Professional Documents
Culture Documents
Brain Module Worksheet
Uploaded by
rayOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brain Module Worksheet
Uploaded by
rayCopyright:
Available Formats
Brain Module Worksheet
Site: BRAIN
Student Name: Raymond Hove Date: 1/05/19
Patient Info:
Age: Gender: M
Presentation:
1. Six week history of migraine, memory, fatigue and unexplained short-temperedness.
a. Raised ICP from the tumor pushing onto the brain would have resulted in the following
symptoms
Diagnosis:
1. Right temporal-parietal Grade 4 Glioblastoma Multiforme
a. most common type of astrocytoma that occurs in adults)
Prognosis
1. Very aggressive = median survival is 9-12 months with RT that is followed by surgery.
2. Infiltrative nature + proximity to critical structure makes surgical resection not feasible without
compromising neurological function and also it makes hard to determine tumour margins accurately
Medical history/comorbidities:
1. not a surgical candidate due to his co-morbidities (ischaemic heart disease)
2. Biopsy is also not possible therefore tumor cannot be graded
Prescription: Long course: 60Gy in 30#, 2Gy/#, I#/day over 6 weeks to the ICRU Reference
point
Intent: Curative dose with a palliative Intent of prolonging pt life
Other treatments for this diagnosis: concurrent chemotherapy (TMZ) which a
radiosensitizer
Department of Radiation Therapy, University of Otago Wellington 2019
CT:
Positioning/Immobilisation:
How would this pt be set-up in your department?
1. HFS
2. H/N Board
3. Thermoplastic mask
4. Mattress
5. NRM
6. LR
7. HOA + ring
CT preparation required:
Is there anything this pt needs to do to prepare for CT in your department?
Contrast
Scan Levels:
What anatomy needs to be included in the scan and why?
1. Scano: SUP margin of H/N Board to Mid chest
2. Scan Levels: SUP same as Scano & INF to just below the shoulders
a. For vertex beams and below the shoulders for planners if they want couch kick and ensure we
got all OARS
Do any markers/wires or bolus or packing need to be placed for CT?:
1. Angiocaths
a. Ant M/L forehead
b. 2 Laterals in general location we’re treating (stable position)
Planning:
Volumes:
List the volumes present, what is included in each (including margin size) and whether the
margin seems appropriate.
1. CTV
2. PTV – has a uniform margin around the CTV of approximately 1cm in the
anterior, left and right aspect of the CTV however in the post margin its around
1.8cm
For the PTV note the size, shape and location (this will influence beam arrangement)
o Size: Medium
o Shape: circular
o Location: Right, slightly inferior and posterior
Department of Radiation Therapy, University of Otago Wellington 2019
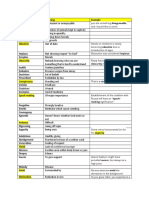
OAR:
List the OAR present and their tolerance doses (use departmental tolerance doses where
applicable). Indicate which structures will need to be contoured.
OARs Departmental tolerances
(max dose)
Brainstem <60Gy
Optic nerves <60Gy
Lens <6Gy cataract
Optic chiasm <60Gy
Inhomogeneities:
List inhomogeneities present and their RED’s. Indicate if any density overrides are required.
1. Soft Tissue = 1.0
2. Bone = 1.3 -1.8
Proposed Beam Arrangement:
Consider size, shape and location of PTV as well as surrounding OAR - draw a diagram
below: 3 Field arrangement = LPO + RAO + RPO
Energy:
Considering depth to the PTV and entry and exit dose to OAR, indicate which energies you
think you will use for each beam
1. Considering size, shape, and location of tumour – 6/10MV (tumor is relatively more
superficial)
Weightings:
Considering depth to the PTV and entry and exit dose to OAR, list your beams below in order
of expected weighting, highest to lowest
1. Right will be weighted the highest because its closer to PTV so have the highest dose
affecting less amount of tissue
2. evenly weighted: RPO contributing dose to the most tissue therefore low weight to
decrease dose to OARs
Wedges:
List the beams which will require wedges, note the orientation and estimate the size (this may
just be “large” or “small”)
1. LPO and RAO will have 45o EDW due to the beam arrangement to alter dose
distribution to medial aspect of PTV. The beams are fairly close to each other causing
beam overlaps = high dose regions hence why we need large wedges
Department of Radiation Therapy, University of Otago Wellington 2019
Treatment:
Isocentre position:
What information will you need to give treatment so that they can locate the planned
treatment isocentre? Think about the process you have seen in your department on day 1 of
treatment.
