Professional Documents
Culture Documents
Wearing An N95 Respiratory Mask: An Unintended Exercise Benefit?
Uploaded by
Nicolas CasanovaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wearing An N95 Respiratory Mask: An Unintended Exercise Benefit?
Uploaded by
Nicolas CasanovaCopyright:
Available Formats
CORRESPONDENCE
Wearing an N95 vomiting.4 Simultaneously, the augmented resistance to
inspiratory (15% of maximum) and expiratory flow, when
Respiratory Mask experienced for greater than 10 min, results in respiratory
alkalosis, increased lactate levels, fatigue, and impaired
physical work capacity.5
An Unintended Exercise Benefit? However, a number of exercise benefits can be achieved
with surprisingly low effort while wearing an N95 mask. At
2 metabolic equivalents, the inspiratory resistance load of 6
to 7 cm H2O (4.5 to 5 mmHg; normal, 1.3 mmHg [men]
to 1.6 mmHg [women]) of an N95 mask creates a “respira-
To the Editor: tory pump” that decreases intrathoracic, central venous, and
T he N95 or higher-level respirator is an essential ele- intracranial pressures,6 and increases preload, cardiac output,
ment of personal protective equipment to be worn and mean arterial pressure, particularly during hypotensive
when in contact with patients with known or suspected states.7 At 4 metabolic equivalents, consciously taking 30
coronavirus disease 2019 (COVID-19) infection. Three dynamic (fast in) inspiratory efforts twice daily for 4 weeks
varieties are commonly available: preformed/cup, flat fold/ increases respiratory muscle strength. Maintaining 4 meta-
duck bill, and elastomeric.1 Wearing an N95 mask invokes bolic equivalents of activity for 10 to 30 min, 3 to 5 days/
a number of physiologic implications, particularly with week for 4 weeks improves respiratory muscle endurance.
prolonged use (greater than 1 h), higher workloads, or an Such conditioning of respiratory muscle strength and respi-
overlying surgical mask (table 1).2,3 Concomitant surgical ratory muscle endurance improves ventilatory efficiency
mask use augments the impact of a cup mask due to further (e.g., ventilation-perfusion and alveolar capillary exchange),
resistance to airflow, but diminishes the impact of a flat fold oxygen delivery/lactate removal at locomotor muscles, and
mask due to a reduction in deadspace.2 overall exercise performance.5
At 2 metabolic equivalents (e.g., walking slowly during Taken together, to inspire us as we don, sustain us as we
rounds), N95 mask use noticeably increases inhaled car- wear, and cheer us as we doff our N95 masks, we should
bon dioxide, reduces inspired oxygen, and increases the relish in the many beneficial attributes that are possible “all
work of breathing. The resulting inhaled carbon dioxide in a day’s work.”
of 2 to 3% (normal, 0.04%) produces transient acidosis
and compensatory increases in minute ventilation, work Research Support
of breathing, and cardiac output.2 Symptoms include
Support was provided solely from institutional and/or
sweating, visual changes, headache, dyspnea, increased
departmental sources.
irritability, and decreased reasoning, alertness, and exercise
endurance.3 Independently, the inspired oxygen of 17%
(normal, 21%), yields headache, lightheadedness, drowsi- Competing Interests
ness, muscular weakness, dyspnea on exertion, nausea, and The authors declare no competing interests.
