Professional Documents
Culture Documents
GC - Management of COVID-19 Respiratory Distress
GC - Management of COVID-19 Respiratory Distress
Uploaded by
Alfredo Melo RamosCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GC - Management of COVID-19 Respiratory Distress
GC - Management of COVID-19 Respiratory Distress
Uploaded by
Alfredo Melo RamosCopyright:
Available Formats
Clinical Review & Education
JAMA Insights | CLINICAL UPDATE
Management of COVID-19 Respiratory Distress
John J. Marini, MD; Luciano Gattinoni, MD
Acute respiratory distress syndrome (ARDS) can originate tance (low compliance), higher lung weight, and high PEEP
from either the gas or vascular side of the alveolus. Although the por- response. Clearly, types L and H are the conceptual extremes of a
tal for coronavirus disease 2019 (COVID-19) is inhalational, and al- spectrum that includes intermediate stages, in which their charac-
veolar infiltrates are commonly found on chest x-ray or computed teristics may overlap. Another feature consistently reported is a
tomography (CT) scan, the re- highly activated coagulation cascade, with widespread micro- and
spiratory distress appears to in- macro-thromboses in the lung and in other organs (eFigure 1 in the
Author Audio Interview
clude an important vascular in- Supplement); very elevated serum D-dimer levels are a consistent
sult that potentially mandates a finding associated with adverse outcomes.7
Supplemental content different treatment approach These observations indicate the fundamental roles played by
than customarily applied for disproportionate endothelial damage that disrupts pulmonary va-
ARDS. Indeed, the wide variation in mortality rates across different soregulation, promotes ventilation-perfusion mismatch (the pri-
intensive care units raises the possibility that the approach to ven- mary cause of initial hypoxemia), and fosters thrombogenesis. In ad-
tilatory management could be contributing to outcome.1-3 dition, remarkably increased respiratory drive may, if unchecked,
COVID-19 is a systemic disease that primarily injures the vascu- intensify tidal strains and energy loads from a patient’s respiratory
lar endothelium. If not expertly and individually managed with con- effort applied to highly vulnerable tissue, adding P-SILI to the mix
sideration of the vasocentric features, a COVID-19 patient with ARDS of the lung’s inflammatory assault.5,8 When confronting such an un-
(“CARDS”) may eventually develop multiorgan failure, even when familiar and rapidly evolving environment, only certain aspects of
not of advanced age or predisposed by preexisting comorbidity. well-accepted lung-protective approaches to ARDS remain ratio-
nal at these different stages. More important, inattention to the vas-
Standard Approaches to Ventilating ARDS cular side (eg, avoidance of fluid overload, reduction of cardiac out-
Normally, ARDS is characterized by noncardiogenic pulmonary put demands) could inadvertently promote counterproductive
edema, shunt-related hypoxemia, and reduced aerated lung size responses (eg, edema) and iatrogenic damage.
(“baby lung”), which accounts for low respiratory compliance.4 In
such settings, increasing lung size by recruiting previously col- Protecting the CARDS Lung
lapsed lung units is often achieved through the use of high levels of Patients with type L CARDS, having good lung compliance, accept
positive end-expiratory pressure (PEEP), recruiting maneuvers, larger tidal volumes (7-8 mL/kg ideal body weight) than those cus-
and prone positioning. Because high transpulmonary pressure tomarily prescribed for ARDS without worsening the risk of VILI.
induces stress across the lung that is poorly tolerated in ARDS, rela- Actually, in a 70-kg man, with respiratory system compliance of
tively low tidal volumes, together with tolerance for modest 50 mL/cm H2O and PEEP of 10 cm H2O, a tidal volume of 8 mL/kg
(permissive) hypercapnia, facilitate the goal of minimizing yields a plateau pressure of 21 cm H2O and driving pressure of 11 cm
ventilator-induced lung injury (VILI). Indeed, in the early phases of H2O, both well below the currently accepted thresholds for VILI
ARDS, before a patient has fatigued or been sedated, the high protection (30 and 15 cm H2O, respectively). Higher VT could help
transpulmonary pressures associated with spontaneous vigorous avoid reabsorption atelectasis and hypercapnia due to hypoventila-
inspiratory effort may contribute to damage (so-called patient self- tion with lower tidal volumes.
