Professional Documents
Culture Documents
By DR Sumit Gupta Moderator: Prof. S.Rajendra Singh
Uploaded by
Fiky setiawan0 ratings0% found this document useful (0 votes)
16 views55 pagesurodinamik, penjelasan
Original Title
urodynamicstudy-170928170356
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenturodinamik, penjelasan
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views55 pagesBy DR Sumit Gupta Moderator: Prof. S.Rajendra Singh
Uploaded by
Fiky setiawanurodinamik, penjelasan
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 55
By Dr Sumit Gupta
Moderator: Prof. S.Rajendra Singh
NORMAL LUT TWO-PHASE
FUNCTION: Storage & Voiding
Physiology of Micturition
Physiology of Micturition
• Low bladder volumes: SNS is stimulated and PNS is
inhibited.
• Bladder full: PNS stimulated (bladder contracts) SNS
inhibited (internal sphincter relaxes).
• Intravesical pressure > resistance within the urethra: urine
flows.
• Pudendal nerve innervates external sphincter.
UDS
Urodynamics describes a group of physiological tests that
are used in clinical practice to investigate abnormalities of
lower urinary tract function.
Dynamic study of transport, storage & evacuation of
urine.
Main goal of UDS: to reproduce pt.'s symptoms and
determine their cause by various tests.
UDS Armamentarium
Cystometry(most important test), filling cystometry &
voiding cystometry
Uroflowmetry
Urethral pressure studies
Pressure flow micturition studies
Video-urodynamic studies
Electromyography
INDICATIONS
Incontinence:
-incontinence in whom surgery is planned.
-mixed ,urge & stress symptoms.
-associated voiding problems.
-pts. with neurologic disorders.
INDICATIONS (contd..)
Outflow Obstruction:
-pt with LUTS, at least uroflow study.
Neurogenic bladder:
-all neurologically impaired patients with
neurogenic bladder dysfunction.
Children with voiding dysfunction:
-kids with daytime urgency and urge incontinence,
recurrent infection, reflux, or upper tract changes.
Clinical role
Characterization of detrusor function.
Evaluation of bladder outlet.
Evaluation of voiding function.
Diagnosis and characterization of neuropathy.
Three important rules before starting UDS
evaluation:
1. Decide on questions to be answered before starting a
study.
2. Design the study to answer these questions.
3. Customize the study as necessary.
Terminology for Common Urodynamic Terms and Observations
According to the International Continence
Society Standardization Subcommittee
The ICS has now defined the term urodynamic
observations to denote observations that occur during
and are measured by the urodynamics(UDS) test itself.
Two principal methods of urodynamic investigation
exist:
Conventional urodynamic studies: normally take place
in the urodynamic laboratory involving artificial
bladder filling.
Ambulatory urodynamic studies: a functional test of
the lower urinary tract using natural filling and
reproducing the subject’s everyday activities.
The following are required of both types of studies:
Intravesical pressure: the pressure within the bladder.
Abdominal pressure: the pressure surrounding the bladder; currently it
is estimated from rectal, vaginal, or extraperitoneal pressure or a bowel
stoma.
Detrusor pressure: the component of intravesical pressure created by
forces on the bladder wall that are both passive and active.
Filling cystometry: the method by which the pressure and volume
relationship of the bladder is measured during bladder filling.
Physiologic filling rate: a filling rate less than the predicted maximum.
Predicted maximum is the body weight in kilograms divided by 4 and
expressed as milliliters per minute.
Nonphysiologic filling rate: a filling rate greater than the predicted
maximum.
Urodynamic stress incontinence: noted during filling cystometry and
defined as the involuntary leakage of urine during increased abdominal
pressure in the absence of a detrusor contraction. This currently replaces
genuine stress incontinence.
Urethral pressure measurements:
Urethral pressure: the fluid pressure needed to just open a closed urethra.
Urethral pressure profile: a graph indicating the intraluminal pressure along
the length of the urethra.
Urethral closure pressure profile: the subtraction of intravesical pressure from
urethral pressure.
Maximum urethral pressure: the maximum pressure of the measured profile.
