Professional Documents
Culture Documents
F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)
Uploaded by
Dasha VeeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)
Uploaded by
Dasha VeeCopyright:
Available Formats
OBSTETRICS 2
F06. STD and INFECTIONS IN PREGNANCY (Part 1)
Dr. Jandoc | May 03, 2019
OUTLINE
I. INFECTIONS/STI in PREGNANCY
II. PREGNANCY SAFETY INDEX
III. CERVICAL INFECTIONS
IV. VAGINAL INFECTIONS
V. GENITAL ULCER INFECTIONS
VI. CONSIDERATION IN THE MANAGEMENT OF GENITAL ULCERS
I. INFECTIONS/STI in PREGNANCY
Pregnant women CAN become infected with the STI same as non-pregnant women
Pregnancy DOES NOT provide women or their babies any protection against STI
Consequences may be more serious, even life threatening, for a woman and her baby
II. PREGNANCY SAFETY INDEX
(US FDA pregnancy categories)
Category A Proven safe because of controlled studies in women failed to demonstrate a risk to the fetus in the first trimester (and no evidence of a risk in later trimesters) and the
possibility of fetal harm remains remote
Studies in humans and animals
Ex. Pre-natal vitamins, multivitamins
Category B Either animal reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women or animal reproduction studies have shown an adverse
effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the 1st trimester (and there is no evidence of a risk in later trimesters).
Studies on animals not on humans, no abnormalities seen in pregnant women, where most medications belong)
Ex. antibiotics, acid-related disorders medications, analgesic
Category C Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal or other) and no adequate and well-controlled studies in humans. Drugs should be
given only if the potential benefit justifies the potential risk to the fetus
No controlled studies both in animals and humans, but no congenital abnormalities in women who use these drugs
Category D There is positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (e,g if the drug is needed in a life threatening
situation or for a serious disease for which safer drugs cannot be used or are ineffective)
Proven abnormality seen when medication is administered but benefit for use in pregnant women outweighs the risk
Category X Studies in animals or humans have demonstrated fetal abnormalities or there is evidence of fetal risk based on human experience or both, and the risk of the use of the drug in
pregnant women clearly outweighs any possible benefits. The drug is contraindicated in women who are or may become pregnant.
Proven fetal risk and risks outweigh benefits
Ex. anti-convulsant drugs, Tretinoin
*Both categories D and X show fetal risks but the use of category X outweighs the benefits
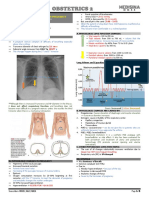
ETIOLOGIC CLINICAL CHARACTERISTICS DIAGNOSIS IMPLICATIONS DURING MANAGEMENT
AGENT PREGNANCY
III. CERVICAL INFECTIONS
A. GONORRHEA Neisseria Gonococcal Cervicitis G/S of endocervical swab Gonococcal infection can have Cefixime 400 mg. orally single dose OR
Gonorrhea Symptoms: yellowish, mucoid cervical (result: Smear shows deleterious effects in any trimester. Ceftriaxone 250 mg IM single dose (1
discharge positive for intracellular In pregnancy is associated with: vial is 500 mg) + 1g oral azithromycin
Hyperemic, edematous gram-negative Low birth weight 3rd-5th generations: Category B
diplococci with few pus Premature delivery safe to give to pregnant
For men who have this condition, they present cells) Preterm rupture of membrane 4th and 5th gen cephalosporins are
more acutely than those women who have Culture Chorioamnionitis for those resistant to earlier
gonorrhoea: Pus on urinalysis (purulent nucleic acid amplification Postpartum sepsis generations
urethral discharge) tests (NAATs) – have Secondary infertility – those PLUS
replaced cultures in most who suffer from PID then tries Treatment for non-gonococcal urethritis
laboratories to get pregnant for the second or cervicitis
time
Conjunctivitis (ophthalmia neonatorum) “sticky Diagnosis may also use
eye” gram staining/culture of
Transcribers: BOMOWEY, ESTEPA, FIANZA Page 1 of 5
OBSTETRICS 2
Purulent conjunctival discharge 2-5 days after conjunctival swab also show
birth intracellular gram-negative
Disseminated neonatal infection diplococci
Extra-genital Gonorrhea:
Arthritis – often affects the knee, may cause
joint destruction
Rash – septicemia/Blood infection
Eye infection: get a thorough history
o By swimming and diving ;P
You have to have suspicion. Try to look at the more
common etiologies rather than the least common
ones. Then check also the partner.
