Professional Documents
Culture Documents
Ophthalmology: Osteo-Odonto-Keratoplasty: A Review
Uploaded by
Anish Kafoor NoordeenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ophthalmology: Osteo-Odonto-Keratoplasty: A Review
Uploaded by
Anish Kafoor NoordeenCopyright:
Available Formats
Sarode et al.
J Clinic Experiment Ophthalmol 2011, 2:10
Clinical & Experimental http://dx.doi.org/10.4172/2155-9570.1000188
Ophthalmology
Review Article
Research Article OpenAccess
Open Access
Osteo-odonto-keratoplasty: A Review
Gargi S. Sarode1*, Sachin C. Sarode2 and Jashika S. Makhasana3
1
Senior Lecturer, Department of Oral Pathology and Microbiology, Dr. D. Y. Patil Dental College and Hospital, Maheshnagar, Pimpri, Pune – 18, Maharashtra, India
2
Associate Professor, Department of Oral Pathology and Microbiology, Dr. D. Y. Patil Dental College and Hospital, Maheshnagar, Pimpri, Pune – 18, Maharashtra, India
3
Department of Oral Pathology and Microbiology, Dr. D. Y. Patil Dental College and Hospital, Maheshnagar, Pimpri, Pune – 18, Maharashtra, India
Abstract
Objectives: To discuss the historical background of osteo-odonto-keratoprosthesis (OOKP), patients’ selection
criteria, preoperative assessment of the patients, OOKP technique in detail and its modifications along with the
complications involved.
Data Sources: Data for this narrative review were identified by searches of MEDLINE, Current Contents, PubMed,
and references from relevant articles using the search term ‘osteo-odonto-keratoprosthesis’, ‘canine’, ‘eye’, ‘blindness’
and ‘Sjogren’s syndrome’. Articles published in English medical literature containing studies and case reports on osteo-
odonto-keratoprosthesis are included in the present review.
Conclusions: OOKP technique is a complex artificial corneal (keratoprosthetic) transplantation procedure in which
an autologus dental root-bone lamina complex and buccal mucosal graft are used to mount a poly-methylmethacrylate
optical cylinder, as an artificial cornea. OOKP surgery is usually the last resort for end-stage corneal blindness, where
other treatments have failed, or will not be successful.
Introduction the procedure has undergone further refinements, which are referred
to as the Rome-Vienna Protocol [18].
Corneal opacification is the second commonest cause of world
blindness affecting an estimated 10 million people [1]. The visual Patient selection criteria
rehabilitation of such patients is a challenging task. Not only the Patients with bilateral corneal blindness resulting from severe end-
conventional corneal graft but a wide variety of materials have been stage Stevens-Johnson syndrome [5,6,9], Lyell syndrome [19], ocular
tried earlier as artificial corneal implants, including metals, ceramics, cicatricial pemphigoid, chemical or thermal burns, end stage trachoma,
glass, plastics and biological tissue, for the anchoring skirts or plates or severe keratitis, dry eyes, multiple failed grafts and graft-versus-host
haptic [2,3]. For the optic, only medical grade polymethylmethacrylate disease and consequences of perforating injuries may be considered
(PMMA) has been used since the last 50 years [4]. The three most for OOKP surgery [20]. The other causes of dry eye are ectodermal
commonly used keratoprosthesis (KPs) are the Dohlman collar button dysplasia, ionizing radiation damage, cicatrizing conjunctivitis from
type [4], the Osteo-Odonto keratoprosthesis (OOKP) by Strampelli [5], topical medication, congenital trigeminal nerve hypoplasia, linear IgA
Falcinelli in Italy and Liu in UK [6] and the Pintucci biointegrable KP disease and nutritional deficiency [20,21]. Though Goosen et al. [22]
by Pintucci in Italy [7,8]. and Chammartin et al. [23] have reported cases of bilateral OOKPs,
the vision of only one eye should be corrected. The better eye, with
The original OOKP technique was pioneered by the late Italian
poor vision is rehabilitated [21]. However patients who are satisfied
surgeon Benedetto Strampelli MD in 1963 [5,9]. OOKP is an eterotopic
with their level of vision, children under the age of 17, eyes that have
autograft and the term stands for osteo (bone)-odonto (tooth)-kerato
no perception of light, evidence of phthisis, advanced glaucoma or
(cornea) prosthesis (artificial device) [10] and thus the technique is
irreparable retinal detachment should be excluded [21].
also known as “a tooth for an eye” technique [11,12]. Recent innovative
changes to the original Strampelli technique have further reduced the Pre operative assessment
incidence of failures to less than 10% of cases [13].
Each patient should undergo detailed evaluation by a team of
OOKP surgery is usually the last resort for severe, end-stage ocular and oral surgeons and radiologists who form a surgical team.
corneal blindness, where other treatments such as corneal grafts [14], This evaluation should include the detailed history and aetiology of loss
stem cell and amniotic membrane transplantations [15,16] and other of vision and a comprehensive ocular and oral examination.
forms of ocular surface reconstruction surgery have failed, or will not
be successful [9].
