Professional Documents
Culture Documents
Echo Hits
Uploaded by
Hany ElbarougyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Echo Hits
Uploaded by
Hany ElbarougyCopyright:
Available Formats
Catheter-based Cardiac Surgery 125
Figure 1. Paraprosthetic and central (wire-related) aortic regurgitation after implantation of an Edwards SAPIEN valve (TEE, midesophageal aortic valve, long-
axis view). Ao ¼ aorta; LA ¼ left atrium; LVOT ¼ left ventricular outflow tract; TEE ¼ transesophageal echocardiography. From Klein AA, Skubas NJ, Ender J:
Controversies and complications in the perioperative management of transcatheter aortic valve replacement. Anesth Analg 2014; 119:784–98. Copyright r
2014, International Anesthesia Research Society.
allows delivery via either a 16 or 19 Fr sheath. TA approaches anesthetic evaluation should also focus on degree of lung
utilize a 26 Fr delivery sheath. The CoreValve system is dif- disease to predict extubation after the procedure, airway
ferent altogether, and utilizes a self-expandable system that anatomy, overall cardiac functional status, neurological
deforms when cold and regains its shape when warmed in the status, and any history of previous anesthetic difficulties.
patient. Sizes available include 22 and 26 mm devices that are TEE is routinely used, so any esophageal pathology that
delivered via 18 or 19 Fr sheaths.34 There is more published might preclude use of TEE should be noted.
experience in the United States with the SAPIEN compared The procedural specifics for the SAPIEN valve typically
with the CoreValve, thus much of this discussion will reflect include placement of standard monitors, adequate intra-
that experience. venous (IV) access, and arterial line, followed by induction
Patient selection and preoperative evaluation for TAVR of general anesthesia and intubation with a single-lumen
varies from the typical patient for whom a multi- endotracheal tube. Frequently, this is followed by central
disciplinary team discussion and selection process is typi- access including placement of a pulmonary artery catheter
cally employed (largely on the basis of a process developed and the TEE probe. The surgical team, consisting of a
in the PARTNER trial).30,31,35 In addition to the usual cardiothoracic surgeon and an interventional cardiologist,
preoperative evaluation for AVR (i.e., symptomatic AV then obtains appropriate femoral access. A temporary
stenosis), TAVR patient selection includes the following pacing wire is placed in the RV, followed by heparinization
criteria for most centers: adequately sized aortic annulus; to an activated clotting time goal of 250 to 300 seconds.
elevated Society of Thoracic Surgeons risk score (typically Repeat imaging by TEE is routinely done to verify size
more than 9 to 10%), denial of surgery by two surgeons, or estimates of the AV annulus. A trial of rapid ventricular
both; advanced lung disease; functional coronary vessels/ pacing (RVP) is undertaken to verify adequate capture, but
grafts; degree of frailty; functional status; and the usual this also gives the anesthesiologist a sense of how the pa-
comorbidities of diabetes, renal disease, and coronary ar- tient will respond once RVP is terminated. Often, there is a
tery disease. Exclusion criteria may include advanced liver 1- or 2-minute period of hypotension after RVP, which
disease, advanced dementia, severe mitral valve disease, may require vasopressors such as phenylephrine or epi-
severe LV failure, nonrevascularized severe coronary ar- nephrine. Often it is helpful to elevate the systolic blood
tery disease, pulmonary hypertension, severe arrhythmias pressure slightly above baseline (to 130 to 140 mmHg)
(atrial fibrillation), and severe chronic obstructive pulmo- before RVP. Once the delivery sheaths are placed, AV bal-
nary disease.34,35 The next phase of diagnostics includes loon valvuloplasty is performed. Next, the device is in-
evaluation of the aortic annulus, typically via transthoracic serted retrograde through the aorta and positioned across
echocardiography or TEE, in addition to computerized the AV annulus with confirmation by TEE and fluoros-
tomography and angiography. Additional critical details copy. RVP from 160 to 200 bpm is then initiated to reduce
are evaluation of the femoral and iliac vessels to determine LV ejection, typically reducing the systolic blood pressure
degree of tortuosity, caliber, and atherosclerotic burden to to 60 to 80 mmHg and pulse pressures to 20 to 30 mmHg.
determine the feasibility of the TF approach.34,35 Pre- During this time, respirations are usually held as well to
Copyright r 2015 American Society of Anesthesiologists. All rights reserved.