Maximum urethral closure pressure (MUCP): the maximum difference
between the urethral pressure and the intravesical pressure.
Functional profile length: the length of the urethra along which the urethral
pressure exceeds intravesical pressure in women.
Abdominal leak point pressure(ALPP): the
intravesical pressure at which urine leakage occurs
because of increased abdominal pressure in the
absence of a detrusor contraction.
Detrusor leak point pressure(DLPP): the lowest
detrusor pressure at which urine leakage occurs in the
absence of either a detrusor contraction or increased
abdominal pressure.
CYSTOMETRY
Measurement of intravesical bladder pressure during
bladder filling(measures volume-pressure relationships).
Used to assess bladder sensation, capacity, compliance,
detrusor activity.
Bladder access by transurethral catheter, or rarely by
percutaneous suprapubic tube.
Filling medium either gas (CO2) or liquid (water, saline, or
contrast material at body temp).
Liquid cystometry is more physiologic.
Ideally, filling should be performed in standing position.
CYSTOMETRY(contd...)
Bladder filling either by diuresis or filling through a catheter.
Filling
slow (up to 10 ml/min), physiologic
medium (10 to 100 ml/min)
fast (> 100 ml/min)
Children and pts with known bladder hyperactivity require
slow fill rates.
All systems should be zeroed to atmospheric pressure.
No air bubbles.
Phases of cystometrogram
Normal CMG:
- Capacity 350-600ml - No leakage on coughing .
- First desire to void between - A voiding detrusor pressure
150- 200 ml. rise of < 70 cm H2O with a
- Constant low pressure that peak flow rate of > 15 ml /
does not reach more than 6- s for a volume > 150 ml.
10 cm H2O above baseline - Residual urine of < 50 ml.
at the end of filling.
- Provocative
maneuvers(cough, fast fill
etc.) should not provoke a
bladder contraction
normally.
CYSTOMETRY(contd...)
Single Vs multi-channel UDS:
-single: Pves only
-multi: Pves, Pdet, Pabd
CMG PARAMETERS
Intravesical pressure(Pves): Total Pressure within the
bladder.
Abdominal pressure(Pabd): Pressure surrounding the
bladder; currently estimated from rectal, vaginal, or
extraperitoneal pressure or a bowel stoma.
Detrusor pressure(Pdet): Component of intravesical
pressure created by forces on the bladder wall, both
passive and active.
True detrusor pressure = Intravesical pressure -
Intraabdominal pressure.(Pdet = Pves-Pabd)
Physiologic filling rate: A filling rate < predicted maximum.
Predicted maximum = body weight in kg divided by 4 and
expressed as ml/min.
Nonphysiologic filling rate: A filling rate > predicted
maximum.
First sensation of bladder filling: Volume at which patient first
becomes aware of bladder filling.
First desire to void: Feeling during filling cystometry that
would lead the patient to pass urine at the next convenient
moment.
Strong desire to void: Persistent desire to void without fear of
leakage.
Compliance:
- Relationship between change in bladder volume and
change in Pdet (Δvolume/Δpressure); measured in
ml/cm H2O.
- Normal bladder is highly compliant, and can hold
large volumes at low pressure.
- Normal pressure rise during the course of CMG in
normal bladder will be only 6-10 cm H2O.
- Decrease compliance < 20 ml/cm H2O, poorly
distensible bladder.
Impaired compliance is seen in:
neurologic conditions: spinal cord injury/lesion, spina
bifida, usually results from increased outlet resistance
(e.g., detrusor external sphincter dyssynergia [DESD])
or decentralization in the case of lower motor neuron
lesions,
Long-term BOO (e.g., from benign prostatic
obstruction),
Structural changes- radiation cystitis or tuberculosis.
Impaired compliance with prolonged elevated storage
pressures is a urodynamic risk factor and needs
treatment to prevent renal damage.
Neurogenic detrusor overactivity: Overactivity
accompanied by a neurologic condition; also k/a
detrusor hyperreflexia.
Idiopathic detrusor overactivity: Detrusor
overactivity without concurrent neurologic cause; also
k/a detrusor instability.
