Professional Documents
Culture Documents
Patellofemoral/Chondromalacia Protocol: Anatomy and Biomechanics
Uploaded by
Ria PuputOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patellofemoral/Chondromalacia Protocol: Anatomy and Biomechanics
Uploaded by
Ria PuputCopyright:
Available Formats
Patellofemoral/Chondromalacia Protocol
Anatomy and Biomechanics
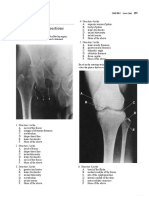
The knee is composed of two joints, the tibiofemoral and the
patellofemoral. The patellofemoral joint is made up of the patella (knee
cap) and the groove of cartilage on the femur in which it sits. The purpose
of the patella and the patellofemoral joint is to allow for greater force
development through the quadriceps muscle by creating a fulcrum
mechanism as the knee is extended. This joint is subject to tremendous
forces when the knee is repetitively loaded in flexion and extension during
sports and physical activity.
Normally the knee cap slides up and down following the natural track of
the groove in the middle of the femur. When the knee cap fails to slide up and down evenly in the
groove this can create irritation of the cartilage on the underside of the knee cap. There are many
potential reasons as to why the patella would not accurately track within its groove. One reason is the
alignment of the bones of the leg and foot. Subtle abnormalities in alignment and boney structure can
cause the patella to sit in a position in which it will create uneven pressure and wear within the groove.
Another potential cause of increased load on the joint is improper pull and
tension from the connective tissue that surrounds the joint and the muscles
that control the movement of the patella. Tight structures surrounding the
patella can cause it to slide toward the outside of its groove when the
quadriceps is contracted. These tight structures also cause the patella to be
compressed into the groove as it slides up and down. Imbalance in strength
between the four heads of the quadriceps and weakness throughout the
muscles of the hip can also cause the patella to be improperly positioned
during weight bearing activities.
When the cartilage on the under surface of the knee cap has been
continually irritated for a long period of time it can begin to wear down and
degenerate. This condition is known as chondromalacia of the patella. This degeneration may be
responsible for the crunching and grinding noise heard in some patients when the knee is bent and
straightened. When significant chondromalacia is present this may undermine the knee’s ability to
respond well to conservative treatments.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 1
in Clinical Collaboration with South Shore Orthopedics
Treatment Options
The severity, and resulting pain and dysfunction, of patellofemoral syndrome and chondromalacia varies
greatly in patients that are affected by it. In each case the physician and his or her staff evaluates the
individual case and determines the best plan of care for the patient. A period of rest followed by activity
modification may be enough to fix some cases. Use of anti-inflammatory medication and ice may also
be recommended. Active patients may be recommended to wear a brace that supports the knee cap
during activity. The physician and his or her staff may also ask the patient to undergo a course of
physical therapy to address the underlying mechanical causes of patellofemoral joint stress. If
conservative measures are unsuccessful in reducing pain and restoring function your physician may
discuss the potential need for arthroscopic surgery in rare cases. Recovery time from this injury is
different in each case. Your individual time table for return to activities will be discussed by your
physician and or physical therapist.
Relative Rest
Regardless of the specific mechanism (alignment, weakness, etc) patellofemoral syndrome is always
caused by the overloading of the patellofemoral joint. As the pain, inflammation and underlying cause
of the patellofemoral syndrome are treated the physician and/or physical therapist will likely
recommend that the patient refrain from participation in the activities that most provide stress to
injured joint. This does not always mean that the patient must stop all exercise. There are often forms
of exercise in which patellofemoral forces are reduced enough to allow for the patient to continue to
exercise while recovering. The patient should consult with the physician and/or physical therapist to
determine individualized exercise guidelines and restrictions.
