Professional Documents
Culture Documents
191 Iajps191092020
Uploaded by
iajpsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
191 Iajps191092020
Uploaded by
iajpsCopyright:
Available Formats
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN : 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
SJIF Impact Factor: 7.187
http://doi.org/10.5281/zenodo.4060784
Available online at: http://www.iajps.com Research Article
RELATIONSHIP OF BODY MASS INDEX WITH MORTALITY
AND MORBIDITY AMONG THE ELDERLY PATIENTS
1Dr.
Laiba Rao, 2Dr. Moazzam Ali, 3Dr. Muhammad Ahmad Rao,
1
CNIC # 36201-4321322-8., 2PMDC# 69036-P., 3PMDC # 109337-P.
Article Received: July 2020 Accepted: August 2020 Published: September 2020
Abstract:
Objective: Obesity may cause many chronic illnesses. Several studies have shown that high body mass index is
associated with mortality and morbidity among the elderly. Therefore, obesity or being overweight could adversely
affect the performance of activities of daily living. In this study our aim was to investigate the association between
Body Mass Index and Activity of Daily Living in Homecare Patients.
Method: The records of 2016 from the homecare unit of Allied hospital faisalabad. During this period, 1105
patients visited this facility. Unconscious or bedridden patients (hemiplegia, hemiparesia, and tetraparesis) and
patients with incomplete data were excluded from the study. Therefore, the survey was completed with 250 files,
which included all the data needed for our research. Age, gender, Body Mass Index and Barthel Index scores were
recorded to the statistical program; p≤0.05 was considered as statistically significant.
Results: One hundred fifty one (60.4%) were women, and 99 (39.6%) were men. The relations between gender and
age, weight, and Barthel index scores were not statistically significant. There was a significant positive correlation
between weight and Barthel index scores as well as between Body Mass Index and
Barthel index scores (r = 0.190; p = 0.003). The patients were divided into two groups: Group-I (underweight and
normal weight) and Group-II (overweight and obese). Group-II exhibited a much higher ability to perform Activity
of Daily Living than Group-I (p = 0.002).
Conclusion: Some studies report that obesity is protective against Activity of Daily Living, but the opposite is
reported in some others. Our study showed increased values of Body Mass Index and Activity of Daily Living ability,
which are indicative of protective effects. The relationship between Body Mass Index and physical disability is not
yet proven to be linear.
Keywords: Aged, Body Mass Index, Homecare Patient, Homecare Services, Obesity, Quality of Life.
Corresponding author:
Dr. Laiba Rao, QR code
CNIC # 36201-4321322-8. Email:star920@yahoo.com
Please cite this article in press Laiba Rao et al, Relationship Of Body Mass Index With Mortality And Morbidity Among The
Elderly Patients., Indo Am. J. P. Sci, 2020; 07(09).
www.iajps.com Page 1091
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
INTRODUCTION: Barthel index comprises 10 items, including the
Overweight or obesity may cause many chronic presence or absence of fecal and urinary incontinence
illnesses. Furthermore, several studies have shown and the need for assistance with grooming, toilet use,
that high body mass index (BMI) is associated with feeding, transfers (e.g., from chair to bed), walking,
mortality and morbidity among the elderly. [1] dressing, climbing stairs, and bathing. In this study,
Mobility is another important topic in relation to the we investigated the association between BMI and
elderly. Difficulties in mobility are often the first sign ADLs in homecare patients.
of functional decline and may indicate the need for
preventive measures. [2] Mobility problems have METHODS:
been reported as a predictor of all-cause mortality, The records for the period between 01 January 2016
and patients with BMI >30 kg/m2 have low scores in and 31 December 2016 from the homecare unit of
the “Time Up to Go” test, which assesses mobility. Allied hospital faisalabad was retrospectively
[3] Mobility problems as well as illnesses leading to reviewed. During this period, 1105 patients visited
cognitive impairment are a cause of dependence. this facility. Unconscious or bedridden patients
Weight loss through diet may be associated with (hemiplegia, hemiparesia, and tetraparesis) and
cognitive improvement in patients with mild patients with incomplete data were excluded from the
cognitive impairment. [4] Therefore, obesity or being study.
overweight could adversely affect the performance of
activities of daily living (ADLs). Therefore, the survey was completed with 250 files,
which included all the data needed for our research.
Barthel index is a simple index of independence, BMI is defined as the body mass divided by the
which is used to score the patients’ ability to perform square of the body height, is universally expressed in
ADLs. Since 1955, this index has been used in units of kg/m2, and is classified as follows.
hospitals for patients with chronic diseases.[5] The
• Underweight <18.50 kg/m2
• Normal range 18.50 ≤ X ≤ 24.99 kg/m2
• Overweight ≥25.00 kg/m2
• Obese ≥30.00 kg/m2
Fig.1: Distribution of age groups according to gender.