Imaging:
What kind of imaging would this patient receive whilst on treatment if they were to be treated
in your department? How frequent would this imaging be? What structures would be matched
to?
1. Daily KV/KV imaging
a. Matching to orbits for L/R and S/I
b. Matching skull A/P and S/I
Treatment preparation:
Is there anything this pt needs to do to prepare for treatment in your department?
1. Because we’re treating the brain, pt may need to take Dex prior to tmt mitigate the
effects of encephalitis which present as headaches, nausea and vomiting, loss of
balance, blurred vision and seizures
Clinical Acceptability:
On completion on your plan state whether or not you think it is a clinically acceptable plan
and why. You will need to consider:
Dose distribution
o ICRU dose variation (dose coverage and CSM)
o Dose homogeneity
o Dose conformity (including hotspots)
Dose to OAR
o Acute reactions that will occur
o Endpoint reactions that will occur
Overall the Plan is clinically acceptable:
1. Dose distribution: CSM is under 107% and it is where I would I expect it to be (where the beams
overlap).
2. Coverage: my 95% is covering 98% of PTV and the minimum of where it is lacking is in location
we’re treating.
Department of Radiation Therapy, University of Otago Wellington 2019
3. Dose is homogenous/even around PTV
4. Dose conformity; - more achievable on lateral aspect of PTV but not medial aspect due to having
square isodose due to beam arrangement but in my plan, I have no hotspots
Dose to OARs
1. all under the dose tolerances so wont expect any endpoint reactions
2. Expect skin reactions – will progress to dry desquamation + temporary hair loss
Additional notes
1. 10 mv is more of an efficient energy because not only does it reduce dose to skin but also
surrounding periphery tissue
2. 10MV less entry but more dose on exit but POP with 10MV, the amount of low entrance from the
entrance outweighs the exit from the exit so therefore less dose on the periphery
3. RPO Contributes more to brain tissue so lower the weighting what about the energy
4. What changes shape of the isodose shape = beam arrangement
5. Note that there is going to be a bolus effect inside the ear and outside so expect some ear reactions
What symptoms is he going to Depended on the part of the brain which is
exhibit affected
What are the problems with Pt won’t be in exact position as there
using MRI fused CT were in CT (not immobilised to
equipment.
Why can’t you plan on MRI Don’t give information on electron
densities which is what we rely when
planning
Department of Radiation Therapy, University of Otago Wellington 2019
You might also like
- Atlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 1: Brain and Neck: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTFrom EverandAtlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 1: Brain and Neck: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTNo ratings yet
- Palliative WorksheetDocument4 pagesPalliative WorksheetrayNo ratings yet
- BREAST Worksheet: Treatment Site: Right BreastDocument4 pagesBREAST Worksheet: Treatment Site: Right BreastrayNo ratings yet
- Hippocampal-Sparing WBRT History of Present Illness: Patient DB Is A 58-Year-Old Male With Now Stage IVDocument10 pagesHippocampal-Sparing WBRT History of Present Illness: Patient DB Is A 58-Year-Old Male With Now Stage IVapi-356936299No ratings yet
- (RADIO 250) LEC 10 Radiation OncologyDocument3 pages(RADIO 250) LEC 10 Radiation OncologyWilliam PinzonNo ratings yet
- Csi Treatment Plan WriteupDocument17 pagesCsi Treatment Plan Writeupapi-632529930No ratings yet
- 6 Total Body IrradiationDocument7 pages6 Total Body Irradiationfreemind_mxNo ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-691277740No ratings yet