Rehabilitation Philosophy
Physical therapy is often recommended for treatment of pain and dysfunction associated with
patellofemoral syndrome and chondromalacia of the patella. The physical therapist will evaluate the
patient’s mobility, flexibility and strength with the purpose of determining the underlying cause of the
abnormal stress on the patella. The patient will be counseled on which activities he or she can safely
continue and which should be avoided. The physical therapist will teach the patient the proper
exercises to reduce patellofemoral stress. In most cases this will include strengthening muscles about
the hip and knee that are weak and stretching ones that are tight.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 2
in Clinical Collaboration with South Shore Orthopedics
Rehabilitation
**The following is an outlined progression for rehab. Advancement from phase to phase as well as
specific exercises performed should be based on each individual patient’s case and sound clinical
judgment by the rehab professional. **
Phase 1 (Acute Phase)
Goals
Control Pain and Inflammation
Begin Pain Free Flexibility Exercises
Establish Quadriceps Activation
Establish Pain Free Knee ROM
Recommended Exercises
Range of Motion and Flexibility
Cycle with Minimal Resistance (if pain free)
Heel Slides (in pain free arc)
Lower Extremity Stretching (based on individual assessment)
Rectus Femoris
IT Band
Hamstring
Hip Rotators
Gastroc
Strength
Quad Sets (intensity and flexion angle guided by pain)
Guidelines
Perform range of motion exercises daily. Do 2-3 sets of 15-20 Reps. Perform stretching program daily.
Hold stretches for 30 seconds and perform 2-3 repetitions of each.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 3
in Clinical Collaboration with South Shore Orthopedics
Phase 2 (Sub-acute Phase A)
Goals
Continued Protection of Injured Joint
Continue to Improve Flexibility
Begin to Strengthen Areas of Weakness/Instability
Recommended Exercises
Range of Motion and Flexibility
Cycle (slow progression of resistance)
Continue Flexibility From Phase 1
Strength
Begin Open Chain Strengthening (based on strength assessment)
Knee Extension (SAQ, If painful use LAQ in painfree arc)
Straight Leg Raise
Hip Abduction
Hip Extensors
Hip External Rotators
Hamstring Curls
Guidelines
Perform stretching program daily. Hold stretches for 30 seconds and perform 2-3 repetitions of each.
Cardio program should be performed no more that 3-5 times a week for 20-35 minutes.
Perform strengthening exercises daily. Do 2-3 sets of 15-20 Reps.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 4
in Clinical Collaboration with South Shore Orthopedics
Phase 3 (Sub-acute Phase B)
Goals
Continue to Avoid Exacerbation of Symptoms
Continue to Maximize Return of Strength and Flexibility
Establish Closed Chain Strength and Stability
Recommended Exercises
Range of Motion and Flexibility
Continue Cycle
Continue Lower Extremity Stretching from Phase 1 and 2
Cardio
Cycle with Progressive Resistance
Elliptical (if pain free)
Swimming
Strengthening
Continue Progression of Open Chain Program with Ankle Weights
Can Add Gym Equipment (Leg Press, Ham Curl, Multi-Hip)
Squats to 90⁰ (Stress Pain Free Range and Proper Frontal/Sagittal Plane Mechanics)
Step Up Progressions (Forward Step Ups, Lateral Step Ups) *Forward Step Downs are not recommended due
to increased patella femoral load*
Pain Free Closed Chain Hip Strengthening
Guidelines
Perform stretching program daily. Hold stretches for 30 seconds and perform 2-3 repetitions of each.
Cardio program should be performed no more that 3-5 times a week for 20-45 minutes.
Perform strengthening exercises 3 times a week. Do 2-3 sets of 15-20 Reps.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 5
in Clinical Collaboration with South Shore Orthopedics
Phase 4 (Return to Sport/Activity Phase)
Goals
Continue to Avoid Patella Femoral Overload
Progress with Single Leg Strengthening
Achieve Adequate Strength and Flexibility to Return to Activity
Recommended Exercises
Flexibility
Continue Daily Stretching
Cardio
Continue Cycle, Elliptical, Swimming
Return to Running Progression (outlined by Physician or Physical Therapist)
Strengthening
Continue SLR Program and Gym Equipment Progression
Continue Step-Up Progressions (lateral step-ups, cross over step-ups) *Forward Step Downs are not
recommended due to increased patella femoral load*
Static Lunge
Lateral Lunge
Progressive Single Leg Strengthening (single leg squat, split squat, single leg dead lift)
Return to Sport
Work with Physician or Physical Therapist to Outline Progressive Return to Sport
Guidelines
Perform stretching program daily. Hold stretches for 30 seconds and perform 2-3 repetitions of each.
