Professional Documents
Culture Documents
When Not To Stop A Clinical Trial.23490736
Uploaded by
Gloria KartikaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
When Not To Stop A Clinical Trial.23490736
Uploaded by
Gloria KartikaCopyright:
Available Formats
When (Not) to Stop a Clinical Trial for Benefit
Stuart J. Pocock
JAMA. 2005;294(17):2228-2230 (doi:10.1001/jama.294.17.2228)
Online article and related content
current as of August 16, 2010. http://jama.ama-assn.org/cgi/content/full/294/17/2228
Correction Contact me if this article is corrected.
Citations This article has been cited 33 times.
Contact me when this article is cited.
Topic collections Medical Practice; Medical Ethics; Randomized Controlled Trial
Contact me when new articles are published in these topic areas.
Related Articles published in Randomized Trials Stopped Early for Benefit: A Systematic Review
the same issue Victor M. Montori et al. JAMA. 2005;294(17):2203.
Subscribe Email Alerts
http://jama.com/subscribe http://jamaarchives.com/alerts
Permissions Reprints/E-prints
permissions@ama-assn.org reprints@ama-assn.org
http://pubs.ama-assn.org/misc/permissions.dtl
Downloaded from www.jama.com at Houston Academy of Medicine on August 16, 2010
EDITORIALS
21. Alliance for Cervical Cancer Prevention. Effectiveness, safety, and acceptabil- 25. Crum CP. The beginning of the end for cervical cancer? N Engl J Med. 2002;
ity of cryotherapy: a systematic literature review. Available at: http://www.path 347:1703-1705.
.org/files/RH_cryo_white_paper.pdf. Accessibility verified October 5, 2005. 26. Skjeldstad FE, Koustsky L; for the Merck Phase III HPV Vaccine Steering Com-
22. Cox JT. Management of cervical intraepithelial neoplasia. Lancet. 1999;353: mittee (FUTURE II). Phase III trial of prophylactic quadrivalent HPV 6, 11, 16, 18
857-859. L1 virus-like particle (VLP) vaccine: prevention of cervical intraepithelial neoplasia
23. Samson SL, Bentley JR, Fahey TJ, McKay DJ, Gill GH. The effect of loop elec- (CIN) 2/3 including adeno- and squamous-cell carcinoma in situ (CIS). Presented
trosurgical excision procedure on future pregnancy outcome. Obstet Gynecol. 2005; at: Infectious Diseases Society of America Late Breaker Session 66, LB-8a; Octo-
105:325-332. ber 7, 2005; San Francisco, Calif.
24. Goldie SJ, Kuhn L, Denny L, Pollack A, Wright TC. Policy analysis of cervical- 27. Blumenthal PD. Immunization against cervical cancer: Who? When? Where?
cancer screening strategies in low-resource settings: clinical benefits and cost Available at: http://www.medscape.com/viewarticle/444979. Accessibility veri-
effectiveness. JAMA. 2001;285:3107-3115. fied October 5, 2005.
When (Not) to Stop a Clinical Trial
for Benefit cal practice, some lenient statistical boundaries are not a sen-
Stuart J. Pocock, PhD
sible choice in the direction of benefit. For instance, the so-
I
N THIS ISSUE OF JAMA, MONTORI AND COLLEAGUES1 PRO- called Pocock boundary9 and the O’Brien-Fleming boundary’s
vide a valuable extensive and critical systemic review last interim look9 both typically require values around P=.02
of clinical trials that were stopped early for benefit. Read- for stopping, which is usually insufficient strength of evi-
ers of the reports of such trials often feel a sense of ex- dence to stop a trial for benefit. Both boundaries can be made
citement, especially when phrases such as “a major treat- more appropriate if the overall type I error is set at 1% rather
ment advance,” “ethical need to stop the inferior treatment,” than the conventional 5%.
