Professional Documents
Culture Documents
PIIS0140673620316056
Uploaded by
Isais NCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PIIS0140673620316056
Uploaded by
Isais NCopyright:
Available Formats
Articles
Immunogenicity and safety of a recombinant adenovirus
type-5-vectored COVID-19 vaccine in healthy adults aged
18 years or older: a randomised, double-blind, placebo-
controlled, phase 2 trial
Feng-Cai Zhu*, Xu-Hua Guan*, Yu-Hua Li, Jian-Ying Huang, Tao Jiang, Li-Hua Hou, Jing-Xin Li, Bei-Fang Yang, Ling Wang, Wen-Juan Wang,
Shi-Po Wu, Zhao Wang, Xiao-Hong Wu, Jun-Jie Xu, Zhe Zhang, Si-Yue Jia, Bu-Sen Wang, Yi Hu, Jing-Jing Liu, Jun Zhang, Xiao-Ai Qian, Qiong Li,
Hong-Xing Pan, Hu-Dachuan Jiang, Peng Deng, Jin-Bo Gou, Xue-Wen Wang, Xing-Huan Wang, Wei Chen
Summary
Background This is the first randomised controlled trial for assessment of the immunogenicity and safety of a Lancet 2020; 396: 479–88
candidate non-replicating adenovirus type-5 (Ad5)-vectored COVID-19 vaccine, aiming to determine an appropriate Published Online
dose of the candidate vaccine for an efficacy study. July 20, 2020
https://doi.org/10.1016/
S0140-6736(20)31605-6
Methods This randomised, double-blind, placebo-controlled, phase 2 trial of the Ad5-vectored COVID-19 vaccine was
See Comment page 448
done in a single centre in Wuhan, China. Healthy adults aged 18 years or older, who were HIV-negative and previous
*Contributed equally
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection-free, were eligible to participate and were
NHC Key Laboratory of Enteric
randomly assigned to receive the vaccine at a dose of 1 × 10¹¹ viral particles per mL or 5 × 10¹⁰ viral particles per mL, or Pathogenic Microbiology,
placebo. Investigators allocated participants at a ratio of 2:1:1 to receive a single injection intramuscularly in the arm. Jiangsu Provincial Center for
The randomisation list (block size 4) was generated by an independent statistician. Participants, investigators, and Disease Control and Prevention,
staff undertaking laboratory analyses were masked to group allocation. The primary endpoints for immunogenicity Nanjing, China (F-C Zhu MSc,
Prof J-X Li PhD, W-J Wang MSc,
were the geometric mean titres (GMTs) of specific ELISA antibody responses to the receptor binding domain (RBD) S-Y Jia MPH, Prof H-X Pan MSc,
and neutralising antibody responses at day 28. The primary endpoint for safety evaluation was the incidence of H-D Jiang BSc); Hubei Provincial
adverse reactions within 14 days. All recruited participants who received at least one dose were included in the Center for Diseases Control and
primary and safety analyses. This study is registered with ClinicalTrials.gov, NCT04341389. Prevention, Wuhan, China
(Prof X-H Guan PhD,
B-F Yang PhD, Z Wang MPH,
Findings 603 volunteers were recruited and screened for eligibility between April 11 and 16, 2020. 508 eligible X-A Qian MPH, Q Li MPH,
participants (50% male; mean age 39·7 years, SD 12·5) consented to participate in the trial and were randomly P Deng MPH); National Institute
assigned to receive the vaccine (1 × 10¹¹ viral particles n=253; 5 × 10¹⁰ viral particles n=129) or placebo (n=126). In the for Food and Drug Control,
Dongcheng, Beijing, China
1 × 10¹¹ and 5 × 10¹⁰ viral particles dose groups, the RBD-specific ELISA antibodies peaked at 656·5 (95% CI (Prof Y-H Li PhD, L Wang PhD,
575·2–749·2) and 571·0 (467·6–697·3), with seroconversion rates at 96% (95% CI 93–98) and 97% (92–99), X-H Wu MSc, J-J Liu MSc); Clinical
respectively, at day 28. Both doses of the vaccine induced significant neutralising antibody responses to live Trial Center, Zhongnan Hospital
SARS-CoV-2, with GMTs of 19·5 (95% CI 16·8–22·7) and 18·3 (14·4–23·3) in participants receiving 1 × 10¹¹ and of Wuhan University, Wuhan,
China (Prof J-Y Huang MD,
5 × 10¹⁰ viral particles, respectively. Specific interferon γ enzyme-linked immunospot assay responses post vaccination Prof X-H Wang MD); Beijing
were observed in 227 (90%, 95% CI 85–93) of 253 and 113 (88%, 81–92) of 129 participants in the 1 × 10¹¹ and 5 × 10¹⁰ Institute of Microbiology and
viral particles dose groups, respectively. Solicited adverse reactions were reported by 183 (72%) of 253 and 96 (74%) of Epidemiology, State Key
Laboratory of Pathogen and
129 participants in the 1 × 10¹¹ and 5 × 10¹⁰ viral particles dose groups, respectively. Severe adverse reactions were
Biosecurity, Beijing, China
reported by 24 (9%) participants in the 1 × 10¹¹ viral particles dose group and one (1%) participant in the 5 × 10¹⁰ viral (Prof T Jiang PhD, Y Hu PhD);
particles dose group. No serious adverse reactions were documented. Beijing Institute of
Biotechnology, Academy of
Military Medical Sciences,
Interpretation The Ad5-vectored COVID-19 vaccine at 5 × 10¹⁰ viral particles is safe, and induced significant immune
Beijing, China
responses in the majority of recipients after a single immunisation. (Prof L-H Hou PhD, S-P Wu PhD,
Prof J-J Xu PhD, Z Zhang PhD,
Funding National Key R&D Programme of China, National Science and Technology Major Project, and CanSino B-S Wang PhD, J Zhang PhD,
Prof W Chen PhD); CanSino
Biologics.
Biologics, Tianjin, China
(J-B Gou PhD); and Shanghai
Copyright © 2020 Elsevier Ltd. All rights reserved. Canming Medical Technology,
Shanghai, China
Introduction COVID-19 has now spread to 216 countries and (X-W Wang MD)
Correspondence to:
Severe acute respiratory syndrome coronavirus 2 territories. Large numbers of cases and deaths are
Prof Wei Chen, Beijing Institute
(SARS-CoV-2) has caused more than 12·1 million cases reported daily from Europe, the USA, Brazil, Russia, of Biotechnology, Fengtai,
of COVID-19 worldwide, resulting in 551 000 deaths and India, and many other countries.3,4 The current pandemic Beijing 100071, China
severe economic disruption.1,2 After the initial outbreak, has highlighted the need for effective preventive cw0226@foxmail.com
with more than 80 000 cases and 3000 deaths in China, solutions to reduce burden and spread of the disease. or
www.thelancet.com Vol 396 August 15, 2020 479
Articles
Prof Xing-Huan Wang,
Zhongnan Hospital of Wuhan Research in context
University, Wuhan 430071,
China Evidence before this study we removed the age cap for the recruitment of participants for
wangxinghuan@whu.edu.cn We searched PubMed on July 16, 2020, for clinical trial reports this phase 2 trial. Older individuals (ie, aged ≥55 years), many of
or with the terms “COVID-19” or “SARS-CoV-2”, “vaccine”, whom often have chronic illness, have a high risk of serious
Prof Feng-Cai Zhu, Jiangsu and “clinical trial”. Using the same terms, we also searched illness and death associated with SARS-CoV-2 infection;
Provincial Center of Disease ClinicalTrials.gov for unpublished trials of COVID-19 vaccines. thus, they are an important target population for a COVID-19
Control and Prevention,
Except for the results of our earlier phase 1 study with the vaccine. Our results suggest a single-dose immunisation
Nanjing 210009, China
jszfc@vip.sina.com adenovirus type-5 (Ad5)-vectored vaccine and a phase 1 clinical schedule of Ad5-vectored COVID-19 vaccine at 5 × 10¹⁰ viral
trial with an mRNA vaccine (mRNA-1273) done in a small particles is an appropriate regimen for healthy adults.
number of participants, no other COVID-19 vaccine data from Compared with the younger population, we found older people
clinical trials have been reported. We found registered trials to have a significantly lower immune response, but higher
with 11 candidate COVID-19 vaccines at ClinicalTrials.gov, tolerability, to the Ad5-vectored COVID-19 vaccine. Therefore,
including three recombinant protein-based vaccines, two viral an additional dose might be needed to induce a better immune
vector-based vaccines, one DNA vaccine, two mRNA vaccines, response in the older population, and this will be evaluated in a
two inactivated virus vaccines, and one autologous dendritic phase 2b trial.
cell-based vaccine loaded with antigens from severe acute
Implications of all the available evidence
respiratory syndrome coronavirus 2 (SARS-CoV-2). The majority
Evidence from this phase 2 study indicates the candidate
of the trials registered were in early phases; only ChAdOx1
Ad5-vectored COVID-19 vaccine has a good safety profile,
nCoV-19 developed by the University of Oxford (Oxford, UK) is
with only mild, transient adverse events related to vaccination
going to be evaluated in a phase 3 trial.
