Professional Documents
Culture Documents
Sanford Antibiotic Chart PDF
Sanford Antibiotic Chart PDF
Uploaded by
Jonathan C. SimmondsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sanford Antibiotic Chart PDF
Sanford Antibiotic Chart PDF
Uploaded by
Jonathan C. SimmondsCopyright:
Available Formats
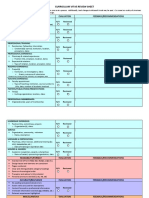
Penicillins Carbapenems Fluoroquinolone Parenteral Cephalosporins Oral Cephalosporins Aminoglyco Macrolides Tetracyclines Glyco/Lipo Ox-lid Poly Other
Penicillin G
Penicillin VK
Nafcillin
Oxacillin
Cloxacillin
Flucloxacillin
Dicloxacillin
Ampicillin
Amoxicillin
Amox-Clav
Amp-Sulb
Pip-Tazo
Doripenem
Ertapenem
Imipenem
Meropenem
Mero-Vabor
Aztreonam
Ciprofloxacin
Delafloxacin
Ofloxacin
Levofloxacin
Moxifloxacin
Norfloxacin
Prulifloxacin
Gemifloxacin
Gatifloxacin
Cefazolin
Cefotetan
Cefoxitin
Cefuroxime
Cefotaxime
Ceftizoxime
Ceftriaxone
Ceftazidime
Cefepime
Ceftaz-Avibac
Ceftaroline
Ceftol-Tazo
Cefadroxil
Cephalexin
Cefaclor
Cefprozil
Cefurox-Axe
Cefixime
Ceftibuten
Cefpodoxime
Cefdinir
Cefditoren
Gentamicin
Tobramycin
Amikacin
Chloramphenicol
Clindamycin
Erythromycin
Azithromycin
Clarithromycin
Telithromycin
Doxycycline
Minocycline
Tetracycline
Tigecycline
Daptomycin
Vancomycin
Teicoplanin
Telavancin
Oritavancin
Dalbavancin
Linezolid
Tedizolid
Polymyxin B
Colistin
Fusidic Acid
Rif (comb)
TMP-SMX
Nitrofurantoin
Fosfomycin (IV)
Fosfomycin (po)
Metronidazole
Quinu-Dalfo
Fluconazole
Itraconazole
Voriconazole
Posaconazole
Isavuconazole
Anidulafungin
Caspofungin
Micafungin
Amphotericin B
Adenovirus
BK Virus
Cytomegalovirus
Hepatitis B
Hepatitis C
Herpes simplex
HPV
Influenza A
Influenza B
JC Virus / PML
RSV
Varicella-zoster
Antibacterials Antifungal Drugs Viruses
Aerobic gram-pos cocci Fungi Hepatitis B
E. faecalis (S) ++ 0 0 0 0 0 0 ++ ++ + + + +/- +/- +/- +/- +/- 0 +/-* + +/- + + + +/-* + + 0 0 0 0 0 0 +/-* 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 +/- 0 0 0 0 0 +/- +/- +/- + + ++ ++ + + + + + 0 0 +/- +/-* 0 + +/- +/- 0 0 Aspergilllus fumigatus 0 +/- ++ + ++ +/- +/- +/- + Adefovir NA NA NA ++ NA NA NA NA NA NA NA NA
E. faecium (S) +/- 0 0 0 0 0 0 +/- +/- +/- +/- +/- 0 0 0 0 0 0 0 0 0 0 +/- 0 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 +/- 0 0 0 0 0 +/- +/- +/- + + +/- +/- +/- + +/- ++ + 0 0 +/- +/-* 0 + +/- +/- 0 + Aspergillus terreus 0 +/- ++ + ++ +/- +/- +/- 0 Emtricitabine NA NA NA +/-* NA NA NA NA NA NA NA NA
E. faecalis (VRE) +/- 0 0 0 0 0 0 +/- +/- +/- +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 +/- 0 0 0 0 0 +/- +/- +/- +/- + 0 0 +/- + 0 ++ + 0 0 0 +/-* 0 + +/- +/- 0 0 Aspergiullus flavus 0 +/- ++ + ++ +/- +/- +/- + Entecavir NA NA NA ++ NA NA NA NA NA NA NA NA
E. faecium (VRE) +/- 0 0 0 0 0 0 +/- +/- +/- +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 NA +/- 0 0 0 0 0 +/- +/- +/- +/- + 0 0 +/- + 0 ++ + 0 0 0 +/-* 0 + +/- +/- 0 + Candida albicans ++ + + + + ++ ++ ++ + Lamivudine NA NA NA +/-* NA NA NA NA NA NA NA NA
S. aureus MSSA +/- +/- ++ ++ ++ ++ ++ +/- +/- + + + +* + + + + 0 0 + + + + 0 0 + + ++ + + + + + + +/- + +/- + ? + + + + + 0 0 + + + +/-* ? ? + + +/- +/- +/- + + + + + + + + + + + + + 0 0 + +/-* + 0 + 0 0 + Candida dubliniensis ++ + + + + ++ ++ ++ ++ Telbivudine NA NA NA +/-* NA NA NA NA NA NA NA NA
S. aureus HA-MRSA 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 +/-* ? ? + +/- 0 0 0 +/- + + +/- + ++ * ++ ++ + + + ++ + 0 0 + +/-* + 0 + 0 0 + Candida glabrata +/- +/- +/- +/- +/- ++ ++ ++ ++ Tenofovir NA NA NA ++ NA +/-* NA NA NA NA NA NA
