Professional Documents
Culture Documents
FP Ago 2020 - Efecto Del Cpap Sobre La Hemodinamia Cerebral en La Hemodinámica Del Prematuro
Uploaded by
julius castelloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
FP Ago 2020 - Efecto Del Cpap Sobre La Hemodinamia Cerebral en La Hemodinámica Del Prematuro
Uploaded by
julius castelloCopyright:
Available Formats
ORIGINAL RESEARCH
published: 21 August 2020
doi: 10.3389/fped.2020.00487
Effects of Nasal Continuous Positive
Airway Pressure on Cerebral
Hemodynamics in Preterm Infants
Han Zhou 1,2† , Xuewen Hou 1† , Rui Cheng 1 , Youyan Zhao 1* and Jie Qiu 1*
1
Department of Newborn Infants, Children’s Hospital of Nanjing Medical University, Nanjing, China, 2 Department of
Paediatrics, Nantong First People’s Hospital, Nantong, China
Background: To evaluate the effects of pressure levels on cerebral hemodynamics in
premature infants receiving nasal continuous positive airway pressure (nCPAP) during
the first 3 days of life.
Methods: Forty-four preterm infants treated with nCPAP were divided into two groups:
very preterm infants [gestational age 1 (GA1), GA < 32 weeks, n = 24] and moderate/late
preterm infants (GA2 group, GA 32–37 weeks, n = 20). During monitoring, pressure
Edited by:
Graeme R. Polglase,
levels were set at 4→6→8→4 cmH2 O, and cerebral hemodynamics was assessed by
Monash University, Australia near-infrared spectroscopy (NIRS). Vital signs, peripheral oxygen saturation (SpO2 ) and
Reviewed by: transcutaneous carbon dioxide pressure (TcPCO2 ) were simultaneously recorded.
Ulrich Herbert Thome,
Leipzig University, Germany Results: Pressures of 4–8 cmH2 O had no significant influence on cerebral
Brett James Manley, hemodynamics, TcPCO2 , SpO2 or other vital signs. The tissue oxygenation index (TOI),
The University of Melbourne, Australia
the difference between oxygenated hemoglobin (1HbO2 ) and deoxygenated hemoglobin
Calum Roberts,
Monash University, Australia (1HHb) (1HbD), and cerebral blood volume (1CBV) were all significantly positively
*Correspondence: correlated with gestational and post-natal age, with fluctuations being greater in the GA1
Youyan Zhao group. 1HbD and 1CBV were also significantly positively correlated with TcPCO2 .
1051661432@qq.com
Jie Qiu Conclusions: No significant differences were observed in cerebral hemodynamics when
qiujie@njmu.edu.cn
the nCPAP pressure was set to 4–8 cmH2 O.
† These authors have contributed
Keywords: cerebral hemodynamics, nasal continuous positive airway pressure, near-infrared spectroscopy,
equally to this work
pressure, preterm infant
Specialty section:
This article was submitted to
INTRODUCTION
Neonatology,
a section of the journal
Neonatal respiratory distress syndrome (RDS) is a common respiratory disorder in premature
Frontiers in Pediatrics
infants. Non-invasive respiratory support is the optimal respiratory support method for RDS.
Received: 27 March 2020 Nasal continuous positive airway pressure (nCPAP), one of the most common non-invasive
Accepted: 13 July 2020
assisted ventilation methods, is widely used in the neonatal intensive care unit (NICU). Although
Published: 21 August 2020
management of RDS is improving, nCPAP is still a crucial therapeutic measure of RDS (1).
Citation:
In recent years, increasing numbers of researchers are paying attention to the effects of nCPAP
Zhou H, Hou X, Cheng R, Zhao Y and
Qiu J (2020) Effects of Nasal
on cerebral hemodynamics (2–4). Some researchers consider the pressure of nCPAP to increase
Continuous Positive Airway Pressure intrathoracic pressure, impede systemic and pulmonary venous return (5), and decrease cardiac
on Cerebral Hemodynamics in output (CO) (6), which may ultimately decrease cerebral perfusion. Egwu et al. demonstrated that
Preterm Infants. Front. Pediatr. 8:487. nCPAP might represent an independent predictor for intraventricular hemorrhage (IVH) in early
doi: 10.3389/fped.2020.00487 preterm neonates (7). There is currently disagreement on the optimal nCPAP pressure for preterm
Frontiers in Pediatrics | www.frontiersin.org 1 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
RDS, and 4–6 cmH2 O is a common range applied in the NICU (3) Apgar scores > 7 at 1, 5, and 10 min. Exclusion criteria were
(3, 4). However, some researchers prefer to use 8 cmH2 O or even one or any combination of the following: (1) peripheral oxygen
higher pressures (8) because 8 cmH2 O has larger end-expiratory saturation (SpO2 ) not maintained in the normal range during
volume and tidal volume, as well as a lower respiratory rate and the monitoring process; (2) infants did not stay calm during
thoracoabdominal asynchrony than when using 2–6 cmH2 O (8). the monitoring process; (3) serious brain injuries caused by
Therefore, in premature infants, it is important that clinically asphyxia, birth injury, intrauterine infection or others; (4) genetic
utilized nCPAP pressures are safe for the developing preterm metabolic diseases; and (5) serious congenital heart disease,
brain. The cost-benefit ratio needs to be weighed to choose an nervous system malformation or other congenital diseases or
appropriate nCPAP pressure. serious complications. This study was approved by the ethics
Although it has been demonstrated that the use of nCPAP committee of Children’s Hospital of Nanjing Medical University,
decreases cerebral perfusion in healthy adult volunteers (9), and consent was obtained from all infants’ parents.
study results in preterm infants are distinct. Dani et al. found All enrolled infants were divided into 2 groups according to
that nCPAP pressures of 2–6 cmH2 O did not affect cerebral GA. The first group comprised very preterm infants (GA1 group,
oxygenation or cerebral blood volume in RDS preterm infants GA < 32 weeks, n = 24) with the following distributions: ① 1-day
with <30 weeks’ gestation during the first 10 days of life (3). group: monitoring within 24 h after birth (n = 7); ② 2-days
Bembich S et al. also found no obvious fluctuations in CBF group: monitoring between 24 and 48 h after birth (n = 9); and
in preterm newborns of 26–33 weeks’ gestation whose ages at ③ 3-days group: monitoring between 48 and 72 h after birth (n =
observation were 2–21 days (median age was 6 days) using 8). The second group comprised moderate to late preterm infants
nCPAP with pressures of 3–8 cmH2 O (4). It is well-known that (GA2 group, GA 32–36+6 weeks, n = 20) with the following
the first 3 days after birth are important for RDS treatment, distributions: ① 1-day group: monitoring within 24 h after birth
and application of nCPAP during this period is vital to cure (n = 6); ② 2-days group: monitoring between 24 and 48 h after
premature infants with RDS. However, during this period, the birth (n = 7); ③ 3-days group: monitoring between 48 and 72 h
CBF of premature infants is very unstable, which may cause IVH, after birth (n = 7).