Abdominal leak point pressure(ALPP): Intravesical
pressure at which urine leakage occurs because of
increased abdominal pressure in the absence of a
detrusor contraction.
ALPP is a measure of sphincteric strength or ability
of the sphincter to resist changes in Pabd
Applicable to stress incontinence; ALPP can be
demonstrated only in a patient with SUI.
There is no normal ALPP, because patients without
stress incontinence will not leak at any physiologic
Pabd.
Lower the ALPP, weaker is the sphincter.
ALPP<60 cm H2O: significant ISD
ALPP 60-90 cm H2O: equivocal
ALPP>90 cm H2O: urethral hypermobility;
little or no ISD
Detrusor leak point pressure(DLPP): Lowest
detrusor pressure at which urine leakage occurs in the
absence of either a detrusor contraction or increased
abdominal pressure (risk with > 40cm H2O).
Its a measure of Pdet in a patient with decreased
bladder compliance.
Higher the urethral resistance, higher the DLPP, the
more likely is upper tract damage as intravesical
pressure is transferred to the kidneys.
UROFLOMETRY
Non invasive study.
Measurement of the rate of urine flow over time.
Estimate of effectiveness of the act of voiding along with PVR.
Influenced by
effectiveness of detrusor contraction
completeness of sphincteric relaxation
patency of the urethra
3 methods used
gravimetric
rotating disk
electronic dipstick
Recorded variables during UFM study:
Voided volume (VV in milliliters)
• Flow rate (Q in milliliters per second)
• Maximum flow rate (Qmax in milliliters per second)
• Average flow rate (Qave in milliliters per second)
• Voiding time (total time during micturition in seconds)
• Flow time (the time during which flow occurred in seconds)
• Time to maximum flow (onset of flow to Qmax in seconds)
• Optimal voids 200 to 400cc.
• Voids < 150cc are difficult to interpret.
• Pt. should be well hydrated with full bladder, but
not overly distended bladder.
• Should be performed in privacy and pt.encouraged
to void in his normal fashion.
• Qmax & shape of curve- more reliable indicators of
BOO.
• Qmax- most reliable variable in detecting abnormal
voiding.
Normal uroflow curve is bell-shaped
Flattened pattern: Obstruction
Interrupted or straining pattern: Impaired bladder contractility,
obstruction, or voiding with/by abdominal straining.
"Box-pattern" : Urethral Stricture
Post Void Residual Urine
Excellent assessment of bladder emptying.
Performed by ultrasound (bladder scan) or
catheterization.
Normally, it is < 0.5ml, but < 10% of voided volume
is considered insignificant.
Urethral pressure profilometry
Urethral pressure profile (UPP): a graph indicating
intraluminal pressure along the length of urethra.
Urethral pressure: fluid pressure needed to just open a
closed urethra.
UPP is obtained by withdrawal of a pressure sensor
(catheter) along the length of urethra.
UPP Parameters:
Urethral closure pressure profile is given by subtraction of
intravesical pressure from urethral pressure.
Maximum urethral pressure is highest pressure measured
along the UPP.
• Maximum urethral closure pressure (MUCP) : maximum
difference between urethral pressure and intravesical
pressure.
Functional profile length: length of urethra along which
urethral pressure exceeds intravesical pressure in women.
In most continent women,
functional urethral length:approx.3 cm &
MUCP is 40 to 60 cm H2O.
MUCP is not always indicative of severity of incontinence
hence not used commonly.
UPP
PRESSURE FLOW
MICTURITION STUDIES
Simultaneous measurement of bladder pressure and
flow rate throughout the micturition cycle.
Best method of quantitatively analyzing voiding
function.
Access to bladder via transurethral or SPC 8F or less.
Intra-abdominal pressure measured by balloon
catheter in rectum or vagina.
Men should void in standing position, while women
seated on commode.
Detrusor pressure at maximal flow(Pdet at Qmax):
Magnitude of micturition contraction at the time when
flow rate is at its maximum.
Pressure <100 cm H2O indicate outlet obstruction
even if the flow rate is normal.
Normal male generally voids with Pdet 40-60 cm H2O
and woman with lower pressure.
Pdet more accurately measures bladder wall
contractions.
