Professional Documents
Culture Documents
Palliative Worksheet
Uploaded by
rayOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Palliative Worksheet
Uploaded by
rayCopyright:
Available Formats
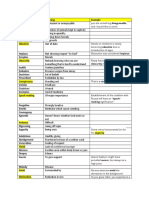
Palliative Worksheet
Site: L4 & LT HIP
Patient Info:
Age: 68 Gender: M
Diagnosis: metastatic prostate cancer
Medical history/comorbidities:
Prostatectomy 2015 for Gleason 4+4 adenocarcinoma
Pt had a rising PSA level since 2017 which reached 20.1 ng/mL- commenced Zoladex which
had a positive effect reducing his PSA to 13.3
Father died of prostate cancer (possible familial link)
Prescription: 20Gy/ 5 fx, 4Gy/# over I week
Intent: Palliative with the intent of relieving his pain
Other treatments for this diagnosis (concurrent or adjuvant?):
Hormone therapy – Zoladex = GnRH agonist
Psychosocial:
1. Recently retired – financial problems since relying on single income assuming the
wife is still working.
MDT -Those undergoing radiotherapy need specialist input from experienced radiographers, nurses
and physiotherapists to help them to rehabilitate and regain neurological function
CT:
Positioning/Immobilisation:
How would this pt be set-up in your department?
1. HFS
2. Mattress
3. NRF
4. LR(not indexed)
CT preparation required:
Is there anything this pt needs to do to prepare for CT in your department?
Pain medication could be taken before CT
Scan Levels:
What anatomy needs to be included in the scan and why?
Do any markers/wires or bolus or packing need to be placed for CT?:
Angiocaths
Department of Radiation Therapy, University of Otago Wellington 2019
Planning:
Volumes:
List the volumes present, what is included in each (including margin size) and whether the
margin seems appropriate.
VOI = volume of interest
For the PTV note the size, shape and location
1. LEFT HIP – VOI is large, circular and located in pelvis region with a margin size of 1 cm
2. L4 VERTEBRAE – VOI is medium size, circular located deep in the abdomen pelvic region
OAR:
List the OAR present and their tolerance doses (use departmental tolerance doses where
applicable). Indicate which structures will need to be contoured.
1. L4 vertebrae – Spinal cord & small bowel
2. Left Hip – Small bowel + bladder + rectum
Inhomogeneities:
List inhomogeneities present and their RED’s. Indicate if any density overrides are required.
Soft tissue
Bone
Gas (small bowel)
Proposed Beam Arrangement:
Consider size, shape and location of PTV as well as surrounding OAR - draw a diagram below
Parallel Opposed Pair for both Plans
Energy:
Considering depth to the PTV and entry and exit dose to OAR, indicate which energies you
think you will use for each beam
1. L4 Plan = 18MV for both tmt field
2. PELVIC = 6MV for ANT beam & 18MV for POST beam
Department of Radiation Therapy, University of Otago Wellington 2019
Weightings:
Considering depth to the PTV and entry and exit dose to OAR, list your beams below in
order of expected weighting, highest to lowest
1. Posterior will be highly weighted because the distance from skin to vertebral bodies will be
small
Wedges:
List the beams which will require wedges, note the orientation and estimate the size (this
may just be “large” or “small”)
At this stage = No
Treatment:
Isocentre position:
What information will you need to give treatment so that they can locate the planned
treatment isocentre? Think about the process you have seen in your department on day 1 of
treatment.
Imaging:
What kind of imaging would this patient receive whilst on treatment if they were to be
treated in your department? How frequent would this imaging be? What structures would
be matched to?
Daily KV Imaging – bony match = for bony matches
Treatment preparation:
Is there anything this pt needs to do to prepare for treatment in your department?
