Professional Documents
Culture Documents
Nasal Congestion and Its Management in Pregnancy Rhinitis: Research Article
Uploaded by
Indah AulliaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nasal Congestion and Its Management in Pregnancy Rhinitis: Research Article
Uploaded by
Indah AulliaCopyright:
Available Formats
Vol 7, No 4
October 2019 Nasal Congestion and its Management 318
Research Article
Nasal Congestion and its Management in Pregnancy Rhinitis
Hidung Tersumbat dan Penatalaksanaannya pada Rinitis Kehamilan
Niken L. Poerbonegoro
Department of Otorhinolaryngology-Head and Neck Surgery
Faculty of Medicine Universitas Indonesia
Dr. Cipto Mangunkusumo General Hospital
Jakarta
Abstract Abstrak
Objective : To elaborate on the pathomechanism of Tujuan : Untuk memaparkan patomekanisme rinitis
pregnancy rhinitis and the proper management of rhinitis kehamilan dan tatalaksana yang tepat dalam mengatasi
symptoms, particularly nasal obstruction. gejala rinitisnya, terutama hidung tersumbat.
Methods: Literature review.
Metode : Tinjauan pustaka.
Methods : Literature review.
Hasil: PGH dan progesterone memiliki efek serupa yaitu
Result: Placental Growth Hormone has a similar effect vasodilatasi perifer dan peningkatan volume ekstraselular.
as progesterone in pregnancy, which is peripheral Peningkatan estrogen selama kehamilan menstimulus
vasodilatation and increases extracellular volume. Increased aktivitas sistem parasimpatetik, yang mana terjadi
estrogen during pregnancy enhances the parasympathetic peningkatan permeabilitas vaskular dan aktivitas kelenjar.
activity, thus increasing vascular permeability and glandular Kebocoran plasma dari pembuluh darah ke stroma akan
activity.Plasma leakage from vascular bed to stroma results menyebabkan edema konka yang bermanifestasi sebagai
in edematous turbinates, causing nasal congestion. This kongesti hidung. Kondisi pembengkakan mukosa ini
mucosal swelling is exaggerated with the presence of thick diperberat dengan adanya hipersekresi.
and profuse secretion.
Kesimpulan : Rinitis kehamilan, dengan manifestasi
Conclusions : Pregnancy rhinitis, manifested as nasal kongesti hidung, dianggap sebagai suatu fenomena yang
congestion, is considered a phenomenon and may become dapat menjadi fatal. Kongesti hidung persisten merupakan
a serious condition. Persistent nasal congestion acts as a faktor risiko terjadinya gangguan tumbuh kembang janin
potential risk factor in affecting fetal growth and development melalui proses hipoksia bertahap. Kondisi ini dapat berlanjut
through gradual hypoxia process. This condition can lead menimbulkan komplikasi seperti hipertensi maternal,
to various complications such as maternal hypertension, preeklamsia, gangguan tumbuh janin, dan skor APGAR
preeclampsia, impaired fetal growth, and low APGAR scores. yang rendah. Memahami patomekanisme sangat utama
In-depth knowledge of pathomechanism is essential as dalam membimbing klinisi memberikan tatalaksana yang
guidance to proper treatment, including conservative and tepat, termasuk terapi konservatif dan farmaka, yang akan
medical therapies, which will lead to an optimal outcome for memberikan keluaran yang optimal baik bagi ibu dan bayi.
both mother and baby.
Kata kunci : estrogen, kongesti hidung, placental growth
Keywords : estrogen, nasal congestion, placental growth hormone, rinitis kehamilan.
hormone, pregnancy rhinitis.
Correspondence author: Niken L. Poerbonegoro. niken_lp@yahoo.com
INTRODUCTION around 10–30% pregnant women suffer more
from their AR symptoms. However, some women
Rhinitis is a common problem during pregnancy, experience rhinitis symptoms only asepisodes
affecting up to 30% of pregnant women.1Rhinitis in their pregnancies. Thus, pregnancy rhinitis is
during pregnancy might occurs as allergic rhinitis, defined as nasal congestion present during the
drug-induced rhinitis, rhinosinusitis, anatomical last six weeks or more of pregnancy, without
variations, and gestational or “pregnancy” other signs of respiratory tract infection and no
rhinitis.2 In women with prior history of allergic known allergic cause.Pregnancy rhinitis usually
rhinitis, nasal symptoms might improve or worsen disappears within two weeks after delivery1, 3
during their pregnancies.3, 4Demoly1 quoted that
Indones J
319 Poerbonegoro Obstet Gynecol
Pregnancy rhinitis is reported in one of five The Effects of Pregnancy Hormones to Nasal
pregnant women.3 The incidence rate from small Physiology
groupsof pregnant women were respectively 30%
of 79 women, 18% of 66 women, and 21% of 160 Throughout the pregnancy, hormonal changes
women. The prevalence of pregnancy rhinitis as affect the physiologic nasal cycle in many ways.
17.17%, with the description as follows: 0% in the Pregnancy-related hormonal changes and
first trimester, 9.38% in the second trimester, and neuropeptides are causing this alteration to the
38.89% in the third trimester.3,4 mucosa of the nose.8
In a questionnaire study, 22% of 599 pregnant Estrogen
women reported having nasal congestion during
their midwife visits. Rhinitis symptoms occurred Estrogen production dramatically increases
in their 7th to 36th week of pregnancies and during pregnancy. Estrogen tends to inhibit
disappeared in second to the fourth week after acetylcholine esterase leading to the production
delivery. Fourty two percent of 2.264 pregnant of acetylcholine and induces Parasympathetic
women had nasal obstruction on the 36th week activity.
of pregnancies.3
Pregnancy rhinitis is considered as the result
of hormonal changes and fluctuation during
pregnancy, which might manifest as nasal
congestion as the most bothersome symptom.