Cardio program should be progressed in preparation for return to sport.
Perform strengthening exercises 3 times a week. Do 2-3 sets of 15-20 Reps.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 6
in Clinical Collaboration with South Shore Orthopedics
Recommended
Phase Emphasis Guidelines
Exercises
Phase 1 *Control Pain and ROM and Flexibility *ROM Daily 2-3 sets of 15-20
Acute Phase Inflammation Cycle (if pain free motion) Reps
*Re-establish Normal Heel Slides (in pain free arc) *Stretching Program Daily 2-3
ROM Lower Extremity Stretching Repetitions of 30 Seconds
*Establish Quadriceps • Rectus Femoris
Activation • IT Band
*Begin Pain Free • Hamstring
Flexibility Program • Hip Rotators
• Gastroc
*based on individual assessment
Strength
Quad Sets
*intensity and flexion angle guided by pain
Phase 2 * Continued ROM and Flexibility * Stretching Program Daily 2-
Sub-acute Protection of Injured Cycle (slow progression of resistance) 3 Repetitions of 30 Seconds
Phase A Joint Continue Flexibility From Phase 1 *Cardio program should be
*Continue to Improve performed no more that 3-5
Flexibility Strength times a week for 20-35
*Begin to Strengthen Begin Open Chain Strengthening minutes.
Areas of • Knee Extension (SAQ, If painful use LAQ *Perform strengthening
Weakness/Instability in painfree arc) exercises daily 2-3 sets of 15-
• Straight Leg Raise 20 Reps
• Hip Abduction
• Hip Extensors
• Hip External Rotators
• Hamstring Curls
*based on individual assessment
Phase 3 * Continue to Avoid Flexibilty * Stretching Program Daily 2-
Sub-acute Exacerbation of Continue Lower Extremity Stretching from 3 Repetitions of 30 Seconds
Phase B Symptoms Phase 1 and 2 *Continue to Stress Proper
*Continue to Gait
Maximize Return of Cardio * Cardio program should be
Strength and Cycle with Progressive Resistance performed no more that 3-5
Flexibility Elliptical (if pain free) times a week for 20-45
*Establish Closed Swimming minutes.
Chain Strength and *Perform strengthening
Stability Strengthening exercises 3 times a week 2-3
Progress OKC Program with Ankle Weights sets of 15-20 Reps.
Can Add Gym Equipment
Squats to 90⁰ (Stress Pain Free Range)
Step Up Progressions (Forward Step Ups,
Lateral Step Ups) *Forward Step Downs are not
recommended due to increased patella femoral
load*
Pain Free Closed Chain Hip Strengthening
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 7
in Clinical Collaboration with South Shore Orthopedics
Phase 4 * Continue to Avoid Flexibility * Stretching Program Daily 2-
Sport Specific Patella Femoral Continue Daily Stretching 3 Repetitions of 30 Seconds
Phase Overload *Cardio program should be
*Progress with Single Cardio progressed in preparation for
Leg Strengthening Cycle, Elliptical, Swimming return to sport.