Indications for pressure-flow studies:
- to differentiate between pts with a low Qmax sec. to
obstruction, from those sec.to poor contractility.
- Identify pt.with normal flow rates but high pressure
obstruction.
- LUTS in pt with hx of neurologic disease(CVA,
Parkinson’s).
- LUTS with normal flow rates (Qmax > 15cc/min).
younger men with LUTS.
- Men with little endoscopic evidence of prostate
occlusion
ICS provisional nomogram
VIDEO-URODYNAMICS
UDS with simultaneous fluoroscopic image of lower
urinary tract.
Equipment and technique:
- CMG + PFS same as before but the study is conducted
on a fluoroscopy table, and the filling medium is a
radiographic contrast agent.
clinical applicability:
complex BOO
evaluation of VUR during storage &/or filling.
neurogenic bladder dysfunction
identification of associated pathology
Primary BNO diagnosis & differentiation from
dysfunctional voiding in women: only on VUDS.
Video-urodynamics
ELECTROMYOGRAPHY
(EMG)
Study of the electric potentials produced by depolarization of
muscle membranes.
In case of UDS, EMG measurement of striated sphincteric
muscles of the perineum is done to evaluate possible
abnormalities of pelvic floor muscle function.
EMG activity is measured during both filling and emptying.
EMG is performed via electrodes placed in (needle
electrodes) or near (surface electrodes) the muscle to be
measured.
Most important information obtained from sphincter EMG
is whether there is coordination or not between the
external sphincter and the bladder.
EMG activity gradually increases during filling
cystometry (recruitment) and then cease and remains so
for the time of voiding.
Failure of the sphincter to relax or stay completely relaxed
during micturition is abnormal.
In pt with neurologic disease, this is called detrusor-
sphincter dyssenergia.
In the absence of neurologic disease, it is called pelvic
floor hyperactivity,or dysfunctional voiding.
CYSTOMETROGRAPH
URODYNAMIC RISK FACTORS
Following urodynamics findings are potentially dangerous and
usually require intervention to prevent upper and lower urinary
tract decompensation:
1. Impaired compliance
2. Detrusor external sphincter dyssynergia (DESD)
3. Detrusor internal sphincter dyssynergia (DISD)
4. High-pressure detrusor overactivity present throughout
filling
5. Elevated detrusor leak point pressure (>40 cm H2O)
6. Poor emptying with high storage pressures
Thank you
You might also like
- Urodynamic Tests ExplainedDocument55 pagesUrodynamic Tests ExplainedFiky setiawanNo ratings yet
- An Overview of Urodynamic StudiesDocument54 pagesAn Overview of Urodynamic StudiesNikesh Doshi100% (1)
- Uro DynamicsDocument64 pagesUro DynamicsSri HariNo ratings yet
- Urodynamics Interpretation Course by Expert UrologistDocument58 pagesUrodynamics Interpretation Course by Expert UrologistDrMohamed ElsonosyNo ratings yet
- 2017 05 13 GSD Cathy Rumble GP Urodynamics Made Easy Information SheetDocument5 pages2017 05 13 GSD Cathy Rumble GP Urodynamics Made Easy Information SheetanjelikaNo ratings yet
- IncontinenceDocument9 pagesIncontinenceHanaNo ratings yet
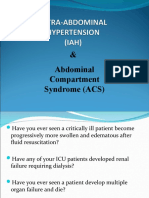
- Intra Abdominal Hypertension AND Abdominal Compartment SyndromeDocument56 pagesIntra Abdominal Hypertension AND Abdominal Compartment SyndromeAmit JaiswalNo ratings yet
