Professional Documents
Culture Documents
Prognosis For Patients With Amyotrophic Lateral Sclerosis: Development and Validation of A Personalised Prediction Model
Uploaded by
Lachimolala ShopOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prognosis For Patients With Amyotrophic Lateral Sclerosis: Development and Validation of A Personalised Prediction Model
Uploaded by
Lachimolala ShopCopyright:
Available Formats
Articles
Prognosis for patients with amyotrophic lateral sclerosis:
development and validation of a personalised prediction model
Henk-Jan Westeneng, Thomas P A Debray, Anne E Visser, Ruben P A van Eijk, James P K Rooney, Andrea Calvo, Sarah Martin,
Christopher J McDermott, Alexander G Thompson, Susana Pinto, Xenia Kobeleva, Angela Rosenbohm, Beatrice Stubendorff, Helma Sommer,
Bas M Middelkoop, Annelot M Dekker, Joke J F A van Vugt, Wouter van Rheenen, Alice Vajda, Mark Heverin, Mbombe Kazoka, Hannah Hollinger,
Marta Gromicho, Sonja Körner, Thomas M Ringer, Annekathrin Rödiger, Anne Gunkel, Christopher E Shaw, Annelien L Bredenoord,
Michael A van Es, Philippe Corcia, Philippe Couratier, Markus Weber, Julian Grosskreutz, Albert C Ludolph, Susanne Petri, Mamede de Carvalho,
Philip Van Damme, Kevin Talbot, Martin R Turner, Pamela J Shaw, Ammar Al-Chalabi, Adriano Chiò, Orla Hardiman, Karel G M Moons,
Jan H Veldink, Leonard H van den Berg
Summary
Background Amyotrophic lateral sclerosis (ALS) is a relentlessly progressive, fatal motor neuron disease with a Lancet Neurol 2018; 17: 423–33
variable natural history. There are no accurate models that predict the disease course and outcomes, which complicates Published Online
risk assessment and counselling for individual patients, stratification of patients for trials, and timing of interventions. March 26, 2017
http://dx.doi.org/10.1016/
We therefore aimed to develop and validate a model for predicting a composite survival endpoint for individual
S1474-4422(18)30089-9
patients with ALS.
See Comment page 386
Department of Neurology,
Methods We obtained data for patients from 14 specialised ALS centres (each one designated as a cohort) in Belgium, Brain Centre Rudolf Magnus,
France, the Netherlands, Germany, Ireland, Italy, Portugal, Switzerland, and the UK. All patients were diagnosed in the University Medical Centre
centres after excluding other diagnoses and classified according to revised El Escorial criteria. We assessed 16 patient Utrecht, Utrecht, Netherlands
characteristics as potential predictors of a composite survival outcome (time between onset of symptoms and non- (H-J Westeneng MD,
A E Visser MD, R P A van Eijk MD,
invasive ventilation for more than 23 h per day, tracheostomy, or death) and applied backward elimination with B M Middelkoop,
bootstrapping in the largest population-based dataset for predictor selection. Data were gathered on the day of diagnosis A M Dekker MD,
or as soon as possible thereafter. Predictors that were selected in more than 70% of the bootstrap resamples were used J J F A van Vugt PhD,
to develop a multivariable Royston-Parmar model for predicting the composite survival outcome in individual patients. W van Rheenen MD,
M A van Es MD,
We assessed the generalisability of the model by estimating heterogeneity of predictive accuracy across external Prof J H Veldink MD,
populations (ie, populations not used to develop the model) using internal–external cross-validation, and quantified Prof L H van den Berg MD);
the discrimination using the concordance (c) statistic (area under the receiver operator characteristic curve) and Department of Epidemiology,
Julius Centre for Health
calibration using a calibration slope.
Sciences and Primary Care,
University Medical Centre
Findings Data were collected between Jan 1, 1992, and Sept 22, 2016 (the largest data-set included data from Utrecht, Utrecht, Netherlands
1936 patients). The median follow-up time was 97·5 months (IQR 52·9–168·5). Eight candidate predictors entered (T P A Debray PhD,
A L Bredenoord PhD,
the prediction model: bulbar versus non-bulbar onset (univariable hazard ratio [HR] 1·71, 95% CI 1·63–1·79), age at
Prof K G M Moons PhD);
onset (1·03, 1·03–1·03), definite versus probable or possible ALS (1·47, 1·39–1·55), diagnostic delay (0·52, Cochrane Netherlands,
0·51–0·53), forced vital capacity (HR 0·99, 0·99–0·99), progression rate (6·33, 5·92–6·76), frontotemporal dementia University Medical Centre
(1·34, 1·20–1·50), and presence of a C9orf72 repeat expansion (1·45, 1·31–1·61), all p<0·0001. The c statistic for Utrecht, Utrecht, Netherlands
(T P A Debray,
external predictive accuracy of the model was 0·78 (95% CI 0·77–0·80; 95% prediction interval [PI] 0·74–0·82) and
Prof K G M Moons); Academic
the calibration slope was 1·01 (95% CI 0·95–1·07; 95% PI 0·83–1·18). The model was used to define five groups with Unit of Neurology, Trinity
distinct median predicted (SE) and observed (SE) times in months from symptom onset to the composite survival Biomedical Sciences Institute,
outcome: very short 17·7 (0·20), 16·5 (0·23); short 25·3 (0·06), 25·2 (0·35); intermediate 32·2 (0·09), 32·8 (0·46); Trinity College, Dublin, Ireland
(J P K Rooney MSc, A Vajda PhD,
long 43·7 (0·21), 44·6 (0·74); and very long 91·0 (1·84), 85·6 (1·96).
M Heverin MSc,
Prof O Hardiman MD); ‘Rita Levi
Interpretation We have developed an externally validated model to predict survival without tracheostomy and Montalcini’ Department of
non-invasive ventilation for more than 23 h per day in European patients with ALS. This model could be applied to Neuroscience, ALS Centre,
University of Torino, Torino,
individualised patient management, counselling, and future trial design, but to maximise the benefit and prevent Italy (A Calvo MD,
harm it is intended to be used by medical doctors only. Prof A Chiò MD); Maurice Wohl
Clinical Neuroscience Institute,
Funding Netherlands ALS Foundation. and United Kingdom Dementia
Research Institute at the
Institute of Psychiatry,
Copyright © 2018 Elsevier Ltd. All rights reserved. Psychology and Neuroscience,
King’s College London, London,
Introduction and strategies for effective palliative care have been UK (S Martin BSc,
Prof C E Shaw MD,
Neurodegenerative diseases impose an enormous limited by disease heterogeneity and the presence of Prof A Al-Chalabi PhD); Sheffield
clinical and economic burden on patients and health overlapping phenotypes.2 Therefore, models that can Institute for Translational
systems.1 Development of disease-modifying therapies reliably predict outcomes at an individual patient level Neuroscience, University of
www.thelancet.com/neurology Vol 17 May 2018 423
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
Sheffield, Sheffield, UK
(Prof C J McDermott PhD, Research in context
M Kazoka, H Hollinger MA,
Prof P J Shaw MD); Nuffield Evidence before this study without tracheostomy or non-invasive ventilation for more
Department of Clinical Prediction of survival in individual patients with amyotrophic than 23 h per day, for individual patients, based on clinical,
Neurosciences, University of lateral sclerosis (ALS) is important but remains elusive. cognitive, and genetic predictors that were defined at
Oxford, Oxford, UK
We searched PubMed without language restrictions using the diagnosis. Most of these predictors can be collected cheaply,
(A G Thompson BMBCh,
Prof K Talbot DPhil, terms “([amyotrophic lateral sclerosis] OR [motor neuron simply, and non-invasively, rendering them useful for the
Prof M R Turner MD); Institute of disease]) AND [survival] OR [mortality] OR [prognosis] OR assessment of individual prognosis in an outpatient clinic
Physiology-Instituto de [prognostic factor] OR [prediction model])” for articles on setting. We assessed the external validity of our model across
Medicina Molecular, Faculty of
Medicine, University of Lisbon,
validated models that predict survival at an individual level and several populations, and showed that it had a probability of
Lisbon, Portugal (S Pinto PhD, articles on clinical, cognitive, and genetic predictors of survival more than 95% for good performance. We defined
M Gromicho PhD, in ALS, published between Jan 1, 1960, and Dec 31, 2017. We five subgroups of patients with distinctive survival times
Prof M de Carvalho MD); searched for well studied predictors of survival that can be (very short, short, intermediate, long, and very long), and
Department of Neurology,
Hannover Medical School,
collected during diagnostic work-up and excluded factors that illustrated the clinical applicability of our model to individual
Hannover, Germany require longitudinal assessments (eg, slope of forced vital patients. All parameters and equations of our model are
(X Kobeleva MD, S Körner MD, capacity) or that are rare (eg, SOD A4V mutations). We identified provided in our appendix to allow improvement of predictions
Prof S Petri MD); Department of 16 variables as predictors of survival in ALS in at least one through continuing research on other prognostic factors or
Neurology, University of Ulm,
Ulm, Germany
peer-reviewed article, but replication was frequently absent, outcome measures.
