Professional Documents
Culture Documents
Surg - Closed Head Injuries PDF
Surg - Closed Head Injuries PDF
Uploaded by
Marianne R. LorenzoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surg - Closed Head Injuries PDF
Surg - Closed Head Injuries PDF
Uploaded by
Marianne R. LorenzoCopyright:
Available Formats
SURGERY April 2020
CLOSED HEAD INJURY Natakneng 2020
Revalida Reviewer Mariano Marcos State University
Outline MEDICAL MANAGEMENT
Introduction Patients with a documented CHI and evidence of intracranial hemorrhage or a
Initial Assessment depressed skull fracture should receive a 17-mg/kg phenytoin loading dose,
Medical Management followed by 1 week of therapeutic maintenance phenytoin, typically 300 to 400
mg/d.
Classification
Phenytoin prophylaxis has been shown to decrease the incidence of early
Types posttraumatic seizures. There is no evidence to support long-term use of
Concussion prophylactic antiepileptic agents.
Contusion Blood glucose levels should be closely monitored by free blood sugar checks
DIA and controlled with sliding scale insulin.
Traumatic Intracranial Hematoma Fevers also should be evaluated and controlled with antipyretics, as well as
Epidural Hematoma source-directed therapy when possible.
Acute Subdural Hematoma Hyperglycemia and hyperthermia are toxic to injured neurons and contribute to
Chronic Subdural Hematoma secondary injury.
Intraparenchymal Hemorrhage Head-injured patients have an increased prevalence of peptic ulceration and GI
bleeding.
Peptic ulcers occurring in patients with head injury or high ICP are referred to
as Cushing’s ulcers. Ulcer prophylaxis should be used.
There are two important factors that affect the outcome of CHI in general.
Compression stockings or athrombic pumps should be used when the patient
The initial impact causes the PRIMARY INJURY, defined as the immediate
cannot be mobilized rapidly for prophylaxis of deep venous thrombosis.
injury to neurons from transmission of the force of impact.
Subsequent neuronal damage due to the sequelae of trauma is referred to as
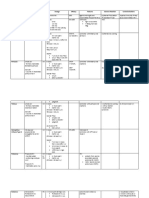
CLASSIFICATION
SECONDARY INJURY.
TBI can be classified as mild, moderate, or severe.
Hypoxia, hypotension, hydrocephalus, intracranial hypertension, thrombosis,
and intracranial hemorrhage may all be mechanisms of secondary injury. For patients with a history of head trauma, classification is as follows:
GCS
INITIAL ASSESSMENT 3-8 MILD
The first three elements of the ABCDs of resuscitation— airway, breathing, 9-12 MODERATE
and circulation—must be assessed and stabilized. 13-15 SEVERE
Hypoxia and hypotension are known to worsen outcome in TBI (due to
secondary injury), making cardiopulmonary stabilization critical. TBI patients who are asymptomatic, who have only headache, dizziness, or
Patients who cannot follow commands require intubation for airway protection scalp lacerations, and who did not lose consciousness, have a low risk for
and ventilator control. intracranial injury and may be discharged home without a head CT scan.
The fourth element, assessment of “D,” for disability, is undertaken next. Patients with a history of altered consciousness, amnesia, progressive
headache, skull or facial fracture, vomiting, or seizure have a moderate risk for
Motor activity, speech, and eye opening can be assessed in a few seconds
intracranial injury and should undergo a prompt head CT.
and a GCS score assigned.
If the CT is normal, and the neurologic examination has returned to baseline
(excluding amnesia of the event), then the patient can be discharged to the care
of a responsible adult, again with printed criteria for returning to the emergency
room. Otherwise the patient must be admitted for a 24-hour observation period.
Patients with depressed consciousness, focal neurologic deficits, penetrating
injury, depressed skull fracture, or changing neurologic examination have a high
risk for intracranial injury. These patients should undergo immediate head
CT and admission for observation or intervention as needed.
TYPES OF CHI
CONCUSSION
The following is an example of how a primary surveyor may efficiently assess defined as temporary neuronal dysfunction following non-penetrating head
disability and GCS: trauma.
Approach the patient and enter his or her field of view. Observe whether the The head CT is normal, and deficits resolve over minutes to hours.
patient is visually attentive. Clearly command: “Tell me your name.” Definitions vary;
Then ask the patient to lift up two fingers on each side sequentially, and some require transient loss of consciousness, while others include
wiggle the toes. patients with any alteration of mental status
A visually or verbally unresponsive patient should be assessed for response Memory difficulties, especially amnesia of the event, are very common
to peripheral stimuli such as nail-bed pressure, or deep central painful
Studies have shown that the brain remains in a hypermetabolic state for up to
stimulation, such as a firm, twisting pinch of the sensitive supraclavicular
a week after injury.
skin.