Age, gender, chronic diseases, BMI, and Barthel statistically significant.
index scores were analyzed using a statistical
program. According to the Shapiro–Wilk test, our RESULTS:
study population had an abnormal distribution (p < Two hundred fifty patients were included in our
0.001). The Mann–Whitney U test was used to study: 151(60.4%) were women and 99 (39.6%) were
compare independent variables between groups. Chi- men. The patient age groups and gender distributions
square was used to analyze relations between two are shown in Fig.1. The number of women aged >65
non-continuous variables; for continuous variables, years was much greater than that of men, and
the correlation test was used. P ≤ 0.05 was considered hypertension was the most commonly occurring
www.iajps.com Page 1092
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
chronic disease (n = 173; 60%; Fig.2). the ability to perform ADLs. The Barthel index
scores are in multiples of five, ranging from 0
Age, weight, height, BMI, and Barthel index scores (completely dependent) to 100 (independent in
stratified by gender are shown in Fig.3. The relations basic). Higher scores represent a higher degree of
between gender and age, weight, and Barthel index independence were taller than the women (p =
scores were not statistically significant (p = 0.050, 0.000), and the women had higher BMIs than the
0.538, and 0.587, respectively). However, The men (p = 0.000).
Barthel index was used as a screening tool to assess
The Barthel index scores are classified as follows:
• 0–20 points: total dependency
• 21–60 points: high-level dependency
• 61–90 points: mid-level dependency
• 91–99 points: low-level dependency
• 100 points: total independence Fig.2: Distribution of chronic diseases.
Fig.3: Age, weight, height, BMI and Barthel index scores stratified by gender.
www.iajps.com Page 1093
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
Gender-based comparisons revealed significant 15.6%). The mean Barthel index scores stratified by
correlations between BMI and Barthel index scores BMI were as follows: underweight, 26.50 ± 20;
only among women (r = 0.299; p = 0.00). normal weight, 22.93 ± 27.13; overweight, 31.51 ±
31.86, and obese, 42.30 ± 31.28. The patients were
There were significant negative correlations between divided into two groups: Group-I (underweight and
age and weight, height, Barthel index scores (i.e., normal weight) and Group-II (overweight and obese).
when age increased, the weight, height, and Barthel Group-II exhibited a much higher ability to perform
index scores decreased). Table-I There was a ADLs than Group-I (p = 0.002).In addition, 28
significant positive correlation between weight and (11.2%) of our patients died in 2016, 15 (53.6%) of
Barthel index scores as well as between BMI and whom were women. We identified no relation between
Barthel index scores (r = 0.190; p = 0.003). Therefore, death and gender (p = 0.433). Furthermore, there was
when age increased, weight, BMI, Barthel index no relation between death and age, BMI, and Barthel
scores, and ability to perform ADLs decreased. index scores (p = 0.482, 0.737, and 0.288,
respectively).
All the items of the Barthel index were not correlated
with BMI. Assistance with feeding, toilet use, DISCUSSION:
dressing, climbing stairs, bathing, and walking as well According to the World Health Organization, 71.4
as urinary and fecal continence were positively years (males: 69.1 years; females: 73.7 years) is the
correlated with BMI. As shown in Table-II, need for average life expectancy at birth, and the life
assistance with grooming and need for transfers (e.g., expectancy over the age of 60 years was 20.4 years
from chair to bed) using a wheelchair were not (males: 18.9 years; females: 21.7 years) among the
correlated. global population in 2015.6 In Turkey, the life
expectancy at birth is 66.2 years.6 According to our
According to their BMIs, the patients were classified national statistics, the elderly population was
as underweight (n = 10; 4%), normal weight (n = 125; 6,651,503 in 2016 and accounted for 8.3% of
50%), overweight (n = 76; 30.4%), and obese (n = 39;
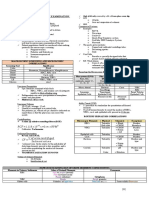
Table-I: Correlations among age, weight, height, BMI, and Barthel index scores.
Correlations
Pearson Correlation
Age 1 - - - -
Sig. (2-tailed)
Pearson Correlation -0.183**
Weight 1 - - -
Sig. (2-tailed) 0.004
Pearson Correlation -0.207** 0.416**
Height - - -
Sig. (2-tailed) 0.001 0.000
Pearson Correlation -0.111 0.898** 0.032
BMI 1 -
Sig. (2-tailed) 0.080 0.000 0.612
Pearson Correlation -0.149* 0.163* 0.037 0.190**
Barthel Index 1
Sig. (2-tailed) 0.019 .010 0.565 0.003
Age Weight Height BMI Barthel Index
**. Correlation is significant at the 0.01 level (2-tailed). *. Correlation is significant at the 0.05 level (2-tailed).
www.iajps.com Page 1094
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
Table-II: Correlations between items of the Barthel index and BMIs.