S. aureus CA-MRSA 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + +/- +/- +/- 0 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 +/-* ? ? + + 0 0 0 +/- + + +/- + ++ * ++ ++ + + + + + 0 0 + +/-* + 0 + 0 0 + Candida guilliermondii ++ ++ ++ ++ + ++ ++ ++ ++ Hepatitis C
Staph coag-neg (S) +/- +/- ++ ++ ++ ++ ++ +/- +/- + + + + + + + + 0 + + + + + 0 + + + ++ + + + + + + +/- + +/- + ? +/- +/- +/- + + 0 0 + + + +/-* ? ? + + +/- +/- +/- + + + + + + + + + + + + + 0 0 + +/-* + 0 + 0 0 + Candida krusei 0 0 + + + ++ ++ ++ ++ Daclatasvir NA NA NA NA ++ NA NA NA NA NA NA NA
Staph coag-neg (R) 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 +/-* ? ? + +/- 0 0 0 +/- +/- +/- +/- + ++ ++ ++ + + + ++ + 0 0 + +/-* + 0 +/- 0 0 + Candida lusitaniae ++ + + + + ++ ++ ++ 0 Dasabuvir NA NA NA NA ++ NA NA NA NA NA NA NA
S. epidermidis (R) 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 +/-* ? ? + +/- 0 0 0 +/- +/- +/- +/- + ++ ++ ++ + + + ++ + 0 0 + +/- + 0 +/- 0 0 + Candida parapsilosis ++ + + + + + + + ++ Elbasir NA NA NA NA ++ NA NA NA NA NA NA NA
S. epidermidis (S) +/- +/- ++ ++ ++ ++ ++ +/- +/- + + + + + + + + 0 + + + + + 0 + + + ++ + + + + + + +/- + +/- + ? + + + + + ? ? + + + +/-* ? ? + + + + + + + + + + + + + + + + + + 0 0 + +/- + 0 + 0 0 + Candida tropicalis ++ + + + + ++ ++ ++ ++ Grazoprevir NA NA NA NA ++ NA NA NA NA NA NA NA
S. lugdunensis +/- +/- ++ ++ ++ ++ ++ +/- +/- + + + + + + + + 0 0 + + + + 0 0 + + ++ + + + + + + +/- + +/- + ? + + + + + ? ? + + + +/-* ? ? + + + + + + + + + + + + + + + + + + 0 0 + +/-* + 0 0 0 0 + Cryptococcus sp. ++ + + + + 0 0 0 ++ Interferon alfa, peg NA NA NA ++ +* NA NA NA NA NA NA NA
S. saprophyticus +/- +/- + + + + + +/- +/- ++ + + + + + + + 0 + + + + + 0 + + + ++ + + + + + + +/- + +/- + ? ++ ++ ++ + + ? ? + + + 0 0 0 + + +/- +/- +/- ? + + + + + + + + ? ? 0 0 0 0 0 0 + + +/- +/- 0 0 Dematiaceous molds 0 ++ ++ + + +/- +/- +/- + Ledipasvir NA NA NA NA ++ NA NA NA NA NA NA NA
Strep. anginosis gp ++ ++ + + + + + + + + + + + + + + + 0 +/- + +/- +/- +/- 0 +/- +/- +/- + + + + + + + + + + + + + + + + + + + + + + +/-* ? ? + + +/- +/- +/- + +/- +/- +/- + 0* + + + + + + + 0 0 ? 0 0 0 0 0 0 + Fusarium sp. 0 +/- +/- +/- +/- 0 0 0 +/- Ombitasvir NA NA NA NA ++ NA NA NA NA NA NA NA
Strep. pyogenes (A) ++ ++ + + + + + + + + + + + + + + + 0 +/- + +/- +/- +/- 0 +/- +/- +/- + + + + + + + + + + + + + + + + + + + + + + +/- 0 0 + + +/- +/- +/- + ? ? ? + + + + + + + + + 0 0 ? 0 +/- 0 + 0 0 + Mucormycosis 0 0 0 + + 0 0 0 ++ Paritaprevir NA NA NA NA ++ NA NA NA NA NA NA NA
Strep. agalactiae (B) ++ ++ + + + + + + + + + + + + + + + 0 +/- + +/- +/- +/- 0 +/- +/- +/- + + + + + + + + + + + + + + + + + + + + + + +/- 0 0 + + +/- +/- +/- + ? ? ? + + + + + + + + + 0 0 ? 0 +/- 0 + 0 0 + Scedo apiospermum 0 0 + +/- +/- 0 0 0 0 Ribavirin +/- NA NA 0 +* NA NA NA NA NA +/-* NA
Strep. gp C,F,G ++ ++ + + + + + + + + + + + + + + + 0 +/- + +/- +/- +/- 0 +/- +/- +/- + + + + + + + + + + + + + + + + + + + + + + +/-* 0 0 + + +/- +/- +/- + ? ? ? + + + + + + + + + 0 0 ? 0 +/- 0 + 0 0 + Lomentospora prolificans 0 0 0 0 0 0 0 0 0 Simeprevir NA NA NA NA +* NA NA NA NA NA NA NA
Strep. pneumoniae ++ ++ + + + + + + + + + + +* + + + + 0 +/- + +/- + + 0 +/- + + + + + + + + + + + + + + + + + + + + + + + + 0 0 0 + + +/- +/- +/- + +/- +/- +/- + +/- + + + ? ? + + 0 0 ? 0 +/- 0 + 0 0 + Trichosporon spp. +/- + + + + 0 0 0 + Sofosbuvir NA NA NA NA ++ NA NA NA NA NA NA NA
Viridans Strep. +/- +/- +/- +/- +/- +/- +/- +/- +/- +/- +/- +/- + + + + + 0 0 + 0 + + 0 0 + + + + + + ++ + ++ +/- + +/- + + + + + 0 + + 0 + + + +/-* 0 0 + +/- +/- +/- +/- + +/- +/- +/- + 0 * ++ ++ + + + + + 0 0 ? 0 ? 0 0 0 0 + Dimorphic Fungi Velpatasvir NA NA NA NA ++ NA NA NA NA NA NA NA