*Achieve Adequate Begin Return to Running Progression *Perform strengthening
Strength and exercises 3 times a week. Do
Flexibility to Return to Strengthening 2-3 sets of 15-20 Reps
Activity Continue OKC Program
Continue Gym Equipment Progression
Continue Step-Up Progressions (lateral step-
ups, cross over step-ups) *Forward Step Downs
are not recommended due to increased patella
femoral load*
Static Lunge
Lateral Lunge
Progressive Single Leg Strengthening (single leg
squat, split squat, single leg dead lift)
Return to Sport
Outlined by PT or MD
*Reviewed by Michael Geary, MD
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 8
in Clinical Collaboration with South Shore Orthopedics
You might also like
- The Whartons' Strength Book: Lower Body: Total Stability for Upper Legs, Hips, Trunk, Lower Legs, Ankles, and FeetFrom EverandThe Whartons' Strength Book: Lower Body: Total Stability for Upper Legs, Hips, Trunk, Lower Legs, Ankles, and FeetRating: 3 out of 5 stars3/5 (3)
- Patellofemoral/Chondromalacia Protocol: Anatomy and BiomechanicsDocument8 pagesPatellofemoral/Chondromalacia Protocol: Anatomy and BiomechanicsGirijashankar KhuntiaNo ratings yet
- The Whartons' Strength Book: Upper Body: Total Stability for Shoulders, Neck, Arm, Wrist, and ElbowFrom EverandThe Whartons' Strength Book: Upper Body: Total Stability for Shoulders, Neck, Arm, Wrist, and ElbowRating: 5 out of 5 stars5/5 (1)
- Hip OA Rehab: A 4-Phase Guide to RecoveryDocument7 pagesHip OA Rehab: A 4-Phase Guide to RecoveryPaul Radulescu - FizioterapeutNo ratings yet
- Exercises for Those Who Suffer a Disk HerniaFrom EverandExercises for Those Who Suffer a Disk HerniaRating: 5 out of 5 stars5/5 (2)
- Lumbar Disc HerniationDocument8 pagesLumbar Disc Herniationandra_scooterNo ratings yet
- ACL Non-Operative ManagmentDocument10 pagesACL Non-Operative ManagmentHammad -ullahNo ratings yet
- The Athlete's Guide to Stretching: Increasing Flexibility For Inury Prevention And RehabilitationFrom EverandThe Athlete's Guide to Stretching: Increasing Flexibility For Inury Prevention And RehabilitationRating: 4 out of 5 stars4/5 (1)
- Rotator Cuff Impingement/Tendinopathy Rehab GuideDocument8 pagesRotator Cuff Impingement/Tendinopathy Rehab GuidemadaleenNo ratings yet
- HK11 Jumpers KneeDocument7 pagesHK11 Jumpers KneeDestinee LegendsNo ratings yet
- Dynamic Stretching: The Revolutionary New Warm-up Method to Improve Power, Performance and Range of MotionFrom EverandDynamic Stretching: The Revolutionary New Warm-up Method to Improve Power, Performance and Range of MotionRating: 5 out of 5 stars5/5 (1)
- Tennis Elbow RehabDocument8 pagesTennis Elbow RehabDarren Willis100% (2)
- Power Flex Stretching - Super Flexibility and Strength for peak performanceFrom EverandPower Flex Stretching - Super Flexibility and Strength for peak performanceRating: 3 out of 5 stars3/5 (3)
- Treatment: Home TreatmentsDocument3 pagesTreatment: Home TreatmentsDhimas Reyhan Putra SayudhaNo ratings yet
- Frozen Shoulder GuideDocument8 pagesFrozen Shoulder GuidefriskaNo ratings yet
- DYNAMIC LUMBAR STABILIZATION TRAINING Dean Farwood, P.T.Document5 pagesDYNAMIC LUMBAR STABILIZATION TRAINING Dean Farwood, P.T.Luis Eduardo Barbosa OrtegaNo ratings yet
- Physical Fitness Notes Second AssessmentDocument116 pagesPhysical Fitness Notes Second AssessmentElena JordanovaNo ratings yet
- How to Treat a Sprained AnkleDocument4 pagesHow to Treat a Sprained AnkleSakthi Annamalai.cNo ratings yet
- Quadriceps Muscle Strain GuideDocument16 pagesQuadriceps Muscle Strain GuideAZOZ 19No ratings yet
- A Weighty Subject: The Ergonomics of Resistance TrainingDocument4 pagesA Weighty Subject: The Ergonomics of Resistance TrainingmailbabuNo ratings yet
