Professional Documents
Culture Documents
Examination of The Breast: 11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK
Uploaded by
Nilakshi Barik Mandal0 ratings0% found this document useful (0 votes)
18 views19 pagesOriginal Title
breast-exam3566-160122102201
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views19 pagesExamination of The Breast: 11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK
Uploaded by
Nilakshi Barik MandalCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 19
Examination of the Breast
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 1
Examination of the breast II
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 2
General
All examiners should normally be chaperoned
The texture of normal breast tissue varies from
smooth to granular
Texture may also vary with the menstrual cycle and
during pregnancy
Nodularity and tenderness often increase towards
the end of the cycle and during menstruation
Breast tissue is usually symmetrical so always
examine both and compare one to the other
This examination could be performed on either
gender
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 3
Inspection
The patient should be undressed to the waist and
seated with arms by side
Breast Nipples
size everted, flat, or inverted
(note if recent change or
symmetry
longstanding
shape of breast
cracking or ‘eczema’
skin colour
gross deviation of the nipple
lumps
bleeding or discharge
skin tethering
Areola: observe for
prominent veins or oedema
of the skin with dimpling like abnormal reddening
orange skin (peau d’orange) thickening
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 4
Inspection II
Ask the patient to raise her arms above
her head (this is particularly important for
inspection of the axilla and axillary tail)
Ask the patient to place hands on hips
and to apply downward pressure to the
hips whilst leaning forward slightly.
An inspection of the breasts should also
be made once the patient is lying flat, as
abnormalities may become more
apparent when the tissue falls against
anterior chest wall
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 5
Inspection III
These positions will:
Stretch the breast tissue and overlying skin
Exaggerate abnormalities of contour and skin
Muscle tethering may be apparent
In health women may have some slight asymmetry
of the breast and nipples
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 6
Breast Palpation I
Patient lies on the couch
When possible lying flat with
one pillow behind the head
arms by her sides or with her
hand(s) behind her head
Get on level with the patient (thus
avoiding pushing into the breast
tissue and causing the patient
discomfort)
Palpate using palmar surface of
middle three fingers
Use a rotary motion to gently
press the breast tissue against
the chest wall
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 7
Breast palpation II
Examine each breast systematically covering the whole
cone of breast tissue using one of the following methods:
zig zag, concentric, or radial paths
A systematic, methodical examination of all the breast
tissue (covering the four quadrants, axillary tail and
areola/nipple) ensures that small lesions are not missed
With large or pendulous breasts, use one hand to steady
the breast on lower border whilst palpating with other
Breast tissue should be palpated against the chest wall
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 8
Palpation of the breast
Breast
Mammary gland
Areola
Nipple
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 9
Systems of breast palpation I
The examiner zigzags up
and down the breast
ensuring all tissue is
palpated.
This method was the
preferred method for self
examination and
It is preferred by some
clinicians as the breast
tissue remains in contact
with the chest wall during
Pictures from the American association of plastic surgeons
palpation.