Aerobic gram-pos bacilli Blastomyces +/- ++ + + + 0 0 0 ++ Voxilaprevir NA NA NA NA ++ NA NA NA NA NA NA NA
Arcanobacter. sp + + ? ? ? ? ? + + + + + + + + + + 0 + ? + + + 0 + + + + + + + + + + + + + + ? + + + + + + + + + ? ? ? ? ? ++ ++ ++ ++ + ++ + + + + ++ + + ? ? + ? 0 0 0 0 0 0 0 0 0 + Coccidioides ++ ++ + + + 0 0 0 ++ Influenza
C. diphtheriae ++ ++ 0 0 0 0 0 + + + + + ? ? ? ? ? 0 ? ? ? ? ? 0 ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 0 0 0 0 + ++ + + ? ? ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 Histoplasma +/- ++ + + + 0 0 0 ++ Amantadine NA NA NA NA NA NA NA +/-* +/-* NA NA NA
C. jeikeium 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? 0 0 +/- 0 0 +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? +* + ++ + + 0 0 + ? 0 0 0 0 0 0 0 0 0 ? Sporothrix +/- ++ + + + 0 0 0 ++ Oseltamivir NA NA NA NA NA NA NA ++ NA + NA NA
L. monocytogenes + 0 0 0 0 0 0 ++ + + + + ? ? ? +/- +/- 0 0 + 0 + + 0 0 + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? 0 0 0 0 + 0 0 0 0 0 Peramivir NA NA NA NA NA NA NA + * + * NA NA NA
Nocardia sp. 0 0 0 0 0 0 0 0 0 +/- ? ? ? 0 ++ + + 0 0 ? 0 0 0 0 0 0 0 0 0 0 0 +/- 0 +/-* 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ * 0 0 0 ? ? ? ? +/- 0 ? 0 0 0 0 0 0 + ? 0 0 0 0 ++ 0 0 0 0 0 Antibacterials Notes: Rimantadine NA NA NA NA NA NA NA +/-* +/-* NA NA NA
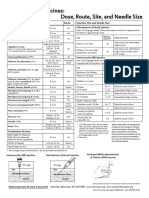
Aerobic GNB - Enteric • Amikacin, Nocardia sp., Use in combination Zanamavir NA NA NA NA NA NA NA ++ + NA NA NA
• Amoxicillin, C. trachomatis, Recommended only as alternate for pregnant women, due to concern that
Aeromonas sp. 0 0 0 0 0 0 0 0 0 +/- +/- + + + + + + + + + + + + 0 + + + 0 0 0 ? + + + + + + ? ? ? 0 ? ? ? ? ? ? ? ? + + + + 0 0 0 0 0 + + 0 + 0 0 0 0 0 0 0 0 + + 0 0 + 0 ? 0 0 0 bacteria persist rather than being killed. Herpes, CMV, VZV, misc.
• Ampicillin, C. trachomatis, Recommended only as alternate for pregnant women, due to concern that
C. jejuni 0 0 0 0 0 0 0 0 0 + 0 0 + + + + + ? + + + + + 0 + + + 0 0 0 0 + + + + + + ? ? 0 0 0 0 0 0 0 0 0 0 + + + ? ? ++ ++ + 0 +/- +/- +/- ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 bacteria persist rather than being killed. Acyclovir NA NA 0 NA NA ++ NA NA NA NA NA +
• Azithromycin, E. coli (S), Enterohemorrhagic E.coli are susceptible
C. freundii 0 0 0 0 0 0 0 0 0 0 0 ++ + + + ++ + +/- + + + + + + + + + 0 0 0 0 +/- +/- +/- +/- ++ + + + 0 0 0 0 0 + + + + ? + + + ? 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- +/- + + 0 0 • Azithromycin, M. genitalium, resistance reported and emerging to all antibiotics including fluoroquinolones
Cidofovir + + ++ NA NA + * NA NA NA + * NA +
C. koseri 0 0 0 0 0 0 0 0 0 0 0 ++ + + + ++ + +/- + + + + + + + + + 0 0 0 0 +/- +/- +/- +/- ++ + + + 0 0 0 0 0 + + + + ? + + + ? 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- +/- + + 0 0 • Azithromycin, U. urealyticum, Link with STI unclear. Some data suggests in patients with symptoms longer Famciclovir NA NA 0 NA NA ++ NA NA NA NA NA +
than 3 weeks, 6 days 500mg qd more efficacious than 1g single dose.
E. aerogenes 0 0 0 0 0 0 0 0 0 0 0 + + + + + + + + + + + + + + + + 0 0 0 0 0 0 0 0 + + 0 + 0 0 0 0 0 0 0 0 0 0 + + + 0 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 + +/- +/- +/- 0 0 • Aztreonam, E. coli, Klebs MBL, Aztreonam is not hydrolyzed by MBLs, but MBL+ strains often have other Foscarnet NA NA ++ NA NA + NA NA NA NA NA +
enzymes that can.