- Trunk Stabilization ProgramDocument20 pagesTrunk Stabilization ProgramLate ArtistNo ratings yet
- North American Spine Society Public Education SeriesDocument12 pagesNorth American Spine Society Public Education SeriesVanitha Ratha KrishnanNo ratings yet
- Patella TendonitisDocument43 pagesPatella Tendonitisvijkris1985100% (2)
- Training System For Enhancing Athletic Performance Al VermeilDocument165 pagesTraining System For Enhancing Athletic Performance Al Vermeilxaviermay100% (7)
- Effective Martial Arts - Training With No Equipment or Partner Vol 2 - Ageless Flexibility and Joint MobilityDocument74 pagesEffective Martial Arts - Training With No Equipment or Partner Vol 2 - Ageless Flexibility and Joint MobilityTamil Vanan NNo ratings yet
- 2010 Rehabilitation of Ankle and FootDocument11 pages2010 Rehabilitation of Ankle and FootRodrigo GarcíaNo ratings yet
- Resistance Exercise For Impaired Muscle Performance: Chapter No 6 DR - Iqra Ashraf DPT, MS-MSKDocument29 pagesResistance Exercise For Impaired Muscle Performance: Chapter No 6 DR - Iqra Ashraf DPT, MS-MSKSania SaeedNo ratings yet
- Swimmer's Shoulder - StatPearlsDocument4 pagesSwimmer's Shoulder - StatPearlsFillipe AgraNo ratings yet
- نسخة light blue creative modern medical clinic presentationDocument33 pagesنسخة light blue creative modern medical clinic presentationFaresNo ratings yet
- Acromioclavicular Joint Injuries and Physical Therapy ManagementDocument12 pagesAcromioclavicular Joint Injuries and Physical Therapy ManagementSereinNo ratings yet
- Hamstring MuscleDocument8 pagesHamstring MuscleMuhamad SdeqNo ratings yet
- Manual Muscle TestingDocument29 pagesManual Muscle Testingcreat1No ratings yet
- Connecting the Core Muscles for Stability and PerformanceDocument5 pagesConnecting the Core Muscles for Stability and PerformanceManos GladxNo ratings yet
- Knee Arthroscopy Meniscectomy Recovery GuideDocument9 pagesKnee Arthroscopy Meniscectomy Recovery Guidebayan salahNo ratings yet
- Strong As An Ox Olympic Weightlifting Program Manual PDFDocument32 pagesStrong As An Ox Olympic Weightlifting Program Manual PDFJonathan Schroeder80% (5)
- Low Back Health through Stabilization ExercisesDocument8 pagesLow Back Health through Stabilization ExercisesDavid StadkindNo ratings yet
- Patellar Tendon Rupture and RehabilitationDocument4 pagesPatellar Tendon Rupture and RehabilitationdedsnetNo ratings yet
- Physiotherapy For Quadriceps Tendon TearDocument2 pagesPhysiotherapy For Quadriceps Tendon TearenadNo ratings yet
- Spine Stabilization PowerpointDocument87 pagesSpine Stabilization PowerpointALLAN COSTA MONTEIRONo ratings yet
- Lower Crossed SyndromeDocument8 pagesLower Crossed SyndromeThaseen75% (4)
- Sports Injuries in UE - Shoulder - Part 3.Document87 pagesSports Injuries in UE - Shoulder - Part 3.salmankhan09215No ratings yet
- Preventing Dance Injuries Through Proper Technique and Self-CareDocument12 pagesPreventing Dance Injuries Through Proper Technique and Self-CareKashima KotaroNo ratings yet
- Hamstring Exercise ProgressionDocument15 pagesHamstring Exercise ProgressionFrancisco De VelascoNo ratings yet
- Therapeutic Gymnasium PDFDocument45 pagesTherapeutic Gymnasium PDFPrabhat SharmaNo ratings yet
- Post-Op Hip Active-Assisted Exercise ProgramDocument3 pagesPost-Op Hip Active-Assisted Exercise ProgramAhmad AfiyyuddinNo ratings yet
- Patellectomy RehabDocument29 pagesPatellectomy RehabKhateeja Tul KubraNo ratings yet
- Frozen ShoulderDocument6 pagesFrozen ShoulderanumolNo ratings yet
- Patellar Tendonitis TreatmentDocument7 pagesPatellar Tendonitis TreatmentRatnaPrasadNalamNo ratings yet