B. NON- Chlamydia If patient has Gonorrhea, most likely she has Culture In pregnancy is associated with: DOC (non-pregnant): Doxcycycline:
GONOCOCCAL Trachomatis Chlamydia NAATs Low birth weight Tetracycline (Category C/D: not safe)
CERVICITIS Gram stain: polymorphonuclear but absence of Premature delivery Choose other meds that are safer which
IP = 1-12 days to 3 Gram (-) diplococci Preterm rupture of membrane could be:
mos. Cervical erosions compared to gonorrhea, Chorioamnionitis Azithromycin: Macrolide (Category B:
chlamydia causes more destruction leading to Postpartum sepsis safe)
pelvic inflammatory disease causing infertility Erythromycin: Macrolide (Category B:
IP = 1-12 days to 3 mos. safe) – avoided because of drug-related
When treating gonorrhea, also treat for chlamydia hepatotoxicity
Both are gastric irritants so advise to
take with full meals but Doxycycline is
the most gastric irritant
IV. VAGINAL INFECTIONS
A. Trichomonas Profuse, frothy, greenish-yellow, vaginal Wet mount: pear-shaped Some studies have linked Metronidazole 2 grams PO single
TRICHOMONIASI vaginalis discharge, “fishy-odor” trichomonads with WBCs trichomonal infection with preterm dose OR
S “Strawberry cervix” because of petechiae birth. A few other studies implicate o also DOC for Ameobiasis TID;
IP: 3-28 days Severe vaginal pruritus leading to this infection with preterm premature Category B: safe
(average 5-10 thickened/reddened vulva rupture of membranes and small-for- Metronidazole 500 mg. BID for 7
days) Dysuria due to vulvar inflammation gestational age newborns days
Dyspareunia
B. BACTERIAL Gardnerella May or may not be sexually transmitted but Gram staining of vaginal Important to treat them Metronidazole 500 mg. PO BID x 7 days
VAGINOSIS vaginalis you have to treat swab because to them, it may be Metronidazole 2 grams. PO SD
Mycoplasma Tell-tale sign is CLUE nothing but it may lead to Metronidazole – category B
Anaerobes Clinical Features: CELLS (indistinct premature rupture of
Homogenous discharge gravid margin and a membranes, preterm labor,
Thin white to greyish homogenous discharge, refractile granular prematurity
coating the walls of the vagina appearance due to a
Asymptomatic in 50% large number of
adherent bacteria)
Clinical Diagnosis:
three of the four following criteria
are present:
1. vaginal pH >4.5;
2. a thin, milky, noninflammatory
vaginal discharge;
3. >20 percent clue cells seen
microscopically; and
4. a fishy odor after addition of
10-percent potassium hydroxide
to vaginal secretion samples (+
whiff test)
Transcribers: BOMOWEY, ESTEPA, FIANZA Page 2 of 5
OBSTETRICS 2
C. VAGINAL Candia Thick, curd-like cheesy vaginal discharge with - Direct visualization of The link between candidiasis and Clotrimazole 100 mg Vaginal
CANDIDIASIS albicans whitish plaques pseudohyphae preterm birth is not robust Suppository OD X 7 days (Category B
Severe pruritus in the vulva/anal region vaginal preparation – safe)
Dysuria / painful urination Clotrimazole 500 mg per vagina SD
Painful sexual intercourse Miconazole 400 mg per vagina each
50% asymptomatic night for 3 days (Broader effect
Not a sexually transmitted infection because however it is under Category C)
there is a certain number of normal flora in the Good personal hygiene
vagina that would show candida but in a small
percentage; may be due to alteration of
immune system in pregnancy - immune system
is down, there is overgrowth of anaerobes
symptomatic
Becomes STI if a woman has contact with a
man with candidiasis
V. GENITAL ULCER INFECTIONS
A. SYPHILIS Treponema a. Primary Lesion (chancre) Dark field microscopic of Fetal infection through several A. Early Syphilis (Primary, Secondary,
Pallidum b. Secondary Lesion – eruption involving skin and specimens obtained from routes (transplacental, Early Latent <2 yrs.)