induced lung injury [P-SILI]).5 The key issue in this early stage is disrupted vasoregulation,
where the pulmonary vasoconstriction that normally occurs in
Clinical Features of CARDS response to hypoxia fails to occur because of an endothelial
Soon after onset of respiratory distress from COVID, patients ini- assault that mismatches perfusion to ventilation and may result in
tially retain relatively good compliance despite very poor profound hypoxemia. The clinician’s first response, boosting FIO2,
oxygenation.1,2 Minute ventilation is characteristically high. Infil- may indeed prove effective early on. If insufficient, noninvasive
trates are often limited in extent and, initially, are usually character- support (eg, high-flow nasal O2, CPAP, Bi-PAP) may stabilize the
ized by a ground-glass pattern on CT that signifies interstitial rather clinical course in mild cases, provided that the patient does not
than alveolar edema. Many patients do not appear overtly dys- exert excessive inspiratory efforts. However, if respiratory drive is
pneic. These patients can be assigned, in a simplified model, to not reduced by oxygen administration and noninvasive support,
“type L,” characterized by low lung elastance (high compliance), persistently strong spontaneous inspiratory efforts simultane-
lower lung weight as estimated by CT scan, and low response to ously increase tissue stresses and raise pulmonary transvascular
PEEP.6 For many patients, the disease may stabilize at this stage pressures, vascular flows, and fluid leakage (ie, P-SILI).8-10 Pro-
without deterioration while others, either because of disease sever- gressive deterioration of lung function (a VILI vortex) may then
ity and host response or suboptimal management, may transition rapidly ensue. Early intubation, effective sedation, and/or paraly-
to a clinical picture more characteristic of typical ARDS. These can sis may interrupt this cycle. Targeting lower PEEP (8-10 cm H2O)
be defined as “type H,” with extensive CT consolidations, high elas- is appropriate. Raising mean transpulmonary pressures by higher
jama.com (Reprinted) JAMA Published online April 24, 2020 E1
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 04/24/2020
Clinical Review & Education JAMA Insights
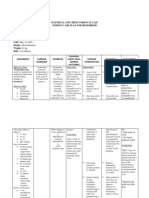
Table. Time Course and Treatment Approach to Ventilation Support for Patients With CARDS
Time
period Objective Respiratory support options Rationale
Before Adequate gas exchange Supplemental oxygen, Powerful respiratory effort can cause
intubation Avoid P-SILI CPAP, NIV, HFNC reinforcing lung and vascular stress,
Awake prone positioning, resulting in injury
Target nonvigorous breathing
During Avoid pulmonary Minimize PEEP, frequency Minimize transpulmonary Abbreviations: ARDS, acute
mechanical deterioration and VILI and tidal volume and vascular stresses respiratory distress syndrome;
ventilation vortex Adjust to acceptable gas exchange CARDS, COVID-19 with ARDS;
Maintain fluid balance CPAP, continuous positive airway
Reduce O2 demand pressure; ECMO, extracorporeal
Consider ECMO
membrane oxygenation;
After Minimize pulmonary Type La: use lower PEEP Lower tidal volumes are unnecessary HFNC, high-flow nasal cannula;
intubation stress (<10 cm H2O) Higher PEEP is ineffective, creates
Optimize O2 Use more liberal tidal volume dead space, and adversely redirects NIV, noninvasive ventilation;
Avoid VILI vortex (7-9 mL/kg) as needed blood flow P-SILI, patient self-inflicted lung
Reduce O2 demand injury; PEEP, positive end-expiratory
Consider prone positioning pressure; VILI, ventilator-induced
Reduce and evenly Type Ha: use higher PEEP More closely behaves and responds lung injury.