and no serious adverse events. Single-dose immunisation with
In the previously reported open-label, non-randomised, phase 1 the vaccine induced rapid onset of immune responses within
trial, we found that the Ad5-vectored COVID-19 vaccine was 14 days and significant humoral and cellular immune responses
tolerable and immunogenic in healthy adults. One dose of the within 28 days in the majority of the recipients. We are
vaccine induced rapid specific T-cell and humoral responses by planning an international multicentre, randomised, double-
14 days. blind, controlled phase 3 effectiveness trial to further evaluate
Added value of this study the efficacy of the vaccine. We are in the midst of a global
This study provides more evidence for the immunogenicity and COVID-19 pandemic; thus, timely sharing of the results of
safety of the Ad5-vectored COVID-19 vaccine in a larger clinical trials with candidate vaccines is critical.
population. To assess the vaccine in a more diverse population,
As long as there is a COVID-19 epidemic in one area in reactions. We therefore carried forward the phase 2 trial
the world, there is a risk of a pandemic. with only the 5 × 10¹⁰ and 1 × 10¹¹ viral particles doses of
Unlike typical vaccine development, which often takes the candidate vaccine, aiming to further evaluate the
decades, developing a vaccine to prevent COVID-19 has immunogenicity and safety in a larger population, and to
become a race between humans and the virus.5 Many determine an appropriate dose for the efficacy study.
countries have accelerated the process of clinical trials to
determine an effective and safe vaccine to prevent Methods
COVID-19 and influence the course of the current Study design and participants
pandemic.6,7 Currently, about 250 candidate vaccines This randomised, double-blind, placebo-controlled,
against SARS-CoV-2 are in development worldwide, phase 2 trial of the Ad5-vectored COVID-19 vaccine was
including mRNA vaccines, replicating or non-replicating done in a single centre in Wuhan (Hubei province,
viral vectored vaccines, DNA vaccines, autologous den China). The study was done in accordance with the
dritic cell-based vaccine, and inactive virus vaccines.8 To Declaration of Helsinki and Good Clinical Practice.
date, at least 17 of these vaccine candidates are under An independent data safety monitoring board was
evaluation in clinical trials. established before the start of the trial to provide
In March 2020, we did a single-centre, open-label, oversight of the safety data during the study. The trial
non-randomised, first-in-human phase 1 trial9 with protocol was reviewed and approved by the National
CanSino Biologics’ (Tianjin, China) adenovirus type-5 Medical Products Administration, China, and the
(Ad5)-vectored COVID-19 vaccine in a dose-escalating institutional review board of the Jiangsu Provincial
For the protocol see http://www. manner (5 × 10¹⁰, 1 × 10¹¹, and 1·5 × 10¹¹ viral particles). Center of Disease Control and Prevention. The protocol
jshealth.com/jkfw/kygz/202007/ Generally, the candidate vaccines had acceptable safety is available online.
t20200713_69079.html
and tolerability profiles and promising immunogenicity Eligible participants were healthy adults aged 18 years
in healthy Chinese adults; however, the high-dose vaccine or older, who were HIV-negative and previous
was associated with an increased risk of severe adverse SARS-CoV-2 infection-free, confirmed by commercial
480 www.thelancet.com Vol 396 August 15, 2020
Articles
human immunodeficiency virus antibody detection kit domain (RBD) using ELISA kits (Beijing Wantai BioPharm,
(InTec products, Xiamen, China) and SARS-CoV-2 rapid Beijing, China). The detection limit for the RBD-specific
test kit (Jinwofu, Beijing, China) using fingertip blood at ELISA antibody test was 1:40. The neutralising antibody
screening. To be included, participants needed to be able responses to live SARS-CoV-2 virus (strain SARS-CoV-2/
to understand the content of informed consent and human/CHN/Wuhan_IME-BJ01/2020, GenBank number
willing to sign the informed consent; able and willing to MT291831.1) or a pseudovirus (a vesicular stomatitis virus
complete all the scheduled study processes; have an pseudovirus system expressing the spike glycoprotein),10
axillary temperature of 37·0°C or less; have a body-mass and cellular immune responses before the vaccination and
index of between 18·5 and 30·0; and have general good 28 days after the vaccination were also measured. The
health as established by medical history and physical detection limits for the neutralising antibody tests to live
examination. Pregnant or breastfeeding women were SARS-CoV-2 virus and a pseudovirus were 1:8 and 1:10,
excluded. People with mental disease, history of allergies, respectively. Undetectable antibody titres in serum were
or serious cardiovascular disease, and some other major assigned values of half the detection limits for calculation.
chronic illnesses were also excluded. A complete list of The cellular immune responses of the expression of inter
the inclusion and exclusion criteria is provided in the feron (IFN) γ stimulated by the overlapping peptide pool
protocol. Participants were recruited through online of spike glycoprotein were detected by enzyme-linked
recruitment advertisements. Written informed consent immunospot (ELISpot) assay (Mabtech, Stockholm,
was obtained from each participant before screening for Sweden). Positive IFNγ-ELISpot response was defined as at
eligibility. least five spot-forming cells per 1 × 10⁵ peripheral blood
mononuclear cells, and a minimum of a two-times increase
Randomisation and masking from baseline. Neutralising antibody titres against the
The Ad5-vectored COVID-19 vaccine was developed by vaccine vector Ad5 were measured with the serum
the Beijing Institute of Biotechnology (Beijing, China) neutralisation assay.11 The follow-ups were scheduled at
and CanSino Biologics, and contained replication-defect days 14 and 28, and month 6 post vaccination for safety and
ive Ad5 vectors expressing the full-length spike gene immunogenicity assessment.
based on Wuhan-Hu-1 (GenBank accession number
YP_009724390). The placebo contained the vaccine Outcomes
excipients only, with no viral particles. The experimental The primary objectives were to evaluate immunogenicity
vaccines and placebos had identical packaging with a and safety of the Ad5-vectored COVID-19 vaccine, and to
randomisation number on each vial as the only identi determine a vaccine dose for a phase 3 efficacy study. The
fiers. The vaccines of 1 × 10¹¹ and 5 × 10¹⁰ viral particles primary endpoint for safety evaluation was the incidence
and placebo were randomised at a 2:1:1 ratio. Eligible of adverse reactions within 14 days after the injection.
participants were sequentially assigned a randomisation The primary endpoints for immunogenicity were the
number, according to a blocked randomisation list geometric mean titres (GMTs) of RBD-specific ELISA
(block size 4) generated by an independent statistician antibody responses and neutralising antibody responses
using SAS software (version 9.4), and injected with an against live virus or pseudovirus at day 28 post vaccination.
experimental vaccine or placebo labelled with the same The secondary endpoints for immunogenicity were RBD-
number. Individuals involved in randomisation and specific ELISA antibody responses at day 14 and month 6
masking had no involvement in the rest of the trial. (6 month data not yet available), and specific T-cell
Participants, investigators, and staff undertaking labora responses at day 28 post vaccination. Seroconversion of
tory analyses were masked to group allocation. the humoral immune responses was also a secondary
endpoint, and was defined as an increase in post-
Procedures vaccination titre of at least four-times from baseline. The
A single injection of the vaccines of 1 × 10¹¹ or 5 × 10¹⁰ secondary safety outcomes included the occurrence of
viral particles per mL, or placebo, were given to adverse events from days 0 to 28 after vaccination,
participants intramuscularly in the arm. Participants and serious adverse events reported up to 6 months.
were monitored for 30 min post injection for immediate Investigators did severity grading of the adverse events
adverse reactions, and followed up for any injection site according to the standard guidelines issued by the China
or systemic adverse reactions within 14 days and adverse State Food and Drug Administration, and the causality
events within 28 days post vaccination. Serious adverse with immunisation before unmasking. Stratified analysis
events self-reported by participants were documented of safety and immunogenicity of the participants was
throughout the study. done based on the baseline Ad5 neutralising antibody
The detailed methods of the assays have been reported titres with a cutoff at 1:200. Post-hoc analysis of the
previously.9 In brief, blood samples were taken from immune responses by age and sex, and the proportion of
participants at day 0 immediately before vaccination, and at vaccine recipients with the composite endpoint of either
days 14 and 28 post vaccination for the measurement of positive cellular or seroconversion of humoral immune
specific antibody responses against the receptor binding responses at day 28 post vaccination were presented.
www.thelancet.com Vol 396 August 15, 2020 481
Articles
immunogenicity data from the phase 1 study were
603 volunteers screened for available, using PASS software (version 11.0). For the
eligibility
RBD-specific antibody, 250 individuals in the 1 × 10¹¹ viral
particles dose group and 125 individuals in the 5 × 10¹⁰
95 excluded viral particles dose group were able to provide at least a
46 did not meet the inclusion criteria* power of 90% to show a difference of the log-transferred
42 met the exclusion criteria
2 withdrew consent titre of 0·176 with an SD of 0·4 between the dose groups,
5 eligible but not enrolled because the at a level of significance of 0·017, considering multiple
number of participants was met
comparisons.
Statistical tests were two-sided with an α value
508 randomised of 0·05, and analysed by an independent statistician
using SAS (version 9.4). The primary immunogenicity
analysis was done in the full-analysis cohort, including all
participants who were injected and donated blood samples
253 assigned to 1 × 1011 vp 129 assigned to 5 × 1010 vp 126 assigned to placebo
for antibody tests post vaccination, while the safety
analysis was done in all enrolled participants who received
253 completed follow-up visits 129 completed follow-up visits 126 completed follow-up visits the vaccination. Correlation analysis of the RBD-specific
within 28 days within 28 days within 28 days ELISA antibody and neutralising antibody was done,
and the Pearson correlation coefficient was calculated.