and “vital to tell the world immediately” are used. How- Many complex methods exist for statistical stopping bound-
ever, experience suggests that early results and enthusi- aries, whereas in practice there is considerable merit in the
asm, especially for modestly sized trials terminated early for simple Haybittle-Peto boundary,9 which requires P⬍.001 as
apparent major benefit, are often moderated as subsequent evidence required to consider stopping a trial early for ben-
reports arise.2 efit. Even so, such a boundary should not be applied too soon,
The skeptic should ask first whether correct and appro- when few outcome events have been observed.
priate structures were in place for analyzing and review- Decisions on early stopping (or not) need to be based on
ing, and making decisions based on, the trial’s accumulat- wise judgments interpreting the totality of available evi-
ing interim data. Having the members of an effective dence, both in the current trial (considering primary and
independent data monitoring committee (DMC) or data and other efficacy outcomes and safety issues) and in other ex-
safety monitoring board as the only individuals accessing ternal evidence (especially from related trials).10 Accord-
and interpreting interim data split by treatment group is now ingly, a statistical stopping boundary is only one useful ob-
considered an essential part of good practice for major ran- jective component in an inevitably more challenging decision-
domized trials.3-5 Still, a substantial minority of reported ma- making process. The ethical dilemma is to safeguard the
jor trials appear not to have a DMC in place.6 interests of patients randomized in the current trial while
Second, with or without a formal DMC recommenda- also protecting society from overzealous premature claims
tion, another question is whether the decision to stop a trial of treatment benefit.11 For instance, if a trial is evaluating a
early and report the results was an appropriate judgment. treatment meant to be given long-term for conditions such
This decision should be aided by a predefined statistical stop- as hypertension or chronic arthritis, short-term benefits, no
ping boundary for a primary outcome,7-9 but some trials have matter how statistically significant, may not merit early stop-
no such guideline. It is important that such a boundary is ping. If a trial is for regulatory approval, the sponsor and
sufficiently stringent (eg, very strong evidence of a treat- trialists should be encouraged not to stop early unless there
ment difference with a very small P value) to match the ethi- is overwhelming evidence of treatment superiority, since the
cal and public health implications of a decision to stop the regulators require substantial evidence of both efficacy and
trial. In a spirit of requiring proof beyond reasonable doubt
that a treatment difference is sufficient to affect future clini- Author Affiliation: Medical Statistics Unit, London School of Hygiene and Tropi-
cal Medicine, London, England.
Corresponding Author: Stuart J. Pocock, PhD, Medical Statistics Unit, London School
See also p 2203. of Hygiene and Tropical Medicine, Keppel St, London WC1E 7HT, England (stuart
.pocock@lshtm.ac.uk).
2228 JAMA, November 2, 2005—Vol 294, No. 17 (Reprinted) ©2005 American Medical Association. All rights reserved.
Downloaded from www.jama.com at Houston Academy of Medicine on August 16, 2010
EDITORIALS
safety, often in at least 2 trials reaching their intended full hence an exaggerated claim of survival benefit was avoided
size and patient follow-up. and important long-term benefits in other outcomes, such
Montori et al1 rightly draw attention to some reports of as cardiovascular death and heart failure hospitalization, were
trials that were stopped early but that did not document realized in each of the 3 component trials of the CHARM
the planned size and circumstances of the relevant interim program.
analysis and stopping boundary. Such deficiencies need So when is it appropriate to stop a trial early? The ASCOT
correcting by authors, peer reviewers, and editors in line factorial trial’s data monitoring experience provides useful
with CONSORT recommendations.12 Indeed, journals insights.15,16 First, in 10305 patients with hypertension, the
should consider rejecting the report of any trial potentially comparison of atorvastatin with placebo was halted when
stopped prematurely and lacking adequate documentation, the difference in the primary end point, major coronary
and access to trial protocols by journals would help in events, at interim analysis reached P⬍.001, the stopping
making this decision. There is probably less need to pre- boundary. With 100 vs 154 primary events in the atorvas-
sent adjusted analyses that attempt to correct for the tatin and placebo groups, respectively, and a risk ratio of
interim monitoring and early stopping, since stopping 0.64 (P=.0005), the published result was clear-cut.15 The
depends on more than a statistical boundary, and com- appropriateness of stopping early was supported by other
plexities of adjustment can clutter the presentation of trials of statins in other populations and by important ben-
results and make interpretation of the findings more diffi- efits in other outcomes, such as stroke.
