Professional Documents
Culture Documents
Emergency Department Intubation Checklist PDF
Emergency Department Intubation Checklist PDF
Uploaded by
xedoyis969Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency Department Intubation Checklist PDF
Emergency Department Intubation Checklist PDF
Uploaded by
xedoyis969Copyright:
Available Formats
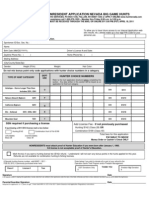
EDICT Emergency Department Intubation ChecklisT
Preparation
Is non-invasive ventilation (CPAP/BiPAP) an option?
Consider the indication for intubation Is the patient DNI status?
Has patient/family consented, if applicable?
5 liters per minute to augment preoxygenation, then
Nasal cannula ≥15 liters per minute post-induction to facilitate apneic oxygenation
≥ 3 min or 8 deep breaths with face mask; O2 regulator turned all the way up
Preoxygenate with high-flow oxygen If inadequate saturation with NC+facemask: use NIV or BVM with PEEP valve
If pt too agitated for preoxygenation: ketamine induction, preox, then paralyze
Difficult laryngoscopy Look externally, Evaluate 3-3-2 rule, Mallampati score, Obstruction, Neck Mobility
Difficult BVM Beard, Obese, No teeth, Elderly, Sleep Apnea / Snoring
Assess for: Difficult extraglottic device Restricted mouth opening, Obstruction, Distorted airway, Stiff lungs or c-spine
Difficult cricothyrotomy Surgery, Hematoma, Obesity, Radiation distortion or other deformity, Tumor*
Determine airway management strategy see bottom of page 2 for cricothyrotomy
Plan B/C/D: Change
patient position, blade, technique; mark membrane prior to
see bottom of page 2 airway attempt if anticipated
for awake technique modality or operator
RSI Prepare for failure Supraglottic Airway
Airway
vs. of intubation and Ventilate
attempt Cricothyrotomy
Awake failure of ventilation
Awake approach preferred when Discuss plan A, B, C, D with team Bag/mask or LMA
Less urgent intubation Equipment for plan A, B, C, D at bedside
More difficult airway features
Post-intubation
Low risk of vomiting management
Check for dentures Dentures in for bag mask ventilation, out for laryngoscopy
Auditory meatus to suprasternal notch (sheets under neck / occiput / shoulders)
Position patient Patient's head to operator's lower sternum (bed height)**
Torso angle of 30° recommended, especially in obesity and upper GI bleed
ECG
Pulse oximetry
Monitoring equipment Blood pressure
Continuous end-tidal capnography - verify function with test breath
IV access Two lines preferable
Equipment Use Broselow tape for sizes in pediatrics
Ambu bag connected to oxygen Size: approximate nasal bridge, malar eminences, alveolar ridge / Err larger
Laryngoscopy handles - verify power At least two
Suction under patient's shoulder - verify function If suspected soiled airway (blood, vomitus, secretions), suction under each shoulder
Laryngoscopy blades - verify bulbs Curved and straight / One size larger, one size smaller
Oral airways Size: Angle of mouth to tragus of ear (usually 80, 90, or 100 mm in adults)
Nasal airways Size: Tip of nose to tragus of ear (usually 26 Fr/6.5 mm, 28/7, or 30/7.5 in adults)
Colorimetric capnometer To be used if continuous not available or not functioning
Endotracheal tubes - verify cuff function Variety of sizes ( ≥ 8.0 mm preferred in adults to facilitate ICU care)
ETT stylet Straight to cuff, 35 degrees**
ETT securing device Tape if no device available
Gum elastic bougie
LMA with lubricant and syringe
Cricothyrotomy tools / video laryngoscope / optical stylet
Difficult airway equipment fiberoptic scope / Magill forceps if suspected foreign body
Drugs
Pretreatment agents are always optional
Pretreatment agents, if applicable Give as bolus 3 minutes prior to induction, except for fentanyl, which should
be the final pretreatment agent, and should be given over 30-60 seconds.