During pregnancy, elevated estrogen and
progesterone levels are associated with nasal
mucosal hyperreactivity. These hormones also
induce mucosal swelling, glandular secretion,
and dilatation of turbinate capillaries, resulting
in worsening of symptoms, especially nasal
Figure 1. Estrogen Effects during Pregnancy11
obstruction.1, 3, 5
This cholinergic activity causesvasodilatation and
It is believed that placental growth hormone oedema to the nasal mucosa.9, 10 (Figure 1)
(PGH) may stimulate mucosal growth and
thus induce nasal congestion.Other than that, In general, estrogen causes nasal turbinates
physiological changes during pregnancy also to be edematous, leading to nasal obstruction,
attribute to symptoms severity. Increased nasal discharge flowing into the throat (postnasal
circulating blood volume during pregnancy, up drip). Untreated conditions may cause olfactory
to 40% of pre-pregnancy, is related to increased function disturbance. These rhinitis symptoms
nasal airway resistance.5 also occur in women with birth control pills and
hormonal replacement therapy.12, 13
Due to similar symptoms with other
inflammatory diseases of the nose, pregnancy Other known effects of estrogen are increased
rhinitis should be suspected by the exclusion of of vascular permeability, protein synthesis,
other causes of rhinitis.6, 7 Rhinitis symptoms glandular activity and increase the sensitivity
in pregnancy might not be considered as fatal, of vasomotor properties in the autonomic
however, worsen symptoms during pregnancy nervous system. Increase of protein synthesis
may impair maternal daily activities and and hyaluronic acid in the nasal mucosa causes
emotional well being. Persistent nasal congestion the mucus to thicken and disrupt the mucociliary
resulting in sleep disturbance during pregnancy clearance of the nasal cycle.9,10In addition, increase
is related to intrauterine growth retardation and of blood pooling due to decreasedα-adrenergic
lower APGAR scores.3 Proper management of smooth muscle tonus in the venous sinusoid,
pregnancy rhinitis must not raise problems, and or oedema caused by plasma leakage from the
worth consider the risk-benefit ratio for mothers vascular bed to the stroma.3
and infants. 3, 6, 7
Vol 7, No 4
October 2019 Nasal Congestion and its Management 320
Excessive mucus production gives a sensation stimulated by progesterone and oxytocin, may
to the throat as post nasal drip, thus enhance enhance nasal congestion. Progesterone-related
nasal congestion. Studied nasal mucosa biopsies fibroblast in the nasal mucosa may also affect the
from pregnant women and those who consumed extracellular matrix.10
birth control pills, which he found glandular
hyperactivities and increased phagocytosis. Nasal Prolactin
congestion is the initial side effect of high dose
estrogen contraceptive pill intake.14 Conducted Production of prolactin by pituitary increases
a cohort study of 568 patients and found a during pregnancy, which suggests the possibility
significant correlation between the incidence of its role in the pathogenesis of pregnancy
of asthma and rhinitis during pregnancy. rhinitis; however, this is contradicted by the
Furthermore, β-estradiol and progesterone have absence of sinus pathology in patients who have
receptors in nasal mucosa that contribute to the prolactinomas. Furthermore, bromocriptine and
nasal congestion pathophysiology in pregnant quinagolide reduce prolactin production which
women.12, 13, 15 eventually develops nasal congestion.3
The significant rise of the plasma volume in Neuropeptides
pregnant womenoccur during the 6 – 8 weeks of
gestation and reach its peak at week 32. Volume A vasoactive intestinal polypeptide (VIP) is
may increase to 4700 to 5200 ml (45% increase to associated with other forms of rhinitis, and a
unpregnant women). This occurrence happened possible mediator for nasal mucosa vasodilation,
due to an increase of estrogen secretion and which is responsible for nasal congestion during
renin angiotensin aldosterone system stimulation, pregnancy. Nasal biopsies of postmenopausal
which attract water and retent natrium. Water women showed an increased immunopositivity
retention produces oedema of the mucosa thus for estradiol, estradiol receptor, VIP, and
resulting nasal congestion.11 substance P (SP) after six months of hormone
replacement therapy. Whereas, there was
Estrogen may trigger an immune reaction a reduction in neuropeptide Y(NPY). Nasal
through the α-estrogen receptor on the mast cell. application of hormone replacement therapy
This reaction peak during the menstrual period, induced stronger VI P changes than did the
pregnancy, oral contraception consumption and transdermal application. Mucociliary transport
hormone replacement therapy. A hypothesisstates time and subjective nasal congestion decreased,
that estrogen and progesterone act as antigen but anterior rhinomanometry was unchanged.
bound to a different protein producing Th2 The investigators proposed that estrogen action
cell, which regulates IgE synthesis and other in the nasal mucosa is mediated by neuropeptides
antibodies. The antibody linked to mast cells an increase of gland secretion and vasodilatation
as well as appropriate antigens (hormone or by VIP and SP and a decrease of NPY-induced
metabolites) will cause degranulation of the mast vasoconstriction.3 VIP relaxes the blood vessels
cell or basophil. Thus releasing histamine, Th2 to the upper airways, trachea, bronchi, and
cytokines, and leukotrienes.16, 17 pulmonary vessels.
Progesterone Innervation of the nasal mucosa is mainly
organized and complex. The autonomic system
There was no difference in blood progesterone regulates the mucosal vasculature and glandular
levelbetween women with and without pregnancy secretion. The efferent nasal reflex arc consists
rhinitis. Other study showed an increase of sympathetic and parasympathetic nerves.
of circulatory blood volume, possibly from Parasympathetic nerve stimulates the release
vasodilatation occurringdue to the increased of acetylcholine, norepinephrine, and VIP.
level of progesterone in pregnant women, which Postganglionic parasympathetic nerve innervates
may induce nasal congestion2. Nasal vascular serous and mucous glands, arteries, veins and
pooling from smooth muscle relaxation related arteriovenous anastomoses. The distribution of
to the increase of progesterone. An increase VIP-immunoreactive fibres corresponds to the
of vasoactive intestinal peptide (VIP) release, cholinergic distribution system. VIP stimulates
Indones J
321 Poerbonegoro Obstet Gynecol
serous cell secretion, dilates nasal vessels, and growth hormone (PGH) was significantly high
may also regulate mucociliary clearance in the during pregnancy. A significantly higher level
nose.18 of PGH in women with pregnancy rhinitis group
on all occasions throughout the pregnancy.
The mechanism of hyperactivity of the nose Presumably, PGH stimulates nasal mucosa similar
remains unknown. The proposed hypothesis to progesterone, thus inducing pregnancy rhinitis.
is increased permeability and increased the PGH has a similar effect as progesterone in
sensitivity of sensory nerve endings and imbalance pregnancy, which is peripheral vasodilatation and
of autonomic nerve regulation caused by changes increases extracellular volume.20 The mechanism
of the nasal mucosa neuroreceptors.18Substance is still unknown; further study is warranted.3, 20
P is produced by the afferent sensory neurons
of the trigeminal nerve within the nasal mucosa. Risk Factors
Neurotransmitter promotes vasodilatation,
increase blood vessels permeability, and According to a questionnaire study done, the
hypersecretion of submucosal glands, leading incidence of pregnancy rhinitis is significantly
to all sorts of nasal symptoms. The exact role of higher among smoking women than non-smoking
this neuropeptide in pregnancy rhinitis remains women (odds ratio: 1,7; CI 95% 1,1-1,5)2,3. Thus,
unclear.19 smoking is considered an irritant agent that most
probably stimulates nasal congestion. In vitro test
Small-diameter of the unmyelinated sensory to 10 airborne allergensin 165 pregnant women,
fibres which areextensively branched, densely in which 83 women had pregnancy rhinitis14.
