Professional Documents
Culture Documents
Pre-Natal Care (Book Based) PDF
Pre-Natal Care (Book Based) PDF
Uploaded by
riczen mae vilaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pre-Natal Care (Book Based) PDF
Pre-Natal Care (Book Based) PDF
Uploaded by
riczen mae vilaCopyright:
Available Formats
OBSTETRICS AND GYNECOLOGY II
PRE-NATAL CARE
From Williams Obstetrics 24th edition
Breast and Skin Changes
LEGEND • Anatomical changes in the breasts that accompany
Lecture Powerpoint, Audio, Textbook pregnancy are characteristic during a first pregnancy
RED FONTCOLOR – MUST KNOWS!!! • Less obvious multiparas
PRENATAL CARE
“A comprehensive antepartum program involves a coordinated Fetal Movement
approach to medical care, continuous risk assessment, and psycho- • Maternal perception of fetal movement depends on factors
logical support that optimally begins before conception and extends such as parity and habitus
throughout the postpartum period and interconceptional period.” – • Multigravid – 16 and 18 weeks gestation
ACOG (2012) • Primigravid - ~20 weeks
• Examiner – ~20 weeks
ASSESSING PRENATAL CARE ADEQUACY
KESSNER INDEX PREGNANCY TESTS
• Commonly employed system and remains useful for • Detection of hCG in maternal blood and urine is the basis for
measuring prenatal care adequacy endocrine assays of pregnancy
• Incorporates three items from the birth certificate • hCG
o Length of gestation o produced by syncytiotrophoblast
o Timing of the first prenatal visit o amount increase exponentially during the fiist trimester
o Number of visits following implantation
• Does not measure the quality of care o α-subunit is identical to those of luteinizing hormone (LH),
follicle-stimulating hormone (FSH), and thyroid-stimulating
DIAGNOSIS OF PREGNANCY hormone (TSH)
o prevents involution of the corpus luteum
SIGNS AND SYMPTOMS ▪ principal site of progesterone formation during the rst 6
Amenorrhea weeks of pregnancy
• Abrupt cessation of menstruation in a healthy reproductive- o hormone can be detected in maternal serum or urine by 8
aged woman who previosly ha experienced spontaneous, to 9 days after ovulation – using a sensitive test
cyclical, predictable menses – highly suggestive of o doubling time of serum hCG concentration is 1.4 to 2.0
pregnancy days
• Not a reliable pregnancy indicator until 10 days or more after o serum hCG levels increase from the day of implantation
expected menses and reach peak levels at 60 to 70 days
o concentration declines slowly until a plateau is reached at
Lower-Reproductive-Tract-Changes approximately 16 weeks
• Chadwick sign – during pregnancy, the vaginal mucosa
usually appears dark-bluish red and congested SONOGRAPHIC RECOGNITION OF PREGNANCY
• Increased cervical softening • Transvaginal sonography
o Happens as pregnancy advances o Commonly used to accurately establish gestational age
o Estrogen-progestin contraceptives may cause similar o Confirms pregnancy location
softening • Gestational sac – first sonographic evidence of pregnancy
• fernlike pattern of mucus o Small anechoic fluid collection within endometrial cavity
o substantial increase in progesterone secretion associated o 4-6 weeks gestation
with pregnancy a ects the consistency and microscopic o normal gestational sac implants eccentrically in the
appearance of cervical mucus endometrium, whereas a pseudosac is seen in the midline
of the endometrial cavity
Uterine Changes • Pseudogestational sac / Pseudosac
• First few weeks of pregnancy o Fluid collection within endometrial cavity with an ectopic
o Uterine size grows principally in the anteroposterior pregnancy
diameter o further evaluation may be warranted if this is the only
▪ Feels doughy or elastic – during bimanual examination sonographic nding, particularly in a patient with pain or
• 6 to 8 weeks menstrual age bleeding
o Hegar sign • Intradecidual sign
▪ firm cervix contrasts with the now softer fundus o anechoic center surrounded by a single echogenic rim
▪ compressible interposed softened isthmus • Double decidual sign
▪ Isthmic softening may be so marked that the cervix and o two concentric echogenic rings surrounding the gestational
uterine body seem to be separate organs sac
• 12 weeks gestation • Pregnancy of unknown location
o uterine body is almost globular, with an average diameter o When sonography yields equivocal findings
of 8 cm o serial serum hCG levels can also help di erentiate a normal
• later in pregnancy intrauterine pregnancy from an extrauterine pregnancy or
o uterine souffle an early miscarriage
▪ soft, blowing sound that is synchronous with the maternal • middle of the fifth week
pulse o Visualization of the yolk sac confirms with certainty an
▪ produced by the passage of blood through the dilated intrauterine location for the pregnancy and can normally be
uterine vessels seen by the
▪ heard most distinctly near the lower portion of the uterus • after 6 weeks
o embryo is seen as a linear structure immediately adjacent
to the yolk sac
o funic souffle o cardiac motion is typically noted at this point
▪ sharp, whistling sound that is synchronous with the fetal
pulse • 12 weeks gestation
▪ caused by the rush of blood through the umbilical o crown-rump length is predictive of gestational age within 4
arteries days
▪ may not be heard consistently
Transcribed by: MM dela Rosa, Reina Abu Page 1 of 9
PRE-NATAL CARE
• use of oral contraceptives (steroidal)
o Because ovu- lation may not have resumed 2 weeks after
the onset of the last withdrawal bleeding and instead may
have occurred at an appreciably later and highly variable
date, using the time of ovulation for predicting the time of
conception in this circum- stance may be erroneous
• Use of sonography in early pregnancy will clarify gestational
age in unpredictable situations
PERSONAL AND SOCIAL HISTORY
Psychosocial Screening
• psychosocial issues as nonbiomedical factors that a ect
mental and physical well-being – AAP and ACOG (2012)
• seek barriers to care, communication obstacles, nutritional
status, unstable housing, desire for pregnancy, safety
concerns that include intimate partner violence, depression,
stress, and use of substances such as tobacco, alcohol, and
illicit drugs
• should be performed on a regular basis, at least once per
trimester, to identify important issues and reduce adverse
pregnancy outcomes
Cigarette Smoking
• Numerous adverse outcomes have been linked to smoking
INITIAL PRENATAL EVALUATION during pregnancy
• Prenatal care should be initiated as soon as there is a o Potential teratogenic effects
reason- able likelihood of pregnancy o twofold risk of placenta previa, placental abruption, and
• Major goals premature membrane rupture
o de ne the health status of the mother and fetus o neonates born to women who smoke are more likely to be
preterm, have lower birth- weights, and are more likely to
o estimate the gesta- tional age
o initiate a plan for continuing obstetrical care die of sudden infant death syndrome (SIDS)
o Risks for spontaneous abortion, fetal death, and fetal digital
anomalies are also increased
DEFINITIONS o children who were exposed to smoking in utero are at
1. Nulligravida - woman who currently is not pregnant nor has increased risk for asthma, infantile colic, and childhood
ever been pregnant obesity
2. Gravida - woman who currently is pregnant or has been in • Smoking cessation is advised
the past, irrespective of the pregnancy outcome
o With the establishment of the first pregnancy, she becomes
a primi- gravida, and with successive pregnancies, a
multigravida.