Fentanyl 3 mcg/kg TBW if high BP a concern (aneurysms, dissections, high ICP, severe CAD)
Lidocaine 1.5 mg/kg TBW for reactive airways or increased ICP
.02 mg/kg IV or IM (min 0.1 mg, max 1 mg) pg. 1
Atropine For infants, especially if receiving succinylcholine
EDICT Emergency Department Intubation ChecklisT
Etomidate 0.3 mg/kg TBW
Propofol 1.5 - 3 mg/kg IBW+(.4)(TBW)
Induction agent Ketamine 2 mg/kg IV or 4 mg/kg IM IBW Reduce dose if hypotensive
Midazolam 0.2 - 0.3 mg/kg TBW
Thiopental 3- 6 mg/kg TBW Contraindications to succinylcholine
History of malignant hyperthermia
Succinylcholine 2 mg/kg IV 4 mg/kg IM TBW Burn or crush injury > 5 days old
Paralytic agent Rocuronium 1.2 mg/kg IBW Stroke or spinal cord injury > 5 days old
Vecuronium 0.3 mg/kg IBW if roc unavailable MS, ALS, or inherited myopathy
Normal saline flushes Known hyperkalemia (absolute)
Renal failure (relative)
For peri-intubation hypotension Suspected hyperkalemia (relative)
Phenylephrine 100 mcg IV push as needed
A/C
FiO2 100% – titrate down over time to SpO2 95%
RR 18 [Asthma/COPD: 6-10]
Post-intubation settings discussed TV 8 mL/kg – use ideal body weight [6 mL/kg if sepsis / prone to lung injury]
I/E 1:2 [Asthma/COPD 1:4 - 1:5]
Inspiratory Flow Rate 60-80 L/min [Asthma/COPD 80-100 L/min]
PEEP 5 cm H20 [CHF 6-12→watch blood pressure] [PEEP 0 in Asthma/COPD]
Personnel MD / RN / RT
RSI or Awake Technique End-tidal CO2 if using colorimetric – bright yellow with six breaths
Esophageal detection device should aspirate without resistence if ETT in trachea
Verify tube placement Bougie hold-up test - see below
Repeat visualization using direct laryngoscopy or alternate device
Auscultation
Post-Intubation Care
Record position at lips
These are starting doses -
Secure ETT Adults: approx 21 cm (female) or 23 cm (male)
reassess frequently and
Pediatrics: approximately ETT size x 3
Orogastric or nasogastric tube rebolus/titrate upward as
Fentanyl 2 mcg/kg bolus then 1 mcg/kg/hour needed.
Portable chest radiograph Morphine 0.1 mg/kg bolus then .1 mg/kg/hour
Propofol 0.5 mg/kg bolus then 15 mcg/kg/min In the just intubated phase,
Opioid then sedative boluses/drips Midazolam 0.05 mg/kg bolus then .025 mg/kg/hour especially if transport and
Lorazepam 0.04 mg/kg bolus then .02 mg/kg/hour procedures are imminent,
Head of bed to 30-45 degrees, higher if very obese aggressively analgese and
Ketamine 1 mg/kg bolus then 1 mg/kg/hour
In-line suction sedate to a RASS† score of
Adjust to minimum pressure required to -4 to -5. In the stable on the
Adjust ETT cuff pressure abolish air leak - usually 15-25 mm Hg by vent stage, titrate down
endotracheal tube cuff manometer sedation and use opioids to
In-line heat-moisture exchanger target a RASS score of -1
Adjust RR (not TV) to appropriate pH and pCO2 to -2. Avoid re-paralysis.
Keep pH > 7.1 for permissive hypercapnia
Blood gas within 30 minutes post-intubation Use incremental FiO2/PEEP chart for oxygenation Fentanyl and ketamine are
Keep plateau pressure < 30 cm H20 least likely to cause or
Foley catheter pCO2 is at least ETCO2 but may be much higher worsen hypotension.