mucous membranes, long periods of latency the chancre and secondary perinatal) Benzathine Penicillin G 2.4 M Units
c. Late/Tertiary Lesions – of skin, bone, viscera, syphilitic lesions IM SD (Category B:safe)
CNS, cardiovascular system Serologic test for syphilis:
RPR If allergic to
If allergic to
1. EARLY infectious Penicillin and
Penicillin
a. Primary: IP 9-90 days Pregnant
b. Secondary: 6 wks. – 6 mos. (4-8 wks. after Doxycycline 200 Ceftriaxone 250
primary lesion) mg orally BID x mg. IM every
c. Latent (early): <2 years 14D other day for 10
Tetracycline doses (Category
2. LATE (non-infectious) 500 mg. orally B)
QID x 14D
-20 years
-40 yrs. B. Late Syphilis (Late Latent >2 years)
Gummatous syphilis 3-12 yrs. after primary Benzathine Penicillin G 2.4 M units
infection IM weekly for 3 doses for a total of
7.2 M units
If allergic to
If allergic to
Penicillin and
Penicillin
Pregnant
Doxycycline 200 Ceftriaxone 250
mg orally BID x mg. IM every
4 weeks other day for 10
Tetracycline doses
500 mg. orally
QID x 4 weeks
1. Primary Solitary and painless lesions
syphilis Red macule that progresses to a papule and finally ulcerates
Inguinal lymph nodes moderately enlarge, painless
Primary lesions will heal w/in 3-10 week, may go unnoticed
Lesions on the cervix, rectum, and anal canal may be asymptomatic
2. Secondary Skin lesions
syphilis Mucous membrane lesions
Generalized lymphadenopathy
Arthritis, arthralgia, and periostitis
Alopecia and neurologic disease
Rare Features:
Hepatitis
Glomerulonephritis, nephritic syndrome
Iridocyclitis and choroidoretinitis
Transcribers: BOMOWEY, ESTEPA, FIANZA Page 3 of 5
OBSTETRICS 2
Neurological disease (meningitis, cranial nerve palsies)
Alopecia
Classic rash - red macules & papules over palms of hand & soles of feet, larger than
herpetic ulcers, & not tender unless secondarily infected.
Papular lesions can become large and coalesce to form large, fleshy masses (condyloma
lata) - seen in anus and labia (genitals)
3. Tertiary Granulomatous, painless lesions 3-12 years after the primary infection
syphilis May occur on the skin, mucous membrane, bone or viscera
a. Neurosyphilis 10-20 years after primary infection
General paralysis of the insane
Irritability, delusions, seizures, etc
Tabes dorsalis (dorsal column impairment)
o Increasing ataxia
o Falling vison, sphincter disturbances, attacks of severe pain
o absent ankle and knee reflexes
b. Cardiovascular Aortic regurgitation, angina, and aortic aneurysm
syphilis 10 – 40yrs after primary infection
B. GENITAL Herpes Simplex Clinical features: Virological: PCR or culture Maternal primary HSV infection Management:
HERPES type ll Painful genital lesions type-specific serological during pregnancy is associated Primary
May start with a prodrome of irritation or tests. with: 1. Acyclovir 400 mg PO TID for 7-10
IP: 2 -14 days after paresthesia at the site of the future lesions Spontaneous abortion <20 days or 200 mg 5x a day for 7-10 days
exposure Lymphadenopathy wks AOG (Category B)
Other systemic manifestations: fever, Low birth weight 2. Famciclovir – 250 mg TID for 7 -10
headache, myalgia Premature delivery >20 wks days (Category B)
Herpes Simplex Recurrent lesions may occur after 1-4 months AOG 3. Valacicclovir – 1gm PO BID for 7-