3. Nullipara – a woman who has never completed a pregnancy
beyond 20 weeks’ gestation
4. Primipara – woman who has been delivered only once of a
fetus or fetuses born alive or dead with an estimated length
of gestation of 20 or more weeks
5. Multipara - woman who has completed two or more preg-
nancies to 20 weeks’ gestation or more
o Parity is determined by the number of pregnancies
reaching 20 weeks
NORMAL PREGNANCY DURATION
• first day of the last normal menstrual period is very close to
280 days or 40 weeks
• Naegele rule – estimate of expected delivery date
o adding 7 days to the date of the rst day of the last normal
menstrual period and counting back 3 months
o a gestational age or menstrual age calculated in this way
assumes pregnancy to have begun approximately 2 weeks
before ovulation, which is not always the case
TRIMESTERS
• FIRST TRIMESTER – 0 to 14 weeks
• SECOND TRIMESTER – 15 to 28 weeks Alcohol
• THIRD TRIMESTER – 29 to 42 weeks • Ethyl alcohol or ethanol
• clinically appropriate unit is weeks of gestation completed o potent teratogen that causes a fetal syndrome
• clinicians designate gestational age using completed weeks characterized by growth restriction, facial abnormalities,
and days and central nervous system dysfunction
PREVIOUS AND CURRENT HEALTH STATUS Illicit Drugs
• same essentials of history taking as in medicine • Agents may include heroin and other opiates, cocaine,
amphetamines, barbiturates, and marijuana
• detailed information regarding previous pregnancies is
• Chronic use of large quantities is harmful to the fetus
essential
• mensttual history is also important • Well-documented sequelae include fetal-growth restriction,
o varies based on frequency and duration of menses low birthweight, and drug withdrawal soon after birth
o without a history of regular, predictable, cyclic,
Intimate partner violence
spontaneous menses that suggest ovulatory cycles,
accurate dating of pregnancy by history and physical • a pattern of assaultive and coercive behav- iors that may
examination is difficult include physical injury, psychological abuse, sexual assault,
Transcribed By: MM dela Rosa, Reina Abu Page 2 of 9
PRE-NATAL CARE
progressive isolation, stalking, deprivation, intimidation, and streptococcal (GBS) cultures be obtained in all women
reproductive coercion (ACOG 2012) between 35 and 37 weeks’ gestation
CLINICAL EVALUATION Gestational Diabetes
• A thorough, general physical examination should be • Laboratory testing between 24 and 28 weeks’
completed at the initial prenatal encounter gestation is the most sensitive approach
• Pelvic examination is performed as part of the evaluation
o Visualization of the cervix using a speculum Selected Genetic Screening
▪ Bluish-red passive hyperemia of the cervix is • Selected screening for certain genetic abnormalities
characteristic, but not of itself diagnostic, of pregnancy should be offered to those at increased risk based on
▪ Dilated, occluded cervical glands bulging beneath the family history, ethnic or racial background, or age
ectocervical mucosa—nabothian cysts—may be
prominent
NUTRITIONAL COUNSELING
▪ e cervix is not normally dilated except at the external os
o Bimanual examination WEIGHT GAIN RECOMMENDATIONS
▪ Completed by palpation • 20th century - limited to less than 20 lb or about 9 kg
▪ special attention to o prevent gestational hypertension and fetal macrosomia
✓ consistency, length, and dilatation of the cervix; • 1970s - at least 25 lb or 11 to 12 kg to prevent preterm birth
✓ uterine and adnexal size; and fetal-growth restriction
✓ bony pelvic architecture; and • The Institute of Medicine and National Research Council
✓ any vaginal or perineal anomalies (2009) revised its guidelines for weight gain in pregnancy and
• Lesions of the cervix, vagina, or vulva should be further continues to stratify suggested weight gain ranges based
evaluated as needed by colposcopy, biopsy, culture, or dark- on prepregnancy body mass index (BMI)
eld examination • There is irrefutable evidence that maternal weight gain during
• The perianal region should be visualized, and digital rectal pregnancy in influences birthweight
examination performed as required for complaints of rectal • Obesity in pregnancy
pain, bleeding, or mass o significantly increased risks for gestational hypertension,
preeclampsia, gestational diabetes, macrosomia, cesarean
SUBSEQUENT PRENATAL VISITS delivery, and other complications
• Prenatal Visits • women with low weight gains in pregnancy
o 4-week intervals until 28 weeks, o higher risk for preterm delivery
o Every 2 weeks until 36 weeks o higher risk for small-for-gestational age newborns
o Weekly thereafter
• Women with complicated pregnancies often require
return visits at 1- to 2-week intervals
PRENATAL SURVEILLANCE
Fundal Height
• Between 20 and 34 weeks, the height of the uterine
fundus measured in centimeters correlates closely with
gestational age in weeks
• Used to monitor fetal growth and amnionic fluid volume
Fetal Heart Sounds
• 10 weeks – detection of fetal heart sound; Doppler
ultrasound
• Normal FHT: 110-160 bpm
• Using a standard nonamplified stethoscope, the fetal
heart may be audible as early as 16 weeks
• Fetal heart was audible by 20 weeks in 80 percent of
women, and by 22 weeks, heart sounds were heard in
all.