cult. Real insight rests more on a full understanding of the A more difficult stopping decision arose in the ASCOT
circumstances at the time of stopping. Also, between the trial for the 19342 patients randomized to receive
moment of making the decision to stop and locking the amlodipine-based and atenolol-based regimens. The pre-
final database used for analysis and publication, substantial defined primary end point was major coronary events,
additional and corrected data may become available for whereas it is well known that the key effect of antihyper-
analysis. Indeed, such data cleaning may justify a pause tensive treatment is in reducing risk of stroke. Thus, when
before any definite decision to stop the trial. there emerged a highly significant reduction in stroke for
From a reader’s perspective, the key problem is whether amlodipine-based compared with atenolol-based treatment
to believe the treatment benefit is truly as great as the data (P⬍.001), much debate ensued on whether to stop the
imply. Montori et al1 appropriately emphasize that trials stop- trial, resulting in a decision to continue to the next interim
ping early will tend to be on a “random high” of observed analysis. Some months later, the trial was stopped early
benefit, and if further data had been collected in either this when there was also a significantly higher rate of mortality
or another trial, some “regression to the truth” to a more in the atenolol-based group, although still no significant
modest effect estimate would occur.2,13 These issues are more difference existed for the primary end point. This example
pronounced in smaller trials. illustrates the complexities and tough decisions that can
Montori et al reported a median of 66 events observed at arise in data monitoring.17
the time trials were stopped. To achieve a difference Can a trial be stopped on the basis of secondary end points?
between treatment that is significant at P⬍.001 requires a Perhaps not, but on occasion, such as with the ASCOT-BPLA
split by treatment group of at least 46 vs 20 events, which study, results of secondary end points (327 strokes with am-
means that risk happens to be reduced by 57% or more. In lodipine vs 422 with atenolol, a 23% risk reduction
most therapeutic areas, this is highly implausible and is [P = .0003]) provide convincing evidence of great public
often associated with relatively short patient follow-up health importance.16 In lay terms, “when early results proved
time. Thus in many settings, trials should not stop so soon, so promising it was no longer fair to keep patients on the
because it is highly likely that the therapeutic claim is older drugs for comparison, without giving them the op-
exaggerated. portunity to change.”18 However, the data in these 2 ex-
The data monitoring experience in the CHARM pro- amples are more substantial compared with those in the ma-
gram in 7599 patients with heart failure provides a thought- jority of trials reviewed by Montori et al. The message is clear:
provoking example.14 At the fourth interim analysis with a most trials stopped early for benefit should not have been
median 1-year follow-up, there were 260 vs 339 deaths in stopped at that point. Stopping for harm or futility is an-
the candesartan and placebo groups, respectively, a 24% risk other matter19 that equally importantly requires future sys-
reduction that crossed the P⬍.001 stopping boundary. For tematic review and comment. Inappropriate stopping of trials
several documented reasons,14 the DMC voted to continue for commercial reasons raises additional serious con-
until the next interim analysis. The treatment mortality dif- cerns.20
ference was then attenuated in subsequent interim analy- In summary, all major randomized trials should have an
ses so that at the trial’s intended completion with a median independent DMC that functions effectively and makes wise
of 3.1 years of follow-up, there were 886 deaths in the can- judgments aided by stringent statistical stopping bound-
desartan group vs 945 deaths in the placebo group, a 9% aries for benefit. It is critical that the DMC, principal inves-
risk reduction (P= .055). Early stopping was resisted, and tigators, executive committees, and sponsors all recognize
©2005 American Medical Association. All rights reserved. (Reprinted) JAMA, November 2, 2005—Vol 294, No. 17 2229
Downloaded from www.jama.com at Houston Academy of Medicine on August 16, 2010
EDITORIALS
the full public health implications of their recommenda- 10. Brocklehurst P, Elbourne D, Alfirevic A. The role of external evidence in moni-
toring clinical trials: reflections from a perinatal trial. BMJ. 2000;320:995-998.
tions and decisions. 11. Pocock SJ. When to stop a clinical trial. BMJ. 1992;305:235-240.
