Professional Documents
Culture Documents
Maternal Obesity and The Risk of Early Onset And.21
Uploaded by
marinanananaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternal Obesity and The Risk of Early Onset And.21
Uploaded by
marinanananaCopyright:
Available Formats
Original Research
Maternal Obesity and the Risk of Early-Onset
and Late-Onset Hypertensive Disorders
of Pregnancy
Matthew J. Bicocca, MD, Hector Mendez-Figueroa, MD, Suneet P. Chauhan, MD, Hon DSc,
Downloaded from https://journals.lww.com/greenjournal by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Le0ic6pTQVAkPIHH+KGau1fYAsMZPhRTKQ0n/B1TNmMoNjN2DHeqLg== on 07/11/2020
and Baha M. Sibai, MD
OBJECTIVE: To evaluate the relationship between tensive disorders of pregnancy was significantly higher in
maternal body mass index (BMI) at delivery and rates women with class 1 obesity (aRR 1.13; 95% CI 1.10–1.16),
of early-onset and late-onset hypertensive disorders of class 2 obesity (aRR 1.57; 95% CI 1.53–1.62), and class 3
pregnancy. obesity (aRR 2.18; 95% CI 2.12–2.24), compared with
METHODS: We performed a population-based, retro- nonobese women. The risk of late-onset hypertensive
spective cohort study using U.S. Vital Statistics period- disorders of pregnancy was also significantly increased
linked birth and infant death certificates from 2014 to in women with class 1 obesity (aRR 1.71; 95% CI 1.70–
2017. Women who delivered a nonanomalous singleton 1.73), class 2 obesity (aRR 2.60; 95% CI 2.58–2.62), and
live neonate from 24 to 41 completed weeks of gestation class 3 obesity (aRR 3.93; 95% CI 3.91–3.96) compared
were included. We excluded women with chronic hyper- with nonobese women.
tension and those with BMIs less than 18.5. The primary CONCLUSION: Compared with nonobese women, the
exposure was maternal BMI, defined as nonobese (BMI risk of early-onset and late-onset hypertensive disorders
18.5–29.9; referent group), class 1 obesity (BMI 30.0– of pregnancy is significantly and progressively increased
34.9), class 2 obesity (BMI 35.0–39.9), and class 3 obesity among women with increased class of obesity.
(BMI 40.0 or greater). The primary outcome was delivery (Obstet Gynecol 2020;136:118–27)
with hypertensive disorders of pregnancy (gestational DOI: 10.1097/AOG.0000000000003901
hypertension, preeclampsia, or eclampsia) at less than
H
34 weeks of gestation or at 34 weeks or more. Multivari-
ypertensive disorders of pregnancy, which in-
able Poisson regression was used to estimate relate risk
cludes gestational hypertension, preeclampsia,
and adjust for confounding variables. Results are pre-
and eclampsia, affect 4–8% of pregnancies and are
sented as adjusted relative risk (aRR) and 95% CIs.
a leading cause of maternal and neonatal morbid-
RESULTS: Of the 15.8 million women with live births ity.1–3 In developed nations, preeclampsia is associ-
during the study period, 14.0 million (88.6%) met
ated with a doubling in the rate of adverse neonatal
inclusion criteria, and 825,722 (5.9%) had hypertensive
events, including sepsis, seizures and neonatal
disorders of pregnancy. The risk of early-onset hyper-
death,4,5 and is responsible for 16% of maternal
deaths.6
From the Department of Obstetrics, Gynecology and Reproductive Sciences, One contemporary view of hypertensive disor-
McGovern Medical School, University of Texas Health Science Center at
Houston, Houston, Texas. ders of pregnancy differentiates two disease subtypes:
Each author has confirmed compliance with the journal’s requirements for
early-onset and late-onset.7–9 Early-onset disease (less
authorship. than 34 weeks of gestation) constitutes 5–10% of
Corresponding author: Matthew J. Bicocca, MD, Department of Obstetrics, hypertensive disorders of pregnancy and is associated
Gynecology and Reproductive Sciences, McGovern Medical School, University of with a fivefold increased risk of perinatal death2 and
Texas Health Science Center at Houston, Houston, TX; email: a twofold to fourfold increased risk of severe cardio-
matthew.bicocca@uth.tmc.edu.
vascular, renal, or hepatic maternal morbidity com-
Financial Disclosure
The authors did not report any potential conflicts of interest. pared with late-onset disease (34 weeks of gestation
© 2020 by the American College of Obstetricians and Gynecologists. Published
or more).3 Early-onset and late-onset hypertensive
by Wolters Kluwer Health, Inc. All rights reserved. disorders of pregnancy share multiple risk factors,
ISSN: 0029-7844/20 including nulliparity, multiple gestation, advancing
118 VOL. 136, NO. 1, JULY 2020 OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
maternal age, African American race, chronic hyper- Our primary outcome was the diagnosis of
tension, and diabetes mellitus.2,10–12 Although obesity hypertensive disorders of pregnancy, which included
is an established risk factor for late-onset disease,6,13–16 any of the following: gestational hypertension, pre-
there are conflicting reports about the link between eclampsia without severe features, preeclampsia with
maternal body mass index (BMI, calculated as weight severe features, and eclampsia. The 2003 birth certif-
in kilograms divided by height in meters squared) and icate revision does not include preeclampsia as
early-onset hypertensive disorders of pregnancy.17–24 a separately reported condition, and all women with
The incongruencies in the literature regarding gestational hypertension or preeclampsia were classi-
obesity and early-onset hypertensive disorders of fied as gestational hypertension.26 Eclampsia was re-
pregnancy may be attributable to sample size, because corded as a separate variable. Chronic hypertension
early-onset hypertensive disorders of pregnancy is was mutually exclusive with gestational hypertension,
uncommon. We therefore undertook this analysis making delineation of superimposed preeclampsia
using U.S. Vital Statistics data with the objective of unfeasible. To account for this limitation, all women
ascertaining whether the rate of early-onset and late- with chronic hypertension were excluded from our
onset hypertensive disorders of pregnancy is signifi- analysis. Additionally, we considered all women with
cantly higher among obese women compared with eclampsia to have a hypertensive disorder of preg-
nonobese women. nancy, regardless of an independent diagnosis of ges-
tational hypertension.