Sonography
• Provides invaluable information regarding fetal
anatomy, growth, and well-being SEVERE UNDERNUTRITION
• mid to late pregnancy nutrition deprivation
SUBSEQUENT LABORATORY TESTS o children were lighter, shorter, and thinner at birth
• If initial results were normal, most tests need not be o higher incidence of sub- sequent diminished glucose
repeated tolerance, hypertension, reactive airway disease,
• Fetal aneuploidy screening may be performed at 11 dyslipidemia, and coronary artery disease
to 14 weeks and/or at 15 to 20 weeks • early pregnancy nutrition deprivation
• Serum screening for neural- tube defects is offered at o increased obesity in adult women but not men
15 to 20 weeks o also linked to increased central nervous system anomalies,
schizophrenia, and schizophrenia-spectrum personality
• Increased risk for HIV acquisition during pregnancy,
disorders
repeat testing is recommended in the third trimester,
preferably before 36 weeks’ gestation • Barker hypothesis
o fetal programming – adult morbidity and mortality are
• Women who engage in behaviors that place them at
related to fetal health
high risk for hepatitis B infection should be retested at
the time of hospitalization for delivery
• Women who are D (Rh) negative and are unsensitized WEIGHT RETENTION AFTER PREGNANCY
should have an antibody screening test repeated at 28 • Not all the weight gained during pregnancy is lost during and
to 29 weeks, with administration of anti-D immune immediately after delivery
globulin if they remain unsensitized • The more weight that was gained during pregnancy, the more
that was lost post- partum
Group B Streptococcal Infection • no relationship between pre- pregnancy BMI or prenatal
• The Centers for Disease Control and Prevention weight gain and weight retention
(2010b) recommend that vaginal and rectal group B
Transcribed By: MM dela Rosa, Reina Abu Page 3 of 9
PRE-NATAL CARE
• Accruing weight with age—rather than parity—is considered MINERALS
the main factor affecting weight gain over time IRON
• approximate 1000 mg of iron required for normal pregnancy
RECOMMENDED DIETARY ALLOWANCES o 300 mg are actively transferred to the fetus and placenta
• Certain prenatal vitamin–mineral supplements may lead to o 200 mg are lost through various normal excretion routes,
intakes well in excess of the recommended allowances primarily the gastrointestinal tract
• use of excessive supplements, which often are self- • 500 mg incorporated into the expanding maternal hemoglobin
prescribed, has led to concern regarding nutrient toxicities mass, nearly all is used after mid- pregnancy
during pregnancy o iron requirements imposed by pregnancy and maternal
• POTENTIALLY TOXIC - iron, zinc, selenium, and vitamins excretion total approximately 7 mg per day
A, B6, C, and D o Few women have sufficient iron stores or dietary iron
o Vitamin A (> 10,000 IU / day) may be teratogenic intake to supply this amount
• Vitamin and mineral intake more than twice the • at least 27 mg of elemental iron supplement be given daily to
recommended daily dietary allowance shown in Table 9-6 pregnant women
should be avoided • at least 30 mg of elemental iron, supplied as ferrous
gluconate, sulfate, or fumarate and taken daily throughout the
CALORIES latter half of pregnancy, provides sufficient iron to meet
• pregnancy requires an additional 80,000 kcal, mostly during pregnancy requirements and to protect preexisting iron
the last 20 weeks stores.
• a caloric increase of 100 to 300 kcal per day is recommended o is amount will also provide for iron requirements of lactation
during pregnancy • Large fetus or win gestation – 60 to 100mg
• is intake increase, however, should not be divided equally • Not necessary to provide iron supplements during first 4
during the course of pregnancy months of pregnancy
o e Institute of Medicine (2006) recommends adding 0, 340, o Slight iron requirements during this time
and 452 kcal/day to the estimated nonpregnant energy o Avoids risk of aggravating nausea and vomiting
requirements in the first, second, and third trimesters, • Ingestion of iron at bedtime or on an empty stomach aids
respectively absorption and appears to minimize the possibility of an
adverse gastrointestinal reaction
PROTEIN
Iodine
• basic protein needs of the nonpregnant woman are added the
• Recommended daily iodine allowance is 220 μg
demands for growth and remodeling of the fetus, placenta,
uterus, and breasts, as well as increased maternal blood • use of iodized salt and bread products is recommended
volume during pregnancy set the increased fetal requirements and
maternal renal losses of iodine
• During the second half of pregnancy, approximately 1000 g of
protein are deposited, amounting to 5 to 6 g/day • Severe maternal iodine deficiency predisposes offspring to
endemic cretinism, characterized by multiple severe
• Most amino-acid levels in maternal plasma fall markedly,
neurological defects
including ornithine, glycine, taurine, and proline
o Exceptions (these increase): glutamic acid and alanine
Calcium
• most protein should be supplied from animal sources, such
as meat, milk, eggs, cheese, poultry, and fish • pregnant woman retains approximately 30 g of calcium
• Most of this is deposited in the fetus late in pregnancy
• increased calcium absorption by the intestine and progressive
retention throughout pregnancy
• Efforts to prevent preeclampsia using routine calcium
supplementation have not proven efficacious
Zinc
• Severe zinc deficiency in a given person may lead to poor
appetite, suboptimal growth, and impaired wound healing.