Financial Disclosures: None reported. 12. Moher D, Schulz KF, Altman DG; CONSORT Group. The CONSORT state-
ment: revised recommendations for improving the quality of reports of parallel-
group randomized trials. JAMA. 2001;285:1987-1991.
REFERENCES 13. Pocock S, White I. Trials stopped early: too good to be true? Lancet. 1999;353:
1. Montori VM, Devereaux PJ, Adhikari NKJ, et al. Randomized trials stopped early 943-944.
for benefit: a systematic review. JAMA. 2005;294:2203-2209. 14. Pocock S, Wang D, Wilhelmsen L, Hennekens CH. The data monitoring ex-
2. Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical perience in the Candarsartan in Heart failure Assessment of Reduction in Mortal-
research. JAMA. 2005;294:218-228. ity and morbidity (CHARM) program. Am Heart J. 2005;149:939-943.
3. Ellenberg S, Fleming T, DeMets D. Data Monitoring Committees in Clinical 15. Sever P, Dahlof B, Poulter NR, et al; ASCOT Investigators. Prevention of coro-
Trials: A Practical Perspective. Chichester, England: John Wiley & Sons; 2002. nary and stroke events with atorvastatin in hypertensive patients who have aver-
4. Draft guidance for clinical trial sponsors on the establishment and operation age or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian
of clinical trial data monitoring committees, 66 Federal Register 58151-58153 Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre ran-
(2001). domised controlled trial. Lancet. 2003;361:1149-1158.
5. DAMOCLES Study Group. A proposed charter for clinical trial data monitoring 16. Dahlöf B, Sever PS, Poulter NR, et al; ASCOT Investigators. Prevention of
committees: helping them to do their job well. Lancet. 2005;365:711-722. cardiovascular events with an antihypertensive regimen of amlodipine adding
6. Sydes M, Altman DG, Babiker AB, Parmar M, Spiegelhalter DJ; DAMOCLES perindopril as required versus atenolol adding bendroflumethiazide as required,
Study Group. Reported use of data monitoring committees in the main published in the Anglo-Scandanavian Cardiac Outcomes Trial—Blood Pressure Lowering Arm
reports of randomised controlled trials: a cross-sectional study. Clin Trials J. 2004; (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366:
1:48-59. 895-906.
7. O’ Brien P. Data and safety monitoring. In: Armitage P, Colton T, eds. Ency- 17. DeMets DL, Furberg CD, Friedman L. Data Monitoring in Clinical Trials: A
clopedia of Biostatistics. Chichester, England: John Wiley & Sons; 1998:1058- Case Studies Approach. Heidelberg, Germany: Springer; 2005.
1066. 18. Hall C. Heart attacks may be cut by half. Daily Telegraph. September 5, 2005:1.
8. Fleming TR, Harrington DP, O’Brien PC. Designs for group sequential tests. 19. DeMets DL, Pocock SJ, Julian DG. The agonising negative trend in monitor-
Control Clin Trials. 1984;5:348-361. ing of clinical trials. Lancet. 1999;354:1983-1988.
9. Schulz KF, Grimes DA. Multiplicity in randomised trials, II: subgroup and in- 20. Psaty BM, Rennie D. Stopping medical research to save money: a broken pact
terim analyses. Lancet. 2005;365:1657-1661. with researchers and patients. JAMA. 2003;289:2128-2130.