METHODS Our primary exposure was maternal BMI at
We performed a population-based, retrospective delivery as a categorical variable. Body mass index
cohort study using U.S. Vital Statistics period-linked was divided into four mutually exclusive categories
birth and infant death certificates from 2014 to 2017. based on the World Health Organization BMI classi-
The data are compiled annually by the U.S. Center fication: 18.5–29.9 (reference), 30.0–34.9 (class 1 obe-
for Health Statistics and undergo unified coding and sity), 35.0–39.9 (class 2 obesity), and 40.0 or greater
quality control before public release by the Centers (class 3 obesity).28 Comparisons among groups were
for Disease Control and Prevention. The methodol- made using Poisson regression with robust error var-
ogy for establishing the national linked record file is iance to estimate relative risk. Multivariate regression
discussed in the annual user guide, along with variable was performed to control for maternal age (younger
definitions.25 The data are de-identified and deemed than 18, 18–34, 35 years or older); race and ethnicity
exempt by the Institutional Review Board of the Uni- (non-Hispanic white, non-Hispanic black, Hispanic,
versity of Texas Health Science Center at Houston Asian, other or unknown); education (less than high
(IRB HSC-MS-16-0931). We included all singleton school, high school or more, unknown); marital status
pregnancies delivering from 24 to 41 completed (married, single, unknown); prenatal care (yes, no,
weeks of gestation. Exclusion criteria were chronic unknown); smoking during pregnancy (yes, no,
hypertension, major fetal anomalies, missing hyper- unknown); nulliparity (yes, no); diabetes (gestational
tension or diabetes status, missing maternal height or pregestational); maternal weight gain (above Insti-
or weight, maternal height 48 inches or less, or mater- tute of Medicine [IOM, now known as the National
nal BMI less than 18.5. Academy of Medicine] recommendations, not above
The demographic and outcome data collected by IOM recommendations); and birth year. Missing or
birth and infant death certificates have undergone unknown values were included in the analysis as an
multiple revisions. The 2003 revision replaced the additional group of their respective covariate. Results
1989 revision, but uptake has been gradual and varied are presented as adjusted relative risks (aRR) with
across the United States. Fewer than 4% of births in 95% CIs. The relationship between hypertensive dis-
2014 used the 1989 revision, decreasing to 1.7% by orders of pregnancy and increasing BMI class was
2015. In 2016 and 2017, the 2003 revision was used assessed using Spearman’s correlation coefficient in
exclusively. By limiting our analysis to births from our crude and adjusted Poisson regression models.
2014 to 2017 reported using the 2003 revision, we The sample size for this analysis was determined
sought to minimize the variations in reported demo- by the number of participants in the database. The
graphics and outcomes,26 and also to standardize the analysis was stratified by gestational age at delivery:
diagnosis of hypertensive disease after the release of early-onset (less than 34 weeks of gestation) compared
the Hypertension in Pregnancy Task Force Report by with late-onset (34 weeks of gestation or more).
the American College of Obstetricians and Gynecol- Gestational age reported in the birth registry was
ogists in November 2013.27 established using the National Center for Health
VOL. 136, NO. 1, JULY 2020 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia 119
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
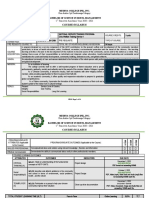
Fig. 1. Flowchart of patient eligibility. *Items not mutually exclusive. BMI, body mass index.
Bicocca. Obesity and Early-Onset vs Late-Onset Preeclampsia. Obstet Gynecol 2020.
Statistics obstetric estimate of gestation at delivery, gestational diabetes. The results are similarly pre-
a technique previously described and shown to sented as aRR (95% CI). All statistics were performed
correlate more accurately with early ultrasound esti- using Stata 16. The STROBE (Strengthening the
mations than use of last menstrual period alone.29,30 Reporting of Observational Studies in Epidemiology)
Rates of hypertensive disorders of pregnancy were guidelines for reporting observational studies were
calculated by analysis of all eligible pregnancies at followed.31
the beginning of the gestational age period of interest.
For early-onset hypertensive disorders of pregnancy, RESULTS
we analyzed all eligible women who delivered from Of the 15,818,980 births between 2014 and 2017,
24 to 41 completed weeks of gestation thus considered 14,018,228 (88.6%) were included in the analysis (Fig.
at-risk for developing the disease. The primary out- 1). Among eligible births, 6,436,936 (45.9%) were
come was defined as delivery before 34 weeks of ges- nonobese, 4,042,052 (28.8%) had class 1 obesity,
tation with a diagnosis of hypertensive disorders of 2,094,140 (14.9%) had class 2 obesity, and 1,445,100
pregnancy. For late-onset hypertensive disorders of (10.3%) had class 3 obesity. The overall rate of hyper-
pregnancy, only women delivering from 34 to 41 tensive disorders of pregnancy was 5.9%, divided
week were analyzed, and any diagnosis of hyperten- between early-onset (0.3%) and late-onset (5.6%).
sive disorders of pregnancy was considered a positive There were statistically significant differences
finding. The analysis was then repeated with cohorts across BMI groups for all measured characteristics
subdivided into gestational age ranges of 24–27, 28– (Table 1). Rates of both gestational and pregestational
30, 31–33, 34–36, and 37–41 weeks of gestation. diabetes increased progressively from 3.8% and 0.4%
To examine the association of maternal BMI on in the nonobese group to 11.0% and 1.9% in the class
hypertensive disorders of pregnancy independent of 3 obesity group, respectively. Rates of gestational
diabetes status, a sensitivity analysis was performed weight gain above IOM recommendations were lower
which excluded all women with gestational or pre- in the nonobese group (40.2%), compared with all
120 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 1. Maternal Characteristics
BMI (kg/m2)
Total 18.5–29.9 30.0–34.9 35.0–39.9 40.0 or Higher
Characteristic (N514,018,228) (n56,436,936) (n54,042,052) (n52,094,140) (n51,445,100) P
Age (y) ,.001
Younger than 18 220,334 (1.6) 129,481 (2.0) 56,149 (1.4) 23,514 (1.1) 11,190 (0.8)
18–34 11,557,594 (82.5) 5,289,178 (82.2) 3,315,209 (82.0) 1,739,971 (83.1) 1,213,236 (84.0)
35 or older 2,240,300 (16.0) 1,018,277 (15.8) 670,694 (16.6) 330,655 (15.8) 220,674 (15.3)
Race and ethnicity ,.001
Non-Hispanic white 7,363,523 (52.5) 3,515,325 (54.6) 2,071,486 (51.3) 1,053,488 (50.3) 723,224 (50.1)
Non-Hispanic black 1,906,260 (13.6) 726,735 (11.3) 539,922 (13.4) 342,841 (16.4) 296,762 (20.5)
Hispanic 3,322,277 (23.7) 1,347,708 (20.9) 1,075,194 (26.6) 557,093 (26.6) 342,282 (23.7)
Asian 888,438 (6.3) 621,614 (9.7) 201,925 (5.0) 50,498 (2.4) 14,401 (1.0)
Other or unknown 537,730 (3.8) 225,554 (3.5) 153,525 (3.8) 90,220 (4.3) 68,431 (4.7)
Education ,.001
Less than high school 1,961,221 (14.0) 881,890 (13.7) 582,277 (14.4) 298,813 (14.3) 198,241 (13.7)
High school or more 11,906,958 (84.9) 5,479,259 (85.1) 3,417,124 (84.5) 1,775,535 (84.8) 1,235,040 (85.5)
Unknown 150,049 (1.1) 75,787 (1.2) 42,651 (1.1) 19,792 (1.0) 11,819 (0.8)
Marital status ,.001
Married 8,146,769 (58.1) 3,926,560 (61) 2,354,234 (58.2) 1,135,486 (54.2) 730,489 (50.6)
Not married 5,436,071 (38.8) 2,301,995 (35.8) 1,560,798 (38.6) 896,458 (42.8) 676,820 (46.8)
Unknown 435,388 (3.1) 208,381 (3.2) 127,020 (3.1) 62,196 (3.0) 37,791 (2.6)
Prenatal care ,.001
Yes 13,535,845 (96.6) 6,191,612 (96.2) 3,913,577 (96.8) 2,029,507 (96.9) 1,401,149 (97.0)
No 186,539 (1.3) 99,826 (1.6) 47,648 (1.2) 23,352 (1.1) 15,713 (1.1)
Unknown 295,844 (2.1) 145,498 (2.3) 80,827 (2.0) 41,281 (2.0) 28,238 (2.0)
Smoking during ,.001
pregnancy
Yes 1,042,618 (7.4) 470,041 (7.3) 277,069 (6.9) 165,514 (7.9) 129,994 (9.0)
No 12,877,840 (91.9) 5,920,087 (92.0) 3,737,682 (92.5) 1,914,727 (91.4) 1,305,344 (90.3)
Unknown 97,770 (0.7) 46,808 (0.7) 27,301 (0.7) 13,899 (0.7) 9,762 (0.7)
Nulliparous 4,481,021 (32.0) 2,219,619 (34.5) 1,237,827 (30.6) 607,736 (29.0) 415,839 (28.8) ,.001
Weight gain above IOM 8,106,409 (57.8) 2,586,426 (40.2) 2,996,656 (74.1) 1,537,319 (73.4) 986,008 (68.2) ,.001
recommendations
Gestational diabetes 796,898 (5.7) 245,632 (3.8) 226,781 (5.6) 165,341 (7.9) 159,144 (11.0) ,.001
Pregestational diabetes 99,611 (0.7) 22,579 (0.4) 26,541 (0.7) 22,812 (1.1) 27,679 (1.9) ,.001
Delivery year ,.001
2014 3,434,220 (24.5) 1,610,602 (25.0) 981,899 (24.3) 500,302 (23.9) 341,417 (23.6)
2015 3,518,902 (25.1) 1,628,367 (25.3) 1,010,781 (25.0) 521,663 (24.9) 358,091 (24.8)
2016 3,569,801 (25.5) 1,628,855 (25.3) 1,032,717 (25.6) 537,298 (25.7) 370,931 (25.7)
2017 3,495,305 (24.9) 1,569,112 (24.4) 1,016,655 (25.2) 534,877 (25.5) 374,661 (25.9)
BMI, body mass index; IOM, Institute of Medicine (now known as the National Academy of Medicine).
