Professional Documents
Culture Documents
Secnidazole Treatment of Bacterial Vaginosis: A Randomized Controlled Trial
Uploaded by
siska tiaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Secnidazole Treatment of Bacterial Vaginosis: A Randomized Controlled Trial
Uploaded by
siska tiaraCopyright:
Available Formats
Original Research
Secnidazole Treatment of Bacterial Vaginosis
A Randomized Controlled Trial
Sharon L. Hillier, PhD, Paul Nyirjesy, MD, Arthur S. Waldbaum, MD, Jane R. Schwebke, MD,
Franklin G. Morgan, MD, Nikki A. Adetoro, MS, PMP, and Carol J. Braun, MD
OBJECTIVE: To evaluate secnidazole as a single oral microbiologic cure. The modified intent to treat was
dose treatment for bacterial vaginosis in a phase 2 used for efficacy analyses and included all randomized
randomized, double-blind, placebo-controlled study. patients who met the enrollment criteria. Assuming
METHODS: In a phase 2, randomized, double-blind, a clinical cure rate of 40% in the active groups and 15%
dose-ranging, placebo-controlled study, women with in the placebo group, a sample size of 52 patients per
bacterial vaginosis who met all Amsel criteria (discharge; group provided approximately 80% power to detect
pH 4.7 or greater; 20% or greater clue cells; positive whiff a significant difference between groups (.05 level [two-
test) were randomized one to one to one at 24 U.S. sided]) using a Cochran-Mantel-Haenszel test.
centers to 1 or 2 g secnidazole compared with placebo. RESULTS: Between May and September 2014, 215 pa-
The primary endpoint was clinical cure (normalization of tients were enrolled. In the intent-to-treat population,
discharge, amine odor, and clue cells) 21–30 days after the clinical cure rate was 65.3% for the 2-g group, 49.3%
treatment. Secondary endpoints included microbiologic for the 1-g group, and 19.4% for the placebo group. The
cure, defined as a Nugent score of 0–3, and therapeutic modified intent-to-treat population included 188 women
cure, defined as meeting criteria for both clinical and (median age 33 years; 32% with four or more bacterial
vaginosis episodes in the previous year; 54% black) with
From the University of Pittsburgh and the Magee-Womens Research Institute, baseline Nugent scores 4 or greater. Clinical, microbio-
Pittsburgh, Pennsylvania; Drexel University School of Medicine, Philadelphia, logic, and therapeutic cure rates were 67.7%, 40.3%, and
Pennsylvania; Downtown Women’s Health Care, Denver, Colorado; the Uni- 40.3% for 2 g secnidazole and 51.6%, 23.4%, and 21.9%
versity of Alabama at Birmingham, Birmingham, Alabama; Tidewater Clinical
Research, Inc, Virginia Beach, Virginia; and Symbiomix Therapeutics, LLC, and
for 1 g secnidazole compared with 17.7%, 6.5%, and
SAJE Consulting LLC, Baltimore, Maryland. 6.5% for placebo, respectively (P,.05 for secnidazole
Funding for this study was provided to Magee-Womens Research Institute (S.L.H.), compared with placebo; all endpoints). Both doses were
Drexel University (P.N.), Downtown Women’s Health Care (A.S.W.), the well-tolerated.
University of Alabama (J.R.S.), and Tidewater Clinical Research, Inc (F.G.M.)
by Symbiomix Therapeutics, LLC, Baltimore, Maryland. Manuscript editing was CONCLUSION: Oral granules containing 1 and 2 g
also supported by Symbiomix Therapeutics, LLC. secnidazole were superior to placebo in bacterial vagi-
Presented at the 42nd Annual Meeting of the Infectious Diseases Society for nosis treatment (P,.001 for both groups). These data
Obstetrics and Gynecology, August 6–8, 2015, Portland, Oregon. support the development of secnidazole for bacterial
The authors thank Maryn Padula, PhD, of Virtuoso Healthcare Communications vaginosis treatment.
for assistance with manuscript editing.
CLINICAL TRIAL REGISTRATION: ClinicalTrials.gov,
Each author has indicated that he or she has met the journal’s requirements for NCT02147899.
authorship.
(Obstet Gynecol 2017;0:1–8)
Corresponding author: Sharon L. Hillier, PhD, Magee-Womens Research
DOI: 10.1097/AOG.0000000000002135
Institute, 204 Craft Avenue, B511 Pittsburgh, PA 15213; email: shillier@
mail.magee.edu.
T
Financial Disclosure reatments for bacterial vaginosis currently rec-
Dr. Hillier has received compensation as a consultant for Symbiomix
Therapeutics, LLC, Perrigo, Merck, and Cepheid Diagnostics. Drs. Hillier,
ommended by the Centers for Disease Control
Nyirjesy, Waldbaum, Schwebke, and Morgan all received grant support from and Prevention (CDC) include multidose oral and
Symbiomix Therapeutics, LLC, to their respective institutions for participation in vaginal formulations of metronidazole and clindamy-
this study. Ms. Adetoro and Dr. Braun (deceased) were employed by Symbiomix
Therapeutics, LLC, during the conduct of this study. cin.1 Alternative regimens include oral formulations
of tinidazole or clindamycin and intravaginal formu-
© 2017 by The American College of Obstetricians and Gynecologists. Published
by Wolters Kluwer Health, Inc. All rights reserved. lations of clindamycin and metronidazole.2,3 Currently,
ISSN: 0029-7844/17 there are no U.S. Food and Drug Administration
VOL. 0, NO. 0, MONTH 2017 OBSTETRICS & GYNECOLOGY 1
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
(FDA)–approved single-dose oral therapy options for assessments, patients self-administered treatments while
the treatment of bacterial vaginosis. at the clinic. Randomization was stratified by the
Secnidazole, a 5-nitroimidazole with a longer half- number of self-reported episodes of bacterial vaginosis,
life than metronidazole (approximately 17 compared including the current episode, in the past 12 months
with approximately 8 hours), has been used for the (three or fewer compared with four or more) as
treatment of bacterial vaginosis, trichomoniasis, and reported during the medical history. Patients were
other indications in Europe and Asia4 but is not avail- contacted by telephone once between days 8 and 10
able in the United States. A single dose of 2 g secni- to inquire about possible adverse events and persistence
dazole was compared with a standard 7-day regimen of symptoms. Patients completed a test of cure visit,
of metronidazole in a European study of women with comprising assessments pertaining to primary and
Nugent scores 7 or greater and found similar resolu- secondary efficacy endpoints and the safety endpoint
tion of bacterial vaginosis between the treatment between days 21 and 30 posttreatment. Patients were
groups.5 In vitro studies demonstrated antimicrobial free to withdraw at any time for any reason. Women
properties of secnidazole against most of the bacterial who requested alternative treatment at any time during
species implicated in bacterial vaginosis. Several pub- the study were offered standard of care bacterial
lished clinical studies have provided both clinical and vaginosis treatment at no cost. If a patient withdrew
microbiologic evidence of activity of secnidazole in before the test of cure visit, an end of study visit,
the treatment of bacterial vaginosis.5–7 Secnidazole, comprising a test of cure assessments, was performed at