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 10
Systems of breast palpation II
The breast tissue is
examined using a
concentric circular
approach
The examiner starts
at the periphery and
ends at the areola
and nipple
Pictures from the American association of plastic surgeons
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 11
Systems of breast palpation III
The examiner divides the
breasts into a series of
segments
The quadrants are
examined methodically in
turn from periphery
towards nipple
The examiner traces a
pattern similar to a clock
face ensuring each
Pictures from the American association of plastic surgeons
segment is overlapped
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 12
Breast Palpation II - the axillary tail
To examine the axillary tail of
Spence, ask the patient to rest her
arms above her head
Feel the tail between thumb and
fingers as it extends from the
upper outer quadrant towards the
axilla
If you feel a breast lump examine
the mass between your fingers
Unlike fat the breast has distinctly
lobular texture which may be
tender to palpation Pictures from the American association of plastic surgeons
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 13
Breast palpation III - the nipple and areola
To examine nipple; hold the areola behind it
between thumb and fingers
Gently compress, attempting to express any
discharge
Note colour of any discharge and send
samples for cytology and microbiology
On completion cover the breasts or offer the
patient the opportunity to put their bra back
on, either after or before examining the axilla
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 14
Examination of axilla 1
With the patient sitting
facing the examiner
The patient’s arm is
raised and supported
The slightly cupped
fingers of the
examiners opposite
hand are inserted into
the apex of the axilla
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 15
Examination of axilla 2
The patient’s forearm is rested
across the examiner’s forearm
The examiner feels for each
group of lymph nodes, whilst
steadying the shoulder with
the other hand
Apical
anterior (posterior surface of
anterior axillary fold)
medial (on the chest wall)
lateral (against the humerus)
posterior (anterior surface of
posterior axillary fold)
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 16
Examination of axilla 3
An alternative is to ask the
patient to rest their hand on
the examiner’s shoulder
The examiner then
methodically feels for each
group of nodes, whilst
steadying the shoulder with
the other hand
Also examine the
supraclavicular and
infraclavicular areas for
nodes
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 17
Record findings
Record any abnormalities
of the breast
Identify which quadrant and
which breast (e.g. right
upper outer quadrant)
LEFT It is often best to record
findings graphically
AT Record presence of any
nodes in the axilla,
UIQ UOQ
supraclavicular or
LIQ LOQ infraclavicular areas
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 18
Recording your findings
Don’t forget when recording your findings
Patient identifier, date (and time), signature and
name
When documenting the size, position and
shape of a swelling, a diagram may often be
useful.
During some examinations you can still note
and record: size, position, shape, consistency,
surface and mobility. This must be done if a
swelling is detected
11/14/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 19
You might also like
- Breast Exam Guide for Medical StudentsDocument11 pagesBreast Exam Guide for Medical Studentscharlyn206No ratings yet