Figure 1: Trial profile Antibody responses are reported as the GMT with 95% CI.
vp=viral particles. *26 did not meet the inclusion criteria of negative IgM/IgG to severe acute respiratory syndrome ANOVA was used for log-transformed antibody titres, and
coronavirus 2.
the Wilcoxon rank-sum test for data that were not normally
distributed. The χ² test or Fisher’s exact test was used for
Vaccine at Vaccine at Placebo
1 × 10¹¹ vp 5 × 10¹⁰ vp (n=126)
categorical data. Mul tiple comparisons were done if a
(n=253) (n=129) significant difference across the treatment groups was
Age, years
noted, using Student Newman-Keuls test or Bonferroni-
adjusted α value when relevant. This trial is registered
18–44 152 (60%) 80 (62%) 77 (61%)
with ClinicalTrials.gov, NCT04341389.
45–54 67 (26%) 32 (25%) 35 (28%)
≥55 34 (13%) 17 (13%) 14 (11%)
Role of the funding source
Mean 40·0 (12·8) 39·7 (12·1) 39·2 (12·5)
The funders of the study were involved in protocol
Sex
design, but not in data collection, statistical analysis, data
Male 126 (50%) 64 (50%) 64 (51%)
interpretation, or writing of the report. All the authors
Female 127 (50%) 65 (50%) 62 (49%)
had full access to all the data in the study and had final
Body-mass index, kg/m² 24·2 (2·8) 24·2 (2·7) 23·3 (2·6)
responsibility for the decision to submit for publication.
Underlying diseases
Yes 8 (3%) 8 (6%) 6 (5%)
Results
No 245 (97%) 121 (94%) 120 (95%) 603 volunteers were recruited and screened for eligibility
Pre-existing adenovirus type-5 neutralising antibody between April 11 and 16, 2020 (figure 1). 95 individuals
≤1:200, titre 127 (50%) 54 (42%) 61 (48%) were excluded, leaving 508 eligible participants who
>1:200, titre 126 (50%) 75 (58%) 65 (52%) consented to participate in the trial and were randomly
Data are number of participants (%) or mean (SD). vp=viral particles. assigned to vaccine or placebo. 253 were randomly
assigned to the 1 × 10¹¹ viral particles dose group, 129 to the
Table 1: Baseline characteristics
5 × 10¹⁰ viral particles dose group, and 126 to the placebo
group. The mean age of the participants was 39·7 years
Statistical analysis (SD 12·5; range 18–83), with 309 (61%) individuals aged
This phase 2 trial was launched before the immuno 18–44 years, 134 (26%) aged 45–54 years, and 65 (13%) aged
genicity data from the phase 1 trial were obtained; 55 years or older across the treatment groups (table 1).
therefore, the sample size was not calculated at the design 254 (50%) of 508 participants were male. Baseline charac
stage. An overall sample size of 500 participants (n=250 teristics of the participants and the pre-existing Ad5
in the 1 ×
10¹¹ viral particles dose group; n=125 in neutralising antibody titres were largely similar across the
the 5 × 10¹⁰ viral particles dose group; and n=125 in the treatment groups. Among the 508 participants, 266 (52%)
placebo group) was determined, based on expert opinion had high pre-existing immunity and 242 (48%) had low
and the minimum sample size requirement in the pre-existing immunity to the Ad5 vector. All the participants
technical guidelines for vaccine clinical trials issued by completed the scheduled safety visits within 28 days post
the National Medical Products Administration, China.12 vaccination and gave blood samples at days 0 and 28, and
We did an ex-post power calculation of this study after the 506 (>99%) donated blood samples at day 14.
482 www.thelancet.com Vol 396 August 15, 2020
Articles
The baseline antibody titres of the participants are participants in the 1 × 10¹¹ and 5 × 10¹⁰ viral particles
given in the appendix (p 1). RBD-specific ELISA antibody dose groups, respectively, at day 28 post vaccination
responses induced by the Ad5-vectored COVID-19 (figure 2). Seroconversion of the neutralising antibody
vaccine were detected from day 14 onwards, with GMTs responses to live SARS-CoV-2 occurred in 148 (59%, See Online for appendix
of 94·5 (95% CI 80·5–110·8) and 85·1 (66·0–109·7) 95% CI 52–65) of 253 participants receiving the 1 × 10¹¹
in the 1 × 10¹¹ and 5 × 10¹⁰ viral particles dose groups, viral particles dose, and in 61 (47%, 39–56) of
respectively (figure 2). At day 28, the RBD-specific ELISA 129 participants receiving the 5 × 10¹⁰ viral particles dose
antibodies peaked at 656·5 (575·2–749·2) in the 1 × 10¹¹ 28 days post vaccina tion. The GMTs of neutralising
viral particles dose group and 571·0 (467·6–697·3) in the antibody responses to pseudovirus were 61·4 (95% CI
5 × 10¹⁰ viral particles dose group. 244 (96%, 95% CI 53·0–71·0) in the 1 × 10¹¹ viral particles dose group and
93–98) of 253 participants in the 1 × 10¹¹ viral particles 55·3 (45·3–67·5) in the 5 × 10¹⁰ viral particles dose
dose group and 125 (97%, 92–99) of 129 participants in group, with seroconversion of 214 (85%, 95% CI 80–89)
the 5 × 10¹⁰ viral particles dose group showed sero and 107 (83%, 76–88), respectively. No significant dif
conversion of RBD-specific ELISA antibodies at day 28, ferences were observed between the two dose groups in
whereas the participants in the placebo group showed no the neutralising antibody responses to live virus and
antibody increase from baseline. pseudovirus.
Both vaccine doses induced significant neutralising Before vaccination, 266 (52%) of 508 participants had
antibody responses to live SARS-CoV-2, with GMTs of high pre-existing anti-Ad5 neutralising antibodies (table 1).
19·5 (95% CI 16·8–22·7) and 18·3 (14·4–23·3) in Participants with low pre-existing anti-Ad5 immunity had
A B
800 GMT 100 800 100
Seroconversion
700 700
80 80
Proportion of ≥4-fold increase
Proportion of ≥4-fold increase
600 600
500 500
60 60
GMT
GMT
400 400
40 40
300 300
200 200
20 20
100 100
0 0 0 0
1 × 1011 vp 5 × 1010 vp Placebo 1 × 1011 vp 5 × 1010 vp Placebo
ELISA antibodies to RBD at day 14 ELISA antibodies to RBD at day 28
C D
75 100 75 100
60 80 60 80
Proportion of ≥4-fold increase
Proportion of ≥4-fold increase
45 60 45 60
GMT
GMT
30 40 30 40
15 20 15 20
0 0 0 0
1 × 1011 vp 5 × 1010 vp Placebo 1 × 1011 vp 5 × 1010 vp Placebo
Neutralising antibodies to live SARS-CoV-2 at day 28 Neutralising antibodies to pseudovirus at day 28
Figure 2: Specific antibody responses to RBD, neutralising antibodies to live severe acute respiratory syndrome coronavirus 2 and pseudovirus post
vaccination
Seroconversion was defined as an increase in post-vaccination titre of at least four-times baseline. The baseline antibody titres are shown in the appendix (p 1).
All comparisons across the three treatment groups are p<0·0001. Multiple comparisons showed no significant difference between the 1 × 10¹¹ vp and 5 × 10¹⁰ vp dose
groups. GMT=geometric mean antibody titre. RBD=receptor binding domain. vp=viral particles.
www.thelancet.com Vol 396 August 15, 2020 483
Articles
RBD-specific ELISA antibody and neutralising antibody dose groups post vaccination, particularly in terms of
levels that were approximately two-times higher than the neutralising antibodies to live virus (appendix pp 7–8).
participants with high pre-existing anti-Ad5 immunity Nevertheless, the ELISA antibodies to RBD and neutral
(appendix pp 2–3). Increasing age was found to be another ising antibodies at day 28 in vaccine recipients were still
independent negative impact factor on the RBD-specific significantly higher than in placebo recipients in this
ELISA antibody (p=0·0018), and neutralising antibody population. Male and female participants who received the
responses to live virus (p<0·0001) or pseudovirus (p=0·046; vaccine showed similar RBD-specific ELISA antibody
appendix pp 4–6). The stratified analysis based on age and neutralising antibody responses post vaccination
found that participants aged 55 years or older were (appendix pp 9–10). Both the ELISA antibody titres to RBD
associated with relative low antibody responses in both and neutralising antibody titres to pseudovirus were
significantly correlated with the neutralising antibody
titres to live virus, with a correlation coefficient of 0·75,
A and 0·72 (p<0·0001), respectively.
p<0·0001 Baseline ELISpot T-cell responses were negative in
103 1 × 1011 vp p<0·0001 506 (>99%) of 508 participants. Ad5-vectored COVID-19
5 × 1010 vp
vaccine induced significant SARS-CoV-2 spike glyco
IFNγ-expressing cells per 1 × 105 PBMCs
Placebo p<0·0001
protein-specific IFNγ-ELISpot responses in 227 (90%,
102 95% CI 85–93) of 253 participants receiving the 1 × 10¹¹
viral particles dose, and 113 (88%, 81–92) of 129 partici
pants receiving the 5 × 10¹⁰ viral particles dose at
day 28 (figure 3). A median of 11·0 spot-forming cells
101
(IQR 5·0–25·0) and 10·0 spot-forming cells (6·0–21·0)
per 1 ×
10⁵ peripheral blood mononuclear cells in
participants in the 1 × 10¹¹ viral particles and 5 × 10¹⁰ viral
0 particles dose groups, respectively, were observed at
day 28, with increases of more than ten-times in both dose
B
p<0·0001 groups. The IFNγ-ELISpot responses were not signifi
103 p<0·0001
cantly different between the dose groups at day 28. No
positive IFNγ-ELISpot T-cell responses were detected in
IFNγ-expressing cells per 1 × 105 PBMCs
p<0·0001
the placebo group post vaccination. Significant increases
of post-vaccination T-cell responses in terms of spot-
102
forming cells were observed both in participants with
high and low pre-existing neutralising antibody at day 28.
