Professional Documents
Culture Documents
Postoperative Management of Complications PART 1
Uploaded by
Isabel CastilloOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postoperative Management of Complications PART 1
Uploaded by
Isabel CastilloCopyright:
Available Formats
Gynecology EXIMIUS
Postoperative Management of Complications PART 1 2021
Corazon W. Adviento, MD March 2020
POSTOPERATIVE PERIOD § Physical examination à lungs, wound, costovertebral
§ Time fromSept-2019
the end of the procedure in the operating room angle, superficial veins and deep veins in the legs
until a woman has resumed her normal routine and § Laboratory evaluation à CBC c PC, UA, CXR
lifestyle § Others : culture, GS, UTZ, CT
§ GOAL § Microatelectasis
§ Restore a woman’s physiologic and psychological § 90% of fevers in the 1st 48 hours of operation
health Drug- induced fever
§ eosinophilia
Risk factors for surgical patients § does not look as ill as the temp course
§ Underlying cardiac and pulmonary disease § Diagnosis of exclusion
§ Smoking § Ex: allopurinol, carbamazepine, lamotrigine, phenytoin,
§ Obesity sulfasalazine, vancomycin, minocycline, dapsone,
§ Prior or recurrent surgery sulfamethoxazole
§ Type of anesthesia § Elderly and HIV patients à inc risk
§ Age ??? Superficial thrombophlebitis
§ Enigmatic fever
POSTOP FEVER § Tenderness on IV site
§ Febrile morbidity § Removal of IV catheter
§ Temp of >38C 24 hours after surgery
§ Incidence: 14-16% à post hysterectomy FALLING HEMOGLOBIN
§ Most common morbidity § Dec urine output à earliest sign of dec in intravascular
§ Causes: volume
§ Atelectesis § Minimum UO à 0.5 mL/kg/hr
§ Pneumonia § Dec in orthostatic BP >10 mmHg à dec in 20% of blood
§ UTI volume
§ Nonseptic phlebitis § Determination of Hgb
§ Wound infection § Done 24 hours and 48-72 hours postop
§ Operative site infection § Normal physiologic response to stress of operation and
§ Operative time >2 hours tissue destruction
§ Necessity for intraop transfusion § Increase levels of aldosterone, cortisol and ADH
§ increase blood loss § Increase in sodium and water retention
§ 20% infectious (Aldostererone)
§ 80% noninfectious § Promote free water retention (ADH)
§ Treat or not to treat § <7g/dL à BT done
§ Broad spectrum antibiotics à for high risk patients or for § 7-8 g/dL à BT done if cardiovascular disease is present
those with fever >48 hours § 8-10 g/dL
§ Pathophysiology
§ Release of cytokines RESPIRATORY COMPLICATIONS
§ Atelectasis
§ Pneumonia
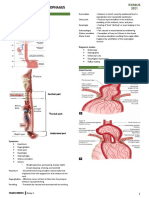
ATELECTASIS
§ Form two Greek words that mean “imperfect expansion”
§ Ranges from small group of bronchioles and alveoli to
complete lung collapse
§ Failure to maintain patency of small pulmonary airways
and alveoli
§ Most common cause of postop fever
§ Postop à dec in functional residual capacity and lung
WORK UP FOR FEVER compliance
§ 5 Ws
§ Wind à atelectasis
§ Water à UTI
§ Wound à infection or hematoma
§ Walk à superficial or deep vein phlebitis
§ Wonder drugs à drug – induced fever
§ Microatelectasis à atelectasis = 1st 72 hours postop
§ Dec in O2 saturation
§ Dec in Po2
§ Normal – low Pco2
§ History
TRANSCRIBERS GROUP 10: AKASH 1
Gynecology EXIMIUS
Postoperative Management of Complications PART 1 2021
Corazon W. Adviento, MD March 2020
Pneumonia- treatment
Sept-2019 § No risk for MDR
§ Ceftriaxone 2g OD
§ Ampisul 3g q6
§ Levofloxacin 750mg OD
§ Moxifloxacin 400 mg OD
§ Ertapenem 1g OD
With risk of MDR
