Professional Documents
Culture Documents
New Zealand Data Sheet: 1 Product Name
Uploaded by
Ahmed Abd El HakimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
New Zealand Data Sheet: 1 Product Name
Uploaded by
Ahmed Abd El HakimCopyright:
Available Formats
NEW ZEALAND DATA SHEET
1 PRODUCT NAME
ELTROXIN® (50 mcg, 100 mcg tablets)
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
Tablets containing 50 micrograms (0.05 mg) or 100 micrograms (0.1 mg) anhydrous
levothyroxine sodium, which is the monosodium salt of the levorotary isomer of thyroxine.
100 mcg levothyroxine is equivalent in activity to 20 to 30 mcg liothyronine or 60 mg thyroid
BP.
For the full list of excipients, see section 6.1
3 PHARMACEUTICAL FORM
Eltroxin 50 microgram (0.05 mg) tablets are white to off-white, round, biconvex tablets,
imprinted with GS 11E on one face and 50 on the other.
Eltroxin 100 microgram (0.1 mg) tablets are white to off-white, round, biconvex tablets,
imprinted with GS 21C on one face and 100 on the other.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Levothyroxine is indicated for the treatment of hypothyroidism.
4.2 Dose and method of administration
Dose
Thyroxine has a narrow therapeutic index. Appropriate thyroxine dosage is based upon
clinical assessment and laboratory monitoring of thyroid function tests. During the initial
titration period, careful dosage titration and monitoring is necessary to avoid the
consequences of under- or over-treatment. The symptoms of excessive thyroxine dosage
are the same as many features of endogenous thyrotoxicosis.
If the dose of thyroxine is increased too rapidly, symptoms such as diarrhoea, nervousness,
rapid pulse, insomnia, tremors and sometimes anginal pain where there is latent myocardial
ischaemia may occur, and the dosage must be reduced or withheld for a day or two, then
restarted at a lower level. A pre-therapy ECG is valuable, as changes induced by
hypothyroidism may be confused with ECG evidence of ischaemia.
Thyroxine tablets should preferably be taken on an empty stomach.
Missed dosage – If a scheduled daily dose is missed, the dose should be taken as soon as
the patient remembers, unless it is almost time for the patient’s next dose. Two doses
should not be taken together.
In patients whose medications include levothyroxine and known interfering agents,
administration should be separated by at least 4 hours (see Section 4.5 Interactions).
Adults
Initially 50 to 100 micrograms daily and adjusted at four or six week intervals by 50
micrograms until attainment of clinical and biochemical euthyroidism. This may require
doses of 100 to 200 micrograms daily.
Patients over 50 years, elderly, or with diabetes or cardiac symptoms
With patients aged over 50 years, it is not advisable to exceed 50 micrograms a day initially.
Where there is cardiac disease 25 micrograms, given as 50 micrograms on alternate days,
is more suitable. In this condition the daily dosage may be slowly increased by 25
micrograms increments (given as 50 micrograms on alternate days) at intervals of perhaps
four weeks. This dosing regimen is illustrated in Table 1 below;
DAILY DOSE DOSING REGIMEN
25 microgram One 50 microgram tablet on alternate days
50 microgram One 50 microgram tablet daily
One 50 microgram tablet daily and one 50 microgram tablet on
75 microgram
alternate days
100 microgram One 100 microgram tablet daily
One 100 microgram tablet daily and one 50 microgram tablet on
125 microgram
alternate days
The initial dose and any dose increments should be carefully chosen in elderly and in
patients with cardiac symptoms, diabetes mellitus or insipidus: too high initial dose or too
rapid increase may cause or aggravate symptoms of angina, arrhythmias, myocardial
infarction, cardiac failure or a sudden raise in blood pressure.
Paediatric population
In congenital hypothyroidism and juvenile myxoedema, the largest dose consistent with
freedom from toxic effects should be given. The dosage is guided by clinical response,
growth assessment and appropriate thyroid function tests - clinically normal pulse rate and
absence of diarrhoea or constipation are the most useful indicators. Thyrotrophin levels
may remain elevated during the first year of life in children with neonatal hypothyroidism
due to resetting of the hypothalamic-pituitary axis.
For infants with congenital hypothyroidism a suitable starting dose is 25 micrograms
levothyroxine sodium given as 50 micrograms every other day is advisable. This may be
slowly increased by increments of 25 micrograms (given as 50 micrograms on alternate
days) every two to four weeks until optimal response is achieved. This dosing regimen is
illustrated in Table 1 above. The same dosing regimen applies to juvenile myxoedema,
except that the starting dose for children older than one year may be 2.5 to 5
micrograms/kg/day. The calculated daily dose equivalent should be rounded to the nearest
25 micrograms to determine the actual prescribed dose.