Sig. (2-tailed) - - - - - -
Pearson
Correlation 0.780** 1 - - - -
NT
Sig. (2-tailed) 0.000 - - - - -
Pearson 0.641*
Correlation 0.713** *
1 - - -
G
Sig. (2-tailed) 0.000 0.000 - - -
Pearson 0.575* 0.627*
Correlation 0.661** * *
1 - -
T
Sig. (2-tailed) 0.000 0.000 0.000 - -
Pearson 0.410* 0.363* 0.608*
Correlation 0.385** * * *
-
B 1
Sig. (2-tailed) 0.000 0.000 0.000 0.000 -
Pearson 0.286* 0.542* 0.577* 0.473*
Correlation 0.450** * * * *
1
W
Sig. (2-tailed) 0.000 0.000 0.000 0.000 0.000
Pearson −0.09 0.296* −0.15
Correlation 0.146* 0.093 6 *
0.014 1*
WC
Sig. (2-tailed) 0.021 0.142 0.129 0.000 0.828 0.017
Pearson 0.356* 0.379* 0.644* 0.517* 0.542
Correlation 0.429** * * * * **
CS
Sig. (2-tailed) 0.000 0.000 0.000 0.000 0.000 0.000
Pearson 0.560* 0.650* 0.836* 0.591* 0.623
Correlation 0.669** * * * * **
D
Sig. (2-tailed) 0.000 0.000 0.000 0.000 0.000 0.000
Pearson 0.652* 0.653* 0.754* 0.570* 0.531
Correlation 0.802** * * * * **
UC
Sig. (2-tailed) 0.000 0.000 0.000 0.000 0.000 0.000
Pearson 0.658* 0.628* 0.779* 0.585* 0.499
Correlation 0.791** * * * * **
FC
Sig. (2-tailed) 0.000 0.000 0.000 0.000 0.000 0.000
Pearson 0.168* 0.223* 0.251
Correlation 0.138* 0.009 * *
0.106 **
Bmı Sig. (2-tailed) 0.029 0.886 0.008 0.000 0.095 0.000
N 250 250 250 250 250 250
Feeding NT G T B W
www.iajps.com Page 1095
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
- - - - - -
1 - - - - -
- - - - -
0.194** 1 - - - -
0.002 - - - -
0.236** 0.701** 1 - - -
0.000 0.000 - -
0.214** 0.620** 0.805** 1 - -
0.001 0.000 0.000 - -
0.253** 0.632** 0.788** 0.902** 1 -
0.000 0.000 0.000 0.000 -
0.092 0.103 0.183** 0.143* 0.164** 1
0.146 0.104 0.004 0.023 0.009
250 250 250 250 250 250
WC CS D UC FC BMI
**. Correlation is significant at the 0.01 level (2-tailed) *. Correlation is significant at the 0.05 level (2-tailed). Help
needed with feeding (F), transfers (NT), grooming (G), toilet use (T), bathing (B), walking (W), wheelchair use
(WC), climbing stairs (CS), and dressing (D) as well as fecal continence (FC) and urinary continence (UC).
All populations (males: 43.9%; females: 56.1%). [7] incurable. The World Health Organization has listed
Similarly, 60.4% of our study group was female, cardiovascular accidents (stroke), cancer, chronic
which is probably the result of the longer life obstructive pulmonary disease, and diabetes as the
expectancy of women. most prevalent chronic illnesses worldwide.11
According to the cause of death statistics in Turkey,
According to the Turkey Statistical Institute, 61.5% 46.3% of elderly people died from circulatory system
of the elderly population are in the age group of 65– diseases in 2015. [8] In a study of a 3-year (2003–
74 years, 30.2% are in the age group of 75–84 years, 2006) Canadian homecare data, the most frequent
and 8.2% are in the age of ≥85 years. [8] chronic illness among 149,378 long-term homecare
patients was chronic renal disorder, followed by
Several studies have shown that most homecare hypertension, diabetes, heart failure, and
patients are aged >65 years. [9,10] In our study, depression.12 A study in Turkey revealed that
16.6% of the elderly population was in the age group hypertension was detected in 41.8% of homecare
of 65–74 years, 39.3% were in the age group of 75– patients. [13] In our study, hypertension was the most
84 years, and 44.1% were in the age group of ≥85 frequently observed chronic disease (n = 173; 60%).
years. These findings are because the need for Moreover, hypertension is observed 30%–45% of the
homecare increases with age; accordingly, most of general population, and this percentage increases
our study population was aged >85 years. with age. [14]
Chronic illnesses are long-term illnesses and usually The prevalence of overweight and obesity is
www.iajps.com Page 1096
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
increasing in the elderly population. [15] Obesity is advise all patients to receive adequate nutrition and
known to have a negative effect on mortality and perform exercises, which will protect them from most
morbidity. [16,17] Numerous cohort studies have chronic diseases and help them with healthy aging.
reported that higher levels of frailty are predicted by
not only cognitive impairment but also various REFERENCES:
frailty-related indicators such as BMI and ADL- 1. Sajjad A, Freak-Poli RL, Hofman A, Roza SJ,
performing ability. [18,19] However, we identified a Ikram MA, Tiemeier H. Subjective measures of
positive correlation between BMI and ADL- health and all-cause mortality–the Rotterdam
performing ability in our population. Similarly, we Study. Psychol Med. 2017;47(11):1971-1980.
obtained controversial results for whether overweight doi: 10.1017/S0033291717000381.
increases the ADL disability [20] or has protective 2. Manty M, Heinonen A, Leinonen R,
effects. [21] This is because ADL-performing ability Tormakangas T, Sakari-Rantala R, Hirvensalo
changes with not only weight but also eating habits, M, et al. Construct and predictive validity of a
and the eating habits of overweight or obese self-reported measure of preclinical mobility
individuals may decrease the malnutrition risk and limitation. Arch Phys Med Rehabil.
may protect against the decline of ADL ability, given 3. 2007;88:1108-1113.