Type I – stomatitis Genital herpes is lifelong chronic condition Stillbirth 10 days (Category B)
(unable to eat, left The virus becomes latent in a local sensory
with semi-solid ganglion Genital Herpes in Pregnancy Secondary
foods because Suspected primary genital Acyclovir 400 mg. orally 3x a day for
lesions are very Main Symptoms: herpes acquired during the 5 days OR
painful) FIRST EPISODE/PRIMARY EPISODE third trimester of pregnancy Valacyclovir 500 mg. orally 2x a day
Multiple painful genital ulcers starting as Offered acyclovir antiviral for 5 days
vesicles (parang singaw sa oral cavity) treatment
Constitutional symptoms: fever, malaise, Delivered by elective LSCS if
headache, photophobia, and occasional labor occurs within six weeks
retention of urine after diagnosis
RECURRENT EPISODES/SECONDARY EPISODE
Less severe ulceration, sometimes preceded by
prodromal symptoms, ie. tingling sensation
C. GRANULOMA Klebsiella Characteristics: Laboratory Diagnosis Oral broad-spectrum Antibiotics
INGUINALE granulomatis Primary lesion: asymptomatic (painless) papule with Giemsa stain: macrophage TMT sulfamethoxazole 800 mg
(formerly elevated & irregular edges which ulcerates giving rise with vacuoles containing BID for 3 days (Category D) OR
calymmatobacteriu to a beefy red ulcer with fresh granulation tissue bipolar- staining bacilli Doxycycline 100 mg BID for
m) (Donovan bodies) – Board minimum of 3 weeks (Category D)
Exam question Alternative:
IP: 1-4 wks. (up to Ciprofloxacin 750mg BID for
6 months) minimum of 3 weeks
Erythromycin base 500 mg
QID for minimum of 3 weeks
(Category B) – more preferred
*Fluoroquinolones – DOC for UTI but not
safe, change to Ceftriaxone
Repeat urinalysis
D. Chlamydia Characteristics: Treatment: Similar for chlamydia
LYMPHOGRANUL trachomatis Chronic infection of lymphatic tissue 1. Doxcycycline 100 mg BID for 21 days
OMA VENEREUM Vulva – most frequent site of infection 2. Erythromycin base 500 mg QID for 21
IP: 3 days – 6 Subclinical infection is common days
Transcribers: BOMOWEY, ESTEPA, FIANZA Page 4 of 5
OBSTETRICS 2
weeks 3 Distinct Phases: 3. I & D of infected nodes
1. Primary infection Extensive surgical reconstruction for the
Shallow and painless papule, pustule or destructive tertiary phase so you have to
vesicles, heals without treatmen clean your wounds
2. Secondary phase
Painful inguinal & perirectal adenopathy
1-4 weeks after primary infection
If untreated, infected nodes become
tender & enlarged forming bubos
3. Tertiary phase
“Groove sign”/double genitocrucal folds
Bubos rupture producing multiple sinuses
& fistulas in 7-15 days
L. CHANCROID Haemophilus Characteristics: Appropriate media are not widely 1. Azithromycin - 1gm single dose
ducreyi Distinct feature: kissing lesion accessible, and no Food and Drug 2. Ceftriaxone - 250 mg IM single dose
Soft, painful, anogenital ulcers Administration (FDA)-cleared PCR 3. Ciprofloxacin - 500 mg BID for 3 days
Ulcers single or multiple test is yet available. Instead, for non-pregnant
Purulent base painful genital ulcer(s) and 4. Erythromycin base - 500 mg QID x 7
Contact bleeding negative screening for syphilis or days
Tender inguinal lymphadenopathy HSV leads to a presumptive
diagnosis.