- Breast Exam: A Systematic ApproachDocument3 pagesBreast Exam: A Systematic ApproachBearaphNo ratings yet
- Please Read 1F Simulations Compilations 1Document36 pagesPlease Read 1F Simulations Compilations 1mendozakaceeyNo ratings yet
- bmj00069 0040Document3 pagesbmj00069 0040hanh minhNo ratings yet
- Breast and Axillae AssessmentDocument146 pagesBreast and Axillae AssessmentFaith madayag100% (2)
- Module 6 Breast Axilla Assessment-Edited 0 0Document13 pagesModule 6 Breast Axilla Assessment-Edited 0 0Laila PasiganNo ratings yet
- FMcase 1Document24 pagesFMcase 1Ryan Townsend100% (2)
- Assessment of The Breast: Jonalyn Sotero Esco RN., MANDocument41 pagesAssessment of The Breast: Jonalyn Sotero Esco RN., MANVan MaverickNo ratings yet
- BreastDocument3 pagesBreastUriel NateNo ratings yet
- Breast Examination - OSCE Guide - Geeky MedicsDocument6 pagesBreast Examination - OSCE Guide - Geeky MedicsJahangir AlamNo ratings yet
- Breast Assessment: Preparing The ClientDocument5 pagesBreast Assessment: Preparing The Clientshannon c. lewisNo ratings yet
- 04 New Obstetric ExaminationDocument44 pages04 New Obstetric Examinationfranny90No ratings yet
- CamaristaCM - BreastCancer (Questions and Answers)Document4 pagesCamaristaCM - BreastCancer (Questions and Answers)Coleen Mae CamaristaNo ratings yet
- Labor Process and Nursing Care GuideDocument9 pagesLabor Process and Nursing Care GuideMary Florence VelardeNo ratings yet
- What Are The Physical Examination On Monitoring The Labour?Document2 pagesWhat Are The Physical Examination On Monitoring The Labour?Nurfi Resni Fitra RamdaNo ratings yet
- Health Talk On BSFDocument11 pagesHealth Talk On BSFjyoti singh100% (1)
- STUDENT COPY Assessment of Breast and AxillaeDocument57 pagesSTUDENT COPY Assessment of Breast and AxillaeRosette Malenab de AsisNo ratings yet
- Colposcopy CourseDocument50 pagesColposcopy CourseNam Le100% (1)
- Nursing Care During LaborDocument12 pagesNursing Care During LaborJulianne B. Dela CruzNo ratings yet
- Breast Self Examination: o o o oDocument3 pagesBreast Self Examination: o o o oDalvin Roy WongNo ratings yet
- NCM 112 Skills Lab Cellular AberrationDocument10 pagesNCM 112 Skills Lab Cellular AberrationMeryville JacildoNo ratings yet
- Breast and Axillae SynthesisDocument3 pagesBreast and Axillae SynthesisEya BaldostamonNo ratings yet
- Amniocentrices (From The Greek Amnion For "Sac" and KenteDocument5 pagesAmniocentrices (From The Greek Amnion For "Sac" and KenteJohn Paolo Tamayo OrioNo ratings yet
- Breast Anatomy and Examination GuideDocument11 pagesBreast Anatomy and Examination GuideKrishna Faith P. DelaraNo ratings yet
- UNIT-VII Assessment of the Breast and AxillaDocument30 pagesUNIT-VII Assessment of the Breast and Axillaraima ayazNo ratings yet
- Prenatal Care: Understanding Pelvic Exams and Fetal AssessmentDocument9 pagesPrenatal Care: Understanding Pelvic Exams and Fetal AssessmentBinita ShakyaNo ratings yet
- Examination of The BreastDocument2 pagesExamination of The BreastAufi FillaNo ratings yet
- 175 Ultrasound in Pregnancy PDFDocument16 pages175 Ultrasound in Pregnancy PDFNestor FerrerNo ratings yet
- Breast Self ExaminationDocument4 pagesBreast Self ExaminationSagar HanamasagarNo ratings yet
- Retensio PlasentaDocument3 pagesRetensio PlasentaAnonymous c4GVTgkvNo ratings yet
- National College of Nursing: Procedure ONDocument6 pagesNational College of Nursing: Procedure ONSumit Yadav100% (1)
- A Cog Practice Bulletin 175 Ultrasound in PregnancyDocument16 pagesA Cog Practice Bulletin 175 Ultrasound in Pregnancyansel7No ratings yet