hypoxic-ischemic brain damage and other brain injuries. It is
important to understand the adaptive changes in the cerebral Procedures
circulation of premature infants during the first 3 days of life NCPAP was provided by the Stephan CPAP system (Stephan;
(10, 11). Therefore, in this study, we investigated the effects Rheinland-Pfalz, Gackenbach, Germany). The pressure was
of nCPAP pressures on cerebral hemodynamics in premature initially set at 4 cmH2 O, and data were recorded for 30 min.
infants during the first 3 days of life. Subsequently, the pressure was raised to 6 and 8 cmH2 O for
Preterm infants receiving nCPAP within the first 3 days of an additional 30 min each of recording. Last, the pressure was
life were selected for examination of cerebral hemodynamics returned to 4 cmH2 O for another 30 min. The nCPAP pressure
using near-infrared spectroscopy (NIRS) when nCPAP pressures was kept constant during each time point. All infants were in the
varied from 4 to 8 cmH2 O. We focused on assessing the safety supine position with mouth closed using pacifiers and were quiet
and stability of nCPAP on cerebral hemodynamics in premature or sleeping during the monitoring process.
infants during the first 3 days of life. The purpose of this study
was to provide a theoretical basis for selecting safe and effective Outcomes
nCPAP pressure levels in premature infants with RDS soon The CBF and oxygenation, the primary outcomes, were
after birth. continuously monitored from the beginning to the end
of the procedures using NIRS (EGOS-600A, EnginMed;
MATERIALS AND METHODS Suzhou, Jiangsu, China). During the recording time, the tissue
oxygenation index (TOI), deoxygenated hemoglobin (1HHb),
Participants oxygenated hemoglobin (1HbO2 ) and total hemoglobin
This study was conducted in the NICU of Children’s Hospital (1tHb) were recorded. Cerebral blood volume (1CBV) and
of Nanjing Medical University from April 2018 to October the difference between 1HbO2 and 1HHb (1HbD) were
2018. Inclusion criteria were as follows: (1) preterm infants with calculated according to the following reported formula: 1CBV
gestational age (GA) <37 weeks; (2) preterm infants diagnosed = 1tHb × 0.89/Hb and 1HbD = 1HbO2 – 1HHb (3). Arterial
with RDS and receiving nCPAP within 3 days after birth; and hemoglobin (Hb) was measured within 12 h before beginning
the study.
Abbreviations: nCPAP, nasal continuous positive airway pressure; NICU, neonatal Secondary outcomes were transcutaneous carbon dioxide
intensive care unit; GA, gestational age; RDS, respiratory distress syndrome;
SpO2 , peripheral oxygen saturation; NIRS, near-infrared spectroscopy; TOI,
tension (TcPCO2 ), SpO2 , and other vital signs. TcPCO2 was
tissue oxygenation index; 1HbO2 , oxygenated hemoglobin; 1HHb, deoxygenated measured using a TCM4 Combim (Radiometer; Brea, California,
hemoglobin; 1tHb, total hemoglobin; 1CBV, cerebral blood volume; 1HbD, United States). For non-invasive monitoring of SpO2 , heart rate
difference between 1HbO2 and 1HHb; Hb, hemoglobin; HR, heart rate; (HR) and respiratory rate (RR), a pulse oximeter probe (N-300
R
,
RR, respiratory rate; MABP, mean systemic arterial blood pressure; TcPCO2 , Nellcor; Minneapolis, Minnesota, United States) was placed
transcutaneous carbon dioxide pressure; IVH, intraventricular hemorrhage; MV,
mechanical ventilation; PS, pulmonary surfactant; EEG, electroencephalography;
around the right wrist/hand. The mean systemic arterial blood
CBF, cerebral blood flow; CBFV, cerebral blood flow velocity; RI, resistance index; pressure (MABP) was measured non-invasively every 30 min
CO, cardiac output. using a neonatal cuff around the slightly outstretched left upper
Frontiers in Pediatrics | www.frontiersin.org 2 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
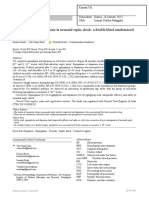
FIGURE 1 | Study profile and patient flow.
arm. Vital signs (SpO2 , HR, RR and MABP) were recorded RESULTS
every 30 min by using an IntelliVue MP50 Monitor (Philips;
Amsterdam, Netherlands). Demographic Variables
From April 2018 to October 2018, 44 preterm infants receiving
nCPAP were enrolled in this study (flow diagram, Figure 1).
Clinical and demographic data are presented in Table 1. Except
Statistical Analysis
for GA and birth weight (P = 0.00), there were no significant
No a priori sample size was determined. However, this sample
differences in sex, multiple births, mode of delivery, Apgar
of 44 preterm infants gives ∼75% power to detect at least
scores, prenatal use of glucocorticoids, premature rupture of fetal
a 10% difference in CBF. SPSS 22.0 was used for statistical
membranes or initial HR, RR, and MABP between the two groups
analysis. Normally distributed data are presented as the mean
(P > 0.05). Among the subgroups in each group, there were no
value ± standard deviation (x̄ ± s), and the t-test was used
significant differences in any variables (P > 0.05).
for comparison between two groups. Analysis of variance was
used to compare multiple groups, and if the difference was
statistically significant, the post-hoc Bonferroni test was used
Effects of Different nCPAP Pressure Levels
for further comparison. Continuous data are presented as the on Cerebral Hemodynamics, TcPCO2 ,
number of cases or percentages (%), and Fisher’s exact test was SpO2 , and Other Vital Signs
used for comparison between two groups. Pearson correlation In enrolled infants, the baseline set nCPAP pressure was 4
was conducted to analyze correlations in the data, and P < 0.05 cmH2 O, and FiO2 was 0.21–0.25 to maintain SpO2 at 92–96%.
was considered statistically significant. The pressure, which was set from 4 to 8 cmH2 O, had no
Frontiers in Pediatrics | www.frontiersin.org 3 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
TABLE 1 | Clinical and demographic characteristics of neonates.