126 We i t z e l
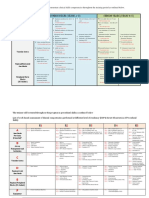
Table 5. Summary of Key Anesthesia Management Factors key to success for anesthesia
Points for TAVR34
management include identifying specific risk
Intervention/
Procedure Anesthetic Management Points* areas for each patient and planning how best
TAVR General anesthesia—but possible with local to counteract them with the knowledge of the
anesthesia and sedation
Arterial line þ TEE monitoring planned procedure.
Adequate IV access required; central access and
possible PAC
Type and cross-match with products immediately
Anesthetic planning for any procedure must take into
available
account a working knowledge of known or possible com-
Cardiothoracic surgeon participation/availability
plications. The list of complications for TAVR includes
Perfusion standby peripheral vascular injury, paravalvular leak, rupture of
Cardiac anesthesiologist† the annulus, heart block, coronary artery occlusion or
*All cases should have standard ASA monitoring in place. Specific anesthesia compromise leading to ischemia, stroke, bleeding, device
planning should be based on individual medical conditions and may be altered
from these recommendations. malposition, and low-output cardiac syndrome after
†There is current debate surrounding whether cardiothoracic anesthesiolo- RVP.32–35 Factors key to success for anesthesia manage-
gists should staff these cases, and the decision may depend on whether
cardiology versus anesthesiology is performing TEE. ment include identifying specific risk areas for each patient
ASA ¼ American Society of Anesthesiologists; IV ¼ intravenous; PAC ¼ pulmo- and planning how best to counteract them with the
nary artery catheter; TAVR ¼ transcatheter aortic valve replacement; TEE ¼
transesophageal echocardiography. knowledge of the planned procedure (Table 5). Also crit-
ical is TEE imaging of the device and device placement,
which may be done by the anesthesia team or a cardiology
team, depending on the scenario. Discussion is encouraged
regarding management with general anesthesia versus IV
reduce patient motion and to allow for the most ideal de- sedation for TAVR, especially since a number of studies
ployment conditions. Immediately after deployment, at- using IV sedation have been published. A recent meta-
tention is focused on resolution of hemodynamics as well analysis that spans seven nonrandomized studies, includ-
as evaluation by TEE and fluoroscopy for proper seating of ing more than 1,500 patients, indicates that the 30-day
the prosthetic valve, degree of paravalvular leak (if any), mortality did not differ between the general anesthesia
pericardial effusion, and any evidence of compromise of versus IV sedation groups.36 One obvious challenge to IV
coronary flow. Occasionally, repeat balloon stenting of the sedation includes lack of TEE capability, as these are
valve is employed to treat paravalvular leak, which re- lengthy procedures and the patient will not tolerate the
quires additional RVP. TEE probe for that duration. Reported advantages of IV
The overall procedure is very similar for the TA sedation include reduced hospital stay, reduced ventilator-
approach, with the obvious exception of the need for associated pneumonia, and shorter overall procedure
minithoracotomy and direct cannulation of the LV apex. times. Given the lack of randomized trials, the authors
TAVR management by the TA approach follows the same were hesitant to make sweeping conclusions, but suggest
induction and monitoring plans as for TF and, like TF, uses that either approach may be appropriate on the basis of
a single-lumen endotracheal tube and two-lung ven- patient, provider, and system preferences. Finally, dis-
tilation. The LV apex is exposed surgically and punctured cussion with the patient and the care team should include
with a needle, a finder wire is then placed into the LV (with the backup plan should there be a severe complication.
visual confirmation by TEE), and the valvuloplasty sheath Often, sternotomy, cardiopulmonary bypass, and SAVR
is introduced, all followed by the deployment sheath. RVP comprise the backup plan, but some patients and surgeons
is utilized as in the TF procedure, and the same consid- may refuse this option.
erations apply. Advantages include no risk of iliac or aortic
intervention, which can be critical in patients with severe
atherosclerosis, as well as an ideal placement angle for the
device.34 Disadvantages include pain associated with the
need for a thoracotomy, risk of myocardial damage, and
CONCLUSIONS
risk of severe bleeding from the LV apex. Initial results Catheter-based cardiac surgery represents an ever-growing
seemed to demonstrate some differences in outcomes be- frontier for anesthesiologists. As techniques improve, pa-
tween TA and TF; however, recent larger-scale and longer- tient volumes will likely follow, and a working knowledge
term studies appear to indicate that procedural success, of these complex procedures is required for appropriate
short-term and long-term mortality, and stroke outcomes anesthetic planning (Supplemental Digital Content 5,
are similar between these two groups.34 http://links.lww.com/ASA/A566).