(A Rosenbohm MD, outcomes of studies were contradictory, and studies used
Implications of all the available evidence
Prof A C Ludolph MD); different sets of covariates in multivariable analyses or adopted
Hans-Berger Department of Our study proposes a set of independent predictors of survival
different variable definitions, which complicated a formal
Neurology, Jena University without tracheostomy or non-invasive ventilation for more
Hospital, Jena, Germany
synthesis of previous findings. Two studies about prediction of
than 23 h per day in patients with ALS and provides a validated
(B Stubendorff PhD, disease progression in ALS (but not survival) were identified.
prediction model. To minimise the risk of potential harm to
T M Ringer MD, A Rödiger MD, These studies used data from 1822 and 3742 patients from the
A Gunkel MD, J Grosskreutz MD); patients if the prediction they receive is shorter than expected,
Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT)
Neuromuscular Diseases Centre/ the online model will be accessible only to medical doctors, who
ALS Clinic, Kantonsspital database. This database includes patients from 23 clinical trials,
have to register and sign in before access is provided. We
St Gallen, St Gallen, Switzerland but not from population-based studies or patient registries. We
encourage implementation of the model in evidence-based,
(H Sommer, Prof M Weber MD); identified no sufficiently powered, externally validated,
Centre de compétence tailored counselling of individual patients and their caregivers,
prediction models of survival in individual patients with ALS.
SLA-fédération Tours-Limoges, and in multidisciplinary care practices, by facilitating the
CHU de Tours, Tours, France Added value of this study selection of appropriate care pathways (eg, frequency of
(Prof P Corcia MD); Centre de
compétence SLA-fédération
In our study of 11 475 patients with ALS from 14 European ALS consultations involving specific disciplines), and in innovative
Tours-Limoges, CHU de centres, we derived and validated, according to the TRIPOD trial design, by refining inclusion and exclusion criteria,
Limoges, Limoges, France guidelines, a multivariable model for the prediction of survival stratification, and subgroup analyses.
(Prof P Couratier MD);
Department of Neurology,
University Hospital Leuven, could become important factors in a precision-medicine documented natural history of ALS,3,6 prediction of
Leuven, Belgium, and approach by improving the potential for prognostic survival in individual patients remains elusive. It is
Department of Neurosciences,
counselling, stratification of patients for trials, and important that such risk predictions are sufficiently
Katholieke Universiteit, Leuven
(University of Leuven) and timing of interventions.2 accurate across different settings and populations. The
Centre for Brain and Disease Amyotrophic lateral sclerosis (ALS) is one of the most development and validation of such models is, however,
Research, VIB, Leuven, Belgium devastating neurodegenerative diseases. It predominantly challenging because few large datasets with individual
(Prof P Van Damme MD); and
Department of Neurology,
affects motor neurons in the brain and spinal cord, participant data and adequate follow-up times are
Beaumont Hospital, Beaumont, leading to weakness of voluntary muscles.3,4 Muscle available.8–10
Ireland (Prof O Hardiman) weakness progresses gradually, spreading from a site of We therefore analysed clinical, cognitive, and genetic
Correspondence to: clinical onset; patients eventually become paralysed and data of patients with ALS from ALS centres in Europe
Prof Leonard H van den Berg, die, usually as the result of respiratory failure.3,4 The with a view to predicting a composite survival outcome—
Department of Neurology,
clinical features of ALS are heterogeneous: the disease time between onset of symptoms and non-invasive
University Medical Centre Utrecht,
Utrecht, 3508 GA, Netherlands. can occur at any adult age, up to 15% of patients develop ventilation for more than 23 h per day, tracheostomy, or
l.h.vandenberg@umcutrecht.nl frontotemporal dementia,5 and 10–15% of patients have a death—for individual patients on the day of diagnosis.
family history of ALS or frontotemporal dementia.4 We aimed to develop and externally validate a prediction
Survival for patients with ALS varies greatly, ranging model in multiple cohorts.
from several months to more than 10 years. Determinants
of survival at group level have been studied extensively:6 Methods
patient characteristics such as older age at onset of Study design and participants
symptoms, the presence of frontotemporal dementia, or We did a two-stage study using clinical, cognitive, and
a repeat expansion in C9orf72 have been associated with genetic data for patients with ALS from 14 specialised
shorter survival.6,7 Unfortunately, despite the well ALS centres (each one designated as a cohort) in Belgium,
424 www.thelancet.com/neurology Vol 17 May 2018
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
France, the Netherlands, Germany, Ireland, Italy, behaviour) that is developed to screen for behavioural
Portugal, Switzerland, and the UK. In the first stage, disturbances in the patient with ALS.
predictor selection was done in the largest cohort, with Genetic predictors were presence of a C9orf72 mutation,
data from consecutive incident patients, diagnosed with and presence of the minor allele homozygous genotype
ALS according to the revised El Escorial criteria, who (C/C) of the UNC13A single nucleotide polymorphism,
participated in an ongoing prospective, population-based which were determined as previously described.7,22–24
study in the Netherlands between Jan 1, 2006, and These two genetic predictors are the most frequent
March 31, 2015.11 In the second stage, data for identified mutations in patients with ALS and were previously
predictors and survival outcomes were requested from shown to be associated with survival outcomes.7,22
13 other centres to develop and externally validate the Data were gathered on the day of diagnosis or as soon
model. All patients were diagnosed in the centres after as possible thereafter. The ALSFRS-R slope was
excluding other diagnoses, and classified according to the determined as follows: (48 minus ALSFRS-R score)/(date
revised El Escorial criteria.12 Written informed consent of the ALSFRS-R score minus date of onset).15 ALSFTD-Q
was obtained from all participants and institutional scores were trichotomised into no, mild, and severe
review boards approved this study (appendix). The study behavioural impairment.21 A detailed overview of See Online for appendix
is reported in accordance with the TRIPOD guidance for predictors is reported in the appendix.
transparent reporting of prediction models.10 All cohorts used the ALSFRS-R score, except the cohort
in Oxford (UK), which used the unrevised version of the
Procedures ALSFRS. The ten questions of the unrevised version are
Survival analyses in ALS research generally use identical to the first ten questions of the ALSFRS-R, but
composite endpoints (ie, events) comprising both death the ALSFRS-R has two additional questions about
and respiratory events.13,14 In our study, survival was respiration. The maximum score per question is 4,
defined as time between onset of symptoms and our resulting in a maximum score of 48 for the ALSFRS-R
composite endpoint of non-invasive ventilation for more and 40 for the ALSFRS. To be able to compare scores, we
than 23 h per day, or tracheostomy, or death. We assessed transformed the ALSFRS score to the ALSFRS-R score by
ten clinical, four cognitive, and two genetic characteristics. multiplying by 1·2. Furthermore, all cohorts used FVC to
All predictors were selected on the basis of a PubMed measure respiratory function, except the cohort in
search. Dublin (Ireland), which used sniff nasal inspiratory
Clinical predictors were sex, site of onset (spinal vs bulbar), pressure (SNIP), which is known to be correlated with
age at onset of weakness or bulbar symptoms, revised El FVC.25 Based on patients in the Dublin cohort for whom
Escorial criteria (definite vs probable or possible ALS),12 we had information about both FVC and SNIP, we
diagnostic delay (time from onset of weakness or bulbar transformed SNIP data of all patients to FVC to allow
symptoms to diagnosis), forced vital capacity (FVC; comparability between cohorts.
percentage of predicted based on normative values for age, We explored patient preferences with regard to
sex, and body height), progression rate defined by the knowing their personalised prognosis by doing an online
slope on the revised ALS Functional Rating Scale survey in 242 Dutch patients with ALS (appendix).