Data are n (%) unless otherwise specified.
classes of obesity (74.1%, 73.4%, and 68.2% for classes pregnancy compared with nonobese women. When
1, 2 and 3, respectively). women with diabetes were excluded from the analy-
The relative risk of early-onset hypertensive sis, the absolute rates of hypertensive disorders of
disorders of pregnancy was significantly and pro- pregnancy decreased across all BMI classes; however,
gressively increased among women with class 1, class the adjusted and unadjusted relative risks remained
2, and class 3 obesity compared with nonobese similar (Table 2).
women (Tables 2 and 3). After adjusting for potential When gestational ages were subdivided, the rates
confounders, the increases remained significant. For of hypertensive disorders of pregnancy increased
late-onset disease, the increased risk of hypertensive across all BMI groups with increasing gestational
disorders of pregnancy was more pronounced, as class age (Fig. 2 and Table 3). Higher levels of obesity were
3 obese women had an approximately fourfold associated with increased rates of hypertensive disor-
increased risk of late-onset hypertensive disorders of ders of pregnancy, a consistent trend across all
VOL. 136, NO. 1, JULY 2020 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia 121
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 2. Rate of Delivery With Hypertensive Disorders of Pregnancy, Early-Onset Compared With Late-
Onset
BMI Total Live Rate/1,000 Live Unadjusted RR Adjusted RR Adjusted RR
Onset (kg/m2) Births n Births (95% CI) (95% CI) (95% CI)*
Early Total 14,018,228 48,007 3.42 (3.39–3.46)
18.5–29.9 6,436,936 15,430 2.40 (2.36–2.44) 1.00 1.00 1.00
(ref)
30.0–34.9 4,042,052 12,781 3.16 (3.11–3.22) 1.32 (1.29–1.35) 1.13 (1.10–1.16) 1.14 (1.11–1.17)
35.0–39.9 2,094,140 9,761 4.66 (4.57–4.75) 1.94 (1.90–1.99) 1.57 (1.53–1.62) 1.61 (1.56–1.66)
40.0 or 1,445,100 10,035 6.94 (6.81–7.08) 2.90 (2.83–2.97) 2.18 (2.12–2.24) 2.25 (2.19–2.32)
higher
Late Total 13,970,221 777,715 55.7 (55.6–55.8)
18.5–29.9 6,421,506 186,630 29.1 (28.9–29.2) 1.00 1.00 1.00
(ref)
30.0–34.9 4,029,271 221,105 54.9 (54.7–55.1) 1.88 (1.87–1.89) 1.71 (1.70–1.73) 1.72 (1.71–1.73)
35.0–39.9 2,084,379 177,774 85.3 (84.9–85.7) 2.92 (2.90–2.94) 2.60 (2.58–2.62) 2.64 (2.62–2.66)
40.0 or 1,435,065 192,206 133.9 (133.4–134.5) 4.59 (4.56–4.62) 3.93 (3.91–3.96) 4.04 (4.01–4.07)
higher
BMI, body mass index; RR, relative risk; ref, referent.
Adjusted for maternal age, race and ethnicity, education, marital status, prenatal care, smoking during pregnancy, nulliparity, diabetes,
maternal weight gain, and birth year.
Bold indicates significant difference.
* Excluding women with gestational or pregestational diabetes.
Table 3. Rate of Hypertensive Disorders of Pregnancy per 1,000 Live Births
Gestational Unadjusted RR Adjusted RR
Age (wk) BMI (kg/m2) Total Live Births n Rate/1,000 Live Births (95% CI) (95% CI)
24–27 Total 14,018,228 6,554 0.47 (0.46–0.48)
18.5–29.9 (ref) 6,436,936 2,337 0.36 (0.35–0.38) 1.00 1.00
30.0–34.9 4,042,052 1,678 0.42 (0.40–0.44) 1.14 (1.07–1.22) 1.03 (0.96–1.11)
35.0–39.9 2,094,140 1,278 0.61 (0.58–0.64) 1.68 (1.57–1.80) 1.43 (1.33–1.55)
40.0 or higher 1,445,100 1,261 0.87 (0.83–0.92) 2.40 (2.24–2.57) 1.91 (1.77–2.06)
28–30 Total 14,011,674 12,209 0.87 (0.86–0.89)
18.5–29.9 (ref) 6,434,599 4,090 0.64 (0.62–0.66) 1.00 1.00
30.0–34.9 4,040,374 3,237 0.80 (0.77–0.83) 1.26 (1.20–1.32) 1.08 (1.02–1.13)
35.0–39.9 2,092,862 2,435 1.16 (1.12–1.21) 1.83 (1.74–1.92) 1.48 (1.41–1.57)
40.0 or higher 1,443,839 2,447 1.69 (1.63–1.76) 2.66 (2.53–2.80) 2.03 (1.93–2.15)
31–33 Total 13,999,465 29,244 2.09 (2.07–2.11)
18.5–29.9 (ref) 6,430,509 9,003 1.40 (1.37–1.43) 1.00 1.00
30.0–34.9 4,037,137 7,866 1.95 (1.91–1.99) 1.39 (1.35–1.43) 1.18 (1.14–1.22)
35.0–39.9 2,090,427 6,048 2.89 (2.82–2.97) 2.06 (2.00–2.13) 1.65 (1.59–1.70)
40.0 or higher 1,441,392 6,327 4.39 (4.28–4.50) 3.13 (3.03–3.23) 2.31 (2.23–2.39)
34–36 Total 13,970,221 115,762 2.09 (2.07–2.11)
18.5–29.9 (ref) 6,421,506 30,501 4.75 (4.70–4.80) 1.00 1.00
30.0–34.9 4,029,271 31,183 7.74 (7.65–7.83) 1.62 (1.59–1.65) 1.38 (1.36–1.40)
35.0–39.9 2,084,379 25,223 12.1 (12.0–12.2) 2.54 (2.49–2.58) 2.03 (1.99–2.07)
40.0 or higher 1,435,065 28,855 20.1 (19.9–20.3) 4.22 (4.15–4.28) 3.12 (3.07–3.18)
37–41 Total 13,854,459 661,953 47.8 (47.7–47.9)
18.5–29.9 (ref) 6,391,005 156,129 24.4 (24.3–24.6) 1.00 1.00
30.0–34.9 3,998,088 189,922 47.5 (47.3–47.7) 1.91 (1.90–1.92) 1.76 (1.75–1.77)
35.0–39.9 2,059,156 152,551 74.1 (73.7–74.4) 2.98 (2.96–3.00) 2.69 (2.67–2.71)
40.0 or higher 1,406,210 163,351 116.2 (115.6–116.7) 4.69 (4.66–4.72) 4.10 (4.07–4.13)
BMI, body mass index; RR, relative risk; ref, referent.