- Urodynamics: Daniel Simanjuntak Samuel Aji Enrico SautDocument54 pagesUrodynamics: Daniel Simanjuntak Samuel Aji Enrico SautDipo Mas SuyudiNo ratings yet
- Stress Urinary IncontinenceDocument93 pagesStress Urinary IncontinenceReshmi S ChellappanNo ratings yet
- Intraabdominal PressureDocument15 pagesIntraabdominal Pressurearditia dwiNo ratings yet
- INCONTINENCE3Document12 pagesINCONTINENCE3allthingali217No ratings yet
- Urodynamic Testing ReportDocument25 pagesUrodynamic Testing Reportzharah180% (1)
- Treatment and Testing of Stress Urinary IncontinenceDocument52 pagesTreatment and Testing of Stress Urinary IncontinenceAlexandriah AlasNo ratings yet
- Theneurogenicbladder: Anupdatewith Managementstrategies Forprimarycare PhysiciansDocument10 pagesTheneurogenicbladder: Anupdatewith Managementstrategies Forprimarycare Physicianschouko catNo ratings yet
- CP Intestinal Obstruction Chap7Document57 pagesCP Intestinal Obstruction Chap7Katherine 'Chingboo' Leonico LaudNo ratings yet
- Skills LabDocument20 pagesSkills LabJei JayNo ratings yet
- Biological and Medical Applications of Pressure and Fluids - PH 2FDocument66 pagesBiological and Medical Applications of Pressure and Fluids - PH 2FRonald Tantiado100% (3)
- Regular Review: Management of Chronic Urinary RetentionDocument2 pagesRegular Review: Management of Chronic Urinary RetentionAndy IbarraNo ratings yet
- Medical and Biological Application of Pressure and Fluids - 2EDocument25 pagesMedical and Biological Application of Pressure and Fluids - 2ERonald Tantiado100% (2)
- Neurogenic BladderDocument38 pagesNeurogenic Bladderminnalesri100% (1)
- Urodynamics: Rustom ManeckshaDocument34 pagesUrodynamics: Rustom ManeckshaVeronica MendozaNo ratings yet
- Leak Point Pressures How Useful Are They Burden Warren AbramsDocument6 pagesLeak Point Pressures How Useful Are They Burden Warren AbramsjayaraghavanrNo ratings yet
- Upper Gi BleedingDocument3 pagesUpper Gi BleedingJohiarra TabigneNo ratings yet
- Vijendra Kumar: Compiled byDocument15 pagesVijendra Kumar: Compiled byvijendrakumarsahuNo ratings yet
- Imaging in Child Intussusception 2013: AuthorDocument33 pagesImaging in Child Intussusception 2013: AuthorartooktaviantoNo ratings yet
- Stress IncontinenceDocument44 pagesStress IncontinenceswatisinghnigeriaNo ratings yet
- Irregular Bowel HabitDocument66 pagesIrregular Bowel Habitfahim ahamedNo ratings yet
- URINARY INCONTINENCE: CAUSES AND EVALUATIONDocument112 pagesURINARY INCONTINENCE: CAUSES AND EVALUATIONPrabhakar KumarNo ratings yet
- Surgery - Female Urology and Incontinence (Tutorial)Document6 pagesSurgery - Female Urology and Incontinence (Tutorial)halesNo ratings yet
- OnLine Pediatric Surgery HANDBOOKDocument6 pagesOnLine Pediatric Surgery HANDBOOKTahir NawazNo ratings yet
- Chapter Six PDFDocument7 pagesChapter Six PDFKhadija KadhimNo ratings yet
- Neurogenic Bladder (Emedicine) : Physiology Filling PhaseDocument4 pagesNeurogenic Bladder (Emedicine) : Physiology Filling PhaseReni FahrianiNo ratings yet
- Detrusor InstabilityDocument7 pagesDetrusor Instabilityapi-3705046No ratings yet
- Abdominal Compartment SyndromeDocument7 pagesAbdominal Compartment Syndromemezgebu alemnehNo ratings yet
- Urinary DiversionDocument2 pagesUrinary DiversionWendy EscalanteNo ratings yet
- The neuropathic lower urinary tractDocument4 pagesThe neuropathic lower urinary tractBarez AminNo ratings yet
- BladderDocument66 pagesBladderPatel Alapkumar Kanubhai100% (1)