Historical background *Corresponding author: Gargi S. Sarode M.D.S, Senior Lecturer, Department
of Oral Pathology and Microbiology, Dr. D. Y. Patil Dental College and Hospital,
The first artificial corneal implant was placed in a human eye by Maheshnagar, Pimpri, Pune – 18, Maharashtra, India, Tel: +919823871462;
E-mail: gargi14@gmail.com
Nussbaum, 150 years ago [3]. Strampelli (1963) [5] had noted that
gutta-percha will remain in the root canal of a tooth indefinitely, but Received August 16, 2011; Accepted October 04, 2011; Published October 14,
2011
will be rejected if implanted into soft tissues. So it would seem probable
that if a plastic acrylic implant could be held in a piece of the patient’s Citation: Sarode GS, Sarode SC, Makhasana JS (2011) Osteo-odonto-
keratoplasty: A Review. J Clinic Experiment Ophthalmol 2:188. doi:10.4172/2155-
tooth and bone, and the whole placed in a corneal envelope, the tooth
9570.1000188
and bone would form an autograft picture-frame for the acrylic, and so
prevent its extrusion [17]. The technique was largely abandoned in the Copyright: © 2011 Sarode GS, et al. This is an open-access article distributed
under the terms of the Creative Commons Attribution License, which permits
1970s due to poor results. An Italian surgeon, Dr. Gian Carlo Falcinelli unrestricted use, distribution, and reproduction in any medium, provided the
made numerous improvements in the 1980s. Over the past few years, original author and source are credited.
J Clinic Experiment Ophthalmol
ISSN:2155-9570 JCEO an open access journal Volume 2 • Issue 10 • 1000188
Citation: Sarode GS, Sarode SC, Makhasana JS (2011) Osteo-odonto-keratoplasty: A Review. J Clinic Experiment Ophthalmol 2:188. doi:10.4172/2155-
9570.1000188
Page 2 of 5
Ophthalmic assessment [21] Psychological assesment [21]
Preoperative examination involves determining an intact and Patients have to understand that they may require multiple
functioning retina and optic nerve. The degree of dry eye is noted, procedures and that there is a significant risk of serious complications
although a severe dry eye is not a contraindication unlike other forms including loss of the eye. The patient must commit to life-long follow-
of KPs. The conjunctiva and cornea are examined and evidence of stem up, and not have unreasonable expectations of outcome and cosmesis.
cell failure, metaplasia, or dysplasia is noted. Thinning of the cornea
Procedure: The technique involves three procedures stages [9]
and evidence of previous corneal perforation, iris adhesion, and degree
of vascularization are also taken into consideration. Stage 1a: Tooth ostectomy, preparation of the osteo-odonto lamina,
cementation of the optic cylinder in the lamina, and submuscular
Oral assessment implantation in the contralateral infraorbital area
The oral assessment must take into account both the buccal Stage 1b: Removal of the ocular surface, harvesting of a full-
mucosal graft donor site and a selection of an appropriate tooth to form thickness buccal mucosal graft, and coverage of the ocular surface with
a dentine/bone lamina. Buccal mucous membrane can be classified as the mucosal graft
being normal, scarred or diseased [9]. Some diseases affecting buccal Stage 2: Retrieval of the keratoprosthesis, lifting of the buccal
mucous membrane are recurrent aphthous ulceration, leukoplakia, mucosal graft and implantation of the keratoprosthesis into the eye
lichen planus and oral submucous fibrosis. Detrimental habits like
Stage 1: The procedure involves the preparation of an osteo-odonto-
smoking and betel nut chewing should be discontinued as it will
lamina tooth by harvesting a single rooted tooth [9,21]. If the surgeon
compromise tissue quality.
does not find the lamina’s surface large enough to allow the insertion of
The vitality of the teeth to be used with caries or restorations an optical cylinder, two teeth can be extracted to prepare two laminae,
should be tested using an electropulp tester. Panoramic and periapical which are then glued together with acrylic resin to prepare a larger
radiographs are taken; to estimate the length of the root in bone. The surface [19]. The resulting alveolar defect is covered with adjacent
healthiest and best-positioned tooth with best shape and size and mucosa. In Japan, surgeons are using artificial mucous membrane graft
good covering of alveolar bone is selected. After evaluation, patients to cover the defect to accelerate wound healing [26]. Casey [17] used
are graded on the basis of their dental condition as being suitable for half of the root after apicectomy and filled the remaining root part.
OOKP, at risk of complication or failure, or unsuitable for OOKP [9]. Prepare a rectangular lamina with the central part comprising
Oral hygiene and periodontal bone loss should be assessed. two third of the lamina and a thin cemental rim. The peripheral one
The most suitable tooth for modified preparation of the osteodental third part is of alveolar bone. The cementum and alveolar bone are
lamina is the maxillary canine9 because it has the longest and largest attached to each other by intact periodontal ligament, as seen in the
root with the greatest quantity of alveolar bone [19]. Contraindications normal tooth histological structure [19]. Stoiber J et al. [27] studied
for using a particular tooth include non-vitality, previous root canal OOKP histologically and found that the preservation of alveolar-dental
therapy, inadequate bone investing the root, peri-radicular pathology ligament seems to be essential for the maintenance of the integrity of
the OOKP. Ideal lamina should be of a size measuring 12 mm x 6 mm
and close proximity of adjacent teeth [9]. Other single-rooted teeth can
x 3 mm [9]. A hole of an average diameter of 3.70 mm (range, 3.3-4.0
be used in the absence of a canine [19]. The choice of upper or lower
mm) is prepared leaving an edge of dentine of 1 to 1.5 mm [19].
canine depends on the proximity of the maxillary sinus and the mental
foramen. In lower canine harvesting, buccal plate is occasionally thin A PMMA optical cylinder is inserted into the hole and cemented
and the lingual muco-periosteum is difficult to preserve. There is a risk to the osteodental lamina by means of biocompatible acrylic resin or
of antrum perforation in case of upper canine [21]. PMMA cement [9,19]. Some operators discourage the use of dental
cement as it may act as an irritant [17]. The optical characteristics of
In the majority of patients, an autologous osteodental lamina is the PMMA optical cylinder are, mean intraocular diameter, 4.1 mm
used. Occasionally when there is no suitable tooth available or in case of (range, 3.6-4.6 mm); mean extraocular diameter, 3.65 mm (range, 3.3-
edentulous patients an allogaft is considered [17]. A tooth from a first- 4.0 mm); mean length, 7.75 mm (range, 7.25-8.25 mm); mean radius
degree relative with the highest number of compatible HLA antigen of the convex extraocular surface, 16 mm; mean radius of the convex
sites can be used [19] but long term results studied by Liu et al. [20] intraocular surface, 6.5 mm; refractive index, 1.49; and equivalent
showed that HLA-matched allografts suffered a higher rate of laminar power, 50.8 diopters [28,29].
