Professional Documents
Culture Documents
Journal Pone 0225479
Uploaded by
khairaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal Pone 0225479
Uploaded by
khairaniCopyright:
Available Formats
RESEARCH ARTICLE
The majority of skin lesions in pediatric
primary care attention could be managed by
Teledermatology
Mara Giavina Bianchi ID*, Andre Pires Santos, Eduardo Cordioli
Department of Telemedicine, Hospital Israelita Albert Einstein, São Paulo, Brazil
* marahgbianchi@gmail.com
Abstract
a1111111111
a1111111111 Background
a1111111111
Teledermatology is a tool that provides accurate diagnosis and has been gaining more
a1111111111
a1111111111 emphasis over time. It can be used for triage in primary care attention to address skin condi-
tions improving access and reducing time to treatment for surgical, severe or even lethal
diseases.
OPEN ACCESS Objectives
Citation: Giavina Bianchi M, Santos AP, Cordioli E Our main goal was to evaluate the proportion of pediatric patient’s lesions that could be
(2019) The majority of skin lesions in pediatric managed using teledermatology in primary care attention. Secondly, we wanted to assess
primary care attention could be managed by
the ten most frequent skin conditions, the most common treatments and the referrals made
Teledermatology. PLoS ONE 14(12): e0225479.
https://doi.org/10.1371/journal.pone.0225479 by the teledermatologists to biopsy, in-presence dermatologist or kept at primary care
attention.
Editor: Mauro Picardo, San Gallicano Dermatologic
Institute, ITALY
Received: May 20, 2019 Methods
Accepted: November 5, 2019 A cross-sectional retrospective study involving 6,879 individuals and 10,126 lesions was
conducted by store-and-forward teledermatology during one year in the city of Sao Paulo,
Published: December 2, 2019
Brazil. If the photographs taken had enough quality, teledermatologist would diagnose, treat
Copyright: © 2019 Giavina Bianchi et al. This is an
and orient each lesion (if possible), and choose one of three options for referral: direct to
open access article distributed under the terms of
the Creative Commons Attribution License, which biopsy, in-presence dermatologist or kept at primary care attention.
permits unrestricted use, distribution, and
reproduction in any medium, provided the original
Results
author and source are credited.
Teledermatology managed 62% of the lesions to be kept at primary care attention, 37%
Data Availability Statement: All relevant data are
within the manuscript and its Supporting were referred to dermatologists and 1% to biopsy, reducing the mean waiting time for an in-
Information files. presence visit in 78%. In patients 0–2 years old, lesions related to eczema and benign con-
Funding: The authors received no specific funding genital lesions predominated. From 3–12 years old, eczema was still a major cause of com-
for this work. plaint, as well as warts and molluscum. From 13–19 years old, acne was the most
Competing interests: The authors have declared significant problem, followed by atopic dermatitis, nevi and warts. The most frequent treat-
that no competing interests exist. ment was emollient.
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 1 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Conclusion
Teletriage addressed 63% of the lesions without the need for an in-presence visit, suggest-
ing that teledermatology can manage common diseases and optimize dermatological
appointments for the most serious, surgical or complex skin illnesses, reducing the mean
waiting time for them.
Introduction
Teledermatology (TD) is a healthcare tool that has been more and more used around the
world, mostly because Dermatology has an emphasis on visual diagnosis. Real-time (RT) or
store-and-forward (SF) are the most common types of delivering images. In SF-TD, the data
and images from a patient are collected and sent to a dermatologist analysis at a later time. In
RT-TD, patients and physicians communicate data and images from separate locations in a
live format [1]. Many studies have shown to improve access to specialized care using store-
and-forward TD, which provides accurate diagnosis and reduces time to treatment, with high
patient satisfaction [2].
Typical skin conditions such as mild atopic dermatitis, acne, fungal infections and others
are common diseases that would be manageable within the primary care attention service.
However, it is not what often happens because the professionals are not well trained to diag-
nose or triage skin diseases. The lack of primary care professional medical specialization can
lead to refer individuals to dermatologists unnecessarily. If there is a shortage of dermatolo-
gists, this creates a situation where appointments are filled by patients who do not need special
care, which can limit the availability of visits for those who do [3].
The city of Sao Paulo has nearly 12 million inhabitants [4], and 58% of them depend exclu-
sively on the public health care system [5]. The instances of public health in Brazil are munici-
pal, state and federal. Public municipal health care is in charge of most primary care attention.
There is a high demand for a public dermatological consultation in the city of Sao Paulo. By
July 2017, 57,832 individuals were waiting for it, which could take up to one year to occur. For
this reason, the municipal health department has decided to implement a project of Teleder-
matology, in conjunction with Hospital Israelita Albert Einstein, a large private hospital in the
city. The project rationale was: if the general doctor could manage some not so complex dis-
eases with the teledermatologist support, more dermatological appointments would be avail-
able, shortening the waiting time for those patients who do need in-presence dermatological
care.
It also is critical for public health to know the prevalence and management of the most
common diseases presented at primary care attention, so policies can address or even prevent
them. Our research had the primary objective to determine the proportion of pediatric
patient’s lesions that could be managed at primary care attention through teledermatology,
avoiding in-presence visits with dermatologists and, secondly, we assessed the frequency, treat-
ment and referrals of the most common skin lesions in children and adolescents assisted in
this project. Both goals were achieved in this study.