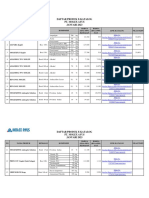
Table 1. Physiologic Implications of N95 Mask Use
Inhaled Carbon Inhaled Peak Inhalation Peak Exhalation
Workload Mask Type Dioxide (%) Oxygen (%) Pressure (mmHg) Pressure (mmHg)
2 Metabolic equivalents Cup 2.49 ± 0.51 17.40 ± 0.81 −6 ± 1 8±2
Cup + surgical mask 2.93 ± 0.38 16.81 ± 0.54 −7 ± 2 8±2
Flat-fold 3.52 ± 0.93 16.10 ± 1.14 −5 ± 2 7±2
Flat-fold + surgical mask 3.14 ± 0.64 16.52 ± 0.79 −6 ± 2 8±2
8 Metabolic equivalents Cup 1.43 ± 0.60 19.33 ± 0.70 −35 ± 6 23 ± 7
Cup + surgical mask 1.75 ± 0.33 18.96 ± 0.37 −41 ± 7 29 ± 7
Flat-fold 1.81 ± 0.82 18.92 ± 0.84 −34 ± 10 24 ± 4
Flat-fold + surgical mask 1.67 ± 0.33 19.05 ± 0.35 −43 ± 16 30 ± 8
Data from Sinkule et al.2
Copyright © 2020, the American Society of Anesthesiologists, Inc. All Rights Reserved. Anesthesiology 2020; XXX:00–00
ANESTHESIOLOGY, V XXX • NO XXX xxx 2020 1
Copyright © 2020, the American Society of Anesthesiologists,
<zdoi; Inc. Unauthorized reproduction of this article is prohibited.
DOI: 10.1097/ALN.0000000000003421>
CORRESPONDENCE
Bryan A. Davis, M.D., M.A., Lawrence C. Tsen, M.D. Brigham among medical intensive care unit nurses. Am J Infect
and Women’s Hospital, Harvard Medical School, Boston, Control 2013; 41:1218–23
Massachusetts (L.C.T.). ltsen@bwh.harvard.edu. 4. Schulte JH: Sealed environments in relation to health
and disease. Arch Environ Health 1964; 8:438–52
DOI: 10.1097/ALN.0000000000003421 5. Álvarez-Herms J, Julià-Sánchez S, Corbi F, Odriozola-
Martínez A, Burtscher M: Putative role of respiratory
References muscle training to improve endurance performance in
hypoxia: A review. Front Physiol 2018; 9:1970
1. Centers for Disease Control and Prevention (NPPTL): 6. Convertino VA: Mechanisms of inspiration that modu-
Respirator Trusted-Source Information. Section 1: late cardiovascular control: The other side of breathing.
NIOSH-Approved Respirators. Available at: https:// J Appl Physiol (1985) 2019; 127:1187–96
www.cdc.gov/niosh/npptl/topics/respirators/disp_ 7. Skytioti M, Søvik S, Elstad M: Respiratory pump
part/respsource.html. Accessed April 18, 2020. maintains cardiac stroke volume during hypovolemia
2. Sinkule EJ, Powell JB, Goss FL: Evaluation of N95 in young, healthy volunteers. J Appl Physiol (1985)
respirator use with a surgical mask cover: effects on 2018; 124:1319–25
breathing resistance and inhaled carbon dioxide. Ann
Occup Hyg 2013; 57:384–98 (Accepted for publication May 18, 2020.)
3. Rebmann T, Carrico R, Wang J: Physiologic and other
effects and compliance with long-term respirator use
2 Anesthesiology 2020; XXX:00–00 Correspondence
Copyright © 2020, the American Society of Anesthesiologists, Inc. Unauthorized reproduction of this article is prohibited.