§ Antipseudomonal cephalosporin
§ Cefepime 2g q8
§ Ceftazidime 2g q8
§ Classic triad Antipseudomoanal carbapenem
§ Fever § Meropenem 1g q8
§ Tachypnea § Imipinem 500mg-1g q6
§ tachycardia § Piptazo 4.5g q 6
§ PE § For patients with severe allergies to penicillins
§ Tubular breathing § Aztreonam 2g q6-8 hour plus
§ Dec breath sounds § Antipseudomonal fluoroquinolone à
§ Moist inspiratory rales ciprofloxacin/ levofloxacin or
à Prominent on bases § Aminogylcoside à gentamycin, tobramycin,
§ Usually resolves spontaneously by 3rd or 5th postop day amikacin
§ Management: § MRSA coverage
§ Ambulation § Linezolid 600 mg q12hours
§ Deep breathing § Telavancin 10 mg/kg IV q 24 hours
§ Cough
§ Turn from side to side ASPIRATION PNEUMONIA
§ Remain semi erect § Occurs due to loss in protective airway reflexes
§ Use of Incentive spirometer during intubation and extubation or related to
postop N/V
PNEUMONIA § Pathogens:
§ Associated with atelectasis because bacterial infections § S. pneumoniae
usually begins at the collapsed lung. § H. influenza
§ Presdisposing factors: § S. aureus
Chronic pulmonary disease § G- rods
§ Heavy cigarette smoking § Treatment
§ Alcohol abuse § Clindamycin 600 mg IV q 8 hrs followed by 300
§ Obesity mg q6 hrs or 450 mg q 8 hrs
§ Advanced age or
§ NGT § Co amoxiclav 875 mg BID
§ Long operative procedures or
§ G(-) bacterial infections § Amoxicillin 500 mg TID plus Metronidazole 500
§ Postop peritonitis mg TID
§ Debilitating infections § Aspiration Pneumonitis
§ S/Sx § 1 in 3000 patients
§ Fever § Sec to aspiration of gastric fluid à severe
§ Cough chemical pneumonitis
§ Dyspnea § Aspiration and its complicationsà causes 30% of
§ Tachypnea anesthetic mortalities
§ Purulent sputum § Risk factors
§ Pain at the back § Older age
§ PE àCoarse rales § Obesity
§ Leukocytosis § Hiatal hernia
§ CXR: diffuse patchy infiltrates § Emergency surgery associated with full
§ GS : used to differentiate between bacterial colonization stomach
and infection
§ Management SLEEP APNEA
§ As atelectasis § Increased soft tissues of the head and neck can lead to
§ Parenteral antibiotics à based on type of airway compromise that leads to intermittent apnea and
pneumonia hypoventilation while a woman sleeps
§ Categories § Increased weight of adipose tissue on the neck, chest and
§ HAP à 48 hrs or more after admission abdominal wall leads to dec pulmonary compliance à
§ VAP à 48-72 hrs post intubation relative hypoxia à systemic as well as pulmonary
§ HCAP hypertension à hypercapnia
§ Morbidly obese patients
TRANSCRIBERS GROUP 10: AKASH 2
Gynecology EXIMIUS
Postoperative Management of Complications PART 1 2021
Corazon W. Adviento, MD March 2020
§ When given higher levels of O2 and narcotics à § Development of shock from acute blood loss depends on
Sept-2019
inc risk for apnea rate of bleeding
§ Develop increased sensitivity to narcotics à § Slow blood loss form venous source à blood
shuts down respiratory drive loss but not shock
§ Postop à O2 sat = 94% § Rapid blood loss of 20% blood volume à mild
§ 96-99% à lose respiratory drive à shock
hypercarbic and acidotic § Rapid blood loss of 40% of blood volume à
Stop – bang questions severe shock
§ Do you Snore?
§ Feel Tired easily? § Massive blood loss
§ Has anyone Observed you to stop breathing during sleep? § Hemorrhage that results in the replacement if
§ Are you being treated for high blood Pressure? 50% of blood volume in 3 hours
§ Is your BMI >35 ?