distribute lung and (<15 cm H2O) like typical ARDS a
Type L: Scattered ground-glass
vascular stresses Lower tidal volume (5-7 mL/kg)
Optimize O2 Reduce O2 demand infiltrates, higher compliance
Avoid VILI vortex Implement prone positioning (>50 mL/cm H2O), not PEEP
Weaning Avoid reversion to Make transitions cautiously Strong spontaneous efforts raise O2 responsive; less dyspnea.
phase previously worsened Avoid abrupt changes demand, increase edema, Type H: Extensive infiltrates of
pulmonary state by Spontaneous trials only at the very and promote P-SILI atelectasis and edema, lower
causing VILI and end of the weaning process compliance, PEEP responsive,
worsening edema
overtly dyspneic.
PEEP or inspiratory-expiratory ratio inversion redirects blood flow vessels that perfuse it9,10 (eFigure 2 in the Supplement). Over time,
away from overstretched open airspaces, accentuating stresses superimposed VILI and unchecked viral disease incite inflammation
on highly permeable microvessels and compromising CO 2 and edema, promoting local and generalized thrombogenesis,
exchange without the benefit of widespread recruitment of func- intense cytokine release, right ventricular overload, and systemic
tional lung units. organ dysfunction. In this advanced state, it is advisable to apply a
If lung edema increases in the type L patient, either because of more conventional lung-protective strategy: higher PEEP (ⱕ15 cm
the disease itself and/or P-SILI, the baby lung shrinks further, and H2O), lower tidal volume (6 mL/kg), and prone positioning while
the type H phenotype progressively develops. Concentrating the en- minimizing oxygen consumption. Whichever the disease type,
tire ventilation workload on an already overtaxed baby lung in- weaning should be undertaken cautiously (Table).
creases its power exposure and blood flow, thereby accentuating COVID-19 causes unique lung injury. It may be helpful to
its potential for progressive injury. categorize patients as having either type L or H phenotype. Differ-
There are 2 major contributors to this VILI vortex of shrinking ent ventilatory approaches are needed, depending on the underly-
the baby lung: airspace VILI8 and intensified stresses within the ing physiology.
ARTICLE INFORMATION REFERENCES 2017;195(4):438-442. doi:10.1164/rccm.201605-
Author Affiliations: Regions Hospital, University of 1. Grasselli G, Zangrillo A, Zanella A, et al; COVID-19 1081CP
Minnesota, Minneapolis/St Paul (Marini); Lombardy ICU Network. Baseline characteristics 6. Gattinoni L, Chiumello D, Caironi P, et al.
Department of Anesthesiology, Intensive Care and and outcomes of 1591 patients infected with COVID-19 pneumonia: different respiratory
Emergency Medicine, Medical University of SARS-CoV-2 admitted to ICUs of the Lombardy treatments for different phenotypes? Intensive Care
Göttingen, Göttingen, Germany (Gattinoni). region, Italy. JAMA. 2020. Published online April 6, Med. 2020. doi:10.1007/s00134-020-06033-2
Corresponding Author: John J. Marini, MD, 2020. doi:10.1001/jama.2020.5394 7. Zhou F, Yu T, Du R, et al. Clinical course and risk
Regions Hospital, University of Minnesota, 2. Arentz M, Yim E, Klaff L, et al. Characteristics factors for mortality of adult inpatients with
640 Jackson St, MS11203B, St Paul, MN 55101 and outcomes of 21 critically ill patients with COVID-19 in Wuhan, China: a retrospective cohort
(marin002@umn.edu). COVID-19 in Washington State. JAMA. 2020. study. Lancet. 2020;395(10229):1054-1062. doi:
Published Online: April 24, 2020. Published online March 19, 2020. doi:10.1001/jama. 10.1016/S0140-6736(20)30566-3
doi:10.1001/jama.2020.6825 2020.4326 8. Marini JJ, Rocco PRM, Gattinoni L. Static and
Conflict of Interest Disclosures: Dr Gattinoni 3. Wang D, Hu B, Hu C, et al. Clinical characteristics dynamic contributors to ventilator-induced lung
reported receiving fees from General Electric for of 138 hospitalized patients with 2019 novel injury in clinical practice. pressure, energy, and
ventilator development and seminars; a grant from coronavirus-infected pneumonia in Wuhan, China. power. Am J Respir Crit Care Med. 2020;201(7):767-
Estor for technical equipment and to perform JAMA. 2020;323(11):1061-1069. doi:10.1001/jama. 774. doi:10.1164/rccm.201908-1545CI
a study; fees from Masimo for technical 2020.1585 9. Vieillard-Baron A, Matthay M, Teboul JL, et al.