†Richmond Agitation Sedation Scale
Dislodgement – check EtCO2 waveform, repeat laryngoscopy
Obstruction – check for high PIP, suction secretions
Pneumothorax – breath sounds / lung sliding on ultrasound, repeat CXR
Equipment failure – disconnect from vent and bag
Stacking breaths / auto-PEEP - bag slowly, push on chest to assist prn
Watch for post-intubation complications
Bougie hold-up test: gently advance intubating stylet through ETT
Verify that airway equipment is ready for the next patient No resistance @ 40 cm: likely esophageal
Resistance @ 26-40 cm (usually <30 cm): likely tracheal and patent
Resistance @ less than 25 cm: likely clogged tube
Awake Intubation Technique Cricothyrotomy Technique
❑ Glycopyrolate 0.2 mg or Atropine .01 mg/kg glyco preferred, ideally given 15 min prior to next step 1. Vertical incision, palpate membrane
❑ Suction then pad dry mouth with gauze 2. Blind horizontal incision through membrane
❑ Nebulized Lidocaine without epi @ 5 lpm ideally 4 cc of 4% lidocaine but can also use 8 cc of 2% lidocaine 3. Blind finger through membrane into trachea
4. Bougie along finger into trachea
❑ Atomized Lidocaine sprayed to oropharynx especially if unable to give full dose of nebulized lidocaine
5. Lubricated 6.0 mm ETT or tracheostomy
❑ Viscous Lidocaine lollipop 2% viscous lido on tongue depressor
tube via bougie
❑ Preoxygenate ❑ Position ❑ Restrain prn ❑ Switch to nasal cannula
❑ Lightly sedate with Versed 2-4 mg or Ketamine 20 mg aliquots q 2 min
❑ Intubate awake or place bougie, then paralyze, then pass tube
R. Strayer / S. Weingart / P. Andrus / R. Arntfield Mount Sinai School of Medicine / v13 / 7.8.2012
*From Walls RM and Murphy MF: Manual of Emergency Airway Management. Philadelphia, Lippincott, Williams and Wilkins, 3rd edition, 2008; with permission.
**From Levitan RM: Airway•Cam Pocket Guide to Intubation. Exton, PA, Apple Press, 2005; with permission. pg. 2
You might also like
- C172N PohDocument73 pagesC172N PohAdam Breindel94% (17)
- (Jeff - Solheim) Emergency Nursing. The Profession PDFDocument489 pages(Jeff - Solheim) Emergency Nursing. The Profession PDFDesrila Indra Sari100% (3)
- Oral Station Scenario PDFDocument3 pagesOral Station Scenario PDFlotuss45No ratings yet
- Jeep EnginesDocument517 pagesJeep EnginesAlessio Prolongo96% (24)
- How To Interpret An ECG in Seven StepsDocument5 pagesHow To Interpret An ECG in Seven StepsCM Najito100% (1)
- Normal Pediatric RR and HRDocument1 pageNormal Pediatric RR and HRRick FreaNo ratings yet
- Drug Nomenclature Suffixes and PrefixesDocument6 pagesDrug Nomenclature Suffixes and PrefixesMariaNo ratings yet
- Patho Exam 3 Study GuideDocument5 pagesPatho Exam 3 Study GuideFarzanaAziziNo ratings yet
- Lillico NR511 SOAP Note Week 3 KatieDocument7 pagesLillico NR511 SOAP Note Week 3 Katie최인선100% (1)
- Zero Based BudgetDocument9 pagesZero Based Budgetapi-447860598No ratings yet
- ACLS (Advanced Cardiac Life Support) Algorithms & NotesDocument4 pagesACLS (Advanced Cardiac Life Support) Algorithms & Notesiamlucil100% (4)
- Medback - Cerebral PalsyDocument47 pagesMedback - Cerebral Palsyyreshgem100% (2)
- Ge Sign A Profile BrochureDocument15 pagesGe Sign A Profile BrochurePaul PichardoNo ratings yet
- A Simplified ECG GuideDocument4 pagesA Simplified ECG GuideMarian Ioan-LucianNo ratings yet
- HO - Burns Environmental EmergenciesDocument7 pagesHO - Burns Environmental EmergenciesSteven Paul DaclesNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- What Is Respiratory Alkalosis?Document3 pagesWhat Is Respiratory Alkalosis?Lorenn AdarnaNo ratings yet
- Cardiovascular EmergenciesDocument20 pagesCardiovascular EmergenciesJohn FisherNo ratings yet
- Lab Values and Vital SignsDocument4 pagesLab Values and Vital SignsWole Olaluwoye100% (1)