§ Are you older than Age 50? Hypotension : DDx
§ Is your Neck size >16 inches for a woman? § Blood loss
§ Is your Gender – male? § Anesthesia
OBSTRUCTIVE SLEEP APNEA § Over sedation
§ 0 – 2 yes à low risk § Postop bleeding
§ 3-4 yes à intermediate risk § Less than ideal ligature/ hemorrhage
§ > 5 à high risk from a vessel that has retracted during
operation
§ Sec to clotting abnormality
DDX FOR POSTOP HEMORRHAGIC SHOCK
§ Pneumothorax
§ Pulmonary embolism
§ Massive pulmonary aspiration
§ MI
§ Acute gastric dilatation
DDX FOR INEFFECTIVE COAGULATION DEFECT
§ Sepsis
§ Fibrinolysis
§ Diffuse Intravascular Coagulopathy
§ Previously unrecognized coagulation defect à von
CARDIOVASCULAR PROBLEMS Willebrand disease
HEMORRHAGIC SHOCK § Coagulopathies can also develop form massive blood
§ Shock à a condition in which circulatory transfusion
insufficiency prevents adequate § Hypofibrinogenemia à 1st to develop
vascular perfusion and reduced capillary filling § Thrombocytopenia à last to be detected
§ If neglected, leads to § Adrenergic response to hemorrhage
§ Oliguria § Perspiration
§ Progressive metabolic acidosis § Tachycradia
§ Multiple organ failure § Peripheral vasoconstriction
§ Produced by: § Early signs of hypovolemia sec to internal bleeding
§ Hemorrhage § Tachycardia
§ Cardiac failure § Dec urine output à due to dec perfusion of the
§ Sepsis kidneys
§ Anaphylactic reaction § With further blood loss
§ Agitation
§ Hypovolemic shock § Weakness
§ Most common cause of circulatory failure in § Pallor
gyne pxs § Cold and clammy extremities
§ Cardiogenic and septic shock à less common § Systolic BP <80 mmHg
§ Seen several hours postop MANAGEMENT GOALS OF POSTOP SHOCK
§ Restore circulating blood volume
§ Tachycardia à classic cardiovascular physiologic response § Maintain oxygenation
to hypotension § Correct coagulopathy
§ Progressive hypovolemia à dec urine output § Maintain body temp
§ Perioperative cause of shock à inadequate hemostasis § Correct biochemical abnormalities
§ Prevent pulmonary and other organ dysfunction
§ Treat underlying cause pf hemorrhage
§ Adequate ventilation
§ Rapid fluid replacement = 3:1 rule!!!
§ Crystalloids vs. colloids
TRANSCRIBERS GROUP 10: AKASH 3
Gynecology EXIMIUS
Postoperative Management of Complications PART 1 2021
Corazon W. Adviento, MD March 2020
§ Classic Sxs
Sept-2019 § Inflammation of the subcutaneous tissue
§ Fever
§ Painful and erythematous induration
Management
§ Removal of IV catheter
§ Mild à rest, elevation and hot compress
§ Moderate – severe à NSAID
§ With proximal progression à IV heparin and antibiotics
HEMATOMA
§ Wound or pelvic hematoma postop
§ Size depends on the potential size to which the hematoma
occurs
§ Increased risk
§ Patients on heparin and aspirin treatment prior
to surgery
§ S/Sx
§ Hgb is unexpectedly low at 3rd postop day
§ Tenderness on the affected area
§ Diagnosis:
§ PE
§ Imaging studies
Management:
§ Conservative à <5 cm
§ Percutaneous drainage : UTZ or CT- guided
§ Large hematomas becomes infected if untreated
even with antibiotics
RETAINED FOREIGN BODY
§ Incidence : 1 in 1200-1500 laparotomies
§ Sponge, ab pack, needles
THROMBOPHLEBITIS AND PULMONARY EMBOLUS
§ Surgery à Hypercoagulable state due to stress response
§ Superficial thrombophlebitis
§ Deep vein thrombosis
§ Pulmonary embolism
SUPERFICIAL THROMBOPHLEBITIS
§ one of the most common complicaitons
§ IV catheter
§ Benign but associated with deep vein thrombophlebitis in