(ALSFRS-R),15 premorbid body-mass index (BMI),16 current
smoking,17 and cigarette pack-years.6 Statistical analysis
Cognitive predictors were the presence of We used a backward elimination procedure with
frontotemporal dementia according to the Neary or bootstrapping to select predictors of the composite
Rascovsky criteria,18 and scores on the verbal fluency survival outcome (appendix).26 Predictors that were
index,19 the Frontal Assessment Battery,20 and the ALS selected in more than 70% of the bootstrap resamples
Frontotemporal Dementia Questionnaire (ALSFTD-Q).21 entered a multivariable prediction model.26 Data from the
For the verbal fluency index participants were asked to 14 cohorts were combined using the internal–external
name as many words as possible beginning with the cross-validation framework.27,28 This developed a model
letter D in 3 min, following which the participants were for predicting our composite survival endpoint in all but
instructed to read aloud the generated words. The index one cohort, after which its external validity was evaluated
was calculated as the number of words generated divided in the omitted cohort. The process was repeated for all
by the time needed to read them aloud. The frontal 14 cohorts (every cohort being omitted once), yielding
assessment battery is a bedside test comprising six tasks multiple estimates of external validity for a given
(maximum of 3 points per task) measuring modelling strategy. A meta-analysis was done to assess
conceptualisation, mental flexibility, motor programming, the overall performance of the model and to identify
sensitivity to interference, inhibition control, and sources of between-study heterogeneity,29 such as
environmental autonomy; this test is sensitive to frontal differences in survival time or differences in
lobe dysfunction. The ALSFRS-Q is a 25-item the definition of predictors between different cohorts,
questionnaire (maximum of 4 points per item) applied to which might affect the generalisability of a model. The
a proxy (ie, a caregiver who is able to assess the patient’s internal–external cross-validation framework thus
www.thelancet.com/neurology Vol 17 May 2018 425
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
426
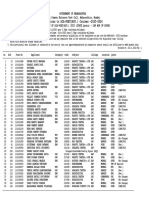
Utrecht, Dublin, Torino, Sheffield, London, Oxford, Leuven, Lisbon, Hannover, Ulm, Jena, St Gallen, Tours, Limoges, Total Hazard ratio
Netherlands Ireland Italy UK UK UK Belgium Portugal Germany Germany Germany Switzerland France France (95% CI)*
Articles
Data source Population- Population- Population- Referral- Referral- Referral- Referral- Referral- Referral- Referral- Referral- Referral- Referral- Referral- ·· ··
based based based based based based based based based based based based based based
N 1936 1818 1022 1187 1266 849 833 594 506 443 343 286 190 202 11 475 ··
(100·0)
Duration of 9·2 20·5 9·2 15·7 23·1 15·2 23·8 17·4 12·9 6·8 8·0 13·0 5·2 5·2 12·9 ··
data (8·3–17·0)
acquisition
(years)
Age at onset 62·7 65·3 68·0 62·3 63·1 63·4 61·2 62·9 60·2 61·1 61·7 60·9 65·5 64·0 63·3 1·03
(years) (55·4–69·8) (56·9–72·4) (60·2–74·3) (52·6– (54·1–70·7) (53·8– (51·4– (54·9– (51·9– (52·0– (52·5– (52·0–69·3) (59·9– (56·9– (54·8–70·7) (1·03–1·03)
69·9) 71·1) 67·8) 70·8) 67·0) 69·3) 68·8) 73·6) 73·6)
Diagnostic 10·1 10·3 9·0 12·1 12·3 12·6 8·9 12·0 8·0 10·4 9·0 11·0 9·0 8·0 10·5 0·52
delay (6·6–16·3) (6·0–16·9) (5·0–13·9) (7·8–21·3) (8·0–21·0) (8·4–20·9) (5·3–13·0) (7·5–17·7) (5·0–14·9) (6·3–17·1) (5·0–17·0) (6·1–21·9) (6·0–14·6) (5·0–14·0) (6·3–17·6) (0·51–0·53)†
(months)
Progression 0·6 0·6 0·7 0·6 0·6 0·5 0·6 0·6 0·6 0·5 0·6 0·4 0·9 0·9 0·6 6·33
rate (ALSFRS (0·3–1·0) (0·3–1·0) (0·3–1·3) (0·3–1·2) (0·3–1·0) (0·2–0·9) (0·3–1·1) (0·4–1·1) (0·3–1·0) (0·3–1·1) (0·4–1·0) (0·2–0·8) (0·4–1·5) (0·5–1·6) (0·3–1·1) (5·92–6·76)‡
points per
month)
Forced vital 91·0 75·5 87·0 83·5 71·0 86·0 94·0 88·0 81·0 74·0 ·· 86·0 89·3 92·0 88·0 0·99
capacity (%) (77·0– (45·7– (66·8– (68·0– (57·0– (68·0– (77·0– (74·0– (67·0– (55·0– (66·0– (70·0– (67·0– (69·0– (0·99–0·99)
105·0) 109·8) 102·0) 102·2) 90·0) 100·0) 110·0) 102·0) 95·0) 92·0) 101·0) 104·2) 107·0) 103·0)
Bulbar onset 610/1855 690/1744 347 (34%) 329 411/1244 200/788 224/831 196/592 121/437 130 (29%) 90/307 82/278 64/178 59 (29%) 3553/ 1·71
(33%) (39%) (28%) (33%) (25%) (27%) (33%) (28%) (29%) (29%) (36%) 11138 (1·63–1·79)
(32%)
Definite 354/1844 942/1642 342/1019 298/1099 329/116 ·· 64/313 146 49 (10%) 227 (51%) 40/239 61/195 68/175 33/188 2953/ 1·47
ALS§ (19%) (57%) (34%) (27%) (28%) (20%) (25%) (17%) (31%) (39%) (18%) 9424 (1·39–1·55)
(31%)
Fronto 60/1576 86/366 127 (12%) 18 (2%) 12 (<1%) 25/813 40 (5%) 31 (5%) 4 (<1%) 21 (5%) ·· 2 (<1%) 17 (9%) 13 (6%) 456/ 1·34
temporal (4%) (23%) (3%) 9284 (5%) (1·20–1·50)
dementia
C9orf72 155/1690 71/698 50/794 51/401 5/59 ·· 99/604 17/121 ·· ·· 4/106 13/274 27 (14%) 15/25 507/ 1·45
repeat (9%) (10%) (6%) (13%) (8%) (16%) (14%) (4%) (5%) (60%) 4962 (1·31–1·61)
expansion (10%)
Time to our 35·8 28·6 30·2 37·0 32·5 35·3 35·0 39·2 36·0 46·2 45·7 55·5 32·9 29·0 34·7 ··
composite (34·8–37·6) (27·3–29·8) (28·3–31·4) (35·4–39·5) (31·3–34·5) (33·5– (32·7– (36·2– (33·6– (40·9– (42·0– (46·3–64·0) (26·9– (26·5– (34·2–
endpoint 38·3) 38·2) 42·0) 39·0) 51·7) 52·9) 40·5) 32·6) 35·3)||
(95% CI)
since onset
(months)¶**
Achieved 1460 1586 834 850 1131 699 645 374 443 191 189 139 114 164 8819 ··
one of the (75%) (87%) (82%) (72%) (89%) (82%) (77%) (63%) (88%) (43%) (55%) (49%) (60%) (81%) (77%)
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
composite
survival
endpoints**
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Data are median (IQR) or number (%) (except where denoted otherwise) for 14 cohorts, one at each ALS centre. ··=unavailable data. ALS=amyotrophic lateral sclerosis. *Hazard ratios were calculated with a univariable random-effects Cox model with the
14 ALS research centres as a grouping factor for the random effects. †Because of non-normally distributed data, a natural logarithm transformation was applied. ‡Because of non-normally distributed data, a square-root transformation was applied.
§Definite ALS according to the revised El Escorial criteria. ¶Time between onset and our composite survival endpoint. ||Calculated with a random-effects Cox model with the 14 ALS research centres as a grouping factor for the random effects.
**Composite endpoint of survival defined as the presence of non-invasive ventilation >23 h per day, or tracheostomy, or death. Different cohorts might have used different definitions (appendix).
Table 1: Patient characteristics
www.thelancet.com/neurology Vol 17 May 2018
Articles
provided a means to learn about the generalisability of the across different populations, which helped to assess the
model across different settings and populations. potential generalisability of the model.29
For model development, we used multivariable Prognostic models for predicting survival and related
Royston-Parmar survival models30 rather than Cox outcomes require adequate discrimination and calibration
survival models, to facilitate the calculation of absolute performance to be clinically useful. We therefore
risks in individual patients when implementing the calculated the joint 95% PI and estimated the probability
model in clinical practice (appendix). We assumed a that the model would achieve a certain predefined c
common baseline hazard for all cohorts, but also reported statistic and calibration slope in future patients (appendix).
values of cohort-specific baseline hazard functions,
which might help to tailor predictions to different Data sharing
populations. We used fractional polynomials to identify For medical doctors, we are making our model freely
non-linear relationships with our composite survival available online. We report all parameters of the model in For the model see http://www.
encalssurvivalmodel.org
endpoint.31 Missing values were multiply imputed using the appendix and further supporting information can be
multilevel joint modelling techniques in accordance with requested online or from the corresponding author.
previous publications (appendix).32,33
For model validation, we assessed discrimination (ie, the Role of the funding source
ability to differentiate between patients who reached our The funders of the study had no role in study design,
composite endpoint and those who did not) and calibration data collection, data analysis, data interpretation, or
(ie, the agreement between observed and predicted times writing of the report. The corresponding author had full
to our composite endpoint). Discrimination was quantified access to all the data in the study and had final
using the concordance (c) statistic, which is the area under responsibility for the decision to submit for publication.
the receiver operator characteristic (ROC) curve generalised
to all possible survival timepoints as defined by the Results
composite endpoint. The c statistic measured the ability of Data were collected between Jan 1, 1992, and Sept 22, 2016,
the model to differentiate between patients who reached for 11 475 patients. The different cohorts had different
our composite endpoint and those who did not: values start and end dates within this period (appendix). Total
close to 1 indicated very good discriminative ability, while follow-up was 40 016 years and median follow-up time
values close to 0·5 indicated poor discriminative ability. was 97·5 months (IQR 52·9–168·5). Patient chara
We also measured time-dependent ROC curves 3 years cteristics are shown in table 1 and the appendix.