- Case Lâm SàngDocument39 pagesCase Lâm SàngHungNo ratings yet
- Neurogenic BladderDocument14 pagesNeurogenic BladderOeyi Mutia SatifaNo ratings yet
- Urinary System DisordersDocument14 pagesUrinary System DisordersGideon P. CasasNo ratings yet
- Intravenous UROGRAMDocument14 pagesIntravenous UROGRAMvijendrakumarsahuNo ratings yet
- Abdominal Compartment Syndrome Review and ManagementDocument39 pagesAbdominal Compartment Syndrome Review and ManagementIdha KurniasihNo ratings yet
- Anorectal Physiology 2003Document5 pagesAnorectal Physiology 2003Ngu Ing SoonNo ratings yet
- Abdominal Hypertension No PhotosDocument33 pagesAbdominal Hypertension No Photosimma_drNo ratings yet
- Benign Prostatic HyperplasiaDocument6 pagesBenign Prostatic HyperplasiaHenny HansengNo ratings yet
- Diagnostic TestsDocument5 pagesDiagnostic TestsCristina L. JaysonNo ratings yet
- BPH 180828154943Document42 pagesBPH 180828154943Amandeep SinghNo ratings yet
- Structures and Functions: Chapter 45: Nursing Assessment: Urinary SystemDocument18 pagesStructures and Functions: Chapter 45: Nursing Assessment: Urinary SystemKennette LimNo ratings yet
- Abdominal ParacentesisDocument4 pagesAbdominal ParacentesisRashmi C S100% (1)
- Abdominal Paracentesis Procedure GuideDocument14 pagesAbdominal Paracentesis Procedure Guideesther100% (1)
- Peritoneal Dialysis Explained: Health Effects, Method, and ComplicationsDocument7 pagesPeritoneal Dialysis Explained: Health Effects, Method, and ComplicationsPrasann RoyNo ratings yet
- Polyglycolic Acid Sutures, Polyglactin 910, Catgut, Poliglecaprone 25 and Polydioxanone SuturesDocument3 pagesPolyglycolic Acid Sutures, Polyglactin 910, Catgut, Poliglecaprone 25 and Polydioxanone SuturesAiza OronceNo ratings yet
- Abdominal Compartment Syndrome (ACS) &Document26 pagesAbdominal Compartment Syndrome (ACS) &Alvin Kurian JijiNo ratings yet
- Urinary RetentionDocument24 pagesUrinary RetentionMuhammad Amri Kautsar100% (1)
- Peritonitis in PD PatientsDocument64 pagesPeritonitis in PD PatientsDaniel SitungkirNo ratings yet
- Stress IncontinenceDocument34 pagesStress IncontinencePallavi Janghela100% (1)
- Continuous Dialysis Techniques ComparedDocument10 pagesContinuous Dialysis Techniques ComparedSanhati Ghosh Banerjee100% (1)
- Rules and Directions for the Employment of Injections in Various DiseasesFrom EverandRules and Directions for the Employment of Injections in Various DiseasesNo ratings yet
- Diagnosing leptospirosis using modified Faine's criteriaDocument8 pagesDiagnosing leptospirosis using modified Faine's criteriaFiky setiawanNo ratings yet
- Significant Haemoglobinopathies: Guidelines For Screening and DiagnosisDocument15 pagesSignificant Haemoglobinopathies: Guidelines For Screening and DiagnosisFiky setiawanNo ratings yet
- Fs Leptospirosis Clinicians Eng 508Document4 pagesFs Leptospirosis Clinicians Eng 508SathyaAgastyaNo ratings yet
- Screening Hbpathies 2012Document15 pagesScreening Hbpathies 2012Fiky setiawanNo ratings yet
- Beta Talasemias Nejm PDFDocument12 pagesBeta Talasemias Nejm PDFFiky setiawanNo ratings yet
- Journal HilangDocument21 pagesJournal HilangFiky setiawanNo ratings yet
- Pemeriksaan Fisik ThorakDocument36 pagesPemeriksaan Fisik ThorakFiky setiawanNo ratings yet
- Tugas Evidence Based MedicineDocument14 pagesTugas Evidence Based MedicineFiky setiawanNo ratings yet