Patients and methods
This study was approved by Hospital Israelita Albert Einstein and Municipal Ethics Commit-
tees (CAAE:97126618.6.3001.0086) and it is in accordance with the ethical standards on
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 2 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
human experimentation and with the Declaration of Helsinki. Data was fully anonymized
before accessed and the IRB waived the requirement for the informed consent. It was a cross-
sectional retrospective cohort conducted in the city of Sao Paulo, where 14,925 individuals up
to 19 years old had been waiting for an appointment with a dermatologist in July 2017. The
municipal health government, in conjunction with Hospital Israelita Albert Einstein, devel-
oped a platform and an app for mobile device to be used by health technicians to take photo-
graphs with the its digital camera and upload them along with a short clinical history and
patient data. All data were collected and uploaded into a platform accessed only by dermatolo-
gists recruited for this project using a secured online process. Patients in the waiting list were
phoned by the public health care service and scheduled to go to an appointment in one of
three public city hospitals enabled to carry out the project. From July 2017-July 2018, thirteen
dermatologists worked in the triage of the patients and they had first to decide if the photo-
graphs taken of the lesions were satisfactory for diagnostic purposes. If not, they would choose
the box "bad photo" in the platform and referred the patient to a face-to-face appointment
with a dermatologist. If the photo had a good quality, they should formulate the most probable
diagnostic hypothesis and choose among three referral options for each lesion assessed: 1)
directly to biopsy (and after that patient would return to a dermatologist appointment with the
result), 2) to a dermatologist visit or 3) back to the pediatrician in primary care attention with
the most probable diagnosis and treatment and/or orientation how to proceed with the investi-
gation or management of the lesion. If the same patient had more than one lesion with differ-
ent referrals, a biopsy referral would prevail over dermatologist referral, that would prevail
over back to pediatrician referral. All patients who attended the project were included in this
study. For better analyze this population, we divided it into 0–2 years old, 3–12 years old and
13–19 years old. Only dermatologists certified by the Brazilian Board of Dermatology partici-
pated in the project in order to decrease the chance of diagnostic error by teledermatology. In
our Municipal Basic Health Unit, the direct exam to search for fungal infection is not done.
For this reason, suspicious cases of superficial fungal infections receive anti-fungal treatment
as therapeutic test and are reevaluated afterwards. If deep fungal infections were suspected,
then t the teledermatologist would refer the patient to Biopsy/Dermatologist and not treat
him/her before the confirmation of the pathogen. All statistical calculations were done using
two-tail Chi-square with Yates’ correction test by Graph Prism 6.0 software.
Results
1) Patients and lesions
From 14,925 patients between 0–19 years old waiting for dermatologist consultation in the city
of Sao Paulo, 6,879 individuals participated in this project (46%) and 6,588 referrals were
made. Table 1 shows patients demographic data. There were more female than male individu-
als waiting for a consultation with a dermatologist in all ages studied. As the age increased, the
presence rate increased from 37% at 0–2 years old to 47% at other ages. Patients referred to a
dermatologist because of the poor quality of photographs totalized 1.4% and a small part of the
patient data went missing due to technical problems (0.4%).
The total number of lesions photographed was 10,658 and 10,126 diagnostics were made.
The mean number of lesions photographed per person was 1.6 (Table 1).
Bleeding was present in only 16% of the lesions, but pruritus was relatively common: 45–
55% depending on age, being more frequent in lesions from individuals 3–12 years old.
Lesions referred to a dermatologist because of the poor quality of photographs totalized 0.9%
and missing data due to technical problems was 0.5%.
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 3 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Table 1. Number of lesions photographed and individuals from 0 to 19 years old waiting for a dermatologist consultation and those who participated in the Tele-
dermatology project, according to age and sex, from July 2017-July 2018, in the city of São Paulo.
0–2 years old(n) 3–12 years old(n) 13–19 years old(n) Total(n)
Patients Female Male Female Male Female Male
Waiting 643 722 3674 3062 4169 2645 14925
Participating 239 271 1723 1419 1952 1275 6879
% of participation 37 38 47 46 47 48 46
Lesions photographed 327 370 2503 2103 3346 2009 10658
Lesions photographed per person 1.4 1.4 1.5 1.5 1.7 1.6 1.6
Poor quality photograph 3 2 25 22 27 14 93
Missing data 20 16 73 74 58 50 291
https://doi.org/10.1371/journal.pone.0225479.t001
2) Referrals and most frequent diseases
Considering patients, referrals back to their primary care pediatrician occurred in 54%, to the
in-presence dermatologist in 45% and directly to biopsy in 1%. If lesions are analyzed, referrals
back to their primary care pediatrician were 62%, to the in-presence dermatologist 37% and
directly to biopsy 1%. (Fig 1). The use of Teledermatology reduced the mean waiting time for
in-presence dermatologist visit from 6.7 to 1.5 months during the time of the project (78%
reduction).
The most common causes of consultation for male and female individuals up to 19 years
old is shown in Fig 2. Diseases frequency varied along the ages. Among patients 0–2 years old,
the most common ICD-10 code for lesions was atopic dermatitis (AD) for both sexes. Boys
were more affected than girls, but with no statistically difference. Other complaints associated
frequently with AD, pityriasis alba and xerosis were also very frequent, summing 37%. Another
frequent cause of consultation was benign tumors, such as hemangiomas, congenital nevus
and hamartomas (verrucous nevus, sebaceous nevus, café-au-lait macule and spilus nevi)
which together with acquired melanocytic nevus, accounted for nearly 20% of the cases. Hem-
angiomas were statistically more frequent in girls than in boys (p = 0.0002). Infectious causes
as molluscum contagiosum and impetigo totalized around 5–6% and seborrheic dermatitis
complete the top ten ICD-10 codes with 3% of the lesions.
From 3–12 years old, AD maintained the first position on the list, as the conditions related:
pityriasis alba, xerosis and keratosis pilaris, summing up to 40%. Congenital malformations no
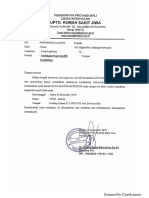
Fig 1. Distribution of the lesions and the patients 0–19 years old who participated in the Teledermatology Project referred to biopsy, dermatologist and back to
pediatrician according to age and sex, from July 2017-July 2018, in the city of São Paulo.
https://doi.org/10.1371/journal.pone.0225479.g001
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 4 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Fig 2. Most frequent diseases in patients 0–19 years old who participated in the Teledermatology Project according to age and sex, from July 2017-July 2018, in
the city of São Paulo.
https://doi.org/10.1371/journal.pone.0225479.g002
longer represented a complaint in that age. Only acquired melanocytic nevus was among the
top complaints, with 3%. Infectious viral diseases, such as molluscum and wart, showed a great
increased (15%) and impetigo continued to be the 10th most common cause of visits, around
2%. Seborrheic dermatitis still accounted for 3% and pigmentation disorders such as vitiligo
and post-inflammatory hyperpigmentation start to appear as frequent causes of consultation,
around 5%.
