Professional Documents
Culture Documents
Full-Balancing AMCs Missions and Health Care Costs - Mission Impossible PDF
Full-Balancing AMCs Missions and Health Care Costs - Mission Impossible PDF
Uploaded by
rafaelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Full-Balancing AMCs Missions and Health Care Costs - Mission Impossible PDF
Full-Balancing AMCs Missions and Health Care Costs - Mission Impossible PDF
Uploaded by
rafaelCopyright:
Available Formats
PERSPE C T I V E balancing amc s ’ missions and health care costs
Balancing AMCs’ Missions and Health Care Costs —
Mission Impossible?
Elizabeth G. Nabel, M.D., Timothy G. Ferris, M.D., M.P.H., and Peter L. Slavin, M.D.
W hen major provisions of the
Affordable Care Act (ACA)
are implemented next January, few
continuity, and care coordina-
tion, relying heavily on data and
measurement.3 We call this ap-
care as the hub for managing
populations’ care through preven-
tive services, care for chronic ill-
institutions will feel the pressure proach population health manage- nesses, and care coordination for
to control costs more acutely than ment, and implementing it poses high-risk patients. We’re expand-
academic medical centers (AMCs), different risks and challenges for ing our cadre of employed PCPs
which must balance the impera- AMCs than for others. Balancing and advanced practice nurses and
tives of clinical care with cost- efforts to contain costs against are committed to ensuring that
intensive missions in research, investment in our missions in- all our primary care practices be-
teaching, and community health. volves trade-offs among impor- come certified by the National
Massachusetts AMCs don’t have tant goals. We view meeting this Committee for Quality Assurance
to guess at the law’s likely im- challenge as a key contribution we (NCQA) as Patient-Centered Med-
pact: in 2006, our state launched can make to health care’s future. ical Homes. So far, about 350
its own health care reform in- In 2011, Brigham and Wom- providers are engaged in practice
volving principles and policy so- en’s Hospital (BWH) and Massa- redesign, and six lead practices
lutions similar to the ACA’s. chusetts General Hospital (MGH), have achieved NCQA recognition.
Massachusetts therefore provides through Partners HealthCare, The most expensive compo-
a laboratory for gauging the ef- chose to participate in risk-based nent of this expanded investment
fects of such reforms. contracts with commercial pay- is 71 “high-risk care managers”
Having largely solved the in- ers and the Centers for Medicare who work closely with PCPs, each
surance problem, Massachusetts and Medicaid Services as a Pio- coordinating the care of approxi-
passed sweeping cost-control leg- neer Accountable Care Organiza- mately 200 high-risk patients.
islation in 2012, including set- tion. Under these contracts, we This program arose from a suc-
ting a target ceiling on growth of share financial risk for the in- cessful Medicare demonstration
total medical expenses. Although crease in total medical expenses project started at MGH in 2006
Massachusetts’ health care costs for patients who see primary care and expanded to BWH in 2009.
are among the highest in the physicians (PCPs) in our network. Independent evaluations have
country in absolute terms, they’re If our cost growth exceeds that found cost reductions of 2.5% to
among the lowest when adjusted of a comparison group, we pay 19% for the care of multiple suc-
for cost of living.1 Nonetheless, penalties; if it’s lower than that cessive cohorts of enrollees —
AMCs’ share of hospital admis- group’s, we share in the savings. for total taxpayer savings of more
sions is higher in Massachusetts These contracts cover more than than $50 million. The nearly
than in any other state, and 400,000 patients — more than three-to-one return on investment
AMCs’ costs are typically higher one third of the patients who re- has made this program the cen-
than those of non-AMC provid- ceive care in our hospitals annu- terpiece of our efforts and given
ers.2 As a national hub for medi- ally. In addition to the financial us greater confidence to take on
cal research and education, Mas- incentive, these contracts help us further cost-containment chal-
sachusetts must carefully limit restrain cost growth by providing lenges.
the growth of health care costs a measuring stick to assess our Unlike the failed managed-care
without undermining the future progress in developing and deploy- efforts of the 1990s, our initia-
of this important resource. ing innovative care-delivery pro- tives involve our specialists as
At the state’s two largest cesses that are more efficient and well. Specialists’ decisions drive a
AMCs, we’ve addressed this chal- more satisfying to patients and large fraction of costs, especially
lenge in part by using known that result in higher-quality care. for commercially insured popula-
methods for improving access, We’ve focused first on primary tions. Having assessed our pri-
994 n engl j med 369;11 nejm.org september 12, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 20, 2015. For personal use only. No other uses without permission.