- Clinical Oncology Assignment RaverDocument7 pagesClinical Oncology Assignment Raverapi-635923017No ratings yet
- CT Dose IssuesDocument28 pagesCT Dose IssuessanyengereNo ratings yet
- Staceysong Csi ProknowlabDocument15 pagesStaceysong Csi Proknowlabapi-634067897No ratings yet
- Automatic Treatment Planning For VMAT-based TotalDocument12 pagesAutomatic Treatment Planning For VMAT-based TotalAmra IbrahimovicNo ratings yet
- Anaesthesia For Paediatric RadiotherapyDocument7 pagesAnaesthesia For Paediatric RadiotherapykhalidNo ratings yet
- Research Paper-Part 4Document15 pagesResearch Paper-Part 4api-635954562No ratings yet
- Csi PaperDocument9 pagesCsi Paperapi-602488644No ratings yet
- Af Final Clincal ProjectDocument12 pagesAf Final Clincal Projectapi-247864638No ratings yet
- Research Proposal Group 10Document6 pagesResearch Proposal Group 10api-483339757No ratings yet
- WCE - RadBioDocument11 pagesWCE - RadBioJames David AlcantaraNo ratings yet
- Csi Written Assignment 1Document10 pagesCsi Written Assignment 1api-633102425No ratings yet
- March Case StudyDocument9 pagesMarch Case Studyapi-247959633No ratings yet
- Zhang 2006Document11 pagesZhang 2006Karina VallesNo ratings yet
- Pet BrochureDocument20 pagesPet BrochureSheikh Hasnain AliNo ratings yet
- HN Interstitial BrachyDocument99 pagesHN Interstitial BrachySayan DasNo ratings yet
- BJR 20190573Document9 pagesBJR 20190573Raul Matute MartinNo ratings yet
- June Case Study Final RevisedDocument18 pagesJune Case Study Final Revisedapi-213108684No ratings yet
- The Applicability of Stitching Cone Beam CT Scans PresentationDocument19 pagesThe Applicability of Stitching Cone Beam CT Scans Presentationapi-498724117No ratings yet
- May Case StudyDocument18 pagesMay Case Studyapi-213055674No ratings yet
- SC 201543Document7 pagesSC 201543esinsubozatliNo ratings yet
- Final Complete Group3 2Document13 pagesFinal Complete Group3 2api-528136686No ratings yet
- Research Paper-Part 2 1 1 - 1 1Document10 pagesResearch Paper-Part 2 1 1 - 1 1api-635954562No ratings yet
- EBM 2018 - Head and CancersDocument136 pagesEBM 2018 - Head and CancersChandramohan SettyNo ratings yet
- Clinical Oncology Assignment 1Document15 pagesClinical Oncology Assignment 1api-576043594No ratings yet
- Clinical Oncology PaperDocument21 pagesClinical Oncology Paperapi-632827798No ratings yet
- Outline 2Document7 pagesOutline 2api-432489466No ratings yet
- Final Draft3ke Group3Document15 pagesFinal Draft3ke Group3api-632741700No ratings yet
- Artigo Carcinoma NUTDocument6 pagesArtigo Carcinoma NUTlorranatayna202201No ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-484758207No ratings yet
- 2012 Effects of RT in Head and NeckDocument10 pages2012 Effects of RT in Head and NeckCamiDavidNo ratings yet
- Cahan 2015Document2 pagesCahan 2015980Denis FernandezNo ratings yet
- WBRT Plus SIB With Image Guided Intensity-Modulated Radiotherapy For Multiple Brain MetastasesDocument2 pagesWBRT Plus SIB With Image Guided Intensity-Modulated Radiotherapy For Multiple Brain Metastasessanti lestariNo ratings yet
- Lung Carcinoma: Radiotherapy PlanningDocument9 pagesLung Carcinoma: Radiotherapy PlanningTowhidulIslamNo ratings yet
- RadiobiologyDocument3 pagesRadiobiologyemilyNo ratings yet
- Metastasis Cerebral NeurologiaDocument9 pagesMetastasis Cerebral NeurologiaDarioNo ratings yet
- Lung Clinical Lab AssignmentDocument13 pagesLung Clinical Lab Assignmentapi-528136686No ratings yet
- J Ijrobp 2004 11 016Document7 pagesJ Ijrobp 2004 11 016AnharNo ratings yet
- Clinical OncologyDocument13 pagesClinical Oncologyapi-585462575No ratings yet
- Final Rectal Cancer GEC ESTRO Handbook of BrachytherapyDocument14 pagesFinal Rectal Cancer GEC ESTRO Handbook of BrachytherapyRakesh JadhavNo ratings yet