after onset, because this is the period reported as median Based on backward elimination in the largest dataset
survival.3 Calibration was assessed by calibration plots and (1936 patients), eight of the 16 candidate predictors were
quantified by the calibration-in-the-large and calibration selected for the multivariable prediction model: age at
slope statistic.28,29,34 A calibration slope of 1 in combination onset (n=10000, 100% of bootstraps), FVC (7598, 76%),
with a calibration-in-the-large of 0 indicated good overall diagnostic delay (10000, 100%), ALSFRS-R slope
calibration (appendix). (10000, 100%), bulbar onset (8094, 81%), definite
We did a complete case analysis and sensitivity analyses
omitting frontotemporal dementia from the model, Univariable HR* Multivariable HR†
omitting the C9orf72 repeat expansion from the model,
Age at onset (years) 1·28 (1·25–1·31) 1·02 (1·02–1·03)
and using time of diagnosis as starting point for
Diagnostic delay (months) 0·48 (0·46–0·49) 0·63 (0·59–0·68)‡
prediction. We compared predicted and observed curves
Progression rate (points per month) 3·05 (2·84–3·27) 3·19 (2·71–3·75)§
for times to reach our composite endpoint for combined
Forced vital capacity (%) 0·76 (0·72–0·80) 0·99 (0·99–0·99)
and individual cohorts as well as the effect of recalibration
of the intercept on predictive performance in different Bulbar onset ·· 1·25 (1·17–1·33)
cohorts.34 Five equal-sized prognostic groups were Definite ALS¶ ·· 1·25 (1·16–1·34)
created based on the linear predictor of the model Frontotemporal dementia ·· 1·18 (1·01–1·37)
(20% of data per group): very short, short, intermediate, C9orf72 repeat expansion ·· 1·37 (1·19–1·57)
long, and very long times to our composite survival Data are hazard ratio (HR; 95% CI). All HRs were estimated using random-effects Cox models with the 14 ALS research
endpoint. A computer algorithm was applied to the full centres as grouping factor for the random effects. This table is intended to provide an indication of the relative effects of
dataset to randomly select five patients from the the transformed predictors, and the random-effects Cox model differs from the Royston-Parmar proportional odds model
that was used to generate the predictions. ALS=amyotrophic lateral sclerosis. ··=not transformed. *Using the different
five prognostic groups (in total 25 patients), illustrating transformed continuous predictors, we made a comparison between the first and third quartile and report the univariable
application of the model to individual patients. HRs (see appendix for applied transformations). This illustrates the relative effects of the continuous predictors after
Because the internal–external cross-validation approach transformation. Because the last four variables were dichotomous, it was not possible to make a comparison between the
first and third quartiles. †This column shows the HRs when all eight predictors were combined (more details in appendix).
allows evaluation of external performance across multiple
The HRs resulted from coefficients and thus did not rely on the quartiles that were used in the univariate HR column.
studies, we meta-analysed estimates of model ‡Because of non-normally distributed data, a natural logarithm transformation was applied. §Because of non-normally
performance and calculated 95% CI, using random- distributed data, a square-root transformation was applied. ¶According to revised El Escorial criteria.
effects meta-analyses.29 We also calculated 95% prediction
Table 2: Relative effects of transformed predictors
intervals (PI) to quantify the range of model performance
www.thelancet.com/neurology Vol 17 May 2018 427
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
ALS (7120, 71%), presence of frontotemporal dementia predictors after transformation are presented in table 2.
(7416, 74%), and the C9orf72 repeat expansion (8679, 87%). Using all imputed datasets, we showed that a proportional
Results for variables that were not included in the model odds Royston-Parmar model with two internal knots,
are reported in the appendix. Age at onset, ALSFRS-R without time-dependent covariates, was most appropriate
slope, diagnostic delay, and FVC were transformed according to the Akaike information criterion and that a
because of non-linear relationships with our composite proportional odds model consistently outperformed a
survival endpoint (appendix); the relative effects of the proportional hazard model (appendix).
A B
Validation cohort c statistic (95% CI) Validation cohort Calibration slope
(95% CI)
Utrecht, Netherlands 0·79 (0·77 to 0·81) Utrecht, Netherlands 1·12 (1·05 to 1·19)
Dublin, Ireland 0·78 (0·76 to 0·80) Dublin, Ireland 0·96 (0·87 to 1·04)
Torino, Italy 0·77 (0·75 to 0·79) Torino, Italy 0·96 (0·87 to 1·04)
Sheffield, UK 0·78 (0·76 to 0·80) Sheffield, UK 0·99 (0·90 to 1·08)
London, UK 0·82 (0·79 to 0·84) London, UK 1·09 (0·96 to 1·21)
Oxford, UK 0·78 (0·75 to 0·81) Oxford, UK 0·99 (0·85 to 1·12)
Leuven, Belgium 0·77 (0·75 to 0·80) Leuven, Belgium 0·96 (0·84 to 1·08)
Lisbon, Portugal 0·77 (0·74 to 0·80) Lisbon, Portugal 0·95 (0·82 to 1·08)
Hannover, Germany 0·74 (0·71 to 0·77) Hannover, Germany 0·83 (0·70 to 0·96)
Ulm, Germany 0·83 (0·78 to 0·88) Ulm, Germany 1·17 (0·95 to 1·39)
Jena, Germany 0·80 (0·75 to 0·85) Jena, Germany 1·12 (0·90 to 1·34)
St Gallen, Switzerland 0·80 (0·74 to 0·86) St Gallen, Switzerland 1·01 (0·80 to 1·22)
Tours, France 0·76 (0·71 to 0·81) Tours, France 1·09 (0·88 to 1·31)
Limoges, France 0·80 (0·73 to 0·86) Limoges, France 1·07 (0·82 to 1·32)
Meta-analysis 0·78 (0·77 to 0·80) Meta-analysis 1·01 (0·95 to 1·07)
95% PI 0·74 to 0·82 95% PI 0·83 to 1·18
0·70 0·75 0·80 0·85 0·90 0·60 0·80 1·00 1·20 1·40
c statistic Miscalibration Miscalibration
C D
Validation cohort Calibration-in-the-large Survival without tracheostomy
(95% CI) or non-invasive ventilation
100 >23 h per day
Utrecht, Netherlands −0·14 (−0·22 to −0·05) Predicted very long
Predicted long
Dublin, Ireland 0·27 ( 0·14 to 0·40)
Predicted intermediate
Torino, Italy 0·09 (−0·03 to 0·20) Predicted short
80
Sheffield, UK 0·34 ( 0·16 to 0·52) Predicted very short
Observed
London, UK 0·05 (−0·07 to 0·16)
Survival probability (%)
Oxford, UK 0·23 ( 0·10 to 0·36)
60
Leuven, Belgium −0·13 (−0·31 to 0·04)
Lisbon, Portugal −0·11 (−0·27 to 0·05)
Hannover, Germany −0·07 (−0·24 to 0·10)
40
Ulm, Germany −0·71 (−0·92 to −0·50)
Jena, Germany −0·78 (−1·14 to −0·42)
St Gallen, Switzerland −0·59 (−0·85 to −0·32)
Tours, France −0·15 (−0·40 to 0·09) 20
Limoges, France −0·16 (−0·44 to 0·13)
Meta-analysis −0·12 (−0·33 to 0·08)
95% PI –0·88 to 0·63 0
–0·50 –1·00 –0·50 0 0·50 1·00 0 12 24 36 48 60 72 84 96 108 120
Time since onset (months)
Underestimation Overestimation
Figure 1: Univariate meta-analysis of predictive performance
Panel A shows the random-effects meta-analysis of discrimination as measured with the c statistic (time-dependent receiver operator characteristic [ROC] curves in the
appendix). Panels B and C show the random-effects meta-analysis of calibration as measured with calibration slope (B) and calibration-in-the-large (C). A calibration
slope of 1 in combination with a calibration-in-the-large of 0 indicated good overall calibration (calibration slope <1: predictions are too extreme; calibration slope >1:
predictions are too similar; further details in the appendix). The black diamonds indicate the mean (95% CI) of the predictive accuracy. 95% prediction intervals (PI),
which indicate predicted accuracy of the model in a single new dataset or patient, are presented as a numeric range (below the 95% CI). Panel D is the visual translation of
A–C in prognostic curves showing the agreement between predicted and observed probability of reaching the composite endpoint as well as indicating good
discriminative power of the model. The curves also illustrate the possibility to stratify patients in different groups based on their predicted prognosis on the day of
diagnosis. Five equal-sized groups were created based on predicted time to our composite endpoint. Omitted cohort label indicates the cohort left out of the
internal–external cross-validation, which was done once for all 14 different cohorts.
428 www.thelancet.com/neurology Vol 17 May 2018
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
The internal-external cross-validation framework dementia or a C9orf72 repeat expansion was not available
resulted in 14 cycles of model development and external and similar results of predictions using date of onset
validation (meta-analysis shown in figure 1 and versus date of diagnosis as starting point for prediction
appendix). The model was used to define five groups (appendix). A survey of patients’ preferences with regard
with distinct median predicted times (SE) and observed to knowing their personalised prognosis is reported in
times (SE) in months to the composite survival outcome the appendix.
since symptom onset: very short 17·7 (0·20), 16·5 (0·23);
short 25·3 (0·06), 25·2 (0·35); intermediate 32·2 (0·09), Discussion
32·8 (0·46); long 43·7 (0·21), 44·6 (0·74); and very long On the basis of data collected from 11 475 patients with
91·0 (1·84), 85·6 (1·96; figure 1). Comparing the other ALS across Europe, we have developed and externally
groups with the group with very long times to our validated a model for prediction of survival without
composite endpoint revealed hazard ratios (HR) of 15·29 tracheostomy or non-invasive ventilation for more than
(95% CI 13·92–16·79) for the very short group, 23 h per day in individual patients. Using recently
7·19 (6·53–7·91) for the short group, 4·30 (3·94–4·69) developed methods, we derived ranges of predictive
for the intermediate group, and 2·49 (2·30–2·70) for the performance across different settings (ie, population-
long group). Visual inspection of calibration plots 3 years based vs referral-based cohorts) and patient populations,
after onset showed good agreement between predicted thereby providing evidence for the potential
and observed probability for most cohorts generalisability of our model. Medical doctors can use
(n=11; appendix). Predicted and observed probabilities of our model freely online to provide estimates of prognosis
reaching our composite endpoint for cohort-specific in individual patients with ALS, with the aim of
curves showed similar results as calibration plots facilitating its use in clinical practice and in innovative
(appendix). For the three cohorts in which agreement trial design.