Copyright © 2013 Massachusetts Medical Society. All rights reserved.
PERSPECTIVE balancing amc s ’ missions and health care costs
mary care population’s unmet cal revenues. Moreover, govern- tensions remain — among them,
needs, we’re adding clinical staff ment payer rates have not kept balancing the imperative of cost-
in such areas as mental health, pace with inflation for more efficient, high-quality clinical care
general cardiology, dermatology, than a decade. Therefore, fund- with our research, education, and
and physical therapy. We are ing for these new AMC costs community health missions, es-
changing the way we provide care, must come from growth in re- pecially as federal budget cuts
using innovative approaches such gional, national, and internation- and payment rule changes im-
as referral management, virtual al referrals and reductions in our pose substantial pressure. We do
visits, one-time home nursing cost structure — a difficult and not yet have solutions to these
visits, team-based care, and home perennial problem that we are difficult challenges, but we’re com-
telemonitoring. We have a pro- addressing. mitted to innovative approaches
cess for actively reviewing and A second difference from 1990s to solving them.
redesigning the way we deliver managed care is our development Fortunately, our teaching mis-
care, condition by condition, that of a coordinated process for shar- sion is wholly compatible with
emphasizes optimizing the pa- ing risk across our AMCs and our care-delivery changes: we are
tient’s care experience (continu- physician groups. Our perfor- educating providers and physi-
ity of information, management mance framework encourages cians-in-training about the future
plan, and relationships) and the shared practices for managing of clinical care. New payment
efficient delivery of services care for populations rather than systems encourage a convergence
throughout an episode of care. holding each physician account- of AMCs’ clinical and communi-
For example, we’ve reduced ad- able for individual patient costs. ty health missions: investments
missions for transient ischemic
attacks by making the required
testing immediately available for
Today’s central challenge is
outpatients; we’ve improved dia- the rising cost of health care.
betes care by automating refer-
rals to diabetes counselors; and
we’ve begun reviewing specialist Accordingly, the financial risk in community health have his-
referrals to identify opportunities shared with payers is held at the torically been charitable but now
for providing consultations with- level of the integrated delivery promise to reduce medical ex-
out requiring face-to-face visits. system. In turn, we’ve created an penses for affected populations.
Changing these processes pre internal incentive system designed The impact on basic, clinical, and
sents unique challenges to AMC to accelerate and reinforce the population-based research is less
physicians, partly because care adoption of primary and special- clear. Innovation distinguishes
delivery is only one of their re- ty care programs and encourage AMCs, and ensuring that basic
sponsibilities, in addition to re- local innovation and strong per- biomedical discovery flourishes
search and teaching. formance on quality and safety as we invest in care delivery will
These changes in clinical pro- metrics. Each AMC has invested require vigilance.
cess require additional investment in the infrastructure required for AMCs’ complex organizational
in information systems and ana- its physicians to meet the inter- structures and historical focus
lytic resources. To ensure consis- nal incentive goals. on tertiary inpatient care may ap-
tent clinical communication and Although we have only 18 pear incongruent with success in
assess our progress in popula- months of experience with risk- contracts requiring commitment
tion health management, we’re based contracts, our approach is to change and reduced use of hos-
consolidating our clinical and ad- showing promise. Our cost trends pital services. Charting our course
ministrative systems onto a sin- have been lower than local and under the current economic pres-
gle electronic platform. This new national comparison benchmarks,4 sures won’t be easy. But our AMCs
infrastructure requires investment, suggesting that even at the cur- have built their reputations by ad-
which is not provided by the risk- rent historically low rates of cost dressing society’s most pressing
based contracts, and success in escalation, our efforts are paying health care challenges, and today’s
these contracts means lower clini- off. Nonetheless, challenges and central challenge is the rising cost
n engl j med 369;11 nejm.org september 12, 2013 995
The New England Journal of Medicine
Downloaded from nejm.org on November 20, 2015. For personal use only. No other uses without permission.
Copyright © 2013 Massachusetts Medical Society. All rights reserved.