resorption. Nail (onycho-keratoprosthesis) can be used instead of a
tooth but it has the disadvantage that it is dead tissue, but if it is taken Hull et al. [30] have concluded that it is possible to increase the
from the nail root, it is liable to grow in the eye. Casay et al. [17] have theoretical maximum visual field through these cylinders. The optical
used a chondro-keratoprosthesis, a piece of cartilage removed from the cylinder with wider diameter offers a wider visual field for the patient
8th costal cartilage and have reported their best results to date. Some [17].
surgeons found tibial bone ie temprano- keratoprosthesis (TKP) as a The prepared complex is inserted beneath the orbicularis oculi
better option [16,24]. muscle just below the contralateral lower orbital rim, for a period of two
and half to four months to allow for osteo-odontal tissue recovery and
Viitala R et al. [25] have tried synthetic analogue (bioceramics)
formation of a fibrovascular covering over the lamina [9,19]. (Figure 1)
instead of OOKP and found that at normal physiologic pH the
degradation of bioceramics was equivalent to tooth and bone. However A buccal mucous membrane graft which is preferred to cover the
at pH of 6.5 to 5 associated with infectious and inflamed tissue, the ocular surface as it contains stem cells. It has proliferating capability and
degradation rate of bioceramics was much higher when compared to is adapted to high bacterial load [21]. The buccal graft of full thickness
bone and teeth. mucosa without including muscle and large enough (approximately
J Clinic Experiment Ophthalmol
ISSN:2155-9570 JCEO an open access journal Volume 2 • Issue 10 • 1000188
Citation: Sarode GS, Sarode SC, Makhasana JS (2011) Osteo-odonto-keratoplasty: A Review. J Clinic Experiment Ophthalmol 2:188. doi:10.4172/2155-
9570.1000188
Page 3 of 5
• 2-year functional survival: 63% for OOKP and 49% for osteo-
keratoprosthesis ,
• 10-year functional survival: 38% for OOKP and 17% for osteo-
keratoprosthesis, with functional survival defined as best corrected
visual acuity above 0.05.
Fong et al. [32] used electron beam tomography (EBT) in imaging
of OOKP to identify early bone and dentine loss. They concluded that
it is important to monitor regularly the dimensions and stability of the
OOKP lamina as it will help detect cases that are at risk of extrusion of
the optical cylinder and consequent endophthalmitis. They also found
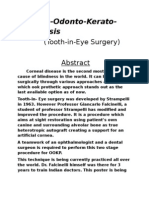
Figure 1: CT scan showing the prepared lamina complex just below the
contralateral lower orbital rim. It is kept for a period of two and half to four out that EBT have excellent resolution and speed and recommend
months to allow the tissue to recover and formation of a fibrovascular covering regular scanning of the lamina in all patients.
over the lamina.
Hille et al. [33] have implanted a total of 35KPs, 29 with biologoic
haptic (25 OOKP and 4 TKPs) and 6 KPs with biocompatible haptic.
3cm in diameter) to extend from medial to lateral canthi and from
There was no significant difference between the various types of KPs
upper to lower lid fornices is harvested taking care to avoid parotid
concerning the best postoperative visual acuity. During long term
duct orifice and lower buccal sulcus (mental nerve injury) [9]. It will follow up, only 1 of the KPs with biologic haptic (TKP) was lost
be vascularized by the time of Stage 2 surgery and will thus provide the compared with 4 out of 6 KPs with biocompatible haptic (P<0.0001).
blood supply to the bone part of the OOKP lamina. The graft is soaked Thus they concluded that OOKP leads to the best results in the long-
in an antibiotic solution like cefuroxime until required. An oval piece term follow up.
of buccal mucosa is prepared [21].
Percorella I et al. [34] biopsied the junction between the osteodental
If the eye is very dry or there is a risk of the mucous membrane acrylic lamina and surrounding modified oral mucosa in 7 patients
graft not taking, it may be better to perform Stage I surgery in two steps. and were examined by light microscopy. Six of the 7 corresponded
The mucous membrane graft to the eye is done first (stage IA), and it microscopically to conjunctiva. Typical oral mucosa could still
is only when the graft has been shown to be well established before be observed overlying the osteodental acrylic lamina. Thus they
the patient is readmitted for tooth harvesting and preparing an OOKP concluded that the production of local regulatory factors is a possible
lamina (stage IB) [21]. explanation for the survival of oral mucosa over the osteodental acrylic
Stage 2: Stage 2 surgery is carried out two to four months after lamina, whereas their absence in distant areas may have induced
Stage 1 [9,31]. The time interval helps graft and lamina to heal and the oral mucosa to transdifferentiate into a conjunctival-type lining.
vascularize properly. The soft tissue invests into the pores of the lamina Alternatively, conjunctival regrowth from forniceal stem cells should
and the lamina recovers from thermal damage and infection if present. be taken into consideration.
It is retrieved and inspected for adequate size. The fibrovascular
capsule is trimmed away from the optical surfaces of the PMMA optical
cylinder.
The buccal mucosal graft is reflected superiorly and cornea is
exposed [21]. Corneal trephination (5 mm-diameter) is done to
create a central opening in the eye. The iris is completely removed.