• the recommended daily intake is approximately 12 mg
• low-birthweight infants of mothers who received zinc had
reduced risks of acute diarrhea, dysentery, and impetigo
• zinc supplementation did not bene fetal developmental
outcome
Magnesium
• Deficiency of this mineral as a consequence of pregnancy
has not been recognized
• during prolonged illness with no magnesium intake, the
plasma level might become critically low, as it would in the
absence of pregnancy
• Supplementation did not improve any measures of pregnancy
outcome
Trace Metals
• Copper, selenium, chromium, and manganese all have
important roles in certain enzyme functions
• most are provided by an average diet
• A severe geochemical selenium deficiency has been
identified in a large area of China
o frequently fatal cardiomyopathy in young children and
reproductive-aged women
Potassium
• concentration of potassium in maternal plasma decreases by
approximately 0.5 mEq/L by midpregnancy
• Potassium deficiency develops in the same circumstances as
in nonpregnant individuals.
Transcribed By: MM dela Rosa, Reina Abu Page 4 of 9
PRE-NATAL CARE
o Monitor weight gain (Goal:~25 to 35 lb in women with
Fluoride normal BMI)
• no evidence that supplemental fluoride during pregnancy is o Explore food intake by dietary recall periodically to discover
beneficial the occasional nutritional errant diet
• fluoride metabolism is not altered appreciably during o Give tablets of simple iron salts that provide at least 27mg
pregnancy of elemental iron daily
• no additional benefits from maternal ingestion of fluoridated o Give folate supplementation before and in early weeks of
water if the offspring ingested such water from birth pregnancy
• Supplemental fluoride ingested by lactating women does not o Provide iodine supplementation in areas of known dietary
increase the fluoride concentration in breast milk insufficiency
o Recheck hematocrit or hemoglobin concentration at 28 to
32 weeks gestation to detect significant decreases.
VITAMINS
• Increased requirements for most vitamins are usually COMMON CONCERNS IN PREGNANCY
supplied by any general diet that provides adequate calories
and protein except folic acid A. Employment
• In other countries, the Family and Medical Leave Act
Folic Acid requires that covered employers must grant up to 12
• Decreased incidence of neural tube defects workweeks of unpaid leave to an employee for the
birth and care of a newborn child
• more than half of all neural-tube defects can be prevented
with daily intake of 400 μg of folic acid throughout the • In the absence of complications, most women can
periconceptional period continue to work until the onset of labor
• A woman with a prior child with a neural-tube defect can • In physically demanding work, 20-60% increase in:
reduce the 2- to 5-percent recurrence risk by more than 70 o pre-term birth
percent with daily 4-mg folic acid supplements the month o fetal-growth restriction
before conception and during the rst trimester. o gestational hypertension
• Occupational fatigue (number of hours standing,
Vitamin A intensity of physical and mental demands,
environmental stressors
• Although essential, this vitamin has been associated with
o increased risk of preterm premature
congenital malformations when taken in higher doses
membrane rupture
o malformations are similar to those produced by the vitamin
• Adequate periods of rest should be provided
A derivative isotretinoin
• Advise women with previous pregnancy complications
o Beta-carotene, the precursor of vitamin A found in fruits
to minimize physical work
and vegetables, has not been shown to produce vitamin A
toxicity
• Vitamin A deficiency, whether overt or subclinical, was B. Exercise
associated with an increased risk of maternal anemia and • The American College of Obstetricians and
spontaneous preterm birth Gynecologists advises a thorough clinical evaluation
before recommending an exercise program.
Vitamin B12 • In the absence of contraindications:
• Maternal plasma vitamin B12 levels decrease in normal o Engage in regular, moderate-intensity
pregnancy mostly as a result of reduced plasma levels of physical activity for 30 minutes or more day
their carrier proteins—transcobalamins • Avoid exercises with a high risk of falling or abdominal
• Vitamin B12 occurs naturally only in foods of animal origin, trauma
and strict vegetarians may give birth to infants whose B12 • AVOID SCUBA DIVING! increased risk for
stores are low decompression sickness
• Excessive ingestion of vitamin C also can lead to a functional • If with certain pregnancy complication, abstain from
deficiency of vitamin B12 exercise or limit physical activity
• Low level of B12 preconceptionally, may increase risk of
neural tube defects, same as folate
Vitamin B6 – Pyridoxine
• For women at high risk for inadequate nutrition—for example,
substance abusers, adolescents, and those with multifetal
gestations—a daily 2-mg supplement is recommended
• vitamin B6, when combined with the antihistamine
doxylamine, is helpful in many cases of nausea and vomiting
of pregnancy
Vitamin C
• recommended dietary allowance for vitamin C during
pregnancy is 80 to 85 mg/day—approximately 20 percent
more than when nonpregnant
Vitamin D
• Unlike most vitamins that are obtained exclusively from
dietary intake, vitamin D is also synthesized endogenously
with expo- sure to sunlight
• maternal deficiency can cause disordered skeletal
homeostasis, congenital rickets, and fractures in the newborn
• adequate intake of vitamin D during pregnancy and lactation
was 15 μg per day (600 IU per day)
PRAGMATIC NUTRITIONAL SURVEILLANCE
• ADVISE PREGNANT WOMAN TO
o Eat what she wants in amounts she desires and salted to
taste
o Ensure food is amply available for socioeconomically
deprived women
Transcribed By: MM dela Rosa, Reina Abu Page 5 of 9
PRE-NATAL CARE
C. Seafood Consumption • Oral-vaginal intercourse is occasionally hazardous.
• Fish – excellent source of protein, low in saturated Aronson and Nelson (1967) described a fatal air
fats, and contain omega-3 fatty acids embolism late in pregnancy as a result of air blown into
• AVOID shark, swordfish, king mackerel, tile fish the vagina during cunnilingus.