Copyright r 2015 American Society of Anesthesiologists. All rights reserved.
Catheter-based Cardiac Surgery 127
REFERENCES fibrillation: 2.3-year follow-up of the PROTECT AF (Watchman Left
Atrial Appendage System for Embolic Protection in Patients with
1. Gruntzig AR, Senning A, Siegenthaler WE: Nonoperative dilatation Atrial Fibrillation) trial. Circulation 2013; 127:720–9.
of coronary-artery stenosis: Percutaneous transluminal coronary 19. Fountain RB, Holmes DR, Chandrasekaran K, et al.: The PROTECT
angioplasty. N Engl J Med 1979; 301:61–8. AF (WATCHMAN Left Atrial Appendage System for Embolic
2. Crossley GH, Poole JE, Rozner MA, et al.: The Heart Rhythm Society PROTECTion in Patients with Atrial Fibrillation) trial. Am Heart J
(HRS)/American Society of Anesthesiologists (ASA) expert consensus 2006; 151:956–61.
statement on the perioperative management of patients with 20. Nietlispach F, Gloekler S, Krause R, et al.: Amplatzer left atrial
implantable defibrillators, pacemakers and arrhythmia monitors: appendage occlusion: Single center 10-year experience. Catheter
facilities and patient management. Heart Rhythm 2011; 8:1114–54. Cardiovasc Interv 2013; 82:283–9.
3. Haines DE, Beheiry S, Akar JG, et al.: Heart Rhythm Society expert 21. Shetty R, Leitner JP, Zhang M: Percutaneous catheter-based left atrial
consensus statement on electrophysiology laboratory standards: appendage ligation and management of periprocedural left atrial
process, protocols, equipment, personnel, and safety. Heart Rhythm appendage perforation with the LARIAT suture delivery system. J
2014; 11:e9–51. Invasive Cardiol 2012; 24:E289–93.
4. Wilkoff BL, Byrd CL, Love CJ, et al.: Pacemaker lead extraction with 22. Bartus K, Han FT, Bednarek J, et al.: Percutaneous left atrial
the laser sheath: Results of the Pacing Lead Extraction with the appendage suture ligation using the LARIAT device in patients with
Excimer Sheath (PLEXES) Trial. J Am Coll Cardiol 1999; 33:1671–6. atrial fibrillation: Initial clinical experience. J Am Coll Cardiol 2013;
5. Byrd CL, Wilkoff BL, Love CJ, Sellers TD, Reiser C: Clinical study of 62:108–18.
the laser sheath for lead extraction: The total experience in the 23. Price MJ, Gibson DN, Yakubov SJ, et al.: Early safety and efficacy of
United States. Pacing Clin Electrophysiol 2002; 25:804–8. percutaneous left atrial appendage suture ligation: Results from the
6. Gaca JG, Lima B, Milano CA, et al.: Laser-assisted extraction of U.S. Transcatheter LAA Ligation Consortium. J Am Coll Cardiol
pacemaker and defibrillator leads: The role of the cardiac surgeon. 2014; 64:565–72.
Ann Thorac Surg 2009; 87:1446–50. 24. Alfieri O, Maisano F, De Bonis M, Stefano PL, Torracca L,
7. Brunner MP, Cronin EM, Duarte VE, et al.: Clinical predictors of Oppizzi M, La Canna G. The double-orifice technique in mitral
adverse patient outcomes in an experience of more than 5000 chronic valve repair: A simple solution for complex problems. J Thorac
endovascular pacemaker and defibrillator lead extractions. Heart Cardiovasc Surg 2001; 122:674–81.
Rhythm 2014; 11:799–805. 25. Feldman T, Foster E, Glower DD, et al.: Percutaneous repair or
8. Moon MR, Camillo CJ, Gleva MJ: Laser-assist during extraction of surgery for mitral regurgitation. N Engl J Med 2011; 364:
chronically implanted pacemaker and defibrillator leads. Ann Thorac 1395–406.
Surg 2002; 73:1893–6. 26. Whitlow PL, Feldman T, Pedersen WR, et al.: Acute and 12-month
9. Roux JF, Page P, Dubuc M, et al.: Laser lead extraction: Predictors of results with catheter-based mitral valve leaflet repair: The EVEREST
success and complications. Pacing Clin Electrophysiol 2007; II (Endovascular Valve Edge-to-Edge Repair) High Risk Study. J Am
30:214–20. Coll Cardiol 2012; 59:130–9.