E. cloacae 0 0 0 0 0 0 0 0 0 0 0 + + + + + + + + + + + + + + + + 0 0 0 0 0 0 0 0 + + 0 + 0 0 0 0 0 0 0 0 0 0 + + + 0 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 + +/- +/- +/- 0 0 • Ceftazidime, Y. enterolitica, Clinical failures reported Ganciclovir +/- NA ++ NA NA + NA NA NA NA NA +
E. coli (S) 0 0 0 0 0 0 0 +/- +/- + + + +* + + + + + + + + + + + + + + + + + + + + + + + + + + +/- +/- +/- + + + + + + ? + + + + 0 0 +/-* 0 0 +/- +/- +/- +* 0 0 0 0 0 0 0 0 + + 0 0 +/- + + + 0 0 • Ceftriaxone, E. faecalis (S) , Use only in combination with ampicillin. Letermovir NA NA ++ * NA NA NA NA NA NA NA NA NA
• Ceftriaxone, F. necrophorum, Use in combination with metronidazole
E. coli, Klebs ESBL 0 0 0 0 0 0 0 0 0 0 0 +/- +* + ++ ++ + 0 +/- +/- +/- +/- +/- +/- +/- +/- +/- 0 +/- +/- 0 0 0 0 0 0 + 0 + 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- +/- 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- +/- + + 0 0 • Ceftriaxone, Nocardia sp., May be used as part of combination therapy; never used as monotherapy Valacyclovir NA NA 0 NA NA ++ NA NA NA NA NA ++
• Cefuroxime, Y. enterolitica, Clinical failures reported
E. coli, Klebs KPC 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- 0 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- +/- +/- +/- 0 0 • Ciprofloxacin, E. faecalis (S) , Most strains +/-, can be used in UTI, not in systemic infection. Valganciclovir +/- NA ++ NA NA + NA NA NA NA NA +
• Daptomycin, S. aureus CA-MRSA, Do not use for pneumonia
E. coli, Klebs MBL 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/-* +/- 0 0 +/- 0 0 +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 + + 0 0 0 0 +/- +/- 0 0 • Daptomycin, S. aureus HA-MRSA, Do not use for pneumonia
Topical Agents
Enterics CRE, NOS 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- 0 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- +/- +/- +/- 0 0 • Daptomycin, Strep. anginosis gp, Despite in vitro susceptibility, resistance to daptomcyin emerges rapidly Imiquimod NA NA NA NA NA NA ++ NA NA NA NA NA
in viridans group streptococci
K. oxytoca 0 0 0 0 0 0 0 0 0 + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + +/- +/- +/- + + + + + + ? + + + + 0 0 0 0 0 0 +/- 0 + 0 0 0 0 0 0 0 0 + + 0 0 +/- + +/- +/- 0 0 • Daptomycin, Viridans Strep., Despite in vitro susceptibility, resistance to daptomcyin emerges rapidly in Penciclovir NA NA 0 NA NA + * NA NA NA NA NA 0
viridans group streptococci
K. pneumoniae (S) 0 0 0 0 0 0 0 0 0 + + + +* + + + + + + + + + + + + + + + + + + + + + + + + + + +/- +/- +/- + + + + + + ? + + + + 0 0 0 0 0 0 +/- 0 +* 0 0 0 0 0 0 0 0 + + 0 0 +/- + +/- +/- 0 0 • Doripenem, A. baumanii, Do not use Doripenem to treat any kind of pneumonia Podofilox NA NA NA NA NA NA ++ NA NA NA NA NA
Morganella sp. 0 0 0 0 0 0 0 0 0 0 0 + + + +/-* + + + + + + + ? + + ? ? 0 + + 0 + + + + ++ + + + 0 0 0 0 0 0 0 0 0 0 + + + ? 0 0 0 0 0 0 0 0 ?* 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 • Doripenem, E. coli (S), Do not use Doripenem to treat any kind of pneumonia Sinecatechins NA NA NA NA NA NA + NA NA NA NA NA
• Doripenem, E. coli, Klebs ESBL, Do not use Doripenem to treat any kind of pneumonia
P. mirabilis 0 0 0 0 0 0 0 + + + + + + + +/-* + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + + ? + + + ? 0 0 0 0 0 0 +/- 0 + 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 + + 0 0 • Doripenem, K. pneumoniae (S), Do not use Doripenem to treat any kind of pneumonia Trifluridine NA NA NA NA NA + * NA NA NA NA NA NA
• Doripenem, P. aeruginosa, Do not use Doripenem to treat any kind of pneumonia
P. vulgaris 0 0 0 0 0 0 0 0 0 + + + + + +/-* + + + + + + + + + + + + 0 + + + + + + + + + ? + 0 0 0 0 0 + + + ? ? + + + +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 +/- +/- 0 0 • Doripenem, S. aureus MSSA, Do not use Doripenem to treat any kind of pneumonia.
• Doripenem, Strep. pneumoniae, Do not use Doripenem to treat any kind of pneumonia.
Providencia sp. 0 0 0 0 0 0 0 0 0 0 0 + ++ ++ +/-* ++ + + + + + + + + + ? ? 0 + + 0 + + + + + + ? + 0 0 0 0 0 + + + ? ? +/- +/- + ? 0 0 0 0 0 0 0 0 ? 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 + + 0 0 • Gatifloxacin, C. burnetii, FQs potential alternative if CNS infected as FQs have good CNS penetration Antiviral Notes:
• Gatifloxacin, M. genitalium, resistance reported and emerging to all antibiotics including fluoroquinolones • Hepatitis B , Emtricitabine, Do not use as mono therapy. High level resistance occurs when emtricitabine is
Salmonella sp. 0 0 0 0 0 0 0 +/- +/- + + + + + + + + + + + + + + 0 + + + 0 ? ? ? + + + + + + ? ? 0 0 0 0 0 + + + + ? + + + + 0 0 + 0 0 +/- +/- 0 +* 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 • Gemifloxacin, C. burnetii, FQs alternative if CNS infected. used alone
Serratia sp. 0 0 0 0 0 0 0 0 0 0 0 + + + + + + + + + + + + 0 + + + 0 + 0 0 + + + + + + ? + 0 0 0 0 0 + 0 0 0 0 + + + 0 0 0 0 0 0 0 0 0 +* 0 0 0 0 0 0 0 0 0 0 0 0 + 0 +/- +/- 0 0 • Gemifloxacin, N. gonorrhoeae, Used in combination with azithro for ceftriaxone resistant strains • Hepatitis B , Lamivudine, Do not use as mono therapy. High level resistance occurs when lamivudine is used
• Gentamicin, Bartonella sp., In combination with doxycycline or azithromycin alone against HBV
Shigella sp. 0 0 0 0 0 0 0 0 0 + + + + + + + + + ++ + + ++ + 0 ++ + + 0 ? ? ? + + + + + + ? ? 0 0 0 0 0 + + + + ? + + + + 0 0 + 0 0 +/- +/- 0 +* 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 • Gentamicin, E. faecalis (S), Use only in combination.