Very preterm infant group (n = 24) Moderate and late preterm group (n = 20)
1 day group 2 days group 3 days group 1 day group 2 days group 3 days group
(n = 7) (n = 9) (n = 8) (n = 6) (n = 7) (n = 7)
Sex 3/4 5/4 4/4 3/3 4/3 3/4
(Male/Female)
Multiple births 1 (14.3) 3 (33.3) 2 (25.0) 1 (16.7) 1 (14.3) 2 (28.6)
[n (%)]
Gestational age 28.6 ± 1.8 29.0 ± 1.5 28.8 ± 1.5 34.4 ± 0.8* 33.6 ± 1.5* 33.3 ± 3.6*
(x̄ ± s, weeks)
Birth weight 1174 ± 170 1314 ± 281 1161 ± 209 2151 ± 125* 2070 ± 184* 1913 ± 298*
(x̄ ± s, g)
Cesarean 3 (42.9) 6 (66.7) 6 (75.0) 4 (66.7) 5 (71.4) 5 (71.4)
[n (%)]
1 min Apgar 8.0 ± 1.0 7.7 ± 1.8 7.6 ± 2.1 8.3 ± 1.0 8.7 ± 1.1 8.6 ± 0.8
(x̄ ± s)
5 min Apgar 8.9 ± 0.7 7.7 ± 0.6 8.8 ± 0.5 9.3 ± 1.0 9.4 ± 0.5 9.3 ± 0.5
(x̄ ± s)
Prenatal use of glucocorticoids 4 (57.1) 6 (66.7) 5 (62.5) 3 (50.0) 4 (57.1) 3 (42.9)
[n (%)]
Premature rupture of fetal 4 (57.1) 4 (44.4) 3 (37.5) 2 (33.3) 5 (71.4) 3 (42.9)
membranes >24 h
[n (%)]
HR 145 ± 7 144 ± 8 142 ± 6 142 ± 8 143 ± 10 140 ± 7
(x̄ ± s)
RR 46 ± 8 45 ± 6 43 ± 7 43 ± 5 45 ± 8 42 ± 6
(x̄ ± s)
MABP 38 ± 8 40 ± 7 42 ± 5 42 ± 6 43 ± 7 45 ± 5
(x̄ ± s)
Gestational age and birth weight of GA2 group were all significant higher than that of GA1 group at the same post-natal age (*P < 0.05).
significant influence on cerebral hemodynamics either in very The TOI, 1HbD and 1CBV of very preterm infants gradually
preterm infants (Figure 2A) or in moderate to late preterm increased during the first 3 days of life, and differences
infants (Figure 2B). Though 1HbD and 1CBV tended to decline between the three groups were significant (P < 0.05). In
at 8 cmH2 O, the difference was not significant (P > 0.05). moderate to late preterm infants, compared with the 1-day
Furthermore, in the very preterm infant (Figure 3A) and the group, TOI and 1CBV markedly increased in the 2- and 3-
moderate to late preterm infant (Figure 3B) groups, nCPAP days groups (P < 0.05). However, TOI and 1CBV were not
pressure levels of 4–8 cmH2 O had no significant influence on significantly different between the 2- and 3-days groups (P >
TcPCO2 , SpO2 or other vital signs (P > 0.05). 0.05), while 1HbD among the three groups exhibited significant
differences (P < 0.05).
Related Factor Analysis of Cerebral
Hemodynamics DISCUSSION
The TOI was significantly positively correlated with GA
(r = 0.749, P < 0.05) and post-natal age (r = 0.799, P < 0.05) In this study, we evaluated the effects of nCPAP pressure on
(Figure 4A). 1HbD was significantly positively correlated with cerebral hemodynamics in premature infants, demonstrating
GA (r = 0.546, P < 0.05), post-natal age (r = 0.844, P < 0.05), and several novel and interesting findings. First, nCPAP pressures
TcPCO2 (r = 0.826, P < 0.05) (Figure 4B). Similarly, 1CBV was of 4–8 cmH2 O had no significant influence on the cerebral
significantly positively correlated with GA (r = 0.905, P < 0.05), hemodynamics, vital signs, SpO2, or TcPCO2 of preterm infants.
post-natal age (r = 0.821, P < 0.05), and TcPCO2 (r = 0.887, Second, TOI, 1HbD, and 1CBV were all significantly positively
P < 0.05) (Figure 4C). correlated with GA and post-natal age. 1HbD and 1CBV were
also significantly positively correlated with TcPCO2 . Finally, TOI,
Effects of GA and Post-natal Age on 1HbD, and 1CBV in moderate to late preterm infants were
Cerebral Hemodynamics significantly higher than in very preterm infants at different
As shown in Figure 5, the TOI, 1HbD and 1CBV in moderate post-natal ages. TOI, 1HbD, and 1CBV in the two groups all
to late preterm infants were all significantly higher than in gradually increased during the first 3 days of life, and fluctuations
very preterm infants at the same post-natal age (P < 0.05). in very preterm infants were even greater.
Frontiers in Pediatrics | www.frontiersin.org 4 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
FIGURE 2 | Effects of nCPAP pressure levels on cerebral hemodynamics. NCPAP pressures of 4–8 cmH2 O had no significant influence on TOI, 1HbD or 1CBV in
either very preterm infants (A) or moderate to late preterm infants (B) (P > 0.05).
NCPAP, the most common respiratory support used in the pressure caused by pressure due to their highly compliant chest
NICU, delivers continuous positive air pressure into the airway wall, which ultimately reduces the effect of pressure on cerebral
to improve oxygenation by maintaining lung volume, increasing hemodynamics (10, 11). Two studies found that nCPAP at
pulmonary functional residual capacity and reducing airway pressure levels of 10 and 12 cmH2 O decreased CBF in adults
resistance. Some researchers think that nCPAP might decrease (9, 17). Hsu et al. (6) also observed that nCPAP affects neonatal
cerebral perfusion by increasing intrathoracic pressure, lowering CO when the nCPAP pressure was 10 cmH2 O. These findings
CO, and increasing central venous and intracranial pressure (12– suggest that extra high pressure affects cerebral hemodynamics.
14). However, Beker et al. (15) found that the CO and MABP were However, our results indicated that pressure at a level of 8 cmH2 O
unchanged at pressure levels of 4, 6, and 8 cmH2 O in preterm had no significant effect on cerebral hemodynamics in preterm
infants. Moritz et al. (16) also demonstrated that nCPAP with a infants. Hence, cerebral hemodynamics in premature infants
mean level of 4 cmH2 O (up to 7 cmH2 O) did not influence CO remains relatively stable when the pressure is set within the range
in preterm infants. Our results also supported that the nCPAP of 4–8 cmH2 O.
pressure that was set from 4 to 8 cmH2 O did not significantly The TOI is a parameter measured directly by NIRS and
influence cerebral hemodynamics. We speculate that infants simply reflects the oxygen content in local brain tissue. 1HbD
may be able to quickly compensate for increased intrathoracic is reported to be a powerful target that sensitively reflects CBF
Frontiers in Pediatrics | www.frontiersin.org 5 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
FIGURE 3 | Effects of nCPAP pressure levels on TcPCO2 , SpO2 and other vital signs. NCPAP pressures of 4–8 cmH2 O had no significant influence on TcPCO2 , SpO2
or other vital signs in either very preterm infants (A) or moderate to late preterm infants (B) (P > 0.05).