like other 5-nitroimidazoles, has limited activity the time of withdrawal. This study was conducted in
against lactobacilli, the beneficial microbes important accordance with the ethical principles of Good Clinical
in establishing vaginal health after treatment. Practice.8
This three-arm, placebo-controlled, phase 2, Patients with a clinical diagnosis of bacterial
dose-ranging study of secnidazole for bacterial vagi- vaginosis were recruited from 24 ambulatory gyne-
nosis treatment was conducted in accordance with cology clinics in the United States, and by design, no
FDA guidance. The objective was to evaluate the single site contributed more than 16% to the study
clinical, microbiologic, and therapeutic efficacy and population. The study population included nonpreg-
safety of a single oral dose of 1 or 2 g secnidazole in nant women who were 18 years of age or older, in
women diagnosed with bacterial vaginosis, based on general good health, had agreed to abstain from
Amsel criteria and Nugent scores 4 or greater. sexual activity and use of intravaginal products for 1
week after treatment, and met the four Amsel criteria
MATERIALS AND METHODS for bacterial vaginosis (discharge; pH 4.7 or greater;
The study received institutional review board approval 20% or greater clue cells; positive whiff test). Women
(Schulman Associates institutional review board, were excluded if they were pregnant, bleeding at
Cincinnati, Ohio; Western institutional review board, baseline, were allergic to metronidazole, unable or
Puyallup and Olympia, Washington; Wayne State unwilling to abstain from alcohol for 3 days after
University Human Investigation Committee, Detroit, treatment, receiving concomitant antimicrobial ther-
Michigan). Patients provided written informed consent apy (topical or oral), or received a recent course
before any study procedures were performed. Patients (within previous 14 days) of antimicrobial or antifun-
determined to be eligible at baseline (day 1) were gal therapy. Baseline vaginal sample slides for Nugent
randomized one to one to one using a centralized scoring and laboratory tests confirming sexually
permuted block randomization process through the transmitted infections (STIs) were evaluated centrally;
data management center to one of the following: one thus, results were unavailable at the time of random-
sealed bottle of granules containing 1 or 2 g secnidazole ization. The study protocol prespecified that patients
or matching placebo granules. The sealed bottles determined to have Nugent scores less than 4 or who
contained the randomization assignment, which was tested positive for a STI after baseline assessment
generated by the study biostatistician before the start of were to be considered screening failures. These
the study. All ingredients of the granules were the same patients underwent an end of study visit and were
with the exception of the addition of a bittering agent to then discontinued from the study. Accordingly, these
the placebo granules to mimic the potential bitter taste patients received the randomized treatment and
of secnidazole granules. All treatment was administered remained in the study until Nugent scores and
orally as a single dose in approximately 4 ounces of baseline laboratory tests became available to the
applesauce under fasted conditions (ie, no food 2 hours investigator. Baseline Nugent scores ultimately were
before through 1 hour after dosing). After baseline used as a criterion for inclusion in the modified
2 Hillier et al Single-Dose Secnidazole for Treatment of BV OBSTETRICS & GYNECOLOGY
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
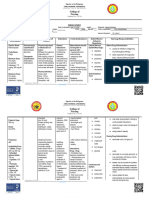
intent-to-treat population, the primary population for No interim analyses of efficacy were performed
efficacy analyses (Fig. 1). and sponsors and investigators remained blinded until
The primary efficacy endpoint was clinical cure, the database was locked. The efficacy analyses were
based on the 1998 FDA guidance regarding evalua- performed on the modified intent-to-treat population,
tion of treatment for bacterial vaginosis: 1) normal defined as all randomized patients who met all study
vaginal discharge, 2) negative 10% potassium hydrox- selection criteria. Clinical cure at the test of cure visit
ide whiff test, and 3) clue cells less than 20% of total was compared between each active secnidazole dose
epithelial cells on microscopic examination of the and placebo using a Cochran-Mantel-Haenszel statis-
vaginal wet mount using saline at the test of cure visit. tical test adjusted for stratification by bacterial vagi-
Secondary efficacy endpoints, also evaluated at this nosis recurrence. The primary comparison was
visit, were Nugent score, with a score of 0–3 consid- between 2 g secnidazole and placebo; comparison
ered Lactobacillus-dominant (ie, microbiologic cure) between 1 g secnidazole and placebo was a secondary
and a score of 4 or greater considered abnormal, analysis. The 2- and 1-g secnidazole doses were not
and therapeutic cure, defined as meeting the criteria compared statistically. Because there was only one
for both clinical and microbiologic cure. primary comparison, no adjustment for multiple
Safety evaluations were based on the incidence, comparisons was indicated. For each secnidazole dose,
intensity, and type of adverse events and changes in an exact 95% binomial confidence interval (CI) was
patients’ physical examination findings, vital signs, calculated for the clinical cure rate. All tests were
and clinical laboratory results, but the study was not performed at a .05 level of significance (two-sided).
statistically powered to detect differences in safety Secondary efficacy endpoints were analyzed similarly.
between groups. In a prespecified analysis, primary and secondary
Assuming a clinical cure rate of 40% in the active endpoints were also analyzed by bacterial vaginosis
groups and 15% in the placebo group, a sample size of strata and baseline Nugent score (4–6, 7–10). Patients
52 patients per group was expected to provide with any missing data required for assessment of pri-
approximately 80% power to detect a statistically mary and secondary efficacy endpoints at either the
significant difference between either secnidazole test of cure or end of study visit as a result of treatment
group and placebo at a .05 level of significance failure or early discontinuation were imputed as non-
(two-sided) using a Cochran-Mantel-Haenszel test. responders for clinical and therapeutic outcomes and
To ensure at least 52 patients met the modified as abnormal for Nugent score.
intent-to-treat criteria, between 71 and 72 patients Safety evaluations were based on the incidence,
were randomized to each treatment group for a total intensity, and type of treatment-emergent adverse
of 215 patients randomized. events and changes in the patient’s physical
Fig. 1. Patient disposition. STI, sexually transmitted infection.
Hillier. Single-Dose Secnidazole for Treatment of BV. Obstet Gynecol 2017.