• Hepatitis B , Telbivudine, Do not use as mono therapy. High level resistance occurs when telbivudine is used
• Gentamicin, E. faecalis (VRE), Use only in combination
Y. enterolitica 0 0 0 0 0 0 0 0 0 +/- +/- + + ? + + + + ++ + + ++ + 0 ++ ? + 0 +/- +/- +/-* ++ + ++ +/-* ++ ? ? ? 0 0 0 0 0 + + ? ? ? + + + 0 0 0 0 0 0 + ? ? ? 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 • Gentamicin, E. faecium (S), Use only in combination. alone
• • Herpes simplex , Tenofovir, Some evidence of activity against HSV
Aerobic GNB - Non-enteric Gentamicin, E. faecium (VRE), Use only in combination
• Gentamicin, F. tularensis, Streptomycin is drug of choice • Hepatitis C , Interferon alfa, peg, No longer 1st line therapy
Bartonella sp. 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ * 0 0 0 0 + ++ ++ ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 0 0 0 0 • Gentamicin, L. monocytogenes, Use only in combination • Hepatitis C , Ribavirin, No longer 1st line therapy
• Gentamicin, S. aureus CA-MRSA, Use only in combination • Hepatitis C , Simeprevir, No longer preferred first line therapy except in special circumstances
B. pertussis 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? ? ? 0 ? ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ++ ++ ? ? ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 • Gentamicin, S. aureus HA-MRSA, Use only in combination
• RSV , Ribavirin, Minimal Activity. Palivizumab is an option for prophylaxis in immunocompromised patients
• Gentamicin, S. aureus MSSA, Use only in combination
B. burgdoferi + 0 0 0 0 0 0 ++ ++ + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + + 0 ++ 0 0 0 0 0 0 0 0 0 ++ 0 0 0 0 0 0 0 0 0 0 + + + ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Gentamicin, S. epidermidis (R), Use only in combination • Influenza A , Amantadine, High level resistance H1N1 (non-swine) in 2008; Swine H1N1 susceptible
Brucella sp. 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? ? ? 0 + ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? + 0 0 0 0 0 + + + ? 0 0 0 0 0 0 0 0 0 0 0 +/-* + 0 0 0 0 0 • Gentamicin, S. epidermidis (S), Use only in combination • Influenza B , Amantadine, Influenza B is intrinsically resistant
• Gentamicin, S. lugdunensis, Use only in combination • Influenza A , Peramivir, Good option for ICU patients who cannot absorb oral agents
Capnocytophagia +/- +/- 0 0 0 0 0 +/- +/- ++ + ++ + ? ++ ++ + 0 +/- ? +/- +/- ? 0 +/- ? ? 0 0 0 0 + ? + + + + 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- + ++ ? ? ? ? + + + ? 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 • Gentamicin, Staph coag-neg (R), Use only in combination • Influenza B , Peramivir, Good option for ICU patients who cannot absorb oral agents
• Gentamicin, Staph coag-neg (S), Use only in combination • Influenza A , Rimantadine, High level resistance H1N1 (non-swine) in 2008; Swine H1N1 susceptible
C. burnetii 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? + + + 0 + +* +* 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 + + + ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 +/-* + 0 0 0 0 0 • Gentamicin, Strep. anginosis gp, Use only in combination
• Influenza B , Rimantadine, Influenza B is intrinsically resistant
• Gentamicin, Strep. gp C,F,G, Use only in combination for Group B strep
Ehrlichia, Anaplas 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? ?* ? 0 ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 0 0 0 0 • Gentamicin, Viridans Strep., Use only in combination
• Herpes simplex , Cidofovir, Best option when ACV resistance is present
• • JC Virus / PML , Cidofovir, Data support its use is inconclusive. When used properly, with appropriate pre-
Eikenella sp +/- +/- 0 0 0 0 0 +/- +/- + + + + + + + + ? + ? + + ? 0 + ? ? 0 ? + 0 + ? + ? ? ? ? ? 0 0 0 ? 0 ? ? ? ? ? +/- 0 0 + 0 0 0 0 0 + + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 Imipenem, Morganella sp., Currently recommended breakpoints for imipenem have significantly reduced
medication with probenecid and fluids, appears to work well vs. JC virus CNS disease
susceptibility rates for imipenem compared to other carbapenems. The clinical significance of this is not
F. tularensis 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ ? ? ? ? 0 ++ ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ * + ? + ? 0 ? ? ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 known but in absence of clinical data of efficacy use of another carbapenem should be considered for • Cytomegalovirus , Letermovir, CMV prophylaxis in transplant pts
infections caused by this organism. • Herpes simplex , Penciclovir, Topical use only
H. ducreyi 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? ? ? ? ++ ? ? + ? 0 ++ ? ? 0 0 0 0 0 0 ++ 0 ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ ++ ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Imipenem, P. mirabilis, Currently recommended breakpoints for imipenem have significantly reduced • Herpes simplex , Trifluridine, For ophthalmic use
susceptibility rates for imipenem compared to other carbapenems. The clinical significance of this is not
H. influenzae 0 0 0 0 0 0 0 +/- +/- ++ ++ + + + + + + + + + + ++ ++ 0 + + + 0 + + + ++ + ++ + + + + + 0 0 +/- + + + + + + + 0 0 0 + 0 0 + + + + + + + 0 0 0 0 0 0 0 0 0 0 0 0 + 0 + 0 0 0 known but in absence of clinical data of efficacy use of another carbapenem should be considered for
Kingella sp. + + 0 0 0 0 0 + + + + + + + + + + ? + + + ++ ? 0 + ? ? + + + + + + ++ + + + + + 0 0 0 + 0 + + + + + + 0 0 + 0 0 ? ? ? + + + + 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 infections caused by this organism.