2230 JAMA, November 2, 2005—Vol 294, No. 17 (Reprinted) ©2005 American Medical Association. All rights reserved.
Downloaded from www.jama.com at Houston Academy of Medicine on August 16, 2010
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Risk Assessment Form: Zibran Anwar SayyadDocument2 pagesRisk Assessment Form: Zibran Anwar SayyadMufid SatamkarNo ratings yet
- Insertion of An Intra-Aortic Balloon Catheter: PurposeDocument4 pagesInsertion of An Intra-Aortic Balloon Catheter: PurposeGloria KartikaNo ratings yet
- Contoh Surat SponsorDocument1 pageContoh Surat SponsorGloria KartikaNo ratings yet
- Survival Analysis, Part 3: Cox Regression: Statistics and Research DesignDocument2 pagesSurvival Analysis, Part 3: Cox Regression: Statistics and Research DesignGloria KartikaNo ratings yet
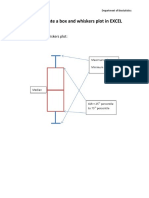
- How To Create A Box and Whiskers Plot in EXCELDocument9 pagesHow To Create A Box and Whiskers Plot in EXCELGloria KartikaNo ratings yet
- MC GowanDocument13 pagesMC GowanGloria KartikaNo ratings yet
- Cardiology Board Review - Carlquist - PT. 1 PDFDocument40 pagesCardiology Board Review - Carlquist - PT. 1 PDFGloria KartikaNo ratings yet
- CLN 66 01 107 PDFDocument5 pagesCLN 66 01 107 PDFGloria KartikaNo ratings yet
- QTinterval Changes During The Management of DHFDocument7 pagesQTinterval Changes During The Management of DHFGloria KartikaNo ratings yet
- Prevalensi Ventricular HypertrophyDocument8 pagesPrevalensi Ventricular HypertrophyGloria KartikaNo ratings yet
- 24 Newsletter Hypertension and ArrhythmiaDocument2 pages24 Newsletter Hypertension and ArrhythmiaGloria KartikaNo ratings yet
- WHO LadderDocument2 pagesWHO LaddertelorkodokNo ratings yet
- 6.21.10 Rose-Jones Board ReviewDocument50 pages6.21.10 Rose-Jones Board ReviewGloria KartikaNo ratings yet
- Clinical Management 07Document22 pagesClinical Management 07Fauzi SatriaNo ratings yet
- Vision2020 ReportDocument97 pagesVision2020 ReportAdelaida Castro NavarreteNo ratings yet
- WHO Blindness Action An 2014-2019Document28 pagesWHO Blindness Action An 2014-2019Gloria KartikaNo ratings yet
- Staining and Tooth DiscolorationDocument14 pagesStaining and Tooth DiscolorationGloria KartikaNo ratings yet
- Kuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)Document17 pagesKuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)DillaNo ratings yet
- WHO Clinical Management 0f Avian InfluenzaDocument83 pagesWHO Clinical Management 0f Avian InfluenzaGloria KartikaNo ratings yet
- Degeneratif Copy 2Document7 pagesDegeneratif Copy 2Gloria KartikaNo ratings yet
- CH 06Document11 pagesCH 06kavitasibalNo ratings yet
- Infeksi Marginalis NadaDocument48 pagesInfeksi Marginalis NadaGloria KartikaNo ratings yet
- Hypertension: H.) or May Be Associated With Other Diseases - Dorland'sDocument1 pageHypertension: H.) or May Be Associated With Other Diseases - Dorland'sGloria KartikaNo ratings yet
- Kuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)Document17 pagesKuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)DillaNo ratings yet
- European Psychiatry: Emma Kinnaird, Catherine Stewart, Kate TchanturiaDocument10 pagesEuropean Psychiatry: Emma Kinnaird, Catherine Stewart, Kate TchanturiaJenderal BesarNo ratings yet
- 2019 Nclex RN Cram SheetDocument7 pages2019 Nclex RN Cram Sheetpjhay93% (82)
- Pathcare Labs Antenatal Test ReportDocument8 pagesPathcare Labs Antenatal Test ReportTrilok TripathiNo ratings yet