10. Smith HJ, Fearnot NE, Byrd CL, et al.: Five-years experience with 27. Wan B, Rahnavardi M, Tian DH, et al.: A meta-analysis of MitraClip
intravascular lead extraction. U.S. Lead Extraction Database. Pacing system versus surgery for treatment of severe mitral regurgitation.
Clin Electrophysiol 1994; 17:2016–20. Ann Cardiothorac Surg 2013; 2:683–92.
11. Lawton JS, Moon MR, Curci JA, et al.: Management of arterial 28. Cribier A, Eltchaninoff H, Bash A, et al.: Percutaneous transcatheter
injuries caused by laser extraction of indwelling venous pace implantation of an aortic valve prosthesis for calcific aortic stenosis:
maker and defibrillator leads. Pacing Clin Electrophysiol 2006; First human case description. Circulation 2002; 106:3006–8.
29:917–20. 29. Rodes-Cabau J, Webb JG, Cheung A, et al.: Transcatheter aortic
12. Jones SO, Eckart RE, Albert CM, Epstein LM: Large, single-center, valve implantation for the treatment of severe symptomatic aortic
single-operator experience with transvenous lead extraction: Out- stenosis in patients at very high or prohibitive surgical risk: Acute and
comes and changing indications. Heart Rhythm 2008; 5:520–5. late outcomes of the multicenter Canadian experience. J Am Coll
13. Shanewise JS, Cheung AT, Aronson S, et al.: ASE/SCA guidelines for Cardiol 2010; 55:1080–90.
performing a comprehensive intraoperative multiplane transesopha- 30. Leon MB, Smith CR, Mack M, et al.: Transcatheter aortic-valve
geal echocardiography examination: Recommendations of the implantation for aortic stenosis in patients who cannot undergo
American Society of Echocardiography Council for Intraoperative surgery. N Engl J Med 2010; 363:1597–607.
Echocardiography and the Society of Cardiovascular Anesthesiolo- 31. Smith CR, Leon MB, Mack MJ, et al.: Transcatheter versus surgical
gists Task Force for Certification in Perioperative Transesophageal aortic-valve replacement in high-risk patients. N Engl J Med 2011;
Echocardiography. Anesth Analg 1999; 89:870–84. 364:2187–98.
14. Glover BM, Watkins S, Mariani JA, et al.: Prevalence of tricuspid 32. Kodali SK, Williams MR, Smith CR, et al.: Two-year outcomes after
regurgitation and pericardial effusions following pacemaker and transcatheter or surgical aortic-valve replacement. N Engl J Med
defibrillator lead extraction. Int J Cardiol 2010; 145:593–4. 2012; 366:1686–95.
15. Massumi A, Chelu MG, Nazeri A, et al.: Initial experience with a 33. Makkar RR, Fontana GP, Jilaihawi H, et al.: Transcatheter aortic-
novel percutaneous left atrial appendage exclusion device in patients valve replacement for inoperable severe aortic stenosis. N Engl J Med
with atrial fibrillation, increased stroke risk, and contraindications to 2012; 366:1696–704.
anticoagulation. Am J Cardiol 2013; 111:869–73. 34. Alfirevic A, Mehta AR, Svensson LG: Transcatheter aortic valve
16. Sakellaridis T, Argiriou M, Charitos C, et al.: Left atrial appendage replacement. Anesthesiol Clin 2013; 31:355–81.
exclusion—Where do we stand? J Thorac Dis 2014; 6:S70–7. 35. Svensson LG, Tuzcu M, Kapadia S, et al.: A comprehensive review
17. Moss JD: Left atrial appendage exclusion for prevention of stroke in of the PARTNER trial. J Thorac Cardiovasc Surg 2013; 145:
atrial fibrillation: Review of minimally invasive approaches. Curr S11–6.
Cardiol Rep 2014; 16:448–51. 36. Fröhlich GM, Lansky AJ, Webb J, et al.: Local versus general
18. Reddy VY, Doshi SK, Sievert H, et al.: Percutaneous left atrial anesthesia for transcatheter aortic valve implantation (TAVR)—
appendage closure for stroke prophylaxis in patients with atrial Systematic review and meta-analysis. BMC Med 2014; 12:41.