- Ring Pessary Effective For Advanced POPDocument8 pagesRing Pessary Effective For Advanced POPputri vinia /ilove cuteNo ratings yet
- 1 GYNE 3 - History, PE, Prevention Interaction of Disease and PhysiologyDocument6 pages1 GYNE 3 - History, PE, Prevention Interaction of Disease and PhysiologyIrene FranzNo ratings yet
- Health-Assessment-Breast-and-AxillaDocument27 pagesHealth-Assessment-Breast-and-AxillaMary Jane M. MorenoNo ratings yet
- Definition: Related Diagnostic TestsDocument8 pagesDefinition: Related Diagnostic TestsQuinn Xylon VillanuevaNo ratings yet
- Breast ModuleDocument2 pagesBreast ModuleDasha Vee100% (1)
- Normal LaborDocument27 pagesNormal LaborRamil BonifacioNo ratings yet
- Breast: Dr. Sylvia N. SaingDocument26 pagesBreast: Dr. Sylvia N. SaingRichard 151289100% (1)
- Emergency Nursing ChecklistDocument6 pagesEmergency Nursing ChecklistMark DomingoNo ratings yet
- Understanding Breast DisordersDocument13 pagesUnderstanding Breast DisordersCalimlim KimNo ratings yet
- Full Term Newborn Delivery Stages and IndicationsDocument34 pagesFull Term Newborn Delivery Stages and IndicationsAaliyaan KhanNo ratings yet
- SDP Vs AFIDocument5 pagesSDP Vs AFINuzma AnbiaNo ratings yet
- How To Measure Cervical Length: Karl Oliver Kagan and Jiri SonekDocument14 pagesHow To Measure Cervical Length: Karl Oliver Kagan and Jiri SoneknidoNo ratings yet
- Apple Peel Small Bowel, A Review of Four Cases: Surgical and Radiographic AspectsDocument8 pagesApple Peel Small Bowel, A Review of Four Cases: Surgical and Radiographic AspectsraecmyNo ratings yet
- Cord Clamping - Physiologic ApproachDocument13 pagesCord Clamping - Physiologic ApproachravyryNo ratings yet
- Leopold's maneuvers determine fetal positionDocument39 pagesLeopold's maneuvers determine fetal positionJayrelle D. SafranNo ratings yet
- Hysteroscopic Differences in Blighted Ovum and Viable PregnancyDocument5 pagesHysteroscopic Differences in Blighted Ovum and Viable PregnancyAgudisarfNo ratings yet
- Heimlich Maneuver PDFDocument7 pagesHeimlich Maneuver PDFMark DomingoNo ratings yet
- Screening of Breast CancerDocument19 pagesScreening of Breast CancerIncredible DivineNo ratings yet
- Self Breast ExaminationDocument11 pagesSelf Breast ExaminationJairene Dave Martinez Cambalon100% (2)
- Teach MeDocument5 pagesTeach Medryasmin95No ratings yet
- Back Et Al - 2017 - Emergent Ultrasound Evaluation of The Pediatric Female PelvisDocument10 pagesBack Et Al - 2017 - Emergent Ultrasound Evaluation of The Pediatric Female PelvisBerry BancinNo ratings yet
- Placenta AccretaDocument5 pagesPlacenta AccretaF3rcitaNo ratings yet
- Effectiveness of Delayed Absorbable Monofila - 2014 - Taiwanese Journal of ObsteDocument3 pagesEffectiveness of Delayed Absorbable Monofila - 2014 - Taiwanese Journal of ObsteSami KahtaniNo ratings yet
- Cervical incompetence diagnosis and managementDocument40 pagesCervical incompetence diagnosis and managementCristian AlbuNo ratings yet
- Physiology of Pregnancy. Perinatal Care of Fetus. Methods of Examination of Pregnant Women.Document15 pagesPhysiology of Pregnancy. Perinatal Care of Fetus. Methods of Examination of Pregnant Women.Erwin SiahaanNo ratings yet
- Breast and AxillaeDocument4 pagesBreast and AxillaeDanesse CapitlyNo ratings yet
- Dental Management of the Pregnant PatientFrom EverandDental Management of the Pregnant PatientChristos A. SkouterisNo ratings yet
- History and Physical Assessment of the Integumentary SystemDocument84 pagesHistory and Physical Assessment of the Integumentary SystemNilakshi Barik MandalNo ratings yet
- Mentalhealthactppt 160524140542Document34 pagesMentalhealthactppt 160524140542Nilakshi Barik MandalNo ratings yet