Daily antiemetics – case to case basis because some people find that they don’t need antiemetics
Department of Radiation Therapy, University of Otago Wellington 2019
Clinical Acceptability:
On completion on your plan state whether or not you think it is a clinically acceptable plan
and why. You will need to consider:
Dose distribution
o ICRU dose variation (dose coverage and CSM)
o Dose homogeneity
o Dose conformity (including hotspots)
Dose to OAR
o Acute reactions that will occur _ faint reddening of skin
o Endpoint reactions that will occur_ None at this point
Department of Radiation Therapy, University of Otago Wellington 2019
You might also like
- Clinical Applications of Nuclear Medicine Targeted TherapyFrom EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNo ratings yet
- BREAST Worksheet: Treatment Site: Right BreastDocument4 pagesBREAST Worksheet: Treatment Site: Right BreastrayNo ratings yet
- Computed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideFrom EverandComputed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideNo ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-691277740No ratings yet
- Atlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrom EverandAtlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrieder BerrNo ratings yet
- Brain Module WorksheetDocument5 pagesBrain Module WorksheetrayNo ratings yet
- Clinical Oncology Assignment RaverDocument7 pagesClinical Oncology Assignment Raverapi-635923017No ratings yet
- March Case StudyDocument13 pagesMarch Case Studyapi-212894050No ratings yet
- March Case StudyDocument7 pagesMarch Case Studyapi-210258673No ratings yet
- Case Study 1Document4 pagesCase Study 1api-271668042No ratings yet
- ClinoncDocument15 pagesClinoncapi-631736561No ratings yet
- June Case Study Final RevisedDocument18 pagesJune Case Study Final Revisedapi-213108684No ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-484758207No ratings yet
- Protocol SummaryDocument4 pagesProtocol Summaryapi-631272802No ratings yet
- Rough Draft 1 - Group 3Document9 pagesRough Draft 1 - Group 3api-376527663No ratings yet
- February Case StudyDocument6 pagesFebruary Case Studyapi-210258673No ratings yet
- UK - Radiotherapy For Operable Invasive Breast Cancer RT PRO 253 V3.0Document24 pagesUK - Radiotherapy For Operable Invasive Breast Cancer RT PRO 253 V3.0senthilonco_21753387No ratings yet
- London Cancer Head and Neck Radiotherapy Protocol March 2013Document10 pagesLondon Cancer Head and Neck Radiotherapy Protocol March 2013handrionoNo ratings yet
- Lung Carcinoma: Radiotherapy PlanningDocument9 pagesLung Carcinoma: Radiotherapy PlanningTowhidulIslamNo ratings yet
- Adaptive Radiotherapy (ART) For A Prostate CaseDocument18 pagesAdaptive Radiotherapy (ART) For A Prostate Caseapi-299189797No ratings yet
- Breast Unit SOP: Checklist While Giving ROIS AppointmentDocument7 pagesBreast Unit SOP: Checklist While Giving ROIS AppointmentAbhinav Ingle100% (1)
- Research Proposal New Group 5 Updated 4 23 24Document4 pagesResearch Proposal New Group 5 Updated 4 23 24api-692385376No ratings yet
- Clinical Oncology Assgn RT Mono BreastDocument9 pagesClinical Oncology Assgn RT Mono Breastapi-511386954No ratings yet
- Meddos Published ArticleDocument6 pagesMeddos Published Articleapi-350437453No ratings yet
- Courses in RadOnc-30Sept2020Document31 pagesCourses in RadOnc-30Sept2020ponderwoodNo ratings yet
- Breast Case StudyDocument15 pagesBreast Case Studyapi-318014709No ratings yet
- Breast Cancer Protocol (Version Date 10-JAN-2018)Document11 pagesBreast Cancer Protocol (Version Date 10-JAN-2018)Eugène NkusiNo ratings yet
- Clinical Oncology AssignmentDocument11 pagesClinical Oncology Assignmentapi-692385376No ratings yet
- Radiation Treatment For Breast CancerDocument13 pagesRadiation Treatment For Breast CancerZuriNo ratings yet
- APBI Journal Club PowerPointDocument20 pagesAPBI Journal Club PowerPointRegan Ward HimeNo ratings yet
- Long-Term Cosmesis Following A Novel Schedule ofDocument7 pagesLong-Term Cosmesis Following A Novel Schedule ofEmin PehlivanogluNo ratings yet
- Group 3 Draft 2Document11 pagesGroup 3 Draft 2api-376527663No ratings yet
- Clinical Oncology AssignmentDocument10 pagesClinical Oncology Assignmentapi-543045416No ratings yet