o Because of potentially high methylmercury
levels G. Dental Care
• It is recommended that pregnant women ingest no • Examination of the teeth should be included in the
more than 12 ounces or two servings of canned tuna prenatal examination, and good dental hygiene is
per week and no more than 6 ounces of albacore or encouraged
“white” tuna • Periodontal disease has been linked to preterm labor
• The Avon Longitudinal Study of Parents and Children,
however, reported beneficial effects on pregnancy H. Immunization
outcomes in women who consumed 340 g or more of
seafood weekly
D. Lead Screening
• Maternal lead exposure has been associated with
several adverse maternal and fetal outcomes across a
range of maternal blood lead levels
o Gestational hypertension
o Spontaneous abortion
o Low birthweight
o Neurodevelopmental impairments in exposed
fetuses
• Blood lead levels ≥ 45 μg/dL are consistent with lead
poisoning may be candidates for chelation therapy
E. Automobile and Air Travel
• Women should be encouraged to wear properly
positioned three-point restraints throughout pregnancy
o The lap portion of the restraining belt should
be placed under the abdomen and across her
upper thighs
o The belt should be comfortably snug
o The shoulder belt also should be firmly
positioned between the breasts
o Airbags should not be disabled for the *See Appendix for bigger pictures
pregnant woman
• Air travel in a properly pressurized aircraft has no I. Biological Warfare and Vaccines
harmful effect on pregnancy • Smallpox vaccination
• American Academy of Pediatrics and the American o Live attenuated vaccinia virus
College of Obstetricians and Gynecologists – o Fetal vaccinia infection – rare
concluded that pregnant women can safely fly up to 36 o May result in abortion, stillbirth, or neonatal
weeks’ gestation death
• Significant risks with travel, especially international o In nonemergency circumstances, smallpox
travel, are infectious disease acquisition and vaccination is contraindicated during
development of complications remote from adequate pregnancy and in women who might become
resources pregnant within 28 days of vaccination
• Anthrax vaccination
F. Coitus o contains no live bacteria and thus would not
• Sexual intercourse is NOT harmful in HEALTHY be expected to pose significant fetal risk
pregnant women
• AVOID if at risk for: J. Caffeine
o Abortion • It is unclear if caffeine consumption is associated with
o Placenta previa pre- term birth or impaired fetal growth
o Preterm labor • The American College of Obstetricians and
• Intercourse late in pregnancy specifically has not been Gynecologists has concluded that moderate
found to be harmful consumption of caffeine—less than 200 mg per day—
does not appear to be associated with miscarriage or
Transcribed By: MM dela Rosa, Reina Abu Page 6 of 9
PRE-NATAL CARE
preterm birth o antacids may provide considerable relief
• The American Dietetic Association (2008) ▪ Aluminum hydroxide, magnesium
recommends that caffeine intake during pregnancy be trisilicate, or magnesium hydroxide
limited to less than 300 mg daily, or approximately alone or in combination
three 5-oz cups of percolated coffee.
O. Pica and Ptyalism
K. Nausea and Vomiting • Pica - craving of pregnant women for strange food
• Common complaints during first half of pregnancy • Craving for nonfoods such as ice—pagophagia,
• Treatment of pregnancy-associated nausea and starch— amylophagia, or clay—geophagia
vomiting seldom provides complete relief, but • If strange “foods” dominate the diet, iron deficiency will
symptoms can be minimized be aggravated or will develop eventually
• Eating small meals at more frequent intervals but • Ptyalism - profuse salivation
stopping short of satiation is valuable
• Mild symptoms: P. Sleeping and Fatigue
o vitamin B6 given along with doxylamine, • Many women experience fatigue and need increased
amounts of sleep
AND/OR
o phenothiazine or H1-receptor blocking anti- • Due to the soporific effect of progesterone but may be
compounded in the first trimester by nausea and
emetics vomiting and in the latter stages of pregnancy by
• In some, hyperemesis gravidarum develops—vomiting general discomforts, urinary frequency, and dyspnea
so severe that dehydration, may cause severe
problems Q. Leukorrhea
o Electrolyte and acid-base disturbances
• Increased mucus secretion by cervical glands in
o Starvation ketosis
response to hyperestrogenemia
L. Backache
R. Cord Blood Banking
• Back pain complaints increase with progressing • Public banks promote allogeneic donation, for use by
gestation and are more prevalent in obese women and a related or unrelated recipient, similar to blood
those with a history of low back pain product donation