- Pain AssessmentDocument12 pagesPain AssessmentFadhilah Asyifa DewantiNo ratings yet
- Pain Scale and Its Types: Quratulain Mughal Batch Iv Doctor of Physical Therapy Isra UniversityDocument11 pagesPain Scale and Its Types: Quratulain Mughal Batch Iv Doctor of Physical Therapy Isra UniversityNilakshi Barik MandalNo ratings yet
- Birth Injuries in Neonates: Pediatrics in Review November 2016Document15 pagesBirth Injuries in Neonates: Pediatrics in Review November 2016Nilakshi Barik MandalNo ratings yet
- Presented By: Sandeep Yadav M.Sc. (N) 1 Year KGMU LucknowDocument93 pagesPresented By: Sandeep Yadav M.Sc. (N) 1 Year KGMU LucknowNilakshi Barik MandalNo ratings yet
- Pptforphysical 130322221925 Phpapp01Document117 pagesPptforphysical 130322221925 Phpapp01Karen Mae Santiago AlcantaraNo ratings yet
- Clinical Examination: Plan of Conduction & Scheme of RecordingDocument112 pagesClinical Examination: Plan of Conduction & Scheme of RecordingNilakshi Barik MandalNo ratings yet
- New Format With Correct LayoutDocument3 pagesNew Format With Correct LayoutNilakshi Barik MandalNo ratings yet
- Gate Control TheoryDocument6 pagesGate Control TheoryNilakshi Barik MandalNo ratings yet
- Physical Examination: Presented To Mrs. Nisha Mane Assistant Professor D.Y.P.S.O.NDocument41 pagesPhysical Examination: Presented To Mrs. Nisha Mane Assistant Professor D.Y.P.S.O.NNilakshi Barik MandalNo ratings yet
- Clinical Examination: Plan of Conduction & Scheme of RecordingDocument112 pagesClinical Examination: Plan of Conduction & Scheme of RecordingNilakshi Barik MandalNo ratings yet
- Efficacy, Safety and Fertility Return of Implanon Contraceptive ImplantDocument4 pagesEfficacy, Safety and Fertility Return of Implanon Contraceptive ImplantNilakshi Barik MandalNo ratings yet
- Monica Rita Hendricks PDFDocument151 pagesMonica Rita Hendricks PDFNilakshi Barik MandalNo ratings yet
- Cardio Pulmonary Resuscitation Adult & Paediatric Definition of Cardiac ArrestDocument8 pagesCardio Pulmonary Resuscitation Adult & Paediatric Definition of Cardiac ArrestNilakshi Barik Mandal0% (1)
- Ijshr0038 PDFDocument9 pagesIjshr0038 PDFNilakshi Barik MandalNo ratings yet
- Medical Surgical Nursing AssignmentDocument166 pagesMedical Surgical Nursing AssignmentSonali Sengar0% (1)
- CamScanner Document ScansDocument48 pagesCamScanner Document ScansNilakshi Barik MandalNo ratings yet
- Ms. Nilakshi Barik Mandal Lecturer Oxford College of Nursing SciencesDocument11 pagesMs. Nilakshi Barik Mandal Lecturer Oxford College of Nursing SciencesNilakshi Barik MandalNo ratings yet
- Oral Hygiene: Mrs - NilakshiDocument11 pagesOral Hygiene: Mrs - NilakshiNilakshi Barik MandalNo ratings yet
- History and Physical Assessment of the Integumentary SystemDocument84 pagesHistory and Physical Assessment of the Integumentary SystemNilakshi Barik MandalNo ratings yet
- Pain Manage Me NT: Ms - Nilakshi Barik MandalDocument14 pagesPain Manage Me NT: Ms - Nilakshi Barik MandalNilakshi Barik MandalNo ratings yet
- PreconceptionDocument29 pagesPreconceptionNilakshi Barik MandalNo ratings yet
- Gate Contro L Theory: Ms - Nilakshi Barik MandalDocument6 pagesGate Contro L Theory: Ms - Nilakshi Barik MandalNilakshi Barik MandalNo ratings yet
- Fetal SkullDocument5 pagesFetal SkullNilakshi Barik MandalNo ratings yet
- Ms. Nilakshi Barik Mandal Lecturer Oxford College of Nursing SciencesDocument11 pagesMs. Nilakshi Barik Mandal Lecturer Oxford College of Nursing SciencesNilakshi Barik MandalNo ratings yet
- Female PelvisDocument7 pagesFemale PelvisNilakshi Barik MandalNo ratings yet