that nutritional status is related to ADL-performing 4. Bergland A, Jorgensen L, Emaus N, Strand BH.
ability in geriatric patients. [22]. Mobility as a predictor of all-cause mortality in
older men and women: 11.8 year follow-up in
Overweight and obesity, as measured by BMI, are the Tromso study. BMC Health Serv Res.
also associated with a higher probability of ADL 2017;17:22. doi: 10.1186/s12913-016-1950-0.
disability among women but not men. [23] By 5. Horie NC, Serrao VT, Simon SS, Gascon MR,
contrast, our study showed that ADL-performing Dos Santos AX, Zambone MA, et al. Cognitive
ability in women positively correlated with BMI. effects of intentional weight loss in elderly obese
This is because elderly individuals lose individuals with mild cognitive impairment. J
approximately 1% of their lean mass (mainly muscle Clin Endocrinol Metab. 2016;101:1104-1112.
mass) per /year, with men losing more muscle mass doi: 10.1210/jc.2015-2315.
than do women, both in absolute and relative terms. 6. Mahoney FI, Barthel D. Functional evaluation:
[24] Hence, increased BMI led to increased ADL- The Barthel Index. MD State Med J.
performing ability among women in our study. 1965;14:56-61.
7. World Health Organisation (2017) Global
Many studies have shown that sarcopenia which is Health Observatory (GHO) datas.
one of the main problems in the elderly, is associated http://www.who.int/gho/
with the decline in muscle mass and strength and is a mortality_burden_disease/life_tables/situation_tr
predictor of poor outcomes, including mortality, ends/ en/. Accessed 22 March 2017.
disability, and poor quality of life. [24] Malnutrition 8. Turkey Statistical Institute (2016) Health
and weight loss are the causes of sarcopenia which is statistics 2015.
associated with functional dependence in the elderly. http://www.turkstat.gov.tr/Start.do;jsessionid=Jr
[25] Accordingly, in our study, when the BMI zZZ3g
decreased, the ADL-performing ability decreased, KQsMntZM2Qsb8KyfvyfHmkvshyBGNCcl6T5
possibly because of the slowing down of activity due 5hRXkH6s Mc!560081250 Accessed 22 March
to malnutrition or sarcopenia. 2017.
9. Turkey Statistical Institute (2017) Elderly
CONCLUSION: statistics Statistical Institute (2017) Elderly
The relationship between obesity and ADL in the statistics
literature is unclear. Some studies report that obesity http://www.turkstat.gov.tr/PreHaberBultenleri
is protective against ADL, but the opposite is do?id=24644. Accessed 16 March 2017.
reported in some others. In our study showed 10. Karaman D, Kara D, ve Atar NY. Care Needs
increased values of BMI and ADL ability, which are And Disease States Of Individuals, Who Home
indicative of protective effects. The relationship Health Care Services Are Provided Evaluating:
between BMI and physical disability is not yet Example Of Zonguldak Province, Gumushane.
proven to be linear. This is because underweight and Uni J Health Sci. 2015;4(3). http://sbd.
obesity have similar risks. Accordingly, we conclude gumushane.edu.tr/media/uploads/sbd/issues/cilt-
that overweight, obesity, and female gender are 4-sayi-3/cilt4-sayi3.pdf. Accessed 22 March
associated with an increase in ADL-performing 2017.
ability in some cases. In general, physicians can 11. Dawani HA, Hamdan-Mansour AM, Ajlouni
www.iajps.com Page 1097
IAJPS 2020, 07 (09), 1091-1098 Laiba Rao et al ISSN 2349-7750
AT. Users’ perception and satisfaction of current instrumental activities of daily living is
situation of home health care services in Jordan. associated with faster rate of decline in cognitive
Health. 2014;6:549-558. function of older adults. J Gerontol A Biol Sci
12. World Health Organization (2005) Overview- Med Sci.
preventing chronic diseases: a vital investment. 2013;68:624-630.
http://www.who.int/ 19. Robertson DA, Savva GM, Kenny RA. Frailty
chp/chronic_disease_report/contents/foreword.pd and cognitive impairment: a review of the
f?ua=1. Accessed 22 March 2017. evidence and causal mechanisms. Ageing Res
13. Wilson DM Truman CD, Hewitt JA, Els C. Are Rev. 2013;12:840-851.
Chronically Ill Patients High Users of Homecare 20. Al Snih S, Ottenbacher KJ, Markides KS, Kuo
Services in Canada? Am J Manag Care. YF, Eschbach K, Goodwin JS. The effect of
2015;21(10):e552-e559. Catak B, Kilinc AS, obesity on disability vs mortality in older
Fadillioglu O, Sutlu S, Sofuoglu AE, Americans. Arch Intern Med. 2007;167:774-780.
Aslan D. Profile of Elderly Patients Who Use doi:
Health Services in their Homes and in-Home 10.1001/archinte.167.8.774.
Care. Turk J Public Health. 21. Rejeski WJ, Marsh AP, Chmelo E, Rejeski JJ.
2012;10:13-21. Obesity, intentional weight loss and physical
14. Mancia G, Fagard R, Narkiewicz K, Redon J, disability in older adults. Obes Rev. 2010;11:671-
Zanchetti 685. doi: 10.1111/j.1467-789X.2009.00679.x.