5%
TRANSCRIBERS GROUP 10: AKASH 4
You might also like
- Med 23 Aug 2023 (A.N)Document21 pagesMed 23 Aug 2023 (A.N)Tauseef AfridiNo ratings yet
- Ch. 31 StudyDocument8 pagesCh. 31 StudyPaige Nicole GauthreauxNo ratings yet
- Dengue Management in Primary CareDocument61 pagesDengue Management in Primary CareDaniel RajNo ratings yet
- Dengue SlideDocument48 pagesDengue SlideKurouSakiNo ratings yet
- Management of Dengue FeverDocument31 pagesManagement of Dengue FeverDaniel RajNo ratings yet
- CEN+Online+Review Module+8 FinalDocument36 pagesCEN+Online+Review Module+8 FinalTamara Cooper100% (2)
- Roxana M. Culcer, M.D., FRACP - Aproach To A Collapsed NeonateDocument32 pagesRoxana M. Culcer, M.D., FRACP - Aproach To A Collapsed Neonatenicu 2021No ratings yet
- FCPS Surgery 26 Aug 2023 (M)Document16 pagesFCPS Surgery 26 Aug 2023 (M)Tauseef AfridiNo ratings yet
- Review A & P Nose and EpistaxisDocument14 pagesReview A & P Nose and EpistaxisVeeliz VaksNo ratings yet
- Presentation On Dengue FeverDocument31 pagesPresentation On Dengue FeverDrMuhammad Ishfaq HabibNo ratings yet
- IM Moonlighting 2015Document291 pagesIM Moonlighting 2015Isabelle SampangNo ratings yet
- Syock & ManagementDocument34 pagesSyock & ManagementIndra Anwari RukmanNo ratings yet
- Obstetrical Anesthesia: ObjectivesDocument10 pagesObstetrical Anesthesia: ObjectivesIsabel CastilloNo ratings yet
- Resuscitation in Retroperitoneal HaemorrhageDocument39 pagesResuscitation in Retroperitoneal Haemorrhagemark chrisatyaNo ratings yet
- Critical Event Checklists PDFDocument27 pagesCritical Event Checklists PDFMateas ZsoltNo ratings yet
- INFECTIOUS CASE - SGD 8Document91 pagesINFECTIOUS CASE - SGD 8PARADISE JanoNo ratings yet
- SPAPedi Crisis Checklists March 2023Document31 pagesSPAPedi Crisis Checklists March 2023marjana.burmuzoskaNo ratings yet
- Q. Necrotizing EnterocolitisDocument3 pagesQ. Necrotizing EnterocolitisRoselle Joy D. RosalejosNo ratings yet
- Dengue Fever ReportDocument7 pagesDengue Fever Reportmefav7778520No ratings yet
- CARDIOVASCULAR-DISEASE Cont.Document6 pagesCARDIOVASCULAR-DISEASE Cont.Kimberly Sharah Mae FortunoNo ratings yet
- Renal Transplant: Siti Husni Binti Entoh 790210-12-5522 Sem 1 (0kt / 2016)Document30 pagesRenal Transplant: Siti Husni Binti Entoh 790210-12-5522 Sem 1 (0kt / 2016)sjamilmdfauzieNo ratings yet
- 7 Dengue FeverDocument6 pages7 Dengue FeverNicole HipolNo ratings yet
- MeningococcemiaDocument34 pagesMeningococcemiaDeni Marie GomonidNo ratings yet
- 418 Septic Shock Sirs and ModsDocument51 pages418 Septic Shock Sirs and ModsApril Ann HortilanoNo ratings yet
- Capillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestDocument4 pagesCapillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestGerly MaglangitNo ratings yet
- Society For Pediatric Anesthesia Emergency Checklist ManualDocument28 pagesSociety For Pediatric Anesthesia Emergency Checklist ManualJill SweetNo ratings yet
- Case Scenario:: Is An Eye Finding Occurring Early inDocument5 pagesCase Scenario:: Is An Eye Finding Occurring Early inDenice Tamayo De GuzmanNo ratings yet
- Emergency Managment of EclampsiaDocument38 pagesEmergency Managment of EclampsiaMemento MagicNo ratings yet
- CEN+Online+Review Module+12 Final GENITODocument26 pagesCEN+Online+Review Module+12 Final GENITOTamara Cooper67% (3)
- Pathology Lecture 1 MSADocument6 pagesPathology Lecture 1 MSAcejix87209No ratings yet