Copyright r 2015 American Society of Anesthesiologists. All rights reserved.
You might also like
- Aneurysm Abdominal AortaDocument8 pagesAneurysm Abdominal AortaMochammad Halim NNo ratings yet
- JTD 13 03 1886Document13 pagesJTD 13 03 1886Nongnapat KettungmunNo ratings yet
- Guidelines TAVI TAVRDocument15 pagesGuidelines TAVI TAVRRossellaDisalvo100% (1)
- 1 s2.0 S1053077022007510 MainDocument16 pages1 s2.0 S1053077022007510 MainCristhian BastidasNo ratings yet
- Article AVI in UKDocument10 pagesArticle AVI in UKFaddy OrahaNo ratings yet
- Part IX: Vascular Surgery: Renal and Spinal Cord ProtectionDocument1 pagePart IX: Vascular Surgery: Renal and Spinal Cord ProtectioncesaliapNo ratings yet
- Transcatheteraorticvalve Replacement: Procedure and OutcomesDocument14 pagesTranscatheteraorticvalve Replacement: Procedure and OutcomesernestoNo ratings yet
- DedicateDocument7 pagesDedicatefelipeNo ratings yet
- Resuscitativeendovascular Balloonocclusionofthe Aorta:: A Practical ReviewDocument18 pagesResuscitativeendovascular Balloonocclusionofthe Aorta:: A Practical ReviewJulian SanchezNo ratings yet
- Ulnar Acces 2006Document10 pagesUlnar Acces 2006Rodrigo MartinNo ratings yet
- Eco DopplerDocument8 pagesEco DopplerClaudia IsabelNo ratings yet
- CHD BookDocument13 pagesCHD BookSanskruthi KurniNo ratings yet
- Kim2012Document5 pagesKim2012Stefanie MelisaNo ratings yet
- Tavi SurgeryDocument10 pagesTavi Surgeryapi-683799701No ratings yet
- AnnCardAnaesth15154-6423638_175036Document10 pagesAnnCardAnaesth15154-6423638_175036ElenaCondratscribdNo ratings yet
- Transesophageal Echocardiography: The Hemodynamic Monitoring UtilizingDocument14 pagesTransesophageal Echocardiography: The Hemodynamic Monitoring UtilizingvegasbabyNo ratings yet
- FormosJSurg51250-7751411 213154Document8 pagesFormosJSurg51250-7751411 213154Deddy WidjajaNo ratings yet
- Eco in Cardiac Sugrery Anesthesic 1-s2.0-S1053077020305875-MainDocument11 pagesEco in Cardiac Sugrery Anesthesic 1-s2.0-S1053077020305875-MainCésar Marriaga ZárateNo ratings yet
- Pen Surgery For Thoracoabdominal Aortic Aneurysm-Is It Still A Horrible SurgeryDocument11 pagesPen Surgery For Thoracoabdominal Aortic Aneurysm-Is It Still A Horrible SurgeryJonathan Frimpong AnsahNo ratings yet
- Percutaneous Aortic Valve Implantation: The Anesthesiologist PerspectiveDocument11 pagesPercutaneous Aortic Valve Implantation: The Anesthesiologist Perspectiveserena7205No ratings yet
- Ecocardiografia Monitoreo Hemodinamico en Critico..Document12 pagesEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNo ratings yet
- Transcatheter Aortic Valve Replacement: Procedure and Outcomes 2-2020Document14 pagesTranscatheter Aortic Valve Replacement: Procedure and Outcomes 2-2020Sergio MuryanNo ratings yet
- ct- cardiac tamponade 2013Document5 pagesct- cardiac tamponade 2013floNo ratings yet
- uCQiPF SdarticleDocument7 pagesuCQiPF Sdarticlequijybo42No ratings yet
- BookDocument21 pagesBookShaastieNo ratings yet
- Cardiac CatheterizationDocument9 pagesCardiac CatheterizationAnurag Gupta100% (1)
- Arritmia SVDocument17 pagesArritmia SVCésar Lobo TarangoNo ratings yet
- 2022 - Anesthetic Management For Open Thoracoabdominal and Abdominal Aortic Aneurysm RepairDocument14 pages2022 - Anesthetic Management For Open Thoracoabdominal and Abdominal Aortic Aneurysm RepairLaura Camila RiveraNo ratings yet
- Pleural Procedures in Critically Ill PatientsDocument9 pagesPleural Procedures in Critically Ill PatientsFlávio VillaNo ratings yet
- s13089 022 00286 2Document11 pagess13089 022 00286 2Maudiel BrionesNo ratings yet
- Tevar (Thoracoendovasular Aortic Repair)Document65 pagesTevar (Thoracoendovasular Aortic Repair)Hossam atefNo ratings yet