FIGURE 4 | Related factor analysis of cerebral hemodynamics. (A) TOI was significantly positively correlated with GA (r = 0.749, P < 0.05) and post-natal age
(r = 0.799, P < 0.05). (B) 1HbD was significantly positively correlated with GA (r = 0.546, P < 0.05), post-natal age (r = 0.844, P < 0.05), and TcPCO2 (r = 0.826,
P < 0.05). (C) 1CBV was significantly positively correlated with GA (r = 0.905, P < 0.05), post-natal age (r = 0.821, P < 0.05), and TcPCO2 (r = 0.887, P < 0.05).
(18, 19). 1CBV reflects cerebral blood volume and is correlated we also demonstrated that cerebral oxygenation and CBF are
with CBF. Our results demonstrated that TOI, 1HbD, and significantly correlated with post-natal age in preterm infants
1CBV are all significantly positively correlated with GA and during the early days of life. The reasons for this may
post-natal age, which is consistent with other reports (18, 20). include increased CO, arterial ductal closure and decreased
TOI, 1HbD, and 1CBV in moderate to late preterm infants intracranial pressure after birth (23). Of note, although cerebral
were significantly higher than in very preterm infants at different hemodynamics in both groups gradually increased during the
post-natal ages. Using Doppler color ultrasonography, Pezzati first 3 days of life, fluctuations in very preterm infants were
et al. found that with increased GA, the resistance index (RI) greater than those in moderate to late preterm infants. We
decreased, and cerebral blood flow velocity (CBFV) subsequently speculate that premature infants of lower GA have weaker
significantly increased in both the anterior cerebral artery and autoregulation of cerebral hemodynamics, leading to larger
the right and left middle cerebral arteries (21). Therefore, fluctuations in blood flow and a greater possibility of brain
we believe that cerebral oxygenation and CBF improve with injury. Hence, clinicians need to avoid blood flow fluctuations in
increased GA through decreasing the RI of cerebral vessels premature infants, especially those who are extremely preterm,
and increasing CBFV. Consistent with previous findings (22), during the first days of life to reduce the risk of brain injuries.
Frontiers in Pediatrics | www.frontiersin.org 6 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
In addition, Dix et al. (24) showed that acute increases in
PaCO2 diminished brain activity, potentially leading to adverse
neurological outcomes in preterm infants. Therefore, clinicians
should also keep PaCO2 levels within a reasonable range and
avoid its fluctuation during the first days of life to reduce
the risk of brain injuries. Dix et al. (24) also found that
acute increases in PaCO2 are associated with increased cerebral
oxygenation. However, Naulaers et al. (20) found that the TOI
was independent of PaCO2 , consistent with our results. The exact
relationship between PaCO2 and cerebral oxygenation requires
further studies.
SpO2 is one of the most common and intuitive indicators used
in the NICU. Some studies have found that higher SpO2 prevents
brain damage through decreasing the incidence of intermittent
apnea, hypoxemia and bradycardia (27, 28). However, our
results did not reveal a correlation between SpO2 and cerebral
hemodynamics. There are several potential reasons for this.
There is a reported correlation between SpO2 and cerebral
oxygenation when SpO2 is severely low (29). However, the values
of SpO2 were high (91–98%) in our study, so this relationship
between SpO2 and cerebral oxygenation was not apparent. In
addition, high peripheral oxygenation does not necessarily lead
to high cerebral oxygenation in preterm infants (4). Thus, SpO2
may not represent cerebral oxygenation and CBF precisely in
preterm infants.
In this study, MABP did not obviously affect cerebral
oxygenation or CBF. MABP is reported to change CBF
when MABP is below 30 mmHg (30), but infants have an
autoregulatory ability to maintain stable CBF when MABP is in a
certain range, such as above 30 mmHg (31, 32). Therefore, some
neonatologists contend that maintaining MABP above 30 mmHg
may reduce the incidence of cerebral white matter lesions and
IVH (33, 34). In addition, Michelet et al. found that MABP does
not markedly influence cerebral oxygenation and CBF unless
it has large fluctuations (35). In this study, MABPs in infants
were all above 30 mmHg and did not exhibit large fluctuations,
FIGURE 5 | Effects of GA and post-natal age on cerebral hemodynamics. which may be the reason why no correlation between MABP and
TOI (A), 1HbD (B), and 1CBV (C) in moderate to late preterm infants (GA2)
cerebral hemodynamics was observed.
were all significantly higher than in very preterm infants (GA1) at the same
post-natal age (*P < 0.05). In both the GA1 and GA2 groups, TOI (A), 1HbD One limitation of this study is that infants were not repeatedly
(B), and 1CBV (C) at 2 and 3 days were significantly higher than at 1 day (a P measured but different infants were recruited for the different
< 0.05). In the GA1 group, TOI (A), 1HbD (B), and 1CBV (C) at 3 days were measurement time points. Because infants in this study were all
all significantly higher than those at 2 days (b P < 0.05). In the GA2 group, only pre-matures, in ethical terms, in order to avoid adverse effects
1HbD (B) at 3 days was significant higher than at 2 days (b P < 0.05).
of frequent operation on the same newborn especially very
preterm infants for three consecutive days, we didn’t measure
the cerebral hemodynamics in the same patient. However, except
GA and birth weight, there were no significant differences in
TcPCO2 is another related factor of cerebral hemodynamics. the clinical and demographic data to rid the different infants’
Our results monitored by TCM showed that TcPCO2 correlates problem. Second, this is a pilot study with a small sample
with CBF indexes, including 1HbD and 1CBV. In recent years, size intended to illustrate basic findings and we didn’t do the
more researchers have begun to realize the close relationship sample size calculation in advance. In the near future, for more
between carbon dioxide pressure (PaCO2 ) and brain injury in precise results, we will calculate the sample size and establish
preterm infants. It has been demonstrated that either overly high a blank control group for a larger study. In addition, besides
or overly low PaCO2 can both damage cerebral autoregulation NIRS, cerebral hemodynamic parameters will be observed using
and increase fluctuations in CBF, causing brain injuries, such transcranial Doppler flow measurements in future research and
as IVH (24, 25). Greisen et al. reported significant neurological long-term follow-up is needed.
abnormalities at 18 months in very-low-birth-weight infants In conclusion, nCPAP used at 4–8 cmH2 O pressure
who endured severe hypocapnia within 24 h of life (26). levels did not affect cerebral hemodynamics. Furthermore,
Frontiers in Pediatrics | www.frontiersin.org 7 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
cerebral hemodynamics in preterm infants with lower GA AUTHOR CONTRIBUTIONS
or post-natal age was more unstable, and maintaining the
stability of TcPCO2 may be crucial for reducing fluctuations JQ and YZ conceptualized and designed the study, coordinated
in CBF. and supervised the experiments, provided the research
materials/reagents, reviewed, and revised the manuscript.
DATA AVAILABILITY STATEMENT HZ conducted the experiments and collected data. XH analyzed
the data and drafted the initial manuscript. RC was involved
The raw data supporting the conclusions of this in data interpretation and manuscript preparation. All authors
article will be made available by the authors, without approved the final manuscript for submission and agreed to be
undue reservation. accountable for all aspects of the work.