The keratoprosthesis is then placed into the opening, which serves
as a strong biological skirt to secure suturing of the keratoprosthesis
in position [9]. The buccal mucosal graft is sutured over the implant
and trephined in the centre to allow the anterior aspect of the optical
cylinder to protrude [9,21]. (Figure 2 and 3)
One month after surgery, a cosmetic prosthesis covering the
external ocular surface can be given [19]. Main outcome measures to
be considered are visual acuity, field of vision, anatomical integrity
and stability and complications related or unrelated to the OOKP
technique [31].
Figure 2: Schematic diagram showing OOKP and its placement in the eye.
Donald et al. [31] performed OOKP surgery on 15 patients, with
a mean follow-up of 19.1 months. Eleven patients (73.3%) attained a
stable best spectacle-corrected visual acuity of at least 20/40 or better,
whereas 9 (60%) attained stable 20/20 vision. Four patients achieved a
visual potential ranging from 20/100 to counting fingers vision.
The follow up of patients for 10 years by Michael et al. [24] yielded
following statistics:
• 10-year anatomical survival: 66% for OOKP and 47% for osteo- Figure 3: Eye with OOKP showing optical cylinder (white arrow) and
surrounding buccal mucosal graft (black arrow).
keratoprosthesis,
J Clinic Experiment Ophthalmol
ISSN:2155-9570 JCEO an open access journal Volume 2 • Issue 10 • 1000188
Citation: Sarode GS, Sarode SC, Makhasana JS (2011) Osteo-odonto-keratoplasty: A Review. J Clinic Experiment Ophthalmol 2:188. doi:10.4172/2155-
9570.1000188
Page 4 of 5
Percorella I et al. [35] demonstrated elastic and precursor fibers 3. Fracture of tooth will render it useless as a lamina for the optical
and distribution of collagen types I to VI in bone and dental tissue cylinder
which were exposed to the ocular surface. 4. Small part of the tooth if left behind in the bed will act as a nidus
Ricci R et al. [36] showed that preservation of the alveolar-dental for infection
ligament plays a definitive role in the maintenance of the prosthesis. If 5. Once the tooth is extracted it will result in cosmetic and functional
this tissue undergoes necrosis, the implanted material is eventually lost. problems like lisping while speaking and extrusion of liquids while
However, when no such event occurs the OOK is well preserved and eating
well tolerated even 20 years after implantation. 6. Palatal or lingual bone fracture
Complications 7. Exposure of roots of adjacent teeth due to poor healing: Damage can
be avoided by using sharp blades and careful technique
Ocular complications 8. Oroantral perforation leading to fistula formation: The damage to
the maxillary sinus can be avoided by not making the apical cut too
1. Forniceal and tarsal conjunctival cicatrization
high but if the root of the tooth is very close to the maxillary sinus,
2. Ocular surface inflammation this complication is unavoidable. (Figure 4)
3. Continuation of primary disease process resulting in shallow 9. Oronasal perforation
fornices, upper or lower lid cicatricial entropion and wide palpebral
10. Damage to mental nerve leading to lip paresthesia in case of
apertures mandibular canines
4. Buccal mucous membrane thinning, ulceration or necrosis
5. Globe perforation Systemic complications
6. Lamina infection: Caiazza et al. reported early and recurrent 1. Complications related to local and general anesthesia [38]
bacterial infections (Staphylococcus epidermidis) which resulted in
destruction of lamina 2. Immunosupression because of corticosteroid administration
7. Lamina resorption: Study by Liu et al. showed that the main factor Other complications
resulting in anatomical failure was OOKP lamina resorption
8. Vitreous haemorrhage Other complications not directly related to device insertion include
9. Choroidal and retinal detachment 1. Retinal detachment related to silicone oil removal
10. Glaucoma or macular disease : reported incidence is up to 75% [16] 2. Endophthalmitis related to endoscopic cyclophotocoagulation
11. . Fistula formation Acknowledgement
12. Extrusion of the optical cylinder: Results of the Strampelli’s OOKP- We would like to thank Mr. C. A. Sarode and Mr. A. R. Zarkar for their constant
technique show good long-term results with 2% loss of prosthesis support and encouragement.
over 27 years [16]. According to Falcinelli et al. 18 years after
surgery, the probability of retaining an intact OOKP was 85% [17]. References
A significant risk of 19% has been estimated by Liu et al. [22] 1. World Health Organization. The World Health Report 1998: life in the 21st
century. Geneva: WHO, 1998:47.
13. Retro implant membrane formation
2. Williams KA, Roder D, Esterman A, Muehlberg SM, Coster DJ (1992) Factors
14. Mild inferior optic tilt predictive of corneal graft survival: report from the Australian Corneal Graft
Registry. Ophthalmology 99: 403–414.
15. Increased intra ocular pressure
3. Quresh B, Maskati, Maskati BT (2006) Asian experience with the Pintucci
16. MRSA colonization keratoprosthesis. Indian J Ophthalmol 54: 89-94.
17. Periostitis of the lamina 4. Cardona H (1962) Keratoprosthesis. Am J Ophthalmol 54: 284. http://www.ijo.
in/article.asp?issn=0301-4738;year=2006;volume=54;issue=2;spage=89;epag
e=94;aulast=Maskati - ft4
Oral complications
5. Strampelli B (1963) Osteo-odonto-Keratoprosthesis. Annali di Ottalmologia e
1. Trismus resulting from submucosal scar formation Clinica Oculistica 89: 1029-1039.
2. Buccal mucous membrane infection 6. Liu C, Tighe B (1998) Striving for the perfect KP, editorial. Br J Ophthalmol
82: 3-4.
7. Geerling G, Liu C, Collin J, Dart J (2002) Cost and gains of complex procedures
to rehabilitate end stage ocular surface disease. Br J Ophthalmol 86: 1220-
1221.
8. Pintucci S, Pintucci F (1993) The Dacron Felt colonisable KP. Refract Corneal
Surg 9: 196-197.