Method of administration
Eltroxin tablets should be swallowed whole, and taken with a full glass of water. Eltroxin
tablets should not be split.
4.3 Contraindications
Hypersensitivity to any component of the preparation.
Thyrotoxicosis.
Acute myocardial infarction
Acute myocarditis
Acute pancarditis.
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 2 of 8
4.4 Special warnings and precautions for use
Adrenal insufficiency
Treatment with thyroxine in patients with panhypopituitarism or other causes predisposing
to adrenal insufficiency may cause reactions including dizziness, weakness, malaise,
weight loss, hypotension and adrenal crisis. It is advisable to initiate corticosteroid therapy
before giving levothyroxine sodium in these cases.
Elderly / cardiac symptoms / diabetes
Special care is needed in the elderly and in patients with symptoms of myocardial
insufficiency or ECG evidence of myocardial infarction or ischaemia and also those with
diabetes mellitus or insipidus.
Levothyroxine raises blood sugar levels and this may upset the stability of patients receiving
antidiabetic agents.
Effects on bone mineral density
Subclinical hyperthyroidism may be associated with bone loss. In women, long-term
levothyroxine sodium therapy has been associated with increased bone resorption, thereby
decreasing bone mineral density, especially in post-menopausal women on greater than
replacement doses or in women who are receiving suppressive doses of levothyroxine
sodium. The increased bone resorption may be associated with increased serum levels and
urinary excretion of calcium and phosphorus, elevations in bone alkaline phosphate and
suppressed serum parathyroid hormone levels. To minimize the risk of osteoporosis,
dosage of levothyroxine should be titrated to the lowest possible effective level.
Paediatric population
Parents of children receiving levothyroxine should be advised that partial loss of hair may
occur during the first few months of therapy, but this effect is usually transient and
subsequent regrowth usually occurs.
Thyroxine should not be used for the treatment of obesity or weight loss
In euthyroid patients, doses within the range of daily hormonal requirements are ineffective
for weight reduction. Larger doses may produce serious or even life threatening
manifestations of toxicity, particularly when given in association with sympathomimetic
amines such as those used for anorectic effects.
Malabsorption syndromes
Thyroxine absorption is decreased in patients with malabsorption syndromes. It is advised
to treat the malabsorption condition to ensure effective thyroxine treatment with regular
thyroxine dose.
Myxoedema
Patients with myxoedema have an increased sensitivity for thyroid hormones; in these
patients the starting dose should be low with slow dosing increments.
Pregnancy
During pregnancy, serum thyroxine levels may decrease with a concomitant increase in
serum TSH level to values outside the normal range. Patients taking levothyroxine should
have their TSH measured during each trimester. An elevated serum TSH level should be
corrected by an increase in the dose of levothyroxine. Since postpartum TSH serum levels
are similar to preconception values, levothyroxine dosage can be reduced to the pre-
pregnancy dose.
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 3 of 8
4.5 Interaction with other medicines and other forms of interaction
Levothyroxine increases the effect of anticoagulants and it may be necessary to reduce the
dose of anticoagulant if excessive hypoprothrombinaemia and bleeding are to be avoided.
Phenytoin levels may be increased by levothyroxine.
Anticonvulsants such as carbamezapine and phenytoin enhance the metabolism of thyroid
hormones and may displace them from plasma proteins. Initiation or discontinuation of
anticonvulsant therapy may alter levothyroxine sodium dose requirements. Enzyme
inducers like rifampicin and barbiturates increase the metabolism and excretion of
thyroxine, resulting in increased thyroxine requirements.
Medicines that (partially) inhibit the peripheral transformation of T4 to T3 – like propranolol,
amiodarone, lithium, iodide, oral contrast agents, propylthiouracil and glucocorticoids –
lower the T3 level and therefore also the therapeutic effect.
If co-administered with cardiac glycosides, adjustment of dosage of cardiac glycoside may
be necessary.
The effects of sympathomimetic agents are also enhanced.
Levothyroxine increases receptor sensitivity to catecholamines thus accelerating the
response to tricyclic antidepressants.
Cholestyramine, calcium-, aluminium-, magnesium-, iron supplements, polystyrene
sulfonates, sucralfate, lanthanum, bile acid sequestrants (e.g. colestipol), anion/cation
exchange resins (e.g. kayexalate, sevelamer), and proton pump inhibitors decrease the
absorption of thyroxine. Separate the dosages of thyroxine and the above mentioned
medicines as much as possible to avoid interaction in the stomach or the small bowel.