- Prevención de Pubalgia Atlética y Dolor Crónico en La Ingle en Jugadores de FútbolDocument4 pagesPrevención de Pubalgia Atlética y Dolor Crónico en La Ingle en Jugadores de FútbolFloren Martil GuijarroNo ratings yet
- Keeping Your Shoulders HealthyDocument38 pagesKeeping Your Shoulders Healthyxyz84No ratings yet
- Long Thoracic Nerve PalsyDocument2 pagesLong Thoracic Nerve PalsyJose Luis Tabueña OrtegaNo ratings yet
- 14 Exercises That Can Worsen HealthDocument4 pages14 Exercises That Can Worsen HealthNmorah QandilNo ratings yet
- Coastal Iliotibial Band 2014Document2 pagesCoastal Iliotibial Band 2014lesterbsbNo ratings yet
- Fasa Akut Selepas PembedahanDocument4 pagesFasa Akut Selepas Pembedahanchris waddleNo ratings yet
- Post Op Cervical Fusion PDFDocument3 pagesPost Op Cervical Fusion PDFNICOLÁS ANDRÉS AYELEF PARRAGUEZNo ratings yet
- How To Maintain Good Knee Joint Health 20160708Document6 pagesHow To Maintain Good Knee Joint Health 20160708rarNo ratings yet
- StretchingDocument32 pagesStretchingTofan Ana88% (8)
- Off-Campus Placement ProjectDocument4 pagesOff-Campus Placement Projectapi-488042467No ratings yet
- Short-Term Effects of Mobilization-With-Movement (MWM) and Auto-Mwm Application in Recreational Runners With Iliotibial Band SyndromeDocument8 pagesShort-Term Effects of Mobilization-With-Movement (MWM) and Auto-Mwm Application in Recreational Runners With Iliotibial Band SyndromeRia PuputNo ratings yet
- ITband Exercises PDFDocument2 pagesITband Exercises PDFShashNo ratings yet
- RPW Shockwave Therapy: Scientific Studies OverviewDocument38 pagesRPW Shockwave Therapy: Scientific Studies OverviewRia Puput100% (1)
- ITBSReview Article RLBRSMFPMR2011Document13 pagesITBSReview Article RLBRSMFPMR2011Ria PuputNo ratings yet
- Low Back Pain: Information For PatientsDocument8 pagesLow Back Pain: Information For PatientsShibli RahmanNo ratings yet
- 0207 ProlotherapyDocument36 pages0207 ProlotherapyRia PuputNo ratings yet
- Effect of Hip Abductor Strengthening Among Non-Professional Cyclists With Iliotibial Band Friction SyndromeDocument11 pagesEffect of Hip Abductor Strengthening Among Non-Professional Cyclists With Iliotibial Band Friction SyndromeRia PuputNo ratings yet
- Closed kinetic exercises improve knee proprioceptionDocument3 pagesClosed kinetic exercises improve knee proprioceptionRia PuputNo ratings yet
- ACR OA Guideline Development Process Knee and HipDocument8 pagesACR OA Guideline Development Process Knee and HipAulia Satria BimantaraNo ratings yet
- Constraining Kinematics During Single-Leg Squats and Step-Ups CanDocument56 pagesConstraining Kinematics During Single-Leg Squats and Step-Ups CanRia PuputNo ratings yet
- Osteoarthritis of The Knee Information Booklet PDFDocument36 pagesOsteoarthritis of The Knee Information Booklet PDFRia PuputNo ratings yet
- Effectiveness of Combined Chain Exercises On PainDocument11 pagesEffectiveness of Combined Chain Exercises On PainJulenda CintarinovaNo ratings yet
- Corrective Exercises in The Treatment of Scoliosis PDFDocument21 pagesCorrective Exercises in The Treatment of Scoliosis PDFRia PuputNo ratings yet
- Home Exercise Program for ScoliosisDocument6 pagesHome Exercise Program for ScoliosisChris SakeNo ratings yet
- Foot and Ankle Ability Measure PDFDocument3 pagesFoot and Ankle Ability Measure PDFFirda Dwi AzizahNo ratings yet
- Static Balance Normsin ChildrenDocument8 pagesStatic Balance Normsin ChildrenRia PuputNo ratings yet
- Ijpr 2018 145Document7 pagesIjpr 2018 145Ria PuputNo ratings yet
- SimpleSet Exercise Program Grid Template SampleDocument2 pagesSimpleSet Exercise Program Grid Template SampleRia PuputNo ratings yet