For individuals 13 to 19 years old, acne is the greatest complaint, with almost 30%. AD
decreases to second place, with 6%. Pityriasis alba and xerosis also decreased by around half,
but, together with keratosis pilaris remain at the top ten causes. Nevi and seborrheic dermatitis
maintained almost the same percentage and molluscum disappeared from the ten most fre-
quent complaints. Warts, in the other hand, kept its place, although less frequent. Post-inflam-
matory hyperpigmentation is on a rise in that period, and fungal infection, such as Tinea
Versicolor, starts to be a frequent motive of consultation (3–4%).
The most frequent lesions referred to biopsy, dermatologist and back to the primary care
pediatrician is shown in Fig 3. Biopsy was chosen in only 1% of all cases. Benign tumors were
the most frequent cause: melanocytic nevus, benign neoplasm such as soft fibroma, acrochor-
don, pyogenic granuloma, epidermoid cyst and congenital melanocytic nevi totalized 27 cases.
However, it was indicated in only a small percentage (around 3% or less). The only situation
where a suspect of a benign lesion had more referrals to biopsy was a pyogenic granuloma
with 21%. For malignant tumors, such as melanoma, the second most frequent lesion biopsied,
it was indicated every time (100%). Wart was also rarely biopsied (0.6%). Lichen nitidus was
the third most common disease to be biopsied, with 4 cases in 25% of the times.
Referrals for dermatologist occurred in 37% of the lesions. Acne and AD were frequent
causes, but only in 35% and 28%, respectively. Infectious diseases that often need in-presence
treatment, such as warts and molluscum, were sent to dermatologists in almost 90% of the
times. Benign lesions such as melanocytic nevus and epidermoid cyst were sent to the specialist
in 52% and 34% of the cases. Vitiligo, alopecia areata and psoriasis were common diseases
referred to a dermatologist (74%, 69% and 64% respectively).
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 5 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Fig 3. Most frequent lesions sent to biopsy, dermatologists and back to pediatrician in patients 0–19 years old who participated in the Teledermatology Project
according to age and sex, from July 2017-July 2018, in the city of São Paulo.
https://doi.org/10.1371/journal.pone.0225479.g003
Teledermatologists sent the patients back to their pediatricians in 62% of the all cases. For
lesions of acne and AD, around 70% of the times, and >85% for Pityriasis alba, xerosis, sebor-
rheic dermatitis, hyperpigmentation post-inflammatory hyperpigmentation, Tinea Versicolor
and impetigo. The most significant exception was melanocytic nevus, with only 44% of the
referrals back to their doctors.
3) Treatment
We also searched for the most frequent treatments prescribed by teledermatolgists (Fig 4). All
products in the top ten list were topical. Emollients were the most frequent prescription in
32% of all cases. Topical corticosteroids combined summed 29%, topical antifungal 12%, topi-
cal anti-acne 11%, sunscreen 9% and topical antibiotics 4%.
Discussion
In our view, the presence of 47% of the individuals called for this project was reasonable. TD is
still very new in our country, both for patients and physicians, and a pioneer project like this,
involving a significant number of people was a challenge. Our TD work had the benefits of a
large cohort and virtually any type of skin disease covered. Most of the TD articles focus on
one disease (melanoma) or a class of diseases (malignant tumors) [6–8]. In this way, we did
find our study very interesting and innovative.
Most of the lesions did not bleed, but pruritus was frequent, in nearly 50% of the cases. The
vast majority of the lesions photographed in our project did not require an in-presence visit
with the dermatologist (63%). This proves that most skin conditions in our primary care set-
ting is of low complexity and, therefore, can be properly addressed in primary care. This find-
ing reinforces the feasibility and the importance of Teledermatology in this context, helping
the pediatricians to manage such conditions and optimizing medical hours and costs, espe-
cially in the public system. The mean waiting time for an in-presence visit with the dermatolo-
gist was reduced 78% during the project (from 6.7 to 1.5 months). Our teledermatology
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 6 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Fig 4. List of most frequent prescriptions made by teledermatologists for patients 0–19 years old who participated in the Teledermatology Project from July
2017-July 2018, in the city of São Paulo.
https://doi.org/10.1371/journal.pone.0225479.g004
project proved to be a well-defined, structured, scalable process with standardized collection
and fairness of care, which might promote the democratization of access to dermatology for
underprivileged patients. Another study with 850 consultations showed that in 50% of the
patients no referral to an in-person dermatologist was needed [3]. Avoiding face-to-face con-
sultations with dermatologists in cases of frequent and manageable diseases by teledermatol-
ogy can optimize access to more severe, surgical or complex illnesses, which do require the
presence of a dermatologist. One important limitation of our work is the chance of error and
bias in teledermatology diagnosis, although many articles have attested a high agreement rate
between teledermatology and in-presence dermatology [6–9].
Most of the referrals for biopsy were benign lesions, but only in a small fraction of them (1–
25% depending on the suspected diagnosis), but 100% all suspects of malignant lesions went
for biopsy. Prevalent diseases, such as acne and atopic dermatitis, do not need biopsy confir-
mation to be managed. In typical lesions, this procedure might also has been avoided because
of the difficulty inherent for the age: younger patients may have to undergo sedation or general
anesthesia, which carry risks, and children, most of the times, do not collaborate in the proce-
dure, turning it into a stressful situation for the them and their relatives.