You might also like
- Artigo 1 - Uso de MáscarasDocument9 pagesArtigo 1 - Uso de MáscarascathyNo ratings yet
- The Frozen ShoulderDocument27 pagesThe Frozen Shoulderleenadevi90No ratings yet
- Andumedic3 From Body and Mind Studio UkDocument28 pagesAndumedic3 From Body and Mind Studio UkAmalia AraújoNo ratings yet
- Guillen Sola2016Document11 pagesGuillen Sola2016augustoNo ratings yet
- Hijama 1-4 FinalDocument4 pagesHijama 1-4 FinalAsaad AlnhayerNo ratings yet
- Intravenous Lidocaine As A Suppressant of Coughing During Tracheal Intubation - Yukioka Et AlDocument4 pagesIntravenous Lidocaine As A Suppressant of Coughing During Tracheal Intubation - Yukioka Et AlnejdNo ratings yet
- L04 - Part LL Updated Oxygen TherapyDocument12 pagesL04 - Part LL Updated Oxygen TherapyTariku GebreNo ratings yet
- Airway Clearance Techniques in Neuromuscular Disorders Toussaint 2017Document10 pagesAirway Clearance Techniques in Neuromuscular Disorders Toussaint 2017Gustavo OlguinNo ratings yet
- FR+x+a +Seco+No+Escaleno+2014Document8 pagesFR+x+a +Seco+No+Escaleno+2014Rafel FisioNo ratings yet
- Máscaras Faciales y La Respuesta Cardiorrespiratoria A La Actividad Física en La Salud y La EnfermedadDocument19 pagesMáscaras Faciales y La Respuesta Cardiorrespiratoria A La Actividad Física en La Salud y La EnfermedadFelipe MartinezNo ratings yet
- What Is Dry Needling MaDocument6 pagesWhat Is Dry Needling MaElanghovan ArumugamNo ratings yet
- Bess On Ne Au and Thomas 2012Document13 pagesBess On Ne Au and Thomas 2012Quoc LongNo ratings yet
- SR22630160310Document4 pagesSR22630160310Mohitha ParlaNo ratings yet
- Using of Cupping Technique As A Therapeutic Model in Treatment of Non-Discogenic Low Back PainDocument11 pagesUsing of Cupping Technique As A Therapeutic Model in Treatment of Non-Discogenic Low Back PainIJAR JOURNALNo ratings yet
- Classification of Cupping Therapy A ToolDocument10 pagesClassification of Cupping Therapy A ToolHenrique CaldasNo ratings yet
- Edgar Cayce’s Quick & Easy Remedies: A Holistic Guide to Healing Packs, Poultices and Other Homemade RemediesFrom EverandEdgar Cayce’s Quick & Easy Remedies: A Holistic Guide to Healing Packs, Poultices and Other Homemade RemediesNo ratings yet
- Administering Oxygen by MaskDocument5 pagesAdministering Oxygen by MaskAndrea Bayaga WaganNo ratings yet
- Complementary Therapies in Clinical PracticeDocument4 pagesComplementary Therapies in Clinical Practicedwi putri ratehNo ratings yet
- Hand Reflexology & Acupressure: A Natural Way to Health through Traditional Chinese MedicineFrom EverandHand Reflexology & Acupressure: A Natural Way to Health through Traditional Chinese MedicineRating: 5 out of 5 stars5/5 (2)
- A Practical Guide To Nebulization TherapyDocument24 pagesA Practical Guide To Nebulization TherapySidhartha Satapathy100% (2)
- Lerch 2020 AchillestendonDocument10 pagesLerch 2020 AchillestendonIvor Wiguna Hartanto WilopoNo ratings yet
- A Review of Analgesic and Emotive Breathing A Multidisciplinary ApproachDocument6 pagesA Review of Analgesic and Emotive Breathing A Multidisciplinary ApproachTeresa BeckNo ratings yet
- IJRR0020Document4 pagesIJRR0020ZANDRA LAVANYA A/P ISAC DEAVADAS STUDENTNo ratings yet
- JPR 11 3151Document10 pagesJPR 11 3151Andani TNo ratings yet