- Nutrition Course PlanDocument7 pagesNutrition Course PlanNilakshi Barik MandalNo ratings yet
- BSc Nursing Unit Plan Nutrition 2019-20Document1 pageBSc Nursing Unit Plan Nutrition 2019-20Nilakshi Barik MandalNo ratings yet
- BreastDocument2 pagesBreastAdrian SantosNo ratings yet
- Axilla Boundaries and ContentDocument47 pagesAxilla Boundaries and Contentchzaheer72No ratings yet
- Axila: Mesole Samuel Bolaji (B.SC M.SC PHD (In-View) ) Course: Anatomy Course Code: Han 3010Document15 pagesAxila: Mesole Samuel Bolaji (B.SC M.SC PHD (In-View) ) Course: Anatomy Course Code: Han 3010Tinotenda KarumeNo ratings yet
- Body LinesDocument1 pageBody LinesAnonymous OAEuN9NE1sNo ratings yet
- 5 Axillary and Epitrochlear Lymph Node Dissection For MelanomaDocument11 pages5 Axillary and Epitrochlear Lymph Node Dissection For MelanomajuanrangoneNo ratings yet
- Surgical Anatomy of The Breast T-HAZEM - CompressedDocument28 pagesSurgical Anatomy of The Breast T-HAZEM - CompressedmohamedhazemelfollNo ratings yet
- Download ebook Selective Anatomy Prep Manual For Undergraduates Vol 1 2E Pdf full chapter pdfDocument67 pagesDownload ebook Selective Anatomy Prep Manual For Undergraduates Vol 1 2E Pdf full chapter pdfcharles.brewer536100% (24)
- Lecture FiveDocument35 pagesLecture FivePiniel MatewosNo ratings yet
- Tilak 2009/2010 ZimaDocument33 pagesTilak 2009/2010 Zima4outdoor.plNo ratings yet
- Breast Exam Detailed Skill SheetDocument1 pageBreast Exam Detailed Skill SheetMuhammed ElgasimNo ratings yet
- Understanding The SelfDocument24 pagesUnderstanding The Selfelvie dijanNo ratings yet
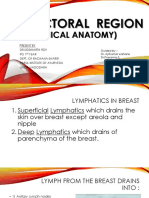
- Lymphatics of the Breast and Clinical Anatomy (39Document28 pagesLymphatics of the Breast and Clinical Anatomy (39SIDDHRATH ROYNo ratings yet
- Bathing An Adult ClientDocument8 pagesBathing An Adult ClientXoisagesNo ratings yet
- Hygiene and Health in IslamDocument37 pagesHygiene and Health in Islamالمدینہ اسلامک ریسرچ سینٹر کراچی100% (1)
- Breast AssessmentDocument3 pagesBreast Assessmenttaé pNo ratings yet
- Breast ExaminationDocument3 pagesBreast ExaminationShum Wing Hei JoanneNo ratings yet
- It Is A Pyramid-Shaped Space Between The Upper Part of The Arm and The Side of The ChestDocument25 pagesIt Is A Pyramid-Shaped Space Between The Upper Part of The Arm and The Side of The ChestMoaiadHusseinNo ratings yet
- Nine Locks - of The Human BodyDocument9 pagesNine Locks - of The Human BodyKalyan PingaliNo ratings yet
- Breast and Lymphatic SysytemDocument3 pagesBreast and Lymphatic SysytemJL RebeseNo ratings yet
- AXILLADocument8 pagesAXILLAImmunity RABOTANo ratings yet
- Locomotor Module Guide by MedAngleDocument15 pagesLocomotor Module Guide by MedAnglefqtyd8ypsjNo ratings yet
- CriolipóliseTM 908A新Document25 pagesCriolipóliseTM 908A新Cyber100% (2)
- Axilla and Cubital Fossa (AYY)Document19 pagesAxilla and Cubital Fossa (AYY)LeeMinhoNo ratings yet
- RTOG Breast Cancer Atlas For Radiation Therapy PlanningDocument71 pagesRTOG Breast Cancer Atlas For Radiation Therapy Planningdoctordoctor80No ratings yet
- The Axilla: Norah AlmudawiDocument14 pagesThe Axilla: Norah AlmudawiF-med440 imamNo ratings yet
- 4 AxillaDocument31 pages4 AxillaRamesh KumarNo ratings yet
- Breast (Mamma)Document69 pagesBreast (Mamma)Wealth AbiodunNo ratings yet
- Tanner Stage Calculator For BoysDocument11 pagesTanner Stage Calculator For BoysFootball Club Allianz0% (1)
- Breast and Axilla 2Document17 pagesBreast and Axilla 2Justine Nyangaresi100% (1)
- Breast Cancer Atlas For RT PlanningDocument26 pagesBreast Cancer Atlas For RT PlanningZuriNo ratings yet