- PSGNDocument23 pagesPSGNalpha mae beltranNo ratings yet
- DengueDocument32 pagesDengueUsamaNo ratings yet
- Med 22 Aug 2023 (M)Document17 pagesMed 22 Aug 2023 (M)Tauseef AfridiNo ratings yet
- Anorectal Disease and Common Anorectal DisordersDocument2 pagesAnorectal Disease and Common Anorectal DisordersIsabel CastilloNo ratings yet
- Joe Carcillo - Hemodynamic Managemnet in Peidtric SepsisDocument92 pagesJoe Carcillo - Hemodynamic Managemnet in Peidtric SepsisMega SeptianaNo ratings yet
- BronchiolitisDocument17 pagesBronchiolitisRizky DarmawanNo ratings yet
- Specimen CollectionDocument4 pagesSpecimen CollectionJiyahnBayNo ratings yet
- Hematology B Bleeding and Cancer PDFDocument143 pagesHematology B Bleeding and Cancer PDFMark Samuel TanchocoNo ratings yet
- Case Report Rupture Ectopic Pregnancy With History of AppendectomyDocument3 pagesCase Report Rupture Ectopic Pregnancy With History of AppendectomyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pedia Tickler Update 2017Document2 pagesPedia Tickler Update 2017Tani BokNo ratings yet
- M33 - Stase IPD - Hassan Assagaf Guidance For The Treatment of Deep Vein Thrombosis and Pulmonary EmbolismDocument16 pagesM33 - Stase IPD - Hassan Assagaf Guidance For The Treatment of Deep Vein Thrombosis and Pulmonary EmbolismHasan AssegafNo ratings yet
- Dengue Fever: A. BackgroundDocument5 pagesDengue Fever: A. BackgroundlavnakNo ratings yet
- Nursing Care For Child With Autoimmune Diseases & GI DisordersDocument4 pagesNursing Care For Child With Autoimmune Diseases & GI Disordersbunso padillaNo ratings yet
- 2.WS Fluid Pathophysiology of Fluid Overload in Critically IllDocument54 pages2.WS Fluid Pathophysiology of Fluid Overload in Critically IllMuhammadHazmiAnzhariNo ratings yet
- History Taking For FeverDocument13 pagesHistory Taking For FeverAfiQsyazwan Abd RaniNo ratings yet
- Luka BakarDocument67 pagesLuka Bakararezki chNo ratings yet
- Management: Sp-A SP-BDocument3 pagesManagement: Sp-A SP-BdocaliNo ratings yet
- Empyema: By-Komal JaiswalDocument29 pagesEmpyema: By-Komal JaiswalOlga GoryachevaNo ratings yet
- Dengue 2Document56 pagesDengue 2Eliz Codilla-SyNo ratings yet
- Respiratory Term 2Document13 pagesRespiratory Term 2Abegail QuintoNo ratings yet
- MIS C Algorithim Version 2Document8 pagesMIS C Algorithim Version 2Saima UmairNo ratings yet
- Leptospirosis - Ferri's Clinical AdvisorDocument2 pagesLeptospirosis - Ferri's Clinical AdvisorAndika GhifariNo ratings yet
- Kuliah EmergensiDocument66 pagesKuliah EmergensiRifqi RamdhaniNo ratings yet
- Thoracic Trauma - Navy - PSPD 2021Document45 pagesThoracic Trauma - Navy - PSPD 2021Naavy LaksmonoNo ratings yet
- Ncma 219 Rle Task 1Document10 pagesNcma 219 Rle Task 1Gina PrancelisoNo ratings yet
- Dengue: History Physical Examination InvestigationDocument4 pagesDengue: History Physical Examination InvestigationNik Hanisah Zuraidi AfandiNo ratings yet
- Post Partum HemorrhageDocument26 pagesPost Partum HemorrhageZulfan ZulfanNo ratings yet
- C19 SPACE ToolKit ChecklistsDocument8 pagesC19 SPACE ToolKit ChecklistsAdrian BălanNo ratings yet
- SURGICAL PATHOLOGY SOFT TISSUES TableDocument4 pagesSURGICAL PATHOLOGY SOFT TISSUES TableIsabel CastilloNo ratings yet
- Ok Ok Notes PediaDocument10 pagesOk Ok Notes PediaIsabel CastilloNo ratings yet
- Surgical Pathology - CNSDocument2 pagesSurgical Pathology - CNSIsabel CastilloNo ratings yet