consultation and Nutrivent; and a patent 4. Gattinoni L, Marini JJ, Pesenti A, Quintel M, Experts’ opinion on management of hemodynamics
licensed to Sidam Biomedical Solutions for Mancebo J, Brochard L. The “baby lung” became an in ARDS patients: focus on the effects of
development of an esophageal balloon for the adult. Intensive Care Med. 2016;42(5):663-673. doi: mechanical ventilation. Intensive Care Med. 2016;
measurement of esophageal pressure together 10.1007/s00134-015-4200-8 42(5):739-749. doi:10.1007/s00134-016-4326-3
with enteral feeding. 5. Brochard L, Slutsky A, Pesenti A. Mechanical 10. Marini JJ, Hotchkiss JR, Broccard AF.
ventilation to minimize progression of lung injury in Bench-to-bedside review: microvascular and
acute respiratory failure. Am J Respir Crit Care Med. airspace linkage in ventilator-induced lung injury.
Crit Care. 2003;7(6):435-444. doi:10.1186/cc2392
E2 JAMA Published online April 24, 2020 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 04/24/2020
You might also like
- RS ARI-Common Cold - PPT 93Document57 pagesRS ARI-Common Cold - PPT 93Dr.P.NatarajanNo ratings yet
- ArdsDocument53 pagesArdsSophy Sony100% (3)
- FON241 Essay QuestionsDocument3 pagesFON241 Essay Questionsatarisgurl080% (1)
- Ccmanejoventilador y TerapiaadjuntaDocument11 pagesCcmanejoventilador y TerapiaadjuntaARELHI ROSARIO GARCIA MONROYNo ratings yet
- ARDSDocument55 pagesARDSSandhya HarbolaNo ratings yet
- Dr. Rajmani: Assistant Professor Department of Medicine J.L.N. Medical College, Ajmer (Raj.)Document63 pagesDr. Rajmani: Assistant Professor Department of Medicine J.L.N. Medical College, Ajmer (Raj.)Ashish SoniNo ratings yet
- Symposium Papers: What Is The Acute Respiratory Distress Syndrome?Document7 pagesSymposium Papers: What Is The Acute Respiratory Distress Syndrome?Zulkifli SalimNo ratings yet
- Acute Respiratory Distress Syndrome: STUDENT: Wajih Gara. GROUP: 1434Document17 pagesAcute Respiratory Distress Syndrome: STUDENT: Wajih Gara. GROUP: 1434Anastasia CebotariNo ratings yet
- Acute Respiratory Distress SyndromeDocument18 pagesAcute Respiratory Distress SyndromeFasiha SamiNo ratings yet
- Fisiopatologia de SDRADocument19 pagesFisiopatologia de SDRARuben HerediaNo ratings yet
- Hypoxemic Resp. FailureDocument52 pagesHypoxemic Resp. FailureLovely Acabado TampocoNo ratings yet
- Ards 2Document7 pagesArds 2LUCIBELLOT1No ratings yet
- Acute Respiratory Distress Syndrome, Mechanical Ventilation, and Inhalation Injury in Burn PatientsDocument13 pagesAcute Respiratory Distress Syndrome, Mechanical Ventilation, and Inhalation Injury in Burn Patientspatriciarreis2991No ratings yet
- Acute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyDocument5 pagesAcute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyARHNo ratings yet
- Pathophysiologyofacute Respiratorydistress Syndromeandcovid-19Lung InjuryDocument28 pagesPathophysiologyofacute Respiratorydistress Syndromeandcovid-19Lung InjuryLuis HernándezNo ratings yet
- Acute Respiratory Distress SyndromeDocument17 pagesAcute Respiratory Distress SyndromeSanjeet Sah100% (1)