9. Tay AB, Tan DT, Lye KW, Theng J, Parthasarathy A, et al. (2007) Osteo-
odonto-keratoprosthesis surgery: a combined ocular–oral procedure for ocular
blindness. Int J Oral Maxillofac Surg 36: 807–813.
10. www.eophtha.com
11. Langan EA, Liu C, Ogden S, Griffiths CE (2010) A tooth for an eye : cicatricial
Figure 4: Oro-antral fistula as a complication of OOKP procedure. pemphigoid and the osteo-odonto-keratoprosthesis. Arch Dermatol 146: 1188-
1189.
J Clinic Experiment Ophthalmol
ISSN:2155-9570 JCEO an open access journal Volume 2 • Issue 10 • 1000188
Citation: Sarode GS, Sarode SC, Makhasana JS (2011) Osteo-odonto-keratoplasty: A Review. J Clinic Experiment Ophthalmol 2:188. doi:10.4172/2155-
9570.1000188
Page 5 of 5
12. Monteiro MJ, Herold J, Liu C, Francis I (2009) Osteo-odonto-keratoprosthesis 26. Fakuda M, Hamada S, Liu C, Shimomura Y (2008) Osteo-odonto-
(OOKP): “a tooth for an eye” technique. Br J Oral Maxillofac Surg 47: e19. keratoprosthesis in Japan. Cornea 27: S56-61.
13. Falcinelli GC, Falsini B, Taloni M, Piccardi M, Falcinelli G (1995) Detection 27. Stoiber J, Csaky D, Schedle A, Ruckhofer J, Grabner G (2002) Histopathologic
of glaucomatous damage in patients with osteo-odontokeratoprosthesis. Br J findings in explanted osteo-odonto-keratoprosthesis. Cornea 21: 200-204.
Ophthalmol 79: 129-134.
28. Falcinelli GC, Barogi G, Colliardo P, Taloni M, Graziani L (1990) New Possibilities
14. Marchi V, Ricci R, Percorella I, Ciardi A, Di Tondu U (1994) Osteo-odonto-
in the Field of OOKP: Contribution to Glaucoma Surgery: Proceedings of the
keratoprosthesis. Description of surgical technique with results in 85 patients.
1st Congress Biomaterials in Ophthalmology: An Interdisciplinary Approach;
Cornea 13: 125-130.
Bologna, Italy. 131-135.
15. Hollick EJ, Watson SL, Dart JK, Luthert PJ, Allan BD (2006) Legeais BioKpro
III keratoprosthesis implantation: long term results in seven patients. Br J 29. Lupelli L, Fletcher RJ, Palumbo P, Menghi A, Taloni M (1999) Improved optics
Ophthalmol 90: 1146–1151. for OOKP. Anales del Instituto Barraque 28: 159-160.
16. Stoiber J, Grabner G (2005) Clinical management of severe ocular surface 30. Hull C, Liu CS, Sciscio A, Eleftheriadis H, Herold J (2000) Optical cylinder
disease. Klin Monbl Augenheilkd 222: 533-551. designs to increase the field of vision in the osteo-odonto-keratoprosthesis.
Graefes Arch Clin Exp Ophthalmol 238: 1002-1008.
17. Casey TA (1966) Osteo-odonto-keratoprosthesis. Proceedings of the Royal
Society of Medicine. 59: 530-531. 31. Tan DT, Tay AB, Theng JT, Lye KW, Parthasarathy A, et al. (2008)
Keratoprosthesis surgery for end-stage corneal blindness in asian eyes.
18. Liu C, Grabner G. Patients give eye teeth to see. www.http://lrd.yahooapis.
Ophthalmology 115: 503-510.e3.
com/
19. Falcinelli G, Falsini B, Taloni M, Colliardo P, Falcinelli G (2005) Modified 32. Fong KC, Ferrett CG, Tandon R, Paul B, Herold J, et al. (2005) Imaging of by
osteo-odonto-keratoprosthesis for treatment of corneal blindness long term electron beam tomography. Br J Ophthalmol 89: 956-959.
anatomical and functional outcomes in 181 cases. Arch Ophthalmol 133: 1319-
33. Hille K, Landau H, Ruprecht KW (2002) Osteo-odonto-keratoprosthesis. A
1329.
summary of 6 years surgical experience. Ophthalmolog 99: 90-95.
20. Liu C, Okera S, Tandon R, Herold J, Hull C, et al. (2008) Visual rehabilitation
in end-stage inflammatory ocular surface disease with the osteo-odonto- 34. Pecorella I, Maurizio T, Antonio C, Giancarlo F (2006) Progressive replacement
keratoprosthesis: results from the UK. Br J Oral Maxillofac Surg 92: 1211–1217. of oral mucosa by conjunctiva in osteo-odonto-keratoprosthesis: preliminary
observations. Cornea 25: 193-195.
21. Liu C, Paul B, Tandon R, Lee E, Fong K, et al. (2005) The Osteo-Odonto-
Keratoprosthesis (OOKP). Semin Ophthalmol 20: 113–128. 35. Pecorella I, Taloni M, Ciardi A, Alexander RA, Falcinelli G. (2006) Osteo-
odonto-keratoprosthesis: a human model of autotransplant. Curr Eye Res 31:
22. Goossen C, Stempels N, Colpaert C, Tassignon MJ (1998) Strampelli osteo- 835-843.
odonto-keratoprosthesis: case report. Bull Soc Belge Ophtalmol 268: 129-133.
36. Ricci R, Pecorella I, Ciardi A, Della Rocca C, Di Tondo U, et al. (1992)
23. Chammartin M, Goldblum D, Fruh B, Wilkens L, Bosshardt D, et al. (2009)
Strampelli’s osteo-odonto-keratoprosthesis. Clinical and histological long-term
Case report of osteo-odonto-keratoprosthesis (Strampelli) and of Dacron
features of three prostheses. Br J Oral Maxillofac Surg 76: 232-234.
keratoprosthesis (Pintucci). Klin Monbl Augenheilkd 226: 180-183.