- Immunosuppressant Drugs Drug Name Class Function Method/Receptor UseDocument3 pagesImmunosuppressant Drugs Drug Name Class Function Method/Receptor UseKristin DouglasNo ratings yet
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocument34 pagesArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212No ratings yet
- Shock Study GuideDocument8 pagesShock Study GuideMadameb1No ratings yet
- 7 Suggestions Paramedic Airway ANAM22 WMDocument5 pages7 Suggestions Paramedic Airway ANAM22 WMcedivadeniaNo ratings yet
- BBB EcgDocument33 pagesBBB EcgLokbre YoasNo ratings yet
- Coumadin Dosing GuideDocument3 pagesCoumadin Dosing Guidemorale28No ratings yet
- ACLS Algorithms (2011)Document6 pagesACLS Algorithms (2011)senbonsakuraNo ratings yet
- PICU Common ProblemDocument49 pagesPICU Common ProblemRawabi rawabi1997No ratings yet
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDocument49 pagesAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNo ratings yet
- Dysrhytmia NotesDocument11 pagesDysrhytmia NoteshannahhwolfNo ratings yet
- Sample Acls For DummiesDocument3 pagesSample Acls For DummiesTodd Cole100% (1)
- Emergency Lecture PDFDocument57 pagesEmergency Lecture PDFDuane Liloc100% (1)
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- Megacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...Document1 pageMegacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...krgduraiNo ratings yet
- KegawatdaruratanDocument164 pagesKegawatdaruratanmeida astriani gozaziNo ratings yet
- Emergency Medicine كتاب ايمرجنسي مفيد للروتيترز الجدد وملخص مفيدDocument46 pagesEmergency Medicine كتاب ايمرجنسي مفيد للروتيترز الجدد وملخص مفيدSri PoopaseNo ratings yet
- 5 ECG Interpretation With AnswersDocument48 pages5 ECG Interpretation With AnswersQusai Ibraheem100% (1)
- Davies Veterinary Specialists UnderstandingDocument3 pagesDavies Veterinary Specialists UnderstandingFelicity HumphreysNo ratings yet
- 1538 Exam 4 Cell Reg & GriefDocument35 pages1538 Exam 4 Cell Reg & GriefJade EdanoNo ratings yet
- Drugs in ObstetricsDocument95 pagesDrugs in ObstetricsPriya jNo ratings yet
- PalsDocument1 pagePalslordroentgenNo ratings yet
- Chest TubesDocument12 pagesChest TubesMark Hammerschmidt100% (4)
- BLS SummaryDocument2 pagesBLS Summaryreyes markNo ratings yet
- Drugs and Defibrillation: Department of Anesthesiology & Reanimation General Hospital TasikmalayaDocument20 pagesDrugs and Defibrillation: Department of Anesthesiology & Reanimation General Hospital TasikmalayaAfrida Sahestina100% (1)
- ACLS Drug TherapyDocument8 pagesACLS Drug TherapySahrensNo ratings yet
- IV PDFDocument63 pagesIV PDFelbagouryNo ratings yet
- Antrim ED Handbook 2019Document238 pagesAntrim ED Handbook 2019Chris Jardine LiNo ratings yet
- Principles of ECGDocument11 pagesPrinciples of ECGDeinielle Magdangal RomeroNo ratings yet
- Dysrhythmias: Sinus Node Dysrhythmias Tachycardia, and Sinus ArrhythmiaDocument5 pagesDysrhythmias: Sinus Node Dysrhythmias Tachycardia, and Sinus ArrhythmiaKayelyn-Rose Combate100% (1)
- Electrocardiography: Dr. Anand PatelDocument155 pagesElectrocardiography: Dr. Anand PatelDeepika PatelNo ratings yet
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDocument23 pagesELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJNo ratings yet
- ARRHYTHMIADocument82 pagesARRHYTHMIAjiluNo ratings yet
- Rhythm Strip ReviewDocument8 pagesRhythm Strip ReviewDouglas Greg Cook100% (2)
- Adenosine: Rapid IV PushDocument4 pagesAdenosine: Rapid IV PushsabboNo ratings yet
- CCU Clinical GuidelinesDocument63 pagesCCU Clinical GuidelinesHAMMYER ALROKHAMINo ratings yet
- HTNDocument54 pagesHTNapi-232466940No ratings yet