innervate the walls of submucosal vessels and Overall sensitization was not increased in women
glandular acini to form the neurosecretory with pregnancy rhinitis, yet sensitization to
varicosities within the vascular and glandular house dust mites frequently occurred in this
area. Neuronal wave evoked by histamine group.Therefore, subjects with a high level of
immediately extends to the peripheral sensory IgE to house dust mites are considered prone
neurons, and the central, brain, as well. Hence, to develop pregnancy rhinitis. However, to
various neuropeptides are released from the differentiate pregnancy rhinitis to allergic rhinitis
nerve endings into the spaces near submucosal in pregnancyis still a challenge.2, 3, 14
vessels and gland to elicit its rapid reactions.19
DIAGNOSIS
Placental Growth Hormone
The diagnosis of pregnancy rhinitis is made by
history taking, consisting thorough information
regarding symptoms and physical examination
to eliminate other cause of other nasal disorders.
This shall exclude allergic rhinitis, vasomotor
rhinitis, septal deviation, polyposis, rhinosinusitis
and many more. It is difficult to differentiate
allergic and nonallergic rhinitis. The common
triggering factor of nonallergic rhinitis may be
weather or temperature changes, food, perfume,
strong odour and smoke. Additional symptoms
may include allergic conjunctivitis (itching, watery,
redness and swelling of the eye).21
Figure 2. nasoendoscopic finding right inferior turbinate
A comprehensive head and neck
in pregnancy rhinitis pre (right) and post (left)
decongestant.3 examination starting with a simple rhinoscopy
or nasoendoscopic examination to exclude
Human Growth Hormone (hGH) is secreted in an other cause of rhinitis (Figure 2). The mucosa
episodic burst in low levels between peaks. This of the nasal and nasal turbinates may appear
pattern is later replaced by continuous secretion swollen and covered with serous to seromucoid
of Placental Growth Hormone (PGH) after the discharge. There are no other specific further
first trimester of gestation. That placental findings (laboratory or other means) to diagnose
Vol 7, No 4
October 2019 Nasal Congestion and its Management 322
pregnancy rhinitis.Pregnancy rhinitis is diagnosed Nasal congestion may also be objectively
based on subjective findings of symptoms and assessed by rhinomanometry, acoustic rhinometry,
physical examination.21 or peak nasal inspiratory flowmetry (PNIF).
Those examinations assess nasal congestion by
measuring nasal resistance, nasal volume, and
nasal airflow.24
DIFFERENTIAL DIAGNOSIS
Figure 3. Visual Analog Scale (VAS)22 Pregnancy rhinitis is a subtype of non-allergic
non-infectious (NANIR). Allergic rhinitis shows
The evaluation of subjective nasal obstruction similar symptoms to pregnancy rhinitis, but
using a Visual Analog Score (VAS) and Nasal the underlying pathology occurred due to
Obstructive Symptom Evaluation (NOSE) scale immunoglobulin E-mediated hypersensitivity.
may assess the quality of daily life (Figure 3 A definitive diagnosis of allergic rhinitis is
and Table 1). Both tools are highly specific and established by skin prick test or specific IgE
sensitive, validated by previous studies on many serology results.2, 3, 25
other nasal pathologies. VAS and NOSE scale are
patient-centred quantitative diagnostic tools. Rhinitis medicamentosa is another differential
VAS score more than 5 and NOSE scale more diagnosis but may also become a complication
than equal to 5 in pregnant women presumably of pregnancy rhinitis. Most women do not
to be pregnancy rhinitis.22 directly disclose a history of prolonged usage of
Table 1. Nasal Obstructive Symptom Evaluation Scale23 intranasaldecongestant. Therefore it is essential
to obtain this information in the history taking.
Mild Moderate Fairly bad Severe
Healthy individuals with rhinitis medicamentosa
Nose obstruction 0 1 2 3 4 no longer have nasal congestion in 2 days after
and stuffiness
Nose obstruction 0 1 2 3 4
they stop using decongestants. During pregnancy,
Trouble breathing 0 1 2 3 4 if congestion persists for more than a week or
through my nose so after reducing intranasal decongestant, the
Trouble of sleeping 0 1 2 3 4 diagnosis should be pregnancy rhinitis.3
Unable to get 0 1 2 3 4
enough air through
my nose during Other differential diagnosis includes upper
exercise or exertion respiratory tract infection and anatomical variation
(septal deviation and hypertrophic turbinates)
Over the past month, how much of a problem which disrupt the mucociliary clearance. Infection
were the following conditions for you? Please may occur due to a virus which causes direct
circle the most correct response. damage to the nasal epithelial barrier and
indirectly by hyperactivity of nasal mucosa, thus
Discharge Inflammation Polyps/Oedema disrupts mucociliary clearance. It is important to
(DIP) score is a clinician-based examination exclude sinusitis by the clinical finding of purulent
validated by previous researches (Table 2). DIP discharge in the middle meatus, facial pain, and
score quantifiesnasoendoscopic findings (more olfactory dysfunction. Sinusitis during pregnancy
than 5 to be considered as pregnancy rhinitis). (common in the second trimester) may not improve
A correlation between VAS, NOSE, and DIP with conservative treatment such as nasal saline
scores toward gestation in evaluating pregnancy irrigation. Secondary bacterial infection may also
rhinitis.4 occur. Typical organisms found in such conditions
are Streptococcus pneumonia, Haemophilus
Table 2. Discharge Inflammation Polyps/Edema (DIP)
Scoring System24 influenza, and Moraxella catarrhalis.26
Absent Moderat Severe IMPACT OF PREGNANCY RHINITIS
0 1 2
Discharge Impact of pregnancy rhinitis to the fetus is
Inflammation indirectly related to sleeping disturbance
Polyps/Edema
Indones J
323 Poerbonegoro Obstet Gynecol
experienced by pregnant women.Besides nasal Doctors must ensure pregnant women that nasal
congestion due to placental hormones, lying congestion is a common occurrence during
down in bedtime (supine position) also cause more pregnancy. Such information should be given at
nasal congestion due to the effect of gravitation. the first antenatal care visit, along with several
Difficulty in breathing through the nose increases treatment options to choose.2, 3
the risk of snoring and mouth breathing during
sleep. Twenty three percent of 502 postpartum Physical Exercise
women reported having to snore at the last weeks
of their pregnancies. Snoring gives a higher risk Physical exercise has been known to have a
of developing hypertension, pre-eclampsia, decongestant effect on the nasal mucosa. Head
intrauterine growth retardation (IUGR), and low elevationat 300– 450 when laying down reduce
APGAR scores. Mouth breathing in pregnancy the likelihood of vena cava syndrome and
rhinitis affects lung vascular tonus or mother/ snoring. Another mechanical mean is using dilator
