Professional Documents
Culture Documents
Cardiovascular Risks From Fine Particulate Air Pollution NEJM
Uploaded by
alejandro toro riveraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Risks From Fine Particulate Air Pollution NEJM
Uploaded by
alejandro toro riveraCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
edi t or i a l s
Cardiovascular Risks from Fine Particulate Air Pollution
Douglas W. Dockery, Sc.D., and Peter H. Stone, M.D.
More than a decade ago, prospective epidemio- PM10), sulfur dioxide, nitrogen dioxide, carbon
logic studies showed that mortality was increased monoxide, and ozone. The WHI study considered
among people living in communities with ele- all of these community air pollutants and found
vated concentrations of fine particulate air pol- cardiovascular risk associated only with PM2.5
lution.1,2 Subsequent research has shown that concentrations. Whereas earlier work compared
particulate air pollution is statistically and mecha- levels of air pollution and rates of death between
nistically linked to increased cardiovascular dis- various cities, the WHI investigators were also
ease.3 New data are beginning to shed light on able to compare areas within individual cities.
which persons are at heightened risk. Their analysis demonstrated a relationship be-
In this issue of the Journal, Miller et al.4 report tween increased levels of fine particulate pollu-
on data from the Women’s Health Initiative (WHI) tion and higher rates of death and complications
observational study, which greatly expands our from cardiovascular and cerebrovascular disease,
understanding of how fine particulate pollution depending not only on which city a person lived
affects health. Earlier long-term prospective co- in but also on where in that city she lived.
hort studies showed an association between lev- Perhaps most important, the WHI study es-
els of air pollution consisting of particulate mat- tablished a stronger statistical association be-
ter of less than 2.5 μm in aerodynamic diameter tween fine particulate air pollution and death
(PM2.5) and an elevated risk of death from all from coronary heart disease than that found in
causes and from cardiovascular disease.1,2,5 The earlier studies. In the WHI study, Miller et al. found
WHI study broadens the scope by finding that an increased relative risk of 1.76 for death from
nonfatal cardiovascular events are also strongly cardiovascular disease for every increase of 10 μg
associated with fine particulate concentrations per cubic meter in the mean concentration of
in the community. Earlier work relied solely on PM2.5.4 By comparison, a study by the American
death certificates to define the rate of death from Cancer Society showed that each increase of 10 μg
cardiovascular disease. In the WHI study, cardio- per cubic meter in the mean PM2.5 concentration
vascular events and mortality were defined by was associated with an increased relative risk of
objective review of medical records. The earlier 1.12 for death from cardiovascular disease, 1.18
studies were designed to identify risk factors for for death from ischemic heart disease (the larg-
respiratory disease1 and cancer2 and therefore had est proportion of deaths), and 1.13 for death from
limited ability to adjust for cardiovascular risk arrhythmia, heart failure, or cardiac arrest.5
factors. The WHI observational study was de- Samples in previous studies consisted of sub-
signed to assess the risk of cardiovascular events jects from the entire population of the cities be-
and therefore could exclude cardiovascular risk ing investigated. The WHI analysis was restrict-
factors as explanations for the observed associ- ed to postmenopausal women with no history
ations with air pollution. of cardiovascular health problems. A 22-year fol-
Earlier studies did not include data on the full low-up of a cohort of nonsmoking white adults
range of regulated community air pollutants in California showed an increased risk of death
— that is, PM2.5 (and the larger particle fraction, from coronary heart disease with rising levels of
n engl j med 356;5 www.nejm.org february 1, 2007 511
The New England Journal of Medicine
Downloaded from nejm.org at STOCKHOLMS UNIVERSTITETSBIBL on August 10, 2015. For personal use only. No other uses without permission.