Soy-containing compounds and high-fibre diets can decrease the intestinal absorption of
thyroxine. Therefore, a dosage adjustment of thyroxine may be necessary, in particular at
the beginning or after termination of nutrition with soy supplements.
Weight loss drugs: Orlistat may decrease levothyroxine absorption which may result in
hypothyroidism. To avoid this orlistat and levothyroxine should be administered at least 4
hours apart. Regular monitoring for changes in thyroid function is required.
Thyroxine can increase the need for insulin or oral antidiabetics in patients with diabetes.
Lowering the dose of thyroxine can cause hypoglycemia if the insulin or oral antidiabetics
dose remains unchanged.
Co-administration of oral contraceptives, as well as a number of other drugs, including
oestrogen, tamoxifene, clofibrate, methadone and 5-fluorouracil may increase serum
concentration of thyroxine-binding globulin, and therefore increase thyroxine dosage
requirements.
Reports indicate that some HMG-CoA reductase inhibitors (statins), such as simvastatin
and lovastatin, may increase thyroid hormone requirements in patients receiving thyroxine
therapy. It is unknown if this occurs with all statins. Close monitoring of thyroid function
and appropriate thyroxine dose adjustments may be necessary when thyroxine and statins
are co-prescribed.
A number of drugs may decrease serum concentration of thyroxine-binding globulin, and
therefore decrease thyroxine dosage requirements, including androgens and anabolic
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 4 of 8
steroids.
False low plasma concentrations have been observed with concurrent anti-inflammatory
treatment such as phenylbutazone or acetylsalicylic acid and thyroxine therapy.
Administration of acetylsalicylic acid together with thyroxine results in an initial transient
increase in serum free T4. Continued administration results in normal free T4 and TSH
concentrations, and therefore, patients become clinically euthyroid.
Treatment with tyrosine kinase inhibitors (eg imatinib and sunitinib) was associated with
increased thyroxine dosage requirements in hypothyroid patients.
The concurrent use of sertraline can reduce serum levels of thyroxine (with concomitant
increased TSH levels).
Post-marketing cases have been reported indicating a potential interaction between
ritonavir containing products and levothyroxine. Thyroid-stimulating hormone (TSH) should
be monitored in patients treated with levothyroxine at least the first month after starting
and/or ending ritonavir treatment.
A number of drugs may affect thyroid function tests and this should be borne in mind when
monitoring a patient on levothyroxine sodium therapy.
4.6 Fertility, pregnancy and lactation
Levothyroxine has been taken by a large number of pregnant women and women of
childbearing age without any form of definite disturbances in the reproductive process
having been observed so far. Thyroid hypo- or hyperactivity in the mother may, however,
unfavourably influence the fetal outcome or well-being.
Levothyroxine is excreted in breast milk in low concentrations and this may be sufficient to
interfere with neonatal screening for hypothroidism.
4.7 Effects on ability to drive and use machines
From the pharmacokinetic and pharmacodynamic properties of levothyroxine, treatment
with Eltroxin would not be expected to interfere with ability to drive or operate machinery.
4.8 Undesirable effects
The following effects are indicative of excessive dosage and usually disappear on reduction
of dosage or withdrawal of treatment for a few days.
The frequency classification for these adverse reactions is not known due to a lack of robust
clinical trial data to accurately determine frequency estimates.
Immune system disorders: Hypersensitivity reactions such as skin rash,
pruritis and anaphylactic reactions
Metabolism and nutrition Increased appetite, excessive loss of weight
disorders:
Gastrointestinal disorders Abdominal cramps, nausea, vomiting and diarrhea
Nervous system disorders: Headache, tremors, seizure. Rare cases of
pseudotumor cerebri (benign intracranial
hypertension) have been reported especially in
children.
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 5 of 8
Psychiatric disorders Anxiety, emotional lability, nervousness,
excitability, insomnia, restlessness, psychotic
depression
Cardiac disorders: Anginal pain, cardiac arrhythmias, palpitations,
tachycardia, increased blood pressure, heart
failure, myocardial infarction
Endocrine disorders Hyperthyroidism
Respiratory, thoracic and Dysponea
mediastinal disorders:
Skin and subcutaneous tissue Sweating, hair loss
disorders:
Vascular disorders Flushing
Musculoskeletal, connective Cramps in the skeletal muscle, muscular
tissue and bone disorders : weakness. Excessive dose may result in
craniosynostosis in infants, and premature closure
of epiphyses in children with compromised adult
height.