and fetus oxygenation. Pregnancy rhinitis might fornostrils. This device dilates the narrowest
induce the presence of obstructive sleep apnea part of the upper airways that is valve area of
(OSA).2,3 Physiologically, inhaled nitric oxide, the nose. External type dilator may improve
which is highly produced inside the maxillary nocturnal nasal congestion related to breathing
sinuses, decreases lung vascular resistance and in pregnant women, while internal type dilator
increases lung oxygenation. Nasal congestion may reduce snoring in men as effective as a nasal
might disturb nitric oxide production. decongestant. The adverse effect from dilator
usage would be local irritation of the skin due to
Another study stated that pregnancy rhinitis pressure.28
impaired women’s quality of life and might cause
OSA, which in turn disturb pregnancy outcome25. Nasal Saline Irrigation
Quality of life impairment was most significant at
the third trimester than the second trimester. In Nasal saline irrigation is effective in improving
addition, there is a significant difference in the symptoms, by repairing mucociliary clearance,
quality of life between women with and without reducing mucosal oedema, reducing inflammatory
pregnancy rhinitis. Prolonged nasal congestion mediators, and cleaning mucus or triggering
may lead to sinusitis development. Furthermore, agents. Nasal irrigation is performed using isotonic
it may cause cognitive and concentration saline solution 30–500 ml (average 200 – 250 ml),
impairment, fatigue, and headache. Pregnancy pH range is 6.2-8.4. Higher volume irrigates a
rhinitis is also associated with increased anxiety. wider area in the nasal cavity. Hypertonic solution
Mouth breathing, on the other hand, causes dry (3% sodium chloride solution) is effective for
mouth and decreases saliva secretion, leading to irrigating thick mucus. Depending on device and
dental caries due to loss of salivary protection volume, nasal irrigation on average is performed
effect. in 1 minute with compression pressure ≥120
mbar to reach areas of the nasal cavity.29
Quality of life in pregnancy rhinitis has not been
fully evaluated, yet in severe cases, women showed Pharmacology Treatment
difficulty in achieving optimum respiratory needs
during the delivery process. Nasal congestion A pharmacological agent is an option when
acts as a potential risk in hampering fetal growth conservative therapy fails to reduce symptoms of
and development by gradual hypoxia.27 pregnancy rhinitis.
MANAGEMENT Decongestant
Conservative treatment Decongestant is a vasoconstrictor agent
effective to reduce nasal obstruction. Most
In the conservative approach, it is essential systemic decongestant (phenylephedrine,
to elaboratetreatment options and goals to pseudoephedrine, and phenylpropanolamine) is
women with pregnancy rhinitis, which is to classified as category C by the United State Food
alleviate symptoms rather than cure the disease. and Drug Administration (US FDA). One study
Vol 7, No 4
October 2019 Nasal Congestion and its Management 324
found 206 cases of gastroschisis due to systemic Long term and repeated systemic
decongestant during pregnancy, although corticosteroid usage should be avoided due to
there has been no study in the effectiveness of its adrenal suppression and other systemic side
systemic decongestant for pregnancy rhinitis.3In effects. A short-term of systemic steroid, less
unpregnant women, a decongestant may cause than two weeks, may give temporary relief. High
systemic side effects such as high blood pressure, dose corticosteroid intake gives many risks in
palpitation, decrease appetite, tremor and sleep the first trimester, for example, fetal blindness,
disturbance.9 lung oedema, uterine contraction inhibition, and
fluid overload.28 Thus, systemic corticosteroids
Topical decongestants (oxymetazoline and generally should be avoided during pregnancy,
phenylephrine) work rapidly to relieve nasal except in serious threatening condition with
congestion. Pregnant women tend to overuse benefit/risk ratio concerns.
nasal decongestant in the long term because
pregnancy rhinitis is a continuous condition. This Antibiotic
will lead to unresolved rhinitis medicamentosa
postdelivery. A topical decongestant will Antibiotic is not indicated in pregnancy rhinitis,
occupy α-adrenergic receptors more. Hence although that would not be the case when
the autoregulation system will cause rebound bacterial sinusitis occurred. Intensive high dose of
mucosal oedema and worsen congestion.10, 11 antibiotic is warranted, Beta-lactam dose should
Benzalkonium chloride, acommon preservative be increased by 50% because ofrenal clearance
in topical decongestantalso aggravate nasal increase during pregnancy and to reach minimum
congestion. Usage of topical decongestant once inhibition concentration. Category B antibiotics,
daily at night for more than four weeks may other than Beta-lactams, include penicillin,
develop into rhinitis medicamentosa.27Therefore cephalosporin, aztreonam (monobactam).
the recommended dose is a short term use of Imipenem is classified as category C.3.
maximum 5-10 days at a lower dosage, unilateral
and alternating nostril administrationin the Antihistamine
evening.3, 28
Antihistamine is indicated if histamine-related
Glucocorticoids symptoms are suspected, particularly effective
for relieving sneezing and nasal itching.3,5
The intranasal steroidgives a very responsive Antihistamine has been used for a long time
therapeutic effect on managing all forms of rhinitis and known to have no adverse effect on
(allergicrhinitis, medicamentosa, NANIR and the fetus. However, classic or 1st generation
sinusitis). Intranasal steroid lowers the need for a antihistamines (i.e. chlorpheniramine, triprolidine,
systemic steroid, and it has an insignificant effect diphenhydramine, cyproheptadine, promethazine,
on pregnancy rhinitis. A RCT study by Ellegard ketotifen) show to have side effects due to
et al2showed insignificant effects of fluticasone their action. Such side effects are drowsiness,
propionate nasal spray given eight weeks to dry mouth, and increase appetite.12 Classic
pregnancy rhinitis, observedfrom symptoms or antihistamines are associated with oral clefts.
acoustic rhinometry data. That study also found Second and new generation antihistamines (i.e.
no impact on cortisol level or fetal growth shown loratadine, cetirizine, fexofenadine, desloratadine,
in the ultrasound. All currently available intranasal levocetirizine) are more preferred due to lack
steroids have extremely low bioavailability,hence of such side effects and no cardiac effects.This
hardly give systemic side effects. Regardless, US group of antihistamine is also clinically proven
FDA classifies mometasone furoate, fluticasone to have anti-inflammatory effects, aside from a
furoate, fluticasone propionate, and triamcinolone known H1-histamine receptor blocker. Cetirizine
acetonide as category C. According to the Swedish and Loratadine are classified as category B.