Referrals to dermatologists were made mostly for treatment of infectious diseases such as
warts and molluscum and for conditions that require follow up, such as vitiligo, psoriasis and
alopecia areata. Probably, most of the cases of acne and atopic dermatitis referred to dermatol-
ogists were moderate to severe, since the vast majority of the cases of those two diseases was
sent back to the pediatrician after being addressed. Benign neoplasms such as nevus and cyst
were also referred to the dermatologist, mostly because it is advisable to look at all nevi with
dermoscopy (that was not available in our project). If we had included it in the project, the
rates of referral would be much smaller [10]. For cysts, dermatologists are trained to palpate
such lesions, so teledermatology might feel insufficient in some cases.
Teletriage diagnosis for children 0–12 years old was mostly associated with atopic dermati-
tis and commonly associated skin disorders, such as pityriasis alba and xerosis (32%). Other
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 7 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
causes were benign lesions such as melanocytic nevus and congenital malformations (heman-
giomas, verrucous nevus, sebaceous nevus, café-au-lait macules) and infectious diseases such
as warts and molluscum. Once patients enter adolescence, acne was the primary cause of com-
plaint (28%), along with AD, melanocytic nevi, post-inflammatory hyperpigmentation and
warts. When we compare our data to other prevalence studies, atopic dermatitis was around
20% in children up to 12 years old and 6% of adolescents as other studies have shown [11,12].
Pityriasis alba is also very common, in our study ranging from 4–10% of all lesions photo-
graphed, compatible with another study that showed 4–7% of the school students in Turkey
[13]. This same study found that nevi are one of the most frequent dermatosis, around 60–
70% [13]. Melanocytic nevi were the primary cause for the teleconsultation in 4–7% of the
individuals up to 19 years old in our project. Another teletriage study showed nevi as 14% of
their cause for consultation [14]. Hemangiomas are a common tumor of the infancy, and its
prevalence is said to be likely around 5%, according to one study [15]. Our project has shown
that hemangiomas were 13% of the complaints in girls and 5% in boys between 0–2 years,
which was statistically significant (p = 0.002), in a proportion of almost 3:1, which in accor-
dance to the literature [16].
Cross-sectional study completed in schools has shown warts to have a prevalence between 2
and 20% in children [17]. We have encountered around 6–8% in children 3–12 years old and
3–5% from 13–19 years old. Molluscum contagiosum meta-analysis suggests a point preva-
lence in children aged 0–16 years of 5–11% [18]. In our study, it was 3% and 8% of the cases in
children from 0–2 and 3–12 years old, respectively. Although the true prevalence of post-
inflammatory hyperpigmentation is not known, it is widespread among Fitzpatrick types
IV-VI, but not so much among Caucasian patients [19]. Our data showed 2–5% of the com-
plaints in children from 3–19 years old. Several extensive studies have reported a prevalence of
adolescent acne ranging from 81 to 95% in young men and 79 to 82% in young women [20].
Our project found acne to be around 30% of the causes to have the teleconsultations. Around
6% of the school students presented xerosis in one study [13] and 7%, 5% and 3% of the chil-
dren between 0–2, 3–12 and 13–19 years old in our research.
Regarding treatment, a list of which drugs were available to the population studied is found
in S1 Table. All physicians involved were encouraged to use as much as possible only medica-
tions from such list, once they are free for patients and, most of them are unable to buy them
otherwise. The results show the importance of emollients in skin conditions, prescribed in 1/3
of the times. Along with other studies that support this, we could suggest that pediatricians
prescribe them routinely for most of the patients, as treatment and prevention of common
skin diseases, such as AD, and xerosis [21,22]. Low potency corticosteroids were the second
most prescribed medication, but moderate and high potency corticosteroids also played an
important rule being in the top ten list. Ketoconazole cream or shampoo for superficial fungi
infections and seborrheic dermatitis was very frequently recommended, as benzoyl peroxide
for acne. Sunscreen is essential in Brazil, especially for post inflammatory hyperpigmentation
in our dark skin population. Drugs containing antibiotics were also in the top ten list, mostly
for secondary infected lesions or impetigo.
There are limitations for Teletriage in Dermatology. The fact that you can receive multiples
photographs of parts of the body and head, and not to examine the body as a whole, makes the
diagnosis more challenging. Also, some important impressions that would help to corroborate
the diagnosis, such as feeling the texture of the skin or proceeding easy tests (p.e. vitrocom-
pression) cannot be done. However, we have shown that the impossibility to palpate the lesion
is not a main issue to the teledermatologists, who became much more confident in Telederma-
tology after working with TD [10].
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 8 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
The patients included in this project were referred to dermatologists by their pediatricians
and if they were not referred to a face-to-face dermatologist by the Teletriage project, the
patients went back to their pediatricians, who received information, recommendations and
management for that disorder. Therefore, there was not a moment when the patient was not
supervised by a physician and we believe that this fact gave us more confidence that potentially
severe, life-threatening or rare diseases were not being overlooked. Also, if any other concern
was raised, there was always the possibility of referring the patient to the dermatologist again.
Sometimes, besides the written concern that moved the pediatrician to refer the patient, while
taking photographs, the parents could spontaneously ask the health technician to include
some other lesions(s), which occurred sometimes, and the teledermatologists would address
those complaints too.
Conclusions
Teledermatology managed 63% of the lesions without the need for an in-presence appoint-
ment with the dermatologist, keeping 62% of them with their own primary care physician and
referring 1% directly to biopsy. Only 37% of the lesions were referred to dermatologists, opti-
mizing consultations for the most serious, surgical or complex skin illnesses, which do require
the presence of a dermatologist. Its use reduced the mean waiting time for these later patients
from 6.7 months to 1.5 during the time of the project (78% reduction). Teledermatology does
not aim to replace face-to-face visit with the dermatologist, but it has been proving to be an
efficient tool for triage and management of less complex dermatosis together with the primary
care pediatrician.
The frequency of skin diseases differed according to age. From 0–2 years old, lesions related
to eczema predominated along with benign congenital lesions. From 3–12 years old, eczema
was still a major cause of complaint, as well as warts and molluscum. From 13–19 years old,
acne was the most significant problem, followed by AD, nevi and warts. The most prescribed
product was emollient in 1/3 of the cases.
Supporting information
S1 Table. List of most common disease included into the disease groups.
