retained Prosthetics - A Case Series With Long-Term Follow-UppankajNo ratings yet
- The Bone Lid Technique in Lateral Sinus Lift: A Systematic Review and Meta-AnalysisDocument20 pagesThe Bone Lid Technique in Lateral Sinus Lift: A Systematic Review and Meta-Analysisdr.hryhorenkoNo ratings yet
- Osseodensificação Com o TarcioDocument7 pagesOsseodensificação Com o Tarcioalessandra camposNo ratings yet
- Implants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitDocument5 pagesImplants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitNIMMY ANTONo ratings yet
- Three-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyDocument10 pagesThree-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyFabian Sanabria100% (1)
- Is Flapless Implant Surgery A Viable Option in Posterior Maxilla? A ReviewDocument8 pagesIs Flapless Implant Surgery A Viable Option in Posterior Maxilla? A ReviewMr-Ton DrgNo ratings yet
- JDentImplant10293-1963477 052714Document6 pagesJDentImplant10293-1963477 052714DrRobin SabharwalNo ratings yet
- Periodontology 2000 - 2023 - Urban 2Document19 pagesPeriodontology 2000 - 2023 - Urban 2Spotify GuillemNo ratings yet
- Immediate Dentoalveolar Restoration in Compromised Sockets: Technique and Bone BiologyDocument14 pagesImmediate Dentoalveolar Restoration in Compromised Sockets: Technique and Bone BiologyMichal PerkowskiNo ratings yet
- Review Cirugía Preprotésica. ArtículoDocument9 pagesReview Cirugía Preprotésica. ArtículoAnita Estela Batz MatulNo ratings yet
- Clinical Case Reports - 2016 - Ronco - A Novel Suturing Approach For Tissue Displacement Within Minimally InvasiveDocument7 pagesClinical Case Reports - 2016 - Ronco - A Novel Suturing Approach For Tissue Displacement Within Minimally InvasiveÄpriolia SuNo ratings yet
- Subperiosteal ImplantsDocument5 pagesSubperiosteal ImplantsHélio AlvesNo ratings yet
- Preprosthetic Surgery: An Adjunct To Complete Denture TherapyDocument3 pagesPreprosthetic Surgery: An Adjunct To Complete Denture TherapyrintanfsNo ratings yet
- Asds 06 1448Document7 pagesAsds 06 1448Joao Carlos JuniorNo ratings yet
- Cricchio 2009Document7 pagesCricchio 2009elver galargaNo ratings yet
- 2 AntonioDocument11 pages2 AntonioDany Gonzalez MartinNo ratings yet
- Windisch 등 - 2021 - Vertical-guided bone regeneration with a titaniumDocument12 pagesWindisch 등 - 2021 - Vertical-guided bone regeneration with a titaniumsupercool0120No ratings yet
- ReviewsDocument5 pagesReviewsEdoardo BiancoNo ratings yet
- Lymphatic DrainageDocument49 pagesLymphatic DrainageMehek BatraNo ratings yet
- SM Jurnal 2Document3 pagesSM Jurnal 2Kurnia SelaNo ratings yet
- Long-Term Effects of Vertical Bone Augmentation: A Systematic ReviewDocument15 pagesLong-Term Effects of Vertical Bone Augmentation: A Systematic ReviewShafira Nur Amalia ZulvaNo ratings yet
- Cranioplasty Review of Materials and TechniquesDocument8 pagesCranioplasty Review of Materials and TechniquesCahyo Adi BaskoroNo ratings yet
- Comparacion Entre Las Fuerzas de Adhesion Entre Distintos AdhesivosDocument7 pagesComparacion Entre Las Fuerzas de Adhesion Entre Distintos AdhesivosMONICA XIMENA ERAS VARGASNo ratings yet
- Alveolar Distraction Osteogenesis For Dental Implant Preparation: An UpdateDocument25 pagesAlveolar Distraction Osteogenesis For Dental Implant Preparation: An UpdateABKarthikeyanNo ratings yet
- Kazanjian implantes IIDocument3 pagesKazanjian implantes IIMaximiliano Jara ContrerasNo ratings yet
- 20 Maxillary Sinus Floor Elevation Techniques With Recent Advances A Literature ReviewDocument18 pages20 Maxillary Sinus Floor Elevation Techniques With Recent Advances A Literature Reviewrahma medikawatyNo ratings yet
- Maxillary Sinus Augmentation: Tarun Kumar A.B, Ullas AnandDocument13 pagesMaxillary Sinus Augmentation: Tarun Kumar A.B, Ullas Anandyuan.nisaratNo ratings yet