VOL. 0, NO. 0, MONTH 2017 Hillier et al Single-Dose Secnidazole for Treatment of BV 3
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
examination findings, vital signs, and clinical safety identified as white. A higher proportion of white pa-
laboratory results. Safety variables were tabulated tients were enrolled in the 2-g secnidazole group (51.
and presented for all patients in the intent-to-treat 6%) compared with the 1-g and placebo groups (28.
population, because they all received the study drug. 1% and 38.7%, respectively), although these differen-
A treatment-emergent adverse event was defined as ces were not statistically significantly different. Other
any adverse event that occurred after administration demographics and baseline characteristics were simi-
of the study drug dose through the end of the study lar across the three treatment arms.
visit. Any event that was considered by the investiga- In the intent-to-treat population, the clinical cure
tor to be study drug–related, regardless of onset time, rate was 65.3% for the 2-g group, 49.3% for the 1-g
or any event that was present at baseline but worsened group, and 19.4% for the placebo group. However, as
in intensity or was subsequently was considered prespecified in the protocol, the modified intent-to-
treatment-related by the investigator. Investigators treat group was designated the primary analysis
were asked to report all adverse events, whether mild, population, because two different criteria for exclu-
moderate, or severe. Adverse events were recorded sion—baseline Nugent scores and results from baseline
verbatim and then coded using preferred Medical laboratory testing—were only available after the pa-
Dictionary for Regulatory Activities terminology. tients were randomized and treated. Clinical, micro-
biologic, and therapeutic cure rates are summarized
RESULTS for the modified intent-to-treat population in Table 2.
A total of 215 women were enrolled at 24 research Eight women were lost to follow-up during the course
centers in the United States between May 28 and of the study and, per the prespecified protocol, were
September 5, 2014. Reasons for exclusion included counted as nonresponders.
baseline STIs (n513 women), Nugent score less than The clinical cure rate was significantly higher for
4 (n514), and clinically significant baseline laboratory the 2-g (68%) and 1-g (52%) doses of secnidazole
abnormality that led to a diagnosis of chronic myeloid compared with placebo (18%) (P,.001 for both com-
leukemia (n51; Fig. 1), leaving 188 women in the parisons). A similar trend was observed with microbi-
modified intent-to-treat population with 62–64 ologic cure, which was 40% for the 2-g dose (P,.001
women per arm. The demographic and baseline char- compared with placebo) and 23% for the 1-g dose
acteristics of the study population are summarized in (P5.007 compared with placebo). As shown in
Table 1 and Appendix 1 (available online at http:// Table 2, the therapeutic cure rate was 40%, 22%,
links.lww.com/AOG/A973). The median age of the and 7% for the 2-g secnidazole, the 1-g, and the pla-
study population was 33 years (range 19–54 years); cebo groups, respectively. A greater treatment effect
more than half of the participants (54%) described was observed with 2 g secnidazole compared with
themselves as black or African American, and 39% placebo on analysis of clinical, microbiologic, and
Table 1. Demographics and Baseline Characteristics (Modified Intent-to-Treat Population) Overall and by
Treatment Group
Secnidazole 1 g Secnidazole 2 g Placebo Overall
Parameter (n564) (n562) (n562) (n5188)
Age (y) 34 (19, 49) 31 (19, 54) 33 (19, 49) 33 (19, 54)
Race
White 18 (28.1) 32 (51.6) 24 (38.7) 74 (39.4)
Black or African American 42 (65.6) 26 (41.9) 34 (54.8) 102 (54.3)
Asian 1 (1.6) 1 (1.6) 2 (3.2) 4 (2.1)
Native American or Alaska Native 1 (1.6) 1 (1.6) 0 2 (1.1)
Other 2 (3.1) 2 (3.2) 2 (3.2) 6 (3.2)
No. of BV episodes in past 12 mo 3 (1, 13) 2 (1, 12) 3 (1, 12) 3 (1, 13)
BV strata: no. of BV episodes in past 12
mo
3 or fewer 44 (68.8) 41 (66.1) 43 (69.4) 128 (68.1)
4 or more 20 (31.3) 21 (33.9) 19 (30.6) 60 (31.9)
Baseline Nugent score 9 (5, 10) 8 (4, 10) 8 (4, 10) 8 (4, 10)
BV, bacterial vaginosis.
Data are median (minimum, maximum) or n (%).
4 Hillier et al Single-Dose Secnidazole for Treatment of BV OBSTETRICS & GYNECOLOGY
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 2. Summary of Primary and Secondary Efficacy Results (Modified Intent-to-Treat Population) at Day
21–30 Visit by Treatment Group
Endpoint Secnidazole 1 g (n564) Secnidazole 2 g (n562) Placebo (n562)
Clinical cure
Primary endpoint* 33 (51.6) 42 (67.7) 11 (17.7)
95% exact binomial CI for responder rate 38.7–64.2 54.7–79.1 9.2–29.5
†
P ,.001 ,.001 —
Microbiologic cure
‡
Secondary endpoint 15 (23.4) 25 (40.3) 4 (6.5)
†
P .007 ,.001 —
Therapeutic cure
§
Secondary endpoint 14 (21.9) 25 (40.3) 4 (6.5)
†
P .011 ,.001 —
Data are n (%) unless otherwise specified.
* Clinical cure was defined as a patient who had all three of the following at days 21–30: normal vaginal discharge, negative potassium
hydroxide whiff test, and clue cells less than 20%.
†
P compared with placebo from a Cochran-Mantel-Haenszel test adjusted for bacterial vaginosis strata (fewer than three or more than three
episodes in the past 12 months).
‡
Microbiologic cure was defined as a Nugent score 0–3, based on centralized review, at days 21–30. Missing Nugent scores were classified
as abnormal.
§
Therapeutic cure was defined as both clinical and microbiologic cure.
therapeutic cure, regardless of the number of prior moderate in intensity. No serious adverse events were
episodes of bacterial vaginosis (three or fewer or four reported. No secnidazole dose relationship or differ-
or more in the past 12 months) in the modified intent- ences from placebo were observed in physical exam-
to-treat population. The study was not powered to ination, clinical laboratory, or vital sign parameters.
determine statistical differences in a three-way strati- Furthermore, no notable differences were observed in
fied comparison. However, with respect to the nomi- the mean, median, minimum, or maximum changes
nal a5.05 level of significance, all three outcomes from baseline in any laboratory parameter.
were favorable in the 2-g treatment arm in the sub-
population of patients with four or more episodes DISCUSSION
(P,.001 for all assessments) and for the clinical cure This study evaluated the efficacy and safety of two
assessment for the 1-g treatment arm (P5.023; doses of secnidazole. Both dose levels of secnidazole
Table 3). Analyses of the primary and secondary end- were superior to placebo, although the study was not
points in the per-protocol population (1-g group, powered to detect differences between the two treat-
n555; 2-g group, n547; placebo group, n550), which ment groups. This study had a balanced inclusion of
included patients in the modified intent-to-treat pop- women having recurrent bacterial vaginosis over the
ulation who had no major protocol violations, also three treatment arms. Although cure rates were lower
showed results similar to those in the modified overall among women having recurrent bacterial
intent-to-treat population (clinical cure: 1 g, 52.7%, vaginosis, the 2-g secnidazole treatment was statisti-
P,.001; 2 g, 72.3%, P,.001; placebo, 20%). cally superior to placebo, even among those women
The safety and tolerability of secnidazole admin- having recurrent infections. A strength of the study
istered in the 2- or 1-g granule form was evaluated in was the recruitment of women from across the United
all 215 randomized patients who were treated with States and substantial representation by African
a single dose of the study drug (Table 4). Treatment- American women.