- The Ultimate Review For MedicalDocument15 pagesThe Ultimate Review For MedicalJap Avila BernasNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- Mayhaw Jelly From LSU ExtensionDocument4 pagesMayhaw Jelly From LSU ExtensionDaniel CrookNo ratings yet
- Introduction To EKG Interpretation v8.0Document84 pagesIntroduction To EKG Interpretation v8.0TrickyRooNo ratings yet
- The Red Eye Challenge: QuestionsDocument5 pagesThe Red Eye Challenge: QuestionsDaniel CrookNo ratings yet
- ACEP Ketamine Guideline 2011Document13 pagesACEP Ketamine Guideline 2011Daniel Crook100% (1)
- Basal Cell Carcinoma 2Document14 pagesBasal Cell Carcinoma 2Daniel CrookNo ratings yet
- Capnography During CPRDocument25 pagesCapnography During CPRDaniel CrookNo ratings yet
- RedbookDocument323 pagesRedbookحسام جبار مجيدNo ratings yet
- Nevada Big Game Application 2011Document1 pageNevada Big Game Application 2011Daniel CrookNo ratings yet
- Resume 2021Document4 pagesResume 2021api-555218722No ratings yet
- Consumer Temperament Towards Top 5 Multi Speciality Hospitals in CoimbatoreDocument11 pagesConsumer Temperament Towards Top 5 Multi Speciality Hospitals in Coimbatorehari krishnanNo ratings yet
- BCBSNC - Profile v1.1Document6 pagesBCBSNC - Profile v1.1srgaurNo ratings yet
- Nurs 151 K4uDocument8 pagesNurs 151 K4uapi-315464968No ratings yet
- Beautiful Results: Simple Procedure 1. Etch 2. Bond 3. RestoreDocument4 pagesBeautiful Results: Simple Procedure 1. Etch 2. Bond 3. RestoreEuclides Soza CalvoNo ratings yet
- Fluidos Pasar A 5 A 10 Min Vs Pasar A 20 MinDocument11 pagesFluidos Pasar A 5 A 10 Min Vs Pasar A 20 MinRudy SanabriaNo ratings yet
- PHTLS Lessone 3Document28 pagesPHTLS Lessone 3Adel AlkaliliNo ratings yet
- What Is Borderline Personality Disorder?Document8 pagesWhat Is Borderline Personality Disorder?aagNo ratings yet
- A Study On Genetic Markers On Human TissuesDocument10 pagesA Study On Genetic Markers On Human TissuesizzomuneNo ratings yet
- CR-4509 PSQH Vocera Ebook FinalDocument22 pagesCR-4509 PSQH Vocera Ebook FinalNurul AdhwaNo ratings yet
- Acutepain PneumoniaDocument3 pagesAcutepain PneumoniaJoy SalvadorNo ratings yet
- Eye Ear Nose ExamDocument1 pageEye Ear Nose ExamCorey JohnsonNo ratings yet
- Introduction To Anesthesia: Dr. Kyat Sidharta, SP AnDocument11 pagesIntroduction To Anesthesia: Dr. Kyat Sidharta, SP AnRiyan AndikaNo ratings yet
- Planning: Reported By: Regiely Prado, RNDocument39 pagesPlanning: Reported By: Regiely Prado, RNbernadeteNo ratings yet
- Fracture FemurDocument28 pagesFracture FemurKulsoom ShahNo ratings yet
- Unani & SiddhaDocument22 pagesUnani & SiddhaMandy BuchananNo ratings yet
- Super Final NCPDocument16 pagesSuper Final NCPNessaly Jane PrestoNo ratings yet
- Teresio Varetto: Vienna 06 October 2015Document27 pagesTeresio Varetto: Vienna 06 October 2015intnpsNo ratings yet
- Signs and Symptoms of Respiratory DiseasesDocument42 pagesSigns and Symptoms of Respiratory DiseasesjabeedNo ratings yet
- Herpez Zoster Dan PHNDocument16 pagesHerpez Zoster Dan PHNRizky FatimahNo ratings yet
- EPC Referral FormDocument1 pageEPC Referral Formwaterbearer85No ratings yet
- Doctor-Patient Communication A ReviewDocument6 pagesDoctor-Patient Communication A ReviewWagiono SuparanNo ratings yet
- Theory and Science Specimen PaperDocument12 pagesTheory and Science Specimen PaperAhmed Yousef100% (3)
- Wound Care BasicDocument3 pagesWound Care BasicVinceNo ratings yet
- Nursing InformaticsDocument22 pagesNursing InformaticsJan Jamison ZuluetaNo ratings yet
- Peri ImplantitisDocument12 pagesPeri ImplantitisbobNo ratings yet
- Choosing A Wound Dressing Based On Common Wound CharacteristicsDocument11 pagesChoosing A Wound Dressing Based On Common Wound CharacteristicsYolis MirandaNo ratings yet