- Endoscopic Transcanal Stapedotomy Our Experiences at A Tertiary Care Teaching Hospital of Eastern IndiaDocument5 pagesEndoscopic Transcanal Stapedotomy Our Experiences at A Tertiary Care Teaching Hospital of Eastern IndiaAbderrahim BOURIALNo ratings yet
- Periodontology 2000 - 2023 - Urban - Minimal Invasiveness in Vertical Ridge AugmentationDocument19 pagesPeriodontology 2000 - 2023 - Urban - Minimal Invasiveness in Vertical Ridge AugmentationLEONARDO ALBERTO CRESPIN ZEPEDANo ratings yet
- Saddle Nose DeformityDocument7 pagesSaddle Nose DeformityjgskNo ratings yet
- JC9 - 2 PDFDocument7 pagesJC9 - 2 PDFshraddhaNo ratings yet
- Clin Implant Dent Rel Res - 2014 - LinkeviciusDocument9 pagesClin Implant Dent Rel Res - 2014 - Linkeviciusfernando vicenteNo ratings yet
- Atraumatic Exo NarativeDocument6 pagesAtraumatic Exo NarativeT.Aditya P.P.No ratings yet
- Ridge Preservation Using Collagen Plug TechniqueDocument9 pagesRidge Preservation Using Collagen Plug TechniqueNancyLiaoNo ratings yet
- Ab 2019Document7 pagesAb 2019Dome CárdenasNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- Stage-Two Surgery For Dental Implants: Overview and Relevance of Advanced ProceduresDocument5 pagesStage-Two Surgery For Dental Implants: Overview and Relevance of Advanced ProceduresasclepiuspdfsNo ratings yet
- Temporal Fascia in Diced Cartilage-Fascia GraftsDocument1 pageTemporal Fascia in Diced Cartilage-Fascia GraftsAlexiNo ratings yet
- Pi Is 0099239916310214Document5 pagesPi Is 0099239916310214Alina AlexandraNo ratings yet
- Floratos Et Al. Bone Window Technique in Endodontic Microsurgery Report of Two Cases. Volume 2 2023Document10 pagesFloratos Et Al. Bone Window Technique in Endodontic Microsurgery Report of Two Cases. Volume 2 2023Edward AbadiaNo ratings yet
- Apexum in EndodonticsDocument4 pagesApexum in EndodonticsAmit KumarNo ratings yet
- Ex Vivo Microbial Leakage Analysis of Polytetrafluoroethylene Tape and Cotton Pellet As Endodontic Access Cavity SpacersDocument7 pagesEx Vivo Microbial Leakage Analysis of Polytetrafluoroethylene Tape and Cotton Pellet As Endodontic Access Cavity SpacersAbhishek Isaac MathewNo ratings yet
- Bone Dust and Diced Cartilage Combined With Blood Glue: A Practical Technique For Dorsum EnhancementDocument5 pagesBone Dust and Diced Cartilage Combined With Blood Glue: A Practical Technique For Dorsum EnhancementVLADIMIR RAMIREZ-BLANCOMDNo ratings yet
- Anterior Ridge Extension Using Modified Kazanjian Technique in Mandible-A Clinical StudyDocument5 pagesAnterior Ridge Extension Using Modified Kazanjian Technique in Mandible-A Clinical StudyHélder MouraNo ratings yet
- VestibuloplastyDocument6 pagesVestibuloplastyZullia TaftyantiNo ratings yet
- Evolution in Preprosthetic Surgery Current Trends: A ReviewDocument7 pagesEvolution in Preprosthetic Surgery Current Trends: A Reviewmirah indrianiNo ratings yet
- Impression Techniques For Management of Flabby Ridges in Complete DenturesDocument6 pagesImpression Techniques For Management of Flabby Ridges in Complete DenturesDr Rohit Kumar Singh100% (1)
- Papilla Preservation Flap Techniques ReviewedDocument7 pagesPapilla Preservation Flap Techniques ReviewedReshmaa RajendranNo ratings yet
- Evolution of Mandibular Defects Reconstruction Procedures: From Older Principles To Newer Techniques and TechnologyDocument11 pagesEvolution of Mandibular Defects Reconstruction Procedures: From Older Principles To Newer Techniques and Technologykarthik kumarNo ratings yet
- Implant Catalogue: Your Local Mentor DistributorDocument36 pagesImplant Catalogue: Your Local Mentor DistributorSofia VasconcellosNo ratings yet
- Arry RodjaniDocument7 pagesArry RodjaniyuliaydjwNo ratings yet
- Review of Surgery For ABSITE and Boards 3rd Edition 2023Document493 pagesReview of Surgery For ABSITE and Boards 3rd Edition 2023Endoskopi İzmir100% (1)
- Nasal Surgery Care GuideDocument3 pagesNasal Surgery Care Guidedrbhattacharyya_dNo ratings yet