- Amandadevine Thebenefitsofchiropracticadjustment 2Document5 pagesAmandadevine Thebenefitsofchiropracticadjustment 2api-506525329No ratings yet
- Cupping Therapy An Alternative Method ofDocument5 pagesCupping Therapy An Alternative Method ofKhadiga AhmadNo ratings yet
- Of Hydrotherapy: Approved by The Oxford School of Chiropractic LTDDocument31 pagesOf Hydrotherapy: Approved by The Oxford School of Chiropractic LTDnellbell1100% (1)
- 02 KnightDocument5 pages02 Knightcristina ArraisNo ratings yet
- SYSTEMATIC REVIEW ArticleDocument33 pagesSYSTEMATIC REVIEW ArticleOui AnyNo ratings yet
- Yo MPDocument4 pagesYo MPRo KohnNo ratings yet
- 2010 Effectiveness of Small Daily Amounts of Progressive Resistance Training For Frequent Neck-Shoulder Pain, Randomised Controlled TrialDocument7 pages2010 Effectiveness of Small Daily Amounts of Progressive Resistance Training For Frequent Neck-Shoulder Pain, Randomised Controlled TrialDiego Enrique Venegas TipianNo ratings yet
- A Comparative Study To Find Out The Effects of Capsular Stretching Over Muscle Energy Technique in The Management of Frozen ShoulderDocument50 pagesA Comparative Study To Find Out The Effects of Capsular Stretching Over Muscle Energy Technique in The Management of Frozen ShoulderjojiNo ratings yet
- Major Project 1Document8 pagesMajor Project 1Pranav SinghNo ratings yet
- Intramuscular Injection TechniquesJOURNALDocument11 pagesIntramuscular Injection TechniquesJOURNALHida Tri NurrochmahNo ratings yet
- Medi 99 E19152Document5 pagesMedi 99 E19152AdeevaNo ratings yet
- Clinician Well-BeingDocument5 pagesClinician Well-BeingPolat CanbolatNo ratings yet
- NL Handout 2013-03-05 PDFDocument21 pagesNL Handout 2013-03-05 PDFsilkofosNo ratings yet
- The Effect of An Integrated Multidisciplinary Rehabilitation Programme For Patients With Chronic Low Back Pain: Long-Term Follow Up of A Randomised Controlled TrialDocument10 pagesThe Effect of An Integrated Multidisciplinary Rehabilitation Programme For Patients With Chronic Low Back Pain: Long-Term Follow Up of A Randomised Controlled TrialOliver JimenezNo ratings yet
- Comparative Study of Myofascial Release and Cold Pack in Upper Trapezius SpasmDocument9 pagesComparative Study of Myofascial Release and Cold Pack in Upper Trapezius SpasmNovella FauduNo ratings yet
- CPR 211003133129Document44 pagesCPR 211003133129Patricia CaladoNo ratings yet
- Effectiveness of Small Daily Amounts of Progressive Resistance Training For Frequent Neck/shoulder Pain: Randomised Controlled TrialDocument7 pagesEffectiveness of Small Daily Amounts of Progressive Resistance Training For Frequent Neck/shoulder Pain: Randomised Controlled TrialkineluzaNo ratings yet
- Cupping Biomechanical PDFDocument11 pagesCupping Biomechanical PDFJoana ValenteNo ratings yet
- Freynet2016 PDFDocument2 pagesFreynet2016 PDFdesthalia cyatraningtyasNo ratings yet
- SoftTissueMobilizationTechniques Foster PDFUpdateDocument11 pagesSoftTissueMobilizationTechniques Foster PDFUpdatemalindamaureen75No ratings yet
- Spontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordDocument2 pagesSpontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordKhanh Ha NguyenNo ratings yet
- The Role of Cupping Therapy in Pain Management A LDocument19 pagesThe Role of Cupping Therapy in Pain Management A LMohitha Parla100% (1)
- Journal of Acupuncture and Meridian StudiesDocument5 pagesJournal of Acupuncture and Meridian StudiesmtamilmaniNo ratings yet