- Avoiding Common Errors in The EdDocument18 pagesAvoiding Common Errors in The EdHandrian RahmanNo ratings yet
- Atlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosFrom EverandAtlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosNo ratings yet
- Aaa RotoDocument11 pagesAaa RotoKarely TapiaNo ratings yet
- Computer-Assisted Transcatheter Heart Valve Implantation in Valve-in-Valve ProceduresDocument8 pagesComputer-Assisted Transcatheter Heart Valve Implantation in Valve-in-Valve ProceduresrédaNo ratings yet
- European Guidelines On Perioperative Venous.6Document4 pagesEuropean Guidelines On Perioperative Venous.6ionut.andruscaNo ratings yet
- Journal Reading Transcatheter Aortic Valve Replacement Under Monitored Anesthesia Care Versus General Anesthesia With IntubationDocument23 pagesJournal Reading Transcatheter Aortic Valve Replacement Under Monitored Anesthesia Care Versus General Anesthesia With IntubationTomy SandriyaNo ratings yet
- Biology Project TheoryDocument16 pagesBiology Project TheoryAntra ashraNo ratings yet
- Transcatheter Mitral Valve-in-Valve Therapy: Jose F. Condado,, Brian Kaebnick,, Vasilis BabaliarosDocument7 pagesTranscatheter Mitral Valve-in-Valve Therapy: Jose F. Condado,, Brian Kaebnick,, Vasilis BabaliarosA Pradana HNo ratings yet
- A Treatment Algorithm For PneumothoracesDocument5 pagesA Treatment Algorithm For Pneumothoracesnanang hidayatullohNo ratings yet
- Review Article: Computed Tomography in The Evaluation For Transcatheter Aortic Valve Implantation (TAVI)Document13 pagesReview Article: Computed Tomography in The Evaluation For Transcatheter Aortic Valve Implantation (TAVI)Paul SchoenhagenNo ratings yet
- Tavi 150923155743 Lva1 App6892Document157 pagesTavi 150923155743 Lva1 App6892Zhivka KostadinovaNo ratings yet
- Transaortic Valve ReplacementDocument11 pagesTransaortic Valve ReplacementManuela CulicaNo ratings yet
- Tavi VS Valvula Rapida ImplanteDocument13 pagesTavi VS Valvula Rapida ImplanteUTI CRUZ AZULNo ratings yet
- DCO After TAVRDocument12 pagesDCO After TAVRBogdan BotezanNo ratings yet
- Bridging Anticoagulation JACC 2015Document12 pagesBridging Anticoagulation JACC 2015Frans LiwangNo ratings yet
- Pi Is 0003497505009550Document7 pagesPi Is 0003497505009550pbchantaNo ratings yet
- 1 s2.0 S1109966616302226 Main PDFDocument6 pages1 s2.0 S1109966616302226 Main PDFdenisseNo ratings yet
- JurnalDocument6 pagesJurnalBhenNo ratings yet
- European Guidelines On Perioperative Venous.4Document6 pagesEuropean Guidelines On Perioperative Venous.4ionut.andruscaNo ratings yet
- 2011 Early Cannulation Grafts in Straight Axillo Axillary AngioaccessesDocument4 pages2011 Early Cannulation Grafts in Straight Axillo Axillary AngioaccessesKindylight KindylightNo ratings yet
- Prognostic Value of Tricuspid Valve Gradient After Transcatheter Edge-to-Edge RepairDocument12 pagesPrognostic Value of Tricuspid Valve Gradient After Transcatheter Edge-to-Edge RepairERIK EDUARDO BRICEÑO GÓMEZNo ratings yet
- Sutureless PPVS外周型Document9 pagesSutureless PPVS外周型shentujin1997No ratings yet
- Pediatric Vascular Access SelectionDocument16 pagesPediatric Vascular Access SelectionNatascha CabralNo ratings yet
- Intervencion Usg EmergenciasDocument22 pagesIntervencion Usg EmergenciasSaul Gonzalez HernandezNo ratings yet
- Supraventricular TachycardiDocument8 pagesSupraventricular TachycardiHairunisa 0049No ratings yet
- Nee TH Ling 2019Document18 pagesNee TH Ling 2019diogofc123No ratings yet
- Anesthesia For Endovascular Aortic Repair - UpToDateDocument48 pagesAnesthesia For Endovascular Aortic Repair - UpToDatematheusbbragacNo ratings yet