Investigations Decreased bone mineral density
Reproductive system and Menstrual irregularity, impaired fertility
breast disorders:
General disorders and Fatigue, heat intolerance, fever
administration site conditions:
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicine is important. It
allows continued monitoring of the benefit/risk balance of the medicine. Healthcare
professionals are asked to report any suspected adverse reactions
https://nzphvc.otago.ac.nz/reporting/
4.9 Overdose
Symptoms and Signs
In addition to exaggeration of side effects the following symptoms may be seen: agitation,
confusion, irritability, hyperactivity, headache, sweating, mydriasis, tachycardia,
arrhythmias, tachypnoea, pyrexia, increased bowel movements and convulsions. The
appearance of clinical hyper-thyroidism may be delayed for up to five days. Thyrotoxic crisis
has been occasionally reported following massive or chronic intoxication, leading to cardiac
arrhythmias, heart failure and coma.
Treatment
The goal of therapy is restoration of clinical and biochemical euthyroid state by omitting or
reducing the thyroxine dosage, and other measures as needed depending on clinical status.
Treatment is symptomatic, and tachycardia has been controlled in adults by 40mg doses
of propranolol given every 6 hr and other symptoms by diazepam and/or chlorpromazine
as appropriate.
Further management should be as clinically indicated or as recommended by the national
poisons centre, where available. For advice on the management of overdose please
contact the National Poisons Centre on 0800 POISON (0800 764766).
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 6 of 8
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Levothyroxine sodium is the monosodium salt of the levorotary isomer of thyroxine.
Levothyroxine (T4) is a naturally occurring hormone produced by the thyroid gland and
converted to the more active hormone triiodothyronine (T3) in peripheral tissues. The
precise signals controlling the conversion of T4 to T3 within the cell are not known. The
thyroid hormones are required for normal growth and development, particularly of the
nervous system. They increase the resting or basal metabolic rate of the whole organism
and have stimulatory effects on the heart, skeletal muscle, liver and kidney. Thyroid
hormones enhance lipolysis and the utilization of carbohydrate.
100 mcg levothyroxine is equivalent in activity to 20 to 30 mcg liothyronine/triiodothyronine
or 60 mg Thyroid BP and/or local pharmacopoeia specification.
5.2 Pharmacokinetic properties
Absorption and Distribution
Following oral administration the absorption of levothyroxine is incomplete and variable
especially when taken with food. The amount absorbed increases during fasting conditions.
Levothyroxine is nearly totally bound to serum protein.
Metabolism and Elimination
The main pathway for the metabolism of levothyroxine (T4) is its conversion, by
deiodination, to the active metabolite triiodothyronine (T3). Further deiodination of T4 and
T3 leads to production of inactive products.
Levothyroxine is eliminated slowly from the body with a half-life of approximately 7 days in
a normal person. This may be reduced in hyperthyroid states or increased in hypothyroid
patients.
Renal or hepatic disease do not appear to have any significant effect on the disposition of
levothyroxine.
In man approximately 20-40% of levothyroxine is eliminated in the faeces and
approximately 30-55% of a dose of levothyroxine is excreted in the urine.
5.3 Preclinical safety data
No data included.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Microcrystalline cellulose, Pregelatinised maize starch, Talc, Colloidal anhydrous silica,
Magnesium stearate.
6.2 Incompatibilities
Not applicable
6.3 Shelf life
24 months
6.4 Special precautions for storage
Store below 25 °C. Protect from light.
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 7 of 8
6.5 Nature and contents of container
50 mcg tablets in a polypropylene bottle fitted with a tamper evident, push-fit, white opaque
low-density polyethylene (LDPE) closure containing 1000 tablets.
100 mcg tablets in a polypropylene bottle fitted with a tamper evident, push-fit, white opaque
low-density polyethylene (LDPE) closure containing 1000 tablets.