The brain is also much more susceptible to injury from even minor head trauma
Watch for eye opening and movement of the extremities, whether
in the first 1 to 2 weeks after concussion (second-impact syndrome)
purposeful or reflexive.
Assess the verbal response. The motor, verbal, and eye-opening scores CONTUSION
may be correctly assigned using this rapid examination.
An initial assessment of the probability of significant head injury can be bruise of the brain, and occurs when the force from trauma is sufficient to cause
made, assuming that pharmacologic and toxic elements have not obscured breakdown of small vessels and extravasation of blood into the brain
the examination. The contused areas appear bright on CT scan
The surveyor must also take note of any external signs of head injury, The frontal, occipital, and temporal poles are most often involved.
including bleeding from the scalp, nose, or ear, or deformation of the skull Contusions themselves rarely cause significant mass effect as they represent
or face. small amounts of blood in injured parenchyma rather than coherent blood clots.
Nani Schwartz, Sabiston 1 of 3
SURG 32: CLOSED HEAD INJURY
Edema may develop around a Prognosis after successful evacuation is better for EDH than subdural
contusion, causing mass effect. Contusions hematoma (SDH).
may enlarge or progress to frank hematoma,
particularly during the first 24 hours.
Contusions also may occur in brain
tissue opposite the site of impact (contre-
coup injury). These contusions result from
deceleration of the brain against the skull.
DIFFUSE AXONAL INJURY
caused by damage to axons throughout the brain, due to rotational acceleration
and then deceleration.
Axons may be completely disrupted and then retract, forming axon balls.
Small hemorrhages can be seen in more severe cases, especially on MRI.
Hemorrhage is classically seen in the corpus callosum and the dorsolateral
midbrain. ACUTE SUBDURAL HEMATOMA
result of an accumulation of blood between the arachnoid membrane and
the dura.
Acute SDH usually results from venous bleeding, typically from tearing of a
bridging vein running from the cerebral cortex to the dural sinuses.
Elderly and alcoholic patients are at higher risk for acute SDH formation after
head trauma due to brain atrophy.
On head CT scan, the clot is bright or mixed-
density, crescent- shaped (lunate), may have a
less distinct border, and does not cross the midline
due to the presence of the falx.
Most SDHs occur over the cerebral hemispheres,
but they may also occur between the hemispheres
or layer over the tentorium.
Open craniotomy for evacuation of acute SDH is
indicated for any of the following:
EPIDURAL HEMATOMA
thickness >1 cm,
EDH is the accumulation of blood between the skull and the dura. midline shift >5 mm,
EDH usually results from arterial disruption, especially of the middle meningeal or GCS drop by two or more points from the time of injury to
artery. hospitalization.
The dura is adherent to bone, and some pressure is required to dissect between
the two. Nonoperatively managed hematomas may stabilize and eventually reabsorb, or
evolve into chronic SDHs.
EDH has a classic, three-stage clinical presentation that is probably seen in only The prognosis for functional recovery is significantly worse for acute SDH than
20% of cases. EDH because it is associated with greater primary injury to brain parenchyma
The patient is initially unconscious from the concussive aspect of the head from high-energy impacts.
trauma.
The patient then awakens and has a “lucid interval,” while the hematoma
subclinically expands.
As the volume of the hematoma grows, the decompensated region of the
pressure-volume curve is reached, ICP increases, and the patient rapidly
becomes lethargic and herniates.
Uncal herniation from an EDH classically causes ipsilateral third nerve palsy
and contralateral hemiparesis.
On head CT the blood clot is bright, biconvex
in shape (lentiform), and has a well-defined
border that usually respects cranial suture
lines.
An EDH is typically found over the convexities
but may rarely occur in the posterior fossa as
well.
Open craniectomy for evacuation of the
congealed clot and hemostasis generally is indicated for EDH.
Patients who meet all of the following criteria may be managed conservatively:
clot volume <30 cm3,
maximum thickness <1.5 cm, and
GCS score >8
NANI Schwartz, Sabiston 2 of 3
SURG 32: CLOSED HEAD INJURY
CHRONIC SUBDURAL HEMATOMA
Chronic SDH is a collection of blood breakdown products that is at least 2 to 3
weeks old.
Acute hematomas are bright white (hyperdense) on CT scan for approximately
3 days, after which they fade to isodensity with brain, and then to hypodensity
after 2 to 3 weeks.
A true chronic SDH will be nearly as dark as CSF on CT.