- Dosimetry of Yttrium-Labelled Radiopharmaceuticals For Internal Therapy: Yor Y Imaging?Document12 pagesDosimetry of Yttrium-Labelled Radiopharmaceuticals For Internal Therapy: Yor Y Imaging?sayed hossein hashemiNo ratings yet
- Clinical Oncology PaperDocument16 pagesClinical Oncology Paperapi-632529930No ratings yet
- Clinical Application CTDocument40 pagesClinical Application CTWalaa MajeedNo ratings yet
- Research Paper FinalDocument15 pagesResearch Paper Finalapi-635954562No ratings yet
- Paper Nuclear PhysicsDocument6 pagesPaper Nuclear PhysicsPurbandiniNo ratings yet
- Csi VijayDocument15 pagesCsi Vijayapi-356919224No ratings yet
- Treatment Planning ProjectDocument7 pagesTreatment Planning Projectapi-631250296No ratings yet
- A Combined PET CT Scanner For Clinical o PDFDocument12 pagesA Combined PET CT Scanner For Clinical o PDFwulanNo ratings yet
- Dose Differences Due To Variance in Contours of The Optic ChiasmDocument15 pagesDose Differences Due To Variance in Contours of The Optic Chiasmapi-527662950No ratings yet
- Jovs 03 86Document6 pagesJovs 03 86Natalindah Jokiem Woecandra T. D.No ratings yet
- ConebeamstatementDocument6 pagesConebeamstatementPaweł SieradzkiNo ratings yet
- Ijcri 1001209201412 MalothDocument10 pagesIjcri 1001209201412 MalothFirah Triple'sNo ratings yet
- A Dosimetric Comparison of Coplanar vs. Non-Coplanar VMAT SBRT Techniques For NSCLCDocument9 pagesA Dosimetric Comparison of Coplanar vs. Non-Coplanar VMAT SBRT Techniques For NSCLCapi-269672910No ratings yet
- ProcedureDocument13 pagesProcedurerayNo ratings yet
- RT Triage SystemDocument4 pagesRT Triage SystemrayNo ratings yet
- EK Chemistry PDFDocument364 pagesEK Chemistry PDFray100% (8)
- Even/homogenous Dose Distribution Across PTV: WedgesDocument5 pagesEven/homogenous Dose Distribution Across PTV: WedgesrayNo ratings yet
- 501 Critical Reading QuestionsDocument283 pages501 Critical Reading Questionsapi-3813392100% (9)
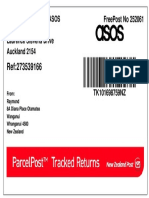
- Rebound Returns - Asos Private Bag 211022 Laurence Stevens Drive Auckland 2154 Freepost No 252061Document1 pageRebound Returns - Asos Private Bag 211022 Laurence Stevens Drive Auckland 2154 Freepost No 252061rayNo ratings yet
- Angry Strong Annoyance or HostilityDocument8 pagesAngry Strong Annoyance or HostilityrayNo ratings yet
- RADT115 2014 Test 2 Posted On Moodle On 9 May 16Document5 pagesRADT115 2014 Test 2 Posted On Moodle On 9 May 16rayNo ratings yet
- Rad 112 Cancer Cell BiologyDocument7 pagesRad 112 Cancer Cell BiologyrayNo ratings yet
- General VocabularyDocument9 pagesGeneral VocabularyrayNo ratings yet
- UMAT 2016 Short Test BookletDocument36 pagesUMAT 2016 Short Test BookletAnonymous rJmcI51No ratings yet
- Radt 215Document5 pagesRadt 215rayNo ratings yet
- MU Calc AnswersDocument2 pagesMU Calc AnswersrayNo ratings yet
- 10cm 1 10cm 1 10cm 1: Decreased FF Increased MUDocument2 pages10cm 1 10cm 1 10cm 1: Decreased FF Increased MUrayNo ratings yet
- Angry Strong Annoyance or HostilityDocument8 pagesAngry Strong Annoyance or HostilityrayNo ratings yet
- Cervix WorksheetDocument4 pagesCervix WorksheetrayNo ratings yet
- Case Study: Raymond HoveDocument20 pagesCase Study: Raymond HoverayNo ratings yet
- Radiobio EQD2 QuestionsDocument2 pagesRadiobio EQD2 QuestionsrayNo ratings yet
- Cervix Formative AssesmentDocument4 pagesCervix Formative AssesmentrayNo ratings yet
- Case StudyDocument8 pagesCase StudyrayNo ratings yet
- Pelatihan Dan Workshop Peningkatan Kompetensi GuruDocument6 pagesPelatihan Dan Workshop Peningkatan Kompetensi Guruhenry jakatariNo ratings yet
- Manual ML 1675 PDFDocument70 pagesManual ML 1675 PDFSergio de BedoutNo ratings yet