24. Michael R, Charoenrook V, de la Paz MF, Hitzl W, Temprano J, et al. (2008) 37. Caiazza S, Falcinelli G, Pintucci S (1990) Exceptional case of bone resorption
„Long-term functional and anatomical results of osteo- and osteoodonto- in an osteo-odonto-keratoprosthesis. A scanning electron microscopy and
keratoprosthesis“. Graefes Arch Clin Exp Ophthalmol 246: 1133–1137. X-ray microanalysis study. Cornea 9: 23-27.
25. Viitala R, Franklin V, Green D, Liu C, Lloyd A, et al. (2009) Towards a synthetic 38. Skelton VA, Henderson K, Liu C (2000) Anaesthetic implications of osteo-
osteo-odonto-keratoprosthesis. Acta Biomaterialia 5: 438-452. odonto-keratoprosthesis surgery. Eur J Anaesth 17: 390-394.
Submit your next manuscript and get advantages of OMICS
Group submissions
Unique features:
• User friendly/feasible website-translation of your paper to 50 world’s leading languages
• Audio Version of published paper
• Digital articles to share and explore
Special features:
• 200 Open Access Journals
• 15,000 editorial team
• 21 days rapid review process
• Quality and quick editorial, review and publication processing
• Indexing at PubMed (partial), Scopus, DOAJ, EBSCO, Index Copernicus and Google Scholar etc
• Sharing Option: Social Networking Enabled
• Authors, Reviewers and Editors rewarded with online Scientific Credits
• Better discount for your subsequent articles
Submit your manuscript at: www.editorialmanager.com/clinicalgroup
J Clinic Experiment Ophthalmol
ISSN:2155-9570 JCEO an open access journal Volume 2 • Issue 10 • 1000188
You might also like
- Innovations in Endoscopic Ear SurgeryFrom EverandInnovations in Endoscopic Ear SurgerySeiji KakehataNo ratings yet
- 2 YdcDocument8 pages2 YdcŞahin ŞahinNo ratings yet
- Osteo-Odonto-Kerato ProsthesisDocument2 pagesOsteo-Odonto-Kerato ProsthesisdrmanudeoraNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyKarina Mega WNo ratings yet
- Five Year PROSE Treatment For Aniridic KojimaOct2016PAPDocument5 pagesFive Year PROSE Treatment For Aniridic KojimaOct2016PAP小島隆司No ratings yet
- Chronological Developmental Study in Cataract SurgeryDocument8 pagesChronological Developmental Study in Cataract SurgeryRagni MishraNo ratings yet
- Priyanka ProfileDocument15 pagesPriyanka ProfilevarunNo ratings yet
- Corneal TransplantationDocument10 pagesCorneal TransplantationKabelo MaruvaNo ratings yet
- Five-Year Results of ViscotrabeculotomyDocument10 pagesFive-Year Results of ViscotrabeculotomyChintya Redina HapsariNo ratings yet
- The Boston KeratoprosthesisDocument6 pagesThe Boston KeratoprosthesisliyaNo ratings yet
- 2018 Autologous Fat Graft For The Treatment of Sighted Posttraumatic Enophthalmos and Sunken Upper EyelidDocument6 pages2018 Autologous Fat Graft For The Treatment of Sighted Posttraumatic Enophthalmos and Sunken Upper EyelidDimitris RodriguezNo ratings yet
- Borgia Gonzalo, Ravecca Tabaré, Fumero Miriam, Pebé PabloDocument13 pagesBorgia Gonzalo, Ravecca Tabaré, Fumero Miriam, Pebé PabloJaime Angel Ortiz DiazNo ratings yet
- Artigo 04Document17 pagesArtigo 04Julia PimentelNo ratings yet
- Ophthalmology: Journal of and Advance ResearchDocument14 pagesOphthalmology: Journal of and Advance ResearchAthenaeum Scientific PublishersNo ratings yet
- Keratopati BulosaDocument7 pagesKeratopati BulosaShafira LusianaNo ratings yet
- JurnalDocument8 pagesJurnalDesi SafitriNo ratings yet
- Rehabilitation of Patient With Ocular Defects-Case ReportDocument4 pagesRehabilitation of Patient With Ocular Defects-Case ReportbhupendraNo ratings yet
- Refractive Surgery: The Never Ending Task of Improving Vision CorrectionDocument2 pagesRefractive Surgery: The Never Ending Task of Improving Vision CorrectiondedypurnamaNo ratings yet
- Surgical and Endodontic Management of Large Cystic Lesion: AbstractDocument5 pagesSurgical and Endodontic Management of Large Cystic Lesion: AbstractanamaghfirohNo ratings yet
- Safety and Efficacy of Colored Iris Reconstruction Lens ImplantationDocument12 pagesSafety and Efficacy of Colored Iris Reconstruction Lens ImplantationDanty IndriastutyNo ratings yet
- JR OrthoDocument6 pagesJR OrthoVirgyan L. SunandarNo ratings yet
- 10 1093@ejo@cjy070Document10 pages10 1093@ejo@cjy070sssrao575No ratings yet
- Jced 10 E1145Document4 pagesJced 10 E1145lily oktarizaNo ratings yet
- Vitreous Function and Intervention of It With Vitrectomy and Other ModalitiesDocument11 pagesVitreous Function and Intervention of It With Vitrectomy and Other Modalitiesmistic0No ratings yet
- The History of Corneal Transplantation: Chad K RostronDocument14 pagesThe History of Corneal Transplantation: Chad K RostronDebby SiltamiNo ratings yet
- 2016 Article 229Document7 pages2016 Article 229nisa_kartikaNo ratings yet
- Lentile ScleraleDocument40 pagesLentile ScleraleLauraNo ratings yet