A, Bohm M, et al. 2013 ESH/ESC Guidelines for 22. Schrader E, Baumgartel C, Gueldenzoph H,
the management of arterial hypertension: the Stehle P, Uter W, Sieber CC, et al. Nutritional
Task Force for the management of arterial status according to Mini Nutritional Assessment
hypertension of the European Society of is related to functional status in geriatric patients-
Hypertension (ESH) and of the European Society -independent of health status. J Nutr Health
of Cardiology (ESC). J Hypertens. Aging. 2014;18:257-263.
2013;31(7):1281-1357. doi: 23. Lisko I, Stenholm S, Raitanen J, Hurme M,
10.1097/01.hjh.0000431740.32696.cc. Hervonen A, Jylha M, et al. Association of Body
15. Mathus-Vliegen EM. Obesity and the Mass Index and Waist Circumference With
Gastroenterol elderly,. J Clin Gastroenterol, Physical Functioning: The Vitality 90+ Study. J
2012;46:533-544 doi: Gerontol A Biol Sci Med Sci. 2015;70(7):885-
10.1097/MCG.0b013e3182 891. doi:
16. Gregg EW, Cheng YJ, Cadwell BL, Imperatore 10.1093/gerona/glu202.
G, Williams DE, Flegal KM, et al. Secular trends 24. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie
in cardiovascular disease risk factors according to Y, Cederholm T, Landi F, et al. Sarcopenia:
body mass index in US adults. JAMA. European consensus on definition and diagnosis:
2005;293:1868-1874. report of the European working group on
17. Adams KF, Schatzkin A, Harris TB, Kipnis V, sarcopenia in older people. Age Ageing.
Mouw T, Ballard-Barbash R, et al. Overweight, 2010;39(4):412-423. doi: 10.1093/ageing/afq034.
obesity, and mortality in a large prospective 25. Carrazco-Pena KB, Tene CE, del Rio-Valdivia J.
cohort of persons 50 to 71 years old. N Sarcopenia and functional disability in aged. Gac
Engl J Med. 2006;355:763-778. Med Mex.
18. Rajan KB, Hebert LE, Scherr PA, Mendes de 2016;152:444-451.
Leon CF, Evans DA. Disability in basic and
www.iajps.com Page 1098
You might also like
- Complementary and Alternative Medical Lab Testing Part 13: DermatologyFrom EverandComplementary and Alternative Medical Lab Testing Part 13: DermatologyRating: 5 out of 5 stars5/5 (4)
- Gender Differences in Factors Associated With Overweight and Obesity Among Civil Servants in Lagos, NigeriaDocument8 pagesGender Differences in Factors Associated With Overweight and Obesity Among Civil Servants in Lagos, Nigerialatifah zahrohNo ratings yet
- A Descriptive Study To Assess The Morbidity Pattern Among Nurses With Special Reference To ObesityDocument9 pagesA Descriptive Study To Assess The Morbidity Pattern Among Nurses With Special Reference To ObesityEditor IJTSRDNo ratings yet
- The Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyDocument11 pagesThe Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyAli HNo ratings yet
- New BMI Criteria for Screening Metabolic SyndromeDocument9 pagesNew BMI Criteria for Screening Metabolic SyndromeRudolf Fernando WibowoNo ratings yet
- 1 s2.0 S2405844020312767 MainDocument7 pages1 s2.0 S2405844020312767 MainIsini sehansa amarathungaNo ratings yet
- The Impact of Age On The Prevalence of Sarcopenic Obesity in Bariatric Surgery CandidatesDocument7 pagesThe Impact of Age On The Prevalence of Sarcopenic Obesity in Bariatric Surgery CandidatesabcsouzaNo ratings yet
- Research Proposal ExampleDocument10 pagesResearch Proposal ExampleNurul FarhahNo ratings yet
- IJAEMR_423Document9 pagesIJAEMR_423RkNo ratings yet
- IMC-Dexa-gordura-Measuring Adiposity in Patients - The Utility of Body Mass Index (BMI), Percent Body Fat, and LeptinDocument8 pagesIMC-Dexa-gordura-Measuring Adiposity in Patients - The Utility of Body Mass Index (BMI), Percent Body Fat, and LeptinFabrício Boscolo Del VecchioNo ratings yet
- Mpi Geri PDFDocument6 pagesMpi Geri PDFJaka SusilaNo ratings yet
- Relationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityDocument4 pagesRelationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityBaru Chandrasekhar RaoNo ratings yet
- The Prevalence of Obesity in Children and Young People With Down SyndromeDocument5 pagesThe Prevalence of Obesity in Children and Young People With Down SyndromeSelvia EvaNo ratings yet
- Shimizu 2016Document6 pagesShimizu 2016Juan Pablo Restrepo UribeNo ratings yet
- Differential Impact of Body Mass Index and Its Change On The Risk of Breast Cancer by Molecular Subtype: A Case - Control Study in Japanese WomenDocument10 pagesDifferential Impact of Body Mass Index and Its Change On The Risk of Breast Cancer by Molecular Subtype: A Case - Control Study in Japanese Womenrazvan_aaaNo ratings yet
- 1 s2.0 S0168822715000522 MainDocument8 pages1 s2.0 S0168822715000522 Maintri1994No ratings yet
- Prevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Document10 pagesPrevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Aboy GunawanNo ratings yet
- Prema EtalDocument6 pagesPrema EtaleditorijmrhsNo ratings yet
- MainDocument9 pagesMainAgeng betaNo ratings yet
- Digital 20282156 S705 Analisis TimbulanDocument8 pagesDigital 20282156 S705 Analisis TimbulanMariobrilliansihombingNo ratings yet
- Janatin Hastuti ThesisDocument356 pagesJanatin Hastuti ThesisNurulR100% (1)
- Effect of Gender On Intra-Abdominal Fat in Teenagers and Young AdultsDocument8 pagesEffect of Gender On Intra-Abdominal Fat in Teenagers and Young AdultsDani KusumaNo ratings yet
- Obesity and The Risk of Cryptogenic Ischemic Stroke in Young AdultsDocument25 pagesObesity and The Risk of Cryptogenic Ischemic Stroke in Young AdultsKhalilullah ArsyiNo ratings yet
- Correlation of lower limb muscle strength and BMI with body balance in elderlyDocument5 pagesCorrelation of lower limb muscle strength and BMI with body balance in elderlymoudiNo ratings yet
- Journal of Occupational Health - 2003 - Anuurad - The New BMI Criteria For Asians by The Regional Office For The WesternDocument9 pagesJournal of Occupational Health - 2003 - Anuurad - The New BMI Criteria For Asians by The Regional Office For The Westernjokeshua34No ratings yet
- En - 2237 9622 Ess 29 04 E2020102Document11 pagesEn - 2237 9622 Ess 29 04 E2020102producao AmazôniaNo ratings yet
- Research Article: Gender Differences in The Association Between Sleep Duration and Body Composition: The Cardia StudyDocument8 pagesResearch Article: Gender Differences in The Association Between Sleep Duration and Body Composition: The Cardia StudyVistaa Vistoo AnasariNo ratings yet
- Obesidad y AptitudDocument21 pagesObesidad y AptitudRuggiero Fernandez MarianellaNo ratings yet
- Intern Research UpdateDocument8 pagesIntern Research Updatemacbook airNo ratings yet
- Assessing Nutritional Status: The Role of BiomarkersDocument9 pagesAssessing Nutritional Status: The Role of Biomarkersparampam21No ratings yet
- Correlation of Blood Pressure With Body Mass Index Waist Circumference and Waist To Hip RatioDocument5 pagesCorrelation of Blood Pressure With Body Mass Index Waist Circumference and Waist To Hip RatioIsini sehansa amarathungaNo ratings yet
- CARDIO METABOLIC RISK FACTORS AMONG POSTMENOPAUSAL SUDANESE WOMEN 17oct (1) Revision-TrackedDocument28 pagesCARDIO METABOLIC RISK FACTORS AMONG POSTMENOPAUSAL SUDANESE WOMEN 17oct (1) Revision-Trackedhadiqa.iq95No ratings yet
- Is BMI The Best Measure of Obesity?: Anthropometric Measures in AdultsDocument4 pagesIs BMI The Best Measure of Obesity?: Anthropometric Measures in AdultsmuthmainnahNo ratings yet
- Percent Body Fat Is A Better Predictor of Cardiovascular Risk Factors Than Body Mass IndexDocument11 pagesPercent Body Fat Is A Better Predictor of Cardiovascular Risk Factors Than Body Mass IndexBrandon HeatNo ratings yet
- Body Mass Index and Body Composition Measures by Dual X-Ray Absorptiometry in Patients Aged 10 To 21 Years With Spinal Cord InjuryDocument8 pagesBody Mass Index and Body Composition Measures by Dual X-Ray Absorptiometry in Patients Aged 10 To 21 Years With Spinal Cord InjuryJoão Pedro PontesNo ratings yet
- Biopsychosocial Factors of Infertility Among Men in Surakarta, Central JavaDocument8 pagesBiopsychosocial Factors of Infertility Among Men in Surakarta, Central Javaannisa habibullohNo ratings yet
- Comparative Studies of Diabetes in Adult Nigerians Lipid Profile and Antioxidants Vitamins A and CDocument5 pagesComparative Studies of Diabetes in Adult Nigerians Lipid Profile and Antioxidants Vitamins A and CEditor IJTSRDNo ratings yet
- Prevalence of Overweight, Obesity and Abdominal Obesity in Bangladeshi University StudentsDocument4 pagesPrevalence of Overweight, Obesity and Abdominal Obesity in Bangladeshi University StudentsTengiz VerulavaNo ratings yet
- 125935571Document3 pages125935571UmialqyNo ratings yet
- Body Mass Index: Is It Relevant For Indians?: SciencedirectDocument4 pagesBody Mass Index: Is It Relevant For Indians?: SciencedirectLeon VásquezNo ratings yet
- BackgroundDocument16 pagesBackgroundDani KusumaNo ratings yet
- Obesity Is Not A RiskDocument7 pagesObesity Is Not A Riskcarlos.alberto.palacios.serratNo ratings yet
- K Winters Lab Report 4Document13 pagesK Winters Lab Report 4api-314083880No ratings yet
- JAPI Body FatDocument6 pagesJAPI Body FatBhupendra MahantaNo ratings yet
- Co-Relation Between Body Mass Index and Intraocular Pressure in AdultsDocument4 pagesCo-Relation Between Body Mass Index and Intraocular Pressure in AdultsAngkat Prasetya Abdi NegaraNo ratings yet