- Integrating The Evidence: Confronting The COVID-19 Elephant: EditorialDocument4 pagesIntegrating The Evidence: Confronting The COVID-19 Elephant: EditorialJose Luis Espino MacielNo ratings yet
- ARDS EngDocument25 pagesARDS EngTofik ShehajNo ratings yet
- Acp - ArdsDocument12 pagesAcp - Ardsapi-3765169No ratings yet
- Part I: IntroductionDocument4 pagesPart I: IntroductionChezka PalolaNo ratings yet
- Acute Respiratory Distress SyndromeDocument10 pagesAcute Respiratory Distress SyndromeMuhammad NurmanNo ratings yet
- Ards Sdra Sira 2022Document14 pagesArds Sdra Sira 2022Alberto Torres OrtaNo ratings yet
- Adult Respiratory Distress SyndromeDocument5 pagesAdult Respiratory Distress SyndromeMeh AdroidNo ratings yet
- Pi Is 0749070421000415Document28 pagesPi Is 0749070421000415Vlady78No ratings yet
- ICU Department ICU DepartmentDocument48 pagesICU Department ICU DepartmentEmad ElhusseinNo ratings yet
- Acute Respiratory Distress SyndromeDocument21 pagesAcute Respiratory Distress Syndromemisseve252100% (1)
- Manajemen VentiDocument2 pagesManajemen VentiBos AseNo ratings yet
- Paediatric Respiratory Reviews: F. Healy, B.D. Hanna, R. ZinmanDocument6 pagesPaediatric Respiratory Reviews: F. Healy, B.D. Hanna, R. ZinmanfadmayulianiNo ratings yet
- ArdsDocument69 pagesArdsdrabdallakawareNo ratings yet
- Acute Respiratory Distress Syndrome: Jesse B. Hall, MD, FCCPDocument12 pagesAcute Respiratory Distress Syndrome: Jesse B. Hall, MD, FCCPMayun CacoellNo ratings yet
- Initiationofmechanical Ventilationinpatients Withdecompensatedrespiratory FailureDocument14 pagesInitiationofmechanical Ventilationinpatients Withdecompensatedrespiratory FailureCarolina Polo TorresNo ratings yet
- Vieillard-Baron Et Al-2023-Intensive Care MedicineDocument3 pagesVieillard-Baron Et Al-2023-Intensive Care Medicineandres ruizNo ratings yet
- Pulmonary Hemorrhage-1Document20 pagesPulmonary Hemorrhage-1ELDHOSE RAJUNo ratings yet
- Ards Thyrotoxicosis Hypothyroidism.Document14 pagesArds Thyrotoxicosis Hypothyroidism.k sanchezNo ratings yet
- 1 s2.0 S003139551730072XDocument21 pages1 s2.0 S003139551730072XvgmanjunathNo ratings yet
- Ventilation Management in Acute Respiratory Failure Related To COVID-19 Versus ARDS From Another Origin - A Descriptive Narrative ReviewDocument11 pagesVentilation Management in Acute Respiratory Failure Related To COVID-19 Versus ARDS From Another Origin - A Descriptive Narrative ReviewntnquynhproNo ratings yet
- Pi Is 0749070421000439Document21 pagesPi Is 0749070421000439Vlady78No ratings yet
- High-Flow, Noninvasive Ventilation and Awake (Nonintubation) Proning in Patients With Coronavirus Disease 2019 With Respiratory FailureDocument11 pagesHigh-Flow, Noninvasive Ventilation and Awake (Nonintubation) Proning in Patients With Coronavirus Disease 2019 With Respiratory FailureCamila Fernanda Rivera ArayaNo ratings yet
- 20 - ARDS Unidad 2 Seccion 4Document8 pages20 - ARDS Unidad 2 Seccion 4Docencia SVHILNo ratings yet