FUNDING
ETHICS STATEMENT
This project was supported by the National Natural Science
This study was approved by the ethics committee of Children’s Foundation of China (No. 81671500), the Jiangsu Provincial Six
Hospital of Nanjing Medical University and achieved agreements Talent Peaks (WSN-157), the 333 project of Jiangsu Province,
from infants’ parents. Written informed consent to participate in Nanjing Sanitation Engineering of Young Talents during the 13th
this study was provided by the participants’ legal guardian/next Five-Years Plan Period (QRX17076), and the Jiangsu Provincial
of kin. Special Program of Medical Science (BL2012018).
REFERENCES atrophy in very preterm infants. Early Hum Dev. (1982) 7:221–38.
doi: 10.1016/0378-3782(82)90085-8
1. Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. 12. Feldman Z, Robertson CS, Contant CF, Gopinath SP, Grossman
European consensus guidelines on the management of respiratory RG. Positive end expiratory pressure reduces intracranial
distress syndrome−2019 update. Neonatology. (2019) 115:432–51. compliance in the rabbit. J Neurosurg Anesthesiol. (1997) 9:175–9.
doi: 10.1159/000499361 doi: 10.1097/00008506-199704000-00013
2. Milan A, Freato F, Vanzo V, Chiandetti L, Zaramella P. Influence 13. Duncan AW, Oh TE, Hillman DR. PEEP and CPAP. Anaesth Intensive Care.
of ventilation mode on neonatal cerebral blood flow and volume. (1986) 14:236–50. doi: 10.1177/0310057X8601400304
Early Hum Dev. (2009) 85:415–9. doi: 10.1016/j.earlhumdev.2009. 14. Clough JB, Duncan AW, Sly PD. The effect of sustained positive airway
01.008 pressure on derived cardiac output in children. Anaesth Intensive Care. (1994)
3. Dani C, Bertini G, Cecchi A, Corsini I, Pratesi S, Rubaltelli FF. Brain 22:30–4. doi: 10.1177/0310057X9402200106
haemodynamic effects of nasal continuous airway pressure in preterm 15. Beker F, Rogerson SR, Hooper SB, Wong C, Davis PG. The effects of nasal
infants of less than 30 weeks’ gestation. Acta Paediatr. (2007) 96:1421–5. continuous positive airway pressure on cardiac function in premature infants
doi: 10.1111/j.1651-2227.2007.00453.x with minimal lung disease: a crossover randomized trial. J Pediatr. (2014)
4. Bembich S, Travan L, Cont G, Bua J, Strajn T, Demarini S. Cerebral 164:726–9. doi: 10.1016/j.jpeds.2013.10.087
oxygenation with different nasal continuous positive airway pressure levels 16. Moritz B, Fritz M, Mann C, Simma B. Nasal continuous positive airway
in preterm infants. Arch Dis Child Fetal Neonatal Ed. (2015) 100:F165–8. pressure (n-CPAP) does not change cardiac output in preterm infants. Am
doi: 10.1136/archdischild-2014-306356 J Perinatol. (2008) 25:105–9. doi: 10.1055/s-2008-1040341
5. Abdel-Hady H, Matter M, Hammad A, El-Refaay A, Aly H. Hemodynamic 17. Kolbitsch C, Lorenz IH, Hörmann C, Schocke M, Kremser C, Zschiegner F,
changes during weaning from nasal continuous positive airway pressure. et al. The impact of increased mean airway pressure on contrast-enhanced
Pediatrics. (2008) 122:e1086–90. doi: 10.1542/peds.2008-1193 MRI measurement of regional cerebral blood flow (rCBF), regional cerebral
6. Hsu HS, Chen W, Wang NK. Effect of continuous positive airway pressure on blood volume (rCBV), regional mean transit time (rMTT), and regional
cardiac output in neonates. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. cerebrovascular resistance (rCVR) in human volunteers. Hum Brain Mapp.
(1996) 37:353–6. (2000) 11:214–22. doi: 10.1002/1097-0193(200011)11:3<214::AID-HBM70>3.
7. Egwu CC, Ogala WN, Farouk ZL, Tabari AM, Dambatta AH. Factors 0.CO;2-I
associated with intraventricular hemorrhage among preterm neonates in 18. Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ. Near infrared
aminu kano teaching hospital. Niger J Clin Pract. (2019) 22:298–304. spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr
doi: 10.4103/njcp.njcp_154_18 Res. (1998) 44:591–5. doi: 10.1203/00006450-199810000-00020
8. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal 19. Noone MA, Sellwood M, Meek JH, Wyatt JS. Postnatal adaptation of cerebral
Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, blood flow using near infrared spectroscopy in extremely preterm infants
et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. undergoing high-frequency oscillatory ventilation. Acta Paediatr. (2003)
(2010) 362:1970–9. doi: 10.1056/NEJMoa0911783 92:1079–84. doi: 10.1111/j.1651-2227.2003.tb02581.x
9. Keller E, Nadler A, Alkadhi H, Kollias SS, Yonekawa Y, Niederer 20. Naulaers G, Morren G, Van Huffel S, Casaer P, Devlieger H. Cerebral tissue
P. Noninvasive measurement of regional cerebral blood flow and oxygenation index in very premature infants. Arch Dis Child Fetal Neonatal
regional cerebral blood volume by near-infrared spectroscopy and Ed. (2002) 87:F189–92. doi: 10.1136/fn.87.3.F189
indocyanine green dye dilution. Neuroimage. (2003) 20:828–39. 21. Pezzati M, Dani C, Biadaioli R, Filippi L, Biagiotti R, Giani T, et al.
doi: 10.1016/S1053-8119(03)00315-X Early postnatal doppler assessment of cerebral blood flow velocity in
10. Noori S, Wlodaver A, Gottipati V, McCoy M, Schultz D, Escobedo M. healthy preterm and term infants. Dev Med Child Neurol. (2002) 44:745–52.
