Professional Documents
Culture Documents
Case Study 2 (COPD)
Uploaded by
honeylemon.co0 ratings0% found this document useful (0 votes)
119 views2 pagespharmacy
Original Title
Case study 2 (COPD)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpharmacy
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
119 views2 pagesCase Study 2 (COPD)
Uploaded by
honeylemon.copharmacy
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
CONFIDENTIAL 1 PH/JUNE 2020/PHD222
UNIVERSITI TEKNOLOGI MARA
COURSE : HOSPITAL PHARMACY
COURSE CODE : PHD222
INDIVIDUAL : 13TH JULY 2020 (To be submitted)
ASSIGNMENT
CASE 2
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
Mr B is a 67-year-old retired miner who presents to hospital as an emergency with acute
shortness of breath and a cough productive of green sputum. Mr B has a past medical
history of COPD and had a myocardial infarction 10 years ago. He smokes 35
cigarettes per day and has done so for the last 45 years. Spirometry has shown that his
FEV1 is 58% of predicted. He weighs 45 kg.
When he is well his assessment test (CAT) score is 8. There are no known drug
allergies.
Mr B’s regular medication is:
• aspirin 75 mg daily,
• bisoprolol 10 mg daily,
• simvastatin 20 mg at night,
• salmeterol 25 microgram pressurized metered dose inhaler (pMDI) two puffs twice
daily.
CONFIDENTIAL 2 PH/JUNE 2020/PHD222
On examination:
• blood pressure (BP) 130/75 mmHg,
• temperature 38.6 °C,
• pulse 98 bpm,
• respiratory rate 28 breaths/min.
Investigations:
• white blood cell count 20.8 × 109 L,
• creatinine 140 mmol/L – his baseline was 93 mmol/L 3 months ago,
• Hb – normal,
• oxygen saturation 84% on 28% oxygen via Venturi mask,
• chest X-ray – no consolidation seen.
Arterial blood gases on 28% oxygen:
pH 7.30 (7.35–7.45)
pO2 7.26 kPa (10–13 kPa)
pCO2 8.3 kPa (4.7–6.0 kPa)
HCO3 24 mmol/L (22–26 mmol/L)
Mr B shows no clinical improvement and appears to be tiring. He is transferred to the
intensive care unit (ICU) in case ventilation (invasive or non-invasive) may be needed.
In the ICU, the intensivists wish to increase his medical treatment.
Few hints as questions for case evaluation;
1. What is the diagnosis, and how was this determined?
2. What do the arterial blood gases show, and how would you suggest this is
managed?
3. What would you expect to see on Mr B’s prescription chart for acute management
of his condition?
4. What options are there?
5. How should aminophylline be administered?
6. What treatment options would you recommend for Mr B once he has recovered
from his acute illness?
7. Are there any other medications that require optimization?
You might also like
- 312312312312312Document5 pages312312312312312Nyeam NyeamNo ratings yet
- Hypertension and 24-hour Ambulatory Blood Pressure MonitoringFrom EverandHypertension and 24-hour Ambulatory Blood Pressure MonitoringNo ratings yet
- Case Study Hypertension 1Document3 pagesCase Study Hypertension 1honeylemon.coNo ratings yet
- Community Acquired PneumoniaDocument21 pagesCommunity Acquired PneumoniaIlyas HalimNo ratings yet
- Rle Case Study - Septic ShockDocument2 pagesRle Case Study - Septic Shockhazel sergioNo ratings yet
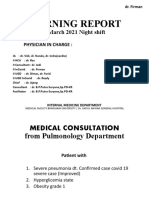
- Morning Report: 2 March 2021 Night ShiftDocument16 pagesMorning Report: 2 March 2021 Night ShiftWilujeng AnggrainiNo ratings yet
- CASE 6 - COVID 19 - OHI - 2021 - Rev Page 3Document12 pagesCASE 6 - COVID 19 - OHI - 2021 - Rev Page 3wahyu kijang ramadhanNo ratings yet
- กรณีศึกษา (case study) อ.เพ็ญนภาDocument8 pagesกรณีศึกษา (case study) อ.เพ็ญนภาKanisthita ChutikittidechapatNo ratings yet
- IGD BAR Confirmed CovidDocument4 pagesIGD BAR Confirmed CovidWilujeng AnggrainiNo ratings yet
- MR Friday NightDocument28 pagesMR Friday NightmuhammadrikiNo ratings yet
- 1024 4076 1 PB 1Document11 pages1024 4076 1 PB 1Yulius TimotiusNo ratings yet
- Journal Reading 1Document34 pagesJournal Reading 1EdiSusantoAhmadTasiNo ratings yet
- Articulo 1 Electiva1Document6 pagesArticulo 1 Electiva1Javier Montero MonteeoNo ratings yet