In the participants with high pre-existing immunity
101 against Ad5, 88% of participants across both groups
(111 of 126 in the 1 × 10¹¹ viral particles dose group, and
66 of 75 in the 5 × 10¹⁰ viral particles dose group) showed
0 positive IFNγ-ELISpot T-cell responses post vaccination.
Sex and age of the participants did not differ their
C IFNγ-ELISpot T-cell responses induced by vaccination
103 p<0·0001
(appendix p 11). In addition, 241 (95%, 95% CI 92–97) of
p<0·0001 253 participants in the 1 × 10¹¹ viral particles dose group,
IFNγ-expressing cells per 1 × 105 PBMCs
p<0·0001 and 118 (91%, 85–95) of 129 participants in the 5 × 10¹⁰ viral
102 particles dose group showed either positive IFNγ-ELISpot
T-cell response or seroconversion of neutralising anti
body to live SARS-CoV-2 at day 28 post vaccination
(appendix p 12).
101
Within 14 days after the vaccination, 183 (72%) of
253 participants in the 1 × 10¹¹ viral particles dose group,
and 96 (74%) of 129 participants in the 5 × 10¹⁰ viral
0 particles dose group reported at least one solicited
Day 0 Day 28
Time post vaccination (days)
adverse reaction, both of which were significantly higher
than the 46 (37%) of 126 participants in the placebo group
Figure 3: Specific T-cell responses measured by ELISpot (p<0·0001; table 2). The most common systemic solicited
The number of specific T cells with secretion of IFNγ at days 0 and 28 in all
reactions in the 5 × 10¹⁰ and 1 × 10¹¹ viral particles dose
participants (A), and stratified by pre-existing adenovirus type-5 neutralising
antibody titres of less than or equal to 1:200 (B) and more than 1:200 (C). groups were fatigue, reported by 42% and 34%; fever,
vp=viral particles. IFN=interferon. PBMC=peripheral blood mononuclear cell. reported by 32% and 16%; and headache, reported by
484 www.thelancet.com Vol 396 August 15, 2020
Articles
29% and 28%, respectively. The most common injection
Vaccine at 1 × 10¹¹ Vaccine at 5 × 10¹⁰ Placebo p value
site solicited reaction was pain, reported by 57% of the vp (n=253) vp (n=129) (n=126)
1 × 10¹¹ viral particles dose group and 56% of the 5 × 10¹⁰
Solicited adverse reactions within 14 days
viral particles dose group. Although most adverse
Any 183 (72%) 96 (74%) 46 (37%) <0·0001
reactions were reported as either mild or moderate,
Grade 3 24 (9%) 1 (1%) 0 <0·0001
24 (9%) of 253 participants receiving the vaccine at
Injection site adverse reactions
1 × 10¹¹ viral particles had severe (grade 3) adverse
Pain 145 (57%) 72 (56%) 11 (9%) <0·0001
reactions, which was significantly higher than those
Induration 12 (5%) 2 (2%) 0 0·014
receiving the vaccine at 5 × 10¹⁰ viral particles (p=0·0011)
Grade 3 induration 2 (1%) 0 0 0·75
or placebo (p=0·0004). The most commonly reported
grade 3 adverse reactions was fever, in 20 (8%) of Redness 5 (2%) 1 (1%) 2 (2%) 0·81
253 participants in the 1 × 10¹¹ viral particles dose group, Swelling 10 (4%) 5 (4%) 0 0·049
and one (1%) of 129 participants in the 5 × 10¹⁰ viral Grade 3 swelling 1 (<1%) 0 0 1·0
particles dose group. High pre-existing Ad5 immunity, Itch 14 (6%) 3 (2%) 0 0·0075
increasing age, and male sex were associated with Systemic adverse reactions
significantly lower occurrence of fever post vaccination Fever (all grades) 82 (32%) 21 (16%) 12 (10%) <0·0001*
(appendix p 13). The grade 3 reactions were self-limited Grade 3 fever 20 (8%) 1 (1%) 0 0·0001†
and resolved within 72–96 h without medication Headache 73 (29%) 36 (28%) 17 (13%) 0·0031
(appendix pp 14–15). The unsolicited adverse reactions Grade 3 headache 2 (1%) 0 0 0·75
within 14 days post vaccination were reported by 19 (8%) Fatigue 106 (42%) 44 (34%) 21 (17%) <0·0001
participants in the 1 × 10¹¹ viral particles dose group, Grade 3 fatigue 1 (<1%) 0 0 1·0
seven (5%) in the 5 × 10¹⁰ viral particles dose group, and Vomiting 4 (2%) 1 (1%) 1 (1%) 0·88
seven (6%) in the placebo group, showing no difference Diarrhoea 19 (8%) 10 (8%) 4 (3%) 0·22
across the groups. Overall, 196 (77%) participants in the Muscle pain 39 (15%) 23 (18%) 3 (2%) 0·0002
1 × 10¹¹ viral particles dose group, 98 (76%) in the 5 × 10¹⁰ Grade 3 muscle pain 1 (<1%) 0 0 1·0
viral particles dose group, and 61 (48%) in the placebo Joint pain 34 (13%) 13 (10%) 4 (3%) 0·0074
group experienced at least one or more adverse event Grade 3 joint pain 1 (<1%) 0 0 1·0
within 28 days after the vaccination. No serious adverse Oropharyngeal pain 22 (9%) 7 (5%) 6 (5%) 0·27
events were documented within 28 days. Cough 12 (5%) 2 (2%) 3 (2%) 0·24
All participants tested were seronegative for the Nausea 20 (8%) 6 (5%) 4 (3%) 0·14
antibodies to nucleocapsid protein of SARS-CoV-2 at Hypersensitivity 0 0 2 (2%) 0·061
day 28, by IgG and IgM rapid test kit (Vazyme Biotech, Dyspnoea 1 (<1%) 0 0 1·0
number CD101, Nanjing, China), suggesting none had Grade 3 dyspnoea 1 (<1%) 0 0 1·0
exposure to SARS-CoV-2 during this study period. Appetite impaired 27 (11%) 7 (5%) 3 (2%) 0·0089
Syncope 1 (<1%) 1 (1%) 0 1·0
Discussion Mucosal abnormality 2 (1%) 2 (2%) 2 (2%) 0·65
This study is the first randomised controlled trial for Pruritus 6 (2%) 4 (3%) 6 (5%) 0·40
evaluation of the immunogenicity and safety of a Unsolicited adverse reactions within 14 days
candidate non-replicating Ad5-vectored COVID-19
Any 19 (8%) 7 (5%) 7 (6%) 0·65
vaccine. The phase 2 trial is a necessary and crucial step
Grade 3 1 (<1%) 0 0 1·0
to turn an early-stage experimental vaccine into a
Overall adverse events within 28 days
promising vaccine candidate in an efficacy trial in a
Any 196 (77%) 98 (76%) 61 (48%) <0·0001
large population. In this study, a single injection of the
Grade 3 24 (9%) 1 (1%) 2 (2%) 0·0002
Ad5-vectored COVID-19 vaccine at 1 × 10¹¹ viral particles
and 5 × 10¹⁰ viral particles induced comparable specific Data are number of participants (%). Any refers to all the participants with any grade adverse reactions or events.
Adverse reactions and events were graded according to the scale issued by the China State Food and Drug
immune responses to the spike glycoprotein at day 28, Administration. Grade 3 is severe (ie, prevented activity). The p value was generated by comparisons across the
with no significant differences noted between the three treatment groups. vp=viral particles. *Multiple comparisons of the dose groups 1 × 10¹¹ vp versus 5 × 10¹⁰ vp;
two groups. The vaccine induced seroconversion of the p=0·0008. †Multiple comparisons of the dose groups 1 × 10¹¹ vp versus 5 × 10¹⁰ vp; p=0·0038.
neutralising antibodies in 59% and 47% of participants, Table 2: Adverse reactions within 14 days and overall adverse events within 28 days after vaccination
and seroconversion of binding antibody in 96% and
97% of participants, in the 1 × 10¹¹ and 5 × 10¹⁰ viral
particles dose groups, respectively. Positive specific T-cell group showed either cellular or humoral immune
responses measured by IFNγ-ELISpot were found in responses at day 28 post vaccination (appendix p 12). Pre-
90% and 88% of participants receiving the vaccine at existing immunity to the Ad5 vector and increasing age
1 × 10¹¹ and 5 × 10¹⁰ viral particles, respectively. 95% of could partially hamper the specific immune responses
participants in the 1 × 10¹¹ viral particles dose group and to vaccination, particularly for the humoral immune
91% of the recipients in the 5 × 10¹⁰ viral particles dose responses.