VI. CONSIDERATION IN THE MANAGEMENT OF GENITAL ULCERS
Patient must be informed about the natural history of the disease:
Potential for recurrent episodes
Asymptomatic viral shedding and sexual transmission
Use of condoms during all sexual exposures with new uninfected partners must be encouraged because it can prevent reinfection
The risk of neonatal infection should be explained
Giving antiviral therapy during recurrent episodes might shorten the duration of lesions
Suppressive antiviral therapy can ameliorate or prevent recurrent outbreaks
CHECKPOINT
a. Syphilis
b. Gonorrhea
c. Candidiasis
d. Bacterial Vaginosis
e. Trichomoniasis
f. Chlamydia
g. Granuloma Inguinale
h. Genital Herpes
i. Chancroid
1. Strawberry Cervix
2. Clue Cells
3. Classic Rash
4. Donovan Bodies 1. E
5. Causes Ophthalmia Neonatorum 2. D
3. A
6. Kissing lesions 4. G
7. Chancre 5. B
8. Pseudohyphae in KOH 6. I
7. A
8. C
Transcribers: BOMOWEY, ESTEPA, FIANZA Page 5 of 5
You might also like
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageFrom EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaNo ratings yet
- EndometritisDocument9 pagesEndometritisSANTIAGO LOPEZ ROJASNo ratings yet
- Monkeypox and Pregnancy - What Maternal-Fetal Medicine Subspecialists Need To KnowDocument7 pagesMonkeypox and Pregnancy - What Maternal-Fetal Medicine Subspecialists Need To KnowariniNo ratings yet
- STI&STDDocument5 pagesSTI&STDRica Joy Sulicipan FiestaNo ratings yet
- Annotated PDFDocument5 pagesAnnotated PDFMatias Alarcon ValdesNo ratings yet
- Types of Spontaneous AbortionDocument5 pagesTypes of Spontaneous AbortionAnnalisa TellesNo ratings yet
- Ectopic PregnancyDocument6 pagesEctopic PregnancyChristine Evan HoNo ratings yet
- Slide 1 STIDocument50 pagesSlide 1 STIMatth N. ErejerNo ratings yet
- Maternal LEC - Week 11 - TransesDocument4 pagesMaternal LEC - Week 11 - TransesEcka- EckaNo ratings yet
- Sexually Transmitted DiseaseDocument3 pagesSexually Transmitted DiseaseBrianna ValerioNo ratings yet
- Management of Varicella Infection (Chickenpox) in Pregnancy: Sogc Clinical Practice GuidelineDocument10 pagesManagement of Varicella Infection (Chickenpox) in Pregnancy: Sogc Clinical Practice GuidelineimeldahermnNo ratings yet
- Care of Mother, Child at Risks With Problems (Acute & Chronic) : Transcript Onsexually Transmitted InfectionDocument4 pagesCare of Mother, Child at Risks With Problems (Acute & Chronic) : Transcript Onsexually Transmitted InfectionMark Gregory Addatu100% (1)
- Chapter 10. Prevention of Pregnancy and Sexually Transmitted InfectionsDocument24 pagesChapter 10. Prevention of Pregnancy and Sexually Transmitted InfectionsMonica CiorneiNo ratings yet
- Pathway:: Abnormal Vaginal Discharge - Management and Laboratory DiagnosisDocument5 pagesPathway:: Abnormal Vaginal Discharge - Management and Laboratory DiagnosisMarsya Yulinesia LoppiesNo ratings yet
- Ob Topic 1 - Pprom - NCPDocument2 pagesOb Topic 1 - Pprom - NCPThelly MargalloNo ratings yet
- Management of Varicella Infection (Chickenpox) in Pregnancy: Sogc Clinical Practice GuidelineDocument6 pagesManagement of Varicella Infection (Chickenpox) in Pregnancy: Sogc Clinical Practice Guidelineabu abdirrahmanNo ratings yet
- Midwifery and Obstetrical Nursing Seminar on InfertilityDocument21 pagesMidwifery and Obstetrical Nursing Seminar on Infertilityshraddha singhNo ratings yet
- NCM 109 Gyne Supplemental Learning Material 1Document25 pagesNCM 109 Gyne Supplemental Learning Material 1Zack Skyler Guerrero AdzuaraNo ratings yet
- Ovarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuDocument5 pagesOvarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuAndriyani MuslimNo ratings yet
- Livret MF GB21Document20 pagesLivret MF GB21mary15eugNo ratings yet
- Emergency Obstetrics1Document74 pagesEmergency Obstetrics1Alphine DalgoNo ratings yet
- Toolbox: Ectopic PregnancyDocument4 pagesToolbox: Ectopic PregnancyLuciana LorenzaNo ratings yet