- Journal Reading 1Document25 pagesJournal Reading 1tikaNo ratings yet
- 2019 Novel Coronavirus Disease With Secondary Ischemic Stroke Two Case Reports2021BMC NeurologyOpen AccessDocument5 pages2019 Novel Coronavirus Disease With Secondary Ischemic Stroke Two Case Reports2021BMC NeurologyOpen Accesssantiago lopezNo ratings yet
- REV MRJagaTengah - MEDCON - ANI - hyperbilirubinemia+transaminitis+AKIDocument22 pagesREV MRJagaTengah - MEDCON - ANI - hyperbilirubinemia+transaminitis+AKILilik AndayatiNo ratings yet
- Correlating Arterial Blood Gas, Acid-Base and Blood Pressure Abnormalities With Outcomes in COVID-19 Intensive Care PatientsDocument7 pagesCorrelating Arterial Blood Gas, Acid-Base and Blood Pressure Abnormalities With Outcomes in COVID-19 Intensive Care PatientsAriqa AzzhraNo ratings yet
- The ABC of HBP-The Art of Blood Pressure TakingDocument44 pagesThe ABC of HBP-The Art of Blood Pressure TakingRenal Association MauritiusNo ratings yet
- กรณีศึกษา (case study) อ.เพ็ญนภาDocument8 pagesกรณีศึกษา (case study) อ.เพ็ญนภาKanisthita ChutikittidechapatNo ratings yet
- Drug Study Case 1Document37 pagesDrug Study Case 1Maria Charis Anne IndananNo ratings yet
- Wates - Presentasi Transport Anak KritisDocument27 pagesWates - Presentasi Transport Anak Kritisbayu ariani chandrasariNo ratings yet
- Case Study 3 CancerDocument4 pagesCase Study 3 Cancerhoneylemon.coNo ratings yet
- Expression of Renal Injury Markers Among Diabetic Patients in The University of Port Harcourt Teaching HospitalDocument8 pagesExpression of Renal Injury Markers Among Diabetic Patients in The University of Port Harcourt Teaching Hospitalijmb333No ratings yet
- Mastering MRCP Vol2Document348 pagesMastering MRCP Vol2mostachek88% (8)
- Verifikator Id enDocument2 pagesVerifikator Id ennovi rista anandaNo ratings yet
- Case Report - Ikmalun NatiqDocument16 pagesCase Report - Ikmalun Natiqkelompok lawangNo ratings yet
- 2022 Care Plan 2Document9 pages2022 Care Plan 2api-601587526No ratings yet
- 2nd Case Scenario BronchitisDocument5 pages2nd Case Scenario BronchitisKasandra Dawn Moquia BerisoNo ratings yet
- Bartlett COVID Case StudyDocument14 pagesBartlett COVID Case StudyFarion birdNo ratings yet
- Fphar 11 00966Document8 pagesFphar 11 00966Cristie SumbillaNo ratings yet
- Case ReportDocument25 pagesCase ReportFadhilah Amirah NasutionNo ratings yet
- Lifestyle Modifications in The Management of Hypertensive Patients in A Secondary Care Center A Descriptive Cross-Sectional StudyDocument5 pagesLifestyle Modifications in The Management of Hypertensive Patients in A Secondary Care Center A Descriptive Cross-Sectional StudyInternational Journal of Innovative Science and Research Technology100% (1)
- COVID-19 Antiviral TX Guidance 4-22-2020Document23 pagesCOVID-19 Antiviral TX Guidance 4-22-2020Lydia IsaacNo ratings yet
- Pulmonary Sequele After COVID-19Document61 pagesPulmonary Sequele After COVID-19Nandha KumarNo ratings yet
- A Short Therapeutic Regimen Based On HydroxychloroDocument19 pagesA Short Therapeutic Regimen Based On HydroxychloroDiego NevesNo ratings yet
- Critical Limits of Laboratory Results For Urgent Clinician NotificationDocument8 pagesCritical Limits of Laboratory Results For Urgent Clinician NotificationMartesciuc VeraNo ratings yet
- Case Studies AssignmentDocument4 pagesCase Studies AssignmentCARRAO, Samuel Jr.No ratings yet
- Clinical Features and Multidisciplinary Treatment Outcome of COVID-19 Pneumonia: A Report of Three CasesDocument8 pagesClinical Features and Multidisciplinary Treatment Outcome of COVID-19 Pneumonia: A Report of Three CasesPutri NoviaNo ratings yet
- Shared RX Modules For FinalsDocument11 pagesShared RX Modules For FinalsOdyNo ratings yet
- COPD CaseDocument5 pagesCOPD Caseshilanhiwa211No ratings yet
- Zidovudineinduced AnaemiaDocument23 pagesZidovudineinduced AnaemiaSuresh ThanneruNo ratings yet
- Niall Cosgrave Email: Ncosgrav@Tcd - IeDocument24 pagesNiall Cosgrave Email: Ncosgrav@Tcd - IeSaoirse MorrinNo ratings yet