(DOCX)
Acknowledgments
The authors would like to thank Raquel Machado de Sousa for her research assistance.
Author Contributions
Conceptualization: Mara Giavina Bianchi, Eduardo Cordioli.
Data curation: Mara Giavina Bianchi, Andre Pires Santos.
Investigation: Mara Giavina Bianchi.
Methodology: Mara Giavina Bianchi, Andre Pires Santos.
Project administration: Andre Pires Santos, Eduardo Cordioli.
Resources: Eduardo Cordioli.
Software: Andre Pires Santos.
Supervision: Eduardo Cordioli.
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 9 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
Validation: Eduardo Cordioli.
Writing – original draft: Mara Giavina Bianchi.
Writing – review & editing: Mara Giavina Bianchi, Andre Pires Santos, Eduardo Cordioli.
References
1. Heffner VA, Lyon VB, Brousseau DC, Holland KE, Yen K. Store-and-forward teledermatology versus in-
person visits: a comparison in pediatric teledermatology clinic. J Am Acad Dermatol. 2009; 60(6):956–
61. https://doi.org/10.1016/j.jaad.2008.11.026 PMID: 19362751
2. O’Connor DM, Jew OS, Perman MJ, Castelo-Soccio LA, Winston FK, McMahon PJ. Diagnostic Accu-
racy of Pediatric Teledermatology Using Parent-Submitted Photographs: A Randomized Clinical Trial.
JAMA Dermatol. 2017; 153(12):1243–8. https://doi.org/10.1001/jamadermatol.2017.4280 PMID:
29141082
3. Ranjani P, Carla B, Toni M. Teledermatology initiative to increase access for community helath center
patients. new england journal of medicine catalyst [Internet]. 2019. Available from: https://catalyst.nejm.
org/teledermatology-access-community-health/.
4. IBGE [Internet]. PANORAMA SÃO PAULO [cited 2019 Sept 07]. Available from: https://cidades.ibge.
gov.br/brasil/sp/sao-paulo/panorama
5. IPEA 2016 [Internet]. Rede Brasil Atual [cited 2019 Sept 07]. Available from: https://www.
redebrasilatual.com.br/saude/2016/10/no-estado-de-sao-paulo-25-milhoes-de-pacientes-dependem-
do-sus-1016.html
6. Kroemer S, Frühauf J, Campbell TM, Massone C, Schwantzer G, Soyer HP, et al. Mobile teledermatol-
ogy for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation
using cellular phones. Br J Dermatol. 2011; 164(5):973–9. https://doi.org/10.1111/j.1365-2133.2011.
10208.x PMID: 21219286
7. Ferrándiz L, Ruiz-de-Casas A, Martin-Gutierrez FJ, Peral-Rubio F, Mendez-Abad C, Rios-Martin JJ,
et al. Effect of teledermatology on the prognosis of patients with cutaneous melanoma. Arch Dermatol.
2012; 148(9):1025–8. https://doi.org/10.1001/archdermatol.2012.778 PMID: 22986852
8. Bruce AF, Mallow JA, Theeke LA. The use of teledermoscopy in the accurate identification of cancerous
skin lesions in the adult population: A systematic review. J Telemed Telecare. 2018; 24(2):75–83.
https://doi.org/10.1177/1357633X16686770 PMID: 28056600
9. Pak H, Triplett CA, Lindquist JH, Grambow SC, Whited JD. Store-and-forward teledermatology results
in similar clinical outcomes to conventional clinic-based care. J Telemed Telecare. 2007; 13(1):26–30.
https://doi.org/10.1258/135763307779701185 PMID: 17288655
10. Giavina Bianchi M, Santos A, Cordioli E. Dermatologists’ perceptions on the utility and limitations of tele-
dermatology after examining 55,000 lesions. J Telemed Telecare. 2019:1357633X19864829.
11. Spergel JM. Epidemiology of atopic dermatitis and atopic march in children. Immunol Allergy Clin North
Am. 2010; 30(3):269–80. https://doi.org/10.1016/j.iac.2010.06.003 PMID: 20670812
12. Laughter D, Istvan JA, Tofte SJ, Hanifin JM. The prevalence of atopic dermatitis in Oregon schoolchil-
dren. J Am Acad Dermatol. 2000; 43(4):649–55. https://doi.org/10.1067/mjd.2000.107773 PMID:
11004621
13. Uludağ A, Kılıc SO, Isık S, Haydar Ertekin Y, Tekin M, Cevizci S, et al. Prevalence of skin disorders in
primary and secondary school age children in Canakkale, Turkey: a community-based survey. Postepy
Dermatol Alergol. 2016; 33(3):176–81. https://doi.org/10.5114/ada.2016.60610 PMID: 27512351
14. Chen TS, Goldyne ME, Mathes EF, Frieden IJ, Gilliam AE. Pediatric teledermatology: observations
based on 429 consults. J Am Acad Dermatol. 2010; 62(1):61–6. https://doi.org/10.1016/j.jaad.2009.05.
039 PMID: 19926163
15. Kilcline C, Frieden IJ. Infantile hemangiomas: how common are they? A systematic review of the medi-
cal literature. Pediatr Dermatol. 2008; 25(2):168–73. https://doi.org/10.1111/j.1525-1470.2008.00626.x
PMID: 18429772
16. Seiffert A, Schneider M, Roessler J, Larisch K, Pfeiffer D. Incidence, Treatment Patterns, and Health
Care Costs of Infantile Hemangioma: Results of a Retrospective German Database Analysis. Pediatr
Dermatol. 2017; 34(4):450–7. https://doi.org/10.1111/pde.13187 PMID: 28675551
17. Kilkenny M, Marks R. The descriptive epidemiology of warts in the community. Australas J Dermatol.
1996; 37(2):80–6. https://doi.org/10.1111/j.1440-0960.1996.tb01010.x PMID: 8687332
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 10 / 11
The majority of skin lesions in pediatric primary care attention could be managed by Teledermatology
18. Olsen JR, Gallacher J, Piguet V, Francis NA. Epidemiology of molluscum contagiosum in children: a
systematic review. Fam Pract. 2014; 31(2):130–6. https://doi.org/10.1093/fampra/cmt075 PMID:
24297468
19. Kaufman BP, Aman T, Alexis AF. Postinflammatory Hyperpigmentation: Epidemiology, Clinical Presen-
tation, Pathogenesis and Treatment. Am J Clin Dermatol. 2018; 19(4):489–503. https://doi.org/10.