Adjusted for maternal age, race and ethnicity, education, marital status, prenatal care, smoking during pregnancy, nulliparity, diabetes,
maternal weight gain, and birth year.
Bold indicates significant difference.
122 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 4. Rate of Hypertensive Disorders of Pregnancy per 1,000 Live Births, Excluding Women With
Gestational and Pregestational Diabetes
Gestational Rate/1,000 Unadjusted RR Adjusted RR
Age (wk) BMI (kg/m2) Total Live Births n Live Births (95% CI) (95% CI)
24–27 Total 13,121,719 5,973 0.46 (0.44–0.47)
18.5–29.9 (ref) 6,168,725 2,209 0.36 (0.34–0.37) 1.00 1.00
30.0–34.9 3,788,730 1,539 0.41 (0.39–0.43) 1.13 (1.06–1.21) 1.03 (0.96–1.11)
35.0–39.9 1,905,987 1,136 0.60 (0.56–0.63) 1.66 (1.55–1.79) 1.44 (1.34–1.56)
40.0 or higher 1,258,277 1,089 0.87 (0.81–0.92) 2.42 (2.25–2.60) 1.97 (1.82–2.13)
28–30 Total 13,115,746 10,830 0.83 (0.81–0.84)
18.5–29.9 (ref) 6,166,516 3,806 0.62 (0.60–0.64) 1.00 1.00
30.0–34.9 3,787,191 2,885 0.76 (0.73–0.79) 1.23 (1.17–1.29) 1.08 (1.02–1.13)
35.0–39.9 1,904,851 2,122 1.11 (1.07–1.16) 1.80 (1.71–1.90) 1.52 (1.44–1.61)
40.0 or higher 1,257,188 2,017 1.60 (1.54–1.68) 2.60 (2.46–2.74) 2.11 (1.99–2.24)
31–33 Total 13,104,916 24,382 1.86 (1.84–1.88)
18.5–29.9 (ref) 6,162,710 8,069 1.31 (1.28–1.34) 1.00 1.00
30.0–34.9 3,784,306 6,702 1.77 (1.73–1.81) 1.35 (1.31–1.39) 1.19 (1.15–1.23)
35.0–39.9 1,902,729 4,912 2.58 (2.51–2.65) 1.97 (1.90–2.04) 1.69 (1.63–1.76)
40.0 or higher 1,255,171 4,699 3.74 (3.64–3.85) 2.86 (2.76–2.96) 2.40 (2.31–2.49)
34–36 Total 13,080,534 92,661 7.08 (7.04–7.13)
18.5–29.9 (ref) 6,154,641 27,098 4.40 (4.35–4.46) 1.00 1.00
30.0–34.9 3,777,604 25,858 6.85 (6.76–6.93) 1.55 (1.52–1.57) 1.39 (1.36–1.41)
35.0–39.9 1,897,817 19,583 10.3 (10.2–10.5) 2.33 (2.29–2.37) 2.06 (2.02–2.11)
40.0 or higher 1,250,472 20,122 16.1 (15.9–16.3) 3.64 (3.57–3.71) 3.19 (3.13–3.25)
37–41 Total 12,987,873 577,488 44.5 (44.4–44.6)
18.5–29.9 (ref) 6,127,543 144,150 23.5 (23.4–23.7) 1.00 1.00
30.0–34.9 3,751,746 169,826 45.3 (45.1–45.5) 1.89 (1.88–1.90) 1.77 (1.75–1.78)
35.0–39.9 1,878,234 131,238 69.9 (69.5–70.2) 2.92 (2.90–2.94) 2.73 (2.71–2.75)
40.0 or higher 1,230,350 132,274 107.5 (107.0–108.1) 4.50 (4.46–4.53) 4.20 (4.17–4.23)
BMI, body mass index; RR, relative risk; ref, referent.
Adjusted for maternal age, race and ethnicity, education, marital status, prenatal care, smoking during pregnancy, nulliparity, diabetes,
maternal weight gain, and birth year.
Bold indicates significant difference.
gestational ages. After adjusting for potential con- prior publications,17,18,21,24 as was the prevalence
founding variables, the aRR of hypertensive disorders of late-onset disease (55.7/1,000).17,21,24
of pregnancy was significantly increased for all BMI The pathophysiology underlying early-onset
groups at all gestational ages except class 1 obesity at hypertensive disorders of pregnancy may be distinct
24–27 weeks of gestation (Fig. 3 and Table 3). The from late-onset hypertensive disorders of pregnancy,
same pattern persisted when patients with diabetes which contributes to uncertainty regarding the role of
were excluded from the analysis (Table 4). obesity. In early-onset disease, abnormal placentation
putatively results in chronic uteroplacental insuffi-
DISCUSSION ciency, focal ischemia, and the eventual release of
Among a nationwide cohort of women, we noted that inflammatory cytokines resulting in systemic maternal
increasing levels of maternal obesity are associated hypertension.9,32,33 Conversely, late-onset hyperten-
with progressively increased risk of both early-onset sive disorders of pregnancy may be secondary to an
and late-onset hypertensive disorders of pregnancy. underlying placental insufficiency coupled with
This risk remained after adjustment for potential chronic oxidative stress from maternal metabolic de-
confounders such as maternal age, race, or nullipar- rangements such as obesity and insulin resistance.7,9,32
ity or when excluding patients with a synergistic Body mass index is therefore linked primarily with
disease process such as diabetes. Moreover, the late-onset hypertensive disorders of pregnancy, and
increased risk of hypertensive disorders of preg- its role in early-onset disease is inconsistently
nancy was evident as early as 24–27 weeks of gesta- described.
tion among women with class 2 and class 3 obesity. Previous retrospective work by Ornaghi et al22
Our observed rate of early-onset hypertensive disor- examined risk factors for early-onset and late-onset
ders of pregnancy (3.2/1,000) was consistent with hypertensive disorders of pregnancy and found BMI
VOL. 136, NO. 1, JULY 2020 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia 123
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Fig. 2. Rate of hypertensive dis-
orders of pregnancy by body mass
index (BMI) and gestational age.
Bicocca. Obesity and Early-Onset vs
Late-Onset Preeclampsia. Obstet Gyne-
col 2020.