- Journal HilangDocument21 pagesJournal HilangFiky setiawanNo ratings yet
- Refrat HiperbilirubinemiaDocument32 pagesRefrat HiperbilirubinemiaFiky setiawanNo ratings yet
- Medical Exam Questions ReviewDocument37 pagesMedical Exam Questions ReviewOpeyemi Omolabake67% (3)
- ANATOMY OF GUINEA PIG (Cavia Porcellus)Document8 pagesANATOMY OF GUINEA PIG (Cavia Porcellus)Daisy KavinskyNo ratings yet
- Urinary System WorksheetDocument4 pagesUrinary System WorksheetTENNESSEE AYALANo ratings yet
- NCPDocument6 pagesNCPAndrea Marie SevillaNo ratings yet
- Module IV PostpartumDocument10 pagesModule IV PostpartumCorillo, Fionnula JeanNo ratings yet
- NCM 109 Finals NotesDocument21 pagesNCM 109 Finals NotesERIKA BOOTS CABALUNANo ratings yet
- Fisiologi Genitourinary SystemDocument14 pagesFisiologi Genitourinary SystemPandu Dian WicaksonoNo ratings yet
- Physiology of MicturitionDocument20 pagesPhysiology of MicturitionSyedaNaveenBatool0% (1)
- SSI and ERAS, Complications of TAHBSODocument18 pagesSSI and ERAS, Complications of TAHBSOCheska MalubayNo ratings yet
- Guidelines On Pain ManagementDocument85 pagesGuidelines On Pain ManagementmelawatiNo ratings yet
- Anatomy Anal CanalDocument14 pagesAnatomy Anal CanalBela Ronaldoe100% (1)
- Boenninghausen's Therapeutic Pocket Book StudyDocument24 pagesBoenninghausen's Therapeutic Pocket Book Studyanamika mishra100% (1)
- Urinary Tract Infectio Case StudyDocument17 pagesUrinary Tract Infectio Case Studyjunex123No ratings yet
- PHYSIOLOGIC CHANGES DURING PREGNANCYDocument4 pagesPHYSIOLOGIC CHANGES DURING PREGNANCYAdamNo ratings yet
- Catheterization Insertion and RemovalDocument5 pagesCatheterization Insertion and RemovalArmySapphireNo ratings yet
- Studer Surgical - Images - of - Ileal - ConduitDocument11 pagesStuder Surgical - Images - of - Ileal - ConduitTomek RNo ratings yet
- Pekana European Remedy Guide: For Licensed Health Care PractitionersDocument68 pagesPekana European Remedy Guide: For Licensed Health Care PractitionersMegan Hughes100% (3)
- Neurology DR - Ahmed MowafyDocument87 pagesNeurology DR - Ahmed MowafyنورهانعزالدينNo ratings yet
- Abdomen (Repaired)Document174 pagesAbdomen (Repaired)Merellyn Hurtado PachecoNo ratings yet
- Declaration of Good Health Form PDFDocument3 pagesDeclaration of Good Health Form PDFvemula shekar100% (1)
- Homotoxicologia Ejercicios ClinicosDocument70 pagesHomotoxicologia Ejercicios ClinicosCelia SteimanNo ratings yet
- Digestion and Excretion: The Excretory SystemDocument4 pagesDigestion and Excretion: The Excretory SystemCAYNEN HARMONNo ratings yet
- 1 Urinary StonesDocument11 pages1 Urinary StonesMohamed Al-zichrawyNo ratings yet
- The Descriptions of Frequent UrinationDocument2 pagesThe Descriptions of Frequent UrinationHayatinur 0302No ratings yet
- Anatomy and Physiology of the Urinary System (39Document18 pagesAnatomy and Physiology of the Urinary System (39Fatima Dacalos FuerzasNo ratings yet
- Klinik Medic Q servicesDocument3 pagesKlinik Medic Q servicesNANTHA KUMARANNo ratings yet
- Hydraulic UrethralDocument2 pagesHydraulic UrethralMalgorzata LisowskaNo ratings yet
- Postpartum Discharge PlanDocument2 pagesPostpartum Discharge PlanNielette R. BASAL100% (1)
- Fetal Renal Pelvic DilatationDocument2 pagesFetal Renal Pelvic DilatationshakkiryousufNo ratings yet
- Diagnostic Management URINALYSISDocument3 pagesDiagnostic Management URINALYSISjhappo31No ratings yet