- Summary Standardised Reporting of Oncology CT Scans 2014Document15 pagesSummary Standardised Reporting of Oncology CT Scans 2014gigipedalaNo ratings yet
- Phase I Rod Group 6Document5 pagesPhase I Rod Group 6api-490791532No ratings yet
- Sethraheeljong Final PaperDocument13 pagesSethraheeljong Final Paperapi-268623363No ratings yet
- Bisa 1Document8 pagesBisa 1justforuroNo ratings yet
- NRG Protocol Radiation Therapy Template - GYN - Endometrial Cancer - FinalDocument12 pagesNRG Protocol Radiation Therapy Template - GYN - Endometrial Cancer - FinalarifpharmjuNo ratings yet
- Capstone Paper Section V 2Document7 pagesCapstone Paper Section V 2api-635186395No ratings yet
- Handbook Rhabdomyosarcoma Winter2018Document14 pagesHandbook Rhabdomyosarcoma Winter2018Rizky AmaliahNo ratings yet
- Icru 50 & Icru 62Document43 pagesIcru 50 & Icru 62Eduardo Torres ZambranoNo ratings yet
- Supafly PaperDocument4 pagesSupafly Paperapi-404851310No ratings yet
- IdentifyinggapsDocument6 pagesIdentifyinggapsapi-426094285No ratings yet
- RO-ILS Case StudyDocument4 pagesRO-ILS Case Studyapi-458422967No ratings yet
- Research Draft 3 FinalDocument14 pagesResearch Draft 3 Finalapi-299270003No ratings yet
- Csi PaperDocument9 pagesCsi Paperapi-602488644No ratings yet
- Clinical Oncology PaperDocument16 pagesClinical Oncology Paperapi-632529930No ratings yet
- Clinical Oncology AssignmentDocument8 pagesClinical Oncology Assignmentapi-598481829No ratings yet
- Protocol SummaryDocument4 pagesProtocol Summaryapi-635954562No ratings yet
- Hybrid Planning Case Study Final DraftDocument20 pagesHybrid Planning Case Study Final Draftapi-313040758No ratings yet
- Clinical Oncology AssignmentDocument6 pagesClinical Oncology Assignmentapi-280366843No ratings yet
- Capstone Paper Section Iii-2Document10 pagesCapstone Paper Section Iii-2api-632529930No ratings yet
- Research Project Second DraftDocument11 pagesResearch Project Second Draftapi-268707929No ratings yet
- Comparison Between Four Modalities of Radiotherapy of Prostate CancerDocument5 pagesComparison Between Four Modalities of Radiotherapy of Prostate CancerEdis ĐedovićNo ratings yet
- SBRT Limits JacmpDocument26 pagesSBRT Limits JacmpgriloucuraNo ratings yet
- 68Ga-DOTATATE PET-Based Radiation Contouring Creates More Precise Radiation Volumes For Patients With MeningiomaDocument7 pages68Ga-DOTATATE PET-Based Radiation Contouring Creates More Precise Radiation Volumes For Patients With MeningiomaandresNo ratings yet
- Response Evaluation Criteria in Solid TumorsDocument4 pagesResponse Evaluation Criteria in Solid TumorsmineresearchNo ratings yet
- Chiong - Clinical Pharmacy Breast CancerDocument8 pagesChiong - Clinical Pharmacy Breast CancerJohn Miguel ChiongNo ratings yet
- Capstone Paper IV Without Submission PacketDocument9 pagesCapstone Paper IV Without Submission Packetapi-484630324No ratings yet
- Nishele Lenards, PHD, CMD, RT (R) (T), FaamdDocument8 pagesNishele Lenards, PHD, CMD, RT (R) (T), Faamdapi-450246598No ratings yet
- Even/homogenous Dose Distribution Across PTV: WedgesDocument5 pagesEven/homogenous Dose Distribution Across PTV: WedgesrayNo ratings yet
- ProcedureDocument13 pagesProcedurerayNo ratings yet
- RT Triage SystemDocument4 pagesRT Triage SystemrayNo ratings yet
- EK Chemistry PDFDocument364 pagesEK Chemistry PDFray100% (8)
- 501 Critical Reading QuestionsDocument283 pages501 Critical Reading Questionsapi-3813392100% (9)
- Rebound Returns - Asos Private Bag 211022 Laurence Stevens Drive Auckland 2154 Freepost No 252061Document1 pageRebound Returns - Asos Private Bag 211022 Laurence Stevens Drive Auckland 2154 Freepost No 252061rayNo ratings yet
- Angry Strong Annoyance or HostilityDocument8 pagesAngry Strong Annoyance or HostilityrayNo ratings yet
- MU Calc AnswersDocument2 pagesMU Calc AnswersrayNo ratings yet
- 10cm 1 10cm 1 10cm 1: Decreased FF Increased MUDocument2 pages10cm 1 10cm 1 10cm 1: Decreased FF Increased MUrayNo ratings yet
- General VocabularyDocument9 pagesGeneral VocabularyrayNo ratings yet
- Rad 112 Cancer Cell BiologyDocument7 pagesRad 112 Cancer Cell BiologyrayNo ratings yet
- RADT115 2014 Test 2 Posted On Moodle On 9 May 16Document5 pagesRADT115 2014 Test 2 Posted On Moodle On 9 May 16rayNo ratings yet
- UMAT 2016 Short Test BookletDocument36 pagesUMAT 2016 Short Test BookletAnonymous rJmcI51No ratings yet