35.0 or greater to be an influencing factor only for women with BMIs of 30.0 or greater, with a similar
late-onset disease in a cohort of 284 women with trend for early-onset hypertensive disorders of preg-
preeclampsia. Similar findings were reported by nancy (adjusted odds ratio 4.07; 95% CI 0.81–20.42)
Poon et al in a cohort of women with early-onset that was not statistically significant.20 A larger
preeclampsia, late-onset preeclampsia, and gesta- cohort study by Durst et al of 10,196 women exam-
tional hypertension, although they used a BMI cut- ined BMI as a risk factor for preeclampsia with
off of 30.0.23 A smaller study by Fang et al severe features. They reported an increased risk of
compared 150 women with preeclampsia (29 with early-onset severe preeclampsia only in morbidly
early-onset) with normotensive women in a control obese women (BMI 40.0 or more) but increased
group. In agreement with our data, they noted a sig- rates of late-onset disease in all overweight and
nificant increase in risk of late-onset disease in obese patients.19
Fig. 3. Results adjusted for maternal
age, race and ethnicity, education,
marital status, prenatal care, smok-
ing during pregnancy, nulliparity,
diabetes, gestational weight gain,
and birth year. Error bars represent
95% CIs. Body mass index (BMI) of
18.5–29.9 kg/m2 used as referent
group.
Bicocca. Obesity and Early-Onset vs
Late-Onset Preeclampsia. Obstet Gyne-
col 2020.
124 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Consistent with other large, population-based effect of obesity in both early-onset and late-onset
studies, we note an association between both early- hypertensive disorders of pregnancy.
onset and late-onset hypertensive disorders of preg- We also acknowledge limitations in our study.
nancy. Using Missouri birth certificate data Maternal comorbidities within the U.S. Vital Statistics
(n5854,085), Mbah et al21 showed the risk of early- database are limited to diabetes and hypertension, and
onset and late-onset preeclampsia progressively there is a possibility of unmeasured confounding
increased with increasing levels of obesity. Their disease processes. Preeclampsia and gestational
adjusted odds ratios were similar to our reported hypertension could not be separately analyzed and
aRRs across all obesity classes, and differences in patients with chronic hypertension had to be excluded
reference groups (BMI 18.5–24.9 vs 18.5–29.9) and as previously discussed. Additionally, we were limited
their use of prepregnancy BMI likely accounts for to gestational age at delivery and could not ascertain
a portion of the observed discrepancy. Sohlberg gestational age at diagnosis of hypertensive disorders
et al24 reported similar findings among Swedish of pregnancy. It is therefore probable that some
women with term preeclampsia (37 weeks of gesta- patients were diagnosed with early-onset hypertensive
tion or more), moderate early preeclampsia (32–36 disorders of pregnancy but delivered beyond 34
weeks of gestation), and early preeclampsia (less than weeks of gestation and were, therefore, included in
32 weeks of gestation), but different gestational age our late-onset group. This would have occurred across
cutoffs makes direct comparison of risk assessment all BMI ranges and it is unlikely to influence our
difficult. Additional data by Catov et al18 suggest that aRRs. Similar to Durst et al,19 we limited our analysis
15–17% of the population risk of early-onset hyper- to maternal BMI at delivery. Although prepregnancy
tensive disorders of pregnancy is associated with BMI is available in the U.S. Vital Statistics Database,
obesity, although their study defined early-onset as it is derived from maternal recall during the delivery
less than 37 weeks of gestation. admission and is therefore subject to recall bias.41
The increasing prevalence of obesity in the Finally, because the associations noted were modest
United States and worldwide highlights the impor- with a large sample size, the possibility of false alarm
tance of our findings and underscores the need for exists.42
prevention of hypertensive disorders of pregnancy in In conclusion, we noted that increasing classes of
this population.28,34 When initiated at less than 16 obesity are associated with progressively increased
weeks of gestation, aspirin is effective in preventing risk of both early-onset and late-onset hypertensive
hypertensive disorders of pregnancy in high-risk pop- disorders of pregnancy, with significant differences
ulations, but questions regarding appropriate dosing apparent by 24 weeks of gestation. The larger effect of
in the obese population remain unanswered.35–37 obesity on rates of hypertensive disorders of preg-
Once at term, induction of labor at 39 weeks of ges- nancy at later gestational ages is consistent with the
tation prevents development of hypertensive disor- contemporary hypothesis that hypertensive disorders
ders of pregnancy in low-risk nulliparous women,38 of pregnancy is the result of multiple pathways
and there have been progressively fewer late-term culminating in a single disease phenotype; addition-
and postterm pregnancies since the 1980s.39,40 These ally, the dichotomous distinction between early-onset
interventions, along with changes in diagnostic crite- and late-onset disease appears to overlap given the
ria, may contribute to the relatively slow increase in early and progressive influence of obesity on rates of
rates of hypertensive disorders of pregnancy in the hypertensive disorders of pregnancy.
face of the obesity epidemic.40
There are notable strengths to our study. The U.S.
REFERENCES
Vital Statistics period-linked birth and infant death
1. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-
certificates are compiled in a standardized fashion eclampsia. Lancet 2010;376:631–44.
across all 50 states and undergo quality control before 2. Lisonkova S, Joseph KS. Incidence of preeclampsia: risk factors
public release.25,26 The extensive demographic infor- and outcomes associated with early- versus late-onset disease.
mation allows for analysis of potential confounding Am J Obstet Gynecol 2013;209:544.e1–12.
variables and the large sample size is well suited to 3. Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS.
Maternal morbidity associated with early-onset and late-onset
study rare outcomes including early-onset hypertensive preeclampsia. Obstet Gynecol 2014;124:771–81.
disorders of pregnancy. Furthermore, the ability to sub-
4. Basso O, Rasmussen S, Weinberg CR, Wilcox AJ, Irgens LM,
divide the study population into narrow gestational age Skjaerven R. Trends in fetal and infant survival following pre-
groups allows delineation of trends, thus clarifying the eclampsia. JAMA 2006;296:1357–62.
VOL. 136, NO. 1, JULY 2020 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia 125
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
5. Stevens W, Shih T, Incerti D. Short-term costs of preeclampsia 24. Sohlberg S, Stephansson O, Cnattingius S, Wikstrom AK.
to the United States health care system. Am J Obstet Gynecol Maternal body mass index, height, and risks of preeclampsia.
2017;217:237–48.e16. Am J Hypertens 2012;25:120–5.
6. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. 25. Centers for Disease Control and Prevention. User guide to
WHO analysis of causes of maternal death: a systematic review. the 2014 period linked birth/infant death public use file.
Lancet 2006;367:1066–74. Available at: http://ftp.cdc.gov/pub/Health_Statistics/
7. Ness RB, Roberts JM. Heterogeneous causes constituting the NCHS/Dataset_Documentation/DVS/periodlinked/Link-
single syndrome of preeclampsia: a hypothesis and its implica- PE14Guide.pdf. Retrieved August 20, 2019.
tions. Am J Obstet Gynecol 1996;175:1365–70. 26. National Center for Health Statistics. Guide to completing the
facility worksheets for the certificate of live birth and report of
8. Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai
BM. The definition of severe and early-onset preeclampsia. fetal death (2003 revision). Available at: https://www.cdc.gov/
Statements from the International Society for the Study of nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. Retrieved
Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens March 17, 2020.