Copyright © 2007 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
fine particulate air pollution in women but not lution has been found to lead to rapid and sig-
in men.6 Does this suggest that the WHI popula- nificant increases in fibrinogen, plasma viscos-
tion, or women in general, are more sensitive to ity, platelet activation, and release of endothelins,
the cardiovascular effects of particulate air pol- a family of potent vasoconstrictor molecules.3
lution? Taken together, these studies suggest that the
Women have a distinctly different profile of status of cardiovascular risk factors has a substan-
coronary disease. In the Women’s Ischemia Syn- tial effect on susceptibility to the adverse effects
drome Evaluation study, the cluster of conditions of particulate air pollution. A particularly ap-
that increase the risk of vascular disease (e.g., hy- pealing aspect of the design of the WHI study is
pertension, diabetes, obesity, and inactivity) was the range of data collected on all subjects, in-
seen more frequently in postmenopausal women cluding demographic and lifestyle characteris-
than in men.7 Women’s coronary arteries are tics, cardiovascular risk factors, medical history,
smaller in size and tend to harbor more diffuse diet, and medications. With this wealth of data,
atherosclerosis than do men’s arteries, and wom- the next generation of analyses should be able to
en’s microvessels appear to be more frequently focus risk stratification even further to identify
dysfunctional than those of men.7 Indeed, in the the characteristics of persons who are most sus-
Euro Heart Survey, although women were less ceptible to the adverse effects of air pollution.
likely than men to have fixed atherosclerotic ob- A multifaceted approach that encompasses
structive disease, among patients undergoing elec- both public health and medical interventions is
tive diagnostic angiography for angina, women needed to reduce the burden of cardiovascular
with confirmed coronary disease had twice the disease attributable to air pollution. Comprehen-
risk of death or myocardial infarction as that of sive management of the harmful effects of fine
men.8 These findings suggest that sex may not particles must start with intensive efforts to re-
define susceptibility to air pollution but, rather, duce this destructive form of air pollution. Fine
may be an indicator of an underlying cardiac sub- particulate air pollution results not only from
strate that puts women at increased risk. the combustion of carbonaceous fuels in our ve-
Characteristics that define increased cardio- hicles, power plants, and factories but also from
vascular susceptibility to particulate air pollution secondary particles produced by oxidation of gas-
have also been identified in men. Stronger asso- eous pollutants emitted by these same sources.
ciations between fine particulate concentrations The evidence that has accumulated thus far re-
and abnormal variability in heart rate were re- garding the health threat from PM2.5 pollution is
ported in asymptomatic men with higher Fra- convincing enough to have prompted the Envi-
mingham cardiovascular risk scores.9 PM2.5 was ronmental Protection Agency (EPA) to lower the
more strongly associated with impaired autonom- short-term (24-hour) standard for fine particu-
ic cardiovascular function in men with genotypic late concentration that communities must achieve.
and phenotypic indicators of increased systemic Unfortunately for public health, the EPA failed
inflammation and oxidative stress than in those to follow the recommendation of its science
without these markers.10 However, the increased advisers and reduce the long-term standard for
susceptibility was not found among men taking fine particles.12 The findings of the WHI study
statins, which both improve lipid profiles and strongly support the recommendation for tight-
reduce systemic inflammation. er standards for long-term fine particulate air
The mechanisms by which fine particulate air pollution.
pollution influence the risk of cardiovascular Even with tighter standards, people will con-
disease are still under investigation. There is evi- tinue to be exposed to fine particulate air pollu-
dence that inhalation of particulate air pollution tion. Although the public health burden of car-
creates and exacerbates both pulmonary and sys- diovascular disease attributable to air pollution is
temic inflammation and oxidative stress, leading large, the evidence suggests that individual risks
to direct vascular injury, atherosclerosis, and au- are modest. If the WHI and other studies can
tonomic dysfunction.3 Buildup of atherosclerotic identify intrinsic and acquired individual factors
plaque, measured by the carotid intima–media that lead to increased adverse cardiovascular re-
thickness, is higher in communities with higher sponses to air pollution, then it should be pos-
mean PM2.5 concentrations.11 Particulate air pol- sible to offer focused interventions to persons who
512 n engl j med 356;5 www.nejm.org february 1, 2007
The New England Journal of Medicine
Downloaded from nejm.org at STOCKHOLMS UNIVERSTITETSBIBL on August 10, 2015. For personal use only. No other uses without permission.