www.thelancet.com Vol 396 August 15, 2020 485
Articles
In this study, most reactions reported post vaccination regimen of the Ad5-vectored COVID-19 vaccine than
were mild or moderate. Although the proportions of people who are young and naive to Ad5. Pre-existing
participants who had adverse reactions such as fever, anti-Ad5 immunity is considered to be the biggest
fatigue, and injection site pain were significantly higher obstacle for the candidate Ad5-vectored COVID-19
in vaccine recipients than those in placebo recipients, vaccine to overcome. A flexible additional dose (between
adverse reactions within 28 days were generally not months 3 and 6) might be a potential solution to provide
severe, and resolved within a short period of time (no enhancement of immune responses, according to our
more than 48 h). Among recipients of either dose of previous experience with an Ad5 vector-based Ebola
the Ad5-vectored COVID-19 vaccines, all grade 3 adverse vaccine in a homologous prime-boost immunisation
reactions were reported from the dose group of study.13 More evidence about the immunogenicity and
1 × 10¹¹ viral particles, with the exception of one from the feasibility of additional dose immunisation in the older
5 × 10¹⁰ viral particles dose group. Although this study was population will be evaluated in a phase 2b trial. However,
powered only to capture common adverse events after the vaccine recipients in this study showed increased
immunisation, the results suggest that the experimental anti-Ad5 neutralising antibodies, by 5·0-times and
Ad5-vectored COVID-19 vaccine has a good safety profile, 3·8-times in the 1 × 10¹¹ viral particles and 5 × 10¹⁰ viral
which was in line with the results of our phase 1 trial in particles dose groups, respectively, at day 28 post
healthy adults.9 vaccination (appendix p 17). The high level of anti-Ad5
We initiated this phase 2 trial before the full analysis of immunity could affect the boosting effect of the vaccine;
the data from the phase 1 study was available. The vaccine therefore, we planned to follow the dynamic change of
doses chosen were mainly based on the safety data from the Ad5-specific antibodies in participants until month 6
the dose-escalating phase 1 trial: a higher proportion of to determine the timing of booster administration.
participants reported grade 3 adverse reactions in the We determined the participants’ serostatus before
high-dose group (1·5 × 10¹¹ viral particles) compared with and after immunisation by ELISA, neutralising tests to
low-dose (5 × 10¹⁰ viral particles) or middle-dose (1 × 10¹¹ live SARS-CoV-2 or pseudovirus, and ELISpot, providing
viral particles) groups (17% vs 6% and 6%, respectively).9 evidence of humoral and cell-mediated immunity for the
Therefore, we assumed that the vaccine doses at 1 × 10¹¹ candidate vaccine. Because the live virus neutralising
and 5 × 10¹⁰ viral particles might have similar safety antibody test needs to be done in biosafety level three
profiles. In addition, an increasing antigen dose is often laboratories, a pseudovirus neutralising antibody test
associated with increasing immunogenicity; thus, we was developed to serve as an alternative.10 However, we
expected the vaccine dose at 1 × 10¹¹ viral particles to be found the magnitudes of neutralising antibody responses
the better of the two doses. Therefore, we designed the to pseudovirus were greater than those to the live virus,
randomisation of this study in a ratio of 2:1:1 for the dose which might be associated with the different methodo
groups of 1 × 10¹¹ and 5 × 10¹⁰ viral particles, and placebo logical principles of the two tests. In the pseudovirus
group, respectively, giving more weight to the first group. neutralising test, when the specific antibody in serum
We found, in contrast to our expectations, that the binds to the pseudovirus, it inhibits the pseudovirus
vaccine at 5 × 10¹⁰ viral particles had a better safety profile from entering the cells, reducing the expression of
than, and comparable immunogenicity to, the vaccine at luciferase on the cell surface. Thus, we can calculate the
1 × 10¹¹ viral particles. amount of neutralising antibodies to pseudovirus by
Age and pre-existing anti-Ad5 immunity of the detecting the total fluorescence. The neutralising
participants could have affected the candidate vaccine’s antibody is detected by measuring the cytopathic effect
safety and immunogenicity. We noted that the after the viral infection. Although, generally, the output
occurrence of fever was associated with decreasing age values of the two methods are correlated, the two
and low pre-existing immunity to the vaccine vector Ad5 methods have different detection sensitivities and the
virus. 19 (90%) of the 21 participants who experienced detection values do not always have a one-to-one
grade 3 fever had no pre-existing immunity to Ad5, with corresponding relationship.
a neutralising antibody titre below detection. Increasing Both neutralising antibody and T-cell responses were
age and high pre-existing anti-Ad5 immunity were important in eliminating the virus and controlling dis
found to be able to significantly reduce the immune ease development in patients with COVID-19 who were
responses to the vaccine. In some participants with high naturally infected by SARS-CoV-2.14,15 Antibodies are very
pre-existing anti-Ad5 immunity, one injection of the likely to be effective against SARS-CoV-2, considering
vaccine might be inadequate to induce a high level of that convalescent serum samples have been applied with
humoral immune responses, particularly for people apparently good clinical results in COVID-19.16 But for the
aged 55 years or older. These results align with the vaccine-induced immune responses, whether neutralising
finding that older people are more likely to have exposure antibody alone is capable of preventing infection remains
history to Ad5, with higher baseline neutralising undetermined. Specific T-cell responses are essential for
antibody to Ad5, which indicates that this population directly attacking and killing virus-infected cells.15 In
might be more tolerant of higher dose or a booster dose addition, the CD4 T-cell responses are critical for the
486 www.thelancet.com Vol 396 August 15, 2020
Articles
cytotoxic T-cell response and the maturating of WHO is facilitating collaboration and efforts to support
neutralising antibodies.17 Thus, the evaluation of the cell- vaccine development by defining the desired charac
mediated responses, in addition to the neutralising teristics of promising candidate vaccines to combat
antibodies, is important for a successful candidate COVID-19.25,26 This situation emphasises the importance
vaccine. of being prepared to initiate an international multicentre,
Our trial has some limitations. First, this phase 2 trial randomised, double-blind, controlled phase 3 effective
started before the full analysis of the data from the phase 1 ness trial as soon as possible.25 One immunisation of the
study was available, so we did not calculate the sample Ad5-vectored COVID-19 vaccine at 5 × 10¹⁰ viral particles
size based on study power in advance, which might lead has a good safety profile (limited to common adverse
to a lack of power to show the difference between dose reactions following immunisation) and could elicit
groups. Second, the participants included in this study significant specific immune responses to SARS-CoV-2,
are all from Wuhan, China. The baseline anti-Ad5 making it a potential candidate for emergency vaccination
immunity of the participants seemed to be representative of acute protective response.
of Chinese adults, according to the previously reported In conclusion, the results of this trial have extended
studies;18 however, anti-Ad5 immunity in adults varies our knowledge of the immunogenicity and safety of the
from place to place globally, with reported proportions of Ad5-vectored COVID-19 vaccines. The results support
adults with neutralising antibodies titres for Ad5 of more testing of the Ad5-vectored COVID-19 vaccine at 5 × 10¹⁰
than 1:200 of about 80% in India, 78% in Kenya, 67% in viral particles in a phase 3 effectiveness trial in healthy
Thailand, 64% in Uganda, around 60% in South Africa, adults.
45% in Sierra Leone, and less than 30% in the USA.19–21 Contributors
We might expect the candidate Ad5-vectored vaccine to F-CZ was the principal investigator, and X-HG and J-YH were
have a superior immunogenicity in the population with a co-principal investigators. F-CZ, WC, X-HG, J-YH, L-HH, J-JX, Y-HL,
J-XL, W-JW, ZW, J-BG, and S-YJ designed the trial and study protocol.
lower pre-existing anti-Ad5 immunity, but an inferior J-XL drafted the Article. WC contributed to critical review and revision
immunogenicity in people with a higher pre-existing anti- of the Article. F-CZ, W-JW, J-XL, H-XP, and L-HH contributed to the
Ad5 immunity than observed in this phase 2 trial. Third, data interpretation and revision of the Article. X-WW was responsible for
this trial did not include children. Although COVID-19 statistical analysis. J-JX, B-SW, and JZ contributed to study supervision.
B-FY, W-JW, ZW, TJ, X-HWa, S-YJ, X-AQ, QL, PD, and H-DJ led and
appears to have a more benign course in children, with participated in the site work, including the recruitment, follow-up,
almost no fatalities reported,22,23 an ideal candidate vaccine and data collection. Y-HL, TJ, YH, LW, X-HWu, and J-JL were responsible
for the ongoing pandemic should cover susceptible for laboratory analyses. ZZ and S-YJ contributed to the literature search.
populations in all ages. Fourth, we report only data within J-BG and S-PW monitored the trial.