- 2023 The Use of Zirconia For Implant-Supported Fixed Complete Dental Prostheses Narrative ReviewDocument14 pages2023 The Use of Zirconia For Implant-Supported Fixed Complete Dental Prostheses Narrative Reviewgerardo telloNo ratings yet
- Rare Case of A Conjunctival Cyst Formation in An Anophthalmic Socket of A 10 Years Old PatientDocument2 pagesRare Case of A Conjunctival Cyst Formation in An Anophthalmic Socket of A 10 Years Old PatientPeertechz Publications Inc.No ratings yet
- Int Endodontic J - 2022 - Bai - Enhanced Conservation of Vital Pulp and Apical Tissues by The Application of Crown RotationDocument7 pagesInt Endodontic J - 2022 - Bai - Enhanced Conservation of Vital Pulp and Apical Tissues by The Application of Crown RotationShakeel AhmedNo ratings yet
- Ankylo PDFDocument8 pagesAnkylo PDFHamba AllahNo ratings yet
- Accepted Manuscript: 10.1016/j.ajo.2014.05.016Document20 pagesAccepted Manuscript: 10.1016/j.ajo.2014.05.016Anonymous iInKGkMCNo ratings yet
- Dentistry: Overcoming Obstacles in OligodontiaDocument4 pagesDentistry: Overcoming Obstacles in Oligodontiarajeev singhNo ratings yet
- Full Mouth Zirconia Based Implant Supported Fixed Dental Prostheses. Five Year - Results of A Clinical Pilot StudyDocument5 pagesFull Mouth Zirconia Based Implant Supported Fixed Dental Prostheses. Five Year - Results of A Clinical Pilot StudyAndres CurraNo ratings yet
- Roll Man 2013Document6 pagesRoll Man 2013SergioNo ratings yet
- Materials 14 07829 PDFDocument19 pagesMaterials 14 07829 PDFQS ZHOUNo ratings yet
- Corneal Transplantation in Modern EraDocument16 pagesCorneal Transplantation in Modern Eraसुनन्दन भट्टNo ratings yet
- Nasal Prosthesis - A Case ReportDocument4 pagesNasal Prosthesis - A Case ReportInternational Organization of Scientific Research (IOSR)No ratings yet
- Resume 15Document9 pagesResume 15Dyah PurwitaNo ratings yet
- Multidisciplinary Treatment Approach To A Complicated Crown Fracture: A Case ReportDocument5 pagesMultidisciplinary Treatment Approach To A Complicated Crown Fracture: A Case Reportramadan ariesthaNo ratings yet
- 10 1111@cid 12748Document8 pages10 1111@cid 12748Behnam TaghaviNo ratings yet
- Cataract Surgery and Dry Eye Disease: A Review: Khayam Naderi, Jack Gormley and David O'BrartDocument16 pagesCataract Surgery and Dry Eye Disease: A Review: Khayam Naderi, Jack Gormley and David O'BrartBima RyandaNo ratings yet
- Implant-Retained Auricular Prosthesis: A Case Report: January 2010 - Vol.4Document4 pagesImplant-Retained Auricular Prosthesis: A Case Report: January 2010 - Vol.4noranNo ratings yet
- Long-Term Survival of Indirect Pulp Treatment Performed in Primary and Permanent Teeth With Clinically Diagnosed Deep Carious LesionsDocument4 pagesLong-Term Survival of Indirect Pulp Treatment Performed in Primary and Permanent Teeth With Clinically Diagnosed Deep Carious LesionsBAHAMON TRUJILLO MAYRA ALEJANDRANo ratings yet
- Implant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyDocument8 pagesImplant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyMohammad Fadyl YunizarNo ratings yet
- Optical Coherence Tomography Angiography Findings in Stargardt DiseaseDocument11 pagesOptical Coherence Tomography Angiography Findings in Stargardt DiseaseYasminSolbergNo ratings yet
- Sonali WordDocument19 pagesSonali Wordsarjak shahNo ratings yet
- Comparison of Postoperative Refractive Outcome in Eyes UndergoingDocument9 pagesComparison of Postoperative Refractive Outcome in Eyes UndergoingAndi Ayu LestariNo ratings yet
- Comparison of The Outcome of Silicone Ahmed Glaucoma Valve Implantation With A Surface Area Between 96 and 184 MM in Adult EyesDocument7 pagesComparison of The Outcome of Silicone Ahmed Glaucoma Valve Implantation With A Surface Area Between 96 and 184 MM in Adult EyesVlady BordaNo ratings yet
- Matrix Metalloproteinase 8 Is The Major Potential C - 2012 - Journal of ProsthodDocument7 pagesMatrix Metalloproteinase 8 Is The Major Potential C - 2012 - Journal of Prosthodradwam123No ratings yet
- Iris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaDocument7 pagesIris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaMuhammad SukriNo ratings yet
- New Perative UlcerDocument5 pagesNew Perative UlcerkautsarreNo ratings yet
- Luyten 2020Document8 pagesLuyten 2020solodont1No ratings yet
- No Post-No Core Approach To Restore Severely Damaged Posterior Teeth - An Up To 10-Year Retrospective Study of Documented Endocrown CasesDocument7 pagesNo Post-No Core Approach To Restore Severely Damaged Posterior Teeth - An Up To 10-Year Retrospective Study of Documented Endocrown CasesDiana FreireNo ratings yet
- Lanza 2017Document7 pagesLanza 2017Promocoes PromoNo ratings yet
- Kjo 32 163Document9 pagesKjo 32 163John ElfranNo ratings yet