emergent adverse events were reported in 19% (14/ Since this study was conducted, the FDA has
72), 13% (9/71), and 10% (7/72) in the 2-g secnida- issued new draft guidance regarding drug develop-
zole, 1-g secnidazole, and placebo groups, respec- ment for bacterial vaginosis. Interpreting the results of
tively. Infections were the most common events in this study requires an understanding of this context, in
all treatment groups, but were similar in incidence which the FDA recommends the inclusion of a con-
across the three treatment groups (Table 4). Vaginal current placebo arm as part of the design and that
yeast infections were infrequent, occurring in seven clinical cure being defined as the resolution of three
women, five of whom received secnidazole. All clinical signs (discharge, amine odor, clue cells) of
treatment-emergent adverse events were mild or bacterial vaginosis.9 Using this definition, cure rates
VOL. 0, NO. 0, MONTH 2017 Hillier et al Single-Dose Secnidazole for Treatment of BV 5
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 3. Summary of Primary and Secondary Efficacy Results (Modified Intent-to-Treat Population) at Day
21–30 Visit Stratified by Number of Episodes of Bacterial Vaginosis in the Past Year
Treatment Group
Secnidazole 1 g Secnidazole 2 g Placebo
3 or Fewer BV 4 or More BV 3 or Fewer BV 4 or More BV 3 or Fewer BV 4 or More BV
Episodes Episodes Episodes Episodes Episodes Episodes
Endpoint (n544) (n520) (n541) (n521) (n543) (n519)
Clinical cure
Primary endpoint* 26 (59.1) 7 (35.0) 30 (73.2) 12 (57.1) 10 (23.3) 1 (5.3)
95% exact 43.2–73.7 15.4–59.2 57.1–85.8 34.0–78.2 11.8–38.6 0.1–26.0
binomial CI for
responder rate
†
P ,.001 .023 ,.001 ,.001 — —
Microbiologic cure
Secondary 13 (29.5) 2 (10.0) 18 (43.9) 7 (33.3) 4 (9.3) 0
‡
endpoint
†
P .018 .162 ,.001 .006 — —
Therapeutic cure
Secondary 13 (29.5) 1 (5.0) 18 (43.9) 7 (33.3) 4 (9.3) 0
§
endpoint
†
P .018 .330 ,.001 .006 — —
BV, bacterial vaginosis.
Data are n (% cured) unless otherwise specified.
* Clinical cure was defined as a patient who had normal vaginal discharge, negative potassium hydroxide whiff test, and clue cells less than
20% at days 21–30.
†
P compared with placebo from a Cochran-Mantel-Haenszel test adjusted for BV strata (three or fewer or four or more episodes in the past
12 months).
‡
Microbiologic cure at days 21–30 was defined as a Nugent score 0–3, based on centralized review, at days 21–30. Missing Nugent scores
were classified as abnormal.
§
Therapeutic cure was defined as both clinical and microbiologic cure.
for oral 500 mg metronidazole twice daily for 7 days mens and similar or superior to the published data for
have been reported to be 58%5; the 7-day clindamycin single-dose clindamycin2 and metronidazole3 intrava-
cream treatment has provided a similar response.2 In ginal treatments. Treatment with a single dose of oral
a multicenter, placebo-controlled randomized trial of secnidazole yielded similar cure rates when compared
oral tinidazole given at either 2 g daily for 2 days or 1 with 7 days of oral metronidazole in a European
g for 5 days, resolution of bacterial vaginosis as study.5 A consistent trend across studies is the lower
defined by absence of three or more Amsel criteria microbiologic cure rate than the clinical rate, suggest-
was reported in 46% of women who received the 2- ing the presence of microbes persist after resolution of
day regimen and in 64% of those who received the 5- clinical symptoms, and lactobacilli species have not
day regimen.10 yet recovered to levels reflective of a healthy vaginal
Two single-dose intravaginal treatments have environment. An improved understanding of the tip-
been FDA-approved for treatment of bacterial vagi- ping point, the point at which the imbalance of vagi-
nosis. Single-dose clindamycin cream has been re- nal microbiota leads to signs and symptoms of
ported to provide clinical and microbiologic cure for bacterial vaginosis, is warranted to further understand
64% and 57% of women, respectively, although only whether differences in microbiologic cure affect risk
47% of enrolled women were evaluable in this study.2 of recurrence.
A single-dose 1.3% metronidazole gel has a reported Side effects of oral metronidazole include nausea,
clinical cure rate of 37% and a microbiologic cure of a metallic taste, headaches, and gastrointestinal dis-
18% at the 21-day visit.3 In the present study, the tress. In this study, the incidence of adverse events
single-dose oral treatment with secnidazole granules was low, with only 1 of 144 women randomized to
provided a clinical cure rate of 68% and a microbio- secnidazole having nausea and only one woman
logic cure rate of 40%, which appears to be similar to reporting a metallic taste. The low incidence of
the efficacy of the current CDC-recommended regi- adverse events is consistent with clinical experience
6 Hillier et al Single-Dose Secnidazole for Treatment of BV OBSTETRICS & GYNECOLOGY
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 4. Patient Incidence of Treatment-Emergent Adverse Events (Intent-to-Treat Population, N5215) by
Treatment Group
Adverse Events Secnidazole 1 g (n571) Secnidazole 2 g (n572) Placebo (n572)
Total no. of participants reporting 1 or more 9 (12.7) 14 (19.4) 7 (9.7)
treatment-emergent adverse event
Any treatment-emergent adverse events with
incidence 2% or greater
Infections
Yeast infections* 3 (4.2) 2 (2.8) 2 (2.8)
Upper respiratory tract infection 0 (0) 0 (0) 2 (2.8)
Treatment-related† treatment-emergent adverse
events 1% or greater
Yeast infection 0 (0) 2 (2.8) 1 (1.4)
Vulvovaginal pruritus 0 (0) 1 (1.4) 0 (0)
Chromaturia 0 (0) 1 (1.4) 0 (0)
Dysgeusia 0 (0) 1 (1.4) 0 (0)
Headache 1 (1.4) 0 (0) 0 (0)
Nausea 0 (0) 1 (1.4) 0 (0)
Alanine aminotransferase increased 0 (0) 1 (1.4) 0 (0)
Aspartate aminotransferase increased 0 (0) 1 (1.4) 0 (0)
Data are n (%).