- Dermatology - Exanthematous Viral DiseasesDocument6 pagesDermatology - Exanthematous Viral DiseasesIsabel CastilloNo ratings yet
- Surgical Pathology - Major and Minor Salivary GlandsDocument2 pagesSurgical Pathology - Major and Minor Salivary GlandsIsabel CastilloNo ratings yet
- DERMATOLOGY - Cuteneous Candidiasis, PityrosporumDocument4 pagesDERMATOLOGY - Cuteneous Candidiasis, PityrosporumIsabel CastilloNo ratings yet
- Pediatric Therapeutics: Eximius 2021Document13 pagesPediatric Therapeutics: Eximius 2021Isabel CastilloNo ratings yet
- Growth and DevelopmentDocument60 pagesGrowth and DevelopmentIsabel CastilloNo ratings yet
- Dermatology - Skin NeoplasmsDocument12 pagesDermatology - Skin NeoplasmsIsabel CastilloNo ratings yet
- Implantataion Placental Development and AbnormalitiesDocument62 pagesImplantataion Placental Development and AbnormalitiesIsabel CastilloNo ratings yet
- EMBRYOGENESIS and Fetal DevtDocument50 pagesEMBRYOGENESIS and Fetal DevtIsabel CastilloNo ratings yet
- Anorectal Disease and Common Anorectal DisordersDocument2 pagesAnorectal Disease and Common Anorectal DisordersIsabel CastilloNo ratings yet
- Irritable Bowel SyndromeDocument3 pagesIrritable Bowel SyndromeIsabel CastilloNo ratings yet
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- AHA-PALS 2010: Pediatric Chain of SurvivalDocument10 pagesAHA-PALS 2010: Pediatric Chain of SurvivalIsabel CastilloNo ratings yet
- Diseases of The Newborn: ObjectivesDocument17 pagesDiseases of The Newborn: ObjectivesIsabel CastilloNo ratings yet
- Acute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankDocument4 pagesAcute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankIsabel CastilloNo ratings yet
- Acute and Chronic PancreatitisDocument8 pagesAcute and Chronic PancreatitisIsabel CastilloNo ratings yet
- Pedia Pre School NewsDocument3 pagesPedia Pre School NewsIsabel CastilloNo ratings yet
- AsthmaDocument4 pagesAsthmaIsabel CastilloNo ratings yet
- Pneumonia: TranscribersDocument6 pagesPneumonia: TranscribersIsabel CastilloNo ratings yet
- Adolescent Medicine: Early AdolescenceDocument2 pagesAdolescent Medicine: Early AdolescenceIsabel CastilloNo ratings yet
- Inflammatory Bowel Disease: Microorganisms That Drive DiseaseDocument4 pagesInflammatory Bowel Disease: Microorganisms That Drive DiseaseIsabel CastilloNo ratings yet
- Interatitial Lung DiseaseDocument2 pagesInteratitial Lung DiseaseIsabel CastilloNo ratings yet
- Pack-Years of Cigarette Smoking Is The Most HighlyDocument5 pagesPack-Years of Cigarette Smoking Is The Most HighlyIsabel CastilloNo ratings yet
- Hyperthyroidism: EpidemiologyDocument8 pagesHyperthyroidism: EpidemiologyIsabel CastilloNo ratings yet
- Causes of HypothyroidismDocument6 pagesCauses of HypothyroidismIsabel Castillo100% (1)
- Mesenteric Vascular Insufficiency: ClassificationDocument2 pagesMesenteric Vascular Insufficiency: ClassificationIsabel CastilloNo ratings yet
- Diseases of Esophagus.Document3 pagesDiseases of Esophagus.Isabel Castillo100% (2)
- Approach To The Patient With Disease of The Respiratory SystemDocument3 pagesApproach To The Patient With Disease of The Respiratory SystemIsabel CastilloNo ratings yet
- Global Report On Atopic Dermatitis 2022Document68 pagesGlobal Report On Atopic Dermatitis 2022chen peng feiNo ratings yet
- Nursing Care of Child With LIFE THREATENING CONDITIONSDocument70 pagesNursing Care of Child With LIFE THREATENING CONDITIONSinno so qtNo ratings yet