Copyright © 2007 Massachusetts Medical Society. All rights reserved.
editorials
are at greatest risk and thereby ameliorate at least 5. Pope CA III, Burnett RT, Thurston GD, et al. Cardiovascular
mortality and long-term exposure to particulate air pollution:
some of the patient-specific damages of air pol- epidemiological evidence of general pathophysiological pathways
lution. of disease. Circulation 2004;109:71-7.
Dr. Dockery reports receiving a stipend from Industrial Eco- 6. Chen LH, Knutsen SF, Shavlik D, et al. The association be-
nomics for participation in an expert-opinion study. No other tween fatal coronary heart disease and ambient particulate air
potential conflict of interest relevant to this article was reported. pollution: are females at greater risk? Environ Health Perspect
2005;113:1723-9. [Erratum, Environ Health Perspect 2006;114:
From the Department of Environmental Health, Harvard School A21.]
of Public Health (D.W.D.), and the Cardiovascular Division, 7. Pepine CJ, Kerensky RA, Lambert CR, et al. Some thoughts
Brigham and Women’s Hospital and Harvard Medical School on the vasculopathy of women with ischemic heart disease. J Am
(P.H.S.) — both in Boston. Coll Cardiol 2006;47:Suppl 3:S30-S35.
8. Daly C, Clemens F, Lopez Sendon JL, et al. Gender differences
1. Dockery DW, Pope CA III, Xu X, et al. An association be- in the management and clinical outcome of stable angina. Cir-
tween air pollution and mortality in six U.S. cities. N Engl J Med culation 2006;113:490-8.
1993;329:1753-9. 9. Chen JC, Stone PH, Verrier RL, et al. Personal coronary risk
2. Pope CA III, Thun MJ, Namboodiri MM, et al. Particulate air profiles modify autonomic nervous system responses to air pol-
pollution as a predictor of mortality in a prospective study of lution. J Occup Environ Med 2006;48:1133-42.
U.S. adults. Am J Respir Crit Care Med 1995;151:669-74. 10. Schwartz J, Park SK, O’Neill MS, et al. Glutathione-S-trans-
3. Brook RD, Franklin B, Cascio W, et al. Air pollution and ferase M1, obesity, statins, and autonomic effects of particles:
cardiovascular disease: a statement for healthcare profession- gene-by-drug-by-environment interaction. Am J Respir Crit Care
als from the Expert Panel on Population and Prevention Science Med 2005;172:1529-33.
of the American Heart Association. Circulation 2004;109:2655- 11. Kunzli N, Jerrett M, Mack WJ, et al. Ambient air pollution
71. and atherosclerosis in Los Angeles. Environ Health Perspect
4. Miller KA, Siscovick DS, Sheppard L, et al. Long-term ex- 2005;113:201-6.
posure to air pollution and incidence of cardiovascular events 12. The politics of breathing. Nature 2006;444:248-9.
in women. N Engl J Med 2007;356:447-58. Copyright © 2007 Massachusetts Medical Society.
The Healing Power of Listening in the ICU
Craig M. Lilly, M.D., and Barbara J. Daly, Ph.D, R.N.