* Investigators reported yeast infections using any of the following acceptable terms: vulvovaginal mycotic infection, Candida infection,
fungal infection, or vulvovaginal candidiasis.
†
Adverse events that were deemed by the investigator to be “possibly” or “probably” related to treatment. All treatment-related treatment-
emergent adverse events were considered mild to moderate.
with secnidazole as treatment outside the United comparing single-dose 2-g secnidazole oral granules
States where it is approved for treatment of parasitic with an active comparator such as metronidazole
diseases and bacterial vaginosis with a well- may be warranted to better understand how a single-
established safety profile.5–7,11,12 dose treatment may compare with a multidose
The 2015 CDC Sexually Transmitted Disease regimen.
Treatment Guidelines recommends treatment of bac-
terial vaginosis for all women having symptoms.1 REFERENCES
Although the primary objective of treatment is reso- 1. Workowski KA, Bolan GA; Centers for Disease Control and
lution of symptoms, other potential benefits of bacte- Prevention. Sexually transmitted diseases treatment guidelines,
rial vaginosis treatment include reduction in the risk 2015. MMWR Recomm Rep 2015;64:1–137.
for acquiring Chlamydia trachomatis, Neisseria gonor- 2. Faro S, Skokos CK; Clindesse Investigators Group. The effi-
cacy and safety of a single dose of Clindesse vaginal cream
rhoeae,13 Trichomonas vaginalis,14 human immunodefi- versus a seven-dose regimen of Cleocin vaginal cream in pa-
ciency virus,15 and herpes simplex type 2.16 Recent tients with bacterial vaginosis. Infect Dis Obstet Gynecol 2005;
studies have evaluated the effect of bacterial vaginosis 13:155–60.
treatment on acquisition of bacterial STIs with mixed 3. Schwebke JR, Marrazzo J, Beelen AP, Sobel JD. A phase 3,
results.17,18 Schwebke18 evaluated home screening for multicenter, randomized, double-blind, vehicle-controlled
study evaluating the safety and efficacy of metronidazole vagi-
bacterial vaginosis to identify and treat asymptomatic nal gel 1.3% in the treatment of bacterial vaginosis. Sex Transm
cases to reduce acquisition of chlamydial and gono- Dis 2015;42:376–81.
coccal infections, but found no difference in incident 4. Videau D, Niel G, Siboulet A, Catalan F. Secnidazole. A 5-
STIs. Results from a study of periodic presumptive nitroimidazole derivative with a long half-life. Br J Vener Dis
1978;54:77–80.
treatment of bacterial vaginosis and yeast vaginitis
5. Bohbot JM, Vicaut E, Fagnen D, Brauman M. Treatment of
demonstrated a reduced incidence of C trachomatis, bacterial vaginosis: a multicenter, double-blind, double-
N gonorrhoeae, and Mycoplasma genitalium.17 Additional dummy, randomised phase III study comparing secnidazole
research is needed to confirm the benefits of periodic and metronidazole. Infect Dis Obstet Gynecol 2010 [epub
ahead of print].
treatment of bacterial vaginosis as a strategy to reduce
6. Donders G. Diagnosis and management of bacterial vaginosis
incident STIs.
and other types of abnormal vaginal bacterial flora: a review.
Results from this study support the further Obstet Gynecol Surv 2010;65:462–73.
development of secnidazole for the treatment of 7. Núñez JT, Gómez G. Low-dose secnidazole in the treatment of
women with bacterial vaginosis. Additional studies bacterial vaginosis. Int J Gynaecol Obstet 2005;88:281–5.
VOL. 0, NO. 0, MONTH 2017 Hillier et al Single-Dose Secnidazole for Treatment of BV 7
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
8. World Medical Association. World Medical Association Decla- 13. Wiesenfeld HC, Hillier SL, Krohn MA, Landers DV, Sweet
ration of Helsinki: ethical principles for medical research RL. Bacterial vaginosis is a strong predictor of Neisseria gonor-
involving human subjects. JAMA 2013;310:2191–4. rhoeae and Chlamydia trachomatis infection. Clin Infect Dis
9. U.S. Department of Health and Human Services, Food and 2003;36:663–8.
Drug Administration, Center for Drug Evaluation and 14. Brotman RM. Vaginal microbiome and sexually transmitted infec-
Research (CDER). Bacterial vaginosis: developing drugs for tions: an epidemiologic perspective. J Clin Invest 2011;121:4610–7.
treatment. Guidance for industry. Silver Spring (MD): U.S.
Food and Drug Administration; 2016. 15. Atashili J, Poole C, Ndumbe PM, Adimora AA, Smith JS. Bac-
terial vaginosis and HIV acquisition: a meta-analysis of pub-
10. Livengood CH III, Ferris DG, Wiesenfeld HC, Hillier SL, lished studies. AIDS 2008;22:1493–501.
Soper DE, Nyirjesy P, et al. Effectiveness of two tinidazole
regimens in treatment of bacterial vaginosis: a randomized con- 16. Cherpes TL, Meyn LA, Krohn MA, Lurie JG, Hillier SL. Asso-
trolled trial. Obstet Gynecol 2007;110:302–9. ciation between acquisition of herpes simplex virus type 2 in
women and bacterial vaginosis. Clin Infect Dis 2003;37:319–25.
11. Gillis JC, Wiseman LR. Secnidazole. A review of its antimicro-
bial activity, pharmacokinetic properties and therapeutic use in 17. Balkus JE, Manhart LE, Lee J, Anzala O, Kimani J, Schwebke J,
the management of protozoal infections and bacterial vaginosis. et al. Periodic presumptive treatment for vaginal infections may
Drugs 1996;51:621–38. reduce the incidence of sexually transmitted bacterial infec-
tions. J Infect Dis 2016;213:1932–7.
12. Moraes ME, Cunha GH, Bezerra MM, Fechine FV, Pontes AV,
Andrade WS, et al. Efficacy of the Mentha crispa in the treat- 18. Schwebke JR, Lee JY, Lensing S, Philip SS, Wiesenfeld HC, Seña
ment of women with Trichomonas vaginalis infection. Arch Gy- AC, et al. Home screening for bacterial vaginosis to prevent sex-
necol Obstet 2012;286:125–30. ually transmitted diseases. Clin Infect Dis 2016;62:531–6.