- COVID-19 Pneumonia ARDS or NotDocument3 pagesCOVID-19 Pneumonia ARDS or NotHydr OrtgaNo ratings yet
- Acute Respiratory Distress Syndrome in Near DrowningDocument30 pagesAcute Respiratory Distress Syndrome in Near DrowningJane SharpsNo ratings yet
- Ventilatory Strategies in Obstructive Lung. Parrilla2014Document10 pagesVentilatory Strategies in Obstructive Lung. Parrilla2014EzeBorjesNo ratings yet
- Management of Patients With Acute Respiratory Distress SyndromeDocument41 pagesManagement of Patients With Acute Respiratory Distress Syndrome8515944No ratings yet
- Ventilation During Lung Resection and Critical Care ComparativeDocument11 pagesVentilation During Lung Resection and Critical Care Comparativeema moralesNo ratings yet
- Editorials: Basing Respiratory Management of COVID-19 On Physiological PrinciplesDocument2 pagesEditorials: Basing Respiratory Management of COVID-19 On Physiological PrinciplesnoviaNo ratings yet
- Adult Respiratory Distress Syndrome: ReviewDocument5 pagesAdult Respiratory Distress Syndrome: ReviewJuliana Rodriguez MariñoNo ratings yet
- Thorax 1Document9 pagesThorax 1Ferry Ferdiansyah HidayatNo ratings yet
- Sdra Reconocimiento Actual 2021Document16 pagesSdra Reconocimiento Actual 2021NATHALY JOVANA CONTRERAS HERRERANo ratings yet
- Jacobs 2015Document6 pagesJacobs 2015rani tiaraNo ratings yet
- ARDSDocument23 pagesARDSDumora FatmaNo ratings yet
- From: Management of COVID-19 Respiratory DistressDocument1 pageFrom: Management of COVID-19 Respiratory DistresshaqiNo ratings yet
- Guidance Document SARS COVID19Document10 pagesGuidance Document SARS COVID19Sebastián CrippaNo ratings yet
- Acute Respiratory FailureDocument11 pagesAcute Respiratory FailureRicardoOswaldoValdiviesoValdiviesoNo ratings yet
- Evolvingepidemiology Anddefinitionsofthe Acuterespiratorydistress Syndromeandearlyacute LunginjuryDocument16 pagesEvolvingepidemiology Anddefinitionsofthe Acuterespiratorydistress Syndromeandearlyacute LunginjuryVijay KumarNo ratings yet
- Murray 1988Document4 pagesMurray 1988mesacarvajalinoNo ratings yet
- AvMed Pneumothorax JRNMSDocument4 pagesAvMed Pneumothorax JRNMShkw8g5snyxNo ratings yet
- Close Lung 2018Document8 pagesClose Lung 2018Sergio CastellanosNo ratings yet
- Chronicobstructivepulmonary Disease:: Clinical Integrative PhysiologyDocument19 pagesChronicobstructivepulmonary Disease:: Clinical Integrative PhysiologyZaina TNo ratings yet
- Respiratory Path PathophysiologyDocument25 pagesRespiratory Path Pathophysiologyaiadalkhalidi100% (1)
- Pulmonary Edema: René P. Michel, Peter GoldbergDocument34 pagesPulmonary Edema: René P. Michel, Peter GoldbergNadya NovianiNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Uraian Kegiatan Pegawai Puskesmas Kajoran 1 Juli 2021Document10 pagesUraian Kegiatan Pegawai Puskesmas Kajoran 1 Juli 2021restuNo ratings yet
- Stroke/Cerebrovascular Accident: Transient Ischemic AttacksDocument5 pagesStroke/Cerebrovascular Accident: Transient Ischemic AttacksCraigNo ratings yet
- MAPEH Health 10 Q3 Episode 4 SLMDocument5 pagesMAPEH Health 10 Q3 Episode 4 SLMCris Ann PausanosNo ratings yet