- Transcatheter Tricuspid Valve Interventions: Landscape, Challenges, and Future DirectionsDocument22 pagesTranscatheter Tricuspid Valve Interventions: Landscape, Challenges, and Future DirectionsgNo ratings yet
- Transcatheter Aortic Valve Replacement: A How-to Guide for Cardiologists and Cardiac SurgeonsFrom EverandTranscatheter Aortic Valve Replacement: A How-to Guide for Cardiologists and Cardiac SurgeonsNo ratings yet
- Intubacion en Paciente DespiertoDocument20 pagesIntubacion en Paciente DespiertoLalo GonzalezNo ratings yet
- 2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportDocument4 pages2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportHany ElbarougyNo ratings yet
- 2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportDocument3 pages2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportHany ElbarougyNo ratings yet
- Obstetrics and RespiratoryDocument54 pagesObstetrics and RespiratoryHany ElbarougyNo ratings yet
- 2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportDocument2 pages2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportHany Elbarougy0% (1)
- DKA Anesthesia Management. DR M MagdyDocument9 pagesDKA Anesthesia Management. DR M MagdyHany ElbarougyNo ratings yet
- AdenotonsilectomyDocument4 pagesAdenotonsilectomyHany ElbarougyNo ratings yet
- 2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportDocument2 pages2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportHany Elbarougy0% (3)
- 2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportDocument2 pages2022 Oxford Handbook of Anaesthesia Oxford Press 5th Edition ExportHany Elbarougy0% (1)
- Valoración PreanestesicaDocument5 pagesValoración PreanestesicaSebastian Hdez BolañosNo ratings yet
- R02Y2014N04A0461Document10 pagesR02Y2014N04A0461Natalija StamenkovicNo ratings yet
- Children For SurgeryDocument7 pagesChildren For SurgeryHany ElbarougyNo ratings yet
- Features: Mindray A7 Anesthesia MachineDocument2 pagesFeatures: Mindray A7 Anesthesia MachineHany ElbarougyNo ratings yet
- Approach To Fluid and Electrolyte DisordersDocument19 pagesApproach To Fluid and Electrolyte DisordersPaul KelnerNo ratings yet
- Electrolyte Disorders: Clinics in Perinatology September 2014Document17 pagesElectrolyte Disorders: Clinics in Perinatology September 2014Nada KopaNo ratings yet
- Electrolyte TextDocument16 pagesElectrolyte TextHany ElbarougyNo ratings yet
- Treatment of Electrolyte Disorders in Adult Patients in The Intensive Care UnitDocument21 pagesTreatment of Electrolyte Disorders in Adult Patients in The Intensive Care UnitBuat TugasNo ratings yet
- No. Topic Objectives: Anesthesia Residents Core ProgramDocument4 pagesNo. Topic Objectives: Anesthesia Residents Core ProgramHany ElbarougyNo ratings yet
- Providing guidance on blood transfusions in resource-limited settingsDocument7 pagesProviding guidance on blood transfusions in resource-limited settingsHany ElbarougyNo ratings yet
- Cardiac Anesthesia: Saudi Board Anesthesia CurriculumDocument6 pagesCardiac Anesthesia: Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- Neonate Intensive Care Unit (Nicu) : Saudi Board Anesthesia CurriculumDocument3 pagesNeonate Intensive Care Unit (Nicu) : Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- Communicator: Saudi Board Anesthesia CurriculumDocument5 pagesCommunicator: Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- THORACIC ANESTHESIA RESIDENCYDocument7 pagesTHORACIC ANESTHESIA RESIDENCYHany ElbarougyNo ratings yet
- Junior Years (Years 1-3) Senior Years (Years 4-5)Document4 pagesJunior Years (Years 1-3) Senior Years (Years 4-5)Hany ElbarougyNo ratings yet