between observed and predicted times to our composite Associations between predictors and survival ourcomes
endpoint was suboptimal, recalibration of the baseline in ALS have previously been reported at the group level.6
hazard improved calibration (appendix). Similar Attempts to translate predictive associations into
results were noted for complete case analysis (appendix). estimates of survival outcomes in individual patients
We assessed all possible two-way interactions
(ie, eight covariates with one interaction comprising 0·05 Survival without tracheostomy
two of the eight covariates), which did not improve or non-invasive ventilation
>23 h per day
predictive accuracy (appendix). The probability of good
Probability density of survival composite endpoint
0·04 Very short
external predictive performance of the model was Short
estimated to be 100·0% for the c statistic and 97·1% for Intermediate
0·03 Long
calibration slope. The joint (combined) probability of Very long
good performance was 98·3% (appendix). Compared to No prediction
estimates of group level data, the model provides more 0·02
accurate and precise predictions of times to our
composite endpoint (figure 2). 0·01
Our prediction of time to our composite survival
endpoint is based on the regression coefficients of the 0
final prediction model (appendix) and can be tailored (ie,
recalibration of the incept) for each of the 14 participating
cohorts. To illustrate its potential use in clinical practice,
0 12 24 36 48 60 72 84 96 108 120
we have provided examples of patients selected from our
Time since onset (months)
dataset and their associated predictions, including
uncertainty at the patient level (figure 3) and provided Figure 2: Group predictions
worked examples (appendix). A large proportion of Probability densities for times to our composite endpoint (y-axis) are shown for the five groups from figure 1D.
patients deviated from the median time to reach the The probability density (or distribution) is not evenly distributed over time, meaning that the largest number of
patients are predicted to die at the time when the curve has the highest density, but there is a small chance that
composite survival endpoint (at the group level): patients will survive without tracheostomy or non-invasive ventilation for more than 23 h per day for much
six patients (24%) had a 75% chance of dying, having a longer—this is reflected by the long, thin tails on the right side of this figure. These predictions curves provide
tracheostomy, or having non-invasive ventilation for guidance for discussing prognosis with patients. Furthermore, if the prediction model is not used (dashed curve),
more than 23 h per day before the median time, whereas estimates of group-level data (ie, average or median survival in ALS, without using a personalised prediction) will
generally be overly positive for groups with short or very short times to the composite endpoint, overly negative
eight other patients (32%) had a 75% chance of living for groups with long and very long times to the composite endpoint, or overly uncertain (for groups with
without tracheostomy or non-invasive ventilation for intermediate times to the composite endpoint). The horizontal bars at the bottom provide the same information
more than 23 h per day for longer than the median time. for the different groups, with dots representing median times to our composite endpoint, thick lines representing
probability IQRs, and thin lines representing 10–90% probability intervals to reach our composite survival
The sensitivity analyses showed that the prediction
endpoint. This figure quantifies the uncertainty of individual predictions because, for example, a participant with a
model also provided accurate predictions when patient- predicted very short time to our composite endpoint still has a 2% chance of surviving up to 5 years after onset
level information about the presence of frontotemporal without tracheostomy or non-invasive ventilation for more than 23 h per day.
www.thelancet.com/neurology Vol 17 May 2018 429
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
Progression Diagnostic Age at FVC* Bulbar Definite Fronto- C9orf72
rate (ALS-FRS delay onset onset ALS† temporal
points per month) (months) (years) dementia
25 0·13 39·0 42·3 105·0 − − − −
● 0·14 36·0 54·9 113·0 − − − −
● 0·14 18·1 37·6 112·0 + − − −
● 0·21 16·9 43·1 81·0 − − − −
● 0·36 25·0 65·3 109·0 − − − −
20 ● 0·22 20·0 73·0 98·0 + − − −
● 0·28 24·0 71·5 125·0 + − − +
● 0·56 23·3 62·9 107·0 − − − −
● 0·17 6·0 42·6 47·0 − − − −
0·94 23·3 63·4 75·0 + −
Individual patient number
● − −
15 ● 0·34 8·6 61·9 101·0 + − − −
● 0·30 11·4 52·5 44·3 − + − −
● 0·38 7·5 66·5 84·0 + − − −
● 0·72 13·9 76·5 98·0 − + − −
● 1·34 9·0 53·4 99·0 − − − −
10 ● 0·95 6·7 51·1 76·0 + − − −
● Survival without 0·46 6·0 76·6 85·0 − − + −
● tracheostomy or 1·75 12·0 67·0 113·0 + − − −
●
non-invasive 1·96 9·2 54·6 98·0 + − − −
ventilation
● 1·69 10·7 74·3 70·0 + − − −
>23 h per day
5 ● 0·87 12·1 70·6 36·0 + − − −
Very long
● 1·41 5·0 56·2 96·0 − − + −
Long
●
Intermediate 2·61 6·9 54·3 81·0 − + + +
● Short 3·92 5·4 74·6 84·0 + − − −
● Very short 1·26 12·0 77·2 36·0 + + + −
0
0 12 24 36 48 60 72 84 96 108 120
Predicted time to composite survival endpoint (months)
Figure 3: Clinical applicability to individual patients
Characteristics of and predictions for 25 randomly selected participants with amyotrophic lateral sclerosis (ALS) are presented to illustrate application of the model to
predict time to the survival composite endpoint for individual patients. Predictions are shown on the left and patient characteristics on the right. Median predicted
times to the composite endpoint for individual patients are represented by the dots. The thick coloured lines represent 25–75% probability IQRs and the thin black
lines represent 10–90% probability intervals. The vertical dashed line represents the median time to the composite endpoint (34·7 months). Predicted times to our
composite endpoint differed substantially between patients, reflecting both heterogeneity in ALS and the ability of the proposed model to stratify patients according
to their characteristics. +=present. –=absent. *Forced vital capacity (FVC) expressed as percentage of predicted (based on normative values for age, sex, and height).
†Definite ALS determined according to revised El Escorial criteria.
with ALS are, however, infrequent and external validation distributions for times to our composite endpoint were
of such models remains elusive.35 It is acknowledged that skewed, point estimates might not be preferred for
the development of reliable prediction models requires predictions in individual patients. Ranges will become
access to large datasets, with at least 200 events for wider for patients with longer times to our composite
validation.8 Hence, the current meta-analysis of endpoint, owing to less steep prognostic curves.
individual participant data is the first study in ALS to Large-scale, European Union funded, collaborative
For more on Euro-MOTOR see enable the investigation of a large number of predictors, projects, such as Euro-MOTOR, SOPHIA, and NETCALS
www.euromotorproject.eu combining them in a prediction model. This is the encourage standardised and harmonised data collection
For more on SOPHIA see first prediction model in ALS that rigorously assessed between the three population-based registries
www.sophiaproject.eu
discrimination and calibration performance across (n=4776, 42%) and 11 referral-based patient registries
For more on NETCALS see
different populations. We identified sources of (n=6699, 58%) that contributed data to our study.36,37
www.jpnd.eu
heterogeneity across the cohorts, and addressed Differences in standard of care and cultural or genetic
transportability issues of the model.27,28 This enabled us to background between registries were taken into account
determine the likely performance when applying the in our model by allowing cohort-specific adjustments for
model in clinical practice, and thus to assess its clinical estimation of prognosis in individual patients.
use in local circumstances. Dependent on requirements Predictors and times to our composite endpoint are
and clinicians’ or patients’ preferences, the model can be likely to differ between different populations, as shown
applied using probabilities of survival without in our study. This might be due to real differences
tracheostomy or non-invasive ventilation for more than between populations. Other possibilities might be
23 h per day, prognostic groups, or point estimates. For referral bias in referral-based versus population-based
clinical care, we prefer the first two options, because registries, variable interpretation of diagnostic criteria,
these provide the possibility of being realistic without differences in standard care, cultural or genetic
being unduly negative (appendix). Because the probability background, or a combination of these factors.
430 www.thelancet.com/neurology Vol 17 May 2018
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
Importantly, internal–external cross-validation in our incurable disease. Furthermore, the outcomes of the
study did not reveal that differences between populations administered questionnaire might differ in patients from
affected predictive performance of our model. other cultural backgrounds; a selection bias might be
Furthermore, differences in times to our composite present in the patients who responded to the survey; and
endpoint between cohorts could not be interpreted as patients might not foresee all consequences of the
being caused by a specific cohort. knowledge, and might regret asking to be informed if the
A weakness of our study is that we did not include predicted time to death, tracheostomy, or non-invasive
treatment with riluzole, the only effective drug with ventilation for more than 23 h per day they receive is
proven effect on survival, as a predictor in our model. shorter than expected. To minimise the risk of such
Reliable information about its usage is missing in most potential harm, the model will be accessible online only to
registries, but is estimated to be at least 75% in Europe.13 medical doctors who have to register and sign in before
Although the effect of riluzole on survival (pooled access is provided. Professional health-care providers
HR 0·84, based on a Cochrane meta-analysis)14 is more might use our model to determine the intensity of care
than ten times smaller than the combined effect of pathways and to tailor counselling of individual patients
predictors in our proposed model (HR up to 15·29), and their caregivers. Prediction models might improve
incorporating riluzole use as well as other treatments, clinical trial design in two ways: use of the predicted
such as ventilation or gastrostomy, into our model will outcome as an inclusion criterion instead of arbitrary
allow further tailoring of predictions. eligibility criteria and use of predicted prognosis instead
Missing data, which is inherent to observational data, of a limited set of prognostic variables to stratify
can lead to biased results when not appropriately randomisation, thereby creating more homogeneous
addressed. We therefore used imputation methods that strata and greater statistical power to detect an effect. This
are proven to prevent such biases, even if a predictor is was, for example, previously shown in patients with
completely missing from one or more cohorts.32 Using glioblastoma who have methylation of the MGMT
internal–external cross-validation, we rigorously assessed (O⁶-methylguanine–DNA methyltransferase) gene.40
the model’s predictive performance in external datasets. In accordance with the TRIPOD statement,10 all
This approach not only allows assessment of the model’s parameters and equations of our model were provided
overall performance in new patients, but also to establish (appendix) to allow improvement of predictions through
whether performance is consistent across the different continuing research into other prognostic factors (eg, wet
cohorts. Internal–external cross-validation therefore helps or imaging biomarkers or newly discovered genetic
to determine to what extent model generalisability might mutations) or implementation of outcome measures
be affected by differences in definition of endpoint, in other than our composite survival endpoint (eg, being
collection of FVC versus SNIP or ALSFRS versus wheelchair-bound or other specific loss of function). This
ALSFRS-R data, in possible recall bias of disease onset, in should also facilitate validation of our model in registries
recruitment of patients between cohorts, in heterogeneity from a non-European background and its application in
of disease characteristics between cohorts, or in the clinical trial populations.