1007/s40257-017-0333-6 PMID: 29222629
20. Skroza N, Tolino E, Mambrin A, Zuber S, Balduzzi V, Marchesiello A, et al. Adult Acne Versus Adoles-
cent Acne: A Retrospective Study of 1,167 Patients. J Clin Aesthet Dermatol. 2018; 11(1):21–5. PMID:
29410726
21. Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-
based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children:
part II. J Eur Acad Dermatol Venereol. 2018; 32(6):850–78. https://doi.org/10.1111/jdv.14888 PMID:
29878606
22. Simpson EL, Chalmers JR, Hanifin JM, Thomas KS, Cork MJ, McLean WH, et al. Emollient enhance-
ment of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol.
2014; 134(4):818–23. https://doi.org/10.1016/j.jaci.2014.08.005 PMID: 25282563
PLOS ONE | https://doi.org/10.1371/journal.pone.0225479 December 2, 2019 11 / 11
You might also like
- Fast Facts: Dermatological Nursing: A practical guide on career pathwaysFrom EverandFast Facts: Dermatological Nursing: A practical guide on career pathwaysNo ratings yet
- Engelman2016 - Volume 32, Issue 11, November 2016, Pages 843-854Document12 pagesEngelman2016 - Volume 32, Issue 11, November 2016, Pages 843-854Choi KhoironNo ratings yet
- TeledermatologiDocument17 pagesTeledermatologiShifa Ainun AzzahraNo ratings yet
- Feasibility and Cost of A Telemedicine-Based Short-Term Plan For Initial Access in General Dermatology in Andalusia, SpainDocument6 pagesFeasibility and Cost of A Telemedicine-Based Short-Term Plan For Initial Access in General Dermatology in Andalusia, SpainBryan NguyenNo ratings yet
- Preprints202206 0384 v1Document12 pagesPreprints202206 0384 v1rakeshsinghpariharNo ratings yet
- The Public Health Control of SDocument13 pagesThe Public Health Control of SYosia KevinNo ratings yet
- The Potential Role of Artificial Intelligence in The Clinical Management of Hansen's Disease (Leprosy)Document7 pagesThe Potential Role of Artificial Intelligence in The Clinical Management of Hansen's Disease (Leprosy)mloureiro17No ratings yet
- Tele 2Document10 pagesTele 2Sajin AlexanderNo ratings yet
- TeleHealth Final ManuscriptDocument127 pagesTeleHealth Final ManuscriptMaxine JeanNo ratings yet
- 005 HCNAchap 5Document88 pages005 HCNAchap 5celine ziadeNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- 2014 Dermatological EmergenciesDocument7 pages2014 Dermatological EmergenciesSejal ThakkarNo ratings yet
- Teledermatology For COVID-19Document8 pagesTeledermatology For COVID-19eva yustianaNo ratings yet
- An Update On The Diagnosis and Treatment of LeprosyDocument10 pagesAn Update On The Diagnosis and Treatment of LeprosyChlarissa WahabNo ratings yet
- Paper 8661Document2 pagesPaper 8661IJARSCT JournalNo ratings yet
- JCDR 10 WC06Document3 pagesJCDR 10 WC06كنNo ratings yet
- Battineni, Gopi (2021)Document12 pagesBattineni, Gopi (2021)Mateus MartinsNo ratings yet
- TelemedicineDocument9 pagesTelemedicineAna CaballeroNo ratings yet
- Gajadi 5. Rapid Implementation of Teledentistry During The Covid-19 LockdownDocument5 pagesGajadi 5. Rapid Implementation of Teledentistry During The Covid-19 LockdownIndah VitasariNo ratings yet
- The Importance of Epidemiology in Optometry: Oriahi, M. ODocument4 pagesThe Importance of Epidemiology in Optometry: Oriahi, M. OSumon SarkarNo ratings yet
- Dermatologia Cães e Gatos Cmpa 1Document12 pagesDermatologia Cães e Gatos Cmpa 1Lilian S F BlumerNo ratings yet
- Teledermatology: Concepts and Applications in MedicineDocument6 pagesTeledermatology: Concepts and Applications in MedicineJesse AguirreNo ratings yet
- Ijerph 18 08941Document21 pagesIjerph 18 08941Martinus CiputraNo ratings yet
- Scabies Application of The No PDFDocument10 pagesScabies Application of The No PDFYosia KevinNo ratings yet
- Dermatitis Ingles PDFDocument12 pagesDermatitis Ingles PDFMelissa KatherineNo ratings yet
- Campbell Etal IntWoundJ 2014Document9 pagesCampbell Etal IntWoundJ 2014SDNo ratings yet
- Skin Disease Detection Using Machine LearningDocument6 pagesSkin Disease Detection Using Machine LearningIJRASETPublicationsNo ratings yet
- Connectionpersonal Hygieneand Occupations With Dermatitis IncidenceDocument7 pagesConnectionpersonal Hygieneand Occupations With Dermatitis IncidenceajiNo ratings yet
- Regional Merting AbbelDocument5 pagesRegional Merting AbbelABBEL AULIANo ratings yet
- Scabies: Application of The Novel Identify-Isolate-Inform Tool For Detection and ManagementDocument8 pagesScabies: Application of The Novel Identify-Isolate-Inform Tool For Detection and Managementraudhatul muttaqinNo ratings yet
- Behavioral Considerations and Impact On Personal Protective Equipment Use: Early Lessons From The Coronavirus (COVID-19) PandemicDocument2 pagesBehavioral Considerations and Impact On Personal Protective Equipment Use: Early Lessons From The Coronavirus (COVID-19) PandemicKalpanaNo ratings yet
- 2014 LeprosyDocument5 pages2014 LeprosySejal ThakkarNo ratings yet