2013;3:44–7. 27. American College of Obstetricians and Gynecologists, Task
Force on Hypertension in Pregnancy. Hypertension in preg-
9. Vatten LJ, Skjaerven R. Is pre-eclampsia more than one dis-
ease? BJOG 2004;111:298–302. nancy. Report of the American College of Obstetricians and
Gynecologists’ Task Force on Hypertension in Pregnancy. Ob-
10. Iacobelli S, Bonsante F, Robillard PY. Comparison of risk fac- stet Gynecol 2013;122:1122–31.
tors and perinatal outcomes in early onset and late onset pre-
28. Obesity: preventing and managing the global epidemic. Report
eclampsia: a cohort based study in Reunion Island. J Reprod
Immunol 2017;123:12–6. of a WHO consultation. World Health Organ Tech Rep Ser
2000;894:1–253.
11. Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet 2005;
365:785–99. 29. Barradas DT, Dietz PM, Pearl M, England LJ, Callaghan WM,
Kharrazi M. Validation of obstetric estimate using early ultra-
12. You SH, Cheng PJ, Chung TT, Kuo CF, Wu HM, Chu PH. sound: 2007 California birth certificates. Paediatr Perinat Epi-
Population-based trends and risk factors of early- and late-onset demiol 2014;28:3–10.
preeclampsia in Taiwan 2001-2014. BMC Pregnancy Child-
birth 2018;18:199. 30. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake
P. Births: final data for 2017. Natl Vital Stat Rep 2018;67:1–
13. Bodnar LM, Catov JM, Klebanoff MA, Ness RB, Roberts JM. 50.
Prepregnancy body mass index and the occurrence of severe
hypertensive disorders of pregnancy. Epidemiology 2007;18: 31. von Elm E, Altman DG, Egger M. The strengthening the re-
234–9. porting of observational studies in epidemiology (STROBE)
statement: guidelines for reporting observational studies. Lan-
14. Dekker G, Sibai B. Primary, secondary, and tertiary prevention cet 2007;370:1453–7.
of pre-eclampsia. Lancet 2001;357:209–15.
32. Egbor M, Ansari T, Morris N, Green CJ, Sibbons PD. Morpho-
15. Duckitt K, Harrington D. Risk factors for pre-eclampsia at ante- metric placental villous and vascular abnormalities in early- and
natal booking: systematic review of controlled studies. BMJ late-onset pre-eclampsia with and without fetal growth restric-
2005;330:565. tion. BJOG 2006;113:580–9.
16. O’Brien TE, Ray JG, Chan WS. Maternal body mass index and 33. Moldenhauer JS, Stanek J, Warshak C, Khoury J, Sibai B. The
the risk of preeclampsia: a systematic overview. Epidemiology frequency and severity of placental findings in women with
2003;14:368–74. preeclampsia are gestational age dependent. Am J Obstet Gy-
17. Anderson NH, McCowan LM, Fyfe EM, Chan EH, Taylor RS, necol 2003;189:1173–7.
Stewart AW, et al. The impact of maternal body mass index on 34. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of
the phenotype of pre-eclampsia: a prospective cohort study. obesity among adults and youth: United States, 2015–2016.
BJOG 2012;119:589–95. NCHS Data Brief 2017;288:1–8.
18. Catov JM, Ness RB, Kip KE, Olsen J. Risk of early or severe 35. Caritis S, Sibai B, Hauth J, Lindheimer MD, Klebanoff M,
pre-eclampsia related to pre-existing conditions. Int J Epidemiol Thom E, et al. Low-dose aspirin to prevent preeclampsia in
2007;36:412–9. women at high risk. National Institute of child health and
19. Durst JK, Tuuli MG, Stout MJ, Macones GA, Cahill AG. human development network of maternal-fetal medicine units.
Degree of obesity at delivery and risk of preeclampsia with N Engl J Med 1998;338:701–5.
severe features. Am J Obstet Gynecol 2016;214:651.e1–5. 36. Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold
20. Fang R, Dawson A, Lohsoonthorn V, Williams MA. Risk fac- E. The role of aspirin dose on the prevention of preeclampsia
tors of early and late onset preeclampsia among Thai women. and fetal growth restriction: systematic review and meta-analy-
Asian Biomed 2009;3:477–86. sis. Am J Obstet Gynecol 2017;216:110–20.e6.
21. Mbah AK, Kornosky JL, Kristensen S, August EM, Alio AP, 37. Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A, de
Marty PJ, et al. Super-obesity and risk for early and late pre- Paco Matallana C, et al. Aspirin versus placebo in pregnancies
eclampsia. BJOG 2010;117:997–1004. at high risk for preterm preeclampsia. N Engl J Med 2017;377:
613–22.
22. Ornaghi S, Tyurmorezova A, Algeri P, Giardini V, Ceruti P,
Vertemati E, et al. Influencing factors for late-onset preeclamp- 38. Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM,
sia. J Matern Fetal Neonatal Med 2013;26:1299–302. Mallett G, et al. Labor induction versus expectant management
in low-risk nulliparous women. N Engl J Med 2018;379:513–
23. Poon LC, Kametas NA, Chelemen T, Leal A, Nicolaides 23.
KH. Maternal risk factors for hypertensive disorders in preg-
nancy: a multivariate approach. J Hum Hypertens 2010;24: 39. Donahue SM, Kleinman KP, Gillman MW, Oken E. Trends in
104–10. birth weight and gestational length among singleton term births
126 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
in the United States: 1990-2005. Obstet Gynecol 2010;115: 42. Grimes DA, Schulz KF. False alarms and pseudo-epidemics: the
357–64. limitations of observational epidemiology. Obstet Gynecol
40. Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the 2012;120:920–7.
United States, 1980-2010: age-period-cohort analysis. BMJ
2013;347:f6564. PEER REVIEW HISTORY
41. Headen I, Cohen AK, Mujahid M, Abrams B. The accuracy of Received February 15, 2020. Received in revised form March 19,
self-reported pregnancy-related weight: a systematic review. 2020. Accepted March 26, 2020. Peer reviews and author corre-
Obes Rev 2017;18:350–69. spondence are available at http://links.lww.com/AOG/B901.