- Nursing Care Plan Hemorrhagic StrokeDocument8 pagesNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- Instruction: The Following Continuous Assessment Sheets Contain Two CategoriesDocument6 pagesInstruction: The Following Continuous Assessment Sheets Contain Two CategoriesfekaduNo ratings yet
- Case Scenario BronchitisDocument4 pagesCase Scenario BronchitisJamelyn AsuncionNo ratings yet
- Case Presentation On:: Rheumatoid Arthritis With Newly Diagnoised Steroid Related DM With Systemic HypertensionDocument12 pagesCase Presentation On:: Rheumatoid Arthritis With Newly Diagnoised Steroid Related DM With Systemic HypertensionSamyuktaNo ratings yet
- Ivermectin As A Potential Therapeutic Agent For COVID-19-CasestudiesDocument3 pagesIvermectin As A Potential Therapeutic Agent For COVID-19-CasestudiesMilly Farisa KurniaNo ratings yet
- 05june2020 20200106 Clinical Management Guidelines For COVID-19 Infection v2Document13 pages05june2020 20200106 Clinical Management Guidelines For COVID-19 Infection v2Murtaza HasanNo ratings yet
- MR - INCOVIT - 30521 - Probable Covid-Complicated UTI - SAHDocument24 pagesMR - INCOVIT - 30521 - Probable Covid-Complicated UTI - SAHIka AyuNo ratings yet
- 2020 Copd Mega Case - KeyDocument5 pages2020 Copd Mega Case - KeyJarmarcus MarshallNo ratings yet
- SDDI-POL-2030 (2hr Post Prandial)Document5 pagesSDDI-POL-2030 (2hr Post Prandial)Christian VasquezNo ratings yet
- FHS Medical Nursing BNTDocument3 pagesFHS Medical Nursing BNTssekali stephenNo ratings yet
- NUR265 Exam 2 Holmes Mock Answered PDFDocument13 pagesNUR265 Exam 2 Holmes Mock Answered PDFNoemi GabayNo ratings yet
- Pharmaceutical SciencesDocument5 pagesPharmaceutical SciencesiajpsNo ratings yet
- 8.1 - Cases - ViralDocument25 pages8.1 - Cases - Viralkoteshwara raoNo ratings yet
- MR AlimuddinDocument10 pagesMR AlimuddinNur Farmawati Humayrah HassaniNo ratings yet
- Henatologi AnalyxerDocument6 pagesHenatologi Analyxerrasyidsaefullah56No ratings yet
- Daniel Aman, MD (Ass'T Professor of Emergency Medicine and Critical Care, SPHMMC)Document52 pagesDaniel Aman, MD (Ass'T Professor of Emergency Medicine and Critical Care, SPHMMC)Temesgen GeletaNo ratings yet
- Soal Praktek-EBM-THTKL-Daniel BramantyoDocument20 pagesSoal Praktek-EBM-THTKL-Daniel BramantyoDaniel BramantyoNo ratings yet
- Outpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020Document37 pagesOutpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020honeylemon.coNo ratings yet
- Pulcer Disease RDocument5 pagesPulcer Disease Rhoneylemon.coNo ratings yet
- Case Study 3 CancerDocument4 pagesCase Study 3 Cancerhoneylemon.coNo ratings yet
- Staphylococci & MicrococciDocument52 pagesStaphylococci & Micrococcihoneylemon.coNo ratings yet
- PHD113 - Professions in PharmacyDocument49 pagesPHD113 - Professions in Pharmacyhoneylemon.co100% (1)
- PHD113 - Professions in PharmacyDocument49 pagesPHD113 - Professions in Pharmacyhoneylemon.co100% (1)
- Self Medication LectureDocument43 pagesSelf Medication Lecturehoneylemon.coNo ratings yet
- PHD211 - Ointment 2019Document147 pagesPHD211 - Ointment 2019honeylemon.co100% (2)
- Pastes: PHD 211 - Semisolid Dosage FormsDocument50 pagesPastes: PHD 211 - Semisolid Dosage Formshoneylemon.coNo ratings yet
- Pharmacotherapy of PneumoniaDocument56 pagesPharmacotherapy of Pneumoniahoneylemon.co100% (1)
- PHD211 - Poultices 2019Document20 pagesPHD211 - Poultices 2019honeylemon.coNo ratings yet
- Suppositories LectureDocument86 pagesSuppositories Lecturehoneylemon.coNo ratings yet
- Elc 2 EvaluativeDocument2 pagesElc 2 Evaluativehoneylemon.coNo ratings yet
- Weighing & MeasurementDocument39 pagesWeighing & Measurementhoneylemon.co100% (1)
- Exp 8 - RedoxDocument4 pagesExp 8 - RedoxAman ParikhNo ratings yet
- KOD Kursus Nama Kursus SE M Penilaian Baru Penilaian Baru Nama RPDocument3 pagesKOD Kursus Nama Kursus SE M Penilaian Baru Penilaian Baru Nama RPhoneylemon.coNo ratings yet
- Exp 8 - RedoxDocument475 pagesExp 8 - Redoxhoneylemon.co100% (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)