presence of unmeasured confounders. Although we did In conclusion, we have developed and externally
not aim to study such differences between cohorts and we validated a model for prediction of survival without
can only speculate about possible causes (eg, intrinsic tracheostomy or non-invasive ventilation more than 23 h
differences of ALS between cohorts, or extrinsic per day in individual patients with ALS. We have shown
differences due to possible differences in, eg, clinical the generalisable and robust predictive performance of
care), these differences did not appear to reduce the this model and made it freely available online. The
predictive performance of our proposed prediction model. outcomes of this study have the potential to facilitate
Our online model is ethically sensitive and demands tailored care and trial design, which will hopefully lead to
thoughtful implementation. It might support clinicians in a more successful discovery of effective treatments for
helping patients to maintain a degree of autonomy and patients with this devastating disease.
help them in planning their lives. Our survey showed that Contributors
some patients preferred to be informed about their H-JW, TPAD, KGMM, JHV, and LHvdB contributed to the study design.
personalised life expectancy (appendix). This is in line H-JW did the literature search and created the figures. H-JW and TPAD
analysed the data. All authors contributed to the data collection and
with previous reports in cancer medicine.38 The ethical interpretation of results, reviewed and critically revised the manuscript,
aspects of tailored predictions in ALS or other and approved the final version for submission.
neurodegenerative diseases have not been studied before, Declaration of interests
but from cancer medicine it is known that early JPKR reports grants from the Irish Health Research Board (grant number
discussions about goals of care are associated with better HPF-2014-537). CJM was supported by the UK Motor Neurone Disease
quality of life, reduced use of non-beneficial medical care Association. MAvE serves on the Motor Neurone Disease Association
biomedical research advisory panel, has consulted for Biogen and received
near death, enhanced goal-consistent care, positive family travel grants from Baxalta, and funding sources include the Netherlands
outcomes, and reduced costs.39 However, many cancers Organization for Health Research and Development (Veni scheme), The
have several modes of therapy, whereas ALS is still an Thierry Latran Foundation, the ALS Foundation Netherlands, and the
www.thelancet.com/neurology Vol 17 May 2018 431
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
European Union (EU) Joint Programme Neurodegenerative Disease 12 Brooks BR, Miller RG, Swash M, Munsat TL, World Federation of
Research (JPND). MW reports personal fees from Biogen Idec and Neurology Research Group on Motor Neuron Disease. El Escorial
Mitsubishi Tanabe Pharma. SP reports grants from the German revisited: revised criteria for the diagnosis of amyotrophic lateral
Neuromuscular Society, the German Federal Ministry of Education and sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 2000;
Research, clinical trial funding from Cytokinetics, GlaxoSmithKline, and 1: 293–99.
Orion Pharma, and speaking fees from Teva Pharmaceutical Industries. 13 Cudkowicz ME, van den Berg LH, Shefner JM, et al.
PVD reports personal fees for advisory work from Cytokinetics, and Dexpramipexole versus placebo for patients with amyotrophic
lateral sclerosis (EMPOWER): a randomised, double-blind,
personal fees for advisory work (paid to his institution) from Biogen,
phase 3 trial. Lancet Neurol 2013; 12: 1059–67.
Pfizer, CSL Behring, and Treeway. KT is supported by the Motor Neurone
14 Miller RG, Mitchell JD, Moore DH. Riluzole for amyotrophic lateral
Disease Association and the UK Medical Research Council (MRC). MRT is
sclerosis (ALS)/motor neuron disease (MND).
supported by the UK MRC and Motor Neurone Disease Association Lady Cochrane Database Syst Rev 2012; 3: CD001447.
Edith Wolfson Senior Clinical Fellowship (MR/K01014X/1). PJS reports
15 Kimura F, Fujimura C, Ishida S, et al. Progression rate of
grants from the UK National Institute of Health Research (NIHR; Senior ALSFRS-R at time of diagnosis predicts survival time in ALS.
Investigator Award), Sheffield NIHR Biomedical Research Centre for Neurology 2006; 66: 265–67.
Translational Neuroscience, the Motor Neurone Disease Association, the 16 Gallo V, Wark PA, Jenab M, et al. Prediagnostic body fat and risk of
EU JPND (STRENGTH project), the UK MRC, EU Horizon 2020 death from amyotrophic lateral sclerosis: the EPIC cohort.
(Modifying Immune Response and Outcomes in ALS [MIROCALS] trial) Neurology 2013; 80: 829–38.
and grants from ReNeuron; and clinical trial funding from Cytokinetics, 17 Calvo A, Canosa A, Bertuzzo D, et al. Influence of cigarette
Orion Pharma, and Biogen Idec. AA-C is a consultant for Mitsubishi smoking on ALS outcome: a population-based study.
Tanabe Pharma, Chronos Therapeutics, Orion Pharma, Cytokinetics, and J Neurol Neurosurg Psychiatry 2016; 87: 1229–33.
Treeway. AC reports grants from Italfarmaco, and personal fees from 18 Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised
Biogen Idec and Mitsubishi. OH is a journal editor for Amyotrophic Lateral diagnostic criteria for the behavioural variant of frontotemporal
Sclerosis and Frontotemporal Degeneration; and reports grants from dementia. Brain 2011; 134: 2456–77.
the Irish Health Research Board (CSA 2012/11), Science Foundation 19 Abrahams S, Leigh PN, Harvey A, Vythelingum GN, Grise D,
Ireland (15/SPP/3244 and 16/ERCD/3854), and the charity Research Motor Goldstein LH. Verbal fluency and executive dysfunction in
Neurone. LHvdB reports grants from The Netherlands ALS Foundation, amyotrophic lateral sclerosis (ALS). Neuropsychologia 2000;
The Netherlands Organization for Health Research and Development 38: 734–47.
(ZonMw; Vici scheme), the EU 7th framework programme (grant number 20 Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal
259867) for the Euro-MOTOR project, The Netherlands Organization for Assessment Battery at bedside. Neurology 2000; 55: 1621–26.
Health Research and Development (Sampling and biomarker 21 Raaphorst J, Beeldman E, Schmand B, et al. The ALS-FTD-Q: a new
OPtimization and Harmonization In ALS and other motor neuron screening tool for behavioral disturbances in ALS. Neurology 2012;
diseases [SOPHIA], funded through JPND), and Baxalta; and personal fees 79: 1377–83.
from Biogen, Cytokinetics, and Baxalta. All other authors declare no 22 Diekstra FP, van Vught PW, van Rheenen W, et al. UNC13A is a
competing interests. modifier of survival in amyotrophic lateral sclerosis.
Neurobiol Aging 2012; 33: 630 e3–8.
Acknowledgments 23 Majounie E, Renton AE, Mok K, et al. Frequency of the C9orf72
The Netherlands ALS Foundation funded this study. We thank all the hexanucleotide repeat expansion in patients with amyotrophic
patients with amyotrophic lateral sclerosis who, notwithstanding their lateral sclerosis and frontotemporal dementia: a cross-sectional
devastating disease, participated in this study. study. Lancet Neurol 2012; 11: 323–30.
24 van Blitterswijk M, DeJesus-Hernandez M, Rademakers R. How do
References
C9ORF72 repeat expansions cause amyotrophic lateral sclerosis and
1 GBD 2015 Mortality and Causes of Death Collaborators.
frontotemporal dementia: can we learn from other noncoding
Global, regional, and national life expectancy, all-cause mortality,
repeat expansion disorders? Curr Opin Neurol 2012; 25: 689–700.
and cause-specific mortality for 249 causes of death, 1980-2015:
a systematic analysis for the Global Burden of Disease Study 2015. 25 Fregonezi G, Araujo PR, Macedo TL, Dourado Junior ME,
Lancet 2016; 388: 1459–544. Resqueti VR, Andrade Ade F. Monitoring respiratory muscle
strength assists in early diagnosis of respiratory dysfunction as
2 Jameson JL, Longo DL. Precision medicine—personalized,
opposed to the isolated use of pulmonary function evaluation in
problematic, and promising. N Engl J Med 2015; 372: 2229–34.
amyotrophic lateral sclerosis. Arq Neuropsiquiatr 2013; 71: 146–52.