VOL. 136, NO. 1, JULY 2020 Bicocca et al Obesity and Early-Onset vs Late-Onset Preeclampsia 127
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
You might also like
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Does Alcohol Increase The Risk of Preterm.5Document7 pagesDoes Alcohol Increase The Risk of Preterm.5BungaNo ratings yet
- Magro-Malosso Et Al-2017-Acta Obstetricia Et Gynecologica ScandinavicaDocument11 pagesMagro-Malosso Et Al-2017-Acta Obstetricia Et Gynecologica ScandinavicaRisnaAyhuNo ratings yet
- Poster Session IV: ObjectiveDocument2 pagesPoster Session IV: ObjectivefujimeisterNo ratings yet
- Peningkatan Tekanan Darah Pada Kehamilan Dini Dan Risiko Morbiditas Ibu Dan BayiDocument11 pagesPeningkatan Tekanan Darah Pada Kehamilan Dini Dan Risiko Morbiditas Ibu Dan BayiFan AccountNo ratings yet
- Tugas Bunda RuriDocument34 pagesTugas Bunda RuriAnzory ErvanNo ratings yet
- Obesidad en El EmbarazoDocument17 pagesObesidad en El Embarazodianaarias1703No ratings yet
- Ong 139 391Document9 pagesOng 139 391abdi syahputraNo ratings yet
- High Rate of Early Onset Preeclampsia in MauritiusDocument4 pagesHigh Rate of Early Onset Preeclampsia in MauritiusHarvey MatbaganNo ratings yet
- Implications of Early Pregnancy Obesity On Maternal, Fetal and Neonatal Health PDFDocument7 pagesImplications of Early Pregnancy Obesity On Maternal, Fetal and Neonatal Health PDFAndhika Dimas ANo ratings yet
- Mjiri 32 104Document5 pagesMjiri 32 104Nur ChusnulNo ratings yet
- Maternal Underweight and The Risk of Spontaneous Abortion: Original ArticleDocument5 pagesMaternal Underweight and The Risk of Spontaneous Abortion: Original ArticleKristine Joy DivinoNo ratings yet
- Pregnancy Exercise Overweight MetaanalysisDocument11 pagesPregnancy Exercise Overweight MetaanalysisAisleenHNo ratings yet
- PIIS0002937821019992Document2 pagesPIIS0002937821019992made dharmaNo ratings yet
- Chasan Taber2008Document10 pagesChasan Taber2008Tudor MotasNo ratings yet
- First-Trimester Prediction of Gestational Hypertension Through The Bioelectrical Impedance Analysis of The Body CompositionDocument6 pagesFirst-Trimester Prediction of Gestational Hypertension Through The Bioelectrical Impedance Analysis of The Body Compositionppdsobginunsrijan23No ratings yet
- Poster Session I: ConclusionDocument2 pagesPoster Session I: ConclusionfujimeisterNo ratings yet
- Maternal and Perinatal Outcome of Maternal Obesity atDocument6 pagesMaternal and Perinatal Outcome of Maternal Obesity attaufik perdanaNo ratings yet
- Pre-Pregnancy Menstrual Cycle Regularity and Length and The Risk of Gestational Diabetes Mellitus: Prospective Cohort StudyDocument10 pagesPre-Pregnancy Menstrual Cycle Regularity and Length and The Risk of Gestational Diabetes Mellitus: Prospective Cohort Studyn2763288No ratings yet
- 2016 Management of Severe Hypertension in PregnancyDocument7 pages2016 Management of Severe Hypertension in PregnancyMaria del Pilar Devis MoralesNo ratings yet
- 1 s2.0 S016041201931935X MainDocument12 pages1 s2.0 S016041201931935X MainYaumil FauziahNo ratings yet
- Chronic Hypertension in PregnancyDocument10 pagesChronic Hypertension in PregnancySalma MaulidiyahNo ratings yet
- Obstetric Outcomes in Women With Sonographically.27Document7 pagesObstetric Outcomes in Women With Sonographically.27Gina Eliana Custodio GonzalesNo ratings yet
- Gestation Specific Vital Sign Ref Ranges in Pregnancy OBGYN 2020 PDFDocument12 pagesGestation Specific Vital Sign Ref Ranges in Pregnancy OBGYN 2020 PDFRaul DoctoNo ratings yet
- Correlation Between Gestational Weight Gain in The Second and Third Trimester and Preeclampsia Risk A Study From IndonesiaDocument7 pagesCorrelation Between Gestational Weight Gain in The Second and Third Trimester and Preeclampsia Risk A Study From IndonesiaAlrika Febi YuarsyahNo ratings yet
- Jurnal 7Document9 pagesJurnal 7chichiNo ratings yet
- Estudio de CohorteDocument5 pagesEstudio de CohorteFlorencia RojoNo ratings yet
- Fertility and Sterility. 2007Document13 pagesFertility and Sterility. 2007Cindy AtikaNo ratings yet
- PIIS0002937819319829Document2 pagesPIIS0002937819319829Edo JeldeNo ratings yet
- 47 Review Article - Sushmitha Ramona KarkadaDocument4 pages47 Review Article - Sushmitha Ramona KarkadaAnjali Rahul AjmeriNo ratings yet
- Lupus and Pregnancy Studies: B - Urowitz, Dafna D. Gladman, Vern T. FarewellDocument6 pagesLupus and Pregnancy Studies: B - Urowitz, Dafna D. Gladman, Vern T. FarewellAhmad AbulegiNo ratings yet
- Risk Factors For Preeclampsia in A High-Risk Cohort of Women Served by A Nursing-Based Home Visiting ProgramDocument1 pageRisk Factors For Preeclampsia in A High-Risk Cohort of Women Served by A Nursing-Based Home Visiting ProgramaniNo ratings yet
- Articulo 5Document6 pagesArticulo 5Monica ReyesNo ratings yet
- Research Article: Age at Menarche, Menstrual Characteristics, and Risk of PreeclampsiaDocument6 pagesResearch Article: Age at Menarche, Menstrual Characteristics, and Risk of PreeclampsiaSyahrul Habibi NasutionNo ratings yet
- Maternal and Perinatal Outcome of Maternal Obesity atDocument7 pagesMaternal and Perinatal Outcome of Maternal Obesity atappNo ratings yet
- Avitanrg RG RDocument2 pagesAvitanrg RG RPrasetio Kristianto BudionoNo ratings yet
- 1 s2.0 S258993332030197X MainDocument10 pages1 s2.0 S258993332030197X MainDzaki Prakoso RamadhanNo ratings yet
- Nej Mo A 1509819Document10 pagesNej Mo A 1509819Fhirastika AnnishaNo ratings yet
- Exercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDocument8 pagesExercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDaniela VenegasNo ratings yet
- 176S Tuesday Posters Obstetrics & GynecologyDocument1 page176S Tuesday Posters Obstetrics & GynecologyJoseph BennettNo ratings yet
- Outcome of Teenage PregnancyDocument5 pagesOutcome of Teenage PregnancyKN DumpNo ratings yet
- Association of Early Menarche Age and Overweight/obesityDocument6 pagesAssociation of Early Menarche Age and Overweight/obesityseptiani hasibuanNo ratings yet
- Maternal Obesity 2Document13 pagesMaternal Obesity 2lalimdNo ratings yet
- Balogunrg RGDocument10 pagesBalogunrg RGPrasetio Kristianto BudionoNo ratings yet
- Oliverwilliams2015 PDFDocument10 pagesOliverwilliams2015 PDFWh SquadNo ratings yet
- Jarvie - Obstetric ManagementDocument6 pagesJarvie - Obstetric ManagementIsabella GrobérioNo ratings yet
- Effect of Birth Weight On Adverse Obstetric.20 PDFDocument6 pagesEffect of Birth Weight On Adverse Obstetric.20 PDFTriponiaNo ratings yet
- Risk of Recurrent Stillbirth in Subsequent.6Document10 pagesRisk of Recurrent Stillbirth in Subsequent.6Meriza RifaniNo ratings yet