• Imipenem, P. vulgaris, Currently recommended breakpoints for imipenem have significantly reduced
K. granulomatis 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ ? ? ? ? 0 ++ ? ? 0 0 + 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? + 0 ++ ++ + 0 ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 0 0 0 0 susceptibility rates for imipenem compared to other carbapenems. The clinical significance of this is not
known but in absence of clinical data of efficacy use of another carbapenem should be considered for
Legionella sp. 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ + ++ ++ ++ 0 ++ + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ ++ ++ + + + + + 0 0 0 0 0 0 0 0 0 0 0 +/-* + 0 0 0 0 0 infections caused by this organism. Recommended (++)
• Imipenem, Providencia sp., Currently recommended breakpoints for imipenem have significantly reduced
Leptospira sp. ++ 0 0 0 0 0 0 + + + + + + + + + + + + + + + + 0 + + + ? ? ? ? ++ ? ++ ? + + ? ? ? ? ? ? ? ? ? ? ? ? 0 0 0 + 0 + ++ + ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 ? 0 0 0 0 0 susceptibility rates for imipenem compared to other carbapenems. The clinical significance of this is not
Agent is a first line therapy: reliably active in vitro, clinically effective, guideline
M. catarrhalis 0 0 0 0 0 0 0 0 0 ++ + + + + + + + + + + + + + 0 + + + 0 + +/- + + + + + + + + + 0 0 +/- + + + + + + + 0 0 0 0 0 + + + + + + + ? 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 known but in absence of clinical data of efficacy use of another carbapenem should be considered for recommended, recommended as a first-line agent or acceptable alternative agent in
infections caused by this organism.
N. gonorrhoeae 0 0 0 0 0 0 0 0 0 0 0 0 + + + + + + +/- ? +/- +/- 0 0 +/- + * 0 +/- +/- +/- 0 +/- +/- ++ ? + ? ? ? 0 0 0 0 0 + 0 + 0 0 0 0 0 0 0 0 + 0 0 +/- +/- +/- ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Levofloxacin, Ehrlichia, Anaplas, Levo active in vitro in one small study the Sanford Guide.
• Moxifloxacin, M. genitalium, resistance reported and emerging to all antibiotics including fluoroquinolone
N. meningitidis + 0 0 0 0 0 0 ++ ++ 0 0 + + + + + + + ? ? ? ? ? 0 ? ? ? 0 0 0 + + + ++ + + + ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Prulifloxacin, E. faecalis (S) , Most strains +/-, can be used in UTI, not in systemic infection. Active (+)
• Rif (comb), Bartonella sp., In combination with doxycycline
P. multocida ++ ++ 0 0 0 0 0 ++ ++ ++ ++ + + + + + + + + + + + + 0 + + + 0 ? ? + + + + ? + ? + + ? 0 0 ? + + ? + + ? +/- +/- +/- ? 0 0 + 0 0 + + + + 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 • Rif (comb), Brucella sp., In combination
Agent is a potential alternative agent (active in vitro, possesses class activity
R. ricketsii 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- ? +/- +/- +/- 0 +/- ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 +/- 0 ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Rif (comb), C. burnetii, In combination comparable to known effective agents or a therapeutically interchangeable agents
• Rif (comb), Chlamydophila sp., In combination
T. pallidum ++ 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 + ? +* ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Rif (comb), E. faecalis (S) , In combination. and hence likely to be clinically effective, but second line due to overly broad
• Rif (comb), E. faecalis (VRE), In combination
V. cholera 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? ? ? 0 + ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + + ? ? + + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Rif (comb), E. faecium (S), In combination. spectrum, toxicity, limited clinical experience, or paucity of direct evidence of
• Rif (comb), E. faecium (VRE), In combination
V. parahemolyticus 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? ? ? ? + ? + + ? 0 + ? ? 0 0 0 0 + + + + + + ? ? 0 0 0 0 0 0 0 0 0 0 ? ? ? + ? ? + 0 0 + ? +* ? 0 0 0 0 0 0 0 0 0 0 0 0 ? 0 0 0 0 0 • Rif (comb), Ehrlichia, Anaplas, In combination
effectiveness).
V. vulnificus 0 0 0 0 0 0 0 0 0 0 0 0 ? ? ? ? ? ? + ? + + ? 0 + ? ? 0 0 0 0 + + + + + + ? ? 0 0 0 0 0 0 0 0 0 0 ? ? ? + 0 0 ? 0 0 + + +* ? 0 0 0 0 0 0 0 0 0 0 0 0 ? 0 0 0 0 0 • Rif (comb), Legionella sp., In combination Variable (+/-)
• Rif (comb), S. aureus CA-MRSA, In combination
Y. pestis 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? ? ? 0 + ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? ? + 0 0 0 0 0 + + + ? 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 • Rif (comb), S. aureus HA-MRSA, In combination Variable activity such that the agent, although clinically effective in some settings or
• Rif (comb), S. aureus MSSA, In combination
Aerobic GNB non-fermenter • Rif (comb), S. lugdunensis, In combination types of infections is not reliably effective in others, or should be used in combination
• Rif (comb), Staph coag-neg (R), In combination
A. baumanii 0 0 0 0 0 0 0 0 0 0 +/- +/- + * 0 ++ +/- +/- 0 +/- ? +/- +/- +/- 0 +/- ? ? 0 0 0 0 0 0 +/- +/- +/- ? ? +/- 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 0 0 +/- +/- + * 0 0 0 0 0 0 0 0 + + 0 0 +/- 0 0 0 0 0 • Rif (comb), Staph coag-neg (S), In combination
with another agent, and/or its efficacy is limited by resistance which has been
B. cepacia 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- + 0 + 0 0 0 0 0 0 +/- 0 0 0 0 0 0 +/- 0 0 0 0 0 0 +/- +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 • Tetracycline, T. pallidum, Not recommended as first line therapy, but a possible alternative in the associated with treatment failure.
penicillin-allergic patient
P. aeruginosa 0 0 0 0 0 0 0 0 0 0 0 + +* 0 + + + + + + 0 + 0 0 + 0 0 0 0 0 0 0 0 0 + + + 0 + 0 0 0 0 0 0 0 0 0 0 + + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + + 0 0 0 0 +/- +/- 0 0 • Tetracycline, V. parahemolyticus, Resistance rates vary markedly geographically and exceed 20% in some Not Recommended (0)
countries.
S. maltophilia 0 0 0 0 0 0 0 0 0 0 0 +/- 0 0 0 0 0 0 0 ? 0 +/- +/- 0 0 ? ? 0 0 0 0 0 0 0 +/- 0 +/- 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 0 0 0 0 + + 0 +* 0 0 0 0 0 0 0 0 + + 0 0 ++ 0 0 0 0 0 • Tetracycline, V. vulnificus, Resistance rates vary markedly geographically and exceed 20% in some Agent is a poor alternative to other agents because resistance to likely to be present
countries.