6.6 Special precautions for disposal
No special requirements for disposal
7 MEDICINE SCHEDULE
Prescription Only Medicine
8 SPONSOR
Pharmacy Retailing (NZ) Limited trading as Healthcare Logistics
58 Richard Pearse Drive
Airport Oaks
Auckland
New Zealand
Telephone: (09) 9185 100
aspen@aspenpharma.co.nz
9 DATE OF FIRST APPROVAL
16 November 2006
10 DATE OF REVISION OF THE TEXT
23 May 2019
SUMMARY TABLE OF CHANGES
Section Changed Summary of New Information
4.5 Addition of ritonavir interaction
4.8 Craniosynostosis ADR moved under
Musculoskeletal and connective tissue
disorders
ELTROXIN (levothyroxine sodium) 50mcg & 100 mcg tablets Page 8 of 8
You might also like
- Eltroxin (New) TabDocument8 pagesEltroxin (New) TabhpradeepNo ratings yet
- The Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016Document10 pagesThe Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016ddandan_2No ratings yet
- Levothyroxine 50mcg Tablets for HypothyroidismDocument7 pagesLevothyroxine 50mcg Tablets for HypothyroidismAnwaar Yousaf SmoreNo ratings yet
- Brand Name Generic Name Indications Dosage Side Effects: HyperthyroidismDocument11 pagesBrand Name Generic Name Indications Dosage Side Effects: HyperthyroidismshieNo ratings yet
- Eltroxin TabletsDocument16 pagesEltroxin TabletsSarthak DixitNo ratings yet
- Eltroxin TabletsDocument17 pagesEltroxin Tabletsdaya A LNo ratings yet
- PALMARES Drug StudyDocument13 pagesPALMARES Drug StudyIvan Jules P. PALMARESNo ratings yet
- ThyroidDocument21 pagesThyroidcombuter0No ratings yet
- LevotiroxinaDocument4 pagesLevotiroxinaIsidora GreeneNo ratings yet
- Propylthiouracil 2Document14 pagesPropylthiouracil 2Magdy Ali ELsherbenyNo ratings yet
- Metformin: Dosing & UsesDocument8 pagesMetformin: Dosing & UsesMaria Alejandra Siachoque JaraNo ratings yet
- Synthroid (Levothyroxine)Document2 pagesSynthroid (Levothyroxine)E100% (2)
- Hypothyroidism MedicationsDocument6 pagesHypothyroidism Medicationsamier90No ratings yet
- PhenytoinDocument6 pagesPhenytoinapi-3797941100% (1)
- New Zealand Data Sheet: 1. Product NameDocument23 pagesNew Zealand Data Sheet: 1. Product NameCarina ColtuneacNo ratings yet
- V. Vijayanthi: Pharmacology & Management of HypothyroidismDocument35 pagesV. Vijayanthi: Pharmacology & Management of HypothyroidismVeena VijayanNo ratings yet
- Package Leaflet: Information For The UserDocument7 pagesPackage Leaflet: Information For The UserpupegufNo ratings yet
- BaclofenDocument11 pagesBaclofenddandan_2No ratings yet
- Allopurinol tablets summary of product characteristicsDocument12 pagesAllopurinol tablets summary of product characteristicsasdwasdNo ratings yet
- Losartan Tablet 50 MG - Summary of Product CharacteristicsDocument81 pagesLosartan Tablet 50 MG - Summary of Product CharacteristicsBrown and Burk UK LtdNo ratings yet
- Solu CortefDocument4 pagesSolu CortefOliver BagarinaoNo ratings yet
- Hypothyroidism and Myxedema ComaDocument53 pagesHypothyroidism and Myxedema ComaKuba ArebaNo ratings yet
- Testoviron Depot DR 1316507293271Document8 pagesTestoviron Depot DR 1316507293271Varun NakraNo ratings yet
- Drug StudyDocument34 pagesDrug StudyMarco MoralesNo ratings yet
- Metformin Hydrochloride PDFDocument4 pagesMetformin Hydrochloride PDFHannaNo ratings yet
- Drug StudyDocument3 pagesDrug Studyanon_11638632No ratings yet
- Endocrine System Chapter on Thyroid Hormones and Antithyroid DrugsDocument40 pagesEndocrine System Chapter on Thyroid Hormones and Antithyroid DrugsMSKCNo ratings yet
- Drug StudyDocument10 pagesDrug StudyFranco ObedozaNo ratings yet
- Euthrox CharacteristicsDocument10 pagesEuthrox Characteristicspavaroti37No ratings yet