• Severe pain also has other uncommon causes, such • Private banks were initially developed to store stem
as pregnancy-associated osteoporosis, disc disease, cells for future autologous use and charged fees for
vertebral osteoarthritis, or septic arthritis initial processing and annual storage
• Acute strain or Fibrositis – muscular spasm and
tenderness
• Treatment:
o Tylenol may be used chronically
o NSAIDs for short courses to avoid fetal
effects
o Muscle relaxants (cyclobenzaprine or
baclofen)
M. Varicosities and Hemorrhoids
VARICOSITIES
• Femoral venous pressures in the supine pregnant
woman increase from 8 mm Hg early to 24 mm Hg at
term
• Treatment (varicosities):
o Periodic rest with leg elevation AND/OR
o Elastic stockings
• Surgical correction is NOT ADVISED during pregnancy
• Vulvar varicosities frequently coexist with leg
varicosities, but they may appear without other venous
pathology
• If these large varicosities rupture, blood loss may be
severe
o Treatment: specially fitted pantyhose
• With particularly bothersome vulvar varicosities, a
foam rubber pad suspended across the vulva by a belt
can be used to exert pressure on the dilated veins
HEMORRHOIDS
• Hemorrhoids are rectal vein varicosities and may first
appear during pregnancy as pelvic venous pressures
increase
• Symptoms: pain and swelling relieved by topical
anesthetics, warm soaks, stool softening agents
• If with thrombosis of external hemorrhoids: incision
and removal of the clot under local analgesia
N. Heartburn
• Most common complaints of pregnant women and is
caused by gastric content reflux into the lower
esophagus
• Increased frequency of regurgitation during pregnancy
most likely results from upward displacement and
compression of the stomach by the uterus, combined
with relaxation of the lower esophageal sphincter
• Treatment:
o frequent but smaller meals
o avoidance of bending over or lying at
Transcribed By: MM dela Rosa, Reina Abu Page 7 of 9
PRE-NATAL CARE
IMMUNIZATION
Transcribed By: MM dela Rosa, Reina Abu Page 8 of 9
PRE-NATAL CARE
Transcribed By: MM dela Rosa, Reina Abu Page 9 of 9
You might also like
- Attaching in Adoption Practical Tools For Today's Parents (Deborah D. Gray)Document395 pagesAttaching in Adoption Practical Tools For Today's Parents (Deborah D. Gray)Rucsandra MurzeaNo ratings yet
- Critique PaperDocument3 pagesCritique PaperKurt Del Rosario100% (4)
- MOPON MCNDocument3 pagesMOPON MCNDannielle EvangelistaNo ratings yet
- MCH BulletsDocument13 pagesMCH BulletsPatziedawn GonzalvoNo ratings yet
- Gender Identity DisorderDocument2 pagesGender Identity DisorderAngelaTrinidadNo ratings yet
- Corporate Parenting FundmentalsDocument2 pagesCorporate Parenting FundmentalsDungani Cheembo100% (4)
- Statement Problem NSGDocument63 pagesStatement Problem NSGManjunath Kinagi83% (89)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Essential Newborn CareDocument5 pagesEssential Newborn CareElaine Iris AbastaNo ratings yet
- 19 Myths and Misconceptions About FP - 0Document3 pages19 Myths and Misconceptions About FP - 0iammerbinpransisko100% (1)
- Midterms-NCM-109-Pedia-Lec-Dean (Repaired)Document28 pagesMidterms-NCM-109-Pedia-Lec-Dean (Repaired)Drannel FajardoNo ratings yet
- Ncma219 Ob Lec: BSN 2Nd Year 2Nd Semester Prelim 2022: Bachelor of Science in Nursing 2YBDocument59 pagesNcma219 Ob Lec: BSN 2Nd Year 2Nd Semester Prelim 2022: Bachelor of Science in Nursing 2YBEARL GERALD RICAFRANCANo ratings yet
- Case StudyDocument48 pagesCase Studysimbarashe tangwadzanaNo ratings yet
- Unit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYDocument5 pagesUnit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYNancy100% (1)
- OB PEDIA Practice Questions (100 Items)Document8 pagesOB PEDIA Practice Questions (100 Items)kara.adolacion-19No ratings yet
- Integratedhealt 150201183122 Conversion Gate02 PDFDocument145 pagesIntegratedhealt 150201183122 Conversion Gate02 PDFVhince PiscoNo ratings yet
- NCM107 - Chapter 04-Lesson 3 Postpartal CareDocument22 pagesNCM107 - Chapter 04-Lesson 3 Postpartal CareJosephine LoriaNo ratings yet
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Exam 1 Midterm Study Guide OBDocument23 pagesExam 1 Midterm Study Guide OBAnnissaLarnardNo ratings yet
- 8. Care of Child With GI Dysfunction (1) ءءءءDocument44 pages8. Care of Child With GI Dysfunction (1) ءءءءNuhaNo ratings yet
- PediaDocument45 pagesPediaWilly BelloNo ratings yet
- MCN Test DrillsDocument20 pagesMCN Test DrillsFamily PlanningNo ratings yet
- NCM 104 - M6 - DOH Programs Related To Family HealthDocument4 pagesNCM 104 - M6 - DOH Programs Related To Family HealthJollan Marie Buenvenida0% (1)
- Pre and Post PregnancyDocument23 pagesPre and Post PregnancyJitendra ChaudharyNo ratings yet
- Topic: 2014 Integrated Management of Childhood IllnessDocument2 pagesTopic: 2014 Integrated Management of Childhood IllnessAndrea ValenciaNo ratings yet