- 10-Effect of Chest Physical Therapy On Pediatrics Hospitalized With Pneumonia PDFDocument8 pages10-Effect of Chest Physical Therapy On Pediatrics Hospitalized With Pneumonia PDFandina100% (1)
- Quality Assurance and Quality Management ConceptDocument8 pagesQuality Assurance and Quality Management ConceptVikas PatreyNo ratings yet
- Integrative Veterinary Medicine (VetBooks - Ir)Document283 pagesIntegrative Veterinary Medicine (VetBooks - Ir)Letícia de Oliveira Sousa100% (1)
- Hic Nsi HepsyDocument59 pagesHic Nsi HepsyNursing Superintendent (SH)No ratings yet
- Curriculum in NursingDocument53 pagesCurriculum in NursingsakshiwiproNo ratings yet
- History Taking Compilation 1Document31 pagesHistory Taking Compilation 1Kabir SiddiquiNo ratings yet
- Iapt 3 Year ReportDocument48 pagesIapt 3 Year Reporttony_jameson-allenNo ratings yet
- Conducta SuicidaDocument371 pagesConducta SuicidaOrlando FuentealbaNo ratings yet
- Resume Abigail RodriguezDocument2 pagesResume Abigail Rodriguezapi-520026903No ratings yet
- Aerb Is-4Document52 pagesAerb Is-4thriller456No ratings yet
- HemodialysisDocument244 pagesHemodialysisKrsrinivasa RajuNo ratings yet
- 23 134 1 PB PDFDocument10 pages23 134 1 PB PDFAriefchsNo ratings yet
- FeverDocument21 pagesFeverTele NursingNo ratings yet
- Nursing Care Plan For HemorrhoidsDocument3 pagesNursing Care Plan For HemorrhoidsFaith Marfil100% (2)
- Evaluación de La Deglución Con NasofibroscopíaDocument7 pagesEvaluación de La Deglución Con NasofibroscopíaLoreto Opazo RojasNo ratings yet
- Form Pru OverseasDocument3 pagesForm Pru OverseasGeorgius AndreNo ratings yet
- Mental Health Studyguide Part 1Document39 pagesMental Health Studyguide Part 1Ngoc TB VoNo ratings yet
- Adherence To Antipsychotics in Schizophrenia PDFDocument168 pagesAdherence To Antipsychotics in Schizophrenia PDFCosmin Ungureanu100% (1)
- APA Formatted Reference ListDocument2 pagesAPA Formatted Reference ListLiz DuncanNo ratings yet
- Economic Evaluation in Health Care,,,,,Methods - Handout.Document8 pagesEconomic Evaluation in Health Care,,,,,Methods - Handout.Wenwa TracyNo ratings yet
- Pharmaceutical Formulation: Principles and Dosage FormsDocument3 pagesPharmaceutical Formulation: Principles and Dosage FormsPharmacistBDNo ratings yet
- Pengaruh Pemberian Token Ekonomi Terhadap Kepatuhan Minum Obat Pada Klien Skizofrenia Di Ruang Kunti Rumah Sakit Jiwa Provinsi BaliDocument11 pagesPengaruh Pemberian Token Ekonomi Terhadap Kepatuhan Minum Obat Pada Klien Skizofrenia Di Ruang Kunti Rumah Sakit Jiwa Provinsi BaliElly UlfaNo ratings yet
- PROFESSIONAL Org-My SeminarDocument31 pagesPROFESSIONAL Org-My SeminarmariaNo ratings yet
- Exploring The Nexus Between Medical Geography and Covid-19 Control in NigeriaDocument16 pagesExploring The Nexus Between Medical Geography and Covid-19 Control in NigeriaHabib IbrahimNo ratings yet
- Diabetes Healthy Feet and Your Patients Feb2014Document2 pagesDiabetes Healthy Feet and Your Patients Feb2014Jianhua ShiNo ratings yet