- Deurenberg Formula Imc para %grasaDocument10 pagesDeurenberg Formula Imc para %grasaAna Cecilia VegaNo ratings yet
- Studies On The Correlation of Anthropometric Measurement With Health Outcome in ElderlyDocument8 pagesStudies On The Correlation of Anthropometric Measurement With Health Outcome in ElderlyAnis RanisNo ratings yet
- Garcia 2020Document8 pagesGarcia 2020professor do valeNo ratings yet
- Height, Weight, and Body Mass Index of Elderly Persons in TaiwanDocument7 pagesHeight, Weight, and Body Mass Index of Elderly Persons in TaiwanSamuel XiaoNo ratings yet
- Article AmalDocument16 pagesArticle Amalsaliha mharchiNo ratings yet
- FONTAINE, K. R. Et Al.. Years of Life Lost Due To ObesityDocument7 pagesFONTAINE, K. R. Et Al.. Years of Life Lost Due To Obesityalline.valleNo ratings yet
- Mid-Upper Arm Circumference As An Indicator of UnderweightDocument7 pagesMid-Upper Arm Circumference As An Indicator of UnderweightgianellaNo ratings yet
- Association of Underweight Status With The Risk of Tuberculosis: A Nationwide Population Based Cohort StudyDocument8 pagesAssociation of Underweight Status With The Risk of Tuberculosis: A Nationwide Population Based Cohort StudygregoriusbudisetiawaNo ratings yet
- Sarcopenic Obesity Predicts Instrumental Activities of Daily Living Disability in The ElderlyDocument10 pagesSarcopenic Obesity Predicts Instrumental Activities of Daily Living Disability in The ElderlyFranchesca OrtizNo ratings yet
- Body Mass Index, Waist Hip Ratio, and Waist Circumference: Which Measure To Classify Obesity?Document10 pagesBody Mass Index, Waist Hip Ratio, and Waist Circumference: Which Measure To Classify Obesity?Riefka Ananda ZulfaNo ratings yet
- JCCM MS Id 000138Document7 pagesJCCM MS Id 000138chiquitaputriNo ratings yet
- A Comparative Study of Association of Lipid Profile With Body Mass Index in General PopulationDocument5 pagesA Comparative Study of Association of Lipid Profile With Body Mass Index in General PopulationIJAR JOURNALNo ratings yet
- 07 MJN 24 (3) Nopphanath Et Al.Document10 pages07 MJN 24 (3) Nopphanath Et Al.Egy SunandaNo ratings yet
- Hyperemesis Gravidarum and Its Relation With Maternal Body Fat CompositionDocument6 pagesHyperemesis Gravidarum and Its Relation With Maternal Body Fat CompositionEver Medina UnchupaicoNo ratings yet
- Bmi ThesisDocument7 pagesBmi ThesisBestOnlinePaperWritingServiceCanada100% (2)
- 192 Iajps192092020 PDFDocument5 pages192 Iajps192092020 PDFiajpsNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 196 Iajps196092020 PDFDocument4 pages196 Iajps196092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureDocument6 pagesPharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureiajpsNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 191 Iajps191092020Document8 pages191 Iajps191092020iajpsNo ratings yet
- 194 Iajps194092020 PDFDocument7 pages194 Iajps194092020 PDFiajpsNo ratings yet
- 195 Iajps195092020 PDFDocument5 pages195 Iajps195092020 PDFiajpsNo ratings yet
- 197 Iajps197092020 PDFDocument5 pages197 Iajps197092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswlDocument6 pagesPharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswliajpsNo ratings yet
- 50 Iajps50102020Document13 pages50 Iajps50102020iajpsNo ratings yet
- Pharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationDocument4 pagesPharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationiajpsNo ratings yet
- Pharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreDocument6 pagesPharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreiajpsNo ratings yet
- Pharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersDocument7 pagesPharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersiajpsNo ratings yet
- 44 Iajps44102020Document4 pages44 Iajps44102020iajpsNo ratings yet
- 46 Iajps46102020Document7 pages46 Iajps46102020iajpsNo ratings yet
- Pharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationDocument4 pagesPharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationiajpsNo ratings yet
- 34 Iajps34102020Document7 pages34 Iajps34102020iajpsNo ratings yet
- 42 Iajps42102020Document8 pages42 Iajps42102020iajpsNo ratings yet
- 40 Iajps40102020Document4 pages40 Iajps40102020iajpsNo ratings yet
- Pharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationDocument12 pagesPharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationiajpsNo ratings yet
- Pharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistanDocument5 pagesPharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistaniajpsNo ratings yet