- 388-Article Text-1059-1-10-20200112Document3 pages388-Article Text-1059-1-10-20200112Nurhaliza AnjliNo ratings yet
- IV - Guidelines For The Management of AD Consensus Statement of PDSDocument24 pagesIV - Guidelines For The Management of AD Consensus Statement of PDSPJ Sandoval BiscarraNo ratings yet
- Accelerating Telemedicine For Cerebral Palsy During The COVID-19 Pandemic and BeyondDocument7 pagesAccelerating Telemedicine For Cerebral Palsy During The COVID-19 Pandemic and BeyondDjNo ratings yet
- Artikel 3Document6 pagesArtikel 3sesiaNo ratings yet
- The Role of Mobile Teledermoscopy in Skin Cancer Triage and Management During The COVID-19 PandemicDocument6 pagesThe Role of Mobile Teledermoscopy in Skin Cancer Triage and Management During The COVID-19 PandemicSherein DiabNo ratings yet
- BMC Infectious Diseases: How To Optimize Tuberculosis Case Finding: Explorations For Indonesia With A Health System ModelDocument10 pagesBMC Infectious Diseases: How To Optimize Tuberculosis Case Finding: Explorations For Indonesia With A Health System ModelEva Tirtabayu HasriNo ratings yet
- Treatment Challenges in Atopic DermatitisDocument25 pagesTreatment Challenges in Atopic DermatitisWirawan AdikusumaNo ratings yet
- (Evaluation) Filtered Sunlight PTDocument5 pages(Evaluation) Filtered Sunlight PTErwin SmithNo ratings yet
- Adiutarini 7Document9 pagesAdiutarini 7Eva Tirtabayu HasriNo ratings yet
- Telemedicine For Healthcare CapabilitiesDocument12 pagesTelemedicine For Healthcare CapabilitiesSandiNo ratings yet
- Dermaology CareDocument2 pagesDermaology CareSankita SandalNo ratings yet
- Incl Cert BunDocument15 pagesIncl Cert Bunalex nanuNo ratings yet
- Diagnosis and Management of Atopic Dermatitis For Primary Care ProvidersDocument10 pagesDiagnosis and Management of Atopic Dermatitis For Primary Care ProvidersMira GNo ratings yet
- Skin Disease Classification Using Hybrid ApproachDocument4 pagesSkin Disease Classification Using Hybrid ApproachInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Teleorthodontics in Covid Era Continuing Treatment Through Remote MonitoringDocument3 pagesTeleorthodontics in Covid Era Continuing Treatment Through Remote MonitoringInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- J Pak Assoc Dermatol 2013 23 3 295 299Document5 pagesJ Pak Assoc Dermatol 2013 23 3 295 299Latifah Amalia ZatiNo ratings yet
- Recent Advances in The Diagnosis of DermatophytosisDocument11 pagesRecent Advances in The Diagnosis of DermatophytosishansmeetNo ratings yet
- Wa0027.Document6 pagesWa0027.CHAMBI MAMANI JESSICA BETTYNo ratings yet
- The Future of Healthcare During and After COVID 19 1596642902Document4 pagesThe Future of Healthcare During and After COVID 19 1596642902Iin TammasseNo ratings yet
- 2023 Tort Et Al. Experiences of TelenursingDocument13 pages2023 Tort Et Al. Experiences of TelenursingchiuasaNo ratings yet
- 132595-Article Text-357320-1-10-20160323Document4 pages132595-Article Text-357320-1-10-20160323Mojahid HamidNo ratings yet
- Tropicalmed 03 00082Document7 pagesTropicalmed 03 00082Andi HardiantyNo ratings yet
- Strategies Adapted For Patient-Oriented Care and Satisfaction During TheDocument7 pagesStrategies Adapted For Patient-Oriented Care and Satisfaction During TheRagni MishraNo ratings yet
- JCM 10 00797Document11 pagesJCM 10 00797alazarNo ratings yet
- Update On The Treatment of Molluscum Contagiosum in ChildrenDocument9 pagesUpdate On The Treatment of Molluscum Contagiosum in Childrensamsara vrindaNo ratings yet
- Telemedicine, Telenursing, Journalism, Mass MediaDocument79 pagesTelemedicine, Telenursing, Journalism, Mass MediaMatei Sailo SailoNo ratings yet
- Journal PNTD 0009246Document19 pagesJournal PNTD 0009246delvisaid16No ratings yet
- Risk Factors For Physical Disability Upon Release FromDocument9 pagesRisk Factors For Physical Disability Upon Release FromRODOLFO JOSÉ DE OLIVEIRA MOREIRANo ratings yet
- Case-Control Study of The Risk Factors For Age Related Macular DegenerationDocument7 pagesCase-Control Study of The Risk Factors For Age Related Macular DegenerationkhairaniNo ratings yet
- JR HM 2Document3 pagesJR HM 2khairaniNo ratings yet
- Skripsi Tanpa Bab Pembahasan PDFDocument76 pagesSkripsi Tanpa Bab Pembahasan PDFkhairaniNo ratings yet
- Dok Baru 2019-12-03 10.01.25 PDFDocument2 pagesDok Baru 2019-12-03 10.01.25 PDFkhairaniNo ratings yet
- Ocular Involvement of Coronavirus Disease (COVID-19) : A Systematic Review of Conjunctival Swab ResultsDocument5 pagesOcular Involvement of Coronavirus Disease (COVID-19) : A Systematic Review of Conjunctival Swab ResultskhairaniNo ratings yet
- Catatan Psikiatri Dea PDFDocument76 pagesCatatan Psikiatri Dea PDFkhairaniNo ratings yet
- Latent Fingerprint On Human Skin: A Silent Diagnosis: Sci Criminol 7 (2) : 205Document4 pagesLatent Fingerprint On Human Skin: A Silent Diagnosis: Sci Criminol 7 (2) : 205khairaniNo ratings yet