- Losartan Potassium 50mg Tablets - Summary of Product Characteristics (SMPC)Document16 pagesLosartan Potassium 50mg Tablets - Summary of Product Characteristics (SMPC)Pharmacist ipsNo ratings yet
- Aminophylline (Theophylline Ethylenediamine) : TruphyllineDocument4 pagesAminophylline (Theophylline Ethylenediamine) : TruphyllineRosalie SepayaNo ratings yet
- VoltarensuppositoriesDocument15 pagesVoltarensuppositoriesasi basseyNo ratings yet
- Lovastatin PDFDocument3 pagesLovastatin PDFHannaNo ratings yet
- EtopexDocument11 pagesEtopexMohammed HaiderNo ratings yet
- Prescribing Information: 1. Name of The Medicinal ProductDocument5 pagesPrescribing Information: 1. Name of The Medicinal Productddandan_20% (1)
- Losartan PotassiumDocument3 pagesLosartan Potassiumapi-3797941100% (1)
- Furosemide Tables:: Pharmacokinetics Bioavailability Peak Plasma Level Plasma Half-Life Active Metabolites EliminationDocument4 pagesFurosemide Tables:: Pharmacokinetics Bioavailability Peak Plasma Level Plasma Half-Life Active Metabolites Eliminationmole_fkNo ratings yet
- Voltfast-Sep 2022.SIN-app260123 PDFDocument14 pagesVoltfast-Sep 2022.SIN-app260123 PDFChelang AbdulkareemNo ratings yet
- Florinef (Fludrocortisone)Document3 pagesFlorinef (Fludrocortisone)E100% (1)
- ImipramineDocument6 pagesImipramineMuhammed Faruk JambazNo ratings yet
- Drug StudyDocument14 pagesDrug StudyKatrina EstoconingNo ratings yet
- Labs Drug Study 1Document17 pagesLabs Drug Study 1Drei LanuzoNo ratings yet
- Drugs For ObesityDocument41 pagesDrugs For ObesityBiplav SinghNo ratings yet
- Summary of RetigabineDocument117 pagesSummary of RetigabineAsher2225No ratings yet
- CarbamazepineDocument5 pagesCarbamazepineapi-3797941100% (2)
- Drug Study 2Document8 pagesDrug Study 2rey_tengNo ratings yet
- Methotrexate Guide for Rheumatoid Arthritis & CancerDocument5 pagesMethotrexate Guide for Rheumatoid Arthritis & CancerDea Sabelle CastroNo ratings yet
- Mkasap Endocrinology NotesDocument6 pagesMkasap Endocrinology NotesUm HamoOdNo ratings yet
- Hydroxyzine GuidelinesDocument13 pagesHydroxyzine GuidelinesMahim JainNo ratings yet
- New Zealand Data Sheet: ActionsDocument17 pagesNew Zealand Data Sheet: Actionsheri siswanto nur sidikNo ratings yet
- VoltarenTablet May2019.SINv1 App110821Document13 pagesVoltarenTablet May2019.SINv1 App110821zahragubil95No ratings yet
- Mini RinDocument5 pagesMini Rinlovely_dyaNo ratings yet
- Zine Hydro ChlorideDocument4 pagesZine Hydro Chlorideapi-3797941No ratings yet
- MTNL Kids SyrupDocument6 pagesMTNL Kids Syrupparth mair100% (1)
- MetFormin Generic Health TabDocument9 pagesMetFormin Generic Health TabNur Ekayani SyamNo ratings yet
- Oxytocin Generic Name: Oxytocin Brand Name: Pitocin/ Syntocinon IndicationsDocument5 pagesOxytocin Generic Name: Oxytocin Brand Name: Pitocin/ Syntocinon IndicationsKish SuguitanNo ratings yet
- Medical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcFrom EverandMedical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Untitled Document PDFDocument1 pageUntitled Document PDFAhmed Abd El HakimNo ratings yet
- Royal College of Psychiatrists: PMPT Overseas Registration FormDocument2 pagesRoyal College of Psychiatrists: PMPT Overseas Registration FormAhmed Abd El HakimNo ratings yet
- Royal College of Psychiatrists: PMPT Overseas Registration FormDocument2 pagesRoyal College of Psychiatrists: PMPT Overseas Registration FormAhmed Abd El HakimNo ratings yet
- March 2019 Recalls PlabKeysDocument50 pagesMarch 2019 Recalls PlabKeysJunaid KhanNo ratings yet
- IMSLP446802-PMLP500461-Thompson - Easiest Course P2 - 2 PDFDocument22 pagesIMSLP446802-PMLP500461-Thompson - Easiest Course P2 - 2 PDFEugenia Cernat DobosNo ratings yet