PERSPE C T I V E balancing amc s ’ missions and health care costs
of health care. Fortunately, AMCs From Brigham and Women’s Hospital Massachusetts. Health Aff (Millwood) 2003;
(E.G.N.), Massachusetts General Hospital 22:130-41.
specialize in innovation. We must (T.G.F., P.L.S.), and Partners HealthCare 3. Milford CE, Ferris TG. A modified “Gold-
now apply that capability not just (E.G.N., T.G.F., P.L.S.) — all in Boston. en Rule” for health care organizations. Mayo
to scientific aspects of medical Clin Proc 2012;87:717-20.
1. Schoen C, Lippa J, Collins S, Radley DC. 4. Partners HealthCare slows cost growth,
care but also to the systems de- improves quality. Press release of partners
State trends in premiums and deductibles,
livering it. 2003-2011: eroding protection and rising HealthCare, July 16, 2013 (http://www
costs underscore need for action. Issue Brief .partners.org/About/Media-center/articles/
Disclosure forms provided by the authors (Commonw Fund) 2012;31:1-39. pioneer-aco-year-1-results.aspx).
are available with the full text of this article 2. Mechanic RE. What will become of the DOI: 10.1056/NEJMp1309179
at NEJM.org. medical mecca? Health care spending in Copyright © 2013 Massachusetts Medical Society.
BECOMING A PHYSICIAN
Signal in the Noise
Raphael P. Rush, M.D.
T he first time I heard an IV
pump beeping was my first
time in the hospital as a medical
The now-gentle tones of IVs pro-
vided the root chords of a melody
made of the cadences of snoring
families had left and the lights
were turned low, patients and
house staff alike would be left
student. Sent to examine a loud, patients and the trills of ringing alone with their to-do lists and
cantankerous patient, I became phones. their thoughts.
concerned when his IV pump be- Certain songs, with their dis- Silence evoked an urge to fill
gan frantically shrieking. After 30 tinctive instruments, repeated it, and it was in those rest beats
seconds of panic and uncertainty, themselves. The beep of a heart that I often found myself cross-
I pulled a resident out of the hall monitor, accompanied by the hiss ing the threshold of a patient’s
into the patient’s room, where, in of mechanical ventilation, provid- room to stop, to sit, to examine
a maneuver that shocked me then ed a backbeat for the trance mu- again, to catch what I had missed
but has since become part of my sic of the ICU. Alarms and suc- during the day. Night was the
repertoire, she promptly hit the tion and overhead pages backed time to notice and address the
“Silence Alarm” button and con- up the lead vocals and heavy- softest sounds: a subtle valvulop-
tinued with her own work. metal stylings of the Code Blue athy, fine crackles, quiet weeping
Hospitals are noisy places, an team leader. behind a curtain after a patient
assault on the ears. As a new At night, after the lullaby of had received difficult news. It
visitor, I was greeted by an array the overhead announcement ush- was a chance to talk with my pa-
of beeps, whistles, and shouts ered visitors out of the hospital, tients, hear the lyrics of their
histories again, chat about the
news, or do crosswords with them
Now, I was expected to pronounce as I looked over their shoulders.
someone dead for the first time. I began rounding a second time
each day, after dark, the quiet
night music serving as my own
made by people and machines, after the formal and choreo- lullaby before I returned to loud
each with a distinct agenda, every graphed day teams gave way to work in the emergency room or
one of them desperate for atten- the improvised jazz of the night- evanescent refuge in the stillness
tion. The impression was of an time residents, the wards would of the call room.
unholy, disorganized din. go dark and silence would fall. One night, early in my resi-
Yet cacophony gave way, over Not in the grungy emergency de- dency, I was listening to the pat-
time, to music. The soft dings partment, which would be loud- ter of rain against the call-room
of arriving elevators mixed with er, busier, and more frantic, but window and sipping midnight
chatter at the nursing station. on the wards, where once the coffee when my pager went off.
996 n engl j med 369;11 nejm.org september 12, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 20, 2015. For personal use only. No other uses without permission.