Traces of white are often seen due to small, recurrent hemorrhages into the
collection. These small bleeds may expand the collection enough to make it
symptomatic (acute-on-chronic SDH)
Chronic SDHs often occur in patients without a clear history of head trauma, as
they may arise from minor head injury.
Alcoholics, the elderly, and patients on anticoagulation are at higher risk for
developing chronic SDH.
Patients may present with headache, seizure, confusion, contralateral
hemiparesis, or coma.
A chronic SDH >1 cm or any symptomatic SDH should be surgically drained.
Unlike acute SDH, which consists of a thick, congealed clot, chronic SDH
typically consists of a viscous fluid with the texture and dark brown color
reminiscent of motor oil.
A simple burr hole can effectively drain most chronic SDHs.
The procedure is converted to open craniotomy if the SDH is too congealed for
irrigation drainage, the complex of membranes prevents effective drainage, or
persistent hemorrhage occurs that cannot be reached with bipolar cautery
through the burr hole.
follow-up head CT scans are required postoperatively and approximately 1
month later to document resolution.
INTRAPARENCHYMAL HEMORRHAGE
most often associated with hypertensive hemorrhage or arteriovenous
malformations (AVMs).
Typically occurs in basal ganglia and internal capsule (Charcot-Bouchard of
lenticulostriate vessels)
Bleeding may occur in a contused area of brain.
Mass effect from developing hematomas may present as a delayed neurologic
deficit.
Delayed traumatic intracerebral hemorrhage is most likely to occur within the
first 24 hours.
Patients with contusion on the initial head CT scan should be reimaged 24 hours
after the trauma to document stable pathology.
Indications for craniotomy include:
any clot volume >50 cm3 or
a clot volume >20 cm3 with referable neurologic deterioration (GCS 6–
8) and associated midline shift >5 mm or basal cistern compression
NANI Schwartz, Sabiston 3 of 3
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Continuo Playing According To Handel - His Figured Bass ExercisesDocument71 pagesContinuo Playing According To Handel - His Figured Bass ExercisesGaxin100% (3)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Yanmar Excavator Yb221u - Yb221uz - b22 - 1 Service Manual + Electrical Wiring Diagrams + Parts CatalogDocument161 pagesYanmar Excavator Yb221u - Yb221uz - b22 - 1 Service Manual + Electrical Wiring Diagrams + Parts CatalogJonas Svidinskas100% (1)
- Recruitment Strategies PDFDocument27 pagesRecruitment Strategies PDFjagatapsv100% (2)
- Secure Access 6.2 Study Guide-OnlineDocument421 pagesSecure Access 6.2 Study Guide-OnlineChalaNo ratings yet
- Supernatural by Graham HancockDocument4 pagesSupernatural by Graham Hancockiftsm50% (2)
- Ase Resentation: Marianne Angelina R. Lorenzo Post-Graduate InternDocument65 pagesAse Resentation: Marianne Angelina R. Lorenzo Post-Graduate InternMarianne R. LorenzoNo ratings yet
- OPHTHA - Histiry and PEDocument6 pagesOPHTHA - Histiry and PEMarianne R. LorenzoNo ratings yet
- Drinking Alcohol. Denies Melena, Hematemesis, Abdominal Pain, Seizures and TremorsDocument12 pagesDrinking Alcohol. Denies Melena, Hematemesis, Abdominal Pain, Seizures and TremorsMarianne R. LorenzoNo ratings yet
- Critical Appraisal For Therapy: CitationDocument2 pagesCritical Appraisal For Therapy: CitationMarianne R. LorenzoNo ratings yet
- Mycobacterium Bovis)Document6 pagesMycobacterium Bovis)Marianne R. LorenzoNo ratings yet
- CHB 1Document1 pageCHB 1Marianne R. LorenzoNo ratings yet
- EBM - Fish OilDocument2 pagesEBM - Fish OilMarianne R. LorenzoNo ratings yet
- Virtual Course DescriptionDocument3 pagesVirtual Course DescriptionMarianne R. LorenzoNo ratings yet
- Citation:: How Serious Is The Risk of Bias?Document2 pagesCitation:: How Serious Is The Risk of Bias?Marianne R. LorenzoNo ratings yet
- As Water Soluble Vitamin and Coenzyme: Vitamin B or ThiamineDocument6 pagesAs Water Soluble Vitamin and Coenzyme: Vitamin B or ThiamineMarianne R. LorenzoNo ratings yet