28 days of vaccination, and do not include data about the Declaration of interests
durability of the vaccine-induced immunity, which was WC reports grants from the National Key R&D Program of China
(2020YFC10841400), and grants from the National Science and
not available at the time of publication. A subset of Technology Major Project (2016ZX10004001, 2018ZX09201005). J-BG is
patients infected with SARS-CoV-2 might not develop an employee of CanSino Biologics. All other authors declare no
long-lasting antibodies to the virus, and S-antibodies competing interests.
were reported to rapidly decline for people infected with Data sharing
seasonal coronaviruses and who recovered from We support sharing of the individual participant data. The individual
participant data that underlie the results reported in this Article,
COVID-19, especially those with mild symptoms or
after de-identification (text, tables, figures, and appendices) will be
asymptomatic infection.24 The ongoing phase 1 and 2 shared. Individual participant data will be available beginning 3 months
trials will enable the continued collection of safety and ending 1 year after publication. Supporting clinical documents
data and assessment of antibody persistence over a including study protocol, statistical analysis plan, and the informed
consent form will be available immediately following publication for at
6-month period. Fifth, in this study, no participants had
least 1 year. Researchers who provide a scientifically sound proposal will
SARS-CoV-2 exposure after the vaccination, so we were be allowed access to the individual participant data. Proposals should be
unable to assess the efficacy of the candidate vaccine or directed to jszfc@vip.sina.com or cw0226@foxmail.com. These
any immunological risk associated with antibody induced proposals will be reviewed and approved by the funder, investigator,
and collaborators on the basis of scientific merit. To gain access, data
by vaccination when exposed to the virus. However, the
requesters will need to sign a data access agreement.
risk of COVID-19 and antibody-enhanced disease on
Acknowledgments
exposure to the virus will be monitored long term. Finally, We thank Yan-Song Sun, Sen Zhang, and Yu-Chang Li, from the Beijing
the clinical significance of these changes is difficult to Institute of Microbiology and Epidemiology (Beijing, China),
assess because of the absence of an identified correlate for laboratory analysis. We thank Jian-Yuan Wu, Hu Wang, Chang Chen,
of protective immunity, and reference standards for and Han-Ning Hu, from Zhongnan Hospital of Wuhan University
(Wuhan, China), and Hai-Ying Zhang, Li Liu, and Lei Wang, from the
measuring neutralising anti bodies against COVID-19. Hubei Provincial Center for Disease Control and Prevention (Wuhan,
Future studies will need to establish an immune correlate China), for on-site implementation. We thank Ke Zhang from the
of protection and a protective threshold to assess the Academy of Military Medical Sciences (Beijing, China), Kun Liu from
feasibility of using the Ad5-vectored COVID-19 vaccine the General Hospital of Central Theater Command (Wuhan, China),
and Chang-Long Fu and his team, from Wuhan Rest Center, Chinese
to provide protection for high-risk populations or for People’s Armed Police Force (Wuhan, China), for management of the
outbreak intervention. clinical trial site.
www.thelancet.com Vol 396 August 15, 2020 487
Articles
References 14 Grifoni A, Weiskopf D, Ramirez SI, et al. Targets of T cell responses
1 WHO. Coronavirus disease (COVID-2019) situation reports. 2020. to SARS-CoV-2 coronavirus in humans with COVID-19 disease and
https://www.who.int/docs/default-source/coronaviruse/situation- unexposed individuals. Cell 2020; 181: 1489–501.
reports/20200710-covid-19-sitrep-172.pdf?sfvrsn=70724b90_2 15 Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of
(accessed July 10, 2020). COVID-19: immunity, inflammation and intervention.
2 Graham BS. Rapid COVID-19 vaccine development. Science 2020; Nat Rev Immunol 2020; 20: 363–74.
368: 945–46. 16 Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically ill patients
3 Cheng HY, Jian SW, Liu DP, Ng TC, Huang WT, Lin HH. with COVID-19 with convalescent plasma. JAMA 2020;
Contact tracing assessment of COVID-19 transmission dynamics in 323: 1582–89.
Taiwan and risk at different exposure periods before and after 17 Walls AC, Xiong X, Park YJ, et al. Unexpected receptor functional
symptom onset. JAMA Intern Med 2020; published online May 1. mimicry elucidates activation of coronavirus fusion. Cell 2019;
https://doi.org/10.1001/jamainternmed.2020.2020. 176: 1026–39.
4 Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 18 Yu B, Zhou Y, Wu H, et al. Seroprevalence of neutralizing
transmissibility and severity in China outside Hubei after control antibodies to human adenovirus type 5 in healthy adults in China.
measures, and second-wave scenario planning: a modelling impact J Med Virol 2012; 84: 1408–14.
assessment. Lancet 2020; 395: 1382–93. 19 Thorner AR, Vogels R, Kaspers J, et al. Age dependence of
5 Lurie N, Saville M, Hatchett R, Halton J. Developing COVID-19 adenovirus-specific neutralizing antibody titers in individuals from
vaccines at pandemic speed. N Engl J Med 2020; 382: 1969–73. sub-Saharan Africa. J Clin Microbiol 2006; 44: 3781–83.
6 Caddy S. Developing a vaccine for covid-19. BMJ 2020; 369: m1790. 20 Pilankatta R, Chawla T, Khanna N, Swaminathan S. The prevalence
7 WHO. Draft landscape of COVID-19 candidate vaccines. 2020. of antibodies to adenovirus serotype 5 in an adult Indian population
https://www.who.int/publications/m/item/draft-landscape-of-covid- and implications for adenovirus vector vaccines. J Med Virol 2010;
19-candidate-vaccines (accessed June 13, 2020). 82: 407–14.
8 CEPI. CEPI-funded COVID-19 vaccine candidates progress to clinical 21 Barouch DH, Kik SV, Weverling GJ, et al. International
trials. 2020. https://cepi.net/news_cepi/cepi-funded-covid-19-vaccine- seroepidemiology of adenovirus serotypes 5, 26, 35, and 48 in
candidates-progress-to-clinical-trials/ (accessed June 25, 2020). pediatric and adult populations. Vaccine 2011; 29: 5203–09.
9 Zhu FC, Li YH, Guan XH, et al. Safety, tolerability, and 22 Chen N, Zhou M, Dong X, et al. Epidemiological and clinical
immunogenicity of a recombinant adenovirus type-5 vectored characteristics of 99 cases of 2019 novel coronavirus pneumonia in
COVID-19 vaccine: a dose-escalation, open-label, non-randomised, Wuhan, China: a descriptive study. Lancet 2020; 395: 507–13.
first-in-human trial. 395: 1845–54. 23 Yonker LM, Shen K, Kinane TB. Lessons unfolding from pediatric
10 Nie J, Li Q, Wu J, et al. Establishment and validation of a pseudovirus cases of COVID-19 disease caused by SARS-CoV-2 infection.
neutralization assay for SARS-CoV-2. Emerg Microbes Infect 2020; Pediatr Pulmonol 2020; 55: 1085–86.
9: 680–86. 24 Long QX, Tang XJ, Shi QL, et al. Clinical and immunological
11 Sprangers MC, Lakhai W, Koudstaal W, et al. Quantifying assessment of asymptomatic SARS-CoV-2 infections. Nat Med 2020;
adenovirus-neutralizing antibodies by luciferase transgene published online June 18. https://doi.org/10.1038/s41591-020-0965-6.
detection: addressing preexisting immunity to vaccine and gene 25 Chi X, Yan R, Zhang J, et al. A neutralizing human antibody binds
therapy vectors. J Clin Microbiol 2003; 41: 5046–52. to the N-terminal domain of the spike protein of SARS-CoV-2.
12 National Medical Products Administration, China. Technical Science 2020; published online June 22. https://doi.org/10.1126/
guidelines for clinical trials of vaccines. 2004. http://www.nmpa. science.abc6952.
gov.cn/WS04/CL2196/323471.html (accessed June 25, 2020). 26 WHO. Criteria for COVID-19 vaccine prioritization. 2020.
13 Li JX, Hou LH, Meng FY, et al. Immunity duration of a https://www.who.int/publications/m/item/criteria-for-covid-19-
recombinant adenovirus type-5 vector-based Ebola vaccine and vaccine-prioritization (accessed June 12, 2020).
a homologous prime-boost immunisation in healthy adults in
China: final report of a randomised, double-blind, placebo-
controlled, phase 1 trial. Lancet Glob Health 2017; 5: e324–34.