- PoliomyelitisDocument57 pagesPoliomyelitisPradnya Warthe100% (1)
- Newborn ScreeningDocument20 pagesNewborn Screeningfeva55No ratings yet
- Nclex QuestionaireDocument4 pagesNclex QuestionaireJelai ParaisoNo ratings yet
- Spontaneous AbortionDocument8 pagesSpontaneous Abortionsaber_fate_11No ratings yet
- Pregnancy Induced HypertensionDocument3 pagesPregnancy Induced HypertensionunagraciaNo ratings yet
- Child Health NursingDocument3 pagesChild Health NursingVikki SinghNo ratings yet
- CHN Lab - Quiz IMCIDocument3 pagesCHN Lab - Quiz IMCIKristine KimNo ratings yet
- MCN Final ExamDocument39 pagesMCN Final ExamAshley RegisNo ratings yet
- High - Risk PregnancyDocument110 pagesHigh - Risk PregnancyAndre DityaNo ratings yet
- Essential Newborn CareDocument3 pagesEssential Newborn CareIan ParrochaNo ratings yet
- Pelvic Inflammatory DiseaseDocument18 pagesPelvic Inflammatory DiseaseVictorNo ratings yet
- NCM 101 (Continuation) Postpartal Period and PediatricsDocument29 pagesNCM 101 (Continuation) Postpartal Period and PediatricsAudi Kyle SaydovenNo ratings yet
- Chapter 19: Nutritional Needs of A NewbornDocument13 pagesChapter 19: Nutritional Needs of A NewbornAlyssaGrandeMontimorNo ratings yet
- Transient Tachypnea of NewbornsDocument16 pagesTransient Tachypnea of NewbornsSelena Marie0% (1)
- Intrapartum QuestionsDocument24 pagesIntrapartum QuestionsAnonymous ZduHBgNo ratings yet
- Imci Worksheet 1Document6 pagesImci Worksheet 1Christian PoroyNo ratings yet
- IMCI NewDocument81 pagesIMCI NewBianca de GuzmanNo ratings yet
- Prenatal Management (Part 4)Document17 pagesPrenatal Management (Part 4)Austine James Sabenicio PantiloNo ratings yet
- PREECLAMPSIADocument60 pagesPREECLAMPSIAMary Grace MasNo ratings yet
- Fundal Height ScreeningDocument10 pagesFundal Height ScreeningDr_Soranus100% (1)
- NCM 107 SL (Care of Mother, Child, Adolescent) Ballard ScoringDocument7 pagesNCM 107 SL (Care of Mother, Child, Adolescent) Ballard ScoringclrssNo ratings yet
- Example QuizDocument17 pagesExample QuizDianne LabisNo ratings yet
- Newborn ScreeningDocument23 pagesNewborn Screeningloglesb1No ratings yet
- High Risk PregnancyDocument14 pagesHigh Risk PregnancyJezrael PueblosNo ratings yet
- High Risk NewbornDocument68 pagesHigh Risk NewbornjeshemaNo ratings yet
- Antenatal CareDocument26 pagesAntenatal CarepluiedecielNo ratings yet
- Pertussis (Whooping Cough)Document14 pagesPertussis (Whooping Cough)CHALIE MEQUNo ratings yet
- A. Dystocia: Problems With PowerDocument48 pagesA. Dystocia: Problems With PowerPauline GarciaNo ratings yet
- Antenatal CareDocument27 pagesAntenatal CareFelaih Binasoy Dela CruzNo ratings yet
- Lesson Plan: S.No Objectives Content Method of Teaching/ Teaching Aid Time in Min EvaluationDocument2 pagesLesson Plan: S.No Objectives Content Method of Teaching/ Teaching Aid Time in Min EvaluationNaqash HamayunNo ratings yet
- Activity 2Document7 pagesActivity 2Karen T. CeletariaNo ratings yet
- 5 Maternal Adaptations To Pregnancy by Dr. Catherine Torres-JisonDocument75 pages5 Maternal Adaptations To Pregnancy by Dr. Catherine Torres-JisonKevin AgbonesNo ratings yet
- Prenatal Management (Part 5)Document36 pagesPrenatal Management (Part 5)Austine James Sabenicio PantiloNo ratings yet
- NCM 109 Care of Mother and Child at RiskDocument10 pagesNCM 109 Care of Mother and Child at RiskMia Fe Cuaya Lorenzo100% (1)
- DOH Maternal Health ProgramDocument5 pagesDOH Maternal Health ProgramErwin Jake TagubaNo ratings yet
- NCM 107a Care of The Pregnant WomanDocument43 pagesNCM 107a Care of The Pregnant WomanMelchizedek Tagarino Torio100% (1)
- NonStress TestDocument2 pagesNonStress TestRama_ichiNo ratings yet
- Maternal and Child Nursing 1 Skills Lab Modele s1Document3 pagesMaternal and Child Nursing 1 Skills Lab Modele s1Crystal MaidenNo ratings yet
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Urine Strips - 1676637648Document1 pageUrine Strips - 1676637648AngelaTrinidadNo ratings yet
- Pterygium & DacryocystitisDocument45 pagesPterygium & DacryocystitisAngelaTrinidadNo ratings yet
- Chronic DiseasesDocument24 pagesChronic DiseasesAngelaTrinidadNo ratings yet
- Cream Modern Vision & Mission PosterDocument2 pagesCream Modern Vision & Mission PosterAngelaTrinidadNo ratings yet
- Varicella Post-ProphylaxisDocument2 pagesVaricella Post-ProphylaxisAngelaTrinidadNo ratings yet
- IRB Roles For ReferenceDocument33 pagesIRB Roles For ReferenceAngelaTrinidadNo ratings yet
- Casestudy Gastric CarcinomaDocument53 pagesCasestudy Gastric CarcinomaAngelaTrinidadNo ratings yet
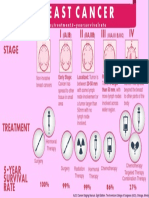
- Breast Cancer InfogrpahicDocument1 pageBreast Cancer InfogrpahicAngelaTrinidadNo ratings yet