Critical care services are highly valued because tions, articulate the patient’s values, express pain-
they can often restore function in patients with ful emotions, discuss concerns, and obtain help
acute life-threatening illnesses. In this context, with managing feelings of guilt.3
advances in medical science have led to increased A clinical course that runs counter to the fami-
expectations for favorable outcomes of episodes ly’s hopes and expectations is extraordinarily
of critical illness, even when the patient has se- stressful and is an important contributor to ICU-
vere coexisting chronic disease. The growing de- related post-traumatic stress disorder (PTSD)
mand for critical care has led both to increased among families.4 A better understanding of how
numbers of patients who survived with desirable intensive care clinicians can support families as
functional outcomes and to increased numbers they make the transition from a goal of cure to
of patients who die in the intensive care unit (ICU). one of comfort and acceptance of death is clear-
Today, many deaths in the ICU occur after a de- ly needed. Recognition of the relationship be-
cision has been made to discontinue or forgo ad- tween satisfaction, on the one hand, and expecta-
vanced supportive technology.1 Decisions to shift tions, perceptions, and prognosis, on the other
from apparently ineffective technology to a treat- hand, can lead to communication processes that
ment plan that focuses primarily on the patient’s synchronize the perceptions of family members
comfort are usually made in discussions between with those of providers and close gaps between
caregivers and family members.2 These discus- reality and expectations. Curtis and colleagues
sions involve complex conversations and are im- have described some of the components of a sys-
portant to families. Communication processes tem of communication that is being increasingly
that have been shown to improve the well-being recognized as an effective means of promoting
of patients and family members include proac- harmony between critical care providers and fam-
tive, multidisciplinary sessions that provide pa- ilies.5 This five-part system, known by the mne-
tients (when they are able to communicate) and monic VALUE, includes the following elements:
family members with the opportunity to ask ques- valuing and appreciating what the family mem-
n engl j med 356;5 www.nejm.org february 1, 2007 513
The New England Journal of Medicine
Downloaded from nejm.org at STOCKHOLMS UNIVERSTITETSBIBL on August 10, 2015. For personal use only. No other uses without permission.
Copyright © 2007 Massachusetts Medical Society. All rights reserved.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- Charcot Bouchard Aneurysm - StatPearls - NCBI BookshelfDocument10 pagesCharcot Bouchard Aneurysm - StatPearls - NCBI Bookshelfalejandro toro riveraNo ratings yet
- Interpreting The Kansas City Cardiomyopathy QuestiDocument12 pagesInterpreting The Kansas City Cardiomyopathy Questialejandro toro riveraNo ratings yet
- Global Prevalence of Injecting Drug Use and Sociodemographic Characteristics and Prevalence of HIV, HBV, and HCV in People Who Inject DrugsDocument16 pagesGlobal Prevalence of Injecting Drug Use and Sociodemographic Characteristics and Prevalence of HIV, HBV, and HCV in People Who Inject Drugsalejandro toro riveraNo ratings yet
- Drug Induced Liver Injury Secondary To Herbal and Dietary SupplementsDocument15 pagesDrug Induced Liver Injury Secondary To Herbal and Dietary Supplementsalejandro toro riveraNo ratings yet
- Liver HistologyDocument14 pagesLiver Histologyalejandro toro riveraNo ratings yet
- Occupational Exposure To Genotoxic AgentsDocument20 pagesOccupational Exposure To Genotoxic Agentsalejandro toro riveraNo ratings yet
- Oxidative Stress and Inflammation Generated DNA Damage by Exposure To Air Pollution ParticlesDocument34 pagesOxidative Stress and Inflammation Generated DNA Damage by Exposure To Air Pollution Particlesalejandro toro riveraNo ratings yet