- Understanding Learners With Difficulty in Mobility (LDM) : Department of EducationDocument60 pagesUnderstanding Learners With Difficulty in Mobility (LDM) : Department of EducationCherry Bobier100% (1)
- Tuberculosis: Tests and DiagnosisDocument3 pagesTuberculosis: Tests and DiagnosisArnie PengNo ratings yet
- 2024self-Report of Medical ConditionsDocument3 pages2024self-Report of Medical Conditionsdiolanto5No ratings yet
- Diarrhea: On This PageDocument6 pagesDiarrhea: On This PageKristine AlejandroNo ratings yet
- Neutrophil-to-Lymphocyte Ratio and Covid-19 Symptom-BasedDocument6 pagesNeutrophil-to-Lymphocyte Ratio and Covid-19 Symptom-BasedRahmi NisaNo ratings yet
- To The Learners: English 8Document9 pagesTo The Learners: English 8Mark Angelo SuarezNo ratings yet
- 9 - Systemic Lupus ErythematosusDocument34 pages9 - Systemic Lupus ErythematosusIrina PopoviciNo ratings yet
- Streptococcus Pneumoniae Menggunakan Gen Autolysin (Lyta) SebagaiDocument9 pagesStreptococcus Pneumoniae Menggunakan Gen Autolysin (Lyta) SebagaiFauzi RidhoNo ratings yet
- FNCPDocument4 pagesFNCPJonalyn Tumanguil100% (2)
- Recognizing and Reporting Red Flags For The Physical Therapist Assistant 1stDocument52 pagesRecognizing and Reporting Red Flags For The Physical Therapist Assistant 1stsummer.yates611100% (40)
- Aplastic Anemia: Edited: Dr. Dairion Gatot SP - PD-KHOMDocument11 pagesAplastic Anemia: Edited: Dr. Dairion Gatot SP - PD-KHOMrubyniNo ratings yet
- Statement of The ProblemDocument13 pagesStatement of The ProblemDaniel LeoNo ratings yet
- How Accountancy Students Affected by This Pandemic?Document3 pagesHow Accountancy Students Affected by This Pandemic?Anica Maye BrosasNo ratings yet
- Post-Test - SWU BSN 4-Medical - Surgical Nursing 3: Total PointsDocument15 pagesPost-Test - SWU BSN 4-Medical - Surgical Nursing 3: Total PointsNaomi VirtudazoNo ratings yet
- Coronavirus: Say True or False Answer The Following QuestionsDocument2 pagesCoronavirus: Say True or False Answer The Following QuestionsLORENA ESPARZA PAJARES33% (3)
- Microbial Risk Analysis: A.B. Boehm, J.A. SollerDocument10 pagesMicrobial Risk Analysis: A.B. Boehm, J.A. Sollermahdi najafzadehNo ratings yet
- HelminthsDocument190 pagesHelminthsSarhan AliNo ratings yet
- Polyserositis: A Diagnostic Challenge: Polyserositis Diagnosis Is ChallengingDocument7 pagesPolyserositis: A Diagnostic Challenge: Polyserositis Diagnosis Is ChallengingAarathi raoNo ratings yet
- Epistaxis Journal PDFDocument4 pagesEpistaxis Journal PDFRia WidyartaNo ratings yet
- Neurological Disorders Practice Test QuestionsDocument6 pagesNeurological Disorders Practice Test QuestionsBenedict AlvarezNo ratings yet
- Tahun 2021Document7 pagesTahun 2021Dina Pratya NiayNo ratings yet
- Hypervolemia NCPDocument2 pagesHypervolemia NCPAlroi Abrantes50% (2)
- Licente Medicina 2022Document93 pagesLicente Medicina 2022Daniela ScurtuNo ratings yet
- Ated Aid1001 PDFDocument5 pagesAted Aid1001 PDFFitri AngginiNo ratings yet
- Nursing Care Plan 1 - DiarrheaDocument7 pagesNursing Care Plan 1 - DiarrheakirbyroohNo ratings yet
- Lec 5 New Castle DiseaseDocument38 pagesLec 5 New Castle Diseasebasit abdulNo ratings yet
- Micro Para ReportDocument27 pagesMicro Para Reportdeathmark1078No ratings yet
- Structure & Characterstics of Normal & Cancer CellsDocument58 pagesStructure & Characterstics of Normal & Cancer CellsVinay SahuNo ratings yet