- Hydrotherapy For LBP FixxDocument22 pagesHydrotherapy For LBP FixxRia PuputNo ratings yet
- 1062 6050 555 16Document10 pages1062 6050 555 16Ria PuputNo ratings yet
- A 4 Shoulder Impinge Appendix 5Document8 pagesA 4 Shoulder Impinge Appendix 5NatuNo ratings yet
- Chest Physiotherapy in Intensive Care Unit (ICU) PDFDocument399 pagesChest Physiotherapy in Intensive Care Unit (ICU) PDFGuillermo Sasso Pacheco83% (6)
- BiomekanikDocument16 pagesBiomekanikRia PuputNo ratings yet
- Hortatory ExpositionDocument7 pagesHortatory ExpositionRia PuputNo ratings yet
- Cat Muscles Study GuideDocument28 pagesCat Muscles Study Guidearvinric100% (1)
- Peranan Fisioterapi Pada Kasus Hallux Valgus (Bunion) Dengan Intervensi NMT Dan Strengthening Untuk Mengurangi NyeriDocument7 pagesPeranan Fisioterapi Pada Kasus Hallux Valgus (Bunion) Dengan Intervensi NMT Dan Strengthening Untuk Mengurangi NyeriShalmaa LarasatiNo ratings yet
- Medial Patellofemoral Ligament MPFLDocument8 pagesMedial Patellofemoral Ligament MPFLImran AshrafNo ratings yet
- Screen Knee Issues for Potential Serious ConditionsDocument120 pagesScreen Knee Issues for Potential Serious Conditionssayles4174100% (1)
- Medical Tests, Signs & Maneuvers Guide: Achilles Squeeze TestDocument12 pagesMedical Tests, Signs & Maneuvers Guide: Achilles Squeeze TestWaqar AhmedNo ratings yet
- The Great and Mysterious ButtDocument6 pagesThe Great and Mysterious ButtaggybongNo ratings yet
- The Asics Natural Running GuideDocument15 pagesThe Asics Natural Running GuideJavalinoshopNo ratings yet
- Ligamento Cruzado Doble FasciculoDocument16 pagesLigamento Cruzado Doble FasciculoAuusto CórdobaNo ratings yet
- Snell Lower Limb Questions AnswersDocument6 pagesSnell Lower Limb Questions AnswersBen95% (37)
- ACIIDA - SP - 1 Direct Anterior ApproachDocument30 pagesACIIDA - SP - 1 Direct Anterior ApproachJayjeet BhoiteNo ratings yet
- Foot DropDocument30 pagesFoot Dropdr_s_ganesh100% (1)
- Genu ValgumDocument3 pagesGenu ValgumBiniam AssefaNo ratings yet
- Foot Orthoses and Other Forms of Conservative Foot CareDocument262 pagesFoot Orthoses and Other Forms of Conservative Foot CareJorge Aguirre Gonzalez100% (1)
- Muscle Flash CardsDocument127 pagesMuscle Flash Cardsjoelh9100% (3)
- Foot Anatomy and PhysiologyDocument9 pagesFoot Anatomy and PhysiologyMarta BłaszczykNo ratings yet
- Treatment and Rehabilitation of Fractures (Stanley Hoppenfeld)Document1 pageTreatment and Rehabilitation of Fractures (Stanley Hoppenfeld)小蓮花No ratings yet
- Squat TestDocument5 pagesSquat TestLuis Espinoza Aramburú100% (1)
- Most Common Surfing Injuries and Accidents - SurflineDocument2 pagesMost Common Surfing Injuries and Accidents - Surflineapi-549909228No ratings yet
- Physical Examination of Knee Ligament Injuries: Review ArticleDocument8 pagesPhysical Examination of Knee Ligament Injuries: Review ArticlenuriajunitNo ratings yet
- Arteries of Lower LimbDocument6 pagesArteries of Lower LimbAlli NdahuraNo ratings yet
- Department of Anatomy Hasanuddin University: Dr. Hasan NyambeDocument57 pagesDepartment of Anatomy Hasanuddin University: Dr. Hasan NyambeMaksi YantoNo ratings yet
- Knee Pain Internal ArtsDocument7 pagesKnee Pain Internal ArtsGabriel PedrozaNo ratings yet
- Ortho TestsDocument23 pagesOrtho TestsAMIRSAM SHAHHOSSEININo ratings yet
- Anatomy of the Lower LimbsDocument84 pagesAnatomy of the Lower LimbsAlviraNo ratings yet
- TFC Seminar Manual (Online)Document5 pagesTFC Seminar Manual (Online)Emanuel SortinoNo ratings yet
- The Ankle in Football - 2014 PDFDocument326 pagesThe Ankle in Football - 2014 PDFRobert TănăsescuNo ratings yet