- Amc Clinical-Examination-Specifications PDFDocument32 pagesAmc Clinical-Examination-Specifications PDFAchyut KanungoNo ratings yet
- صيد الخاطر PDFDocument512 pagesصيد الخاطر PDFغريب أعجميNo ratings yet
- IMSLP609238 PMLP2344 Prelude - Bsnpno PDFDocument3 pagesIMSLP609238 PMLP2344 Prelude - Bsnpno PDFAhmed Abd El HakimNo ratings yet
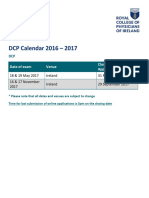
- DCP Calendar 2016 - 2017: Date of Exam Venue Closing Date For ApplicationsDocument1 pageDCP Calendar 2016 - 2017: Date of Exam Venue Closing Date For ApplicationsAhmed Abd El HakimNo ratings yet
- 5th 09Document7 pages5th 09Ahmed Abd El HakimNo ratings yet
- Night: 2. Check Before You Take Panadol NightDocument2 pagesNight: 2. Check Before You Take Panadol NightAhmed Abd El HakimNo ratings yet
- Obsessive-Compulsive Disorder and Body Dysmorphic Disorder: TreatmentDocument44 pagesObsessive-Compulsive Disorder and Body Dysmorphic Disorder: TreatmentAhmed Abd El HakimNo ratings yet
- Guidance On The Use of Electroconvulsive Therapy PDF 2294645984197Document36 pagesGuidance On The Use of Electroconvulsive Therapy PDF 2294645984197Ahmed Abd El HakimNo ratings yet
- IMSLP263280-PMLP02344-Chopin - Prelude Op28 No2 (Franchomme) For Cello and Piano ManuscriptDocument1 pageIMSLP263280-PMLP02344-Chopin - Prelude Op28 No2 (Franchomme) For Cello and Piano ManuscriptAhmed Abd El HakimNo ratings yet
- Night: 2. Check Before You Take Panadol NightDocument2 pagesNight: 2. Check Before You Take Panadol NightAhmed Abd El HakimNo ratings yet
- IMSLP263252-PMLP02344-Chopin - Prelude No15 Op28 (Franchomme) For Cello and Piano ManuscriptDocument4 pagesIMSLP263252-PMLP02344-Chopin - Prelude No15 Op28 (Franchomme) For Cello and Piano ManuscriptAhmed Abd El HakimNo ratings yet
- Practice Test 1 PDFDocument62 pagesPractice Test 1 PDFAhmed Abd El HakimNo ratings yet
- Arr Johnstone PIAZZOLLA 3 Caprices SOLO CELLODocument9 pagesArr Johnstone PIAZZOLLA 3 Caprices SOLO CELLOAhmed Abd El Hakim100% (1)
- 5th 08Document18 pages5th 08Ahmed Abd El HakimNo ratings yet
- IMSLP55338-PMLP54099-Haydn - Cello Concerto C Major HobVIIb No5 Cello SoloDocument15 pagesIMSLP55338-PMLP54099-Haydn - Cello Concerto C Major HobVIIb No5 Cello SoloAhmed Abd El HakimNo ratings yet
- Traditional Dark Eyes 19317Document1 pageTraditional Dark Eyes 19317Ahmed Abd El HakimNo ratings yet
- Mozart - Piano Sonata No. 11 in A Major, K. 331 - II. Menuetto Mozart - Piano Sonata No. 4 in E Flat, K. 282, 2 Mov Minuet 1Document1 pageMozart - Piano Sonata No. 11 in A Major, K. 331 - II. Menuetto Mozart - Piano Sonata No. 4 in E Flat, K. 282, 2 Mov Minuet 1Ahmed Abd El HakimNo ratings yet
- IMSLP108523-PMLP137464-Boccherini - Rondo Op60 No8 Grutzmacher Cello PianoDocument13 pagesIMSLP108523-PMLP137464-Boccherini - Rondo Op60 No8 Grutzmacher Cello PianoAhmed Abd El HakimNo ratings yet
- IMSLP103592-PMLP211630-Popper - Barcarole For Cello and Piano Op38 PnoDocument13 pagesIMSLP103592-PMLP211630-Popper - Barcarole For Cello and Piano Op38 PnoAhmed Abd El HakimNo ratings yet
- Grieg (Arr Goltermann) - Lyric Pieces For Cello and PianoDocument21 pagesGrieg (Arr Goltermann) - Lyric Pieces For Cello and PianoAhmed Abd El HakimNo ratings yet
- Servais - Lestocq Grande Fantaisie Op.12 CelloDocument9 pagesServais - Lestocq Grande Fantaisie Op.12 CelloAhmed Abd El HakimNo ratings yet
- Albeniz - Tango Op.165 N°2 (Violin and Piano) PDFDocument4 pagesAlbeniz - Tango Op.165 N°2 (Violin and Piano) PDFrroowwllffNo ratings yet
- IMSLP12263-Dvorak-Limskov - Melody Cello and PianoDocument4 pagesIMSLP12263-Dvorak-Limskov - Melody Cello and PianomraisikNo ratings yet
- IMSLP23591-PMLP18850-Haydn - Cello Concerto in D HobVII2 Cello SoloDocument15 pagesIMSLP23591-PMLP18850-Haydn - Cello Concerto in D HobVII2 Cello SoloAhmed Abd El HakimNo ratings yet