488 www.thelancet.com Vol 396 August 15, 2020
You might also like
- Sample: Georgia Department of Public HealthDocument1 pageSample: Georgia Department of Public HealthWSB-TV Assignment DeskNo ratings yet
- Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid ImmunityDocument12 pagesProtective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid ImmunityCTV CalgaryNo ratings yet
- Souvenir Book Updated Compressed-1 PDFDocument184 pagesSouvenir Book Updated Compressed-1 PDFManju Kumari100% (1)
- 2B. Deventer CalculatorDocument10 pages2B. Deventer CalculatorJhon Edi DVMNo ratings yet
- PIIS0140673620312083Document10 pagesPIIS0140673620312083kayegi8666No ratings yet
- Articles: BackgroundDocument11 pagesArticles: BackgroundCRS1973No ratings yet
- Remdesivir in Adults With Severe COVID-19: A Randomised, Double-Blind, Placebo-Controlled, Multicentre TrialDocument10 pagesRemdesivir in Adults With Severe COVID-19: A Randomised, Double-Blind, Placebo-Controlled, Multicentre TrialKinshuk ShekharNo ratings yet
- Piis0140673620310229 PDFDocument10 pagesPiis0140673620310229 PDFkayegi8666No ratings yet
- COVID 19 Vacunación en NiñosDocument13 pagesCOVID 19 Vacunación en NiñosSMIBA MedicinaNo ratings yet
- Wu 2015Document7 pagesWu 2015Noel Saúl Argüello SánchezNo ratings yet
- Sinovac JournalDocument10 pagesSinovac JournalGeulissa AddiniNo ratings yet
- Jurnal EED 3Document10 pagesJurnal EED 3Garsa GarnolNo ratings yet
- Final Efficacy Analysis, Interim Safety AnalysisDocument12 pagesFinal Efficacy Analysis, Interim Safety AnalysisGêmili BalbinotNo ratings yet
- 1 s2.0 S0140673621027537 MainDocument12 pages1 s2.0 S0140673621027537 Mainwaciy70505No ratings yet
- Artigo Lancet Coronavac 17-11-2020Document14 pagesArtigo Lancet Coronavac 17-11-2020Carlos LinsNo ratings yet
- Lectura de InmunologiaDocument10 pagesLectura de InmunologiaLuzmarina LinoNo ratings yet
- Background: OnlineDocument12 pagesBackground: OnlineCRS1973No ratings yet
- Safety, Tolerability and Immunogenicity of An Inactivated Sars-Cov-S VaccineDocument12 pagesSafety, Tolerability and Immunogenicity of An Inactivated Sars-Cov-S Vaccinezakaria alfajriNo ratings yet
- Jama Al Kaabi 2021 Oi 210057 1621966324.79302Document11 pagesJama Al Kaabi 2021 Oi 210057 1621966324.79302Rafiq Khanani DUHSNo ratings yet
- 四价登革热疫苗能有效预防亚洲健康儿童的登革热感染Document8 pages四价登革热疫苗能有效预防亚洲健康儿童的登革热感染Albert SongNo ratings yet
- CE (Ra) F (SH) PF1 (SY OM) PFA (OM) PN (KM)Document6 pagesCE (Ra) F (SH) PF1 (SY OM) PFA (OM) PN (KM)SUBHADIPNo ratings yet
- Fase 1.2Document11 pagesFase 1.2Verliatesya TugasNo ratings yet
- Efek Samping RemdesifirDocument11 pagesEfek Samping Remdesifirelsie versieNo ratings yet
- International Immunopharmacology: Meta-Analysis of Randomized Controlled TrialsDocument9 pagesInternational Immunopharmacology: Meta-Analysis of Randomized Controlled TrialsPujiNo ratings yet
- Articles: BackgroundDocument9 pagesArticles: Backgroundgilang_8899No ratings yet
- Gilbert2005 Studi HivDocument12 pagesGilbert2005 Studi HivErnawati HidayatNo ratings yet
- P009 Assessing The Status Quo Ulcerative Colitis.10Document2 pagesP009 Assessing The Status Quo Ulcerative Colitis.10Santiago ZamudioNo ratings yet
- Effectiveness of 2 Doses of Varicella Vaccine in Children: MajorarticleDocument4 pagesEffectiveness of 2 Doses of Varicella Vaccine in Children: MajorarticleYuni Eun WijayaNo ratings yet
- Candidiasis in PICUDocument6 pagesCandidiasis in PICUMeirinda HidayantiNo ratings yet
- Safety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineDocument35 pagesSafety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineAristegui NoticiasNo ratings yet
- MainDocument5 pagesMainFerdous HakimNo ratings yet
- Viral GeneticDocument10 pagesViral Geneticfirdaus.kabiruNo ratings yet
- PAPER FINALnejmoa2202261Document15 pagesPAPER FINALnejmoa2202261anitamanriquefcbNo ratings yet
- Safety and Immunogenicity of A Single Dose, Live-Attenuated Tetravalent Dengue Vaccine Feb 2022Document8 pagesSafety and Immunogenicity of A Single Dose, Live-Attenuated Tetravalent Dengue Vaccine Feb 2022Reinaldi octaNo ratings yet
- Articles: BackgroundDocument12 pagesArticles: BackgroundBudi Haryadi PNo ratings yet
- Different Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsDocument5 pagesDifferent Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsagboxNo ratings yet
- Remdesivir Covid 19Document10 pagesRemdesivir Covid 19nanaNo ratings yet
- Espondilodiscitis Infecciosa Por Patógenos Poco ComunesDocument5 pagesEspondilodiscitis Infecciosa Por Patógenos Poco ComunesOthoniel RamirezNo ratings yet
- Fase II: Oxford y AstraZeneca Publicaron en The Lancet Que Lograron 99% de Eficacia en Su Vacuna Contra El COVID-19Document15 pagesFase II: Oxford y AstraZeneca Publicaron en The Lancet Que Lograron 99% de Eficacia en Su Vacuna Contra El COVID-19Urgente24No ratings yet
- Estudio Publicado en Guangdong, China, Sobre La Contagiosidad de La Variante Delta de CoronavirusDocument18 pagesEstudio Publicado en Guangdong, China, Sobre La Contagiosidad de La Variante Delta de Coronavirussofia crottiNo ratings yet
- LC PDFDocument10 pagesLC PDFJorge Andres Balza GranadosNo ratings yet
- Nejmoa 1310422Document11 pagesNejmoa 1310422mz zumrodinNo ratings yet
- Community Acquired Pneumonia In+childrenDocument4 pagesCommunity Acquired Pneumonia In+childrendai shujuanNo ratings yet
- Pmid 36550736 IpiDocument6 pagesPmid 36550736 Ipiajaya basnetNo ratings yet
- Antibiotics 10 01088Document16 pagesAntibiotics 10 01088ahridulfoNo ratings yet
- Toxicology Reports: SciencedirectDocument6 pagesToxicology Reports: SciencedirectNoNWONo ratings yet
- Correlates of Protection Against Symptomatic and Asymptomatic Sars-Cov-2 InfectionDocument31 pagesCorrelates of Protection Against Symptomatic and Asymptomatic Sars-Cov-2 InfectionAbasyakira RaihanNo ratings yet
- High Prevalence of Azithromycin Resistance To Treponema Pallidum in Geographically Different Areas in ChinaDocument5 pagesHigh Prevalence of Azithromycin Resistance To Treponema Pallidum in Geographically Different Areas in Chinaselvia emilyaNo ratings yet
- Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine CandidatesDocument12 pagesSafety and Immunogenicity of Two RNA-Based Covid-19 Vaccine CandidatesOKE channelNo ratings yet
- Medi 96 E5864Document6 pagesMedi 96 E5864mono1144No ratings yet
- Article 1Document6 pagesArticle 1AMILA SYAZLINANo ratings yet
- Safety, Tolerability, and Immunogenicity of COVID-19 Vaccines A Systematic Review and PRE PRINTDocument31 pagesSafety, Tolerability, and Immunogenicity of COVID-19 Vaccines A Systematic Review and PRE PRINTVitória GabrieleNo ratings yet
- IDR 368857 Diagnosis and Treatment To A Post Craniotomy Intracranial inDocument7 pagesIDR 368857 Diagnosis and Treatment To A Post Craniotomy Intracranial inKadriye OvalıNo ratings yet
- Carbapenem-Pseudomonas AeruginosaDocument11 pagesCarbapenem-Pseudomonas AeruginosaMAYANo ratings yet
- Impact of Corticosteroid Therapy On Outcomes of Persons With Sars-Cov-2, Sars-Cov, or Mers-Cov Infection: A Systematic Review and Meta-AnalysisDocument9 pagesImpact of Corticosteroid Therapy On Outcomes of Persons With Sars-Cov-2, Sars-Cov, or Mers-Cov Infection: A Systematic Review and Meta-AnalysisMax CamargoNo ratings yet
- Efficacy and Safety of Rezafungin and Caspofungin in Candidaemia and Invasive CandidiasisDocument10 pagesEfficacy and Safety of Rezafungin and Caspofungin in Candidaemia and Invasive Candidiasisluis sanchezNo ratings yet
- Colistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM EvidenceDocument27 pagesColistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM Evidencerac.oncologyNo ratings yet
- PIIS1473309924000306Document11 pagesPIIS1473309924000306sazzad suvroNo ratings yet
- CDC Study On Effectiveness of COVID-19 VaccinesDocument8 pagesCDC Study On Effectiveness of COVID-19 VaccinesWSYX/WTTENo ratings yet
- Efficacy of Clinacanthus Nutans Extracts in PatientsDocument7 pagesEfficacy of Clinacanthus Nutans Extracts in Patientsconrad9richterNo ratings yet
- IDR 445826 Nirmatrelvir Ndash Ritonavir Reduced Mortality in HospitalizDocument11 pagesIDR 445826 Nirmatrelvir Ndash Ritonavir Reduced Mortality in HospitalizRowell NavarroNo ratings yet
- Diagnostic Imaging of Novel Coronavirus PneumoniaFrom EverandDiagnostic Imaging of Novel Coronavirus PneumoniaMinming ZhangNo ratings yet
- Rapid On-site Evaluation (ROSE): A Practical GuideFrom EverandRapid On-site Evaluation (ROSE): A Practical GuideGuoping CaiNo ratings yet
- Rates of Dark CO2 Fixation Are Driven by Microbial Biomass in A Temperate Forest SoilDocument58 pagesRates of Dark CO2 Fixation Are Driven by Microbial Biomass in A Temperate Forest SoilIsais NNo ratings yet