8 Hillier et al Single-Dose Secnidazole for Treatment of BV OBSTETRICS & GYNECOLOGY
Copyright Ó by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
You might also like
- Comparison of Combined Probiotic and Antibiotic Therapy Versus Antibiotic Therapy Alone in Treatment of Bacterial VaginosisDocument4 pagesComparison of Combined Probiotic and Antibiotic Therapy Versus Antibiotic Therapy Alone in Treatment of Bacterial VaginosisHerdian KusumaNo ratings yet
- Giardia 2Document6 pagesGiardia 2Martha SánchezNo ratings yet
- Nejmoa 2104535Document12 pagesNejmoa 2104535niken maretasariNo ratings yet
- 33 - 4 - 07-Dr - KhademDocument5 pages33 - 4 - 07-Dr - Khademedy744No ratings yet
- polyhexamethyleneERMPS2008Document8 pagespolyhexamethyleneERMPS2008Bosko SimicNo ratings yet
- Probiotics For The Prevention of Pediatric Antibiotic-Associated DiarrheaDocument7 pagesProbiotics For The Prevention of Pediatric Antibiotic-Associated DiarrheaJUAN SEBASTIAN AVELLANEDA MARTINEZNo ratings yet
- Nejmoa 1811867Document13 pagesNejmoa 1811867yasserNo ratings yet
- Lactobacillus rhamnosus GG vs Placebo for Acute Gastroenteritis in ChildrenDocument21 pagesLactobacillus rhamnosus GG vs Placebo for Acute Gastroenteritis in ChildrenMarsella Epifania SuwignyoNo ratings yet
- A Randomized Controlled Trial of Ceftriaxone and Doxycycline, With or Without Metronidazole, For The Treatment of Acute Pelvic Inflammatory DiseaseDocument9 pagesA Randomized Controlled Trial of Ceftriaxone and Doxycycline, With or Without Metronidazole, For The Treatment of Acute Pelvic Inflammatory DiseaseobgynlaosNo ratings yet
- Oral Intake of Lactobacilli Can Be Helpful in Symptomatic Bacterial Vaginosis: A Randomized Clinical StudyDocument6 pagesOral Intake of Lactobacilli Can Be Helpful in Symptomatic Bacterial Vaginosis: A Randomized Clinical Studyrichir karlNo ratings yet
- Tinidazol Vs Metronidazol en VBDocument6 pagesTinidazol Vs Metronidazol en VBnautilus81No ratings yet
- Leitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseDocument7 pagesLeitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseEdgar SimmonsNo ratings yet
- Mebendazole Compared With Secnidazole in The Treatment of Adult GiardiasisDocument16 pagesMebendazole Compared With Secnidazole in The Treatment of Adult GiardiasisJanessa DalidigNo ratings yet
- Rifampicina TBMR NEJM 2019Document13 pagesRifampicina TBMR NEJM 2019carolinaNo ratings yet
- Nejmoa 1310480Document11 pagesNejmoa 1310480mz zumrodinNo ratings yet
- One in Five Patients Experience Rebound COVID After Taking Paxlovid, New Study Finds Mass General BrighamDocument1 pageOne in Five Patients Experience Rebound COVID After Taking Paxlovid, New Study Finds Mass General BrighamJan CundiffNo ratings yet
- Colistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM EvidenceDocument27 pagesColistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM Evidencerac.oncologyNo ratings yet
- Probiotics For The Prevention of Pediatric Antibiotic-Associated Diarrhea (Review)Document4 pagesProbiotics For The Prevention of Pediatric Antibiotic-Associated Diarrhea (Review)EvelynRuizNo ratings yet
- Synthesis Paper Final DraftDocument11 pagesSynthesis Paper Final Draftapi-332323350No ratings yet
- Colombo Et Al 2022 The Canova Study Real World Evidence of Biologic Treatments in Moderate Severe Psoriasis in Italy ADocument8 pagesColombo Et Al 2022 The Canova Study Real World Evidence of Biologic Treatments in Moderate Severe Psoriasis in Italy AvotuyetdongtrinhNo ratings yet
- Efficacy of A Single-Dose, Inactivated Oral Cholera Vaccine in BangladeshDocument10 pagesEfficacy of A Single-Dose, Inactivated Oral Cholera Vaccine in BangladeshLiseth LisethNo ratings yet
- Single-Dose Azithromycin Versus Penicillin G Benzathine For The Treatment of Early SyphilisDocument9 pagesSingle-Dose Azithromycin Versus Penicillin G Benzathine For The Treatment of Early SyphilisMomon ManiezNo ratings yet
- YgygyygDocument6 pagesYgygyygAnonymous dkEBxwVJONo ratings yet
- Efficacy and Safety of Gonorrhea TreatmentsDocument9 pagesEfficacy and Safety of Gonorrhea TreatmentsSamuelRexyNo ratings yet
- What Is The Role of Antiemetics For Children With Acute Gastroenteritis in The Developing World?Document4 pagesWhat Is The Role of Antiemetics For Children With Acute Gastroenteritis in The Developing World?Shafa AudryNo ratings yet
- Cancers 08 00084Document10 pagesCancers 08 00084Benny Chris TantoNo ratings yet
- Conclusions: Background:: Oral Abstracts / J Pediatr Adolesc Gynecol (2013) E47ee53 E49Document2 pagesConclusions: Background:: Oral Abstracts / J Pediatr Adolesc Gynecol (2013) E47ee53 E49fujimeisterNo ratings yet
- Bacterial Vaginosis Draft Evidence ReviewDocument206 pagesBacterial Vaginosis Draft Evidence Reviewaisa mutiaraNo ratings yet
- Cancer Controversies Clinical Trials Confirm But Don't Innovate-ConDocument3 pagesCancer Controversies Clinical Trials Confirm But Don't Innovate-ConadssaNo ratings yet
- Christine Tagliaferri Rael Doyel Das Jose Bauermeister Cody Lentz Alex Carballo Diéguez Rebecca Giguere Rachel K. Scott Craig W. HendrixDocument19 pagesChristine Tagliaferri Rael Doyel Das Jose Bauermeister Cody Lentz Alex Carballo Diéguez Rebecca Giguere Rachel K. Scott Craig W. HendrixMichael DeniNo ratings yet
- Taylor 2018Document11 pagesTaylor 2018YUYUMNo ratings yet
- Tele The Ruthr AbotuDocument5 pagesTele The Ruthr AbotukhanjanNo ratings yet
- Efficacy of Clinacanthus Nutans Extracts in PatientsDocument7 pagesEfficacy of Clinacanthus Nutans Extracts in Patientsconrad9richterNo ratings yet
- 21 Iajps21102017 PDFDocument9 pages21 Iajps21102017 PDFBaru Chandrasekhar RaoNo ratings yet
- Abul-Husn Et Al. - 2014 - Implementation and Utilization of Genetic Testing in Personalized Medicine PDFDocument14 pagesAbul-Husn Et Al. - 2014 - Implementation and Utilization of Genetic Testing in Personalized Medicine PDFflashjetNo ratings yet