- Pharmaceutical SciencesDocument5 pagesPharmaceutical SciencesiajpsNo ratings yet
- Pharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleDocument6 pagesPharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleiajpsNo ratings yet
- 37 Iajps37102020Document9 pages37 Iajps37102020iajpsNo ratings yet
- 33 Iajps33102020Document6 pages33 Iajps33102020iajpsNo ratings yet
- 35 Iajps35102020Document4 pages35 Iajps35102020iajpsNo ratings yet
- Pharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsDocument8 pagesPharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsiajpsNo ratings yet
- Pharmaceutical Sciences: Clinical Manifestations of Sars-Cov-2 (Covid19)Document5 pagesPharmaceutical Sciences: Clinical Manifestations of Sars-Cov-2 (Covid19)iajpsNo ratings yet
- Pharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaDocument3 pagesPharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaiajpsNo ratings yet
- Reading and Writing Ophthalmology NotesDocument8 pagesReading and Writing Ophthalmology NotesayuniNo ratings yet
- DIURETICS Flow ChartDocument3 pagesDIURETICS Flow Chartdonnam86No ratings yet
- Phase 1/2/3 COVID-19 Vaccine Candidate StudyDocument28 pagesPhase 1/2/3 COVID-19 Vaccine Candidate StudychamniezbuntowanyNo ratings yet
- Pantoea Agglomerans - ADocument9 pagesPantoea Agglomerans - AmadelaineNo ratings yet
- Virex II 256: Broad Spectrum Environmental Cleaner & DisinfectantDocument4 pagesVirex II 256: Broad Spectrum Environmental Cleaner & DisinfectantYOGENDER NIJHAVANNo ratings yet
- Natriuretic Peptide Measurement in NonDocument2 pagesNatriuretic Peptide Measurement in NonAde YonataNo ratings yet
- Cancer Case StudyDocument23 pagesCancer Case StudyMeynard AndresNo ratings yet
- NYU Langone Cobble Hill Fact SheetDocument2 pagesNYU Langone Cobble Hill Fact SheetPaco Dave Abraham0% (1)
- PSMID COVID-19 Interim Management Guidelines v.0330204134599980641528159Document47 pagesPSMID COVID-19 Interim Management Guidelines v.0330204134599980641528159kira santosNo ratings yet
- Pathophysiology Cushing S SyndromeDocument4 pagesPathophysiology Cushing S SyndromeMaria Luisa VillalunaNo ratings yet
- ComDocument2 pagesComKit LaraNo ratings yet
- Care For Critically Ill Patients With COVID-19: Clinical UpdateDocument2 pagesCare For Critically Ill Patients With COVID-19: Clinical UpdateNicole BatistaNo ratings yet
- Pediatric Critical Care, 3rd Edition 2009 DR - NaggarDocument389 pagesPediatric Critical Care, 3rd Edition 2009 DR - NaggarmariamNo ratings yet
- Presented by DR - Asha V Sasi 2 MD CR DeptDocument32 pagesPresented by DR - Asha V Sasi 2 MD CR DeptSariIdaMihartiNo ratings yet
- Emergency Radiology With QuizDocument115 pagesEmergency Radiology With QuizJustisia PadmiyatiNo ratings yet
- 4 Byron Burlingame 2Document72 pages4 Byron Burlingame 2watimelawatiNo ratings yet
- Alcoholic KetoacidosisDocument3 pagesAlcoholic KetoacidosisFaishal HanifNo ratings yet
- Microbiology EssayDocument14 pagesMicrobiology Essaykgdelacruz24810No ratings yet
- Rarwrdqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrdqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Myasthenia Gravis and Physical ExerciseDocument12 pagesMyasthenia Gravis and Physical ExerciseRajkamal SarmaNo ratings yet
- Diabetic Foot SyndromeDocument121 pagesDiabetic Foot SyndromeCristian RajagukgukNo ratings yet
- Community Medicine Solved BCQs 8th Semester MBBS LUMHS-1Document27 pagesCommunity Medicine Solved BCQs 8th Semester MBBS LUMHS-1rameez ahmedNo ratings yet
- Hindu News Issue 04-2015Document24 pagesHindu News Issue 04-2015LiberBlissNo ratings yet
- Epstein Barr VirusDocument13 pagesEpstein Barr VirusDianaLorenaNo ratings yet
- Bahasa Inggris 2 Teknik Mesin Kamis 1-PM/2ME-A/B/2TPKM Dra. Mulyati Khorina, M.Hum. 4 90Document5 pagesBahasa Inggris 2 Teknik Mesin Kamis 1-PM/2ME-A/B/2TPKM Dra. Mulyati Khorina, M.Hum. 4 90purnaNo ratings yet
- Neet Pedigree Questions Worksheet 5ef6eb6eca031Document8 pagesNeet Pedigree Questions Worksheet 5ef6eb6eca031sarudarshinij.s123No ratings yet
- Practical Applications of Immunology Written ReportDocument9 pagesPractical Applications of Immunology Written ReportVincent Drystan AdronNo ratings yet
- Analysis Story of An HourDocument4 pagesAnalysis Story of An HourChristian Lenain100% (1)
- Nutrition Follow-Up Progress ReportDocument3 pagesNutrition Follow-Up Progress Reportapi-545899804No ratings yet
- Critical Care Nursing: Airway Obstruction ManagementDocument8 pagesCritical Care Nursing: Airway Obstruction ManagementMichelle MallareNo ratings yet