Medical Birth Registry, there is no increment
of congenital malformation incidencein rhinitis Other Methods of Management
patients using budesonide inhalation in the early
gestation. Hence it is classified as category B.2, 3, Nasal Continous Positive Airway Pressure (CPAP)
28
is indicated in pregnancy rhinitis with severe
Indones J
325 Poerbonegoro Obstet Gynecol
obstructive sleep apnea (OSA). In unpregnant REFERENCES
patient, nasal CPAP is highly effective as shown
by the improvement in polysomnography 1. Demoly P, Piette V, Daures J-P. Treatment of Allergic
Rhinitis During Pregnancy. Drugs. 2003;63 (17):1813-
results. Pressure adjustment must be made in 20.
pregnant women. A study shows that nasal CPAP 2. Ellegård EK. Clinical and Pathogenetic Characteristics of
significantly reduces the nocturnal blood pressure Pregnancy Rhinitis. Clinical Reviews in Allergy Immunol.
in pre-eclamptic women without OSA.3 2004 26(04):149-9.
3. Ellegård EK. Pregnancy Rhinitis. Immunol Allergy Clin N
Am. 2006;26:119-35.
Surgery 4. Ulkumen B, Ulkumen B, Pala H, Celik O, Sahin N, Karaca
G. Pregnancy rhinitis in Turkish women: Do gestational
Surgery will only be in consideration in cases with week, BMI and parity affect nasal congestion? Pak J
worst prognosis due to failure of conservative, Med Sci. 2016;32(4):950-4.
5. Keles N. Treatment of allergic rhinitis during pregnancy.
pharmacological therapy, and other noninvasive Am J Rhinol. 2004;18(1):23-8.
measures, such as CPAP. It should be thoroughly 6. Osur SL. The Management of Asthma and Rhinitis during
considered that pregnancy rhinitis is a self-limiting Pregnancy. J Women's Health. 2005;14(3):263-76.
disease in a certain period.3For refractory nasal 7. Toll K. Pregnancy rhinitis: pathophysiological effects
obstruction due to hypertrophic turbinate, less of oestrogen and treatment with oral decongestants.
Stockholm, Sweden: Karolinska Institutet; 2007.
invasive surgical measures include electrocautery, 8. Akkoca AN, Özler GS, Kurt RK, Karapınar OS, Özdemir
cryotherapy, laser or radiofrequency may be ZT, Yanık S. Ear, nose and throat changes observed
applied to reduce inferior turbinate volume. during three trimesters of pregnancy. Scien J Clin Med.
2014;3(3):52-6 Epub June 30, 2014.
9. Lekas MD. Rhinitis during pregnancy and rhinitis
CONCLUSION medicamentosa. Otolaryngol Head Neck Sur.
1992;107:845-9.
Researchers describe pregnancy rhinitis as nasal 10. Philpott CM, Conboy P, Al-Azzawi F, Murty G. Nasal
congestion that occurred in6 weeks ormore of physiological changes during pregnancy. Clin
the last final trimester of pregnancy, without a OtolaryngolAllied Scien. 2004;29(4):343-51. Epub
2004/07/24.
sign of respiratory infection and known allergy, 11. Indirani B, Raman R, Omar SZ. Hormonal changes
which may resolve completely in 2–4 weeks causing rhinitis in pregnancy among Malaysian women.
postpartum. The most bothersome symptom is J Laryngol Otol 2013;127:876-81.
nasal obstruction, and other symptom includes 12. Bousquet J, Van Cauwenberge P, Khaltaev N, Aria
Workshop G, World Health O. Allergic rhinitis and its
watery rhinorrhea. Its pathomechanism remains impact on asthma. JAllergyClinImmunol. 2001;108(5
unclear, although it is believed that estrogen, Suppl):S147-334. Epub 2001/11/15.
human chorionic gonadotropin hormone (HCG), 13. Shusterman D. Toxicology of nasal irritants. Curr Allergy
human placental lactogen (HPL), and placental Asthma Rep. 2003;3(3):258-65. Epub 2003/03/29.
growth hormone (PGH) play roles. Risk factors 14. Toppozada H, Michaels L, Toppozada M, El-Ghazzawi
I, Talaat M, Elwany S. The human respiratory nasal
include smoking and sensitization. mucosa in pregnancy. An electron microscopic and
histochemical study 1982. 613-26.
There is no drug of choice to manage 15. Kircher S, Schatz M, Long L. Variables affecting asthma
pregnancy rhinitis. Women with pregnancy course during pregnancy. Ann Allergy Asthma Immunol.
2002;89(5):463-6. Epub 2002/11/28.
rhinitis should receive proper education 16. Bonds RS, Midoro-Horiuti T. Estrogen effects in allergy
regarding their conditions. Although most and asthma. CurrOpinion Allergy Clin Immunol.
pregnancy rhinitis spontaneously resolvedafter 2013;13(1):92-9. Epub 2012/10/24.
giving birth, symptoms may significantly 17. Shah S. Hormonal link to autoimmune allergies. ISRN
decrease quality of life, and medical attention allergy. 2012;2012:910437. Epub 2012/01/01.
18. Kim D-H, Park I-H, Cho J-S, Lee Y-M, Choi H, Lee H-M.
is needed. Management includes conservative Alterations of vasoactive intestinal polypeptide receptors
and pharmacology treatment, which aimed to in allergic rhinitis. Am J Rhinol Allergy 2011;25:e44–e7.
relieve nasal congestion and other symptoms. 19. Chaen T, Watanabe N, Mogi G, Mori K, Takeyama M.
Nonetheless, pregnancy is a specific condition Substance P and vasoactive intestinal peptide in nasal
secretions and plasma from patients with nasal allergy.
that needs specific consideration. The final goal Annals Otol Rhinol Laryngol. 1993;102(1 Pt 1):16-21.
is to have an optimal outcome for both mother Epub 1993/01/01.
and baby. 20. Ellegård EK, Oscarsson J, Bougoussa M, et al. Serum level
of placental growth hormone is raised in pregnancy
rhinitis. Arch Otolaryngol Head Neck Sur. 1998;124:439-
43.
Vol 7, No 4
October 2019 Nasal Congestion and its Management 326
21. Flint PW. Cummings Otolaryngology: Head and Neck 25. Gilbey P, McGruthers L, Morency AM, Shrim A.
Surgery: Elsevier, Saunders; 2015. Rhinosinusitis-related quality of life during pregnancy.
22. Bousquet PJ, Combescure C, Klossek JM, Daures JP, Am J Rhinol Allergy. 2012;26(4):283-6. Epub
Bousquet J. Change in visual analog scale score in a 2012/07/18.
pragmatic randomized cluster trial of allergic rhinitis. 26. Incaudo GA, Takach P. The diagnosis and treatment
J Allergy Clin Immunol. 2009;123(6):1349-54. Epub of allergic rhinitis during pregnancy and lactation.