- Ditas Cristina D Decena MD MPH: Recomendation For Preventing Exposure To Toxic ChemicalsDocument29 pagesDitas Cristina D Decena MD MPH: Recomendation For Preventing Exposure To Toxic ChemicalsAngelaTrinidadNo ratings yet
- Minimally Invasive Surgery (Mis) : Roberto O. Domingo, M.D.,FPCSDocument51 pagesMinimally Invasive Surgery (Mis) : Roberto O. Domingo, M.D.,FPCSAngelaTrinidadNo ratings yet
- Pharma - M6L2 - Drug Therapy For OA and Gouty ArthritisDocument8 pagesPharma - M6L2 - Drug Therapy For OA and Gouty ArthritisAngelaTrinidadNo ratings yet
- San Beda College of Medicine Batch 2017 Neuro-Pedia ChecklistDocument9 pagesSan Beda College of Medicine Batch 2017 Neuro-Pedia ChecklistAngelaTrinidadNo ratings yet
- Sample Case 1Document4 pagesSample Case 1AngelaTrinidadNo ratings yet
- Neuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansDocument29 pagesNeuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansAngelaTrinidad100% (2)
- Trinidad, Alyssa Angela ADocument4 pagesTrinidad, Alyssa Angela AAngelaTrinidadNo ratings yet
- NCPDocument6 pagesNCPAngelaTrinidadNo ratings yet
- Preoperative Evaluation HandoutDocument2 pagesPreoperative Evaluation HandoutAngelaTrinidadNo ratings yet
- RRL Hypertension ComplianceDocument30 pagesRRL Hypertension ComplianceAngelaTrinidadNo ratings yet
- Examination of Cerebellum and MeningesDocument4 pagesExamination of Cerebellum and MeningesAngelaTrinidadNo ratings yet
- Introduction To EpidemiologyDocument10 pagesIntroduction To EpidemiologyAngelaTrinidadNo ratings yet
- Broncho FinalDocument11 pagesBroncho FinalAngelaTrinidadNo ratings yet
- State of Our HeartsDocument5 pagesState of Our HeartsAngelaTrinidadNo ratings yet
- CHEM 11.1/2: General Chemistry I (Laboratory)Document1 pageCHEM 11.1/2: General Chemistry I (Laboratory)AngelaTrinidadNo ratings yet
- EVS Lesson 4 Ans 5.... Book and Copy WorkDocument10 pagesEVS Lesson 4 Ans 5.... Book and Copy WorkArpita AgarwalNo ratings yet
- Maternal and Child Chapter 6 (Margot-Desevo)Document12 pagesMaternal and Child Chapter 6 (Margot-Desevo)Jesse ParkNo ratings yet
- Lesson 3 Stages of Development and Developmental TasksDocument23 pagesLesson 3 Stages of Development and Developmental TasksMary Ann MendezNo ratings yet
- Reading - Types of FamiliesDocument3 pagesReading - Types of FamiliesFernanda SalesNo ratings yet
- Alim Lesson Assesment 2021 Eng 1stDocument2 pagesAlim Lesson Assesment 2021 Eng 1stJibbul KayesNo ratings yet
- Solved CMAT 2019 Question Paper Paper With SolutionsDocument39 pagesSolved CMAT 2019 Question Paper Paper With SolutionsŘohan DhakalNo ratings yet
- The Lived Experiences of The Selected Middle Children in Senior High School in A Private SchoolDocument10 pagesThe Lived Experiences of The Selected Middle Children in Senior High School in A Private SchoolPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Stephenie Rascol ResumeDocument2 pagesStephenie Rascol Resumeapi-335892001No ratings yet
- Child DevelopmentDocument11 pagesChild DevelopmentRose Ann Baloloy PayteNo ratings yet
- Parenting Strong-Willed ChildDocument126 pagesParenting Strong-Willed ChildMarianaNo ratings yet
- PPH Case StudyDocument76 pagesPPH Case StudyDhanashree Anil Pore100% (33)
- Module 3 - Developmental Stages in Middle and Late AdolescenceDocument42 pagesModule 3 - Developmental Stages in Middle and Late AdolescenceJaymark AgsiNo ratings yet
- Blood Relations: Click To Add TextDocument50 pagesBlood Relations: Click To Add TextVaishu GoudNo ratings yet
- PartogramDocument20 pagesPartogramKasumba ChandaNo ratings yet
- Coping With TantrumsDocument25 pagesCoping With TantrumsAlex Bojovic100% (1)
- 5.1.7 Anaemia in Pregnancy - MauwaDocument17 pages5.1.7 Anaemia in Pregnancy - MauwaSetlhare MotsamaiNo ratings yet
- Little Boy Calls 911 For Math Homework HelpDocument9 pagesLittle Boy Calls 911 For Math Homework Helpafesbibdy100% (1)
- Bnap (New) 2020Document1 pageBnap (New) 2020Jomalyn punzalanNo ratings yet
- Baby Friendly Hospital Initiative: by Nadia Fitra RahmaDocument6 pagesBaby Friendly Hospital Initiative: by Nadia Fitra RahmaNadya Fitra RahmaNo ratings yet
- Common Look UpsDocument1,491 pagesCommon Look Upsbalasuk0% (1)
- OB 2.01 - Hypertensive Disorders in PregnancyDocument5 pagesOB 2.01 - Hypertensive Disorders in PregnancyvetinaNo ratings yet
- EE Final 1Document19 pagesEE Final 1bturanNo ratings yet
- Surprise PassengerDocument2 pagesSurprise PassengerMontalvan EmiNo ratings yet
- What's A Midlife CrisisDocument1 pageWhat's A Midlife CrisisНовак КнежевићNo ratings yet
- Adopted (5e Background) - D&D WikiDocument1 pageAdopted (5e Background) - D&D WikiX itaNo ratings yet
- On The Psychogenesis of Homosexuality: Gerard J.M. Van Den Aardweg, PH.DDocument25 pagesOn The Psychogenesis of Homosexuality: Gerard J.M. Van Den Aardweg, PH.DCamilo GallegoNo ratings yet