- Conjunctivitis Can Be The Only Presenting Sign and PDFDocument7 pagesConjunctivitis Can Be The Only Presenting Sign and PDFkhairaniNo ratings yet
- Anesthetics and AnesthesiologyDocument5 pagesAnesthetics and AnesthesiologykhairaniNo ratings yet
- Cerebro Spinal Fluid and The Meninges: Dr. Setyawati Asih Putri, SPS, M.Kes, FinaDocument30 pagesCerebro Spinal Fluid and The Meninges: Dr. Setyawati Asih Putri, SPS, M.Kes, FinakhairaniNo ratings yet
- Falling Stroke Rates During COVID-19 Pandemic at A Comprehensive Stroke Center: Cover Title: Falling Stroke Rates During COVID-19Document8 pagesFalling Stroke Rates During COVID-19 Pandemic at A Comprehensive Stroke Center: Cover Title: Falling Stroke Rates During COVID-19khairaniNo ratings yet
- Journal of Clinical Neuroscience: Imran Ahmad, Farooq Azam RathoreDocument5 pagesJournal of Clinical Neuroscience: Imran Ahmad, Farooq Azam RathorekhairaniNo ratings yet
- 10.1136@bjophthalmol 2019 315280 PDFDocument5 pages10.1136@bjophthalmol 2019 315280 PDFkhairaniNo ratings yet
- Clinical Review: Common Skin Infections in ChildrenDocument5 pagesClinical Review: Common Skin Infections in ChildrenkhairaniNo ratings yet
- 3 Jurnal EnglishDocument7 pages3 Jurnal EnglishkhairaniNo ratings yet
- Surgical Treatment of Severe Osteoporosis Includin-DikonversiDocument6 pagesSurgical Treatment of Severe Osteoporosis Includin-DikonversikhairaniNo ratings yet
- GeriatricDermatoses PDFDocument15 pagesGeriatricDermatoses PDFkhairaniNo ratings yet
- GeriatricDermatoses 3 PDFDocument1 pageGeriatricDermatoses 3 PDFkhairaniNo ratings yet
- Courier: A Thousand WordsDocument20 pagesCourier: A Thousand WordsAnonymous 9eadjPSJNgNo ratings yet
- Global Clinical Engieering 15-31-PB VOL 4 N3-2022Document57 pagesGlobal Clinical Engieering 15-31-PB VOL 4 N3-2022John Jairo CárdenasNo ratings yet
- Thesis SynopsisDocument17 pagesThesis SynopsisOmar FarookNo ratings yet
- Of The Secretary: OfficeDocument59 pagesOf The Secretary: OfficeJoanna MarieNo ratings yet
- ACGME Program RequirementsDocument39 pagesACGME Program RequirementsTopher JentoftNo ratings yet
- Aromatherapy: and Occupational TherapyDocument5 pagesAromatherapy: and Occupational TherapyelenastaseNo ratings yet
- Effective Exercises For A Short FrenumDocument2 pagesEffective Exercises For A Short FrenumlblessingerNo ratings yet
- Principles of Endodontic Diagnosis - 2020Document9 pagesPrinciples of Endodontic Diagnosis - 2020Ina BogdanNo ratings yet
- Challenges To Implementation of The Pharmaceutical Care Practice in Davao City.Document11 pagesChallenges To Implementation of The Pharmaceutical Care Practice in Davao City.JessieLynMolinaNo ratings yet
- Degree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentDocument24 pagesDegree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentRJ DealcaNo ratings yet
- Factitious Disorder PaperDocument9 pagesFactitious Disorder Paperapi-116302187100% (1)
- IbandronateDocument2 pagesIbandronatePratik R JobaliaNo ratings yet
- Book Review: Available Online atDocument3 pagesBook Review: Available Online atFransiska DewiNo ratings yet
- 130300-Standards For Acute and Critical Care NursingDocument12 pages130300-Standards For Acute and Critical Care Nursingapi-315277523No ratings yet
- What Works in Therapy?Document12 pagesWhat Works in Therapy?Ariel PollakNo ratings yet
- Textbook of Medical Parasitology Protozoology HelmDocument2 pagesTextbook of Medical Parasitology Protozoology HelmramyadevidurairajNo ratings yet
- Day 2Document9 pagesDay 2Anil SoniNo ratings yet
- ThnkupoDocument3 pagesThnkupoJessica Anne SapnoNo ratings yet
- SJAIT Broj 4 CeoDocument155 pagesSJAIT Broj 4 CeoNatalija StamenkovicNo ratings yet
- Operating Room Surgical ProceduresDocument197 pagesOperating Room Surgical ProceduresChin Chan100% (6)
- COPARDocument5 pagesCOPARErica Keil MoleNo ratings yet
- Future Challenges and Objectives For Pda in Asiapac: Connecting People, Science and RegulationDocument11 pagesFuture Challenges and Objectives For Pda in Asiapac: Connecting People, Science and RegulationhuykhiemNo ratings yet
- NSTP Module 4Document35 pagesNSTP Module 4Lannie GarinNo ratings yet
- Question Bank: Paper 3 - Organisation of Hospital ServicesDocument5 pagesQuestion Bank: Paper 3 - Organisation of Hospital ServicesDr. Rakshit SolankiNo ratings yet
- LAB Owners Haryana RajsthanDocument27 pagesLAB Owners Haryana RajsthanOFC accountNo ratings yet
- DAFTAR PUSTAKA SiapDocument3 pagesDAFTAR PUSTAKA SiapRatria Andika PutraNo ratings yet
- KADS6 SpanishDocument4 pagesKADS6 SpanishKemish MartinezNo ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- Dr. Umashankar R: 22 Years Experience Overall (19 Years As Specialist)Document10 pagesDr. Umashankar R: 22 Years Experience Overall (19 Years As Specialist)Venkatesha SNo ratings yet
- 2012 Children Flu DrillDocument1 page2012 Children Flu DrillNewzjunkyNo ratings yet