- OB-GYN 101: Vaginal DischargeDocument8 pagesOB-GYN 101: Vaginal Dischargemadmax500No ratings yet
- Ginekologi Di FKTPDocument27 pagesGinekologi Di FKTPNadyNo ratings yet
- STI Prevention and TreatmentDocument6 pagesSTI Prevention and TreatmentGenelly Anne Argañoza RamosNo ratings yet
- Urogenital Infections Linked to Preterm LaborDocument4 pagesUrogenital Infections Linked to Preterm LaborPangalanitaNo ratings yet
- M. Preterm and Postterm - NewDocument92 pagesM. Preterm and Postterm - NewTry Ariditya UtomoNo ratings yet
- Puerperium ComplicationsDocument28 pagesPuerperium ComplicationsyayayanizaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyThomas Regina PutraNo ratings yet
- Ectopic Pregnancy Definition of DisorderDocument48 pagesEctopic Pregnancy Definition of DisorderWRONGHEAR100% (1)
- 076 Rubella IgG-V2.5-EN-20130806Document4 pages076 Rubella IgG-V2.5-EN-20130806Iancu Adina FloricicaNo ratings yet
- Journal Pone 0272828Document10 pagesJournal Pone 0272828Amanda ShermanNo ratings yet
- 6 of Vaginal DischargeDocument4 pages6 of Vaginal DischargePanjul NugrohoNo ratings yet
- Jurnal 2Document18 pagesJurnal 2Muhammad Pebri Nilhakim ZavbmNo ratings yet
- Vaginal DischargeDocument7 pagesVaginal DischargeInggitaDarmawanNo ratings yet
- 2020 Schindler Cystic-Ovarian-EndometriosisDocument4 pages2020 Schindler Cystic-Ovarian-EndometriosisAvicenna 2016No ratings yet
- Postpartum Uterine Infections: Department of Theriogenology University of Veterinary & Animal Sciences, LahoreDocument24 pagesPostpartum Uterine Infections: Department of Theriogenology University of Veterinary & Animal Sciences, LahoreMuhammad JameelNo ratings yet
- Obstetrics: Positive, But Upon Workup There Is No Pregnancy. It's D/T Cross Reaction To HCGDocument6 pagesObstetrics: Positive, But Upon Workup There Is No Pregnancy. It's D/T Cross Reaction To HCGPencenk AzznewNo ratings yet
- Gynaecology: Gum, Fertility, Contraception, and UrogynaecologyDocument46 pagesGynaecology: Gum, Fertility, Contraception, and UrogynaecologyOccamsRazorNo ratings yet
- Chapterone ProblemanditsscopeDocument5 pagesChapterone ProblemanditsscopeIbraNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument40 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Gynaecology: Dr. Chintamani Mohanta Dr. Kumudini PradhanDocument7 pagesGynaecology: Dr. Chintamani Mohanta Dr. Kumudini PradhanPrima Hari PratamaNo ratings yet
- Ectopic PregnancyDocument2 pagesEctopic PregnancyKryzl Anne LigsayNo ratings yet
- Journal ReadingDocument21 pagesJournal ReadingMelvita KurniawanNo ratings yet
- Idog 03 210Document7 pagesIdog 03 210jwmeadow2401No ratings yet
- Causes and management of common vaginal dischargesDocument8 pagesCauses and management of common vaginal dischargesMELVYN HAROLD CHAVEZ MAURICIONo ratings yet
- Dermatological Disorders Unique To Pregnancy: January 2009Document14 pagesDermatological Disorders Unique To Pregnancy: January 2009mutmainnahNo ratings yet
- Yayin Ob: 2. Trichomonas VaginalisDocument3 pagesYayin Ob: 2. Trichomonas VaginalisYayin PestañoNo ratings yet
- Definition of Premature Rapture of Membrane (Document3 pagesDefinition of Premature Rapture of Membrane (Merly Grael LigligenNo ratings yet
- Infectious Diseases in PregnancyDocument8 pagesInfectious Diseases in PregnancyPabinaNo ratings yet
- Case 3 CP 1Document14 pagesCase 3 CP 1Rose Nene BuenavistaNo ratings yet
- Selecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)Document7 pagesSelecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)eva yustianaNo ratings yet
- Jama Owens 2020 Us 200005Document7 pagesJama Owens 2020 Us 200005jimenacuadradoanguloNo ratings yet
- In Vitro FertilizationDocument10 pagesIn Vitro FertilizationMoe AboamNo ratings yet
- Ectopic PregnancyDocument76 pagesEctopic PregnancyVivian Jean TapayaNo ratings yet