- Biomonitoring Human Exposure To Household Air Pollution and Association With Self-Reported Health Symptoms - A Stove Intervention Study in PeruDocument9 pagesBiomonitoring Human Exposure To Household Air Pollution and Association With Self-Reported Health Symptoms - A Stove Intervention Study in Perualejandro toro riveraNo ratings yet
- Hypoparathyroidism NEJM 2019 PDFDocument10 pagesHypoparathyroidism NEJM 2019 PDFalejandro toro riveraNo ratings yet
- Ambient Air Pollution and Mortality in 652 Cities NEJMDocument4 pagesAmbient Air Pollution and Mortality in 652 Cities NEJMalejandro toro riveraNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
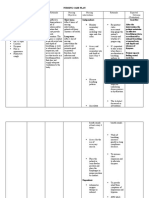
- NCP ScribdDocument3 pagesNCP ScribdAngela AyalaNo ratings yet
- MICROQUESDocument32 pagesMICROQUESYangyang R. AzradNo ratings yet
- Template-PPT-UEU-Pertemuan-4 - Giving Direction, Explaining, DescribingDocument16 pagesTemplate-PPT-UEU-Pertemuan-4 - Giving Direction, Explaining, DescribingNining SagitaNo ratings yet
- AJGP 06 2021 Clinical Patel When Eyes Are Dry WEBDocument8 pagesAJGP 06 2021 Clinical Patel When Eyes Are Dry WEBalex.ttkNo ratings yet
- Rheumatic Fever& IE MCQDocument7 pagesRheumatic Fever& IE MCQLedia EssamNo ratings yet
- Italy Responds To COVID-19Document102 pagesItaly Responds To COVID-19Zerohedge100% (1)
- SD Bioline Influenza Ag A B A h1n1 PandemicDocument1 pageSD Bioline Influenza Ag A B A h1n1 PandemicYunescka MorenoNo ratings yet
- Laboratory Studies: FecalysisDocument2 pagesLaboratory Studies: FecalysisKris TejereroNo ratings yet
- The Pentagon Bio-Weapons - Dilyana - BGDocument1 pageThe Pentagon Bio-Weapons - Dilyana - BGTW100% (4)
- PREVENTIVEDocument12 pagesPREVENTIVEDivine SangutanNo ratings yet
- CAREPLAN For CholangitisDocument3 pagesCAREPLAN For CholangitisNatty-oneBonafide100% (2)
- Hair Growth Disorders N Pigmentary DisordersDocument7 pagesHair Growth Disorders N Pigmentary Disordersmrosaregina michelleNo ratings yet
- Guía Manejo Del Shock 2023Document67 pagesGuía Manejo Del Shock 2023Alvaro ArriagadaNo ratings yet
- AmebiasisDocument34 pagesAmebiasisashuNo ratings yet
- Dermoscopy ChallengeDocument2 pagesDermoscopy ChallengegongutzNo ratings yet
- Immunization InstructionsDocument2 pagesImmunization InstructionsAli SadeqiNo ratings yet
- STD StiDocument2 pagesSTD StiDexter PasionNo ratings yet
- Food Allergy-1Document27 pagesFood Allergy-1donald duckNo ratings yet
- Prep 2015Document792 pagesPrep 2015Imran A. IsaacNo ratings yet
- Overlooked 150 Year Old Household Cleaner A Remedy For Swine Flu?Document4 pagesOverlooked 150 Year Old Household Cleaner A Remedy For Swine Flu?nsmith7100% (2)
- Correspondence: Enteric Involvement in Hospitalised Patients With COVID-19 Outside WuhanDocument2 pagesCorrespondence: Enteric Involvement in Hospitalised Patients With COVID-19 Outside WuhanSeri Agustin SartikaNo ratings yet
- Module 2: Diagnosis and Staging of Paediatric HIVDocument69 pagesModule 2: Diagnosis and Staging of Paediatric HIVAlvin OmondiNo ratings yet
- Infectious and Non-Infectious DiseasesDocument2 pagesInfectious and Non-Infectious DiseasesJanice ChingNo ratings yet
- MononucleosisDocument9 pagesMononucleosisLucas TobingNo ratings yet
- Nurse Np1 Board CramsheetDocument8 pagesNurse Np1 Board CramsheetZero TwoNo ratings yet
- Adjuvant and Neoadjuvant ChemotherapyDocument22 pagesAdjuvant and Neoadjuvant Chemotherapyprabushankar7No ratings yet
- Classification of Periodontal Diseases PerioDocument42 pagesClassification of Periodontal Diseases PerioFourthMolar.comNo ratings yet
- Critical Health Concerns of The 21st CenturyDocument2 pagesCritical Health Concerns of The 21st CenturySafa AamirNo ratings yet
- What Are The Similarities Between Flu and CovidDocument1 pageWhat Are The Similarities Between Flu and CovidZakya Oumelbanine KlNo ratings yet
- DermatitisDocument6 pagesDermatitisNader SmadiNo ratings yet