- Orthokeratology - WikipediaDocument29 pagesOrthokeratology - WikipediatyasNo ratings yet
- 12 DecDocument43 pages12 DecJayesh ThakkarNo ratings yet
- Ocular ProsthesisDocument3 pagesOcular ProsthesisAmar BhochhibhoyaNo ratings yet
- Ocular Damage in Craniofacial Orbital Trauma About 170 CasesDocument8 pagesOcular Damage in Craniofacial Orbital Trauma About 170 CasesAthenaeum Scientific PublishersNo ratings yet
- Scapulothoracic Dissociation 2165 7548.1000142Document2 pagesScapulothoracic Dissociation 2165 7548.1000142Fadlu ManafNo ratings yet
- C14 - Coloana Vertebrala Engleza 2Document109 pagesC14 - Coloana Vertebrala Engleza 2Andreea DanielaNo ratings yet
- Direct Sputum Smear Microscopy (DSSM) PDFDocument23 pagesDirect Sputum Smear Microscopy (DSSM) PDFSnowie BalansagNo ratings yet
- Bearded Dragon Periodontal Disease-Aurora Animal HospitalDocument1 pageBearded Dragon Periodontal Disease-Aurora Animal HospitalPedro Trotsky DeathMaskNo ratings yet
- Muhammad Rashid, Humaira Saleem, Saeed Bin Ayaz, Ijaz-Un-Nabi, Rashida Hussain, Faisal ManzoorDocument7 pagesMuhammad Rashid, Humaira Saleem, Saeed Bin Ayaz, Ijaz-Un-Nabi, Rashida Hussain, Faisal ManzoorEMIRZA NUR WICAKSONONo ratings yet
- COVID 19 Science Report Therapeutics 4 May PDFDocument41 pagesCOVID 19 Science Report Therapeutics 4 May PDFjolamo1122916No ratings yet
- AGA Manejo CU Leve A Moderada 2019Document17 pagesAGA Manejo CU Leve A Moderada 2019Residentes CirugiaNo ratings yet
- Ketamine and Its Effects On Sensory PerceptionDocument4 pagesKetamine and Its Effects On Sensory Perceptionapi-557854804No ratings yet
- The Impact of Cyberspace Usage Affecting Sleep DeprivationDocument8 pagesThe Impact of Cyberspace Usage Affecting Sleep DeprivationYeh HeetNo ratings yet
- Dental TrumaDocument26 pagesDental TrumaAseelNo ratings yet
- InsuracneDocument4 pagesInsuracnesathishbabuNo ratings yet
- Monitoring Public Health Reporting: Data Tracking in Cancer RegistriesDocument11 pagesMonitoring Public Health Reporting: Data Tracking in Cancer RegistriesMihaela BarbuNo ratings yet
- Entrepreneurship No.1 (AutoRecovered)Document6 pagesEntrepreneurship No.1 (AutoRecovered)Joeriel Agtas100% (1)
- Covid SOP Dated 24 To 31 August 2021Document15 pagesCovid SOP Dated 24 To 31 August 2021dadan vishwakarmaNo ratings yet
- 02 - Role of Taxonomy in SurveillanceDocument29 pages02 - Role of Taxonomy in Surveillanceserielt88No ratings yet
- Nims TariffDocument136 pagesNims TariffVaRmA67% (3)
- Viral Diseases in Honey BeesDocument7 pagesViral Diseases in Honey BeesMalsawmsanga ChhakchhuakNo ratings yet
- Rhu SurveyDocument9 pagesRhu SurveyAtiqah GULAMNo ratings yet
- Ekor Jantan: Brugia Malayi Mikrofilaria Brugia Timori Mikrofilaria Wuchereria Bancrofti MikrofilariaDocument9 pagesEkor Jantan: Brugia Malayi Mikrofilaria Brugia Timori Mikrofilaria Wuchereria Bancrofti MikrofilariavindychanNo ratings yet
- EXERCISE Last DecDocument9 pagesEXERCISE Last DecAzahwa 84No ratings yet
- Car&Ane&Pra&ASP&Sar&Gva&1 STDocument334 pagesCar&Ane&Pra&ASP&Sar&Gva&1 STAna Belén Artero CastañoNo ratings yet
- Asessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale EvaluationDocument3 pagesAsessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale EvaluationHikari 光 Shidou50% (2)
- Anabolic SteroidDocument23 pagesAnabolic SteroidBishal ChauhanNo ratings yet
- The Iceman: Discovery and Imaging1: Radiology April 2003Document17 pagesThe Iceman: Discovery and Imaging1: Radiology April 2003Nusrat Omar AntaraNo ratings yet
- Standar Singkatan RSCMDocument54 pagesStandar Singkatan RSCMyannastiNo ratings yet
- Policy NN012203163316 PrintNewDocument22 pagesPolicy NN012203163316 PrintNewPrabhakar bhaleraoNo ratings yet
- Medical Examiner InvestigationDocument11 pagesMedical Examiner InvestigationColleen WelcherNo ratings yet
- Hockenberry & Wilson - Wong - S Essentials of Pediatric Nursing, 8th EditionDocument20 pagesHockenberry & Wilson - Wong - S Essentials of Pediatric Nursing, 8th EditionJill Hill60% (5)
- The Role of Adaptogens in Stress ManagementDocument10 pagesThe Role of Adaptogens in Stress ManagementLevente BalázsNo ratings yet
- Possible Preeclampsia As Health DeficitDocument3 pagesPossible Preeclampsia As Health DeficitCharisse BulasaNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (39)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (3)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Fun Habit: How the Pursuit of Joy and Wonder Can Change Your LifeFrom EverandThe Fun Habit: How the Pursuit of Joy and Wonder Can Change Your LifeRating: 4.5 out of 5 stars4.5/5 (19)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Story of Philosophy: The Lives and Opinions of the Greater PhilosophersFrom EverandThe Story of Philosophy: The Lives and Opinions of the Greater PhilosophersNo ratings yet