- The Efficacy and Safety of Gentamicin Plus Azithromycin and Gemifloxacin Plus Azithromycin As Treatment of Uncomplicated GonorrheaDocument9 pagesThe Efficacy and Safety of Gentamicin Plus Azithromycin and Gemifloxacin Plus Azithromycin As Treatment of Uncomplicated GonorrheaCindy Julia AmandaNo ratings yet
- High-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisDocument10 pagesHigh-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisSoleh SundawaNo ratings yet
- Predicting Adherence To Antiretroviral Therapy Among Pregnant Women in Guyana: Utility of The Health Belief ModelDocument10 pagesPredicting Adherence To Antiretroviral Therapy Among Pregnant Women in Guyana: Utility of The Health Belief ModelRiska Resty WasitaNo ratings yet
- Multidrug-Resistant Tuberculosis and Culture Conversion With BedaquilineDocument10 pagesMultidrug-Resistant Tuberculosis and Culture Conversion With BedaquilinerennacahyadiNo ratings yet
- Ijerph 16 03859 v2 PDFDocument13 pagesIjerph 16 03859 v2 PDFIrwin FitriansyahNo ratings yet
- OAMJMS Full AtricleDocument4 pagesOAMJMS Full AtricleJoana MihaniNo ratings yet
- LSHTM Research Online: Usage GuidlinesDocument11 pagesLSHTM Research Online: Usage GuidlinesnomdeplumNo ratings yet
- MetronidazoleDocument6 pagesMetronidazolevenus healthklinik3No ratings yet
- T2DM Treatment Costs in MumbaiDocument2 pagesT2DM Treatment Costs in MumbaiRoxana SlujitoruNo ratings yet
- Cefpodoxime Vs Cefixime in LRTI, IndianJPediatrDocument5 pagesCefpodoxime Vs Cefixime in LRTI, IndianJPediatrAnonymous so6ZnlKyw100% (1)
- Short-Course Intraabdominal InfectionDocument10 pagesShort-Course Intraabdominal Infectionnicolás idárragaNo ratings yet
- Diarr 20Document4 pagesDiarr 20Pablo Pinaya SotomayorNo ratings yet
- A Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in AdultsDocument4 pagesA Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in Adults林新中No ratings yet
- Heczko2015 Article SupplementationOfStandardAntibDocument12 pagesHeczko2015 Article SupplementationOfStandardAntibeva yustianaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofprabuNo ratings yet
- Treatment for Preventing Tuberculosis in Children and AdolescentsDocument18 pagesTreatment for Preventing Tuberculosis in Children and AdolescentsPrillye DeasyNo ratings yet
- A Blinded, Randomized Controlled Trial of High-Dose Vitamin D Supplementation To Reduce Recurrence of Bacterial VaginosisDocument13 pagesA Blinded, Randomized Controlled Trial of High-Dose Vitamin D Supplementation To Reduce Recurrence of Bacterial VaginosisAlex Chungandro VillacrésNo ratings yet
- Nejmoa1911998 PDFDocument11 pagesNejmoa1911998 PDFStella NoviaNo ratings yet
- Anidula VS FluconDocument11 pagesAnidula VS FluconHarsha KuriNo ratings yet
- Jo Howard Long TermDocument11 pagesJo Howard Long TermKuliah Semester 4No ratings yet
- Literature Review 1Document10 pagesLiterature Review 1Rithik ModiNo ratings yet
- Use of Complementary and Alternative Medicines During The Third TrimesterDocument8 pagesUse of Complementary and Alternative Medicines During The Third Trimesteraisyalfi pratimiNo ratings yet
- BongDocument1 pageBongRod Reynon BorceNo ratings yet
- Complementary Therapies in Medicine: Contents Lists Available atDocument13 pagesComplementary Therapies in Medicine: Contents Lists Available atAndi UmmahNo ratings yet
- Optimizing Advanced Therapies in Ulcerative Colitis: Is Your Practice Up to Date? A Focus on Clinical Evidence and Guideline RecommendationsFrom EverandOptimizing Advanced Therapies in Ulcerative Colitis: Is Your Practice Up to Date? A Focus on Clinical Evidence and Guideline RecommendationsNo ratings yet
- Management of Inverted Papilloma Review PDFDocument6 pagesManagement of Inverted Papilloma Review PDFsiska tiaraNo ratings yet
- Diphtheria An Emerging Disease PDFDocument3 pagesDiphtheria An Emerging Disease PDFsiska tiaraNo ratings yet
- Crossm: Prognostic Indicators of Recurrence of Bacterial VaginosisDocument9 pagesCrossm: Prognostic Indicators of Recurrence of Bacterial Vaginosissiska tiaraNo ratings yet
- Endoscopic Management of Maxillary Sinus Inverted Papilloma Atachment Sites To Minimize Disease Recurrance PDFDocument5 pagesEndoscopic Management of Maxillary Sinus Inverted Papilloma Atachment Sites To Minimize Disease Recurrance PDFsiska tiaraNo ratings yet
- A Rare Presentation of A Paediatric Sinonasal Inverted PapillomaDocument3 pagesA Rare Presentation of A Paediatric Sinonasal Inverted Papillomasiska tiaraNo ratings yet
- Ajo 01 29Document4 pagesAjo 01 29aulianaNo ratings yet
- Letter To The Editors: The Outbreak of Diphtheria in IndonesiaDocument5 pagesLetter To The Editors: The Outbreak of Diphtheria in IndonesiaHellena Hildegard TambunanNo ratings yet
- Vaginosis BakterialisDocument7 pagesVaginosis Bakterialisdoktermudaobgyn februariaprilNo ratings yet
- Imaging Modalities For The Classi Fication of Gout: Systematic Literature Review and Meta-AnalysisDocument8 pagesImaging Modalities For The Classi Fication of Gout: Systematic Literature Review and Meta-Analysissiska tiaraNo ratings yet
- Prolonged Labor Incidences: Passage-Passenger Factors Analyzed (Descriptive Study in RSUD Dr. Koesma Tuban)Document5 pagesProlonged Labor Incidences: Passage-Passenger Factors Analyzed (Descriptive Study in RSUD Dr. Koesma Tuban)siska tiaraNo ratings yet
- Clinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled AnalysisDocument29 pagesClinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled Analysissiska tiaraNo ratings yet
- A Meta-Analysis of The Association of Estimated GFR, AlbuminuriaDocument19 pagesA Meta-Analysis of The Association of Estimated GFR, Albuminuriasiska tiaraNo ratings yet