Aerobic - cell wall-deficient • Tigecycline, A. baumanii, Use only if no other treatment option. Use in combination
or occur, due to poor drug penetration to site of infection or an unfavorable toxicity
C. trachomatis 0 0 0 0 0 0 0 +* +* 0 0 0 0 0 0 0 0 0 0 ? ++ ++ + 0 0 + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ++ + ? ++ + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Tigecycline, C. freundii, FDA recommends use only if no other option profile, or limited or anecdotal clinical data to support effectiveness.
• Tigecycline, C. jeikeium, Do not use unless no other option
Chlamydophila sp. 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? + + + 0 + + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + 0 + + + + ++ + + + 0 0 0 0 0 0 0 0 0 0 0 +/-* 0 0 0 0 0 0 • Tigecycline, C. koseri, FDA recommends use only if no other option
• Tigecycline, E. aerogenes, FDA suggests avoidance unless no other treatment option
M. genitalium 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? 0 +/- ++ * 0 0 ? +* 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ? ++ * ? ? +/- +/- +/- ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Tigecycline, E. cloacae, FDA recommends use only if no other option Insufficient Data (?)
• Tigecycline, E. coli (S), Use only if no other treatment option
M. pneumoniae 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? + ++ ++ 0 + + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 +/- +/- +/- +/- ++ ++ ++ + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Tigecycline, E. coli, Klebs ESBL, Use only if no other options
Insufficient data to recommend use.
U. urealyticum 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 + ? + + + 0 + ? ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ ++ * + ? ++ + + ? 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 • Tigecycline, E. coli, Klebs KPC, Use only if no other option Not Applicable (NA)
• Tigecycline, Enterics CRE, NOS, Use only if no other option
Anaerobic GNB • Tigecycline, K. pneumoniae (S), Use only if no other option Agent has no activity against this pathogen.
• Tigecycline, Morganella sp., Use only if no other option Editorial Note: The data provided are intended to serve as a general guide to antibacterial usefulness based on treatment guidelines and
B. fragilis 0 0 0 0 0 0 0 0 0 ++ + ++ + ++ ++ ++ + 0 0 + 0 0 +/- 0 0 0 0 0 +/- +/- 0 0 + 0 0 0 0 0 + 0 0 0 0 0 0 0 0 0 0 0 0 0 + +/- 0 0 0 0 +/- +/- +/- + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 • Tigecycline, S. maltophilia, Do not use unless no other treatment options recommendations, in vitro activity, predominant patterns of susceptibility or resistance and/or demonstrated clinical effectiveness. Variability in
• Tigecycline, Salmonella sp., Use only if no other treatment option
F. necrophorum +/- +/- 0 0 0 0 0 +/- +/- + + + + + + + + 0 0 ? 0 0 ? 0 0 ? ? 0 + + ? + ? +* ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 0 0 0 + + 0 0 0 0 + + + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 • Tigecycline, Serratia sp., Use only if no other treatment option
resistance patterns due to regional differences or as a consequent of clinical setting (e.g., community-onset vs. ICU-acquired infection) should be taken
into account when using this table because activities of certain agents can differ significantly from what is shown in the table, which are by necessity
P. melaninogenica +/- +/- 0 0 0 0 0 +/- +/- + + + + + + + + 0 0 ? 0 +/- + 0 0 ? ? 0 + + ? ? ? ? ? ? ? ? + ? ? ? ? ? ? ? ? ? ? 0 0 0 + + +/- +/- +/- 0 + + + + 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 • Tigecycline, Shigella sp., Use only if no other treatment option based on aggregate information.
Anaerobic gram-positive
Actinomyces sp. ++ ++ 0 0 0 0 0 ++ ++ + + + + + + + + 0 0 ? 0 ? ? 0 0 ? ? 0 ? + 0 + + + ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 0 0 0 + ++ ++ + + ? + + + ? 0 ? 0 ? 0 0 + ? 0 0 0 0 0 0 0 0 0 +
Cairo University Specialized Pediatric Hospital,
C. difficille 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 0 0 0 0 0 0 0 0 0 0 0 0 0 ++ 0 Medication Consultation Unit, Clinical Pharmacy Dept.
Clostridum sp. ++ + 0 0 0 0 0 + + + + + + + + + + 0 0 + 0 0 0 0 0 0 0 0 + + ? + + + ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 0 0 0 + + + + + ? + + + + +/- + + + + + + 0 0 0 0 0 0 0 0 0 + + Data extracted from The Sanford® Guide to Antimicrobial Therapy
P. acnes ++ + ? ? ? ? ? + + + + + + + + + + 0 +/- 0 +/- +/- +/- 0 +/- ? ? + + + + + + ++ + + + + + + 0 + + + + + ? ? ? + ? ? + +/- +/- +/- +/- ? + + + + + + + + + + 0 0 0 0 0 0 +/- 0 0 0 0 0 Digital content update - January 2018 - Sanford Android App
www.pediamcu.com Designed and Edited by: Hossam A. Elgnainy, Clinical Pharmacist
Peptostreptococci ++ ++ 0 0 0 0 0 ++ ++ + + + + + + + + 0 0 + 0 + + 0 0 ? + + + + + + + + + + + + + + + + + + + + + ? ? 0 0 0 + + +/- +/- +/- ? + + + + + + + + + + + ? 0 0 0 0 0 0 + 0 +/- ?