- Topical Antibacterial Preparations: Dermatologic Pharmacology Natakneng 2020Document1 pageTopical Antibacterial Preparations: Dermatologic Pharmacology Natakneng 2020Marianne R. LorenzoNo ratings yet
- Smoking, AlcoholDocument2 pagesSmoking, AlcoholMarianne R. LorenzoNo ratings yet
- Experiment On Isolation and Purification of ProteinDocument6 pagesExperiment On Isolation and Purification of ProteinMarianne R. LorenzoNo ratings yet
- Holoprosencephaly (Arhinencephaly Figure 7.35) : Fetal Alcohol SyndromeDocument3 pagesHoloprosencephaly (Arhinencephaly Figure 7.35) : Fetal Alcohol SyndromeMarianne R. LorenzoNo ratings yet
- Experiment On Color ReactionsDocument4 pagesExperiment On Color ReactionsMarianne R. Lorenzo100% (1)
- Cri Du ChatDocument3 pagesCri Du ChatMarianne R. LorenzoNo ratings yet
- CholeraDocument3 pagesCholeraMarianne R. LorenzoNo ratings yet
- Facts: Geographic DistributionDocument3 pagesFacts: Geographic DistributionMarianne R. LorenzoNo ratings yet
- Investigatory Project by Erika Sheane Estera and Jomel MaromaDocument21 pagesInvestigatory Project by Erika Sheane Estera and Jomel MaromaI-Ruby707997% (59)
- Information Paper: Northern Territory Skilled Occupation Priority ListDocument10 pagesInformation Paper: Northern Territory Skilled Occupation Priority ListHarjit Singh MangatNo ratings yet
- Subject:: Social Science (For Mid-Term Exams.)Document2 pagesSubject:: Social Science (For Mid-Term Exams.)SKULL XT GAMINGNo ratings yet
- Creative Nonfiction - Week 1Document23 pagesCreative Nonfiction - Week 1Mae Sheilou Conserva PateroNo ratings yet
- Facilitate - Training MatrixDocument2 pagesFacilitate - Training MatrixLovely DoranoNo ratings yet
- Pull System-Raymond GP ProjectDocument17 pagesPull System-Raymond GP ProjectAnushka SharmaNo ratings yet
- The Sovereignty of God Part 05Document7 pagesThe Sovereignty of God Part 05Alan D Cobourne-SmithNo ratings yet
- Piano Playing MechanismsDocument245 pagesPiano Playing MechanismsShawBoy2100% (1)
- Demerath 2018Document17 pagesDemerath 2018Aura TabaraNo ratings yet
- LESSON 3 - Information LiteracyDocument10 pagesLESSON 3 - Information LiteracyAngel Trisha MariNo ratings yet
- Article 05 MehboobDocument20 pagesArticle 05 MehboobMUHAMMAD HASHAAMNo ratings yet
- Heart Block and Their Best Treatment in Homeopathy - Bashir Mahmud ElliasDocument13 pagesHeart Block and Their Best Treatment in Homeopathy - Bashir Mahmud ElliasBashir Mahmud Ellias67% (3)
- Asma y CovidDocument18 pagesAsma y CovidSMIBA MedicinaNo ratings yet
- People of The Philippines, Petitioner, vs. EDGARDO V. ODTUHAN, RespondentDocument12 pagesPeople of The Philippines, Petitioner, vs. EDGARDO V. ODTUHAN, RespondentEnverga Law School Corporation Law SC DivisionNo ratings yet
- Potato Gratin Recipe - Google SearchDocument1 pagePotato Gratin Recipe - Google Searchadinda putri safriniNo ratings yet
- Vsphere Esxi 703 Installation Setup GuideDocument238 pagesVsphere Esxi 703 Installation Setup GuideErdem EnustNo ratings yet
- TwisterDocument4 pagesTwisterapi-355601906No ratings yet
- Understanding Shared Memory and Semaphores - Oracle FAQDocument7 pagesUnderstanding Shared Memory and Semaphores - Oracle FAQHari SuryakanthNo ratings yet
- Guide To Firewalls and VPNS, 3 Edition: Chapter One Introduction To Information SecurityDocument47 pagesGuide To Firewalls and VPNS, 3 Edition: Chapter One Introduction To Information SecurityDominica McCoyNo ratings yet
- Post Test IkmDocument2 pagesPost Test IkmjiyankhaylilaNo ratings yet
- Soal Uas B Inggris Kls 11 SM 1Document8 pagesSoal Uas B Inggris Kls 11 SM 1Kirigaya HideyoshiNo ratings yet
- Layers of EarthDocument13 pagesLayers of EarthJazrel D. De Los SantosNo ratings yet
- Nep 2022 Volume 1Document1,410 pagesNep 2022 Volume 1Roldz LariosNo ratings yet
- Book of PriestcraftDocument130 pagesBook of PriestcraftEduardo Luiz Pinto100% (1)
- Cyber Security Interview QuestionsDocument6 pagesCyber Security Interview QuestionsUmesh KanadeNo ratings yet