- OSCADocument146 pagesOSCAGamiHiokNo ratings yet
- Advances in Mechanical Ventilation 4AH PDFDocument11 pagesAdvances in Mechanical Ventilation 4AH PDFsérgio_nakano_2No ratings yet
- Intradermal Mesotherapy Versus Intravenous DexketoDocument9 pagesIntradermal Mesotherapy Versus Intravenous DexketoMetin SabuncuNo ratings yet
- Effects of Low Level Laser Therapy Vs Ultrasound Therapy in The Management of Active Trapezius Trigger PointsDocument12 pagesEffects of Low Level Laser Therapy Vs Ultrasound Therapy in The Management of Active Trapezius Trigger PointsABIN ABRAHAM MAMMEN (PHYSIOTHERAPIST)No ratings yet
- MinimizingDocument5 pagesMinimizingAryananda Kondre AndikaNo ratings yet
- The Effectiveness of Eccentric Exercise Training On Pain and Disability in Supraspinatus Tendinopathy in Adjunct To Conventional Physical Therapy A Quasi-Experimental StudyDocument7 pagesThe Effectiveness of Eccentric Exercise Training On Pain and Disability in Supraspinatus Tendinopathy in Adjunct To Conventional Physical Therapy A Quasi-Experimental StudyInternational Journal of Innovative Science and Research Technology100% (1)
- NCP CoughDocument4 pagesNCP CoughKingJayson Pacman06No ratings yet
- Curso Liberação 8Document8 pagesCurso Liberação 8IzabelNo ratings yet
- KTLBPtrial JoP2014Document8 pagesKTLBPtrial JoP2014Ju ChangNo ratings yet
- Working With Headaches Part I: Musculoskeletal Headaches (Myofascial Techniques)Document5 pagesWorking With Headaches Part I: Musculoskeletal Headaches (Myofascial Techniques)Advanced-Trainings.com100% (5)
- The Healing Effect of Pistacia Lentiscus Fruit Oil On Laser Burnpharmaceutical BiologyDocument9 pagesThe Healing Effect of Pistacia Lentiscus Fruit Oil On Laser Burnpharmaceutical BiologyRihabNo ratings yet
- Neutralizing Antibodies in Patients With Severe Acute Respiratory Syndrome-Associated Coronavirus InfectionDocument8 pagesNeutralizing Antibodies in Patients With Severe Acute Respiratory Syndrome-Associated Coronavirus InfectionNicolas CasanovaNo ratings yet
- Pulmonary Post-Mortem Findings in A Large Series of COVID-19 Cases From Northern ItalyDocument11 pagesPulmonary Post-Mortem Findings in A Large Series of COVID-19 Cases From Northern ItalyfikriafisNo ratings yet
- On The Clear Evidence of The Risks To Children From Smartphone and WiFi Radio Frequency Radiation - FinalDocument20 pagesOn The Clear Evidence of The Risks To Children From Smartphone and WiFi Radio Frequency Radiation - FinalNicolas CasanovaNo ratings yet
- Clase 3 Derecho Economico LaboralDocument37 pagesClase 3 Derecho Economico LaboralNicolas CasanovaNo ratings yet
- Wave Propagation Over Flat Earth: August 2017Document9 pagesWave Propagation Over Flat Earth: August 2017Nicolas CasanovaNo ratings yet
- The Flat-Earth Approximation To The Solution of Electromagnetic Propagation in A Stratified Terrestrial AtmosphereDocument95 pagesThe Flat-Earth Approximation To The Solution of Electromagnetic Propagation in A Stratified Terrestrial AtmosphereNicolas CasanovaNo ratings yet
- The Real Measures of The Flat EarthDocument327 pagesThe Real Measures of The Flat EarthNicolas Casanova100% (2)
- Brevets Nicola Tesla CompletDocument499 pagesBrevets Nicola Tesla CompletkozlhooNo ratings yet