Copyright © 2013 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Cabin Crew ManualDocument626 pagesCabin Crew ManualBilly Eres93% (29)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivation Statement Talent Scouting UI Revised 1Document2 pagesMotivation Statement Talent Scouting UI Revised 1Dennis Pranata100% (2)
- Hamlet Act 2 2 Part 5Document2 pagesHamlet Act 2 2 Part 5api-240934338No ratings yet
- SM7 Ch05 DistributionDocument36 pagesSM7 Ch05 DistributionMayank SharmaNo ratings yet
- LABREL 6th WEEKDocument54 pagesLABREL 6th WEEKSometimes goodNo ratings yet
- Dilation - FormalDocument14 pagesDilation - Formalapi-355095027No ratings yet
- Mehndi Zaveri (For Debo)Document2 pagesMehndi Zaveri (For Debo)vipin HNo ratings yet
- Succession Planning Case Study: © The Talent Company Ltd. 2013Document1 pageSuccession Planning Case Study: © The Talent Company Ltd. 2013Rekha SainiNo ratings yet
- Design and Fabrication of Rocker Bogie Mechanism Geosurvey RoverDocument7 pagesDesign and Fabrication of Rocker Bogie Mechanism Geosurvey RovershivaNo ratings yet
- Crossing Functional LinesDocument7 pagesCrossing Functional LinesmanmeetassignmentNo ratings yet
- 05 Barriers To Communication UNIT 4Document15 pages05 Barriers To Communication UNIT 4Arun PrasadNo ratings yet
- CSTP 2 Bermudez 1210Document9 pagesCSTP 2 Bermudez 1210Brenda BermudezNo ratings yet
- Investigation and Prosecution)Document8 pagesInvestigation and Prosecution)Baishnavi ShahNo ratings yet
- Human Resource Management Performance Evaluation ProcessDocument3 pagesHuman Resource Management Performance Evaluation ProcessJohn Michael MejillanoNo ratings yet
- Sustainable-Responsible Tourism Discourse - Towards Responsustable' TourismDocument11 pagesSustainable-Responsible Tourism Discourse - Towards Responsustable' TourismamalNo ratings yet
- Intro To Marketing Primer 158Document158 pagesIntro To Marketing Primer 158fchavarria7No ratings yet
- Rup Vs ScrumDocument9 pagesRup Vs ScrumMehdi AmiriNo ratings yet
- Certification of ComplianceDocument1 pageCertification of ComplianceSanFabian Pangasinan Bfp RegionOneNo ratings yet
- Writing Task 1Document34 pagesWriting Task 1Nguyên BảoNo ratings yet
- Huntingfield Pony & Riding Club Inc PreDocument4 pagesHuntingfield Pony & Riding Club Inc Preapi-26187582No ratings yet
- Versant English Placement Test Practice Materials: 1. Predicting ContentDocument18 pagesVersant English Placement Test Practice Materials: 1. Predicting ContentMelike Erdem100% (1)
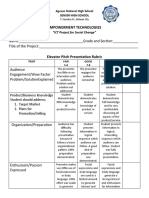
- Elevator Pitch Rubrics (ICT For Social Chnage)Document2 pagesElevator Pitch Rubrics (ICT For Social Chnage)Dran OteroNo ratings yet
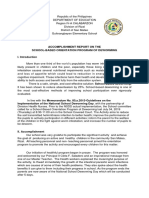
- Accomplishment Report of DEWORMING ORIENTATIONDocument3 pagesAccomplishment Report of DEWORMING ORIENTATIONGeraldin Joy Dela Cruz100% (1)
- Energy Modelling Guidelines (British Columbia) PDFDocument42 pagesEnergy Modelling Guidelines (British Columbia) PDFSchreiber_DiesesNo ratings yet
- Sales and Distribution Management: Mba II Year I SemesterDocument35 pagesSales and Distribution Management: Mba II Year I SemesterY ARUN KUMARNo ratings yet
- ME-6703-Computer Integrated Manufacturing: Unit-IDocument8 pagesME-6703-Computer Integrated Manufacturing: Unit-IJayakrishnaNo ratings yet
- Salmorin Daniel Emmanuel Venturanza, Aklan State UniversityDocument5 pagesSalmorin Daniel Emmanuel Venturanza, Aklan State UniversityRenwen LataNo ratings yet
- Cover PageDocument9 pagesCover PageFania Brace AnnNo ratings yet
- 12 WI FormworkDocument9 pages12 WI FormworkSafdar AliNo ratings yet
- Carter Case 1: Q. Make A List of Five Specific HR Problems You Think Carter Cleaning Will Have To Grapple WithDocument2 pagesCarter Case 1: Q. Make A List of Five Specific HR Problems You Think Carter Cleaning Will Have To Grapple WithNitesh Mehla100% (1)