- Management of Disease and Disorders by Prebiotics and Probiotic Therapy: Probiotics in Bacterial VaginosisDocument9 pagesManagement of Disease and Disorders by Prebiotics and Probiotic Therapy: Probiotics in Bacterial Vaginosissiska tiaraNo ratings yet
- Management of Disease and Disorders by Prebiotics and Probiotic Therapy: Probiotics in Bacterial VaginosisDocument9 pagesManagement of Disease and Disorders by Prebiotics and Probiotic Therapy: Probiotics in Bacterial Vaginosissiska tiaraNo ratings yet
- HypertiroidDocument9 pagesHypertiroidsiska tiaraNo ratings yet
- Tematica Ex Specialitate Ocupare Post Obstetrica GinecologieDocument4 pagesTematica Ex Specialitate Ocupare Post Obstetrica GinecologieAncuta Raluca TiperciucNo ratings yet
- Hep ViralDocument14 pagesHep Viralsiska tiaraNo ratings yet
- Clinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled AnalysisDocument29 pagesClinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled Analysissiska tiaraNo ratings yet
- Anemia Def Besi PDFDocument10 pagesAnemia Def Besi PDFsiska tiaraNo ratings yet
- Hep ViralDocument14 pagesHep Viralsiska tiaraNo ratings yet
- Clinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled AnalysisDocument29 pagesClinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled Analysissiska tiaraNo ratings yet
- Imaging Modalities For The Classi Fication of Gout: Systematic Literature Review and Meta-AnalysisDocument8 pagesImaging Modalities For The Classi Fication of Gout: Systematic Literature Review and Meta-Analysissiska tiaraNo ratings yet
- Original Investigation A Meta-Analysis of The Association of Estimated GFR, Albuminuria, Age, Race, and Sex With Acute Kidney InjuryDocument11 pagesOriginal Investigation A Meta-Analysis of The Association of Estimated GFR, Albuminuria, Age, Race, and Sex With Acute Kidney Injurysiska tiaraNo ratings yet
- JurnalDocument12 pagesJurnalIrara RaNo ratings yet
- Wms GINA 2018 Strategy Report V1.1 PDFDocument161 pagesWms GINA 2018 Strategy Report V1.1 PDFEdson ArmandoNo ratings yet
- Brunham2010-Cholesterol in Β-cell Dysfunction the Emerging Connection Between HDL Cholesterol and Type 2 DiabetesDocument6 pagesBrunham2010-Cholesterol in Β-cell Dysfunction the Emerging Connection Between HDL Cholesterol and Type 2 Diabetessiska tiaraNo ratings yet
- Aki PDFDocument11 pagesAki PDFsiska tiaraNo ratings yet
- Pemeriksaan THTDocument3 pagesPemeriksaan THTsiska tiaraNo ratings yet
- 602 1126 1 SMDocument5 pages602 1126 1 SMbeatriceNo ratings yet
- Metronidazole PoDocument5 pagesMetronidazole PoFlower Flower FlowerNo ratings yet
- Pigeon Racing PigeonDocument7 pagesPigeon Racing Pigeonsundarhicet83No ratings yet
- Basic and Essential PharmacologyDocument75 pagesBasic and Essential PharmacologyIorjiim WaltersNo ratings yet
- AntimicrobialDocument211 pagesAntimicrobialSanaz Niksefat100% (1)
- Vaginitis: Diagnosis and TreatmentDocument9 pagesVaginitis: Diagnosis and TreatmentAbigail MargarethaNo ratings yet
- Emergency Antibiotic Guide A6 105 1048mm February9 2022Document48 pagesEmergency Antibiotic Guide A6 105 1048mm February9 2022Iain HarrisonNo ratings yet
- Causes, Symptoms and Treatments of VaginitisDocument16 pagesCauses, Symptoms and Treatments of VaginitisMae Christelle Hamoy100% (2)
- CDS Andreas KalckerDocument36 pagesCDS Andreas KalckerevimaggNo ratings yet
- Amoxil 3Document9 pagesAmoxil 3sisnaingaungNo ratings yet
- Cefu, Metro, KetoDocument4 pagesCefu, Metro, KetoSethlyn_Gomez_5337No ratings yet
- Odontogenic Infections: Ickman Setoaji W, DRG., MMDocument66 pagesOdontogenic Infections: Ickman Setoaji W, DRG., MMAmeliza Putri AlindNo ratings yet
- Pharma Past PaperDocument11 pagesPharma Past PaperMasood MughalNo ratings yet
- Treatment of Giardiasis: Linical Icrobiology EviewsDocument15 pagesTreatment of Giardiasis: Linical Icrobiology EviewscherrypickerNo ratings yet
- Case Plan On Diarrhoea (Medical Surgical Nursing)Document15 pagesCase Plan On Diarrhoea (Medical Surgical Nursing)kamini ChoudharyNo ratings yet
- Pregabalin for pain and seizuresDocument6 pagesPregabalin for pain and seizuresMa R DyNo ratings yet
- Drug Study (m9)Document5 pagesDrug Study (m9)Angelie CuencoNo ratings yet
- Handbook of Surgical Care For House OfficersDocument20 pagesHandbook of Surgical Care For House OfficersCharity AtsuNo ratings yet
- Nitazoxanide: 842 AntiprotozoalsDocument2 pagesNitazoxanide: 842 Antiprotozoalszavate_ciprianNo ratings yet
- Fistulas Enterocutaneas MaingotDocument20 pagesFistulas Enterocutaneas MaingotroyvillafrancaNo ratings yet
- Anti-Infective Therapy "Antibiotics": Definitions Chemotherapeutic Agent Anti-Microbial AgentDocument8 pagesAnti-Infective Therapy "Antibiotics": Definitions Chemotherapeutic Agent Anti-Microbial AgentMohamed EbrahimNo ratings yet
- Dental RoshetttaDocument29 pagesDental RoshetttaKORMAX LEAGUENo ratings yet
- TRICHOMONIASISDocument39 pagesTRICHOMONIASISAlunaficha Melody KiraniaNo ratings yet
- Early Source Control Key to Reducing MortalityDocument65 pagesEarly Source Control Key to Reducing MortalityKamran SherazNo ratings yet
- Bagong DrugsDocument7 pagesBagong DrugsmcensoredNo ratings yet
- Drug StudyDocument7 pagesDrug Studykakienz100% (7)
- Anti-Protozoal Agents: Medicinal Chemistry-IIIDocument21 pagesAnti-Protozoal Agents: Medicinal Chemistry-IIIHimanshu Barman100% (1)
- Obat - BMDocument50 pagesObat - BMNovita PermataNo ratings yet
- What Is Bacterial Vaginosis and What Are The Symptoms?Document3 pagesWhat Is Bacterial Vaginosis and What Are The Symptoms?Mymy SofiNo ratings yet
- Microbial Infection TypesDocument14 pagesMicrobial Infection TypesMay Chelle ErazoNo ratings yet
- CPG Management of Genital Ulcers and DischargesDocument103 pagesCPG Management of Genital Ulcers and DischargesardhianiNo ratings yet