2009/04/17. Immunol Allergy Clin North Am. 2006;26(1):137-54.
23. Stewart M, Witsell DL, Smith TL, Weaver EM, Yueh Epub 2006/01/31.
B, Hannley MT. Development and validation of the 27. Ellegård EK. Etiology and Management of Pregnancy
Nasal Obstruction Symptom Evaluation (NOSE) scale. Rhinitis. Am J Respir Med 2003;2(6):469-75.
Otolaryngol Head Neck Sur. 2004;130:157–63. 28. Ellegård EK. Special considerations in the treatment of
24. Wu P, Wang Z, Zhang L, et al. [Application of the pregnancy rhinitis. Women's Health. 2005;1(1):105-14.
discharge, inflammation, polyps/edema (DIP) 29. Bastier PL, Lechot A, Bordenave L, Durand M, de Gabory
endoscopic scoring system in patients with chronic L. Nasal irrigation: From empiricism to evidence-based
rhinosinusitis]. Zhonghua er bi yan hou tou jing wai medicine. A review. Eur Ann Otorhinolaryngol Head
ke za zhi = Chin J Otorhinolaryngol Head Neck Sur. Neck Dis. 2015;132(5):281-5. Epub 2015/09/08.
2015;50(2):151-4. Epub 2015/04/29.
You might also like
- Respiratory DrugsDocument56 pagesRespiratory DrugsIra G. Delos Santos100% (1)
- Drugs Acting On Respiratory System 6640Document137 pagesDrugs Acting On Respiratory System 6640Umar Bakshi100% (1)
- Management of Asthma in PregnancyDocument59 pagesManagement of Asthma in PregnancyakokpanasNo ratings yet
- RhinitisDocument23 pagesRhinitisDr. T. BalasubramanianNo ratings yet
- Snake BiteDocument206 pagesSnake BiteElviraThaherNo ratings yet
- The Common Cold GuideDocument27 pagesThe Common Cold Guidehappyscottlee3438No ratings yet
- Respiratory Distress of The New BornDocument15 pagesRespiratory Distress of The New BornJicko Street HooligansNo ratings yet
- Slide JurnalDocument30 pagesSlide Jurnalmeta medianaNo ratings yet
- Journal Reading Rhinitis and PregnancyDocument29 pagesJournal Reading Rhinitis and PregnancyDestiWindaUtamiNo ratings yet
- 1 s2.0 S0385814622000323 MainDocument7 pages1 s2.0 S0385814622000323 MainFakhri KartanegaraNo ratings yet
- Rhinitis and Pregnancy Literature ReviewDocument7 pagesRhinitis and Pregnancy Literature ReviewFranklin Pito JellaNo ratings yet
- Jper 17-0557Document16 pagesJper 17-0557Yury Tenorio CahuanaNo ratings yet
- Asthma in Pregnancy 2020Document10 pagesAsthma in Pregnancy 2020Rosintchi MirsalNo ratings yet
- Otorhinolaryngology: Rhinitis and Pregnancy: Literature ReviewDocument7 pagesOtorhinolaryngology: Rhinitis and Pregnancy: Literature ReviewShebaTariganNo ratings yet
- Respiratory Physiology PregnancyDocument13 pagesRespiratory Physiology PregnancyAlejandra RequesensNo ratings yet
- Asthma in Pregnant WomenDocument9 pagesAsthma in Pregnant WomenICU RSBSMGNo ratings yet
- Treatment of AsthmaDocument6 pagesTreatment of AsthmaEdmond HubertNo ratings yet
- 3239-Article Text-35659-2-10-20230707Document14 pages3239-Article Text-35659-2-10-20230707ariniNo ratings yet
- 4 Respiratory Distress Syndrome in The NewbornDocument3 pages4 Respiratory Distress Syndrome in The NewbornChristine Danica BiteraNo ratings yet
- Rinitis 2Document5 pagesRinitis 2gemala wahabNo ratings yet
- Rinitis 8Document4 pagesRinitis 8gemala wahabNo ratings yet
- Obstructing Sleep Apnea in Pregnancy: Journal of AnesthesiologyDocument4 pagesObstructing Sleep Apnea in Pregnancy: Journal of AnesthesiologyjoitNo ratings yet
- Pulmonary Disorders: Dr. Manal Shafik Swelem Lecturer of Obstetrics & GynecologyDocument48 pagesPulmonary Disorders: Dr. Manal Shafik Swelem Lecturer of Obstetrics & Gynecologysalah subbahNo ratings yet
- 4Document7 pages4UgaugaaNo ratings yet
- 05 N293 35232Document21 pages05 N293 35232Agung RezpectorNo ratings yet
- LR Rhinitis in Pregnancy BKDocument38 pagesLR Rhinitis in Pregnancy BKadithyaNo ratings yet
- Efek ProgesteronDocument5 pagesEfek ProgesteronRomannaNo ratings yet
- Eview Rticle: Journal of Advanced Medical and Dental Sciences ResearchDocument8 pagesEview Rticle: Journal of Advanced Medical and Dental Sciences ResearchIndah AmaliaNo ratings yet
- 37004-Article Text-130842-2-10-20180629Document5 pages37004-Article Text-130842-2-10-20180629nishita biswasNo ratings yet
- Management of Asthma During Pregnancy: Symposium ContDocument6 pagesManagement of Asthma During Pregnancy: Symposium ContWulan CerankNo ratings yet
- MCP 1Document5 pagesMCP 1RENITA USWATUN HASANAH 1No ratings yet
- Falla Respiratoria & Embarazo - Lapinsky 2015Document7 pagesFalla Respiratoria & Embarazo - Lapinsky 2015Fabiola Buelna GaxiolaNo ratings yet
- Anaesthetic Considerations For Non-Obstetric Surgery During PregnancyDocument7 pagesAnaesthetic Considerations For Non-Obstetric Surgery During PregnancyniaNo ratings yet
- Transient Tachypnea of The Newborn: BackgroundDocument9 pagesTransient Tachypnea of The Newborn: BackgroundAnnisa YusufNo ratings yet
- Journal Reading-Critical AppraisalDocument28 pagesJournal Reading-Critical AppraisalHanifah RahmaniaNo ratings yet
- Management of Pregnant Patients in Dental Practice: Pramod - Mats@yahoo - Co.inDocument8 pagesManagement of Pregnant Patients in Dental Practice: Pramod - Mats@yahoo - Co.inYashaswiniTateneniNo ratings yet
- Kurien 2013Document11 pagesKurien 2013Atena VenturaNo ratings yet
- Umj 1x Mentariang 3429 1 Artikel F PDFDocument10 pagesUmj 1x Mentariang 3429 1 Artikel F PDFRestu PurwistaNo ratings yet
- Preterm / Premature Labor: EtiologyDocument8 pagesPreterm / Premature Labor: EtiologyCheney BalbuenaNo ratings yet