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- HR Toolkit For Small and Medium Nonprofit Actors PDFDocument28 pagesHR Toolkit For Small and Medium Nonprofit Actors PDFsara elalfy100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Initial Data Base For Family Nursing PracticeDocument9 pagesInitial Data Base For Family Nursing PracticeAlyanna Crisologo100% (2)
- Abbas Basic Immunology 3eDocument7 pagesAbbas Basic Immunology 3ePatricia Snowden100% (1)
- Safe Motherhood ProgramDocument17 pagesSafe Motherhood ProgramNiel A.No ratings yet
- Skaggs Interviewing Guide (Employment)Document11 pagesSkaggs Interviewing Guide (Employment)sara elalfyNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 57Document14 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 57sarasjunk100% (1)
- Municipal Health Organizational ChartDocument10 pagesMunicipal Health Organizational ChartJPJessiePaulNo ratings yet
- Values-Based Leadership - How Our Personal Values Impact The Workp PDFDocument9 pagesValues-Based Leadership - How Our Personal Values Impact The Workp PDFsara elalfyNo ratings yet
- Competitive Salaries & Incentive Schemes: Read MoreDocument3 pagesCompetitive Salaries & Incentive Schemes: Read Moresara elalfyNo ratings yet
- Examples Poor Organizational Structure Companies 61056.html PDFDocument4 pagesExamples Poor Organizational Structure Companies 61056.html PDFsara elalfy0% (1)
- 8 Types of Organisational Structures Their Advantages and Disadvantages PDFDocument14 pages8 Types of Organisational Structures Their Advantages and Disadvantages PDFsara elalfyNo ratings yet
- Job Analysis Interview Questions 2Document3 pagesJob Analysis Interview Questions 2sara elalfy0% (1)
- Pharmacy Resume Review Rubric PDFDocument3 pagesPharmacy Resume Review Rubric PDFsara elalfyNo ratings yet
- HR Toolkit For Small and Medium Nonprofit Actors PDFDocument28 pagesHR Toolkit For Small and Medium Nonprofit Actors PDFsara elalfyNo ratings yet
- Job DescriptionDocument3 pagesJob Descriptionsara elalfyNo ratings yet
- Job DescriptionDocument3 pagesJob Descriptionsara elalfyNo ratings yet
- Copy of Interview Evaluation FormDocument2 pagesCopy of Interview Evaluation Formsara elalfyNo ratings yet
- Copy of Interview Evaluation FormDocument2 pagesCopy of Interview Evaluation Formsara elalfyNo ratings yet
- CDC's Appendix B-Pink Book - Vaccines - Ingredient ListDocument4 pagesCDC's Appendix B-Pink Book - Vaccines - Ingredient ListmickelleNo ratings yet
- p3085 PDFDocument1 pagep3085 PDFEivon Eyaf Love TormonNo ratings yet
- Biology Investigation 2 PDFDocument15 pagesBiology Investigation 2 PDFNoella RalteNo ratings yet
- Care ProspectusDocument50 pagesCare ProspectusJeya LakshmiNo ratings yet
- Peace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationDocument6 pagesPeace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- TS Vaccine Stability Table PDFDocument17 pagesTS Vaccine Stability Table PDFDimitrios DalagiorgosNo ratings yet
- Recording Form 1: Masterlist of Grade 1 Students: School-Based ImmunizationDocument1 pageRecording Form 1: Masterlist of Grade 1 Students: School-Based ImmunizationJesse100% (1)
- Rescue DiverDocument2 pagesRescue DiverPatrick SweetNo ratings yet
- Limit of FlocullationDocument7 pagesLimit of FlocullationPharma 24No ratings yet
- Khalequ Zaman, Sheikh Farzana Zaman, Farzana Zaman, Asma Aziz, Sayeed-Bin Faisal, Magali Traskine, MD Ahsan Habib, Javier Ruiz-Guiñazú, Dorota BorysDocument9 pagesKhalequ Zaman, Sheikh Farzana Zaman, Farzana Zaman, Asma Aziz, Sayeed-Bin Faisal, Magali Traskine, MD Ahsan Habib, Javier Ruiz-Guiñazú, Dorota Borysputri dewiNo ratings yet
- Dog Release - Consultation FormDocument5 pagesDog Release - Consultation Formapi-242369647No ratings yet
- Role of The Circulatory System in The Body's Defence MechanismsDocument15 pagesRole of The Circulatory System in The Body's Defence MechanismsArash Halim67% (3)
- Cat Vaccine Initial Kitten Vaccination (At or Under 16 Weeks) Initial Adult Cat Vaccination (Over 16 Weeks) Booster Recommendation CommentsDocument1 pageCat Vaccine Initial Kitten Vaccination (At or Under 16 Weeks) Initial Adult Cat Vaccination (Over 16 Weeks) Booster Recommendation CommentsAbdlHameed FareedahNo ratings yet
- Vis RabiesDocument2 pagesVis RabiesSanjay KumarNo ratings yet
- NCPDocument10 pagesNCPRobin HaliliNo ratings yet
- Latihan UN B.inggrisDocument6 pagesLatihan UN B.inggrisShella KhoiriyahNo ratings yet
- Vaccination Essay FinalDocument2 pagesVaccination Essay Finalapi-285950168No ratings yet
- The Questionnaire To Survey The Level of Knowledge, Attitudes and Practices (KAPs)Document4 pagesThe Questionnaire To Survey The Level of Knowledge, Attitudes and Practices (KAPs)Venty Muliana SNo ratings yet
- 08 - Microorganisms and Their Effects On Living ThingsDocument5 pages08 - Microorganisms and Their Effects On Living ThingsMie IsaNo ratings yet
- The Role of Vaccination in Salmonella ControlDocument51 pagesThe Role of Vaccination in Salmonella ControlDr. Aja Ogboo Chikere100% (1)
- Typhoid Fever Follow-Up PDFDocument16 pagesTyphoid Fever Follow-Up PDFPlot BUnniesNo ratings yet
- Hester Inactiv IBD ND IB REODocument4 pagesHester Inactiv IBD ND IB REOwahyu haryantoNo ratings yet
- Antibiotics and Penicillin Allergy: Contra-Indicated Contra - Indicated Contra - IndicatedDocument1 pageAntibiotics and Penicillin Allergy: Contra-Indicated Contra - Indicated Contra - IndicatedJeferson BraxtonNo ratings yet
- NewbornDocument2 pagesNewbornonijinoNo ratings yet
- M.B.B.S D.Epi M.P.HDocument9 pagesM.B.B.S D.Epi M.P.HAbhijit DeyNo ratings yet