- Physicswallah Mediclaim BenefitDocument17 pagesPhysicswallah Mediclaim BenefitᎷᏒ ᏗᏕᏂᎥᏕᏂ ᎶᏬᎮᏖᏗNo ratings yet
- ColdDrinksandAssociatedHealthIssues PDFDocument3 pagesColdDrinksandAssociatedHealthIssues PDFKunal KumarNo ratings yet
- Peads Quiz MCQSDocument10 pagesPeads Quiz MCQSM.A. Ch.No ratings yet
- Emotional DisturbanceDocument11 pagesEmotional DisturbancekhristiemariejNo ratings yet
- 特 定 技 能 外 国 人 の 履 歴 書 Curriculum Vitae Of The Specified Skilled WorkerDocument25 pages特 定 技 能 外 国 人 の 履 歴 書 Curriculum Vitae Of The Specified Skilled WorkerAoi BaraNo ratings yet
- PM 303 Assignment Example DayCareCentre NewDocument13 pagesPM 303 Assignment Example DayCareCentre NewSalman SultanNo ratings yet
- The Sleep Solution by W. Chris Winter, M.DDocument9 pagesThe Sleep Solution by W. Chris Winter, M.DsimasNo ratings yet
- Hello G10 Semester 2Document136 pagesHello G10 Semester 2romaehab201912No ratings yet
- E60 FullDocument232 pagesE60 FullPedro PerezNo ratings yet
- Staff Selection Commission: Combined Graduate Level Examination, 2021Document3 pagesStaff Selection Commission: Combined Graduate Level Examination, 2021Akshat RNo ratings yet
- Safety Questions and AnswersDocument30 pagesSafety Questions and Answersmiaicarba86% (50)
- SodaPDF Converted KERTAS TRIAL ENGLISH PERLIS K1 SET B 2021Document14 pagesSodaPDF Converted KERTAS TRIAL ENGLISH PERLIS K1 SET B 2021Nur HafezaNo ratings yet
- Workers Welfare Standards Qatar 2022 v2Document12 pagesWorkers Welfare Standards Qatar 2022 v2Ali ImamNo ratings yet
- Bangalore DR ListDocument11 pagesBangalore DR Listkrisveli76% (42)
- Ody Temperature As Evidenced by Temperature of 38.5Document1 pageOdy Temperature As Evidenced by Temperature of 38.5Jordz PlaciNo ratings yet
- Final Agenda - Deciphering MorphologyDocument4 pagesFinal Agenda - Deciphering MorphologySaket KumarNo ratings yet
- Pathophysiology of ChorioamnionitisDocument1 pagePathophysiology of Chorioamnionitisjhobarry0% (1)
- NursingDocument6 pagesNursingMarco DadoNo ratings yet
- Group 3 200 QuestionsDocument8 pagesGroup 3 200 QuestionsLory TangpusNo ratings yet
- Imperforate Hymen With Hydrocolpos: A Case Report: TanehDocument5 pagesImperforate Hymen With Hydrocolpos: A Case Report: TanehQonny WelendriNo ratings yet
- PUSH-UPPULL-UP New PlanDocument21 pagesPUSH-UPPULL-UP New Planvictor manuel100% (1)
- Daftar Harga E-Katalog - Pt. Molex Ayus - Januari 2023-1Document2 pagesDaftar Harga E-Katalog - Pt. Molex Ayus - Januari 2023-1AmmilaMasruriRahmawatiNo ratings yet
- Krister Ann Jimenez ACTIVITY 14 ParagraphDocument17 pagesKrister Ann Jimenez ACTIVITY 14 ParagraphJamie JimenezNo ratings yet
- Donald Supers TheoryDocument20 pagesDonald Supers TheorytereNo ratings yet
- Surgical Techniques CageDocument14 pagesSurgical Techniques CageJulian VargasNo ratings yet
- LexDocument32 pagesLexThuỳ Linh Đinh TháiNo ratings yet
- FLORIDA DEPARTMENT OF CHILDREN AND FAMILIES Statement of Estimated Regulatory Costs (SERC)Document12 pagesFLORIDA DEPARTMENT OF CHILDREN AND FAMILIES Statement of Estimated Regulatory Costs (SERC)The Federalist100% (1)
- Manual Working Fallout Narcissistic AbuseDocument142 pagesManual Working Fallout Narcissistic AbuseOmega CapricorniNo ratings yet
- FlexibilidadDocument11 pagesFlexibilidadHernan RamirezNo ratings yet
- Prof - Ed Part 14 PDFDocument10 pagesProf - Ed Part 14 PDFpatrick mavNo ratings yet