- Anatomy, Bony Pelvis and Lower Limb, Leg Bones: February 2019Document8 pagesAnatomy, Bony Pelvis and Lower Limb, Leg Bones: February 2019Chess NutsNo ratings yet
- The Human Foot Anatomy, Deformities and Treatment A Volume Containing A Complete and Comprehensive Description of The Anatomy of The FootDocument402 pagesThe Human Foot Anatomy, Deformities and Treatment A Volume Containing A Complete and Comprehensive Description of The Anatomy of The FootEjup MajollariNo ratings yet
- Case PresentationDocument19 pagesCase PresentationIbad Ur RehmanNo ratings yet
- Bones of Upper and Lower Limbs - RevisionDocument15 pagesBones of Upper and Lower Limbs - RevisionChess Nuts100% (1)
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.From EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Rating: 4 out of 5 stars4/5 (2)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Body by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekFrom EverandBody by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekRating: 4.5 out of 5 stars4.5/5 (84)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- Hero Maker: 12 Weeks to Superhero Fit: A Hollywood Trainer's REAL Guide to Getting the Body You've Always WantedFrom EverandHero Maker: 12 Weeks to Superhero Fit: A Hollywood Trainer's REAL Guide to Getting the Body You've Always WantedRating: 4 out of 5 stars4/5 (1)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- 7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassFrom Everand7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassRating: 4 out of 5 stars4/5 (2)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (95)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (781)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsFrom EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsRating: 4.5 out of 5 stars4.5/5 (7)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (110)
- SAS Training Manual: How to get fit enough to pass a special forces selection courseFrom EverandSAS Training Manual: How to get fit enough to pass a special forces selection courseRating: 4 out of 5 stars4/5 (3)
- Meat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesFrom EverandMeat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesRating: 3.5 out of 5 stars3.5/5 (8)
- Calisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysFrom EverandCalisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysRating: 3 out of 5 stars3/5 (5)
- The Calisthenics Codex: Fifty Exercises for Functional FitnessFrom EverandThe Calisthenics Codex: Fifty Exercises for Functional FitnessRating: 4 out of 5 stars4/5 (9)
- Calisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesFrom EverandCalisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesRating: 3 out of 5 stars3/5 (5)
- 7 Weeks to 50 Pull-Ups: Strengthen and Sculpt Your Arms, Shoulders, Back, and Abs by Training to Do 50 Consecutive Pull-UpsFrom Everand7 Weeks to 50 Pull-Ups: Strengthen and Sculpt Your Arms, Shoulders, Back, and Abs by Training to Do 50 Consecutive Pull-UpsRating: 3.5 out of 5 stars3.5/5 (2)
- Applied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthFrom EverandApplied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthNo ratings yet
- Deezify's Epic Workout Handbook: An Illustrated Guide to Getting SwoleFrom EverandDeezify's Epic Workout Handbook: An Illustrated Guide to Getting SwoleRating: 5 out of 5 stars5/5 (1)
- Beastmode Calisthenics: A Simple and Effective Guide to Get Ripped with Bodyweight TrainingFrom EverandBeastmode Calisthenics: A Simple and Effective Guide to Get Ripped with Bodyweight TrainingNo ratings yet