- Memon Medical Institute Hospital: Laboratory Rate ListDocument26 pagesMemon Medical Institute Hospital: Laboratory Rate List1123456789000% (1)
- Vitamins and minerals quizDocument1 pageVitamins and minerals quizKristine Joyce Quilang AlvarezNo ratings yet
- Thy 2010 0417Document66 pagesThy 2010 0417priskavkNo ratings yet
- Amiodarone Hydrochloride in JDocument18 pagesAmiodarone Hydrochloride in JChrizzna HaryantoNo ratings yet
- Breast Cancer .2Document3 pagesBreast Cancer .2TESL3062217 Nur Irsha Binti Shahidan SureshNo ratings yet
- Thyroid and Antithyroid PharmaDocument31 pagesThyroid and Antithyroid PharmaxaviermargaridaNo ratings yet
- Normal Lab Values For PediatricsDocument15 pagesNormal Lab Values For PediatricsJE MagbanuaNo ratings yet
- Nutrition 321-E-Lesson-4 PDFDocument21 pagesNutrition 321-E-Lesson-4 PDFteshome teklehaimanotNo ratings yet
- Anand Diagnostic Laboratory Test Price DetailsDocument6 pagesAnand Diagnostic Laboratory Test Price Detailsvamsiswetha SNo ratings yet
- Nurseslabs Normal Lab Values 1.2 PDFDocument5 pagesNurseslabs Normal Lab Values 1.2 PDFPrincess BaciaNo ratings yet
- Anatomy and Physiology Finals Chapter Quiz Endocrine System and The BloodDocument13 pagesAnatomy and Physiology Finals Chapter Quiz Endocrine System and The BloodMartin ManuelNo ratings yet
- Endocrine Exam 1 ReviewDocument11 pagesEndocrine Exam 1 ReviewJohn SmithNo ratings yet
- MyxedemaDocument3 pagesMyxedemaBobet ReñaNo ratings yet
- IFUk en 311611 10 PDFDocument5 pagesIFUk en 311611 10 PDFKhaled AlkhawaldehNo ratings yet
- ABIM Lab Test Reference Ranges GuideDocument22 pagesABIM Lab Test Reference Ranges Guidemsk ahmadNo ratings yet
- Anatomy and Physiology Chapter 17Document21 pagesAnatomy and Physiology Chapter 17Dawlat SlamaNo ratings yet
- What Is Goitre?: Thyroid GlandDocument3 pagesWhat Is Goitre?: Thyroid Glandflex gyNo ratings yet
- Egg Quality in Fish - What Makes A Good EggDocument30 pagesEgg Quality in Fish - What Makes A Good EggShahbaz AkhtarNo ratings yet
- Metabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistDocument124 pagesMetabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistLyn LynNo ratings yet
- Endocrine System of FishesDocument5 pagesEndocrine System of FishesmonjitpaulNo ratings yet
- Basic ENT-HNSDocument19 pagesBasic ENT-HNSKris Anne EstoestaNo ratings yet
- Physiology Passmrcog 2016Document73 pagesPhysiology Passmrcog 2016Mona HelouNo ratings yet
- Histology and Microtechniques Biology 160 Prof. Maria Luisa J. Landingin Thyroid GlandDocument2 pagesHistology and Microtechniques Biology 160 Prof. Maria Luisa J. Landingin Thyroid GlandDavid YapNo ratings yet
- Deepika.R:::: Patient Age / Sex 26 Y / Female BranchDocument2 pagesDeepika.R:::: Patient Age / Sex 26 Y / Female BranchkannanNo ratings yet
- Adult-2, Unit 1, Metabolic and EndocrineDocument157 pagesAdult-2, Unit 1, Metabolic and EndocrineBav VAansoqnuaetzNo ratings yet
- Effects of Heat Stress On Animal Physiology, Metabolism, and Meat QualityDocument13 pagesEffects of Heat Stress On Animal Physiology, Metabolism, and Meat QualityDaniel AriasNo ratings yet
- Hyperthyroidism in PregnancyDocument21 pagesHyperthyroidism in PregnancyCharisse Aser Flores AquinoNo ratings yet
- DUAL ROLE OF BETEL LEAF EXTRACT ON THYROID FUNCTION in Male MiceDocument4 pagesDUAL ROLE OF BETEL LEAF EXTRACT ON THYROID FUNCTION in Male MiceVIGNESHNo ratings yet
- Thyroid Gland NotesDocument21 pagesThyroid Gland NotesbryanNo ratings yet
- Metabolic Diseases and Their Oral ManifestationsDocument39 pagesMetabolic Diseases and Their Oral ManifestationsriyaNo ratings yet