- Endometrial MicrobiotaDocument12 pagesEndometrial MicrobiotaHAVIZ YUADNo ratings yet
- Paper On Bact VaginosisDocument16 pagesPaper On Bact VaginosisWael GaberNo ratings yet
- Ncbi NLM Nih Gov@pmc2760892Document2 pagesNcbi NLM Nih Gov@pmc2760892aisyahNo ratings yet
- Early and Late Infections in Newborns: Where Do We Stand? A ReviewDocument9 pagesEarly and Late Infections in Newborns: Where Do We Stand? A ReviewfadmayulianiNo ratings yet
- GYNE 4.01a EndometriosisDocument4 pagesGYNE 4.01a EndometriosisGray SnellNo ratings yet
- The Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDocument14 pagesThe Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDasha VeeNo ratings yet
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 pagesF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeNo ratings yet
- Pulmonary Disorders in PregnancyDocument5 pagesPulmonary Disorders in PregnancyDasha VeeNo ratings yet
- OB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDocument1 pageOB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDasha VeeNo ratings yet
- WJR 5 113Document13 pagesWJR 5 113Valian IndrianyNo ratings yet
- Diagnostico y Manejo de Masas AnexialesDocument6 pagesDiagnostico y Manejo de Masas AnexialesChristopher Hernán Valenzuela ArancibiaNo ratings yet
- F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDocument10 pagesF.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDasha VeeNo ratings yet
- F.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDocument5 pagesF.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDasha VeeNo ratings yet
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Document48 pagesPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeNo ratings yet
- F.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDocument4 pagesF.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDasha VeeNo ratings yet
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 pagesF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeNo ratings yet
- Practice Bulletin: Management of Adnexal MassesDocument14 pagesPractice Bulletin: Management of Adnexal MassesDasha VeeNo ratings yet
- Embryogenesis & Fetal DevelopementDocument38 pagesEmbryogenesis & Fetal DevelopementDasha Vee100% (1)
- Pulmonary Disorders in PregnancyDocument5 pagesPulmonary Disorders in PregnancyDasha VeeNo ratings yet
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Document4 pagesObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeNo ratings yet
- 2011 Full Page Calendar - TomKat StudioDocument12 pages2011 Full Page Calendar - TomKat StudioThe TomKat StudioNo ratings yet
- m.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Document4 pagesm.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Dasha VeeNo ratings yet
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Document3 pagesP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeNo ratings yet
- Thyroid PDFDocument9 pagesThyroid PDFDasha VeeNo ratings yet
- Mental HealthDocument4 pagesMental HealthDasha VeeNo ratings yet
- DiagnosisDocument8 pagesDiagnosisDasha VeeNo ratings yet
- Antiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDocument8 pagesAntiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDasha VeeNo ratings yet
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocument140 pagesPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingNo ratings yet
- P.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Document4 pagesP.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Dasha VeeNo ratings yet
- Ob Osce.04 CTG ReadingDocument6 pagesOb Osce.04 CTG ReadingDasha VeeNo ratings yet
- M.10B Drugs Used in Gastrointestinal DisordersDocument3 pagesM.10B Drugs Used in Gastrointestinal DisordersDasha VeeNo ratings yet
- F.09 BONE RADIOLOGY - Dr. GalangDocument11 pagesF.09 BONE RADIOLOGY - Dr. GalangDasha VeeNo ratings yet