- Etoposide As Salvage Therapy For Cytokine Storm Due To COVID-19Document16 pagesEtoposide As Salvage Therapy For Cytokine Storm Due To COVID-19Adi permadiNo ratings yet
- Customization and External Validation of The Simplified Mortality Score For The Intensive Care Unit (SMS-ICU) in Brazilian Critically Ill PatientsDocument7 pagesCustomization and External Validation of The Simplified Mortality Score For The Intensive Care Unit (SMS-ICU) in Brazilian Critically Ill PatientsIsais NNo ratings yet
- Venous Blood Lactate Concentrations in Patients With Shock: Interesting But Not Really HelpfulDocument2 pagesVenous Blood Lactate Concentrations in Patients With Shock: Interesting But Not Really HelpfulIsais NNo ratings yet
- Risk of Incident Bleeding After Acute Kidney Injury: A Retrospective Cohort StudyDocument32 pagesRisk of Incident Bleeding After Acute Kidney Injury: A Retrospective Cohort StudyIsais NNo ratings yet
- Rates of Dark CO2 Fixation Are Driven by Microbial Biomass in A Temperate Forest SoilDocument58 pagesRates of Dark CO2 Fixation Are Driven by Microbial Biomass in A Temperate Forest SoilIsais NNo ratings yet
- The Opportunity Costs of Caring For People With Dementia in Southern SpainDocument7 pagesThe Opportunity Costs of Caring For People With Dementia in Southern SpainIsais NNo ratings yet
- Covid 19 y Tratamiento Embolia PulmonarDocument27 pagesCovid 19 y Tratamiento Embolia PulmonarSMIBA Medicina100% (1)
- Electrolyte Measurement - Myths and Misunderstandings - Part IIDocument11 pagesElectrolyte Measurement - Myths and Misunderstandings - Part IIIsais NNo ratings yet
- Should We Ban Live Surgery?Document2 pagesShould We Ban Live Surgery?Isais NNo ratings yet
- Risk of Incident Bleeding After Acute Kidney Injury: A Retrospective Cohort StudyDocument32 pagesRisk of Incident Bleeding After Acute Kidney Injury: A Retrospective Cohort StudyIsais NNo ratings yet
- Initial Assessment, Risk Stratification, and Early Management of Acute Nonvariceal Upper Gastrointestinal HemorrhageDocument15 pagesInitial Assessment, Risk Stratification, and Early Management of Acute Nonvariceal Upper Gastrointestinal HemorrhageIsais NNo ratings yet
- Inadequate Prophylactic Effect of Low-Molecular Weight Heparin in Critically Ill COVID-19 PatientsDocument4 pagesInadequate Prophylactic Effect of Low-Molecular Weight Heparin in Critically Ill COVID-19 PatientsIsais NNo ratings yet
- Emerging Endoscopic Treatments For Nonvariceal Upper Gastrointestinal HemorrhageDocument14 pagesEmerging Endoscopic Treatments For Nonvariceal Upper Gastrointestinal HemorrhageIsais NNo ratings yet
- Foreword Upper and Lower Gastrointestinal Bleeding: Everything You Need To KnowDocument2 pagesForeword Upper and Lower Gastrointestinal Bleeding: Everything You Need To KnowIsais NNo ratings yet
- Initial Assessment, Risk Stratification, and Early Management of Acute Nonvariceal Upper Gastrointestinal HemorrhageDocument15 pagesInitial Assessment, Risk Stratification, and Early Management of Acute Nonvariceal Upper Gastrointestinal HemorrhageIsais NNo ratings yet
- Development and Licensure of Vaccines To Prevent COVID-19 Guidance For IndustryDocument24 pagesDevelopment and Licensure of Vaccines To Prevent COVID-19 Guidance For IndustryIsais NNo ratings yet
- J. Hauer Et Al Leukemia 2020 PrePrintDocument8 pagesJ. Hauer Et Al Leukemia 2020 PrePrintIsais NNo ratings yet
- The Key Role of Education in The Europe 2020 Strategy: SSRN Electronic Journal October 2010Document20 pagesThe Key Role of Education in The Europe 2020 Strategy: SSRN Electronic Journal October 2010Isais NNo ratings yet
- Europe 2020: A Europe Strategy For Smart, Sustainable and Inclusive Growth.Document37 pagesEurope 2020: A Europe Strategy For Smart, Sustainable and Inclusive Growth.EKAI CenterNo ratings yet
- Endotherapy of Peptic Ulcer BleedingDocument13 pagesEndotherapy of Peptic Ulcer BleedingIsais NNo ratings yet
- The Europe 2020Document18 pagesThe Europe 2020Isais NNo ratings yet
- Vaccination Schedule: Infants Toddlers Children Adolescents AdultsDocument1 pageVaccination Schedule: Infants Toddlers Children Adolescents AdultsIsais NNo ratings yet
- Undocumented Migrants and The Europe 2020 Strategy:: Making Social Inclusion A Reality For All Migrants inDocument20 pagesUndocumented Migrants and The Europe 2020 Strategy:: Making Social Inclusion A Reality For All Migrants inIsais NNo ratings yet
- Canada-COVID-19 Vaccine Letter May 21st 2020 - UpdatedDocument4 pagesCanada-COVID-19 Vaccine Letter May 21st 2020 - UpdatedIsais NNo ratings yet
- 2020-European Semester Country-Report-Germany enDocument93 pages2020-European Semester Country-Report-Germany enIsais NNo ratings yet
- Suspending Classes Without Stopping Learning: China's Education Emergency Management Policy in The COVID-19 OutbreakDocument6 pagesSuspending Classes Without Stopping Learning: China's Education Emergency Management Policy in The COVID-19 OutbreakMeicy CimeNo ratings yet
- Covid-19: Russia Approves Vaccine Without Large Scale Testing or Published ResultsDocument2 pagesCovid-19: Russia Approves Vaccine Without Large Scale Testing or Published ResultsIsais NNo ratings yet
- Germany: Economic Growth Is Driven Increasingly by Domestic DemandDocument3 pagesGermany: Economic Growth Is Driven Increasingly by Domestic DemandIsais NNo ratings yet
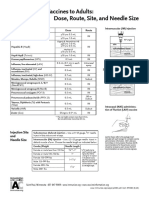
- Administering Vaccines To Adults: Dose, Route, Site, and Needle SizeDocument1 pageAdministering Vaccines To Adults: Dose, Route, Site, and Needle SizeAkashNo ratings yet
- Pediatric TB and HIV: The Potential of New TB VaccinesDocument27 pagesPediatric TB and HIV: The Potential of New TB VaccinesBarnabasNatambaNo ratings yet
- Portfolio IN Community Health Nursing: Submitted byDocument7 pagesPortfolio IN Community Health Nursing: Submitted byJay VillasotoNo ratings yet
- 67166-Apvma Veterinary Medicines Technical Report TemplateDocument42 pages67166-Apvma Veterinary Medicines Technical Report Templateali aimanNo ratings yet
- Office: Directors FOR Health OF Health Region Directors Medical Treatment RehabilitationDocument4 pagesOffice: Directors FOR Health OF Health Region Directors Medical Treatment RehabilitationDiwata OndeNo ratings yet
- Immunization P & SDocument122 pagesImmunization P & SnebilNo ratings yet
- Coronavirus (COVID-19) RecordsDocument2 pagesCoronavirus (COVID-19) RecordsVivek ElangovanNo ratings yet
- Irr Final DraftDocument7 pagesIrr Final Draftapi-571861077No ratings yet
- Annotated Bibliography Aasha TurnerDocument8 pagesAnnotated Bibliography Aasha Turnerapi-644326339No ratings yet
- Postest Imunitation-Alif Sachrul M-I1J020006-1Document3 pagesPostest Imunitation-Alif Sachrul M-I1J020006-1ARUM APRIANI 1No ratings yet
- CertificateDocument1 pageCertificateSubhajit MandalNo ratings yet
- Amicus BriefDocument27 pagesAmicus BriefThe FederalistNo ratings yet
- Perbedaan IPV Dan OPVDocument9 pagesPerbedaan IPV Dan OPVIntan SaraswatiNo ratings yet
- Materi - Webinar - Dr. Apt. Tiana Milanda, M.si.Document39 pagesMateri - Webinar - Dr. Apt. Tiana Milanda, M.si.DWI RAHMA HALIDANo ratings yet
- Aefi Reporting, Investigation & ManagementDocument23 pagesAefi Reporting, Investigation & ManagementPrabir Kumar ChatterjeeNo ratings yet
- Adjuvants Used in VaccinesDocument15 pagesAdjuvants Used in VaccinesVon Valentine MhuteNo ratings yet
- Narrative Report: Polio Outbreak Response Immunization Bopv Round 2Document4 pagesNarrative Report: Polio Outbreak Response Immunization Bopv Round 2Cristina MelloriaNo ratings yet
- Small Pox: General VirologyDocument24 pagesSmall Pox: General VirologyFahad HassanNo ratings yet
- Research Proposal: Statement in BOLD)Document4 pagesResearch Proposal: Statement in BOLD)sana mehtabNo ratings yet
- BSMT Ay 2021-2022Document45 pagesBSMT Ay 2021-2022Crystal AnnNo ratings yet
- India's COVID-19 Vaccina On Program: CFM Individual Wri/en Assignment 1Document3 pagesIndia's COVID-19 Vaccina On Program: CFM Individual Wri/en Assignment 1Ayushi ThakkarNo ratings yet
- G2 Travel COVID-19 Update - May 2021Document38 pagesG2 Travel COVID-19 Update - May 2021Megawati SyahfitriNo ratings yet
- Marketing ManagenentDocument2 pagesMarketing Managenentsiyam sharifNo ratings yet
- Harvard Epidemiologist Says The Case For COVID Vaccine Passports Was Just DemolishedDocument6 pagesHarvard Epidemiologist Says The Case For COVID Vaccine Passports Was Just DemolishedMassimo RiserboNo ratings yet
- Vaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDADocument1 pageVaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDAAbdul YounusNo ratings yet
- Community Health Nursing: Unit Title/SDocument4 pagesCommunity Health Nursing: Unit Title/SNicole LantinNo ratings yet
- Citizenship and Social Development (Sample Paper)Document7 pagesCitizenship and Social Development (Sample Paper)JamieNo ratings yet