- Acta 88 134Document9 pagesActa 88 134Andre ErlisNo ratings yet
- Care Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsDocument7 pagesCare Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsSubhasish GiriNo ratings yet
- The Recurrence of Cervical Intraepithelial NeoplasiaDocument5 pagesThe Recurrence of Cervical Intraepithelial NeoplasiaIsmaelJoséGonzálezGuzmánNo ratings yet
- DR Rashmi S R Consultant NephrologyDocument1 pageDR Rashmi S R Consultant Nephrologyanant chauhanNo ratings yet
- 2023 - Analysis On Key Parameters in Subretinal Injection Facilitating A Predictable and Automated Robot-Assisted Treatment in Gene TherapyDocument9 pages2023 - Analysis On Key Parameters in Subretinal Injection Facilitating A Predictable and Automated Robot-Assisted Treatment in Gene Therapycjws80293No ratings yet
- Hospital Network List As On 17-03-2020Document292 pagesHospital Network List As On 17-03-2020Naga Balaram-panduNo ratings yet
- Medi 97 E0094Document5 pagesMedi 97 E0094greenNo ratings yet
- Father of Surgery Ayurveda Kashiraj Divodas DhanvantariDocument12 pagesFather of Surgery Ayurveda Kashiraj Divodas DhanvantariDhruv VaghasiyaNo ratings yet
- Handbook of Equine Respiratory EndosDocument127 pagesHandbook of Equine Respiratory EndosIoana Corbu CostacheNo ratings yet
- BP - LippincottDocument7 pagesBP - LippincottForrest LloydNo ratings yet
- Guided Tissue Regeneration For Implants Placed Into Extraction Sockets and For Implant Dehiscences - Surgical Techniques and Case ReportDocument17 pagesGuided Tissue Regeneration For Implants Placed Into Extraction Sockets and For Implant Dehiscences - Surgical Techniques and Case ReportEugenioNo ratings yet
- Discontinuing IvDocument2 pagesDiscontinuing IvJamaica Leslie NovenoNo ratings yet
- Effect of Platelet-Rich Plasma Injections Vs Placebo On Ankle Symptoms and Function in Patients With Ankle OsteoarthritisDocument11 pagesEffect of Platelet-Rich Plasma Injections Vs Placebo On Ankle Symptoms and Function in Patients With Ankle OsteoarthritisYang LiuNo ratings yet
- Stanford Ortho CurriculumDocument13 pagesStanford Ortho CurriculumGyörgy FabianNo ratings yet
- Total Hip Replacement Protocol Oct 07Document3 pagesTotal Hip Replacement Protocol Oct 07Śĥìmàâ El.mobayedNo ratings yet
- Long-Term Follow Up of 103 Ankylosed Permanent Incisors Surgically Treated With Decoronation - A Retrospective Cohort StudyDocument7 pagesLong-Term Follow Up of 103 Ankylosed Permanent Incisors Surgically Treated With Decoronation - A Retrospective Cohort StudyAnaMariaCastroNo ratings yet
- Operation Theater TechnicianDocument26 pagesOperation Theater TechnicianMohammadSaqibMinhasNo ratings yet
- AIA Group Dental PPO-Plus Panel ClinicsDocument55 pagesAIA Group Dental PPO-Plus Panel ClinicsFoong Ngai Keong0% (1)
- Inca and Pre-Inca MedicineDocument6 pagesInca and Pre-Inca MedicineVALERIA BORJA GIONTINo ratings yet
- Hiroko Minagawa - The Resurrection Fireplace (Retail) (Azw3)Document376 pagesHiroko Minagawa - The Resurrection Fireplace (Retail) (Azw3)Juli?n r?osNo ratings yet
- Tamagond 2011Document5 pagesTamagond 2011Eko SiswantoNo ratings yet
- Techniques of Local Anesthesia: DR Amna Muzaffar BDS Assistant Professor, OmfsDocument123 pagesTechniques of Local Anesthesia: DR Amna Muzaffar BDS Assistant Professor, OmfsAbdul MananNo ratings yet
- Surgical Techniques For Pancreas Transplantation: Ugo Boggi, Gabriella Amorese and Piero MarchettiDocument10 pagesSurgical Techniques For Pancreas Transplantation: Ugo Boggi, Gabriella Amorese and Piero MarchettiNatalindah Jokiem Woecandra T. D.No ratings yet
- Lesson Plan On Hospital PlanningDocument63 pagesLesson Plan On Hospital PlanningSamba SukanyaNo ratings yet
- Torts Cases IIDocument32 pagesTorts Cases IIRgenieDictado100% (1)
- Teekshana Kshara Method for Hemorrhoids CureDocument4 pagesTeekshana Kshara Method for Hemorrhoids CureDrHassan Ahmed ShaikhNo ratings yet