- Angry Strong Annoyance or HostilityDocument8 pagesAngry Strong Annoyance or HostilityrayNo ratings yet
- Radt 215Document5 pagesRadt 215rayNo ratings yet
- Cervix WorksheetDocument4 pagesCervix WorksheetrayNo ratings yet
- Case Study: Raymond HoveDocument20 pagesCase Study: Raymond HoverayNo ratings yet
- Cervix Formative AssesmentDocument4 pagesCervix Formative AssesmentrayNo ratings yet
- Case StudyDocument8 pagesCase StudyrayNo ratings yet
- Radiobio EQD2 QuestionsDocument2 pagesRadiobio EQD2 QuestionsrayNo ratings yet
- Literature Review Exclusion CriteriaDocument9 pagesLiterature Review Exclusion Criteriaea6mkqw2100% (1)
- Master - Birmingham Community Asset Directory - November2018Document26 pagesMaster - Birmingham Community Asset Directory - November2018anas kabarNo ratings yet
- The Development of Face Morphing Task To Assess Self Other DifferDocument122 pagesThe Development of Face Morphing Task To Assess Self Other DifferSHARIFA KHATUN ANANYANo ratings yet
- Bangalore DR ListDocument11 pagesBangalore DR Listkrisveli76% (42)
- 5 Gifts For An Abundant Life. Create A Consciousness of Wealth (PDFDrive)Document178 pages5 Gifts For An Abundant Life. Create A Consciousness of Wealth (PDFDrive)AGANAH EmmanuelNo ratings yet
- Hope2 G11 Q4 TQDocument6 pagesHope2 G11 Q4 TQnorietrose.cabante001No ratings yet
- A Quick Guide To Ventral Vagal AnchorsDocument2 pagesA Quick Guide To Ventral Vagal AnchorsAry ZuchettiNo ratings yet
- On Standing OrderDocument25 pagesOn Standing OrderPiyush Dutta100% (2)
- Josephson - Clinical Cardiac Electrophysiology Techniques AnDocument451 pagesJosephson - Clinical Cardiac Electrophysiology Techniques Anmobilica100% (5)
- Puti Mustika Swandyani, Agus Santoso, Yohanes KristiantoDocument11 pagesPuti Mustika Swandyani, Agus Santoso, Yohanes KristiantoAnonimNo ratings yet
- Donald Supers TheoryDocument20 pagesDonald Supers TheorytereNo ratings yet
- NCM 100 SKILLS Nursing Process HandoutsDocument10 pagesNCM 100 SKILLS Nursing Process HandoutsPearl IbisateNo ratings yet
- Prof - Ed Part 14 PDFDocument10 pagesProf - Ed Part 14 PDFpatrick mavNo ratings yet
- Usia Dan ParitasDocument16 pagesUsia Dan ParitasNurulismi SubbeNo ratings yet
- The Role of Women in Community Resilience To Climate - 2022 - Women S Studies IDocument13 pagesThe Role of Women in Community Resilience To Climate - 2022 - Women S Studies IHenry Andrew Barbosa SalamancaNo ratings yet
- CP - IndustrialDocument53 pagesCP - IndustrialIlham ArdiansyahNo ratings yet
- ColdDrinksandAssociatedHealthIssues PDFDocument3 pagesColdDrinksandAssociatedHealthIssues PDFKunal KumarNo ratings yet
- Food NutritionDocument2 pagesFood NutritionLuise MauieNo ratings yet
- The ADHD Diagnosis GuideDocument13 pagesThe ADHD Diagnosis GuideArunima KapoorNo ratings yet
- Krister Ann Jimenez ACTIVITY 14 ParagraphDocument17 pagesKrister Ann Jimenez ACTIVITY 14 ParagraphJamie JimenezNo ratings yet
- Running Head: Sexual Assault On Black Women 1Document4 pagesRunning Head: Sexual Assault On Black Women 1Preet ChahalNo ratings yet
- Term Exam Answer Sheet EnglishDocument11 pagesTerm Exam Answer Sheet Englishsameera gupteNo ratings yet
- A Study On Employee Morale With Special Reference To Butterfly Gandhimathi Appliance PVT LTDDocument18 pagesA Study On Employee Morale With Special Reference To Butterfly Gandhimathi Appliance PVT LTDAnandNo ratings yet
- Literature Review 2Document8 pagesLiterature Review 2api-511258439No ratings yet
- SodaPDF Converted KERTAS TRIAL ENGLISH PERLIS K1 SET B 2021Document14 pagesSodaPDF Converted KERTAS TRIAL ENGLISH PERLIS K1 SET B 2021Nur HafezaNo ratings yet
- Pas Big Ganjil 2022 Kls 9 Edit BIMA 40 Nomer + 5 ESSAYDocument7 pagesPas Big Ganjil 2022 Kls 9 Edit BIMA 40 Nomer + 5 ESSAYSyamsul ArifinNo ratings yet
- Chap. 1. New Waves in Social Psychology. SpringerDocument24 pagesChap. 1. New Waves in Social Psychology. SpringerRaudelioMachinNo ratings yet
- Pros and Cons of Research in E.H.Document3 pagesPros and Cons of Research in E.H.goldMINDNo ratings yet
- Nuclear Lab 2 GeneratorDocument12 pagesNuclear Lab 2 GeneratorSatish PaswanNo ratings yet
- After The Rain Alexandra ElleDocument3 pagesAfter The Rain Alexandra ElleCocobutter VivNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (4)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)