- PNP Loan Application Form February 2021 16Document6 pagesPNP Loan Application Form February 2021 16Wilhelm RegaladoNo ratings yet
- Time-Temperature Charge Function of A High Dynamic Thermal Heat Storage With Phase Change MaterialDocument15 pagesTime-Temperature Charge Function of A High Dynamic Thermal Heat Storage With Phase Change Materialgassoumi walidNo ratings yet
- Oxygenation - NCPDocument5 pagesOxygenation - NCPCazze SunioNo ratings yet
- Training Structure - Thinkific Plus TemplateDocument7 pagesTraining Structure - Thinkific Plus TemplateQIONG WUNo ratings yet
- Baumer Tdp02 Tdpz02 Ds enDocument4 pagesBaumer Tdp02 Tdpz02 Ds enQamar ZiaNo ratings yet
- Benefits and Drawbacks of Thermal Pre-Hydrolysis For Operational Performance of Wastewater Treatment PlantsDocument7 pagesBenefits and Drawbacks of Thermal Pre-Hydrolysis For Operational Performance of Wastewater Treatment PlantsmartafhNo ratings yet
- 2017 Hu Spence Why Globalization Stalled and How To Restart ItDocument11 pages2017 Hu Spence Why Globalization Stalled and How To Restart Itmilan_ig81No ratings yet
- The Frozen Path To EasthavenDocument48 pagesThe Frozen Path To EasthavenDarwin Diaz HidalgoNo ratings yet
- RF Based Dual Mode RobotDocument17 pagesRF Based Dual Mode Robotshuhaibasharaf100% (2)
- Title - Dating Virtual To Coffee Table Keywords - Dating, Application BlogDocument3 pagesTitle - Dating Virtual To Coffee Table Keywords - Dating, Application BlogRajni DhimanNo ratings yet
- The Meanings of Goddess PT IIIDocument14 pagesThe Meanings of Goddess PT IIILevonce68No ratings yet
- Benson Ivor - The Zionist FactorDocument234 pagesBenson Ivor - The Zionist Factorblago simeonov100% (1)
- The 100 Best Books For 1 Year Olds: Board Book HardcoverDocument17 pagesThe 100 Best Books For 1 Year Olds: Board Book Hardcovernellie_74023951No ratings yet
- Cooperative LinuxDocument39 pagesCooperative Linuxrajesh_124No ratings yet
- Statistics and Probability Course Syllabus (2023) - SignedDocument3 pagesStatistics and Probability Course Syllabus (2023) - SignedDarence Fujihoshi De AngelNo ratings yet
- Nursing Care Plan For AIDS HIVDocument3 pagesNursing Care Plan For AIDS HIVFARAH MAE MEDINA100% (2)
- Warranty FormDocument13 pagesWarranty FormEmpyrean Builders Corp.No ratings yet
- ReflectionDocument3 pagesReflectionapi-174391216No ratings yet
- Saunders & Cornnet Solution Chapter 1 Part 1Document5 pagesSaunders & Cornnet Solution Chapter 1 Part 1Mo AlamNo ratings yet
- Amazon VS WalmartDocument5 pagesAmazon VS WalmartBrandy M. Twilley100% (1)
- Exchange 2010 UnderstandDocument493 pagesExchange 2010 UnderstandSeKoFieNo ratings yet
- Visvesvaraya Technological University: Jnana Sangama, Belgavi-590018, Karnataka, INDIADocument7 pagesVisvesvaraya Technological University: Jnana Sangama, Belgavi-590018, Karnataka, INDIAShashi KaranNo ratings yet
- Myth or Fact-Worksheet 1Document1 pageMyth or Fact-Worksheet 1Zahraa LotfyNo ratings yet
- Contemporary Architecture Is The Architecture of The 21st Century. No Single Style Is DominantDocument2 pagesContemporary Architecture Is The Architecture of The 21st Century. No Single Style Is DominantShubham DuaNo ratings yet
- Classroom Activty Rubrics Classroom Activty Rubrics: Total TotalDocument1 pageClassroom Activty Rubrics Classroom Activty Rubrics: Total TotalMay Almerez- WongNo ratings yet
- Industrial Automation Using PLCDocument29 pagesIndustrial Automation Using PLCAditya JagannathanNo ratings yet
- Kalitantra-Shava Sadhana - WikipediaDocument5 pagesKalitantra-Shava Sadhana - WikipediaGiano BellonaNo ratings yet
- Hssive-Xi-Chem-4. Chemical Bonding and Molecular Structure Q & ADocument11 pagesHssive-Xi-Chem-4. Chemical Bonding and Molecular Structure Q & AArties MNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)