3 Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral
26 Heymans MW, van Buuren S, Knol DL, van Mechelen W,
sclerosis. Lancet 2011; 377: 942–55.
de Vet HC. Variable selection under multiple imputation using the
4 van Es MA, Hardiman O, Chio A, et al. Amyotrophic lateral bootstrap in a prognostic study. BMC Med Res Methodol 2007; 7: 33.
sclerosis. Lancet 2017; 390: 2084–98.
27 Debray TP, Moons KG, Ahmed I, Koffijberg H, Riley RD.
5 Ringholz GM, Appel SH, Bradshaw M, Cooke NA, Mosnik DM, A framework for developing, implementing, and evaluating clinical
Schulz PE. Prevalence and patterns of cognitive impairment in prediction models in an individual participant data meta-analysis.
sporadic ALS. Neurology 2005; 65: 586–90. Stat Med 2013; 32: 3158–80.
6 Chio A, Logroscino G, Hardiman O, et al. Prognostic factors in 28 Debray TP, Riley RD, Rovers MM, Reitsma JB, Moons KG,
ALS: a critical review. Amyotroph Lateral Scler 2009; 10: 310–23. Cochrane IPDM-aMg. Individual participant data (IPD)
7 van Rheenen W, van Blitterswijk M, Huisman MH, et al. meta-analyses of diagnostic and prognostic modeling studies:
Hexanucleotide repeat expansions in C9ORF72 in the spectrum of guidance on their use. PLoS Med 2015; 12: e1001886.
motor neuron diseases. Neurology 2012; 79: 878–82. 29 Snell KI, Hua H, Debray TP, et al. Multivariate meta-analysis of
8 Collins GS, Ogundimu EO, Altman DG. Sample size considerations individual participant data helped externally validate the
for the external validation of a multivariable prognostic model: performance and implementation of a prediction model.
a resampling study. Stat Med 2016; 35: 214–26. J Clin Epidemiol 2016; 69: 40–50.
9 Riley RD, Ensor J, Snell KI, et al. External validation of clinical 30 Royston P, Parmar MK. Flexible parametric proportional-hazards
prediction models using big datasets from e-health records or IPD and proportional-odds models for censored survival data, with
meta-analysis: opportunities and challenges. BMJ 2016; 353: i3140. application to prognostic modelling and estimation of treatment
10 Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent effects. Stat Med 2002; 21: 2175–97.
reporting of a multivariable prediction model for individual 31 Sauerbrei W, Royston P. Building multivariable prognostic and
prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ diagnostic models: transformation of the predictors by using
2015; 350: g7594. fractional polynomials. J R Stat Soc Series A Stats Soc 1999; 162: 71–94.
11 Huisman MH, de Jong SW, van Doormaal PT, et al. Population based 32 Quartagno M, Carpenter JR. Multiple imputation for IPD
epidemiology of amyotrophic lateral sclerosis using capture-recapture meta-analysis: allowing for heterogeneity and studies with missing
methodology. J Neurol Neurosurg Psychiatry 2011; 82: 1165–70. covariates. Stat Med 2016; 35: 2938–54.
432 www.thelancet.com/neurology Vol 17 May 2018
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
Articles
33 Sterne JA, White IR, Carlin JB, et al. Multiple imputation for 37 Hardiman O, Al-Chalabi A, Brayne C, et al. The changing picture of
missing data in epidemiological and clinical research: potential and amyotrophic lateral sclerosis: lessons from European registers.
pitfalls. BMJ 2009; 338: b2393. J Neurol Neurosurg Psychiatry 2017; 88: 557–63.
34 Royston P, Altman DG. External validation of a Cox prognostic 38 Innes S, Payne S. Advanced cancer patients’ prognostic information
model: principles and methods. BMC Med Res Methodol 2013; preferences: a review. Palliat Med 2009; 23: 29–39.
13: 33. 39 Bernacki RE, Block SD, American College of Physicians High Value
35 Elamin M, Bede P, Montuschi A, Pender N, Chio A, Hardiman O. Care Task Force. Communication about serious illness care goals:
Predicting prognosis in amyotrophic lateral sclerosis: a simple a review and synthesis of best practices. JAMA Intern Med 2014;
algorithm. J Neurol 2015; 262: 1447–54. 174: 1994–2003.
36 D’Ovidio F, Rooney JPK, Visser AE, et al. Critical issues in ALS 40 Hegi ME, Diserens A, Gorlia T, et al. MGMT gene silencing and
case-control studies: the case of the Euro-MOTOR study. benefit from temozolomide in glioblastoma. N Engl J Med 2005;
Amyotroph Lateral Scler Frontotemporal Degener 2017; 18: 411–18. 352: 997–1003.
www.thelancet.com/neurology Vol 17 May 2018 433
Descargado para Anonymous User (n/a) en Universidad Libre de Colom de ClinicalKey.es por Elsevier en febrero 07, 2019.
Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2019. Elsevier Inc. Todos los derechos reservados.
You might also like
- Long-Term Prognosis After Childhood Convulsive Status Epilepticus: A Prospective Cohort StudyDocument9 pagesLong-Term Prognosis After Childhood Convulsive Status Epilepticus: A Prospective Cohort Studynadia pramitha157No ratings yet
- MR Clean Late LancetDocument10 pagesMR Clean Late LancetLetícia JanuziNo ratings yet
- Kim 2015Document9 pagesKim 2015Ke XuNo ratings yet
- S974 Abstract Book ESTRO 2022: Variable N (%)Document1 pageS974 Abstract Book ESTRO 2022: Variable N (%)andresNo ratings yet
- Prognostic Factors For Relapse and Outcome in Pediatric Acute Transverse MyelitisDocument11 pagesPrognostic Factors For Relapse and Outcome in Pediatric Acute Transverse Myelitisyusak sampeNo ratings yet
- PrognosisDocument7 pagesPrognosisMuhammad Rafli AkbarNo ratings yet
- Screening TBC in HIV RSDocument9 pagesScreening TBC in HIV RSCesar E Sanchez AlvarezNo ratings yet
- A Comparison of Machine Learning Models Versus Clinical Evaluation For Mortality Prediction in Patients With SepsisDocument15 pagesA Comparison of Machine Learning Models Versus Clinical Evaluation For Mortality Prediction in Patients With SepsisMariana NannettiNo ratings yet
- Articles: BackgroundDocument11 pagesArticles: BackgroundricardojosesotofontalvoNo ratings yet
- Craniectomia 3Document8 pagesCraniectomia 3Vlady78No ratings yet
- 1 s2.0 S1474442220304397 MainDocument9 pages1 s2.0 S1474442220304397 MainanankastikNo ratings yet
- Eficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaDocument11 pagesEficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaSMIBA MedicinaNo ratings yet
- Antonio Jose GrandeDocument23 pagesAntonio Jose Grandeagung dwi darmawanNo ratings yet
- Mortality Risk Factors in Primary Sjögren Syndrome: A Real-World, Retrospective, Cohort StudyDocument16 pagesMortality Risk Factors in Primary Sjögren Syndrome: A Real-World, Retrospective, Cohort Studygiorgio.cavazziniNo ratings yet
- Flaherty 2016Document6 pagesFlaherty 2016Diornald MogiNo ratings yet
- Ficha 4Document12 pagesFicha 4mariaNo ratings yet
- Malignant External Otitis: Factors Predicting Patient OutcomesDocument6 pagesMalignant External Otitis: Factors Predicting Patient OutcomesYogaPriambudiNo ratings yet
- (10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenDocument6 pages(10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenFatima RamirezNo ratings yet
- Definition and Validation of Serum Biomarkers For Optimal Differentiation of Hyperferritinaemic Cytokine Storm Conditions in Children - A Retrospective Cohort StudyDocument11 pagesDefinition and Validation of Serum Biomarkers For Optimal Differentiation of Hyperferritinaemic Cytokine Storm Conditions in Children - A Retrospective Cohort StudyntnquynhproNo ratings yet
- Vandenbent 2021Document11 pagesVandenbent 2021bugNo ratings yet
- Intravenous Tenecteplase Compared With Alteplase For Acute IschaemicDocument9 pagesIntravenous Tenecteplase Compared With Alteplase For Acute IschaemicVictoria JacoboNo ratings yet
- Disseminated Intravascular Coagulation Initial Score As A Predictor ofDocument6 pagesDisseminated Intravascular Coagulation Initial Score As A Predictor ofPriska ForceveeanaNo ratings yet
- Two-Year Outcome After Endovascular Treatment For Acute Ischemic StrokeDocument9 pagesTwo-Year Outcome After Endovascular Treatment For Acute Ischemic Strokedoni anandaNo ratings yet
- The Evans' Index RevisitedDocument5 pagesThe Evans' Index RevisitedLuciano AlvesNo ratings yet
- ShearWave Elastography Thyroid NodulesDocument8 pagesShearWave Elastography Thyroid Nodulesinfo8089No ratings yet
- Presición de EcografíaDocument3 pagesPresición de Ecografíasamuelfdiaz.0103No ratings yet
- National Institutes of Health Stroke ScaleDocument9 pagesNational Institutes of Health Stroke ScaleMARSYA TRILAKSMI HAPSARINo ratings yet