Transitional changes in cardiac and cerebral hemodynamics in term neonates doi: 10.1111/j.1469-8749.2002.tb00281.x
at birth. J Pediatr. (2012) 160:943–8. doi: 10.1016/j.jpeds.2011.12.008 22. Meek JH, Tyszczuk L, Elwell CE, Wyatt JS. Cerebral blood flow increases over
11. Thorburn RJ, Lipscomb AP, Stewart AL, Reynolds EOR, Hope PL. the first three days of life in extremely preterm neonates. Arch Dis Child Fetal
Timing and antecedents of periventricular haemorrhage and of cerebral Neonatal Ed. (1998) 78:F33–7. doi: 10.1136/fn.78.1.F33
Frontiers in Pediatrics | www.frontiersin.org 8 August 2020 | Volume 8 | Article 487
Zhou et al. nCPAP Pressures and Cerebral Hemodynamics
23. Arri SJ, Muehlemann T, Biallas M, Bucher HU, Wolf M. Precision of cerebral 31. Wyatt JS, Edwards AD, Cope M, Delpy DT, McCormick DC, Potter A,
oxygenation and hemoglobin concentration measurements in neonates et al. Responses of cerebral blood volume to changes in arterial carbon
measured by near-infrared spectroscopy. J Biomed Opt. (2011) 16:047005. dioxide tension in term and preterm infants. Pediatr Res. (1991) 29:553–7.
doi: 10.1117/1.3570303 doi: 10.1203/00006450-199106010-00007
24. Dix LML, Weeke LC, de Vries LS, Groenendaal F, Baerts W, van Bel F. Carbon 32. Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth weight
dioxide fluctuations are associated with changes in cerebral oxygenation infants have reduced cerebral blood flow. Pediatrics. (2004) 114:1591–6.
and electrical activity in infants born preterm. J Pediat. (2017) 187:66–72. doi: 10.1542/peds.2004-1073
doi: 10.1016/j.jpeds.2017.04.043 33. Miall-Allen VM, de Vries LS, Whitelaw AG. Mean arterial blood
25. Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, et al. Cerebral pressure and neonatal cerebral lesions. Arch Dis Child. (1987) 62:1068–9.
intravascular oxygenation correlates with mean arterial pressure in critically doi: 10.1136/adc.62.10.1068
ill premature infants. Pediatrics. (2000) 106:625–32. doi: 10.1542/peds.106. 34. Watkins AM, West CR, Cooke RW. Blood pressure and cerebral haemorrhage
4.625 and ischaemia in very low birthweight infants. Early Hum Dev. (1989) 19:103–
26. Greisen G, Munck H, Lou H. Severe hypocarbia in preterm infants 10. doi: 10.1016/0378-3782(89)90120-5
and neurodevelopmental deficit. Acta Paediatr Scand. (1987) 76:401–4. 35. Michelet D, Arslan O, Hilly J, Mangalsuren N, Brasher C, Grace R, et al.
doi: 10.1111/j.1651-2227.1987.tb10489.x Intraoperative changes in blood pressure associated with cerebral desaturation
27. Upton CJ, Milner AD, Stokes GM. Apnoea, bradycardia, and oxygen in infants. Paediatr Anaesth. (2015) 25:681–8. doi: 10.1111/pan.12671
saturation in preterm infants. Arch Dis Child. (1991) 66:381–5.
doi: 10.1136/adc.66.4_Spec_No.381 Conflict of Interest: The authors declare that the research was conducted in the
28. Finer NN, Barrington KJ, Hayes BJ, Hugh A. Obstructive, mixed, and central absence of any commercial or financial relationships that could be construed as a
apnea in the neonate: physiologic correlates. J Pediatr. (1992) 121:943–50. potential conflict of interest.
doi: 10.1016/S0022-3476(05)80349-X
29. Olbrecht VA, Skowno J, Marchesini V, Ding L, Jiang Y, Ward CG, et al. Copyright © 2020 Zhou, Hou, Cheng, Zhao and Qiu. This is an open-access article
An international, multicenter, observational study of cerebral oxygenation distributed under the terms of the Creative Commons Attribution License (CC BY).
during infant and neonatal anesthesia. Anesthesiology. (2018) 128:85–96. The use, distribution or reproduction in other forums is permitted, provided the
doi: 10.1097/ALN.0000000000001920 original author(s) and the copyright owner(s) are credited and that the original
30. Greisen G, Børch K. White matter injury in the preterm neonate: the publication in this journal is cited, in accordance with accepted academic practice.
role of perfusion. Dev Neurosci. (2001) 23:209–12. doi: 10.1159/0000 No use, distribution or reproduction is permitted which does not comply with these
46145 terms.
Frontiers in Pediatrics | www.frontiersin.org 9 August 2020 | Volume 8 | Article 487
You might also like
- HESI Evolve MED Surg Mini Questions-SmallDocument3 pagesHESI Evolve MED Surg Mini Questions-SmallVictor Ray Welker67% (12)
- Early Human Development: SciencedirectDocument8 pagesEarly Human Development: SciencedirectYurika Elizabeth SusantiNo ratings yet
- Progressive Anemia of Prematurity Is Associated With A Critical Increase in Cerebral Oxygen Extraction2020Early Human DevelopmentDocument7 pagesProgressive Anemia of Prematurity Is Associated With A Critical Increase in Cerebral Oxygen Extraction2020Early Human DevelopmentJuan Diego Vilca PinedaNo ratings yet
- EPNS/SFNP Guideline On The Anticoagulant Treatment of Cerebral Sinovenous Thrombosis in Children and NeonatesDocument10 pagesEPNS/SFNP Guideline On The Anticoagulant Treatment of Cerebral Sinovenous Thrombosis in Children and NeonatesMohammedNo ratings yet
- WRIGHT 2016_Continuous Positive Airway Pressure to Prevent Neonatal Lung InjuryDocument10 pagesWRIGHT 2016_Continuous Positive Airway Pressure to Prevent Neonatal Lung InjuryRafael JustinoNo ratings yet
- Jnksreenan 2001Document5 pagesJnksreenan 2001fitriNo ratings yet
- Noradrenaline safety in preterm infants with cardiovascular issuesDocument7 pagesNoradrenaline safety in preterm infants with cardiovascular issuesnzunaNo ratings yet
- Machine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyDocument9 pagesMachine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyNodi MNo ratings yet
- Kulthida Baingam, MD Manapat Phatigomet, MD Anucha Thatrimontrichai, MD Gunlawadee Maneenil, MD Supaporn Dissaneevate, MD Waricha Janjindamai, MDDocument9 pagesKulthida Baingam, MD Manapat Phatigomet, MD Anucha Thatrimontrichai, MD Gunlawadee Maneenil, MD Supaporn Dissaneevate, MD Waricha Janjindamai, MDdjonesthoracicNo ratings yet
- Inotropicos en Neonatos 2Document13 pagesInotropicos en Neonatos 2Paola DiazNo ratings yet