- Zona Kedokteran - Vol. 11 No. 2 Mei 2021: Correlation Age and Parity With Hiperemesis GravidarumDocument6 pagesZona Kedokteran - Vol. 11 No. 2 Mei 2021: Correlation Age and Parity With Hiperemesis GravidarumTeuku Ilham AkbarNo ratings yet
- PregnancyDocument5 pagesPregnancyRezky RahmayantiNo ratings yet
- Management of Pregnant Patient in Dentistry: February 2013Document11 pagesManagement of Pregnant Patient in Dentistry: February 2013Nirma JerabunNo ratings yet
- Corticosteroid For Septic Shock PatientsDocument3 pagesCorticosteroid For Septic Shock PatientsstevenmattarunganNo ratings yet
- Laryngomalacia PDFDocument6 pagesLaryngomalacia PDFFilologus SiwabessyNo ratings yet
- Perinatal - Outcome - in - Oligohydramnios SynopsisDocument16 pagesPerinatal - Outcome - in - Oligohydramnios SynopsisdhanrajramotraNo ratings yet
- Perawatan Asma Pada Wanita HamilDocument12 pagesPerawatan Asma Pada Wanita HamilWulan CerankNo ratings yet
- Report Introduction and Nursing With Maternity Premature Rupture of MembranesDocument13 pagesReport Introduction and Nursing With Maternity Premature Rupture of MembranessyaifulNo ratings yet
- The Effects of Pregnancy On AsthmaDocument34 pagesThe Effects of Pregnancy On AsthmaShawn DyerNo ratings yet
- Comparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.Document54 pagesComparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.prasadNo ratings yet
- Vol-2 Issue-1 Approach To Respiratory Distress in The Newborn 19Document13 pagesVol-2 Issue-1 Approach To Respiratory Distress in The Newborn 19salamredNo ratings yet
- Maternal Adaptations To Pregnancy: Gastrointestinal TractDocument21 pagesMaternal Adaptations To Pregnancy: Gastrointestinal Tractkabulkabulovich5No ratings yet
- Current Concepts in Migraine and Their Relevance To PregnancyDocument6 pagesCurrent Concepts in Migraine and Their Relevance To PregnancyWiwit Zuriati UnoNo ratings yet
- Karya Ilmiah NersDocument13 pagesKarya Ilmiah NersYusmira SusantiNo ratings yet
- Iadt04i5p333 PDFDocument7 pagesIadt04i5p333 PDFBilly UntuNo ratings yet
- Respiratory Distress in The Newborn: Pediatrics in Review October 2014Document16 pagesRespiratory Distress in The Newborn: Pediatrics in Review October 2014turigauNo ratings yet
- Shimokaze Et Al-2015-Journal of Obstetrics and Gynaecology ResearchDocument8 pagesShimokaze Et Al-2015-Journal of Obstetrics and Gynaecology ResearchMusa LandeNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument40 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Askep Maternity Group 4Document61 pagesAskep Maternity Group 4Rahayu RahmatikaNo ratings yet
- Respiratory Disorders and PregnancyDocument23 pagesRespiratory Disorders and PregnancyAngelie RojasNo ratings yet
- Pustotina (2019) 19 - Effects of Antibiotictherapy in Women With The Amniotic FluidsDocument14 pagesPustotina (2019) 19 - Effects of Antibiotictherapy in Women With The Amniotic FluidsRodrigo MelloNo ratings yet
- 3234 6050 1 SMDocument9 pages3234 6050 1 SMPutri RamadhaniNo ratings yet
- Hormonal Causes of Recurrent Pregnancy Loss RPLDocument10 pagesHormonal Causes of Recurrent Pregnancy Loss RPLQONITA PRASTANo ratings yet
- Gambaran Gingivitis Pada Ibu HamilDocument9 pagesGambaran Gingivitis Pada Ibu HamilHamzah SahagNo ratings yet
- Allergology International: Mehtap Haktanir Abul, Wanda PhipatanakulDocument8 pagesAllergology International: Mehtap Haktanir Abul, Wanda Phipatanakulfirst nameNo ratings yet
- Characterization of Children With Recurrent Episodes of Stevens Johnson SyndromeDocument17 pagesCharacterization of Children With Recurrent Episodes of Stevens Johnson SyndromeIndah AulliaNo ratings yet
- Pediatric Patient With A Rash: Ase EportDocument3 pagesPediatric Patient With A Rash: Ase EportIndah AulliaNo ratings yet
- Peserta KKLPPM MARET 2021Document4 pagesPeserta KKLPPM MARET 2021Indah AulliaNo ratings yet
- Knowledge Attitude and Practices of MothersDocument4 pagesKnowledge Attitude and Practices of MothersalfinNo ratings yet
- No. Waybill Tanggal Pengiriman Tempat Tujuan Berat AktualDocument2 pagesNo. Waybill Tanggal Pengiriman Tempat Tujuan Berat AktualIndah AulliaNo ratings yet
- CASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationDocument4 pagesCASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationwatiNo ratings yet
- Edi Sunardi 10/17/2018: Designed by Checked by Approved by Date DateDocument1 pageEdi Sunardi 10/17/2018: Designed by Checked by Approved by Date DateIndah AulliaNo ratings yet
- Chen2019 Article MenAtRiskOfGonococcalUrethritiDocument7 pagesChen2019 Article MenAtRiskOfGonococcalUrethritiIndah AulliaNo ratings yet
- CASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationDocument4 pagesCASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationwatiNo ratings yet
- 3418-Article Text-6894-1-10-20140701 PDFDocument8 pages3418-Article Text-6894-1-10-20140701 PDFKids 30No ratings yet
- CSR AnalysisDocument10 pagesCSR AnalysisNikita AgustinNo ratings yet
- Jurnal Sains Kebidanan: Olesan Minyak Zaitun Mengurangi Derajat Ruam Popok Pada Anak 0-24 BulanDocument5 pagesJurnal Sains Kebidanan: Olesan Minyak Zaitun Mengurangi Derajat Ruam Popok Pada Anak 0-24 BulanIndah AulliaNo ratings yet