- Communicator: Saudi Board Anesthesia CurriculumDocument6 pagesCommunicator: Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- Core Program (All Residents) : Saudi Board Anesthesia CurriculumDocument4 pagesCore Program (All Residents) : Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- Management of Cardiac Patients & TechniquesDocument4 pagesManagement of Cardiac Patients & TechniquesHany ElbarougyNo ratings yet
- SAUDI BOARD ExportDocument3 pagesSAUDI BOARD ExportHany ElbarougyNo ratings yet
- Chapter One: Introduction: Saudi Board Anesthesia CurriculumDocument6 pagesChapter One: Introduction: Saudi Board Anesthesia CurriculumHany ElbarougyNo ratings yet
- 543Document6 pages543Hany ElbarougyNo ratings yet
- Reflective EssayDocument5 pagesReflective Essaybwood17No ratings yet
- GeographyDocument18 pagesGeographyAshley Morgan88% (8)
- PU Timing Belt-SINOCONVE Belt 2022Document25 pagesPU Timing Belt-SINOCONVE Belt 2022Marcelo Renteria VidaurreNo ratings yet
- Geometry QuotesDocument2 pagesGeometry Quotesalecksander2005No ratings yet
- Grove RT422 22T PDFDocument4 pagesGrove RT422 22T PDFJulio QuilarqueNo ratings yet
- Quilling Letter BDocument2 pagesQuilling Letter BGueureNo ratings yet
- Air-To-Air Claims and Credits For Navy and Marine Corps Patrol Type Aircraft During World War II (Appendix 4)Document18 pagesAir-To-Air Claims and Credits For Navy and Marine Corps Patrol Type Aircraft During World War II (Appendix 4)MCGunnerNo ratings yet
- Price List Lang Technovation 02072019Document5 pagesPrice List Lang Technovation 02072019api-541004165No ratings yet
- Economics Examples of Calculus of Multivariable Function in EconomicsDocument6 pagesEconomics Examples of Calculus of Multivariable Function in Economicskayesalingay3No ratings yet
- Case 1Document6 pagesCase 1Rewaa MerwadNo ratings yet
- Experiment 91 Consumer ChemistryDocument8 pagesExperiment 91 Consumer ChemistryDascaliuc DanielNo ratings yet
- ClientleDocument1 pageClientleRaghvendra ManiNo ratings yet
- Telemecanique Integral 32 Motor StarterDocument52 pagesTelemecanique Integral 32 Motor StarterJaime IxtaNo ratings yet
- MCQs in Oral Surgery by Babu SParmarDocument517 pagesMCQs in Oral Surgery by Babu SParmarAmr KhattabNo ratings yet
- Bittersweet Tragedy - Melanie Martinez - LETRASDocument2 pagesBittersweet Tragedy - Melanie Martinez - LETRASFlávia FernandesNo ratings yet
- Calculation of Insulation Thickness For PipesDocument2 pagesCalculation of Insulation Thickness For PipesnarmathaNo ratings yet
- Edward Jumper: Willow & Lark 2017 Designed UsingDocument9 pagesEdward Jumper: Willow & Lark 2017 Designed UsingMiraNo ratings yet
- History of Nano FiltrationDocument42 pagesHistory of Nano FiltrationKieran Sexton100% (2)
- Basics For BJJ SC - V3Document20 pagesBasics For BJJ SC - V3Teo Tolo100% (2)
- ECI 80 Structural Steel DeckingDocument3 pagesECI 80 Structural Steel Deckingkishore varmaNo ratings yet
- KA350 Pilot Checklist PN-73 PDFDocument142 pagesKA350 Pilot Checklist PN-73 PDFCarlos Anderez100% (13)
- IBPhysics Particle Practice KeyDocument2 pagesIBPhysics Particle Practice KeyOnur YavuzcetinNo ratings yet
- Mswin 9Document388 pagesMswin 9KZNo ratings yet
- Citroen c3Document3 pagesCitroen c3yoNo ratings yet
- Savannah Air Cargo ComplexDocument2 pagesSavannah Air Cargo Complexsavannahnow.comNo ratings yet
- 1 Scalars and Vectors Exam Qs and MsDocument81 pages1 Scalars and Vectors Exam Qs and MsAnh TranNo ratings yet
- Industrial Pollution Crisis in GujaratDocument2 pagesIndustrial Pollution Crisis in GujaratsmagrurakNo ratings yet
- Crux v20n04 AprDocument35 pagesCrux v20n04 AprMauricioNo ratings yet
- Catalogo RobinsonDocument8 pagesCatalogo RobinsonclerigonsaNo ratings yet
- The Wall Street Journal - 24-11-2021Document30 pagesThe Wall Street Journal - 24-11-2021Samuel GiovanelliNo ratings yet