- Effect of Hemodynamic Significant Patent Ductus Arteriosus On Tissue Oxygenation in Preterm Infants Using Near-Infrared SpectrosDocument7 pagesEffect of Hemodynamic Significant Patent Ductus Arteriosus On Tissue Oxygenation in Preterm Infants Using Near-Infrared SpectrosLissaberti AmaliahNo ratings yet
- E351 Full PDFDocument13 pagesE351 Full PDFajes coolNo ratings yet
- A Review of Normal Values of Infant Sleep PolysomnographyDocument6 pagesA Review of Normal Values of Infant Sleep PolysomnographyGil CLNo ratings yet
- Ogs 63 293Document12 pagesOgs 63 293DavidNo ratings yet
- Infants: Analysis of Systemic Effects and Neonatal Clinical Outcomes Dopamine Versus Epinephrine For Cardiovascular Support in Low Birth WeightDocument12 pagesInfants: Analysis of Systemic Effects and Neonatal Clinical Outcomes Dopamine Versus Epinephrine For Cardiovascular Support in Low Birth WeightJuan Antonio Herrera LealNo ratings yet
- Prognostic Markers of Neonatal Outcomes in Full Term Neonates Suffering From Perinatal Asphyxia 2167 0897 1000193Document5 pagesPrognostic Markers of Neonatal Outcomes in Full Term Neonates Suffering From Perinatal Asphyxia 2167 0897 1000193Claudia BrînzaNo ratings yet
- Fped 2019 00453Document7 pagesFped 2019 00453rifqiNo ratings yet
- Estado Hemodinamico La Primera Semana de Vida en VLBWDocument7 pagesEstado Hemodinamico La Primera Semana de Vida en VLBWMaluNo ratings yet
- 2021 Article 817Document10 pages2021 Article 817Muriel FialiwanNo ratings yet
- End-Tidal Carbon Dioxide Measurement in Preterm Infants With Low Birth WeightDocument10 pagesEnd-Tidal Carbon Dioxide Measurement in Preterm Infants With Low Birth WeightAnalia ZeinNo ratings yet
- CPAP For Prevention CVE in OSADocument13 pagesCPAP For Prevention CVE in OSAenNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Early Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsDocument8 pagesEarly Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsKatharina GoeralNo ratings yet
- 10 1016@j Jpeds 2020 10 045Document24 pages10 1016@j Jpeds 2020 10 045YasintaUnusNo ratings yet
- Schmidt Et Al-2018-Pediatric PulmonologyDocument10 pagesSchmidt Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Efecto Del Surfatante Menos Invasivo Sobre La Oxigenación CerebralDocument9 pagesEfecto Del Surfatante Menos Invasivo Sobre La Oxigenación CerebralRonald MoralesNo ratings yet
- Epinephrine Versus Dopamine in Neonatal Septic Shock - A Double-BlindDocument12 pagesEpinephrine Versus Dopamine in Neonatal Septic Shock - A Double-Blindarman_cerberuzNo ratings yet
- Ductus ArteriosoDocument17 pagesDuctus ArteriosoJohn Romero CevallosNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- A Randomized Placebo-Controlled Pilot Trial of Early Targeted Non-Steroidal AntiInflammatory Drugs in Preterm Infants With A Patent Ductus ArteriosusDocument22 pagesA Randomized Placebo-Controlled Pilot Trial of Early Targeted Non-Steroidal AntiInflammatory Drugs in Preterm Infants With A Patent Ductus ArteriosusGlydenne Glaire Poncardas GayamNo ratings yet
- BMM 2018 0348Document14 pagesBMM 2018 0348Harpreet SinghNo ratings yet
- Evaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryDocument8 pagesEvaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryAudra Firthi Dea NoorafiattyNo ratings yet
- Hipertensi EnsefalopatiDocument6 pagesHipertensi EnsefalopatiLeonardo JeversonNo ratings yet
- Background: Corresponding AuthorDocument8 pagesBackground: Corresponding AuthorPratiwi UmbohNo ratings yet
- ND ACDocument6 pagesND ACEsther Najera GalarretaNo ratings yet
- Journal ReadingDocument5 pagesJournal ReadingRoma WestNo ratings yet
- JR NeuroanestesiDocument11 pagesJR Neuroanestesiliashuban29No ratings yet
- Non Invasive HFO Time For Consideration 2017Document3 pagesNon Invasive HFO Time For Consideration 2017OsmanyNo ratings yet
- Pediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDDocument6 pagesPediatric Neurology: Hye-Ryun Yeh MD, Min-Jee Kim MD, Tae-Sung Ko MD, PHD, Mi-Sun Yum MD, PHD, Su-Jeong You MD, PHDAdrian KhomanNo ratings yet
- Pinchefsky 2019Document10 pagesPinchefsky 2019Devi Albaiti JannatiNo ratings yet
- Bassler 2018 Ensayo CohorteDocument10 pagesBassler 2018 Ensayo Cohortewisdom loverNo ratings yet
- Atik Jurnal Nicu 1950695Document17 pagesAtik Jurnal Nicu 1950695atikNo ratings yet
- LAMPLAND 2009_Observational Study of Humidified High-Flow Nasal Cannula Compared With Nasal Continuous Positive Airway PressureDocument8 pagesLAMPLAND 2009_Observational Study of Humidified High-Flow Nasal Cannula Compared With Nasal Continuous Positive Airway PressureRafael JustinoNo ratings yet
- Early Functional and Morpholical Brain RCIUDocument6 pagesEarly Functional and Morpholical Brain RCIUAndrea PederziniNo ratings yet
- Transabdominal ultrasound of lung bases predicts bronchopulmonary dysplasia in preterm neonatesDocument5 pagesTransabdominal ultrasound of lung bases predicts bronchopulmonary dysplasia in preterm neonatesBunga alaraafNo ratings yet
- Periodic Breathing and Apnea in Preterm InfantsDocument4 pagesPeriodic Breathing and Apnea in Preterm InfantsIvan VeriswanNo ratings yet
- Chronotherapy For Hypertension in Obstructive Sleep Apnoea (CHOSA) : A Randomised, Double-Blind, Placebo-Controlled Crossover TrialDocument9 pagesChronotherapy For Hypertension in Obstructive Sleep Apnoea (CHOSA) : A Randomised, Double-Blind, Placebo-Controlled Crossover TrialLooner TorrealbaNo ratings yet
- 2017-Journal of Paediatrics and Child HealthDocument1 page2017-Journal of Paediatrics and Child HealthAna SopaNo ratings yet
- Efficacy and Safety of SildenafilDocument9 pagesEfficacy and Safety of SildenafilArif Nurhadi AtmokoNo ratings yet
- Hypotension in Preterm Infants (HIP) Randomised Trial: Original ResearchDocument6 pagesHypotension in Preterm Infants (HIP) Randomised Trial: Original ResearchYurika Elizabeth SusantiNo ratings yet
- Neoreviews 201533Document11 pagesNeoreviews 201533Dmitri KaramazovNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- Karabulut2019 PDFDocument9 pagesKarabulut2019 PDFMuhammad Arief SaputraNo ratings yet