- Association of High Sensitivity C Reactive Protein Serum LevelsDocument5 pagesAssociation of High Sensitivity C Reactive Protein Serum LevelsJesslynBernadetteNo ratings yet
- BMI in PregnancyDocument4 pagesBMI in PregnancyCitra KristiNo ratings yet
- Association Between Asymptomatic Bacteriuria and Pre-Eclampsia.Document5 pagesAssociation Between Asymptomatic Bacteriuria and Pre-Eclampsia.alfiahNo ratings yet
- D'Souza-2019-Maternal Body Mass Index and PregDocument17 pagesD'Souza-2019-Maternal Body Mass Index and PregMARIATUL QIFTIYAHNo ratings yet
- Feto-Maternal Comlications in Pregancy With Metabolic Syndrome - A Hospital Based StudyDocument7 pagesFeto-Maternal Comlications in Pregancy With Metabolic Syndrome - A Hospital Based StudyIJAR JOURNALNo ratings yet
- Gestation-Specific Vital Sign Reference Ranges in Pregnancy: Original ResearchDocument12 pagesGestation-Specific Vital Sign Reference Ranges in Pregnancy: Original Researchdian_067No ratings yet
- Sdarticle 132 PDFDocument1 pageSdarticle 132 PDFRio Michelle CorralesNo ratings yet
- Early Onset and Late Onset Preeclampsia-Maternal and Perinatal Outcomes in A Rural Teritiary Health CenterDocument4 pagesEarly Onset and Late Onset Preeclampsia-Maternal and Perinatal Outcomes in A Rural Teritiary Health CenterPutri Maghfirah BahriNo ratings yet
- Artigo PrincipalDocument7 pagesArtigo PrincipalVictoria AlmeidaNo ratings yet
- Randomized Trial of A Lifestyle Program in Obese Infertile WomenDocument12 pagesRandomized Trial of A Lifestyle Program in Obese Infertile WomenNatalia NaganNo ratings yet
- Jurnal CohortDocument21 pagesJurnal CohortAstri Anindita UtomoNo ratings yet
- Ijogr 3 (4) 407-409Document3 pagesIjogr 3 (4) 407-409Yuni Astuti DjoyomiharjoNo ratings yet
- K10 Kuliah NefrourologiDocument170 pagesK10 Kuliah NefrourologimarinanananaNo ratings yet
- DAPUSDocument5 pagesDAPUSmarinanananaNo ratings yet
- Antibiotics IN GENITOURINARY: Dr. Rachmat Hidayat, M.SCDocument20 pagesAntibiotics IN GENITOURINARY: Dr. Rachmat Hidayat, M.SCmarinanananaNo ratings yet
- PR TGMDocument24 pagesPR TGMmarinanananaNo ratings yet
- Perkembangan & Pertumbuhan System UrogenitalaDocument35 pagesPerkembangan & Pertumbuhan System UrogenitalamarinanananaNo ratings yet
- Pekerjaan Rumah Urinary SystemDocument22 pagesPekerjaan Rumah Urinary SystemmarinanananaNo ratings yet
- Preterm Parturition and Pre-Eclampsia: The Confluence of Two Great Gestational SyndromesDocument7 pagesPreterm Parturition and Pre-Eclampsia: The Confluence of Two Great Gestational SyndromesmarinanananaNo ratings yet
- Hepatic Encephalopaty: Dr. Suyata, SPPD, K-Geh, FinasimDocument25 pagesHepatic Encephalopaty: Dr. Suyata, SPPD, K-Geh, FinasimmarinanananaNo ratings yet
- Skenario A Blok 22 Day 1Document39 pagesSkenario A Blok 22 Day 1marinanananaNo ratings yet
- Jurnal ObgynDocument8 pagesJurnal ObgynmarinanananaNo ratings yet
- Skenario A Blok 23 Kelompok 4Document34 pagesSkenario A Blok 23 Kelompok 4marinanananaNo ratings yet
- NSTP-CWTS Syllabus Prelim-MidtermDocument16 pagesNSTP-CWTS Syllabus Prelim-MidtermKobe BryNo ratings yet
- Psychotherapy Psychologist Arnold Lazarus Psychological: Behavior TherapyDocument2 pagesPsychotherapy Psychologist Arnold Lazarus Psychological: Behavior Therapyusmaafzal55100% (1)
- Physical DisabilitiesDocument11 pagesPhysical DisabilitiesBobo Wong100% (2)
- Chapter 38 Test BankDocument12 pagesChapter 38 Test BankelizabethenNo ratings yet
- Upper Limb OrthosisDocument83 pagesUpper Limb OrthosisAwaisNo ratings yet
- Achievement Test Q7 MAPEHDocument4 pagesAchievement Test Q7 MAPEHRongel GuingayanNo ratings yet
- Insulin AdministrationDocument3 pagesInsulin AdministrationByne BarasiNo ratings yet
- Vortioxetine On Cognition in Schizophrenia: Materials and Methods Study DesignDocument5 pagesVortioxetine On Cognition in Schizophrenia: Materials and Methods Study Designhevi_tarsumNo ratings yet
- Glaucoma Management Approach: Simple Literature ReviewDocument4 pagesGlaucoma Management Approach: Simple Literature ReviewElrach CorpNo ratings yet
- Mortuary ServicesDocument30 pagesMortuary ServicesYogesh ChandraNo ratings yet
- National Health Sector Strategic Plan 2010 - 2015 - Ministry of Health and Sanitation (GoSL)Document64 pagesNational Health Sector Strategic Plan 2010 - 2015 - Ministry of Health and Sanitation (GoSL)MaxxNo ratings yet
- High Blood PressureDocument5 pagesHigh Blood PressureHelena AzevedoNo ratings yet
- BRONCHOPULMONARY DYSPLASIA ModifiedDocument48 pagesBRONCHOPULMONARY DYSPLASIA ModifiedajanmjNo ratings yet
- Woodruff CVDocument56 pagesWoodruff CVThe State NewsNo ratings yet
- Case Presentation in Geriatric Ward "Cancer of The Larynx"Document130 pagesCase Presentation in Geriatric Ward "Cancer of The Larynx"Christina GutierrezNo ratings yet
- Clinical BacteriologyDocument123 pagesClinical Bacteriologykurotsukki todoroki100% (1)
- TETANUSDocument41 pagesTETANUSruchikakaushal1910No ratings yet
- CLIA Requirements For Analytical Quality - WestgardDocument4 pagesCLIA Requirements For Analytical Quality - Westgardruth pinos100% (1)
- Circulatory System EssayDocument5 pagesCirculatory System Essayfz75587x100% (2)
- Adverse Drug Event of Hypokalaemia-Induced Cardiotoxicity Secondary To The Use of Laxatives: A Systematic Review of Case ReportsDocument10 pagesAdverse Drug Event of Hypokalaemia-Induced Cardiotoxicity Secondary To The Use of Laxatives: A Systematic Review of Case ReportsNadial uzmahNo ratings yet
- Legal Issues CHNDocument17 pagesLegal Issues CHNSamjhana NeupaneNo ratings yet
- Trauma DentoalveolarDocument6 pagesTrauma Dentoalveolarandres gabrielNo ratings yet
- Carbohydrate To Insulin Ratio - Breakfast-Lunch-DinnerDocument5 pagesCarbohydrate To Insulin Ratio - Breakfast-Lunch-Dinnermario rodriguezNo ratings yet
- Antibiotics 12 00399 With CoverDocument20 pagesAntibiotics 12 00399 With CoverRAGHAVENDRA VAGYANNAVARNo ratings yet
- S Grof The Cosmic GameDocument298 pagesS Grof The Cosmic GameMarius Păunescu100% (2)
- SOFIE FAP Webinar 2023Document42 pagesSOFIE FAP Webinar 2023Shibin JayakrishnanNo ratings yet
- Observational Study DesignDocument25 pagesObservational Study DesignlenyNo ratings yet
- Etiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsDocument33 pagesEtiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsNatasya Ayusandra MahersaputriNo ratings yet
- Annotated Final - Copy-1Document16 pagesAnnotated Final - Copy-1ValarmathiNo ratings yet
- Tri Active PlusDocument8 pagesTri Active PlusRex_333No ratings yet