- Faktor-Faktor Yang Berpengaruh Terhadap Kejadian Demam Berdarah Dengue Pada Anak Usia 6-12 Tahun Di Kecamatan TembalangDocument10 pagesFaktor-Faktor Yang Berpengaruh Terhadap Kejadian Demam Berdarah Dengue Pada Anak Usia 6-12 Tahun Di Kecamatan Tembalangasri TripkarNo ratings yet
- RagozineDocument28 pagesRagozineMoisés MedinaNo ratings yet
- Nutrients: Malnutrition As A Strong Predictor of The Onset of SarcopeniaDocument13 pagesNutrients: Malnutrition As A Strong Predictor of The Onset of SarcopeniaIndah AulliaNo ratings yet
- Nutrients: Poor Oral Health As A Determinant of Malnutrition and SarcopeniaDocument17 pagesNutrients: Poor Oral Health As A Determinant of Malnutrition and SarcopeniaIndah AulliaNo ratings yet
- Diagnosis of Acute Appendicitis Selected For Critical Appraisal 1-4-2011 Gr2Document8 pagesDiagnosis of Acute Appendicitis Selected For Critical Appraisal 1-4-2011 Gr2Paulo Henrique DuarteNo ratings yet
- 2020 06 18 Coronavirus Covid 19 Infection in PregnancyDocument61 pages2020 06 18 Coronavirus Covid 19 Infection in PregnancyIndah AulliaNo ratings yet
- Gonococcal Urethritis Caused by A Multidrug Resistant Neisseria Gonorrhoeae Strain With High Level Resistance To Spectinomycin in ChinaDocument4 pagesGonococcal Urethritis Caused by A Multidrug Resistant Neisseria Gonorrhoeae Strain With High Level Resistance To Spectinomycin in ChinaIndah AulliaNo ratings yet
- "New Insights On Bone Modeling and Remodeling in Response To Mechanical Loading" X. Edward Guo, Ph.D. Columbia UniversityDocument1 page"New Insights On Bone Modeling and Remodeling in Response To Mechanical Loading" X. Edward Guo, Ph.D. Columbia UniversityIndah AulliaNo ratings yet
- Jurnal Obgyn Kel 7Document25 pagesJurnal Obgyn Kel 7Indah AulliaNo ratings yet
- AdverseDocument3 pagesAdverseRini Novita SariNo ratings yet
- Incidence and Risk Factors For Postpartum Hemorrhage Among Transvaginal Deliveries at A Tertiary Perinatal Medical Facility in JapanDocument8 pagesIncidence and Risk Factors For Postpartum Hemorrhage Among Transvaginal Deliveries at A Tertiary Perinatal Medical Facility in Japanayu prima kusuma putriNo ratings yet
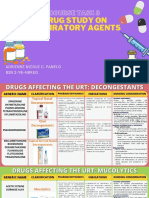
- Course Task 8 Drug Study On Respiratory AgentsDocument23 pagesCourse Task 8 Drug Study On Respiratory AgentsAdrienne Nicole PaneloNo ratings yet
- Get Rid of A Cough 1Document8 pagesGet Rid of A Cough 1Sridhara SriNo ratings yet
- List of Poison Drug (Ed Vers)Document34 pagesList of Poison Drug (Ed Vers)adam malikNo ratings yet
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocument13 pagesChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonNo ratings yet
- SyrupDocument5 pagesSyrupgsd mindNo ratings yet
- Cough, Cold, and Allergy: AntitussivesDocument8 pagesCough, Cold, and Allergy: AntitussivesSalsabila RaniahNo ratings yet
- Allergic Rhinitis: PathophysiologyDocument28 pagesAllergic Rhinitis: Pathophysiologysneh1509No ratings yet
- Boots ROI Healthcare Assistant Programme Module 1 WorkbookDocument82 pagesBoots ROI Healthcare Assistant Programme Module 1 WorkbookevacawleyNo ratings yet
- Quiz 1: General MOADocument38 pagesQuiz 1: General MOASajeda A. HadiNo ratings yet
- Ent-Hns Clinical Practice Guidelines: Acute Bacterial RhinosinusitisDocument11 pagesEnt-Hns Clinical Practice Guidelines: Acute Bacterial RhinosinusitisClarice VillanuevaNo ratings yet
- Nasal Decongestant: Hibah AL-Abri Eyman AL-Harbi Jawaher AL-AmoudiDocument23 pagesNasal Decongestant: Hibah AL-Abri Eyman AL-Harbi Jawaher AL-AmoudiRonak Patel80% (5)
- Drugs Acting On Respiratory SystemDocument3 pagesDrugs Acting On Respiratory SystemAlyssa Audrey CaoagasNo ratings yet
- An Overview of Anti-Allergic Drug Therapy and The Histamine-1 AntihistaminesDocument7 pagesAn Overview of Anti-Allergic Drug Therapy and The Histamine-1 Antihistaminesalinamatei1000000No ratings yet
- Villareal - NCMA216 Drug StudyDocument10 pagesVillareal - NCMA216 Drug StudyRozen VillarealNo ratings yet
- EAC BASIC Respiratory Pharmacology DrugsDocument130 pagesEAC BASIC Respiratory Pharmacology DrugsMARK RYAN HERNANDEZNo ratings yet
- Practice Giving Advice For These Problems: InstructionsDocument3 pagesPractice Giving Advice For These Problems: InstructionsMaier OlimpiuNo ratings yet
- What Is Allergic Rhinitis Urdu Meaning, CausesDocument1 pageWhat Is Allergic Rhinitis Urdu Meaning, CausesfariitrustNo ratings yet
- Drugs On RespiratoryDocument17 pagesDrugs On RespiratoryIrwan M. IskoberNo ratings yet
- Drugs Affecting The Respiratory System: Department of Pharmacology Medical Faculty Brawijaya UniversityDocument79 pagesDrugs Affecting The Respiratory System: Department of Pharmacology Medical Faculty Brawijaya UniversitySatya BimantaraNo ratings yet
- Pharm 28 29 30 ExamDocument3 pagesPharm 28 29 30 Examkay belloNo ratings yet
- Nasal Decongestants, Diet Pills and StimulantsDocument5 pagesNasal Decongestants, Diet Pills and Stimulantsphoton090109572No ratings yet
- Nasal Decongestant: Done byDocument25 pagesNasal Decongestant: Done byRHYDHM0% (1)
- MCC32 PhenylephrineDocument19 pagesMCC32 Phenylephrinemanoj_raju1688No ratings yet
- 2ARandomizedControlledVol24No2 3june Sep2006P97Document7 pages2ARandomizedControlledVol24No2 3june Sep2006P97I Made AryanaNo ratings yet
- DecongestantsDocument3 pagesDecongestantskNo ratings yet
- Pseudoephedrine HydrochlorideDocument6 pagesPseudoephedrine HydrochlorideAbdelrhman AboodaNo ratings yet
- Drug StudyDocument2 pagesDrug StudyGel Marie LobatonNo ratings yet