- MEDICAL CERTIFICATIONDocument7 pagesMEDICAL CERTIFICATIONDasha VeeNo ratings yet
- f.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Document4 pagesf.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Dasha VeeNo ratings yet
- Biosecurity On Pig FarmDocument10 pagesBiosecurity On Pig FarmBim ShiddiNo ratings yet
- Evaluación Diagnóstica Inglés - 5 QuintoDocument6 pagesEvaluación Diagnóstica Inglés - 5 Quintonadia cespedes cruzNo ratings yet
- Communicable & Non-Communicable Disease: CreatedbyDocument17 pagesCommunicable & Non-Communicable Disease: CreatedbyRATNA NOVITANo ratings yet
- MALNUTRITIONDocument23 pagesMALNUTRITIONPrincess Alane MorenoNo ratings yet
- A Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportDocument4 pagesA Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportAbdullah KhanNo ratings yet
- Skin Rash Station Worksheet and HandoutDocument5 pagesSkin Rash Station Worksheet and HandoutLou EscobarNo ratings yet
- The Neonatal Eating Assessment Tool: Development and Content ValidationDocument9 pagesThe Neonatal Eating Assessment Tool: Development and Content ValidationdeboraNo ratings yet
- Busy Ants Montessori - Application Form: Child Accompanied byDocument2 pagesBusy Ants Montessori - Application Form: Child Accompanied byjxjjjfbNo ratings yet
- 4 Protein NotesDocument4 pages4 Protein NotesChitogeNo ratings yet
- Obesity Obesity OverviewDocument6 pagesObesity Obesity OverviewLorena IbarrolaNo ratings yet
- Impacts and Socio-Economic Implications of COVID-19 in Bangladesh and Role of The Social Determinants of HealthDocument12 pagesImpacts and Socio-Economic Implications of COVID-19 in Bangladesh and Role of The Social Determinants of HealthManir Hosen100% (1)
- Acute Respiratory Distress SyndromeDocument18 pagesAcute Respiratory Distress SyndromeFasiha SamiNo ratings yet
- Epstein-Barr Virus (Infectious Mononucleosis)Document3 pagesEpstein-Barr Virus (Infectious Mononucleosis)KanayaNo ratings yet
- Beta Blocker TitrationDocument2 pagesBeta Blocker TitrationAwalunisa IstiqomahNo ratings yet
- 1-Aarogyam B + Covid Ab IgG - PO3827226873-180Document16 pages1-Aarogyam B + Covid Ab IgG - PO3827226873-180Rohit PandeyNo ratings yet
- Phlegm Misting-Disturbing EJOM - PDFDocument6 pagesPhlegm Misting-Disturbing EJOM - PDFpeter911x2134No ratings yet
- My Lecture On IndicesDocument111 pagesMy Lecture On IndicesyogeshNo ratings yet
- 6 DR NarsimuluDocument67 pages6 DR Narsimulushirish gundalaNo ratings yet
- Oral Patho Test 1Document11 pagesOral Patho Test 1Vijay K PatelNo ratings yet
- Total Knee Replacement: Done By: Sajeda Moha'dDocument27 pagesTotal Knee Replacement: Done By: Sajeda Moha'dlolo223No ratings yet
- Comparative Immunogenicity of BNT162b2 MRNA Vaccine With Natural SARS-CoV-2 InfectionDocument13 pagesComparative Immunogenicity of BNT162b2 MRNA Vaccine With Natural SARS-CoV-2 InfectionChristian GaraffaNo ratings yet
- Good Health and Well-Being in BangladeshDocument10 pagesGood Health and Well-Being in BangladeshRedwan RahmanNo ratings yet
- Mak Roo 2018Document7 pagesMak Roo 2018my accountNo ratings yet
- ISLAB P2 - Anti-Streptolysin ODocument4 pagesISLAB P2 - Anti-Streptolysin ODanielle Anne LambanNo ratings yet
- Acute Phase Proteins: Blood Markers for InflammationDocument29 pagesAcute Phase Proteins: Blood Markers for InflammationMorgan100% (1)
- About Psychic AttacksDocument8 pagesAbout Psychic AttacksKeith Ryan100% (1)
- Research Paper in The Field of Health ScienceDocument3 pagesResearch Paper in The Field of Health ScienceRan DomNo ratings yet
- The Transmission of Epidemic Influenza by R. Edgar Hope-Simpson (1992) (257pp) PDFDocument257 pagesThe Transmission of Epidemic Influenza by R. Edgar Hope-Simpson (1992) (257pp) PDFSlim Jim100% (2)
- Cave Rescue ExerciseDocument3 pagesCave Rescue ExerciserajeshNo ratings yet
- Antihypertensive Drugs GuideDocument11 pagesAntihypertensive Drugs GuideRanes AndyNo ratings yet