- Pearls in Medicine For Students PDFDocument303 pagesPearls in Medicine For Students PDFGabriela Cordova Goicochea100% (2)
- Drug StudyDocument2 pagesDrug Studykev mondaNo ratings yet
- Knowledge and Hygiene Practice of Prisoners Towards Dermatophytosis - A Study in Nakkhu Prison, NepalDocument15 pagesKnowledge and Hygiene Practice of Prisoners Towards Dermatophytosis - A Study in Nakkhu Prison, Nepalbibek karkiNo ratings yet
- Dermatitis and HomoeopathyDocument18 pagesDermatitis and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Leukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNDocument41 pagesLeukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNRahul DhakerNo ratings yet
- COVID-19 MRNA Vaccine MRNA-1273 ModernaDocument4 pagesCOVID-19 MRNA Vaccine MRNA-1273 ModernawalkrogNo ratings yet
- The Early Identification of Autism: The Checklist For Autism in Toddlers (CHAT)Document43 pagesThe Early Identification of Autism: The Checklist For Autism in Toddlers (CHAT)melaniNo ratings yet
- Manajemen Asuhan Kebidanan Pada Ibu Hamil Dengan Hiperemesis Gravidarum Tingkat IDocument8 pagesManajemen Asuhan Kebidanan Pada Ibu Hamil Dengan Hiperemesis Gravidarum Tingkat IErni ChanNo ratings yet
- Hiv PresentationDocument10 pagesHiv Presentationapi-534814911No ratings yet
- COVID-19: Dr. Moe Yee Soe Assistant Lecturer Department of Microbiology UM1Document42 pagesCOVID-19: Dr. Moe Yee Soe Assistant Lecturer Department of Microbiology UM1Naing Lin SoeNo ratings yet
- Basic Pharmacology: NTA Level 4 Semester 2Document16 pagesBasic Pharmacology: NTA Level 4 Semester 2MabusiNo ratings yet
- Allied Health ProfessionalsDocument19 pagesAllied Health ProfessionalsReihnard RosariioNo ratings yet
- Pedh ExamDocument12 pagesPedh ExamJames100% (2)
- Critical Values List: Arterial Blood GasesDocument3 pagesCritical Values List: Arterial Blood Gasesiq_dianaNo ratings yet
- Welcome To The Morning SessionDocument20 pagesWelcome To The Morning SessionGENERAL sharpNo ratings yet
- Internal DiseaseDocument55 pagesInternal Diseaseshilpa sekhar278No ratings yet
- The Prevalence of Stroke and Associated DisabilityDocument6 pagesThe Prevalence of Stroke and Associated DisabilityRaymond LinatocNo ratings yet
- Anesthesia For Patients With Diabetes Mellitus - UpToDateDocument31 pagesAnesthesia For Patients With Diabetes Mellitus - UpToDateEduardoNo ratings yet
- Statistical Analysis On Risk Factors of Prevalence of Malaria in Z/ Dugda Woreda, Oromia, East ArsiDocument31 pagesStatistical Analysis On Risk Factors of Prevalence of Malaria in Z/ Dugda Woreda, Oromia, East Arsitewodrosmolalign19No ratings yet
- Case Presentation Non-Hodgkin's LymphomaDocument13 pagesCase Presentation Non-Hodgkin's LymphomaMau Gallevo100% (4)
- User Manual: (High Intensity Focused Ultrasound)Document11 pagesUser Manual: (High Intensity Focused Ultrasound)Agha SoroushNo ratings yet
- Laws in HealthDocument1 pageLaws in Healthrouya100% (3)
- Utilizing Battling Rope Exercises For HIIT and SMITDocument50 pagesUtilizing Battling Rope Exercises For HIIT and SMITJaydaa Kamel EL ArabyNo ratings yet
- Personality DisordersDocument125 pagesPersonality DisordersDevendra Singh Baryah100% (2)
- Professional-grade dermatoscope for early skin cancer detectionDocument2 pagesProfessional-grade dermatoscope for early skin cancer detectionHemkerovner Keresztszegh von Kolowrat-KrakowskyNo ratings yet
- Skin CancerDocument24 pagesSkin CancerMister David anthonyNo ratings yet