- TIPSDocument14 pagesTIPSNayibe Avila MNo ratings yet
- Cerebro NeonatalDocument8 pagesCerebro NeonatalRodri EspinNo ratings yet
- SDR Segun EdadDocument9 pagesSDR Segun EdadLuzbenia ChaparroNo ratings yet
- Dexmedetomidine As An Adjunct For Sedation in Patients With Traumatic Brain InjuryDocument7 pagesDexmedetomidine As An Adjunct For Sedation in Patients With Traumatic Brain InjuryMárcia SanchesNo ratings yet
- Ann Neonatol J 2021 - Effect of Phototherapy On Cardiac Functions in Neonates With Hyperbilirrubinemia. A Prospective Cross-Sectional StudyDocument19 pagesAnn Neonatol J 2021 - Effect of Phototherapy On Cardiac Functions in Neonates With Hyperbilirrubinemia. A Prospective Cross-Sectional StudyCharlie CharcapeNo ratings yet
- Neonatal Seizures: Current Management and Future ChallengesFrom EverandNeonatal Seizures: Current Management and Future ChallengesLakshmi NagarajanRating: 4 out of 5 stars4/5 (2)
- Nejmoa1800566 AppendixDocument13 pagesNejmoa1800566 Appendixjulius castelloNo ratings yet
- Ehd Ago 2020 - Tiempo de Alimentación Oral Completa Luego de NEC y Neurodesarrollo A Los 2-3 AñosDocument8 pagesEhd Ago 2020 - Tiempo de Alimentación Oral Completa Luego de NEC y Neurodesarrollo A Los 2-3 Añosjulius castelloNo ratings yet
- Jper Ago 2020 - Marcadores de Enfermedad Osea en Prematuros PDFDocument6 pagesJper Ago 2020 - Marcadores de Enfermedad Osea en Prematuros PDFjulius castelloNo ratings yet
- FP Ago 2020 - Mecanismos Moleculares y Mecánicos Que Regulan El Cierre Del Ductus en PrematurosDocument19 pagesFP Ago 2020 - Mecanismos Moleculares y Mecánicos Que Regulan El Cierre Del Ductus en Prematurosjulius castelloNo ratings yet
- Jper Ago 2020 - Marcadores de Enfermedad Osea en Prematuros PDFDocument6 pagesJper Ago 2020 - Marcadores de Enfermedad Osea en Prematuros PDFjulius castelloNo ratings yet
- Jama Ago 2020 - No Intervencion Vs Ibuprofeno Oral en PcaDocument9 pagesJama Ago 2020 - No Intervencion Vs Ibuprofeno Oral en Pcajulius castelloNo ratings yet
- Gupta2018 Article WhatIsNewInTheManagementOfChilDocument9 pagesGupta2018 Article WhatIsNewInTheManagementOfChilSatnam KaurNo ratings yet
- Infant CAP 2018Document18 pagesInfant CAP 2018julius castelloNo ratings yet
- Guías de Atención NeonatalDocument376 pagesGuías de Atención NeonatalkattvaldesNo ratings yet
- 4 Nutrition in InfancyDocument92 pages4 Nutrition in InfancyramszlaiNo ratings yet
- Sleep Tips For Older AdultsDocument9 pagesSleep Tips For Older AdultsleesinNo ratings yet
- Lacquer Thinner Safety Data SheetDocument8 pagesLacquer Thinner Safety Data SheetM.FAIZAN ARSHADNo ratings yet
- Certificate of Immunization FormDocument1 pageCertificate of Immunization FormShaikahamedNo ratings yet
- Neuro-pharmacological and analgesic effects of Arnica montana extractDocument4 pagesNeuro-pharmacological and analgesic effects of Arnica montana extractCristina Elena NicuNo ratings yet
- AMISOM Troops From The Djiboutian Contingent Donate Medical Supplies To Needy Residents in Villages in Belet WeyneDocument3 pagesAMISOM Troops From The Djiboutian Contingent Donate Medical Supplies To Needy Residents in Villages in Belet WeyneAMISOM Public Information ServicesNo ratings yet
- Pub Paediatric Imaging Manual Notes in RadiologyDocument167 pagesPub Paediatric Imaging Manual Notes in RadiologydrAlbertoVV100% (1)
- Managing Elderly Skin Care and Common ConditionsDocument46 pagesManaging Elderly Skin Care and Common ConditionsRobbyNo ratings yet
- Acitivty Sheets Q1W1 W2Document8 pagesAcitivty Sheets Q1W1 W2Christian BejarinNo ratings yet
- 08 ICSH Recommendations For Measurement of ESRDocument6 pages08 ICSH Recommendations For Measurement of ESRMuslim Majlis UojNo ratings yet
- What Is The Flu? How Is The Flu Spread?Document2 pagesWhat Is The Flu? How Is The Flu Spread?porfirio ruizNo ratings yet
- Lyme Times - Pedi LymeDocument3 pagesLyme Times - Pedi LymeVirginia Savely DNPNo ratings yet
- Managing hospitals during public health emergenciesDocument25 pagesManaging hospitals during public health emergenciesRahma YunitaNo ratings yet
- Body Plethysmography AvneetDocument54 pagesBody Plethysmography Avneetsalimtajamul100% (3)
- Teitcher 2022 Ic 220142 1657735397.32063Document3 pagesTeitcher 2022 Ic 220142 1657735397.32063Orlin ZlatarskiNo ratings yet
- J Parenter Enteral Nutr - 2017 - Worthington - When Is Parenteral Nutrition AppropriateDocument54 pagesJ Parenter Enteral Nutr - 2017 - Worthington - When Is Parenteral Nutrition AppropriateToño ZsucaritasNo ratings yet
- Filaria Tool KitDocument64 pagesFilaria Tool KitdeepikaNo ratings yet
- Nasal Spray (1222)Document11 pagesNasal Spray (1222)Kapital SenturiNo ratings yet
- 2024 ApplesDocument2 pages2024 Applesapi-335970527No ratings yet
- Telesom NewsLetter Issue 16 Mar 2013Document35 pagesTelesom NewsLetter Issue 16 Mar 2013Telesom CompanyNo ratings yet
- Lesson 6 - Anxiety-DisordersDocument74 pagesLesson 6 - Anxiety-DisordersKristian Dave DivaNo ratings yet
- Acute Suppurative Parotitis: Related SummariesDocument7 pagesAcute Suppurative Parotitis: Related SummariesFarida Dwi IrnawatiNo ratings yet
- Deficient KnowledgeDocument3 pagesDeficient KnowledgeCamilleAnneRoseRabinoNo ratings yet
- Blood and Blood SpatterDocument24 pagesBlood and Blood Spatterapi-302019977No ratings yet
- Arthropods 121228103317 Phpapp02Document110 pagesArthropods 121228103317 Phpapp02Purwaningtyas KusumaningsihNo ratings yet
- What Is A Lobotomy, History, Uses and SummaryDocument8 pagesWhat Is A Lobotomy, History, Uses and SummaryHussain AfzalNo ratings yet
- Gram-Positive & Gram-Negative Cocci: Unit 3: Neisseriaceae and Moraxella CatarrhalisDocument18 pagesGram-Positive & Gram-Negative Cocci: Unit 3: Neisseriaceae and Moraxella CatarrhalisKathleen RodasNo ratings yet
- Cell Structure and FunctionDocument31 pagesCell Structure and FunctionYoussef samehNo ratings yet
- Anatomy Lymphatic SystemDocument46 pagesAnatomy Lymphatic SystemJenise MuLatto Franklin100% (2)