- Risk Factors For and The Role of Dental Extractions in Osteoradionecrosis of The Jaws: A National-Based Cohort StudyDocument9 pagesRisk Factors For and The Role of Dental Extractions in Osteoradionecrosis of The Jaws: A National-Based Cohort Studyita mustainahNo ratings yet
- American Journal of Emergency MedicineDocument5 pagesAmerican Journal of Emergency MedicineMaria teresa salinas merelloNo ratings yet
- Hou, Et Al., 2021Document9 pagesHou, Et Al., 2021NyomantrianaNo ratings yet
- 1gorgan BrainAbcessesDocument8 pages1gorgan BrainAbcessesGema Rizki PratamaNo ratings yet
- HSCRP (High-Sensitivity C - Reactive Protein) and Its Association With Short Term Prognosis Following Ischaemic StrokeDocument5 pagesHSCRP (High-Sensitivity C - Reactive Protein) and Its Association With Short Term Prognosis Following Ischaemic Strokeahc4allNo ratings yet
- Prognostic Tools For ....Document15 pagesPrognostic Tools For ....I'am AjhaNo ratings yet
- 2020-Incremental Prognostic Value and Underlying Biological Pathways of Radiomics Patterns in MedulloblastomaDocument10 pages2020-Incremental Prognostic Value and Underlying Biological Pathways of Radiomics Patterns in Medulloblastoma原彬科No ratings yet
- Pmed 1002313 PDFDocument19 pagesPmed 1002313 PDFgizandhNo ratings yet
- Prognosis CRCDocument22 pagesPrognosis CRCmehwishsardar0024No ratings yet
- Shared Genetic Susceptibility To Ischemic Stroke and Coronary Artery DiseaseDocument28 pagesShared Genetic Susceptibility To Ischemic Stroke and Coronary Artery DiseaseJimmy ROMANNo ratings yet
- Diagnosis and Classification in MRI of Brucellar SpondylitisDocument6 pagesDiagnosis and Classification in MRI of Brucellar SpondylitisMANGNo ratings yet
- 2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeDocument7 pages2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeSafitri MuhlisaNo ratings yet
- Long-Term Mortality and Epilepsy in Patients Afterbrain Abscess A Nationwide Population-Based Matched Cohort StudyDocument29 pagesLong-Term Mortality and Epilepsy in Patients Afterbrain Abscess A Nationwide Population-Based Matched Cohort StudyAnisa Iswari Pombaile-NgurawanNo ratings yet
- Delirium Detection Using Wearable Sensors and Machine Learning in Patients With Intracerebral HemorrhageDocument7 pagesDelirium Detection Using Wearable Sensors and Machine Learning in Patients With Intracerebral HemorrhageedavioNo ratings yet
- Surgical Neurology International: Socioeconomic Status Does Not Affect Prognosis in Patients With Glioblastoma MultiformeDocument9 pagesSurgical Neurology International: Socioeconomic Status Does Not Affect Prognosis in Patients With Glioblastoma MultiformeALINo ratings yet
- JamdaDocument9 pagesJamdaw5rh7kqg6pNo ratings yet
- 1 s2.0 S0001299822000587 MainDocument14 pages1 s2.0 S0001299822000587 MainIsabella ToribioNo ratings yet
- Surgical Neurology International: Chronic Subdural Hematoma: Surgical Management and OutcomeDocument9 pagesSurgical Neurology International: Chronic Subdural Hematoma: Surgical Management and OutcomeSelfa YunitaNo ratings yet
- Choroid Plexus Volume in Multiple Sclerosis Vs Neuromyelitis Optica Spectrum DisorderDocument14 pagesChoroid Plexus Volume in Multiple Sclerosis Vs Neuromyelitis Optica Spectrum DisorderYaquelin del valle torres DomínguezNo ratings yet
- 701 2010 Article 878Document9 pages701 2010 Article 878Rifqi FNo ratings yet
- Bjs 11306Document11 pagesBjs 11306Carlos Perez RiveraNo ratings yet
- HydrocephalusDocument8 pagesHydrocephaluscaliptra36No ratings yet
- Autologous: Journal HomepageDocument9 pagesAutologous: Journal HomepageSiddharth DhanarajNo ratings yet
- Lancet Oncol 2013 VermorkenDocument14 pagesLancet Oncol 2013 Vermorkens007972No ratings yet
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahNo ratings yet
- Meeting Abstracts From The 7th Danish Emergency Medicine ConferenceDocument8 pagesMeeting Abstracts From The 7th Danish Emergency Medicine ConferenceVille SalmensuuNo ratings yet
- Abstracts of The 18th Congress of The European Geriatric Medicine SocietyDocument439 pagesAbstracts of The 18th Congress of The European Geriatric Medicine SocietyCristina Fernández DíazNo ratings yet
- 2361 15492 1 PBDocument6 pages2361 15492 1 PBAndri ArdhanyNo ratings yet
- Life Expectancy at Birth in Duchenne Muscular Dystrophy: A Systematic Review and Meta AnalysisDocument11 pagesLife Expectancy at Birth in Duchenne Muscular Dystrophy: A Systematic Review and Meta AnalysisAngella MariaNo ratings yet
- Predicting Opioid Overdose Risk of PatientsDocument8 pagesPredicting Opioid Overdose Risk of PatientsSabin TabircaNo ratings yet
- 026 Prof-2033Document4 pages026 Prof-2033dgina8800No ratings yet
- Idrovo 2010Document6 pagesIdrovo 2010GatoNo ratings yet
- 3in1 Shoulder BlockDocument2 pages3in1 Shoulder BlockTejasvi ChandranNo ratings yet
- Guidance COVID-19Document5 pagesGuidance COVID-19hemkumar DahalNo ratings yet
- OB-Reviewer With AlgorithmDocument29 pagesOB-Reviewer With Algorithmriczen mae vilaNo ratings yet
- Pediatric Musculoskeletal Summary For Osce ExamDocument53 pagesPediatric Musculoskeletal Summary For Osce Examopscurly100% (2)
- Health FormsDocument5 pagesHealth FormsBianca Louise SengcoNo ratings yet
- Ectopic Pregnancy (m104)Document13 pagesEctopic Pregnancy (m104)Alphine DalgoNo ratings yet
- Legal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DDocument6 pagesLegal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DarciblueNo ratings yet
- Urn Uvci 01 Ro O0el5r27d48j5197y9nx3vwpgq96km#bDocument2 pagesUrn Uvci 01 Ro O0el5r27d48j5197y9nx3vwpgq96km#bgrigore sinteanuNo ratings yet
- CHN Finals ExamDocument10 pagesCHN Finals ExamJhayneNo ratings yet
- Lesson Plan Genito UrinaryDocument26 pagesLesson Plan Genito UrinaryEllen AngelNo ratings yet
- Efficacy of Glimepiride/metformin Combination Versus Glibenclamide/ Metformin in Patients With Uncontrolled Type 2 Diabetes MellitusDocument4 pagesEfficacy of Glimepiride/metformin Combination Versus Glibenclamide/ Metformin in Patients With Uncontrolled Type 2 Diabetes Mellitusfannia nabillaNo ratings yet
- Abnormal Illness BehaviorDocument7 pagesAbnormal Illness Behavioransha2011p0% (1)
- CV Dr. Eko Arianto SpU 2021Document10 pagesCV Dr. Eko Arianto SpU 2021Bedah ManadoNo ratings yet
- Atrial Fibrillation Topic DiscussionDocument23 pagesAtrial Fibrillation Topic Discussionapi-567600964No ratings yet
- Diagnostic Criteria Decision Tree PDFDocument2 pagesDiagnostic Criteria Decision Tree PDFNor Nadia ZakariaNo ratings yet
- Onco-Critical Care An Evidence-Based ApproachDocument539 pagesOnco-Critical Care An Evidence-Based ApproachZuriNo ratings yet
- Occupational Safety and HealthDocument9 pagesOccupational Safety and HealthWan SaitamaNo ratings yet
- Marijuana and EpilepsyDocument17 pagesMarijuana and EpilepsyOmar AntabliNo ratings yet
- Mental Health and Hindu Psicology by Swami AkhilanandaDocument245 pagesMental Health and Hindu Psicology by Swami Akhilanandaapi-19985927100% (3)
- Devoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)Document4 pagesDevoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)ferchichi halimaNo ratings yet
- 6th Charles Merieux Conference 2019 Pre Post Analytical Errors in HematologyDocument7 pages6th Charles Merieux Conference 2019 Pre Post Analytical Errors in HematologyYaser MNo ratings yet
- Nutrition & LongevityDocument28 pagesNutrition & LongevityHAFIZ MUHAMMAD IMTIAZNo ratings yet
- Nonoperative Management of Femoroacetabular ImpingementDocument8 pagesNonoperative Management of Femoroacetabular ImpingementRodrigo SantosNo ratings yet
- Pga R3Document71 pagesPga R3Samruddhi PataitNo ratings yet
- Revitears Study 2Document16 pagesRevitears Study 2office.hospimedNo ratings yet
- Adverse Drug ReactionDocument15 pagesAdverse Drug ReactionPuji Arifianti RamadhanyNo ratings yet
- Animals Should Not Be Used As A Laboratory ToolsDocument6 pagesAnimals Should Not Be Used As A Laboratory ToolsLuisa Castillo100% (1)
- Toxicity Review Natural ProductsDocument5 pagesToxicity Review Natural Productsamino12451No ratings yet
- Parkinson S Disease Epidemiology,.9Document5 pagesParkinson S Disease Epidemiology,.9bacharelado2010No ratings yet
- Sensitivity and SpecificityDocument12 pagesSensitivity and Specificitymia farrowNo ratings yet